Abstract
Despite significant progress in the understanding of the frontotemporal dementias (FTDs), there remains no disease-modifying treatment for these conditions, and limited effective symptomatic treatment. Behavioural variant frontotemporal dementia (bvFTD) is the most common FTD syndrome, and is characterized by severe impairments in behaviour, personality and cognition. Neuropsychiatric symptoms are common features of bvFTD but are present in the other FTD syndromes. Current treatment strategies therefore focus on ameliorating the neuropsychiatric features. Here we review the rationale for current treatments related to each of the main neuropsychiatric symptoms forming the diagnostic criteria for bvFTD relevant to all FTD subtypes, and two additional symptoms not currently part of the diagnostic criteria: lack of insight and psychosis. Given the paucity of effective treatments for these symptoms, we highlight how contributing mechanisms delineated in cognitive neuroscience may inform future approaches to clinical trials and more precise symptomatic treatments for FTDs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Current evidence-based treatments to date for neuropsychiatric symptoms of frontotemporal dementias (FTDs) modulate serotonergic and dopaminergic systems. |
Although off-label use of medications for neuropsychiatric symptoms of FTDs may provide some improvement in symptoms, often efficacy is modest at best. |
Future clinical trials aiming to treat neuropsychiatric symptoms in FTDs may consider targeting the specific underlying cognitive mechanisms and neurotransmitter systems that contribute to the symptoms and that may vary between patients. |
1 Introduction
Frontotemporal dementias (FTDs) are a group of neurodegenerative conditions featuring neurodegenerative pathology in the frontal and or temporal lobes, and hallmark impairments in behaviour and/or language. The most common type of FTD, behavioural variant FTD (bvFTD), typically affects adults < 65 years old and is characterized by severe impairments in behaviour, personality and cognition [1]. According to the International Behavioural Variant FTD Criteria Consortium (FTDC) revised diagnostic criteria, bvFTD features progressive changes in behaviour and cognition, and requires at least three of the following: behavioural disinhibition; apathy; loss of sympathy or empathy; perseverative, stereotyped or compulsive behaviours; hyperorality and dietary changes; and/or executive deficits [2]. Of significance, the revised criteria do not include the loss of insight that was originally described by Neary and colleagues and is a widely recognized feature of bvFTD [3]. The neuropsychiatric symptoms observed in bvFTD are common in these other clinical subtypes of FTD.
Frontotemporal lobar degeneration (FTLD) refers to the underlying neuropathological classification that encompasses several clinical syndromes including FTD, cortical basal syndrome (CBS), progressive supranuclear palsy syndrome (PSPS) and amyotrophic lateral sclerosis-frontotemporal spectrum disorder (ALS-FTD) (as reviewed by [1, 4]). The main FTD syndromes are bvFTD, semantic variant primary progressive aphasia (svPPA) and non-fluent variant PPA (nfvPPA) [1,2,3, 5].
The molecular subtypes of FTLD are typified by the dominant protein abnormality, which are most commonly tau, transactive response DNA binding protein of 43 kDa (TDP43), and fused in sarcoma (FUS), Ewing sarcoma protein and TATA-binding protein associated factor 15 (TAF15) (FET proteins) [6]. Recent estimates indicate that approximately 90% of FTLD are FTLD-tau or FTLD-TDP43 [6, 7]. Importantly, most cases of FTLD are sporadic, however genetic FTD syndromes account for 20% of the disease spectrum [4]. Mutations in C9orf72, progranulin (GRN) and microtubule-associated protein tau (MAPT) genes account for nearly 50% of autosomal dominant inherited FTLD [4]. In patients with symptomatic FTD, these three genetic forms of FTD are all associated with high prevalence (> 50%) of each of the core neuropsychiatric symptoms of FTD [8].
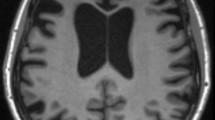
Advances in imaging have revealed patterns of network degeneration that are considered important in the pathology of bvFTD and contribute to the clinical phenotypes and overlapping symptomatology. Lesional and functional imaging studies have characterized the salience network (SN), which is important in mediating emotional and social behaviour [9], with two recent subnetworks proposed; a SN-frontotemporal network with impaired empathetic concern and hyperorality, and a SN-frontal network associated with significant executive dysfunction [10]. Patients with involvement of the semantic appraisal network (SAN), which includes the temporal pole, ventral striatum, cingulate and basolateral amygdala, exhibit disinhibition, but preserved empathy and interpersonal warmth [10]. These overarching networks are important to consider when evaluating the clinical presentation of patients with FTD and will likely be informative in more precise targeting of neuropsychiatric symptoms.
2 Search Strategy
This article reviews the structural, functional and neurochemical basis for the neuropsychiatric symptoms of FTDs, with a focus on bvFTD given the majority of treatment studies for neuropsychiatric symptoms in FTD to date have focussed on this subtype. While executive function is one of the main criteria for diagnosis, it is not discussed as it is not commonly considered a neuropsychiatric manifestation.
Medline (PubMed) and PsychINFO databases were used to search for studies of pharmacological management of neuropsychiatric symptoms of FTD. We used the following medical subject heading (MeSH) terms: FTD OR behavioural variant frontal temporal dementia OR frontotemporal lobar degeneration AND treatment OR pharmacological therapy. Each neuropsychiatric feature was added to the search query individually (i.e. behavioural disturbance OR disinhibition OR impulse control; obsessive-compulsive behaviours OR compulsions OR obsession; apathy; empathy OR prosocial behaviour; loss of insight OR self awareness; psychosis). All relevant studies between 1990 and 2021 that were published in English language were reviewed. The studies included in this review are found in Table 1.
3 Disinhibition
Abnormal, disinhibited behaviour is often an early and prominent sign of bvFTD [1, 5, 11, 12]. Disinhibited behaviours can result from dysfunction in action initiation, motivation or impaired inhibition [13,14,15,16,17]. Impulsivity is a related predisposition towards unplanned reaction to stimuli without consideration of negative consequence [18]. Patients with FTD may exhibit behavioural disinhibition in the form of impulsivity, loss of etiquette, excessive or perseverative actions, sexual inappropriateness and other transgressive behaviours such as shoplifting [19]. Examples of disinhibition we have observed in patients with FTD include approaching strangers with unwanted comments on appearance without regard for interpersonal boundaries, loss of tact in social interactions, inappropriate jocularity, and impulsive spending [20].
3.1 Structural and Functional Correlations of Disinhibition in Patients with Frontotemporal Dementia (FTD)
Studies of disinhibition in FTD have identified involvement of networks involving inferior frontal, ventromedial prefrontal cortex (VMPFC), orbital frontal cortex (OFC), anterior cingulate cortex (ACC), ventral striatum, amygdala, insula and temporal areas [21,22,23], which parallel early lesional studies of behavioural disinhibition [24,25,26]. In a study of FTLD patients, clinical measures of apathy and disinhibition were positively correlated, suggesting an interaction between these two symptoms [13]. In a functional study of FTLD, patients with a disinhibited-predominant presentation demonstrated hypometabolism based on positron emission tomography with F-18 fluorodeoxyglucose (18F-FDG-PET) in the limbic structures including the cingulate, nucleus accumbens, amygdala and hippocampus, whereas apathetic-predominant patients demonstrated more medial frontal and dorsolateral frontal hypometabolism [27]. Consideration of the cognitive roles of specific regions and networks most affected in patients with disinhibition further supports a more precise phenotypic approach when considering how to address these symptoms. The OFC has a critical role in reversal learning in which behaviour is modified by negative feedback [28, 29]. The lateral prefrontal cortex (PFC) including the OFC and insula are implicated in punishment avoidance [30]. The nucleus accumbens evaluates risk and reward, and together with the amygdala, forms key structures of the mesolimbic-ventral prefrontal-striatal dopaminergic system for motivation and goal-directed behaviour (as reviewed by [21, 31]). Specific motor response inhibition has been attributed to a network involving the right inferior gyrus, subthalamic nucleus and pre-supplementary motor area [32, 33].
3.2 Neurotransmitter Systems Associated with Disinhibition in FTD
Dysfunctional neurotransmission within the frontostriatal, mesocortical and mesolimbic circuits contribute to the disinhibition and impulsivity in bvFTD [13, 34]. Reduction in serotonin and postsynaptic receptor densities have been associated with impulsivity and depression [35]. In post-mortem studies of patients with bvFTD, serotonin 5HT1A and 5HT2A receptors were reduced in the hypothalamus, frontal and temporal cortices [36, 37]. PET studies have demonstrated reduced 5-HT2A receptor binding in bilateral ventromedial frontopolar, medial frontal, ACC and midbrain in bvFTD [27]. Dopamine dysfunction in FTD contributes to the extrapyramidal and neuropsychiatric features of FTD (as reviewed by [34]). Using single photon-emission computed tomography (SPECT), Frisoni and colleagues demonstrated reduced uptake in the frontal regions in patients with FTD as compared with Alzheimer disease (AD) [38]. The nigrostriatal dopamine deficit was demonstrated on 11 C-2-carbomethoxy-3-(4-fluorophenyl) tropane (11C-CFT) PET and likely contributes to extrapyramidal motor dysfunction [39]. In post-mortem studies, decreased dopamine was identified in the striatum of patients with FTD [40], while higher dopamine levels were detected in frontal areas as compared with patients with AD [41].
Glutamate is predominantly regarded as an excitatory neurotransmitter with physiologic roles in learning and working memory via its actions in the hippocampus and dorsolateral prefrontal cortex (DLPFC) [42,43,44]; however, excess glutaminergic function may lead to excitotoxicity [45]. In a murine human tau model, N-methyl-d-aspartate (NMDA) receptor hypofunction was correlated with repetitive and disinhibited behaviours that were ameliorated with an NMDA agonist [46]. Magnetic resonance spectroscopy (MRS) in patients with FTD demonstrated reduced glutamate and glutamine levels in the frontal and temporal areas [47, 48]. Recently, anti-GluA3 antibodies were isolated in 23% of patients with FTD [49]. The implications of the anti-GluA3 antibody in the pathogenesis of FTD is a topic of current investigation.
Gamma-aminobutyric acid (GABA) is an inhibitory neurotransmitter [50], and lower GABA levels have been detected in CSF of participants with poor stop signal reaction time [51]. Using 7 T H-MRS, Murley and colleagues demonstrated decreased GABA concentration in the right inferior frontal gyrus in patients with FTLD that was associated with impaired response inhibition on the stop signal reaction time task as compared with healthy controls [52].
3.3 Treatment Approaches to Date for Disinhibition in FTD
Following an early study demonstrating improvement in behaviour with fluoxetine, sertraline or paroxetine in 11 FTD patients [53], subsequent studies of selective serotonin reuptake inhibitors (SSRIs) in bvFTD have shown variable clinical efficacy for treating disinhibition. In a 6-week open-label study, the effects of citalopram were assessed on broad behavioural disturbances in FTD. Citalopram, titrated to 40 mg daily, reduced disinhibition as measured by the Neuropsychiatric Inventory (NPI) and Frontal Behavioural Inventory (FBI) [54]. In a single-dose, cross-over challenge study targeting impulsivity, citalopram was associated with normalization of an event-related potential metric of response inhibition during a go-no-go task, though no behavioural effect was observed [55]. In a placebo-controlled crossover study of patients with bvFTD targeting behaviour and cognition broadly, paroxetine did not improve outcomes on the NPI or Cambridge Behavioural Inventory (CBI) at 6 weeks [56]. Furthermore, paroxetine-treated patients had decreased accuracy on paired learning, reversal learning and delayed pattern recognition [56]. Trazodone is primarily a serotonin 5-HT2A antagonist and serotonin reuptake inhibitor that increases serotonin in the frontal cortex [57]. In a placebo-controlled trial evaluating neuropsychiatric behaviours in FTD, treatment with trazodone improved NPI total score and agitation at 6 weeks [58]. Subscore analysis revealed significant improvement in eating abnormalities, irritability, agitation and depressive symptoms but not disinhibition specifically [58]. In a small, placebo-controlled cross-over study, a single dose of methylphenidate reduced risk-taking on the Cambridge Gamble Task (CGT) versus placebo in patients with bvFTD [59]. The benefit was attributed to improved dopamine transmission between the midbrain and ventral striatum, and activity within the OFC; however, these results must be reproduced before general clinical recommendation [59]. In a cross-over study of eight patients with FTD comparing dextroamphetamine 20 mg and quetiapine 150 mg on a variety of behaviours in FTD, dextroamphetamine was associated with a reduction in the total NPI score in comparison to baseline, with a noted improvement in disinhibition. No treatment effect was observed with quetiapine [60]. Aripiprazole is an atypical antipsychotic that acts as an antagonist of the serotonin 5-HT2A receptor and agonist of the serotonin 5-HT1A and dopamine D2 receptors [61]. Several case reports have demonstrated some improvement in behavioural disinhibition in patients with FTD [61]. Treatment with typical and atypical antipsychotics is associated with an increased risk of cardiovascular adverse events and mortality in the elderly, as well as increased sensitivity to extrapyramidal side effects in some patients with FTD, which caution against use in patients with FTD [62, 63].
Cholinesterase inhibitors have not demonstrated consistent benefit in bvFTD. An early open-label study comparing rivastigmine or standard treatment (antipsychotic, benzodiazepine and selegiline) reported that rivastigmine improved the NPI total score, with greatest improvement in NPI agitation, appetite and eating subscales [64]. However, subsequent studies of cholinesterase inhibitors have not replicated this, with worsening observed in some behaviours. In an open trial of donepezil versus behavioural measures, patients treated with donepezil had worsening disinhibition and compulsive behaviour as measured by caregiver reports and FTD Inventory scores [65]. In a placebo-controlled extension trial of galantamine in patients with bvFTD and PPA, there was no overall difference in behaviour as indexed by FBI, Clinical Global Impression—Severity (CGI-S) or Clinical Global Impression—Improvement (CGI-I) scales; however, galantamine-treated patients in the PPA subgroup demonstrated stable language function [66].
Despite the purported role of glutamate transmission in FTD, a randomized controlled trial of memantine (NMDA receptor antagonist) assessing behaviour and cognition did not demonstrate benefit in patients with bvFTD [67]. A subsequent study of memantine demonstrated a trend of improvement on the NPI in patients with moderate to severe disease but no benefit in patients with mild disease as defined by the Mini Mental State Examination (MMSE) [68].
In a case series of three patients with FTD, improvements in agitation and behavioural symptoms were identified after treatment with lithium [69]. Importantly, a trial of lithium in PSPS and CBS was halted prematurely due to poor tolerance [70]. There is an ongoing trial of low-dose lithium for behavioural symptoms in FTD, including agitation, disinhibition and repetitive behaviours (ClinicalTrials.gov Identifier: NCT02862210).
4 Perseverative, Obsessive-Compulsive and Hoarding Behaviours
Compulsive, repetitive behaviours and hoarding are variably observed in patients with FTD, with reported rates of 5–15% for compulsive behaviours and up to 95% for behavioural stereotypies [1, 71,72,73]. These behaviours are most common in the semantic dementia and bvFTD phenotypes [72, 74]. Repetitive behaviours such as repeating words, pacing, simple motor stereotypies, unnecessary trips to the bathroom, washing and hoarding are amongst the most common types of compulsive behaviours [72, 73, 75]. On average, patients with FTD may experience fewer obsessive thoughts or pre-act anxiety than persons with obsessive compulsive disorder (OCD), suggesting these behaviours represent compulsive-impulsive spectrum rather than the typical obsessive-compulsive symptoms of OCD [73]. In our experience, patients with FTD who develop hoarding behaviours have mixed responses to removal of items, with some patients showing no concern, while others show distress typical of hoarding disorder [76].
The diagnostic criteria of bvFTD also includes eating abnormalities such as hyperphagia, changes or rigid dietary preferences, or mouthing of inedible objects [2]. These abnormal eating behaviours can resemble compulsions however may have distinct patterns and neuropathology [77]. These aberrant eating behaviours can pose significant risk to the patient and can be challenging for caregivers [78].
4.1 Structural and Functional Correlations of Obsessions and Compulsions in Patients with FTD
Significant insights into behavioural compulsions have been gained from research in OCD, which is characterized by obsessive thoughts and behavioural compulsions [76, 79, 80]. Classically, patients with OCD have altered function in the cortical-striatal-pallidal-thalamic-cortical circuit [81, 82], with involvement in the orbitofrontal, limbic, parietal, temporal, and less commonly the brainstem and cerebellum ([82,83,84,85,86,87,88], as reviewed by [89]). In a study of 11 patients with bvFTD, severity of obsessive-compulsive behaviours was correlated to volume loss in the left putamen, bilateral globus pallidus and lateral temporal lobes [75]. The authors hypothesize that the repetitive behaviours in FTD originate from dysfunctional frontotemporal areas, which may be triggered by internal or external stimuli and are not appropriately inhibited by the frontal-striatal circuit [75]. A recent neuroanatomical study of patients with FTD and obsessive-compulsive behaviours identified atrophy in bilateral amygdala, hippocampi and anterior cingulate [72]. Hoarding was uniquely associated with atrophy in the left temporal, left insula and subcortical temporal areas suggestive of a distinct neuroanatomical localization [72].
A comparative study of altered feeding behaviour in patients with bvFTD, AD and healthy controls identified lower levels of ghrelin and cortisol, and higher levels of insulin in patients with bvFTD relative to healthy controls [90]. In patients who overate, higher levels of leptin were also identified, which was hypothesized to be a compensatory response in bvFTD [90]. In a separate study, patients with svPPA and eating abnormalities had preserved hypothalamic volume but high levels of agouti-related peptide (AgRP), which is associated with hyperphagia and obesity [91, 92]. These findings suggest both shared and unique pathophysiology of compulsive and aberrant eating in FTD and point toward potential therapeutic targets for compulsive eating related to metabolic signalling pathways.
4.2 Neurotransmitter Systems Associated with the Obsessive and Compulsive Behaviours in FTD
In addition to serotonin and dopamine, as discussed above, glutamate and its role in the corticostriatal and thalamic circuit has been implicated in the pathophysiology of obsessive and compulsive behaviours [93].
4.3 Treatment Approaches To Date for Obsessive and Compulsive Behaviours in FTD
There is limited evidence for the treatment of compulsive behaviours in bvFTD. Based on their efficacy in patients with OCD, SSRIs and tricyclic antidepressants (TCAs) have been trialled with limited response. In an open-label, 12-week trial of fluvoxamine evaluating behaviours broadly in patients with FTD and semantic dementia, patients demonstrated improvement in NPI and the Stereotypy Rating Scale, with particular improvement in NPI motor behaviour, stereotypic eating and cooking behaviours, roaming, speaking and movements [94]. As mentioned above, patients treated with trazodone for 6 weeks exhibited improvement in hyperorality and eating behaviours [58]. While early studies suggested some improvement in social behaviour and eating problems with paroxetine, a subsequent controlled trial demonstrated no benefit of paroxetine in patients with FTD [56]. In an open-label trial of sertraline in 18 patients with FTD, there was noted improvement in stereotypical movement on the Abnormal Involuntary Movement Scale (AIMS) at 6 months in those with stereotypical behaviours [95].
Several medications have been described in case reports for compulsive behaviours in FTD [96]. Clomipramine is an antidepressant that prevents serotonin and norepinephrine reuptake and has been investigated in use in OCD [96, 97]. Furlan and colleagues [97] reported improvement in compulsive behaviour in a case study of three patients with bvFTD treated with clomipramine. Ciproterone, a progesterone-based anti-androgen, improved compulsive masturbation in a patient with bvFTD [98]. The combination of topiramate and fluvoxamine was associated with reduction in impulsive smoking, overeating and skin picking in a patient with FTD [99]. In a small case series, two out of three patients with FTD and abnormal eating behaviours demonstrated improvement with topiramate [100].
5 Apathy
Apathy is generally defined as a loss of motivation, resulting in diminished goal-directed behaviour (GDB), cognitive activity and affective reactivity from one’s baseline [101,102,103,104]. Apathy can be divided into cognitive, emotional and behavioural subdomains [105]. Apathy is often an early, debilitating feature of bvFTD that causes significant caregiver burden [106]. Patients with FTD may disengage from social interactions, hobbies, physical activity, and basic personal care due to apathy.
5.1 Structural and Functional Correlations of Apathy in Patients with FTD
Lesional studies have classically implicated the medial frontal, ACC and striatal regions in apathy and abulia; however, there has been expanding recognition of related subcortical structures and the underlying network failure for amotivated behaviour [107,108,109]. A review of apathy across neurodegenerative disorders identified that the frontostriatal network is most consistently affected, including the dorsal ACC, ventral striatum and nucleus accumbens [109]. In addition, degeneration of the reticular activating system may impair alertness and attention, leading to vegetative function [13].
Across patients with FTD, apathy is most consistently correlated with atrophy or hypometabolism in the OFC, ACC, ventral medial superior frontal gyrus, anterior insula, caudate and DLPFC, suggesting broad network dysfunction ([13, 21, 27, 110,111,112], see review by [104]). Apathy has been associated with cognitive and behavioural impairments in executive function, motivation, arousal, reward processing and inhibition in FTD [13, 102]. Similar to disinhibition, we propose that consideration of the different roles of these regions and associated networks may be necessary to target an individual patient’s apathy more precisely and effectively. The OFC is a main component of the limbic network, which integrates stimulus and reward via its connections to the ventral striatum, ACC, insula and uncinate fasciculus [102, 113,114,115]. Dysfunction in the ventral PFC, ACC and amygdala likely impairs the ability to evaluate social stimuli and to modify social behaviours based on affective cues [23, 114, 116, 117]. The anterior insula may contribute to motivation due to its role in perception of emotional stimuli, integration of interoceptive inputs and connection with prefrontal structures [118, 119]. In this way, the interaction of emotional function and goal-directed behaviour can be simultaneously affected in bvFTD [112]. The involvement of the DLPFC and lateral temporal areas support overlap between cognitive apathy and executive functions more broadly.
The subdomains or subtypes of apathy have been investigated in FTD and may help to explain the variability across studies using apathy as an umbrella symptom term. Specifically, poor motivation, emotional apathy, initiation apathy and cognitive apathy have been described and associated with both distinct and overlapping brain regions [104, 109, 110, 112].
5.2 Neurotransmitter Systems Associated with Apathy in FTD
The structural networks implicated in apathy are largely sub-served by the mesolimbic-mesocortical pathway, which relies primarily on dopamine afferents from the substantia nigra pars compacta, ventral tegmental area (VTA) and nigrostriatal pathways [120,121,122,123,124]. There is a nigrostriatal deficit with loss of pre-synaptic dopaminergic neurons and reduced dopamine binding in bvFTD, which may contribute to the extrapyramidal and cognitive deficits [39, 125]. Further, there are reduced D2 receptors in frontal area of patients with FTD [38]. Apathy may also arise from dysfunction of serotoninergic, cholinergic, noradrenergic neurotransmitter systems supplying the amygdala, ventral striatum and PFC [114]. While higher levels of norepinephrine were identified in neuropathological samples from patients with FTD compared with those from AD patients [41], and normal levels of noradrenergic metabolite 4-hydroxy-3-methoxy-phenylglycol (HMPG) were demonstrated in the CSF of patients with FTD [126], it is posited that norepinephrine may be modulated by irregular serotonin tone on the locus ceruleus from the raphe nuclei [127].
5.3 Treatment Approaches to Date for Apathy in FTD
While dopamine agonists have some demonstrated benefit in apathy in patients with Parkinson’s disease [128], there is considerable variability in the effect of dopamine modulation in FTD. In a cross-over trial of dextroamphetamine 20 mg and quetiapine 150 mg in eight patients with bvFTD, patients treated with dextroamphetamine had improvements from baseline in their NPI total and apathy subscale scores at 9 weeks. No significant effect was observed after treatment with quetiapine [60]. In a randomized cross-over study, 24 patients with bvFTD were randomized to agomelatine, a melatonergic agonist and antagonist of 5-HT2C receptors, at a dose of 50 mg/day or melatonin 10 mg/day for 20 weeks [129]. Patients treated with agomelatine demonstrated a reduction in apathy as measured by the Apathy Evaluation Scale (clinician version) (AES-C) and NPI-Apathy, but not the Frontal Assessment Battery (FAB) [129]. Agomelatine is posited to increase prefrontal dopaminergic and noradrenergic tone [130].
Despite case reports of improvement in apathy, agitation and anxiety with memantine [131], randomized control studies of memantine in bvFTD produced negative results [67]. Case reports have demonstrated improvement in apathy with bupropion [132] and aripiprazole [133], however these results have not been replicated. Yokukansan and Souvenaid are two nutraceutical agents that have described improvement in apathy in bvFTD, however both agents are not widely available [134, 135]. There is an ongoing randomized controlled trial of intranasal oxytocin (OT) for social apathy and empathy deficits in FTD (ClinicalTrials.gov Identifier: NCT03260920).
6 Loss of Empathy and Prosocial Behaviour
bvFTD is often characterized by early and prominent impairments in emotional processing with diminished empathy and loss of personal warmth [136, 137]. Empathy can be defined as an affective response that arises from understanding another’s emotional state [138]. Empathy is a multifaceted concept that includes affective and cognitive components [136, 139, 140], and contributes to prosocial motivation and behaviour [136, 141]. Loss of empathy is a central feature of bvFTD as patients may be unable to recognize emotional expression in others or express appropriate empathetic behaviour [136, 142, 143]. Patients may exhibit diminished responses to others’ feelings, emotional blunting, disregard for their spouse, callousness, and indifference to the harm of children.
6.1 Structural and Functional Correlations of Empathy Deficits in Patients with FTD
In neurodegenerative disorder and lesion studies, impaired empathy has been correlated most often with volume loss in the right anteromedial temporal, insula and inferior frontal structures [118, 144,145,146,147]. When compared with healthy controls, patients with bvFTD have demonstrated altered activity in response to facial expression. In particular, patients with bvFTD demonstrated decreased functional magnetic resonance imaging (fMRI) activation in the insula in response to disgusted and fearful faces; in the ventrolateral prefrontal cortex during angry stimuli; and in the amygdala when viewing happy faces [148]. Clinical trials for empathy deficits may need to consider the subcomponents of these complex behaviours, including emotion recognition, affect sharing and cognitive empathy [143, 145, 149,150,151]. Patients with bvFTD commonly have deficits in each of these facets of empathy, yet as they are subserved by both overlapping and distinct neural regions, effective treatments may need to address several separate mechanisms. A more recent facet of empathy, relevant to both empathy and apathy and targeting of underlying behavioural mechanisms in FTD, is prosocial motivation. Prosocial motivation is generally recognized as the desire to participate in helpful behaviour [152, 153]. In addition to involvement of brain regions related to cognitive empathy, it has been proposed that prosocial motivation involves a reward pathway, including the nucleus accumbens, caudate and the inferior frontal gyrus [141].
6.2 Neurotransmitter Systems Associated with Empathy Deficits in FTD
Oxytocin and vasopressin are related neuropeptides implicated in social cognition and prosocial behaviour (as reviewed by [154,155,156]). Both are synthesized in the paraventricular and supraoptic nuclei of the hypothalamus, which project to the posterior pituitary for release into the peripheral circulation and centrally to influence subcortical networks [157]. Immunohistochemical studies have identified oxytocin receptors in the hypothalamus and basal forebrain including the anterior cingulate, amygdala, olfactory nucleus, limbic and basal ganglia [157]. In contrast, more diffuse distribution of vasopressin receptors has been identified throughout the brain [158]. Oxytocin may mediate prosocial and affective behaviour by increasing trust [159] and social emotional recognition [160], but it has also been shown to increase envy [161]. When given intranasal oxytocin, healthy human participants exhibited greater fixation towards the eyes of various facial stimuli and demonstrated enhanced activation in the right posterior amygdala on fMRI. This supports a possible functional coupling of the amygdala and superior colliculus for social emotional recognition that can be enhanced with oxytocin [162]. Oxytocin has anxiolytic properties and may attenuate activation of amygdala and anterior insula due to negative social stimuli [163].
In a study of healthy males, intranasal vasopressin was shown to increase recognition of neutral facial expressions and elicited a corrugator electromyography (EMG) response similar to that induced by angry facial expressions [164]. This suggests that vasopressin may create a tendency to perceive and respond to neutral or ambiguous stimuli as though they were aggressive or threatening [164]. Current studies are underway for vasopressin receptor antagonists for autism spectrum disorder [165].
With demonstration of co-activation of dopamine (D2) and oxytocin receptors in the nucleus accumbens during pair bonding formation in voles [166], it is postulated that oxytocin may enhance the release of dopamine in the mesolimbic cortical system and foster attention and appraisal of salient stimuli (as reviewed by [167]). This is supported by the network of dopaminergic neurons in the VTA that project to the medial PFC, amygdala and nucleus accumbens [167]. The interaction of oxytocin and serotonin has been investigated in social function. For instance, recent work in mice has suggested coordinated activity of oxytocin-mediated serotonin release from the dorsal raphe nucleus to the nucleus accumbens that facilitates social reward [168]. Lower levels of oxytocin have been identified in children with autism spectrum disorder and impaired social function [169] and there is ongoing work investigating the reciprocal interaction of serotonin and oxytocin in social function [170].
6.3 Treatment Approaches to Date for Empathy Deficits in FTD
There have been recent investigations into the use of oxytocin to improve the social behaviours, specifically empathy and social apathy, in FTD. In a phase II study, the safety and tolerability of oxytocin therapy was established at three doses (24, 48 and 72 units) given twice daily to patients with FTD over 1 week [171]. This was followed by a randomized placebo-controlled crossover trial in which patients with bvFTD were given oxytocin 72 units intranasally or placebo, and performed behaviour tests including the Behavioural View and Imitate Task, Multifaceted Empathy Test (MET) and Postural Knowledge Test (PKT) [172, 173]. These patients also took part in instructed behavioural mimicry of facial expressions during fMRI. After oxytocin treatment, there was a noted increased fMRI activation in the frontal, bilateral anterior insula, inferior frontal gyrus, caudate, right anterior cingulate and inferior parietal areas. Despite demonstrated improvement in activation on imaging, there were inconsistent results on clinical testing. Patients treated with placebo provided high ratings of empathic concern on MET versus those on oxytocin. However, patients on oxytocin were more accurate on the PKT than those on placebo [173]. As noted above, an ongoing randomized control trial (RCT) will evaluate whether repeated administration of intranasal oxytocin is associated with reduction of empathy deficits in patients with FTD.
7 Loss of Insight
Early loss of insight is a common feature in patients with FTD [3, 174]. Despite drastic changes in personality and behaviour, patients with FTD are unable to appreciate their deficits and thus minimize related consequences. In clinic, patients may dismiss behavioural irregularities, contest accounts from concerned caregivers, and resist treatment and behavioural interventions. Patients with bvFTD more consistently demonstrate impairments in insight compared with patients with svPPA, nfvPPA or logopenic PPA [175, 176].
7.1 Structural and Functional Correlations of Lack of Insight in Patients with FTD
Classical lesional studies identified neglect and impaired awareness of motor deficits with non-dominant parietal injury [177]. In healthy participants, there is increased right DLPFC activation during self-appraisal tasks [178]. In patients with FTD, anosognosia or the lack of awareness about one’s illness has been generally associated with dysfunction in the right frontotemporal areas [179], with more recent evidence suggesting that insight and self awareness may be distributed across several brain regions (as reviewed by [176]). The SAN has recently been proposed to mediate personal evaluation. This network includes the temporal pole, ventral striatum, subgenual cingulate, amygdala, caudate, OFC and nucleus accumbens [9, 10]. Studies of self-appraisal, insight and self-awareness in FTD have identified correlations with atrophy mainly in the OFC, ACC, insula, ventromedial and frontopolar prefrontal cortex [175, 176, 180, 181].
The ACC is involved in self-regulation, error monitoring and facilitates self-reference [182, 183]. The medial OFC is implicated in valuating present stimulus reward while the lateral OFC is required in updating outcome and reward associations [115, 184], thus errors in behaviour monitoring or outcome valuation may lead to overall impairment of self awareness. Poor self-appraisal has been associated with loss of grey matter density in the VMPFC and cingulate cortices [183, 185]. The medial PFC may have a crucial role in self reflection and evaluation, and likely mediates semantic knowledge about self [180]. This is consistent with previous work on self-referential behaviour that implicates the cortical midline structures [186].
7.2 Treatment Approaches to Date for Lack of Insight in FTD
Treatment approaches for impaired insight are lacking in FTD. Non-pharmacological interventions such as cognitive behavioural therapy, motivational interviewing and social skills training have been used with some benefit on insight in patients with schizophrenia [187]. There have been no such trials to date in FTD.
8 Psychosis
Psychosis can occur in FTD and contributes to diagnostic and treatment challenges [188]. In a cohort study of 22 patients with bvFTD, positive psychotic features including delusions and hallucinations occurred in 22% of patients, while the majority of these patients had at least one negative feature of psychosis such as blunted affect and withdrawal (95%) or formal thought disorder (81%) [189]. Within genetic FTD, patients with mutations in MAPT, GRN and especially those with C9orf72 repeat expansions appear to be at higher risk of psychosis [190,191,192,193]. A recent neuropathological analysis revealed patients with FTLD-TDP43 were more likely to have early delusions of misidentification, grandiosity or erotomania than FTLD-tau [192]. In patients with GRN mutations, psychotic features correlated with grey matter atrophy in the anterior insula, left thalamus, cerebellum, frontal, parietal and occipital areas [194]. In C9orf72 repeat expansion carriers, delusions appeared to correlate with left frontal cortical atrophy [194]. An older clinicopathological study demonstrated that patients with C9orf72 repeat expansions and delusions had greater left parietal precuneus atrophy and FTD-TDP pathology [195]. The cognitive mechanisms underlying these varied psychotic phenomenon in FTD have not yet been delineated.
8.1 Treatment Approaches to Date for Psychosis in FTD
Treatment with typical antipsychotic medications may exacerbate extrapyramidal symptoms in FTD given the pre-existing dopamine deficit [196]. Typical antipsychotics may also pose an increased risk of cerebrovascular events and overall mortality in patients with dementia. Thus, atypical antipsychotics such as quetiapine, olanzapine and clozapine are preferred [34, 62, 191]. In a large RCT of aripiprazole in AD, improvement on the NPI-NH psychosis subscale was observed; however, significant adverse events including agitation, asthenia and cerebrovascular events were identified in the treatment arm [197]. Recently, pimavanserin, an inverse agonist and antagonist of serotonin 5-HT2A receptors, demonstrated benefit in a randomized, placebo-controlled study in dementia-related psychosis including patients with FTD [198]. Given the higher prevalence of psychotic features in genetic FTD, there are opportunities for exploring genetic therapies in the remedy of psychosis in FTD.
9 Conclusion
The neuropsychiatric symptoms of FTD are myriad. Thus far, despite numerous promising case reports and open-label trials, effective symptomatic treatments have largely been elusive. We propose the heterogeneity of cognitive mechanisms giving rise to each of the current core neuropsychiatric symptoms needs to be modeled in future clinical trial designs. For example, a patient with FTD may demonstrate disinhibition due to poor response inhibition, reduced sensitivity to negative feedback, heighted valuation of a reward, or some combination thereof. Each of these mechanisms may be mediated by distinct circuits and neurotransmitters. Information on the functional and structural integrity of the neural regions supporting each of the core cognitive functions, and possibly genotyping related to neurotransmitter system function, may further improve predictions regarding patient’s response to a specific treatment. Further research is required to delineate these cognitive models and their specific associations with neuropsychiatric symptoms in FTD. Additionally, the vast majority of clinical trials to date in FTD have not specifically considered the interaction between the target symptom and other neuropsychiatric symptoms. Consideration and evaluation of such potential symptom interactions may provide additional clues as to the common cognitive deficits underlying the symptoms, and therefore key targets, as well as more precise modelling of individual treatment responses.
References
Bang J, Spina S, Miller BL. Frontotemporal dementia. Lancet Lond Engl. 2015;386:1672–82.
Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011;134:2456–77.
Neary D, Snowden JS, Gustafson L, Passant U, Stuss D, Black S, et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology. 1998;51:1546–54.
Rosen HJ, Boeve BF, Boxer AL. Tracking disease progression in familial and sporadic frontotemporal lobar degeneration: recent findings from ARTFL and LEFFTDS. Alzheimers Dement. 2020;16:71–8.
Snowden JS, Bathgate D, Varma A, Blackshaw A, Gibbons ZC, Neary D. Distinct behavioural profiles in frontotemporal dementia and semantic dementia. J Neurol Neurosurg Psychiatry. 2001;70:323–32.
Young JJ, Lavakumar M, Tampi D, Balachandran S, Tampi RR. Frontotemporal dementia: latest evidence and clinical implications. Ther Adv Psychopharmacol. 2018;8:33–48.
Panza F, Lozupone M, Seripa D, Daniele A, Watling M, Giannelli G, et al. Development of disease-modifying drugs for frontotemporal dementia spectrum disorders. Nat Rev Neurol. 2020;16:213–28.
Benussi A, Premi E, Gazzina S, Brattini C, Bonomi E, Alberici A, et al. Progression of behavioral disturbances and neuropsychiatric symptoms in patients with genetic frontotemporal dementia. JAMA Netw Open. 2021;4: e2030194.
Seeley WW, Allman JM, Carlin DA, Crawford RK, Macedo MN, Greicius MD, et al. Divergent social functioning in behavioral variant frontotemporal dementia and Alzheimer disease: reciprocal networks and neuronal evolution. Alzheimer Dis Assoc Disord. 2007;21:S50-57.
Ranasinghe KG, Rankin KP, Pressman PS, Perry DC, Lobach IV, Seeley WW, et al. Distinct subtypes of behavioral variant frontotemporal dementia based on patterns of network degeneration. JAMA Neurol. 2016;73:1078–88.
Hodges JR. Frontotemporal dementia (Pick’s disease): clinical features and assessment. Neurology. 2001;56:S6-10.
Borroni B, Grassi M, Premi E, Gazzina S, Alberici A, Cosseddu M, et al. Neuroanatomical correlates of behavioural phenotypes in behavioural variant of frontotemporal dementia. Behav Brain Res. 2012;235:124–9.
Lansdall CJ, Coyle-Gilchrist ITS, Jones PS, Vázquez Rodríguez P, Wilcox A, Wehmann E, et al. Apathy and impulsivity in frontotemporal lobar degeneration syndromes. Brain. 2017;140:1792–807.
Robbins TW. Shifting and stopping: fronto-striatal substrates, neurochemical modulation and clinical implications. Philos Trans R Soc B Biol Sci. 2007;362:917–32.
Devinsky O, Morrell MJ, Vogt BA. Contributions of anterior cingulate cortex to behaviour. Brain J Neurol. 1995;118(Pt 1):279–306.
Brewer JA, Potenza MN. The neurobiology and genetics of impulse control disorders: relationships to drug addictions. Biochem Pharmacol. 2008;75:63–75.
Fineberg NA, Potenza MN, Chamberlain SR, Berlin HA, Menzies L, Bechara A, et al. Probing compulsive and impulsive behaviors, from animal models to endophenotypes: a narrative review. Neuropsychopharmacology. 2010;35:591–604.
Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, Swann AC. Psychiatric aspects of impulsivity. Am J Psychiatry. 2001;158:1783–93.
Liljegren M, Landqvist Waldö M, Frizell Santillo A, Ullén S, Rydbeck R, Miller B, et al. Association of neuropathologically confirmed frontotemporal dementia and alzheimer disease with criminal and socially inappropriate behavior in a swedish cohort. JAMA Netw Open. 2019;2: e190261.
Finger EC. Frontotemporal dementias. Contin Minneap Minn. 2016;22:464–89.
Zamboni G, Huey ED, Krueger F, Nichelli PF, Grafman J. Apathy and disinhibition in frontotemporal dementia: Insights into their neural correlates. Neurology. 2008;71:736–42.
Sheelakumari R, Bineesh C, Varghese T, Kesavadas C, Verghese J, Mathuranath PS. Neuroanatomical correlates of apathy and disinhibition in behavioural variant frontotemporal dementia. Brain Imaging Behav. 2020;14:2004–11.
Passamonti L, Lansdall C, Rowe J. The neuroanatomical and neurochemical basis of apathy and impulsivity in frontotemporal lobar degeneration. Curr Opin Behav Sci. 2018;22:14–20.
Harlow JM. Recovery from the passage of an iron bar through the head. Hist Psychiatry. 1993;4:274–81.
Cummings JL. Anatomic and behavioral aspects of frontal-subcortical circuits. Ann N Y Acad Sci. 1995;769:1–13.
Bechara A, Tranel D, Damasio H. Characterization of the decision-making deficit of patients with ventromedial prefrontal cortex lesions. Brain. 2000;123:2189–202.
Franceschi M, Anchisi D, Pelati O, Zuffi M, Matarrese M, Moresco RM, et al. Glucose metabolism and serotonin receptors in the frontotemporal lobe degeneration. Ann Neurol. 2005;57:216–25.
Dias R, Robbins TW, Roberts AC. Dissociation in prefrontal cortex of affective and attentional shifts. Nature. 1996;380:69–72.
Chamberlain SR, Müller U, Blackwell AD, Clark L, Robbins TW, Sahakian BJ. Neurochemical modulation of response inhibition and probabilistic learning in humans. Science. 2006;311:861–3.
Jean-Richard-Dit-Bressel P, McNally GP. Lateral, not medial, prefrontal cortex contributes to punishment and aversive instrumental learning. Learn Mem. 2016;23:607–17.
Morgane PJ, Galler JR, Mokler DJ. A review of systems and networks of the limbic forebrain/limbic midbrain. Prog Neurobiol. 2005;75:143–60.
Rubia K, Smith AB, Brammer MJ, Taylor E. Right inferior prefrontal cortex mediates response inhibition while mesial prefrontal cortex is responsible for error detection. Neuroimage. 2003;20:351–8.
Aron AR, Behrens TE, Smith S, Frank MJ, Poldrack RA. Triangulating a cognitive control network using diffusion-weighted magnetic resonance imaging (MRI) and functional MRI. J Neurosci. 2007;27:3743–52.
Murley AG, Rowe JB. Neurotransmitter deficits from frontotemporal lobar degeneration. Brain J Neurol. 2018;141:1263–85.
Huey ED, Putnam KT, Grafman J. A systematic review of neurotransmitter deficits and treatments in frontotemporal dementia. Neurology. 2006;66:17–22.
Sparks DL, Markesbery WR. Altered serotonergic and cholinergic synaptic markers in Pick’s disease. Arch Neurol. 1991;48:796–9.
Bowen DM, Procter AW, Mann DMA, Snowden JS, Esiri MM, Neary D, et al. Imbalance of a serotonergic system in frontotemporal dementia: implication for pharmacotherapy. Psychopharmacology. 2008;196:603–10.
Frisoni GB, Pizzolato G, Bianchetti A, Chierichetti F, Ferlin G, Battistin L, et al. Single photon emission computed tomography with [99Tc]-HM-PAO and [123I]-IBZM in Alzheimer’s disease and dementia of frontal type: preliminary results. Acta Neurol Scand. 1994;89:199–203.
Rinne JO, Laine M, Kaasinen V, Norvasuo-Heilä MK, Någren K, Helenius H. Striatal dopamine transporter and extrapyramidal symptoms in frontotemporal dementia. Neurology. 2002;58:1489–93.
Kanazawa I, Kwak S, Sasaki H, Muramoto O, Mizutani T, Hori A, et al. Studies on neurotransmitter markers of the basal ganglia in Pick’s disease, with special reference to dopamine reduction. J Neurol Sci. 1988;83:63–74.
Vermeiren Y, Janssens J, Aerts T, Martin J-J, Sieben A, Van Dam D, et al. Brain serotonergic and noradrenergic deficiencies in behavioral variant frontotemporal dementia compared to early-onset Alzheimer’s disease. J Alzheimers Dis. 2016;53:1079–96.
Hollmann M, Heinemann S. Cloned glutamate receptors. Annu Rev Neurosci. 1994;17:31–108.
Erecińska M, Silver IA. Metabolism and role of glutamate in mammalian brain. Prog Neurobiol. 1990;35:245–96.
Woodcock EA, Anand C, Khatib D, Diwadkar VA, Stanley JA. Working memory modulates glutamate levels in the dorsolateral prefrontal cortex during 1H fMRS. Front Psychiatry. 2018. https://doi.org/10.3389/fpsyt.2018.00066.
Wong PC, Cai H, Borchelt DR, Price DL. Genetically engineered mouse models of neurodegenerative diseases. Nat Neurosci. 2002;5:633–9.
Warmus BA, Sekar DR, McCutchen E, Schellenberg GD, Roberts RC, McMahon LL, et al. Tau-mediated NMDA receptor impairment underlies dysfunction of a selectively vulnerable network in a mouse model of frontotemporal dementia. J Neurosci. 2014;34:16482–95.
Ernst T, Chang L, Melchor R, Mehringer CM. Frontotemporal dementia and early Alzheimer disease: differentiation with frontal lobe H-1 MR spectroscopy. Radiology. 1997;203:829–36.
Sarac H, Zagar M, Vranjes D, Henigsberg N, Bilić E, Pavlisa G. Magnetic resonance imaging and magnetic resonance spectroscopy in a patient with amyotrophic lateral sclerosis and frontotemporal dementia. Coll Antropol. 2008;32(Suppl 1):205–10.
Borroni B, Stanic J, Verpelli C, Mellone M, Bonomi E, Alberici A, et al. Anti-AMPA GluA3 antibodies in Frontotemporal dementia: a new molecular target. Sci Rep. 2017. https://doi.org/10.1038/s41598-017-06117-y.
Curtis DR, Watkins JC. The pharmacology of amino acids related to gamma-aminobutyric acid. Pharmacol Rev. 1965;17:347–91.
Hermans L, Leunissen I, Pauwels L, Cuypers K, Peeters R, Puts NAJ, et al. Brain GABA levels are associated with inhibitory control deficits in older adults. J Neurosci. 2018;38:7844–51.
Murley AG, Rouse MA, Jones PS, Ye R, Hezemans FH, O’Callaghan C, et al. GABA and glutamate deficits from frontotemporal lobar degeneration are associated with disinhibition. Brain. 2020;143:3449–62.
Swartz JR, Miller BL, Lesser IM, Darby AL. Frontotemporal dementia: treatment response to serotonin selective reuptake inhibitors. J Clin Psychiatry. 1997;58:212–6.
Herrmann N, Black SE, Chow T, Cappell J, Tang-Wai DF, Lanctôt KL. Serotonergic function and treatment of behavioral and psychological symptoms of frontotemporal dementia. Am J Geriatr Psychiatry. 2012;20:789–97.
Hughes LE, Rittman T, Regenthal R, Robbins TW, Rowe JB. Improving response inhibition systems in frontotemporal dementia with citalopram. Brain J Neurol. 2015;138:1961–75.
Deakin JB, Rahman S, Nestor PJ, Hodges JR, Sahakian BJ. Paroxetine does not improve symptoms and impairs cognition in frontotemporal dementia: a double-blind randomized controlled trial. Psychopharmacology. 2004;172:400–8.
Stahl SM. Mechanism of action of trazodone: a multifunctional drug. CNS Spectr. 2009;14:536–46.
Lebert F, Stekke W, Hasenbroekx C, Pasquier F. Frontotemporal dementia: a randomised, controlled trial with trazodone. Dement Geriatr Cogn Disord. 2004;17:355–9.
Rahman S, Robbins TW, Hodges JR, Mehta MA, Nestor PJ, Clark L, et al. Methylphenidate (‘Ritalin’) can ameliorate abnormal risk-taking behavior in the frontal variant of frontotemporal dementia. Neuropsychopharmacology. 2006;31:651–8.
Huey ED, Garcia C, Wassermann EM, Tierney MC, Grafman J. Stimulant treatment of frontotemporal dementia in 8 patients. J Clin Psychiatry. 2008;69:1981–2.
Reeves RR, Perry CL. Aripiprazole for sexually inappropriate vocalizations in frontotemporal dementia. J Clin Psychopharmacol. 2013;33:145–6.
Kuehn BM. FDA warns antipsychotic drugs may be risky for elderly. JAMA. 2005;293:2462.
Czarnecki K, Kumar N, Josephs KA. Parkinsonism and tardive antecollis in frontotemporal dementia–increased sensitivity to newer antipsychotics? Eur J Neurol. 2008;15:199–201.
Moretti R, Torre P, Antonello RM, Cattaruzza T, Cazzato G, Bava A. Rivastigmine in frontotemporal dementia: an open-label study. Drugs Aging. 2004;21:931–7.
Mendez MF, Shapira JS, McMurtray A, Licht E. Preliminary findings: behavioral worsening on donepezil in patients with frontotemporal dementia. Am J Geriatr Psychiatry. 2007;15:84–7.
Kertesz A, Morlog D, Light M, Blair M, Davidson W, Jesso S, et al. Galantamine in frontotemporal dementia and primary progressive aphasia. Dement Geriatr Cogn Disord. 2008;25:178–85.
Boxer AL, Knopman DS, Kaufer DI, Grossman M, Onyike C, Graf-Radford N, et al. Memantine in patients with frontotemporal lobar degeneration: a multicentre, randomised, double-blind, placebo-controlled trial. Lancet Neurol. 2013;12:149–56.
Li P, Quan W, Zhou Y-Y, Wang Y, Zhang H-H, Liu S. Efficacy of memantine on neuropsychiatric symptoms associated with the severity of behavioral variant frontotemporal dementia: a six-month, open-label, self-controlled clinical trial. Exp Ther Med. 2016;12:492–8.
Devanand DP, Pelton GH, D’Antonio K, Strickler JG, Kreisl WC, Noble J, et al. Low-dose lithium treatment for agitation and psychosis in Alzheimer’s disease and frontotemporal dementia: a case series. Alzheimer Dis Assoc Disord. 2017;31:73–5.
Gonin R. A pilot trial of lithium in subjects with progressive supranuclear palsy or corticobasal degeneration | National Institute of Neurological Disorders and Stroke. 2015. https://www.ninds.nih.gov/Disorders/Clinical-Trials/Pilot-Trial-Lithium-Subjects-Progressive-Supranuclear-Palsy-or. Accessed 26 Apr 2021
Ames D, Cummings JL, Wirshing WC, Quinn B, Mahler M. Repetitive and compulsive behavior in frontal lobe degenerations. J Neuropsychiatry Clin Neurosci. 1994;6:100–13.
Mitchell E, Tavares TP, Palaniyappan L, Finger EC. Hoarding and obsessive-compulsive behaviours in frontotemporal dementia: clinical and neuroanatomic associations. Cortex. 2019;121:443–53.
Moheb N, Charuworn K, Ashla MM, Desarzant R, Chavez D, Mendez MF. Repetitive behaviors in frontotemporal dementia: compulsions or impulsions? J Neuropsychiatry Clin Neurosci. 2019;31:132–6.
Bozeat S, Gregory CA, Ralph MA, Hodges JR. Which neuropsychiatric and behavioural features distinguish frontal and temporal variants of frontotemporal dementia from Alzheimer’s disease? J Neurol Neurosurg Psychiatry. 2000;69:178–86.
Perry DC, Whitwell JL, Boeve BF, Pankratz VS, Knopman DS, Petersen RC, et al. Voxel-based morphometry in patients with obsessive-compulsive behaviors in behavioral variant frontotemporal dementia. Eur J Neurol. 2012;19:911–7.
American Psychiatric Association. Obsessive-compulsive and related disorders. In: Diagnostic and statistical manual of mental disorders. 5th ed. American Psychiatric Association; 2013. https://doi.org/10.1176/appi.books.9780890425596.dsm06
Ahmed RM, Irish M, Henning E, Dermody N, Bartley L, Kiernan MC, et al. Assessment of eating behavior disturbance and associated neural networks in frontotemporal dementia. JAMA Neurol. 2016;73:282–90.
Piguet O. Eating disturbance in behavioural-variant frontotemporal dementia. J Mol Neurosci MN. 2011;45:589–93.
Leckman JF, Denys D, Simpson HB, Mataix-Cols D, Hollander E, Saxena S, et al. Obsessive-compulsive disorder: a review of the diagnostic criteria and possible subtypes and dimensional specifiers for DSM-V. Depress Anxiety. 2010;27:507–27.
Stein DJ, Kogan CS, Atmaca M, Fineberg NA, Fontenelle LF, Grant JE, et al. The classification of obsessive-compulsive and related disorders in the ICD-11. J Affect Disord. 2016;190:663–74.
Saxena S, Brody AL, Schwartz JM, Baxter LR. Neuroimaging and frontal-subcortical circuitry in obsessive-compulsive disorder. Br J Psychiatry Suppl. 1998;35:26–37.
Menzies L, Chamberlain SR, Laird AR, Thelen SM, Sahakian BJ, Bullmore ET. Integrating evidence from neuroimaging and neuropsychological studies of obsessive-compulsive disorder: the orbitofronto-striatal model revisited. Neurosci Biobehav Rev. 2008;32:525–49.
Baxter LR, Phelps ME, Mazziotta JC, Guze BH, Schwartz JM, Selin CE. Local cerebral glucose metabolic rates in obsessive-compulsive disorder. A comparison with rates in unipolar depression and in normal controls. Arch Gen Psychiatry. 1987;44:211–8.
Kwon JS, Kim J-J, Lee DW, Lee JS, Lee DS, Kim M-S, et al. Neural correlates of clinical symptoms and cognitive dysfunctions in obsessive-compulsive disorder. Psychiatry Res. 2003;122:37–47.
Whiteside SP, Port JD, Abramowitz JS. A meta–analysis of functional neuroimaging in obsessive–compulsive disorder. Psychiatry Res Neuroimaging. 2004;132:69–79.
Szeszko PR, Robinson D, Alvir JM, Bilder RM, Lencz T, Ashtari M, et al. Orbital frontal and amygdala volume reductions in obsessive-compulsive disorder. Arch Gen Psychiatry. 1999;56:913–9.
Figee M, Luigjes J, Smolders R, Valencia-Alfonso C-E, van Wingen G, de Kwaasteniet B, et al. Deep brain stimulation restores frontostriatal network activity in obsessive-compulsive disorder. Nat Neurosci. 2013;16:386–7.
Rasgon A, Lee WH, Leibu E, Laird A, Glahn D, Goodman W, et al. Neural correlates of affective and non-affective cognition in obsessive compulsive disorder: a meta-analysis of functional imaging studies. Eur Psychiatry. 2017;46:25–32.
Stein DJ, Costa DLC, Lochner C, Miguel EC, Reddy YCJ, Shavitt RG, et al. Obsessive–compulsive disorder. Nat Rev Dis Primer. 2019;5:1–21.
Woolley JD, Khan BK, Natesan A, Karydas A, Dallman M, Havel P, et al. Satiety-related hormonal dysregulation in behavioral variant frontotemporal dementia. Neurology. 2014;82:512–20.
Ahmed RM, Latheef S, Bartley L, Irish M, Halliday GM, Kiernan MC, et al. Eating behavior in frontotemporal dementia: peripheral hormones vs hypothalamic pathology. Neurology. 2015;85:1310–7.
Graham M, Shutter JR, Sarmiento U, Sarosi I, Stark KL. Overexpression of Agrt leads to obesity in transgenic mice. Nat Genet. 1997;17:273–4.
Wu K, Hanna GL, Rosenberg DR, Arnold PD. The role of glutamate signalling in the pathogenesis and treatment of obsessive-compulsive disorder. Pharmacol Biochem Behav. 2012;100:726–35.
Ikeda M, Shigenobu K, Fukuhara R, Hokoishi K, Maki N, Nebu A, et al. Efficacy of fluvoxamine as a treatment for behavioral symptoms in frontotemporal lobar degeneration patients. Dement Geriatr Cogn Disord. 2004;17:117–21.
Mendez MF, Shapira JS, Miller BL. Stereotypical movements and frontotemporal dementia. Mov Disord. 2005;20:742–5.
Ackerman DL, Greenland S. Multivariate meta-analysis of controlled drug studies for obsessive-compulsive disorder. J Clin Psychopharmacol. 2002;22:309–17.
Furlan JC, Henri-Bhargava A, Freedman M. Clomipramine in the treatment of compulsive behavior in frontotemporal dementia: a case series. Alzheimer Dis Assoc Disord. 2014;28:95–8.
Fonseca L, Simões S, Ferreira P, Mesquita J, Machado A. Ciproterone effect on compulsive masturbation in a frontotemporal dementia patient. J Neuropsychiatry Clin Neurosci. 2010;22:352.e3.
Pompanin S, Jelcic N, Cecchin D, Cagnin A. Impulse control disorders in frontotemporal dementia: spectrum of symptoms and response to treatment. Gen Hosp Psychiatry. 2014;36(760):e5-7.
Shinagawa S, Tsuno N, Nakayama K. Managing abnormal eating behaviours in frontotemporal lobar degeneration patients with topiramate. Psychogeriatrics. 2013;13:58–61.
Robert P, Onyike CU, Leentjens AFG, Dujardin K, Aalten P, Starkstein S, et al. Proposed diagnostic criteria for apathy in Alzheimer’s disease and other neuropsychiatric disorders. Eur Psychiatry. 2009;24:98–104.
Massimo L, Powers JP, Evans LK, McMillan CT, Rascovsky K, Eslinger P, et al. Apathy in frontotemporal degeneration: neuroanatomical evidence of impaired goal-directed behavior. Front Hum Neurosci. 2015. https://doi.org/10.3389/fnhum.2015.00611.
Husain M, Roiser JP. Neuroscience of apathy and anhedonia: a transdiagnostic approach. Nat Rev Neurosci. 2018;19:470–84.
Ducharme S, Price BH, Dickerson BC. Apathy: a neurocircuitry model based on frontotemporal dementia. J Neurol Neurosurg Psychiatry. 2018;89:389–96.
Levy R, Dubois B. Apathy and the functional anatomy of the prefrontal cortex-basal ganglia circuits. Cereb Cortex N Y N. 1991;2006(16):916–28.
Merrilees J, Dowling GA, Hubbard E, Mastick J, Ketelle R, Miller BL. Characterization of apathy in persons with frontotemporal dementia and the impact on family caregivers. Alzheimer Dis Assoc Disord. 2013;27:62–7.
Cohen RA, Kaplan RF, Zuffante P, Moser DJ, Jenkins MA, Salloway S, et al. Alteration of intention and self-initiated action associated with bilateral anterior cingulotomy. J Neuropsychiatry Clin Neurosci. 1999;11:444–53.
Siegel JS, Snyder AZ, Metcalf NV, Fucetola RP, Hacker CD, Shimony JS, et al. The circuitry of abulia: Insights from functional connectivity MRI. NeuroImage Clin. 2014;6:320–6.
Le Heron C, Apps MAJ, Husain M. The anatomy of apathy: a neurocognitive framework for amotivated behaviour. Neuropsychologia. 2018;118:54–67.
Kumfor F, Zhen A, Hodges JR, Piguet O, Irish M. Apathy in Alzheimer’s disease and frontotemporal dementia: distinct clinical profiles and neural correlates. Cortex. 2018;103:350–9.
Rosen HJ, Allison SC, Schauer GF, Gorno-Tempini ML, Weiner MW, Miller BL. Neuroanatomical correlates of behavioural disorders in dementia. Brain J Neurol. 2005;128:2612–25.
Wei G, Irish M, Hodges JR, Piguet O, Kumfor F. Disease-specific profiles of apathy in Alzheimer’s disease and behavioural-variant frontotemporal dementia differ across the disease course. J Neurol. 2019. https://doi.org/10.1007/s00415-019-09679-1.
Hare TA, Camerer CF, Knoepfle DT, O’Doherty JP, Rangel A. Value computations in ventral medial prefrontal cortex during charitable decision making incorporate input from regions involved in social cognition. J Neurosci. 2010;30:583–90.
Pagonabarraga J, Kulisevsky J, Strafella AP, Krack P. Apathy in Parkinson’s disease: clinical features, neural substrates, diagnosis, and treatment. Lancet Neurol. 2015;14:518–31.
Rolls ET, Cheng W, Feng J. The orbitofrontal cortex: reward, emotion and depression. Brain Commun. 2020;2:fcaa196.
Cardinal RN, Parkinson JA, Hall J, Everitt BJ. Emotion and motivation: the role of the amygdala, ventral striatum, and prefrontal cortex. Neurosci Biobehav Rev. 2002;26:321–52.
Marschner A, Mell T, Wartenburger I, Villringer A, Reischies FM, Heekeren HR. Reward-based decision-making and aging. Brain Res Bull. 2005;67:382–90.
Craig ADB. How do you feel–now? The anterior insula and human awareness. Nat Rev Neurosci. 2009;10:59–70.
Critchley HD. Neural mechanisms of autonomic, affective, and cognitive integration. J Comp Neurol. 2005;493:154–66.
Schultz W. Predictive reward signal of dopamine neurons. J Neurophysiol. 1998;80:1–27.
Schultz W. Dopamine signals for reward value and risk: basic and recent data. Behav Brain Funct. 2010;6:24.
Wise RA. Dopamine, learning and motivation. Nat Rev Neurosci. 2004;5:483–94.
Björklund A, Dunnett SB. Dopamine neuron systems in the brain: an update. Trends Neurosci. 2007;30:194–202.
Grace AA, Floresco SB, Goto Y, Lodge DJ. Regulation of firing of dopaminergic neurons and control of goal-directed behaviors. Trends Neurosci. 2007;30:220–7.
Kertesz A, McMonagle P, Jesso S. Extrapyramidal syndromes in frontotemporal degeneration. J Mol Neurosci. 2011;45:336–42.
Sjögren M, Minthon L, Passant U, Blennow K, Wallin A. Decreased monoamine metabolites in frontotemporal dementia and Alzheimer’s disease. Neurobiol Aging. 1998;19:379–84.
Yang Y, Schmitt HP. Frontotemporal dementia: evidence for impairment of ascending serotoninergic but not noradrenergic innervation. Immunocytochemical and quantitative study using a graph method. Acta Neuropathol (Berl). 2001;101:256–70.
Mele B, Van S, Holroyd-Leduc J, Ismail Z, Pringsheim T, Goodarzi Z. Diagnosis, treatment and management of apathy in Parkinson’s disease: a scoping review. BMJ Open. 2020;10: e037632.
Callegari I, Mattei C, Benassi F, Krueger F, Grafman J, Yaldizli Ö, et al. Agomelatine improves apathy in frontotemporal dementia. Neurodegener Dis. 2016;16:352–6.
Racagni G, Riva MA, Molteni R, Musazzi L, Calabrese F, Popoli M, et al. Mode of action of agomelatine: synergy between melatonergic and 5-HT2C receptors. World J Biol Psychiatry. 2011;12:574–87.
Swanberg MM. Memantine for behavioral disturbances in frontotemporal dementia: a case series. Alzheimer Dis Assoc Disord. 2007;21:164–6.
Lin C-P, Chu C-P, Liu H-C. Bupropion improved apathy in behavioral variant frontotemporal dementia: a case report. Neurocase. 2016;22:466–8.
Fellgiebel DA, Müller MJ, Hiemke C, Bartenstein P, Schreckenberger M. Clinical improvement in a case of frontotemporal dementia under aripiprazole treatment corresponds to partial recovery of disturbed frontal glucose metabolism. World J Biol Psychiatry. 2007;8:123–6.
Kimura T, Hayashida H, Furukawa H, Takamatsu J. Pilot study of pharmacological treatment for frontotemporal dementia: effect of Yokukansan on behavioral symptoms. Psychiatry Clin Neurosci. 2010;64:207–10.
Pardini M, Serrati C, Guida S, Mattei C, Abate L, Massucco D, et al. Souvenaid reduces behavioral deficits and improves social cognition skills in frontotemporal dementia: a proof-of-concept study. Neurodegener Dis. 2015;15:58–62.
Rankin KP, Kramer JH, Miller BL. Patterns of cognitive and emotional empathy in frontotemporal lobar degeneration. Cogn Behav Neurol. 2005;18:28–36.
Finger EC. New potential therapeutic approaches in frontotemporal dementia: oxytocin, vasopressin, and social cognition. J Mol Neurosci. 2011;45:696–701.
Eisenberg N, Fabes RA. Prosocial behavior and empathy: a multimethod developmental perspective. In: Prosocial behavior. Thousand Oaks: Sage Publications Inc; 1991. p. 34–61.
Decety J. The neurodevelopment of empathy in humans. Dev Neurosci. 2010;32:257–67.
Shamay-Tsoory SG. The neural bases for empathy. Neuroscientist. 2011;17:18–24.
Shdo SM, Ranasinghe KG, Gola KA, Mielke CJ, Sukhanov PV, Miller BL, et al. Deconstructing empathy: neuroanatomical dissociations between affect sharing and prosocial motivation using a patient lesion model. Neuropsychologia. 2018;116:126–35.
Rosen HJ, Pace-Savitsky K, Perry RJ, Kramer JH, Miller BL, Levenson RW. Recognition of emotion in the frontal and temporal variants of frontotemporal dementia. Dement Geriatr Cogn Disord. 2004;17:277–81.
Bora E, Walterfang M, Velakoulis D. Theory of mind in behavioural-variant frontotemporal dementia and Alzheimer’s disease: a meta-analysis. J Neurol Neurosurg Psychiatry. 2015;86:714–9.
Kumfor F, Piguet O. Disturbance of emotion processing in frontotemporal dementia: a synthesis of cognitive and neuroimaging findings. Neuropsychol Rev. 2012;22:280–97.
Rankin KP, Gorno-Tempini ML, Allison SC, Stanley CM, Glenn S, Weiner MW, et al. Structural anatomy of empathy in neurodegenerative disease. Brain J Neurol. 2006;129:2945–56.
Leigh R, Oishi K, Hsu J, Lindquist M, Gottesman RF, Jarso S, et al. Acute lesions that impair affective empathy. Brain. 2013;136:2539–49.
Tippett DC, Godin BR, Oishi K, Oishi K, Davis C, Gomez Y, et al. Impaired recognition of emotional faces after stroke involving right Amygdala or Insula. Semin Speech Lang. 2018;39:87–100.
Virani K, Jesso S, Kertesz A, Mitchell D, Finger E. Functional neural correlates of emotional expression processing deficits in behavioural variant frontotemporal dementia. J Psychiatry Neurosci. 2013;38:174–82.
Snowden JS, Austin NA, Sembi S, Thompson JC, Craufurd D, Neary D. Emotion recognition in Huntington’s disease and frontotemporal dementia. Neuropsychologia. 2008;46:2638–49.
Dermody N, Wong S, Ahmed R, Piguet O, Hodges JR, Irish M. Uncovering the neural bases of cognitive and affective empathy deficits in Alzheimer’s disease and the behavioral-variant of frontotemporal dementia. J Alzheimers Dis. 2016;53:801–16.
Carr AR, Mendez MF. Affective empathy in behavioral variant frontotemporal dementia: a meta-analysis. Front Neurol. 2018. https://doi.org/10.3389/fneur.2018.00417.
Decety J, Bartal IB-A, Uzefovsky F, Knafo-Noam A. Empathy as a driver of prosocial behaviour: highly conserved neurobehavioural mechanisms across species. Philos Trans R Soc B Biol Sci. 2016. https://doi.org/10.1098/rstb.2015.0077.
Eisenberg N, Miller PA. The relation of empathy to prosocial and related behaviors. Psychol Bull. 1987;101:91–119.
Lee R, Ferris C, Van de Kar LD, Coccaro EF. Cerebrospinal fluid oxytocin, life history of aggression, and personality disorder. Psychoneuroendocrinology. 2009;34:1567–73.
Stoop R. Neuromodulation by oxytocin and vasopressin. Neuron. 2012;76:142–59.
Benarroch EE. Oxytocin and vasopressin: social neuropeptides with complex neuromodulatory functions. Neurology. 2013;80:1521–8.
Boccia ML, Petrusz P, Suzuki K, Marson L, Pedersen CA. Immunohistochemical localization of oxytocin receptors in human brain. Neuroscience. 2013;253:155–64.
Freeman SM, Walum H, Inoue K, Smith AL, Goodman MM, Bales KL, et al. Neuroanatomical distribution of oxytocin and vasopressin 1a receptors in the socially monogamous coppery titi monkey (Callicebus cupreus). Neuroscience. 2014;273:12–23.
Kosfeld M, Heinrichs M, Zak PJ, Fischbacher U, Fehr E. Oxytocin increases trust in humans. Nature. 2005;435:673–6.
Fischer-Shofty M, Levkovitz Y, Shamay-Tsoory SG. Oxytocin facilitates accurate perception of competition in men and kinship in women. Soc Cogn Affect Neurosci. 2013;8:313–7.
Shamay-Tsoory SG, Fischer M, Dvash J, Harari H, Perach-Bloom N, Levkovitz Y. Intranasal administration of oxytocin increases envy and schadenfreude (gloating). Biol Psychiatry. 2009;66:864–70.
Gamer M, Zurowski B, Büchel C. Different amygdala subregions mediate valence-related and attentional effects of oxytocin in humans. Proc Natl Acad Sci USA. 2010;107:9400–5.
Chen X, Hackett PD, DeMarco AC, Feng C, Stair S, Haroon E, et al. Effects of oxytocin and vasopressin on the neural response to unreciprocated cooperation within brain regions involved in stress and anxiety in men and women. Brain Imaging Behav. 2016;10:581–93.
Thompson R, Gupta S, Miller K, Mills S, Orr S. The effects of vasopressin on human facial responses related to social communication. Psychoneuroendocrinology. 2004;29:35–48.
Umbricht D, del Valle RM, Hollander E, McCracken JT, Shic F, Scahill L, et al. A single dose, randomized, controlled proof-of-mechanism study of a novel vasopressin 1a receptor antagonist (RG7713) in high-functioning adults with autism spectrum disorder. Neuropsychopharmacology. 2017;42:1914–23.
Liu Y, Wang ZX. Nucleus accumbens oxytocin and dopamine interact to regulate pair bond formation in female prairie voles. Neuroscience. 2003;121:537–44.
Shamay-Tsoory SG, Abu-Akel A. The social salience hypothesis of oxytocin. Biol Psychiatry. 2016;79:194–202.
Dölen G, Darvishzadeh A, Huang KW, Malenka RC. Social reward requires coordinated activity of nucleus accumbens oxytocin and serotonin. Nature. 2013;501:179–84.
Husarova VM, Lakatosova S, Pivovarciova A, Babinska K, Bakos J, Durdiakova J, et al. Plasma oxytocin in children with autism and its correlations with behavioral parameters in children and parents. Psychiatry Investig. 2016;13:174–83.
Hammock E, Veenstra-VanderWeele J, Yan Z, Kerr TM, Morris M, Anderson GM, et al. Examining autism spectrum disorders by biomarkers: example from the oxytocin and serotonin systems. J Am Acad Child Adolesc Psychiatry. 2012;51:712-721.e1.
Finger EC, MacKinley J, Blair M, Oliver LD, Jesso S, Tartaglia MC, et al. Oxytocin for frontotemporal dementia: a randomized dose-finding study of safety and tolerability. Neurology. 2015;84:174–81.
Finger E, Berry S, Cummings J, Coleman K, Hsiung R, Feldman HH, et al. Adaptive crossover designs for assessment of symptomatic treatments targeting behaviour in neurodegenerative disease: a phase 2 clinical trial of intranasal oxytocin for frontotemporal dementia (FOXY). Alzheimers Res Ther. 2018. https://doi.org/10.1186/s13195-018-0427-2.
Oliver LD, Stewart C, Coleman K, Kryklywy JH, Bartha R, Mitchell DGV, et al. Neural effects of oxytocin and mimicry in frontotemporal dementia: a randomized crossover study. Neurology. 2020;95:e2635–47.
O’Keeffe FM, Murray B, Coen RF, Dockree PM, Bellgrove MA, Garavan H, et al. Loss of insight in frontotemporal dementia, corticobasal degeneration and progressive supranuclear palsy. Brain J Neurol. 2007;130:753–64.
Hornberger M, Yew B, Gilardoni S, Mioshi E, Gleichgerrcht E, Manes F, et al. Ventromedial-frontopolar prefrontal cortex atrophy correlates with insight loss in frontotemporal dementia and Alzheimer’s disease. Hum Brain Mapp. 2014;35:616–26.
Muñoz-Neira C, Tedde A, Coulthard E, Thai NJ, Pennington C. Neural correlates of altered insight in frontotemporal dementia: a systematic review. NeuroImage Clin. 2019;24: 102066.
Babinski J. Anosognosie. Paris: Revue Neurologique; 1918.
Schmitz TW, Kawahara-Baccus TN, Johnson SC. Metacognitive evaluation, self-relevance, and the right prefrontal cortex. Neuroimage. 2004;22:941–7.
Zamboni G, Grafman J, Krueger F, Knutson KM, Huey ED. Anosognosia for behavioral disturbances in frontotemporal dementia and corticobasal syndrome: a voxel-based morphometry study. Dement Geriatr Cogn Disord. 2010;29:88–96.
Shany-Ur T, Lin N, Rosen HJ, Sollberger M, Miller BL, Rankin KP. Self-awareness in neurodegenerative disease relies on neural structures mediating reward-driven attention. Brain J Neurol. 2014;137:2368–81.
Levy S, Gansler D, Huey E, Wassermann E, Grafman J. Assessment of patient self-awareness and related neural correlates in frontotemporal dementia and corticobasal syndrome. Arch Clin Neuropsychol. 2017;33:519–29.
Bush G, Luu P, Posner M. Cognitive and emotional influences in anterior cingulate cortex. Trends Cogn Sci. 2000;4:215–22.
Rosen HJ, Alcantar O, Rothlind J, Sturm V, Kramer JH, Weiner M, et al. Neuroanatomical correlates of cognitive self-appraisal in neurodegenerative disease. Neuroimage. 2010;49:3358.
Noonan MP, Mars RB, Rushworth MFS. Distinct roles of three frontal cortical areas in reward-guided behavior. J Neurosci. 2011;31:14399–412.
Massimo L, Libon DJ, Chandrasekaran K, Dreyfuss M, McMillan CT, Rascovsky K, et al. Self-appraisal in behavioural variant frontotemporal degeneration. J Neurol Neurosurg Psychiatry. 2013;84:148–53.
Northoff G, Heinzel A, de Greck M, Bermpohl F, Dobrowolny H, Panksepp J. Self-referential processing in our brain—a meta-analysis of imaging studies on the self. Neuroimage. 2006;31:440–57.
Pijnenborg GHM, de Vos AE, Timmerman ME, Van der Gaag M, Sportel BE, Arends J, et al. Social cognitive group treatment for impaired insight in psychosis: a multicenter randomized controlled trial. Schizophr Res. 2019;206:362–9.
Ducharme S, Dols A, Laforce R, Devenney E, Kumfor F, van den Stock J, et al. Recommendations to distinguish behavioural variant frontotemporal dementia from psychiatric disorders. Brain J Neurol. 2020;143:1632–50.
Gossink FT, Vijverberg EG, Krudop W, Scheltens P, Stek ML, Pijnenburg YA, et al. Psychosis in behavioral variant frontotemporal dementia. Neuropsychiatr Dis Treat. 2017;13:1099–106.
Kertesz A, Ang LC, Jesso S, MacKinley J, Baker M, Brown P, et al. Psychosis and hallucinations in frontotemporal dementia with the C9ORF72 mutation: a detailed clinical cohort. Cogn Behav Neurol. 2013;26:146–54.
Shinagawa S, Nakajima S, Plitman E, Graff-Guerrero A, Mimura M, Nakayama K, et al. Psychosis in frontotemporal dementia. J Alzheimers Dis. 2014;42:485–99.
Naasan G, Shdo SM, Rodriguez EM, Spina S, Grinberg L, Lopez L, et al. Psychosis in neurodegenerative disease: differential patterns of hallucination and delusion symptoms. Brain J Neurol. 2021. https://doi.org/10.1093/brain/awaa413.
Devenney EM, Landin-Romero R, Irish M, Hornberger M, Mioshi E, Halliday GM, et al. The neural correlates and clinical characteristics of psychosis in the frontotemporal dementia continuum and the C9orf72 expansion. NeuroImage Clin. 2017;13:439–45.
Sellami L, Bocchetta M, Masellis M, Cash DM, Dick KM, van Swieten J, et al. Distinct neuroanatomical correlates of neuropsychiatric symptoms in the three main forms of genetic frontotemporal dementia in the GENFI cohort. J Alzheimers Dis. 2018;65:147–63.
Shinagawa S, Naasan G, Karydas AM, Coppola G, Pribadi M, Seeley WW, et al. Clinicopathological study of patients with C9ORF72-associated frontotemporal dementia presenting with delusions. J Geriatr Psychiatry Neurol. 2015;28:99–107.
Pijnenburg YL, Sampson EL, Harvey RJ, Fox NC, Rossor MN. Vulnerability to neuroleptic side effects in frontotemporal lobar degeneration. Int J Geriatr Psychiatry. 2003;18:67–72.
Mintzer JE, Tune LE, Breder CD, Swanink R, Marcus RN, McQuade RD, et al. Aripiprazole for the treatment of psychoses in institutionalized patients with Alzheimer dementia: a multicenter, randomized, double-blind, placebo-controlled assessment of three fixed doses. Am J Geriatr Psychiatry. 2007;15:918–31.
Tariot P, Foff EP, Cummings JL, Soto-Martin M-E, McEvoy B, Stankovic S. HARMONY study: pimavanserin significantly prolongs time to relapse of dementia-related psychosis. Innov Aging. 2020;4:163–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Physician Services Incorporated Foundation Clinical Research Award to Dr E. Finger, and CIHR grant #363926.
Conflicts of interest/Competing interests
Dr Le has no conflicts to report. Dr Finger has received personal compensation for serving on a Scientific Advisory Committee for Biogen, Vigil Neuro, and Denali Therapeutics, for serving as a section editor for NeuroImage Clinical, and for serving as a course director for the AAN Annual Meeting. Dr Finger has received research support paid to her institution (UWO) from CIHR and the Weston Foundation to conduct an ongoing study of oxytocin in FTD, from Alzheimer Society of Canada, and the Physicians and Services Incorporated Foundation, the Ministry of Research and Innovation of Ontario for research, and for site participation in clinical trials sponsored by Alector, Biogen, and TauRx.
Availability of data and material
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Code availability
Not applicable.
Authors' contributions
C. Le and E. Finger were involved in the concept, literature review, design, writing and critical revision of this manuscript. Both authors approve the final version of the manuscript for submission and publication and are accountable for information provided in the manuscript.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Rights and permissions
About this article
Cite this article
Le, C., Finger, E. Pharmacotherapy for Neuropsychiatric Symptoms in Frontotemporal Dementia. CNS Drugs 35, 1081–1096 (2021). https://doi.org/10.1007/s40263-021-00854-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-021-00854-5