Abstract
Background and Objectives
Nasal esketamine is indicated for the treatment of adults with treatment-resistant depression and depressive symptoms in adults with major depressive disorder with acute suicidal ideation or behavior. Primary objectives of this study were to evaluate the effect of nasal decongestant pretreatment in patients with allergic rhinitis and the impact of daily nasal corticosteroid administration by healthy subjects on nasal esketamine pharmacokinetics.
Methods
Patients with allergic rhinitis self-administered 56 mg of nasal esketamine after pretreatment with nasal oxymetazoline (0.05%) at 1 h before esketamine and without oxymetazoline pretreatment. They were exposed to grass pollen in an allergen challenge chamber to induce allergic rhinitis symptoms at approximately 2 h before each esketamine administration until 1 h after. Healthy subjects self-administered esketamine (56 mg) before and after administration for 16 consecutive days of mometasone (200 µg), with the second esketamine dose administered 1 h after the last mometasone dose. The plasma pharmacokinetics of esketamine and noresketamine were assessed after each esketamine administration. The tolerability of esketamine, including effects on dissociative and potential psychotomimetic symptoms and level of sedation and suicidal ideation and behavior, was evaluated.
Results
The rate of esketamine absorption was slightly greater in patients exhibiting symptoms of allergic rhinitis (decrease in median tmax from 32 min to 22 min). Increases in esketamine Cmax and AUC were also small (mean, ≤ 21%). The pharmacokinetics of esketamine was not affected by oxymetazoline or mometasone pretreatment. Esketamine was well tolerated when it was administered with or without pretreatment of oxymetazoline or mometasone.
Conclusions
Patients exhibiting symptoms of rhinitis may receive nasal esketamine spray without dose adjustment. In addition, esketamine may be administered 1 h after using a nasal decongestant or corticosteroid.
Trial Registration
The study was registered in the Clinical Trials (NCT02154334) and EudraCT (2014‐000534‐38) registries.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Nasal esketamine is indicated for the treatment of adults with treatment-resistant depression and depressive symptoms in adults with major depressive disorder with acute suicidal ideation or behavior. |
This study had three main objectives: (1) to compare esketamine pharmacokinetics in patients with allergic rhinitis and healthy subjects; (2) to evaluate the effects of oxymetazoline (a nasal decongestant) on the pharmacokinetics of esketamine, and (3) to evaluate the effects of mometasone (a nasal corticosteroid) on the pharmacokinetics of esketamine. Esketamine was administered as a nasal spray throughout the study. |
Esketamine exposure was similar in patients exhibiting symptoms of allergic rhinitis and healthy subjects. The pharmacokinetics of esketamine was not affected by pretreatment with oxymetazoline in patients with rhinitis or with mometasone in healthy adults. |
Adjustment of the esketamine dose is not needed in patients who are exhibiting symptoms of allergic rhinitis or when administered ≥ 1 h after using a nasal decongestant or corticosteroid. |
1 Introduction
Depression is a common illness worldwide. An estimated 3.8% of the population is affected, including 5.0% among adults and 5.7% among adults aged > 60 years [1]. Many psychopharmacological agents that are currently available for the treatment of major depressive disorder target monoaminergic neurotransmission and typically take several weeks to show efficacy [2]. Approximately two-thirds of patients with major depressive disorder achieve remission after the first or second course of treatment using currently approved drugs. Remission rates following subsequent therapy are lower, and relapse rates are higher and occur more quickly [3]. Therefore, there is a significant need for novel, safe, and fast-acting treatments based upon relevant pathophysiologic pathways of major depressive disorder.
Nasally administered esketamine has been approved by health authorities in the USA, Europe, and other regions worldwide to be used in conjunction with an oral antidepressant for the treatment of treatment-resistant depression in adults [4, 5]. Esketamine is also approved for the treatment of depressive symptoms in adults with major depressive disorder with acute suicidal ideation or behavior. Rapid onset of antidepressant effects has been observed in patients with treatment-resistant depression as early as 24 h after single-dose nasal esketamine administration [6]. Nasal esketamine is intended to be self-administered by the patient under the direct supervision of a health care professional. Because of the possibility of sedation and dissociation, patients are to be monitored by a health care professional for at least 2 h [4] or as clinically warranted [5].
The mechanisms underlying the antidepressant effects of esketamine are complex. Evidence in the literature suggests that, through non-competitive N-methyl-d-aspartate receptor antagonism, esketamine produces a transient increase in glutamate release. This leads to increases in α-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid receptor stimulation and subsequently to increases in neurotrophic signaling that restore synaptic function in brain regions that regulate mood and emotional behavior [7,8,9,10].
The nasal route has been used for delivery of drugs for treatment of local diseases such as nasal allergy, nasal congestion, and nasal infections. Since the nasal cavity has a large surface area and a highly vascularized mucosa, the nasal route can also be used for non-invasive systemic delivery of drugs that are not easily administered by routes other than injection (e.g., drugs that have poor oral bioavailable due to first-pass metabolism) or where rapid onset of action is required [11, 12].
The pharmacokinetics of nasally administered esketamine in healthy subjects and patients with depression have been characterized [4, 5, 13]. The mean absolute bioavailability of 84 mg of esketamine administered as a nasal spray by human subjects is approximately 48%. Esketamine exposure increases with dose from 28 to 84 mg. Esketamine is extensively metabolized by the cytochrome P450 enzymes (CYP), mainly CYP3A4 and CYP2B6. N-demethylation of esketamine to form noresketamine is the major metabolic pathway [14, 15]. Noresketamine is further metabolized by CYP-dependent pathways. Following intravenous or oral administration of radiolabeled esketamine by human subjects, ≥ 78% of administered radioactivity was recovered in urine and a smaller fraction (≤ 2%) was recovered in feces. Less than 1% of the administered dose was excreted in urine as unchanged drug.
Allergic rhinitis is a common chronic condition. Over 400 million people suffer from allergic rhinitis worldwide [16]. The symptoms associated with this disorder, such as inflammation of the nasal mucosa, may affect the absorption of nasally administered drugs. Furthermore, medications that are used to treat the symptoms of allergic rhinitis, such as nasal vasoconstrictors and corticosteroids, may affect the bioavailability of drugs administered by the nasal route. Therefore, the pharmacokinetics and tolerability of nasal esketamine was evaluated in patients experiencing allergic rhinitis. In addition, the effects of a nasally administered vasoconstrictor (oxymetazoline hydrochloride) and corticosteroid (mometasone furoate monohydrate) on the pharmacokinetics and tolerability of nasal esketamine were evaluated in patients who were experiencing allergic rhinitis symptoms at the time of drug administration and in healthy subjects, respectively.
2 Methods
2.1 Study Population
Participants (both men and women) in this study were required to be aged 18–55 years, have a body mass index (BMI) of 18–30 kg/m2, and ascertained to be healthy by clinical examination, medical history, routine laboratory tests, and an electrocardiogram. They were required to be non-smokers or habitually smoke no more than 10 cigarettes, or 2 cigars per day for at least 6 months before first study drug administration. Women had to be not of child-bearing potential or be practicing an effective method of birth control. It was ensured that pregnancy tests were negative at screening and throughout the study. The criteria for exclusion included any contraindication to the use of ketamine or esketamine, use of any prescription or nonprescription medication or herbal supplements within 14 days (or 1 month for any inducer of hepatic CYP activity) before the first scheduled dose of the study drug with the exception of hormonal contraceptives and hormonal therapy or have an anatomical or medical conditions that could impede delivery or absorption of study medication.
Patients eligible for Cohort 1 (interaction with oxymetazoline hydrochloride) were required to have history of moderate seasonal or perennial allergic rhinitis, based on self-reporting, and a positive prick test for grass pollen at screening. In addition, during screening, they had to be classified as symptomatic after being exposed to grass pollen to be eligible for continued participation in the study. The patients were exposed to 4000 ± 800 grains/m3 of Dactylis glomerata (grass) pollen (Allergon AB, Ängelholm, Sweden), for approximately 2 h to induce allergic rhinitis symptoms via an allergen challenge chamber. Technical and procedural details of the allergen challenge chamber have been described extensively previously [17,18,19]. Four symptoms were assessed and documented before and every 15 min during the pollen challenge including runny nose (anterior rhinorrhea/postnasal drainage), itchy nose, nasal congestion (stuffy nose), and sneezing. The severity of each symptom was rated on a 4-point scale (0 = none, 1 = mild, 2 = moderate, 3 = severe). Patients were deemed symptomatic and eligible for continued participation in the study if they had a total nasal symptom score of ≥ 6 with a nasal congestion score of ≥ 2 on at least one occasion during the 2-h screening challenge. Each patient’s lung function was monitored prior to entering the allergen challenge chamber until the next morning after the challenge had been completed. The allergen challenge was to be terminated if the subject’s volume of air that had been exhaled at the end of the first second of forced expiration (FEV1) was below 50% of the subject’s baseline value during pollen exposure.
2.2 Study Design and Procedures
This was an open-label study with 2 cohorts of participants (Cohort 1: patients with allergic rhinitis; Cohort 2: healthy subjects). Written informed consent was obtained prior to the participation in any study-related procedures. They were evaluated during screening to determine study eligibility and admitted into the study center on the preceding day of each administration of nasal esketamine. The participants remained at the center for 2 overnight stays and were discharged shortly after collection of the last esketamine pharmacokinetic sample.
Participants consented to abstain from use of most medications (the exceptions being hormonal contraception, hormonal therapy, and occasional acetaminophen use) during the study or ingestion of food or beverages containing alcohol or quinine from 24 h (or 72 h in the case of grapefruit juice and Seville oranges) before each pharmacokinetic sample collection day and during confinement. They were instructed to refrain from the use of methylxanthine-containing products from 48 h before administration of study drug and during confinement. Food was restricted for at least 8 h starting from the evening before dosing until 2 h after each esketamine administration. Drinking water or any other beverages was restricted for 30 min before and after the esketamine nasal spray. The participants were provided standardized meals while they remained at the study center.
On the day prior to the first administration of esketamine, all participants practiced the self-administration of esketamine using a nasal spray device that was identical to that used to deliver esketamine, but instead filled with an aqueous solution of denatonium benzoate (0.001 mg/mL) and benzalkonium chloride (0.3 mg/mL). In addition, the investigator (or designee) ensured that each participant understood how to self-administer the esketamine nasal device by reviewing the instructions for use prior to each administration. Throughout the study, participants were instructed to recline their head at about 45 degrees during administration of esketamine or denatonium benzoate and benzalkonium chloride solution to keep the liquid inside the nose.
2.2.1 Study Medication
Esketamine was supplied as a clear, colorless nasal solution of esketamine hydrochloride (16.14%). The solution consisted of 161.4 mg/mL esketamine hydrochloride (equivalent to 14% or 140 mg/mL of esketamine base). Inactive ingredients include ethylenediaminetetraacetic acid, citric acid monohydrate, sodium hydroxide, and water for injection. Esketamine was administered by nasal spray pump, which delivered 16.14 mg esketamine hydrochloride (14 mg esketamine base) per 100 µL spray. Throughout this publication, esketamine hydrochloride are referred to as “esketamine”.
Nasal oxymetazoline was made available as a solution of oxymetazoline hydrochloride (0.05% w/v) in a nasal spray pump (Nasivin, Merck Sharp & Dohme GmbH).
Nasal mometasone was made available as an aqueous suspension of mometasone furoate monohydrate (50 µg per spray calculated on the anhydrous basis) (Nasonex Nasal Spray 50 μg, Merck Sharp & Dohme GmbH). The subjects followed the directions for use in the respective labeling when self-administering oxymetazoline hydrochloride or mometasone furoate monohydrate. Participants were instructed to maintain their head in an upright position when administering either drug study. Throughout this publication, the medications are referred to as “oxymetazoline” and “mometasone”, respectively.
2.2.2 Effect of Allergic Rhinitis and Interaction with Oxymetazoline
On Day 1 of each of the 2 treatment periods, the patients deemed eligible for inclusion were exposed to pollen using an environmental challenge chamber with a load of 4000 ± 800 grains/m3 for 3 h and 10 min in total. Twenty-two patients were randomly assigned to one of two sequences. One sequence consisted of self-administration of 0.05% oxymetazoline solution (2 sprays in each nostril) on Day 1 of Period 1 at 1 h and 10 min after the start of pollen exposure and self-administration of 56 mg of esketamine at 2 h and 10 min after the start of pollen exposure. On Day 1 of Period 2 of this sequence, esketamine was administered at the same time relative to the start of pollen exposure, but without oxymetazoline pretreatment. The alternate sequence consisted of the same treatments administered in two periods but in the opposite order (Fig. 1).
In each treatment period, the total dose of esketamine was 56 mg, which was self-administered as a total of 4 sprays (14 mg in each 100-µL spray): one spray in each nostril, followed by a 5-min rest period, followed by one spray in each nostril. The esketamine dose of 56 mg selected to be tested in this study is the initial recommended dose for the indication of treatment-resistant depression [4, 5]. A washout period of 5–10 days separated each 56-mg dose of esketamine in Periods 1 and 2.
2.2.3 Interaction with Mometasone
Twenty-four healthy subjects were assigned to a fixed treatment sequence in an open-label manner. Each subject self-administered 56 mg of esketamine solution as a total of 4 sprays of 14 mg of esketamine solution (see description above). On the following day, after the last esketamine pharmacokinetic sample was collected and prior to being discharged, the subjects self-administered the first nasal dose of mometasone (2 sprays of 50 µg/spray mometasone suspension in each nostril for a total dose of 200 µg). They continued to self-administer 200 µg of mometasone once every morning for 13 consecutive days on an out-patient basis. Subjects kept a diary to document the date and time of each self-administration of mometasone that was not witnessed by the investigator. In addition, the investigator contacted each subject by telephone at least once during the study to confirm compliance with the daily administration of mometasone. Subjects returned to the study center so that the 15th and 16th morning nasal administrations of 200 µg mometasone could be witnessed. The subjects self-administered a second 56-mg nasal dose of esketamine at 1 h after the 16th nasal dose of 200 µg mometasone.
2.3 Study Endpoints
2.3.1 Pharmacokinetic Assessments
Blood samples were collected at predetermined times (i.e., from pre-dose until up to 30 h after the first nasal spray of each 56-mg dose of esketamine) for measurement of esketamine and noresketamine concentrations in plasma. Therefore, two pharmacokinetic profiles were collected per participant (i.e., esketamine alone and following pretreatment with oxymetazoline or mometasone). Plasma was immediately separated and stored at −20 °C or lower until analyzed.
The concentration of esketamine was measured in heparinized plasma samples and collected prior to dosing and at predetermined timepoints on days during which pharmacokinetic samples were collected. Since noresketamine is a non-selective N-methyl-d-aspartate receptor antagonist and has analgesic properties, albeit weaker than esketamine [20,21,22,23], the concentration of this metabolite was measured in the same plasma samples mentioned above for analysis of esketamine concentration. No arketamine (i.e., the R stereoisomer of ketamine) was detected in the plasma of healthy subjects and surgical patients who received intravenous esketamine [24,25,26]. Therefore, non-chiral, specific, and sensitive assays, used for the quantification of ketamine and norketamine in human heparin plasma were developed and validated at Contract Research Organization Frontage Laboratories, Exton, USA. The assays consisted of a solid phase extraction sample preparation after addition of stable isotope labelled internal standards (ketamine-D4 and norketamine-D4). Aliquots (25 µL) of sample were extracted on Oasis µ-elution MCX plates (Waters). The resulting extracts were evaporated to dryness, reconstituted in 400 µL of 2 mM ammonium formate and 0.1% formic acid in methanol/water 25:75 v/v and 10 µL of the extract was injected on a reversed phase high performance liquid chromatography column (Phenomenex Synergi Polar-RP 50 × 2 mm, 4 µm) using a gradient method with 2 mM ammonium formate and 0.1% formic acid in water as mobile phase A and 2 mM ammonium formate and 0.1% formic acid in methanol as mobile phase B. Detection was done by tandem mass spectrometry (Sciex API4000) in the multiple reaction monitoring mode with TurboIonSprayTM ionization in the positive ion mode optimized for the quantification of ketamine and norketamine (MRM transition m/z 238.1 > 125.0 and 224.1 > 125.0, respectively) and for the internal standards ketamine-D4 and norketamine-D4 (m/z 242.1 > 129.0 and 228.1 > 129.0, respectively). A linear regression model with 1/x2 weighing was used, peak area ratios of the analyte to its internal standard were plotted against the analyte concentrations. The concentrations in samples were calculated by interpolation from the standard curve. The inter-day coefficients of variation (number of quality control samples) for ketamine and norketamine varied from 2.7 to 5.1% (n = 37) and 2.7 to 4.1% (n = 35), respectively, at relevant plasma concentrations. The inter-day accuracy (expressed as percent bias) for ketamine and norketamine varied from − 5.3 to − 1.5% (n = 37) and − 4.8 to − 1.0% (n = 35), respectively, at relevant plasma concentrations. The lower limit of quantification was 0.500 ng/mL for both analytes.
The peak plasma concentrations (Cmax) and corresponding times (tmax) of esketamine and metabolite noresketamine were observed directly from the data. The first-order elimination rate constant and the terminal half-life (t1/2) were calculated by means of standard non-compartmental methods. The area under the plasma concentration–time curve until the last measured esketamine or noresketamine concentration value, which was above the quantitation limit (AUClast) was calculated by the linear trapezoidal rule. The area under the plasma concentration–time curve with extrapolation to infinite time (AUC∞) was calculated from AUClast by using the respective elimination rate constant value.
2.3.2 Safety and Tolerability
The safety of the protocol-related procedures and treatments was assessed from the time of consent until the end of the study and included: adverse events, singular 12-lead electrocardiogram, vital signs, pulse oximetry, clinical laboratory results, and physical examinations. The potential effects of nasal esketamine on dissociative and psychotomimetic symptoms were evaluated using the Clinician-Administered Dissociative States Scale (CADSS) and the Brief Psychiatric Rating Scale positive symptoms subscale, respectively [27]. The level of sedation was assessed using the Modified Observer’s Assessment of Alertness/Sedation (MOAA/S) [28]. The Columbia Suicide Severity Rating Scale was performed to assess suicidal ideation and behavior [29]. These scales were completed by the investigator or a designated representative. Changes from baseline were determined for many of safety endpoints listed above. Baseline was defined as the pre-dose value in Period 1 and Period 2 for patients with rhinitis (Cohort 1) or the pre-dose value prior to the first nasal dose of esketamine to healthy subjects (Cohort 2).
Targeted nasal examinations were conducted in addition to above safety assessments. The objective of the examination at screening was to rule out any potential participants with anatomical or medical conditions that may impede drug delivery or absorption. Subsequent examinations consisted of a visual inspection of the nostrils, nasal mucosa, and throat for nasal erythema, rhinorrhea, rhinitis, capillary/blood vessel disruption and epistaxis and graded as follows: none, mild, moderate, or severe. For Cohort 1 (patients with allergic rhinitis), the subsequent examinations were conducted during both periods on Day − 1, 4 h and 24 h after each administration of esketamine, and at the end of the study. For Cohort 2 (healthy subjects), the examinations were performed at 4 h and 24 h after the first dose (Day 1), on Day 15, at 4 h and 24 h after the second dose (Day 16) of esketamine, and at the end of the study.
2.4 Statistical Analysis
The intrasubject coefficient of variation for Cmax and AUC of nasal esketamine is estimated to be ≤ 27%, based on data from other Phase 1 studies conducted with nasal esketamine (data on file). Using a conservative estimate of coefficient of variation of 30% for pharmacokinetic parameters of esketamine, a sample size of 20 subjects was predicted to be sufficient to ensure that the estimate of the ratio of mean pharmacokinetic parameters of esketamine (with and without oxymetazoline in patients with rhinitis and with and without mometasone in healthy subjects) would fall within 85% and 118% of the true value with 90% confidence.
The pharmacokinetics of nasally administered esketamine was compared between patients with allergic rhinitis and healthy subjects in the absence of pretreatment with the nasal decongestant or corticosteroid using an analysis of variance model that was fitted to log-transformed esketamine and noresketamine Cmax and AUCs (i.e., AUClast and AUC∞) with subject group (i.e., cohort) as a factor. Ninety percent confidence intervals (CIs) for the ratios (rhinitis patients versus healthy subjects) of the mean and Cmax and AUC of esketamine were constructed using estimated least squares means (LSM) and inter-subject variances.
The effect of pretreatment with nasal oxymetazoline on the pharmacokinetics of nasally administered esketamine was statistically analyzed with a mixed-effect model. The model, which included treatment (with oxymetazoline, without oxymetazoline) as fixed effect and subject as a random effect, was used to estimate the LSM and intra-subject variance. Using these estimated LSM and intra-subject variance, the point estimate and 90% CIs for the difference in means on a log scale between the two treatments were calculated. The limits of the CIs were retransformed using antilogarithms to obtain 90% CIs for the ratio of the means Cmax and AUCs of esketamine and noresketamine with and without oxymetazoline. A similar analysis was conducted to evaluate the effects of pretreatment with nasal mometasone on the pharmacokinetics of esketamine. Only the data from participants who completed the study were included in the statistical analysis.
3 Results
3.1 1Demographic Characteristics
Written informed consent was obtained from a total of forty-six Caucasian participants (mean [range], 36 [20–54] years; BMI range, 25 [20–30] kg/m2). Twenty-two were patients with allergic rhinitis (12 females and 10 males) and enrolled in the study. Twenty patients with rhinitis completed the study. One female patient was withdrawn by the investigator after completing Period 1. She experienced palpitations of moderate intensity, at 1 h 50 min after oxymetazoline, which corresponds to 50 min after esketamine, that were considered probably related to study drug (oxymetazoline and esketamine). Before resolving, she also had intermittent palpitations (especially nocturnal) of moderate intensity during the washout that were deemed possibly related to study drug. Another female patient received esketamine alone and completed the study-related assessments in Period 1, but then withdrew consent for personal reasons. Of the 46 participants from whom informed consent was obtained, 24 were healthy subjects (12 of each sex) and enrolled in the study. Twenty-three healthy subjects completed the study. One male subject was withdrawn after experiencing Wolff-Parkinson-White syndrome at 13 days after the single dose of nasal esketamine was administered and while administering mometasone daily over this period. The event was considered by the investigator as not related to study drug.
3.2 Total Nasal Symptom Scores
Patients with allergic rhinitis exhibited an increase in the mean total nasal symptom score at approximately 0.5 h after the start of exposure to pollen (i.e., approximately 1.5 h before esketamine was administered). The scores remained elevated up to 1 h after exposure to pollen was terminated (i.e., up to 2 h after esketamine was administered). The mean total scores were similar in the periods during which subjects received nasal oxymetazoline followed by nasal esketamine and nasal esketamine alone. Eleven and 13 patients had a total nasal symptom score ≥ 6 and congestion ≥ 2 (i.e., at least moderate congestion) on at least 1 occasion when esketamine was given with and without oxymetazoline pretreatment, respectively. The remaining patients had a total nasal symptom score of 4 or 5 and a nasal congestion score of 1 (i.e., mild congestion) or 2 (i.e., moderate congestion) on at least 1 occasion.
3.3 Esketamine Pharmacokinetics
3.3.1 Patients with Allergic Rhinitis versus Healthy Subjects
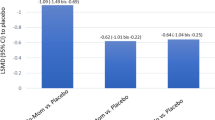
Esketamine was more rapidly absorbed in patients with rhinitis (median tmax, 0.37 h [or 22 min] without pretreatment oxymetazoline) relative to when esketamine was administered to healthy subjects (median tmax, 0.54 h [or 32 min]) (Table 1, Fig. 2). The patients also exhibited a 21% higher mean esketamine Cmax in plasma. The mean of AUClast and AUC∞ were similar with geometric mean ratios (rhinitis patients/healthy subjects) of 1.14, and 1.04, respectively. The corresponding 90% CIs for most of the geometric mean ratios exceeded the upper limit of typical criteria to demonstrate bioequivalence (i.e., 0.80–1.25). For noresketamine, the geometric mean ratios (rhinitis patients/healthy subjects) for Cmax, AUClast, and AUC∞ were 0.91, 0.98, and 0.99, respectively, and the corresponding 90% CIs for the mean AUC ratios were within 0.80–1.25. In addition, there were minor differences in the mean terminal half-life values of esketamine and noresketamine in plasma between participants in each cohort.
3.3.2 Effect of Oxymetazoline
The time to reach esketamine Cmax was prolonged when patients with allergic rhinitis were pretreated with oxymetazoline (median, 0.67 h [or 40 min]) relative when to esketamine administration to patients without oxymetazoline (median tmax, 0.37 h [or 22 min]). There were minor differences in the other pharmacokinetic parameters of esketamine. The geometric mean ratios (esketamine with oxymetazoline/esketamine) for Cmax, AUClast, and AUC∞ were approximately 0.93, 1.00, and 1.01, respectively (Table 2, Fig. 3). The corresponding 90% CIs for the mean ratios were within 0.80 to 1.25. A small increase in noresketamine exposure was observed following coadministration with oxymetazoline with geometric mean ratios (esketamine with oxymetazoline/esketamine) for noresketamine Cmax, AUClast, and AUC∞ of approximately 1.23, 1.15, and 1.14, respectively. The upper limit of the corresponding 90% CIs of the geometric mean ratios for each noresketamine pharmacokinetic parameter exceeded the limits of 0.80–1.25. The decline in plasma esketamine and noresketamine concentrations was not affected by the coadministration of oxymetazoline.
Arithmetic mean (± standard deviation in the main figure) concentrations of esketamine (left) and noresketamine (right) in plasma of patients with allergic rhinitis. Each patient self-administered 56 mg of nasal esketamine with and without pretreatment of 0.05% oxymetazoline (2 sprays in each nostril at 1 h prior to nasal esketamine)
3.3.3 Effect of Mometasone
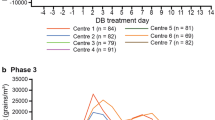
The pharmacokinetics of esketamine was similar when healthy subjects self-administered esketamine following daily nasal administration of mometasone as compared with esketamine alone (Table 1, Fig. 4). There were minor differences in the median tmax (0.67 h [or 40 min] and 0.54 h [or 32 min], respectively). Further, the geometric mean ratios (esketamine with mometasone/esketamine) for Cmax, AUClast, and AUC∞ were approximately 0.96, 0.93, and 0.92, respectively. The corresponding 90% CI for the mean ratios (esketamine with mometasone/esketamine) were within 0.80–1.25. For noresketamine, the relative bioavailability based on Cmax, AUClast, and AUC∞ was approximately 1.09, 1.05, and 1.05, respectively, and the corresponding 90% CIs for noresketamine were also within 0.80–1.25. In addition, the decline in plasma esketamine and noresketamine concentrations, based on the mean terminal half-life values, was not affected by coadministration of mometasone.
Arithmetic mean (± standard deviation in the main figure) concentrations of esketamine (left) and noresketamine (right) in plasma of healthy subjects. Each subject self-administered 56 mg of nasal esketamine before and after daily nasal administration of 200 μg of mometasone for 16 days. The second dose of nasal esketamine was administered at 1 h after the last dose of mometasone
3.4 Safety and Tolerability
3.4.1 Clinical Laboratory and Vital Sign Assessments
There were no clinically relevant mean changes from baseline to end of the study observed in any hematology, chemistry, and urinalysis parameters. The single doses of esketamine produced transient increases in supine heart rate and supine blood pressure. The mean (standard deviation [SD]) changes from baseline in heart rate at the first scheduled measurement of 50 min post-dose (i.e., close to when maximum esketamine concentrations in plasma were observed) were 12.6 (10.9) and 9.4 (9.8) beats per minute when esketamine was administered with oxymetazoline or given alone, respectively, and − 2.7 (13.8) and 3.1 (9.3) beats per minute when esketamine was administered with mometasone and alone, respectively. At 50 min post-dose, the mean (SD) changes from baseline in systolic blood pressure were 8.6 (13.5) and 10.2 (8.4) with and without oxymetazoline, respectively, and 2.1 (10.1), and 9.2 (11.9) mmHg with and without mometasone, respectively. For diastolic blood pressure, the changes at 50 min post-dose were 1.9 (6.44) and 5.9 (8.5) with and without oxymetazoline, respectively, and 3.8 (7.2), and 6.0 (4.9) mmHg with and without mometasone, respectively. Supine heart rate and systolic and diastolic blood pressure returned to near baseline by the next scheduled measurement (i.e., 90 min post-dose). Apart from the case of Wolff-Parkinson-White syndrome described above, there were no clinically relevant changes or clinically meaningful treatment-related trends in electrocardiogram parameters observed in this study. In addition, treatment with the study drugs had no clinically meaningful effects on respiratory rate or oxygen saturation as measured by pulse oximetry.
3.4.2 Nasal Examination
Examination of participants in Cohort 1 revealed moderate nasal erythema in three patients, mild nasal erythema in one patient, and mild epistaxis in one patient when esketamine was administered alone. Mild nasal erythema was observed in four patients when oxymetazoline followed by esketamine were administered. One healthy subject in Cohort 2 exhibited mild nasal crusts after being administered esketamine alone. One healthy subject exhibited mild nasal erythema and another had mild epistaxis after treatment with mometasone and esketamine.
3.4.3 Clinician-Administered Dissociative States Scale
At baseline, the mean (SD) CADSS total scores were 0.0 (0.0) and 0.1 (0.22) when patients in Cohort 1 with allergic rhinitis received esketamine with and without pretreatment with oxymetazoline, respectively, and 0.0 (0.0) prior to when the healthy subjects in Cohort 2 received esketamine after pretreatment with mometasone and esketamine alone. The CADSS total scores increased, indicative of dissociation, at 40 min post-dose following each treatment administered by participants in both cohorts. For the patients with rhinitis, the mean (SD) scores were 13.1 (12.2) (oxymetazoline followed by esketamine) and 20.6 (15.2) (esketamine alone). For healthy subjects, the mean (SD) scores were 1.6 (2.8) (mometasone followed by esketamine) and 3.3 (4.1) (esketamine alone). Mean CADSS total scores returned to baseline (i.e., 0.0) by 2 h when the patients received esketamine alone and when the heathy subjects received esketamine with and without mometasone pretreatment. Mean scores returned to baseline by 4 h post-dose when the patients received esketamine after oxymetazoline pretreatment.
3.4.4 Brief Psychiatric Rating, Modified Observer’s Assessment of Alertness/Sedation, and Columbia Suicide Severity Rating Scales
A majority of participants in the two cohorts had a total score of zero (i.e., no evidence of symptoms) on the Brief Psychiatric Rating Scale positive symptoms subscale at baseline, which remained unchanged during the study. No clinically meaningful psychoses-like symptoms were seen in any participants. Few participants experienced sedation. Four of the patients with rhinitis in Cohort 1 (1 patient after treatment with esketamine and oxymetazoline and also after esketamine alone and 3 patients after treatment with esketamine alone) had MOAA/S scores of 3 (i.e., responded after name called loudly or repeatedly), all of which were reported within 32 min after dosing and resolved within 10–28 min. All healthy subjects in Cohort 2 had a MOAA/S score of 5 (i.e., responded readily to name spoken in normal tone) or 4 (i.e., lethargic response to name spoken in normal tone) at all time points of assessment. No study participant had a post-baseline occurrence of suicidal ideation and/or suicidal behavior.
4 Discussion
Allergic rhinitis is defined as an immunoglobulin E–mediated inflammatory response of the nasal mucous membranes after exposure to inhaled allergens [30]. The inflammation associated with rhinitis produces an increase in the permeability of the nasal mucosa, nasal blood flow, and secretions permeate from the nasal glands [31]. Symptoms of allergic rhinitis include rhinorrhea, nasal congestion, nasal itching, and sneezing. These factors may affect the epithelium and vascular permeability of the nasal mucosa and absorption of a nasally administered drug. The results of the present study indicate the rate of esketamine absorption administered as a nasal spray slightly increased in patients exhibiting symptoms of allergic rhinitis compared to healthy controls, whereas a smaller effect was observed on the extent of absorption. For example, the median tmax of esketamine in plasma was 22 min for patients with rhinitis and 32 min for the healthy subjects and Cmax was on average 21% higher in the patients. Esketamine AUC∞ was only 4% higher in patients with rhinitis as compared to healthy subjects. The pharmacokinetics of metabolite noresketamine were only slightly altered (i.e., on average the Cmax and AUC∞ were ≤9% lower in patients with rhinitis). These changes in the pharmacokinetics of esketamine are not expected to be clinically significant given that they are quite small, particularly in comparison to the interindividual variability of the corresponding parameters.
A higher mean CADSS total score was observed after self-administration of 56 mg of nasal esketamine by patients with rhinitis in Cohort 1, relative to healthy subjects in Cohort 2. In addition, four patients had MOAA/S scores of 3 whereas all of the healthy subjects had a MOAA/S score of 4 or 5 after esketamine administration. The apparent differences between cohorts in CADSS and MOAA/S scores might have been caused by the faster absorption that was observed in subjects in Cohort 1 compared to Cohort 2. However, it is difficult to draw definitive conclusions given that the plasma Cmax and AUC esketamine were only ≤ 21% higher in Cohort 1, there was a high degree of inter-patient variability in CADSS, and a relatively small number of subjects was enrolled in each cohort. In addition, CADSS and MOAA/S scores observed in the present study are within the range of scores observed in patients with treatment-resistant depression who were treated with nasal esketamine [6].
The small effects of rhinitis on the pharmacokinetics of nasal esketamine are consistent with those reported for other drugs. The pharmacokinetics of nasally administered fentanyl, hydromorphone hydrochloride, ipratropium bromide, triamcinolone acetonide, and butorphanol were not affected by the presence of allergic rhinitis or an upper respiratory infection [32,33,34,35,36,37]. However, the rate of absorption of nicotine was reduced in subjects who were experiencing rhinitis symptoms [38].
Nasally administered decongestants are often used by patients for the treatment of allergic rhinitis. These agents are α-sympathomimetics that bind to mucosal α-adrenoceptors, activating them, and causing vasoconstriction of mucosal blood vessels. This constriction results in reduced filling of the capacity vessels and thus reduced swelling of the nasal mucous membranes [39]. The results of the present study indicate that the pharmacokinetics of nasally administered esketamine in patients exhibiting symptoms of allergic rhinitis is minimally affected by pretreatment with oxymetazoline. For example, the Cmax and AUC∞ of esketamine were 7% lower and 1% higher, respectively, when the patients were pretreated with a single dose of the decongestant, relative to when the same patients were administered esketamine without oxymetazoline pretreatment. Furthermore, there was little difference in the mean Cmax and AUC∞ of esketamine in patients with allergic rhinitis pretreated with the decongestant relative to mean esketamine Cmax and AUC∞ values in healthy subjects. Pretreatment with the decongestant increased the Cmax and AUC∞ of noresketamine by 23% and 14%, respectively. It is unclear if these minor effects on noresketamine pharmacokinetics are attributable to pretreatment with oxymetazoline. Noresketamine is formed by metabolic transformation of esketamine mediated by CYP enzymes in the gastrointestinal tract (a fraction of the nasal dose is swallowed [13]), and the liver.
In other pharmacokinetic interaction studies, there was a substantial and potentially clinically relevant decrease in the Cmax of nasally administered fentanyl and butorphanol and a delay in the tmax of these drugs in subjects who were pretreated with oxymetazoline spray [32, 37]. A small delay was observed in the rate of nicotine absorption whereas there was no effect on nasal hydromorphone pharmacokinetics with oxymetazoline pretreatment [34, 38]. Overall exposure (i.e., AUC values) of these four drugs was not affected by pretreatment with the decongestant.
Corticosteroids have numerous applications in treating inflammation and diseases of immune function based on their significant anti-inflammatory and immunosuppressive effects. By the nasal route, they are an effective therapy for treating moderate-to-severe allergic rhinitis [40, 41]. These agents reduce inflammation of the nasal mucosa and improve mucosal pathology through their anti-inflammatory mechanism of action. The mean ratios (with and without 2-week mometasone pretreatment) for Cmax and AUC of esketamine and noresketamine ranged from 0.92 to 1.09 in healthy subjects in the present study. Thus, repeated administration of nasal mometasone produced only small changes in the pharmacokinetics of nasally administered esketamine.
The 56-mg dose of nasal esketamine spray was well tolerated by the patients with allergic rhinitis (with and without oxymetazoline) and healthy subjects (with and without mometasone). There were no new or unexpected safety concerns observed relative to previous studies during which esketamine was given by the nasal and intravenous routes to patients with treatment-resistant depression [6, 42]. Transient increases in blood pressure after the dose were observed, particularly increases in systolic blood pressure, which support an increase in cardiac output as the underlying mechanism, consistent with previous reports for ketamine [43, 44]. Analysis of perceptual change symptoms (measured by CADSS assessment) indicated that onset began shortly after esketamine administration and resolved by 2 h when esketamine was administered alone as single agent or after pretreatment with mometasone or by 4 h when the patients received oxymetazoline pretreatment. No clinically meaningful psychoses-like symptoms were seen in any of the participants, based on the Brief Psychiatric Rating Scale positive symptoms subscale, and no participants had treatment-emergent suicidal behavior or suicidal intent, based on the Columbia Suicide Severity Rating Scale.
This study carries some limitations. First, sample size was small in this interventional study. However, considerations regarding variability of pharmacokinetic parameters with disease or intervention have indicated that meaningful conclusions can be drawn. Second, this study was not blinded but conducted as an open label study. While this might potentially impact on subjective outcomes and safety, the primary aim of this study was pharmacokinetic outcomes which are considered to be robust against blinding-bias. Finally, the effect of mometasone was studied in healthy subjects and not in patients with allergic disease. Given that the symptoms of nasal rhinitis wax and wane over time and are difficult to control, the authors chose to study the effects of chronic corticosteroid and potential subsequent changes in nasal mucosa on the pharmacokinetics of nasal esketamine in healthy subjects.
5 Conclusion
We conclude that the rate of absorption of nasal esketamine was slightly greater in patients exhibiting symptoms of allergic rhinitis. The small increases in esketamine Cmax and AUC do not warrant adjustment of the esketamine dose for these patients. In addition, the pharmacokinetics of nasal esketamine was not affected by pretreatment with a single dose of oxymetazoline at 1 h prior to nasal esketamine in these same patients or when compared to the healthy subjects. Daily administration of mometasone for approximately 2 weeks (with the last dose administered at 1 h prior to esketamine administration) by healthy subjects did not alter the pharmacokinetics of nasal esketamine. Further, esketamine nasal spray was well tolerated by the study participants, when it was administered with or without pretreatment with oxymetazoline or mometasone. Based on the results of this study, patients with major depressive disorder and exhibiting symptoms of allergic rhinitis may receive nasal esketamine spray without dose adjustment. In addition, esketamine may be administered 1 h after using a nasal decongestant or corticosteroid.
Change history
05 August 2023
A Correction to this paper has been published: https://doi.org/10.1007/s40262-023-01290-y
References
WHO Fact Sheet on Depression 13 September 2021; http://www.who.int/news-room/fact-sheets/detail/depression. Assessed 6 Mar 2023.
Machado-Vieira R, Salvadore G, Luckenbaugh D, et al. Rapid onset of antidepressant action: a new paradigm in the research and treatment of major depression. J Clin Psychiatry. 2008;69(6):946–58. https://doi.org/10.4088/jcp.v69n0610.
Rush A, Trivedi M, Wisniewski S, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: A STAR*D report. Am J Psychiatry. 2006;163(11):1905–17. https://doi.org/10.1176/ajp.2006.163.11.1905.
SPRAVATO (esketamine) nasal spray [package insert]. Janssen Pharmaceuticals Companies, Titusville, NJ; 2019. https://www.janssenlabels.com/package-insert/product-monograph/prescribing-information/SPRAVATO-pi.pdf. Accessed 16 June 2023.
SPRAVATO (esketamine) nasal spray EMA Summary of Product Characteristics. https://www.ema.europa.eu/en/documents/product-information/spravato-epar-product-information_en.pdf. Accessed 16 June 2023.
Daly E, Singh J, Fedgchin M, et al. Efficacy and safety of intranasal esketamine adjunctive to oral antidepressant therapy in treatment-resistant depression. A randomized clinical trial. JAMA Psychiat. 2018;75(2):139–48. https://doi.org/10.1001/jamapsychiatry.2017.3739.
Zanos P, Moaddel R, Morris P, et al. Ketamine and ketamine metabolite pharmacology: Insights into therapeutic mechanisms. Pharmacol Rev. 2018;70(3):621–60. https://doi.org/10.1124/pr.117.015198.
Duman R, Aghajanian G, Sanacora G, et al. Synaptic plasticity and depression: new insights from stress and rapid-acting antidepressants. Nat Med. 2016;22(3):238–49. https://doi.org/10.1038/nm.4050.
Manji H, Drevets W, Charney D. The cellular neurobiology of depression. Nat Med. 2001;7(5):541–7. https://doi.org/10.1038/87865.
Murrough J, Abdallah C, Mathew S. Targeting glutamate signaling in depression: progress and prospects. Nat Rev Drug Discov. 2017;16(7):472–86. https://doi.org/10.1038/nrd.2017.16.
Illum L. Nasal drug delivery-possibilities, problems and solutions. J Controlled Release. 2003;87(1–3):187–98. https://doi.org/10.1016/s0168-3659(02)00363-2.
Türker S, Onure E, Özer Y. Nasal and drug delivery systems. Pharm World Sci. 2004;26(3):137–42. https://doi.org/10.1023/b:phar.0000026823.82950.ff.
Perez-Ruixo C, Rossenu S, Zannikos P, et al. Population pharmacokinetics of esketamine nasal spray and its metabolite noresketamine in healthy subjects and patients with treatment-resistant depression. Clin Pharmacokinetics. 2021;60(4):501–16. https://doi.org/10.1007/s40262-020-00953-4.
Portmann S, Kwan H, Theurillat R, et al. Enantioselective capillary electrophoresis for identification and characterization of human cytochrome P450 enzymes which metabolize ketamine and norketamine in vitro. J Chromatogr A. 2010;1217(51):7942–8. https://doi.org/10.1016/j.chroma.2010.06.028.
Yanagihara Y, Kariya S, Ohtani M et al. Involvement of CYP2B6 in N-demethylation of ketamine in human liver microsomes. Drug Metab Dispos. 2001;29(6):887-890. https://dmd.aspetjournals.org/content/29/6/887.long. Accessed 16 June 2023.
www.worldallergy.org/education-and-programs/education/allergic-disease-resource-center/professionals/in-depth-review-of-allergic-rhinitis. Assessed 6 Mar 2023.
Krug N, Loedding H, Hohlfeld J, et al. Validation of an environmental exposure unit for controlled human inhalation studies with grass pollen in patients with seasonal allergic rhinitis. Clin Exp Allergy. 2003;33(12):1667–74. https://doi.org/10.1111/j.1365-2222.2003.01810.x.
Hohlfeld JM, Holland-Letz T, Larbig M, et al. Diagnostic value of outcome measures following allergen exposure in an environmental challenge chamber compared with natural conditions. Clin Exp Allergy. 2010;40(7):998–1006. https://doi.org/10.1111/j.1365-2222.2010.03498.x.
Badorrek P, Dick M, Hecker H, et al. Anti-allergic drug testing in an environmental challenge chamber is suitable both in and out of the relevant pollen season. Ann Allergy Asthma Immunol. 2011;106(4):336–41. https://doi.org/10.1016/j.anai.2010.12.018.
Eberta B, Mikkelsen S, Thorkildsen C, et al. Norketamine, the main metabolite of ketamine, is a non-competitive NMDA receptor antagonist in the rat cortex and spinal cord. Eur J Pharmacol. 1997;333(1):99–104. https://doi.org/10.1016/s0014-2999(97)01116-3.
Holtman J, Crooks P, Johnson-Hardy J, et al. Effects of norketamine enantiomers in rodent models of persistent pain. Pharmacol Biochem Behav. 2008;90(4):676–85. https://doi.org/10.1016/j.pbb.2008.05.011.
Swartjes M, Morariu A, Niesters M, et al. Nonselective and NR2B-selective N-methyl-D-aspartic acid receptor antagonists produce antinociception and long-term relief of allodynia in acute and neuropathic pain. Anesthesiology. 2011;115(1):165–74. https://doi.org/10.1097/ALN.0b013e31821bdb9b.
Moaddel R. Sub-anesthetic concentrations of (R, S)-ketamine metabolites inhibit acetylcholine-evoked currents in α7 nicotinic acetylcholine receptors. Eur J Pharmacol. 2013;698(1–3):228–34. https://doi.org/10.1016/j.ejphar.2012.11.023.
Geisslinger G, Hering W, Thomann P, et al. Pharmacokinetics and pharmacodynamics of ketamine enantiomers in surgical patients using a stereoselective analytical method. Br J Anaesth. 1993;70(6):666–71. https://doi.org/10.1093/bja/70.6.666.
Ihmsen H, Geisslinger G, Schuttler J. Sterioselective pharmacokinetics of ketamine: R(-)-ketamine inhibits the elimination of S(+)-ketamine. Clin Pharmacol Ther. 2001;70(5):431–8. https://doi.org/10.1016/S0009-9236(01)06321-4.
Hartvig P. Central nervous system effects of subdissociative doses of (S)-ketamine are related to plasma and brain concentrations measured with positron emission tomography in healthy volunteers. Clin Pharmacol Ther. 1995;58(2):165–73. https://doi.org/10.1016/0009-9236(95)90194-9.
Bremner J, Krystal J, Putnam F, et al. Measurement of dissociative states with the Clinician-Administered Dissociative States Scale (CADSS). J Trauma Stress. 1998;11(1):125–36. https://doi.org/10.1023/A:1024465317902.
Pambianco D, Vargo J, Pruitt R, et al. Computer-assisted personalized sedation for upper endoscopy and colonoscopy: a comparative, multicenter randomized study. Gastrointest Endosc. 2011;73(4):765–72. https://doi.org/10.1016/j.gie.2010.10.031.
Posner K, Oquendo M, Gould M, et al. Columbia classification algorithm of suicide assessment (C-CASA): classification of suicidal events in the FDA’s pediatric suicidal risk analysis of antidepressants. Am J Psychiatry. 2007;164(7):1035–43. https://doi.org/10.1176/appi.ajp.164.7.1035.
Seidman M, Guideline Otolaryngology Development Group. AAO-HNSF. Clinical practice guideline: allergic rhinitis. Otolaryngol Head Neck Surg. 2015;152(S1):S1–43. https://doi.org/10.1177/0194599814561600.
Dykewicz M, Hamilos D. Rhinitis and sinusitis. J Allergy Clin Immunol. 2010;125(2):S103–15. https://doi.org/10.1016/j.jaci.2009.12.989.
Perelman M, Fisher A, Smith A, et al. Impact of allergic rhinitis and its treatment on the pharmacokinetics of nasally administered fentanyl. Int J Clin Pharmacol Ther. 2013;51(5):349–56. https://doi.org/10.5414/CP201825.
Nave R, Sides E, Colberg T, et al. Pharmacokinetics of intranasal fentanyl spray (INFS) in subjects with seasonal allergic rhinitis with and without prior administration of oxymetzoline. Eur J Pain. 2009;13(S1):S55–285. https://doi.org/10.1016/S1090-3801(09)60721-7.
Davis G, Rudy A, Archer S, et al. Bioavailability and pharmacokinetics of intranasal hydromorphone in patients experiencing vasomotor rhinitis. Clin Drug Invest. 2004;24(11):633–9. https://doi.org/10.2165/00044011-200424110-00002.
Wood C, Fireman P, Grossman J, et al. Product characteristics and pharmacokinetics of intranasal ipratropium bromide. J Allergy Clin Immunol. 1995;95(5 Pt 2):1111–6. https://doi.org/10.1016/s0091-6749(95)70214-8.
Argenti D, Colligon I, Heald D, et al. Nasal mucosal inflammation has no effect on the absorption of intranasal triamcinolone acetonide. J Clin Pharmacol. 1994;34(8):854–8. https://doi.org/10.1002/j.1552-4604.1994.tb02051.x.
Shyu W, Pittman K, Robinson D, et al. The absolute bioavailability of transnasal butorphanol in patients experiencing rhinitis. Eur J Clin Pharmacol. 1993;45(6):559–62. https://doi.org/10.1007/BF00315315.
Lunell E, Molander L, Andersson M. Relative bioavailability of nicotine from a nasal spray in infectious rhinitis and after use of a topical decongestant. Eur J Clin Pharmacol. 1995;48(1):71–5. https://doi.org/10.1007/BF00202176.
Klimek L, Sperl A, Becker S, et al. Current therapeutical strategies for allergic rhinitis. Expert Opin Pharmacother. 2019;20(1):83–9. https://doi.org/10.1080/14656566.2018.1543401.
Williams D. Clinical pharmacology of corticosteroids. Respir Care. 2018;63(6):655–70. https://doi.org/10.4187/respcare.06314.
Wallace D. The diagnosis and management of rhinitis: An updated practice parameter. J Allergy Clin Immunol. 2008;122(2 Suppl):S1–84. https://doi.org/10.1016/j.jaci.2008.06.003.
Singh JB, Fedgchin M, Daly E, et al. Intravenous esketamine in adult treatment-resistant depression: a double-blind, double-randomization, placebo-controlled study. Biol Psychiatry. 2016;80(6):424–31. https://doi.org/10.1016/j.biopsych.2015.10.018.
Singh J, Fedgchin M, Daly E, et al. A double-blind, randomized, placebo-controlled, dose-frequency study of intravenous ketamine in patients with treatment-resistant depression. Am J Psychiatry. 2016;173(8):816–26. https://doi.org/10.1176/appi.ajp.2016.16010037.
Murrough J, Iosifescu D, Chang L, et al. Antidepressant efficacy of ketamine in treatment-resistant major depression: a two-site randomized controlled trial. Am J Psychiatry. 2013;170(10):1134–42. https://doi.org/10.1176/appi.ajp.2013.13030392.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The clinical study and the analyses presented were supported by research funding from Janssen Research and Development, LLC.
Conflict of Interest
Peter Zannikos, Bhavna Solanki, Marc De Meulder, and Jaskaran Singh were employed by Janssen Research & Development, LLC at the time the study was conducted and, as such, may have been eligible for stock and stock options.
Data Availability and Material
The datasets generated and/or analyzed during the study belong to Janssen Research & Development, LLC and are not publicly available.
Ethics Approval
The protocol was approved by an Institutional Review Board (Medizinische Hochshule Hannover Carl-Neuberg-Strasse 1, 30625 Hannover, Germany). The study was conducted at a single center (Fraunhofer Institute for Toxicology and Experimental Medicine, Hannover, Germany) in accordance with the ethical principles that have their origin in the Declaration of Helsinki and that are consistent with Good Clinical Practices and applicable regulatory requirements. The study was registered in the Clinical Trials (NCT02154334) and EudraCT (2014‐000534‐38) registries.
Consent to Participate
Written informed consent was obtained from each participant before enrollment in the study after being advised of the potential risks and benefits of the study, as well as the investigational nature of the study.
Consent for Publication
All authors provided final approval of the published version.
Code Availability
Not applicable.
Author Contribution
All authors participated in the study design and implementation and/or conduct of the study. All authors read and approved the final manuscript.
Additional information
The original online version of this article was revised to correct Table 1 footnote.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zannikos, P., Solanki, B., De Meulder, M. et al. Pharmacokinetics of Nasal Esketamine in Patients with Allergic Rhinitis with and Without Nasal Decongestant Pretreatment and in Healthy Subjects with and Without Nasal Corticosteroid Pretreatment. Clin Pharmacokinet 62, 1315–1328 (2023). https://doi.org/10.1007/s40262-023-01273-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-023-01273-z