Abstract
Sodium-glucose cotransporter inhibitors are a new class of oral antihyperglycemic drugs that have been approved for the treatment of patients with type 2 diabetes mellitus. Sodium-glucose cotransporter inhibitors reduce glucose reabsorption in the kidneys, which lowers blood glucose. In addition, they offer significant cardiovascular benefits and renal protection. Multiple phase III trials of sodium-glucose cotransporter inhibitors in patients with type 1 diabetes have been completed. The European Medicines Agency approved dapagliflozin as an adjuvant therapy to insulin for patients with type 1 diabetes who have poor blood glucose control with the optimal dose of insulin alone (body mass index ≥ 27 kg/m2). As adjuvants to insulin for patients with type 1 diabetes, sodium-glucose cotransporter inhibitors improve blood glucose control and reduce total daily insulin dose and body weight. However, there is also concern about diabetic ketoacidosis caused by sodium-glucose cotransporter inhibitors. In this review, the mechanisms of hypoglycemic action, pharmacokinetics, clinical efficacy, and safety of sodium-glucose cotransporter inhibitors for the treatment of type 1 diabetes are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Sodium-glucose cotransporter (SGLT) inhibitors include the SGLT-2 inhibitors dapagliflozin, empagliflozin, canagliflozin, and ertugliflozin. and the SGLT-1/2 inhibitor sotagliflozin. SGLT-2 inhibitors inhibit glucose reabsorption in renal tissue; SGLT-1/2 inhibitors inhibit glucose absorption in the intestine and glucose reabsorption in renal tissue. |
Phase III clinical trials have confirmed that SGLT inhibitor adjunct therapy with insulin treatment can improve glycemic control in patients with type 1 diabetes mellitus and reduce patient weight without increasing the risk of hypoglycemic events. However, there is also concern about diabetic ketoacidosis caused by SGLT inhibitors. |
The European Medicines Agency approved dapagliflozin as an adjuvant therapy to insulin for patients with type 1 diabetes who have poor blood glucose control with the optimal dose of insulin alone (body mass index ≥ 27 kg/m2). |
1 Introduction
Type 1 diabetes mellitus is a chronic disease characterized by autoimmune-mediated destruction of B cells, resulting in reduced insulin secretion or an absolute deficiency [1, 2]. The occurrence of the disease may be related to autoimmune disorders or environmental factors [3,4,5]. The incidence of type 1 diabetes varies from country to country. East Asian and American Indian populations have the lowest incidence (0.1–8 per 100,000), while Finland has the highest incidence (64.2 per 100,000) [6]. Type 1 diabetes is more common in children and adolescents, but it can occur at any age and requires life-long dependence on insulin therapy [7]. Fewer than one in five children and adolescents with type 1 diabetes in the USA meet the glycosylated hemoglobin (HbA1c) values (< 7.5%) recommended by the American Diabetes Association. To make matters worse, despite the continuous advancement of medical technology, this proportion has gradually decreased [8]. In addition to common complications such as cardiovascular disease, diabetic nephropathy, and diabetic eye disease, patients with type 1 diabetes are more likely to develop diabetic ketoacidosis, and even the incidence of depression is associated with adolescent type 1 diabetes [9,10,11,12]. Insulin therapy is currently the most widely recognized treatment method, but lifelong insulin injection therapy has problems such as weight gain, hypoglycemia, and increased insulin requirements [13]. In addition, insulin therapy does not prevent or delay the progressive destruction of pancreatic islet function, thus patients have lower blood glucose compliance rates.
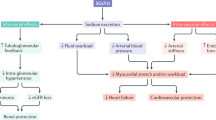
Sodium-glucose cotransporters (SGLTs) are important transporters mediating glucose reabsorption in the small intestine and kidney. Sodium-glucose cotransporter-2 is localized in the S1 segment of the proximal tubule of the kidney [14] and is responsible for ~ 90% of glucose reabsorption in the kidney [15]. Sodium-glucose cotransporter-2 inhibitors, including dapagliflozin, empagliflozin, canagliflozin, and ertugliflozin, are noninsulin-dependent oral antihyperglycemic agents that have been widely approved for the treatment of type 2 diabetes [16,17,18,19]. In DECLARE-TIMI 58, 17,160 patients with type 2 diabetes were treated with dapagliflozin. The reduced risk of cardiovascular death or hospitalization for heart failure had a hazard ratio range from 0.79 (0.58–1.06) in patients with a diabetes duration < 5 years to 0.75 (0.55–1.03) in those with a duration > 20 years (interaction trend p-value 0.76). The hazard ratio of major adverse cardiovascular events had a range from 1.08 (0.87–1.35) in patients with a diabetes duration ≤ 5 years to 0.67 (0.52–0.86) in patients with a duration > 20 years (interaction trend p-value 0.004) [20]. Another DAPA-HF study assessing the role of dapagliflozin in patients with heart failure and a reduced ejection fraction showed that the risk of worsening heart failure or death from cardiovascular causes was lower among those who received dapagliflozin than among those who received placebo, regardless of the presence or absence of diabetes [21]. Based on these two studies, the US Food and Drug Administration granted dapagliflozin fast-track status for adult patients with heart failure. Sodium-glucose cotransporter-1 is mainly localized in the small intestine [14]. The SGLT-1/2 dual inhibitor sotagliflozin is different from SGLT-2 inhibitors; it can work with the kidneys and intestines to reduce glucose absorption [22].
In March 2019, dapagliflozin was successively approved in Europe and Japan as an oral adjuvant therapy to insulin for the treatment of adult patients with type 1 diabetes with poor glycemic control using optimal insulin alone (body mass index ≥ 27 kg/m2); sotagliflozin was subsequently approved for the same indication in Europe [23, 24]. The National Institute for Health and Care Excellence issued guidelines recommending the use of dapagliflozin for the treatment of type 1 diabetes in adults who do not achieve adequate glycemic control despite optimal insulin therapy [25]. The US Food and Drug Administration is relatively cautious about SGLT inhibitors as an adjuvant in the treatment of type 1 diabetes and has rejected applications for dapagliflozin, empagliflozin, and sotagliflozin [26,27,28].
The evidence on the efficacy of SGLT inhibitors as adjuvant therapies for insulin in patients with type 1 diabetes is positive, but more long-term safety evidence is still needed. This article aims to provide guidance for clinicians and pharmacists by reviewing the published efficacy and safety data of this type of therapy.
2 Pharmacokinetics and Pharmacodynamics
2.1 Pharmacokinetics/Pharmacodynamics of Dapagliflozin
Dapagliflozin has similar pharmacokinetic properties in patients with type 1 diabetes and patients with type 2 diabetes, and the systemic exposure (maximum concentration and area under the curve) of dapagliflozin in both patient populations increased similarly in a dose-dependent manner, while a dose-dependent 24-hour increase in urinary glucose excretion was observed [29]. Three studies (NCT01498185, NCT02325206, NCT02582840) showed that the time to maximum concentration of 5–10 mg of dapagliflozin in patients with type 1 diabetes was 1–2 hours, the maximum concentration was 66–167 ng/mL, and the area under the curve was 269–702 ng·h/mL [30,31,32]. The specific data are summarized in Table 1. All doses of dapagliflozin increased urinary glucose levels. The 10-mg dose of dapagliflozin in the three studies had urine glucose excretions of 98.77 (57.53), 134.44 (56.87), and 115.6 (17.2), respectively. Henry et al. reported that dapagliflozin 5 and 10 mg were associated with a reduction in mean percentage changes in baseline total insulin doses of 219.3% (95% confidence interval [CI] 230.1–26.8) and 216.2% (95% CI 229.4–20.5), respectively, on day 7 [30]. Two other studies have also confirmed that the use of dapagliflozin reduced daily total insulin use (Table 1).
A two-compartment model with first-order absorption was used to fit dapagliflozin pharmacokinetics data, and body weight was found to be an important covariate for dapagliflozin exposure. Based on the observed data (NCT01498185 and NCT02325206), in the study, adolescents/young adults had a higher urinary glucose excretion response (138.0 g/24 h) than adults with type 1 diabetes (70.5 g/24 h) [33].
2.2 Pharmacokinetics/Pharmacodynamics of Sotagliflozin
A phase I trial of a dose study was performed in healthy subjects, assessing the pharmacokinetics and pharmacodynamic properties of sotagliflozin. On the seventh day after the multiple-dose administration, the maximum plasma concentration of sotagliflozin was 165 ng/mL, the total exposure (AUC0−tau, area under the concentration−time curve (AUC) at a dosing interval (AUCtau)) was 1172 ng·h/mL, and the pharmacokinetic half-life was 29 h, supporting once-daily dosing. The maximum urinary glucose excretion on day 7 after multiple administrations was 36 g. This urinary glucose excretion reflects the effect on SGLT2 in the kidney but was lower than that of high doses of SGLT2 inhibitors. Sotagliflozin is eliminated mainly in urine in the form of glucuronic acid, while the other eliminations in stool are unaltered components. The study of sotagliflozin in patients with type 2 diabetes expanded pharmacokinetic data by evaluating single doses up to 2000 mg and multiple doses up to 800 mg once daily [22].
3 Efficacy
3.1 Dapagliflozin
Two 24-week phase III studies, DEPICT-1 and DEPICT-2, evaluated the efficacy of dapagliflozin as an adjuvant for insulin in adults with type 1 diabetes [34, 35]. The doses of dapagliflozin were 5 mg and 10 mg once a day, and other detailed data are summarized in Table 2. In each study, subjects were patients with type 1 diabetes with poor glycemic control who had been treated with insulin for at least 12 months. Patients underwent an 8-week run-in period and were randomly assigned using an interactive voice response system. Primary outcome measures were the adjusted average change in glycosylated hemoglobin (HbA1c) from baseline at week 24. Secondary outcome measures included the adjusted average percentage change in total daily insulin dose, the average percentage change in body weight adjusted from baseline, and the proportion of subjects with at least a 0.5% reduction in HbA1c from baseline without severe hypoglycemic events.
After 24 weeks of dapagliflozin adjuvant insulin therapy, blood glucose control of subjects improved significantly. The proportion of subjects with a ≥ 0.5% reduction in HbA1c without severe hypoglycemia was twice that of the placebo group, but there was no difference between the 5-mg group and the 10-mg group (Table 2). In addition, the total daily insulin use also decreased significantly from baseline; compared with that in the placebo group, the decline was 8.8–13.17% (Table 2). In terms of weight reduction, subjects in each treatment group of dapagliflozin also lost 3–4% of their body weight from baseline compared with subjects in the placebo group.
Glycosylated hemoglobin is an important measure of glycemic control for diabetes (reflecting overall glucose exposure over time), but it does not assess blood glucose variability. In contrast, continuous glucose monitoring (CGM) measures important blood glucose variables that contribute to clinical outcomes throughout the day. Continuous glucose monitoring data from the DEPICT-1 and DEPICT-2 studies show that patients receiving dapagliflozin 5 mg or 10 mg have blood glucose levels in the range of > 3.9 to ≤ 10.0 mmol/L for longer periods of time within 24 h. At week 24, the time-adjusted mean (standard error) change from baseline in the placebo, 5-mg, and 10-mg groups was − 2.59% (0.61), 6.48% (0.60), and 8.08% (0.60), respectively [36].
Some subjects in DEPICT-1 and DEPICT-2 participated in a 28-week extension trial. In the DEPICT-1 study, over 52 weeks, dapagliflozin 5 mg and 10 mg led to clinically significant reductions in HbA1c (difference vs placebo, − 0.33% and − 0.36%, respectively) and body weight (difference vs. placebo, − 2.95% and − 4.54%, respectively). In the DEPICT-2 study, at 52 weeks, the adjusted mean HbA1c changes from baseline in the dapagliflozin 5-mg and placebo groups were − 0.27% and 0.06%, respectively, and the adjusted mean change in body weight from baseline for the dapagliflozin 5-mg group was − 4.42%. In two DEPICT studies, compared to placebo, the total daily insulin in the dapagliflozin treatment group remained low during 52 weeks of treatment (detailed data not reported) [37, 38].
Another 52-week phase III clinical trial (DEPICT-5) involving 151 patients from Japan with type 1 diabetes also evaluated the efficacy and safety of dapagliflozin 5-mg and 10-mg adjuvant therapy [39]. At week 24, the adjusted mean (95% CI) HbA1c levels in the 5-mg group and the 10-mg group were − 0.52% (− 0.66, − 0.38) and − 0.66% (− 0.80, − 0.53), respectively. At week 52, the mean corrected HbA1c changes from baseline were − 0.33% (− 0.50, − 0.15) and − 0.36% (− 0.53, − 0.18), respectively. The proportions of patients whose HbA1c decreased by ≥ 0.5% without severe hypoglycemia at week 24 were 60.8% and 61.3%, respectively, and then at 52 weeks were 51.4% and 41.3%, respectively. At week 52, the average daily average insulin dose changes (95% CI) were − 12.27% (− 15.92, − 8.46) and − 13.13% (− 16.77, − 9.33), respectively.
3.2 Empagliflozin
Two large-scale phase III clinical trials, EASE-2 and EASE-3, enrolled a total of 1707 patients with type 1 diabetes to evaluate the effectiveness and safety of empagliflozin as an adjuvant for insulin therapy [40]. The EASE-2 and EASE-3 trials lasted 52 and 26 weeks, respectively. Detailed data are summarized in Table 3. After 26 weeks of empagliflozin-assisted insulin treatment, all empagliflozin doses resulted in a statistically significant reduction in HbA1c after 26 weeks. In the EASE-2 study, the effect on HbA1c persisted at 52 weeks. After 26 weeks of treatment, empagliflozin resulted in a placebo-adjusted weight loss (to 3.4 kg) and a reduction in total daily insulin dose (to 12.7%).
3.3 Sotagliflozin
Three phase III clinical trials (inTandem1-3) recruited approximately 3000 patients with type 1 diabetes to assess the safety and effectiveness of insulin therapy with sotagliflozin as adjuvant therapy [41,42,43]. Detailed data are summarized in Table 4. The design of the inTandem1 and inTandem2 studies was similar; both were conducted for 52 weeks, and the sotagliflozin dose was 200 mg or 400 mg. The primary study endpoint was the change in HbA1c from baseline to 24 weeks. After 24 weeks of treatment, HbA1C was reduced by 0.36% (95% CI − 0.45, − 0.27) and 0.41% (95% CI − 0.50, − 0.32) in placebo-adjusted inTandem1 participants using 200 mg and 400 mg of sotagliflozin, respectively (p < 0.001). The results of the inTandem2 test were 0.37% (95% CI − 0.48, − 0.25) and 0.35% (95% CI − 0.47, − 0.24), similar to inTandem1 (p < 0.001). The benefit of reducing HbA1c was still significant at 52 weeks, although it decreased to 0.2–0.3%. Similar to SGLT-2 inhibitors, SGLT1/2 inhibitors sotagliflozin can also reduce the total daily insulin dose in patients with type 1 diabetes (at weeks 24 and 52, a placebo-adjusted reduction up to − 6.38 and − 8.74, respectively, compared to baseline). Again, after 24 weeks of adjuvant treatment with 200 mg and 400 mg of sotagliflozin, the subject’s weight decreased by 2.35 and 4.3 kg, respectively.
The primary endpoint of the inTandem3 study is the safety endpoint, which will be discussed separately in subsequent sections. The secondary endpoint in effectiveness was similar to the other two studies. In the inTandem3 study, the least-squares mean change from baseline in the sotagliflozin group was significantly higher than that in the placebo group, with HbA1c (a difference of − 0.46 percentage points), body weight (− 2.98 kg), and the mean daily total insulin (− 2.98 IU/day) [both p ≤ 0.002].
4 Safety and Tolerability
4.1 General Safety Adverse Events
Combining data from both the DEPICT-1 and DEPICT-2 studies, 67.7% of subjects experienced at least one adverse event within 24 weeks. The severity of most adverse events was mild, with little difference between the dapagliflozin-treated and placebo groups. The incidence of drug-related adverse events in the dapagliflozin treatment group was 27.8% higher than the 12% in the placebo group, mainly because of increased urinary tract and genital infections associated with increased urination [34, 35] (Table 4). Summarizing the adverse event data of two phase III clinical studies of EASE-1 and EASE-2, similar to dapagliflozin, the incidence of adverse events related to the treatment drug in the empagliflozin treatment group was increased compared with that of the control group (empagliflozin 5 mg or 10 mg vs placebo; 45% or 46% vs 32%). Again, the increased incidence of adverse events is also due to increased urinary tract and genital infections associated with increased urination (Table 5). According to the inTandem1-3 study, there was no difference in the incidence of at least one adverse event between the sotagliflozin treatment group and the placebo group. Similar to SGLT-2 inhibitors, the proportion of genital infections in the sotagliflozin treatment group was higher than that in the placebo group (sotagliflozin 200 mg, 400 mg, placebo; 8%, 9%, 3%, respectively) (Table 5).
4.2 Hypoglycemia
Sodium-glucose cotransporter inhibitors reduce intestinal glucose absorption or renal glucose reabsorption without relying on insulin to decrease blood glucose levels and when used alone, do not cause hypoglycemia. According to phase III clinical studies, dapagliflozin, empagliflozin, or sotagliflozin as adjuvant insulin therapy did not increase hypoglycemia, and the incidence of serious hypoglycemic events did not increase significantly in the various studies compared to the placebo group (Table 5).
4.3 Diabetic Ketoacidosis
People with type 1 diabetes are vulnerable to diabetic ketoacidosis, and the use of SGLT inhibitors increases the incidence of ketone-related events. Adjuvant therapy with SGLT inhibitors reduced total daily insulin doses in patients with type 1 diabetes. When low doses of insulin are not sufficient to inhibit the lipolysis of surrounding adipose tissue, ketone bodies are increased.
In the DEPICT-1 and 2 studies, more patients in the dapagliflozin group were judged to have definitive diabetic ketoacidosis (week 52, DKA; 4.0%, 3.4%, and 1.9% in the dapagliflozin 5-mg, 10-mg, and placebo groups, respectively) [37]. Similarly, in the DECLARE-TIMI 58 study, the incidence of DKA was slightly higher in subjects receiving treatment (0.3%) compared with those receiving placebo (0.1%) [44]. Another phase III clinical study conducted in Japan with safety as the primary endpoint also showed a higher overall incidence of diabetic ketoacidosis in patients with type 1 diabetes (2.6% and 1.3% in the 5-mg and 10-mg groups, respectively) [39]. Analyzing the data in the EASE-1 and 2 studies, the incidence of ketone-related events in the 10-mg and 25-mg empagliflozin treatment groups was 4% and 5%, respectively, compared with 2% in the control group [40]. In a combined analysis of three phase III clinical trials of sotagliflozin, the numbers of patients with at least one DKA event in the sotagliflozin 200-mg and 400-mg treatment groups were 15 (2.4%) and 41 (3.3%), which was higher than the six (0.5%) in the control group [41,42,43]. A meta-analysis including six randomized placebo-controlled trials showed that the rate of DKA of sotagliflozin 400 mg was significantly higher than that of placebo (p < 0.001, risk ratio 4.41; 95% CI 1.92–10.12) and 200 mg (risk ratio 3.65; 95% CI 0.83–15.94) [45].
5 Pharmacoeconomics
Indications for SGLT-2 inhibitors or SGLT-1/2 inhibitors adjuvant therapy for type 1 diabetes have just been approved in some regions, and there are a few studies on the cost-effectiveness of such drugs as adjuvant therapy for type 1 diabetes. A cost-utility analysis was performed to compare the addition of dapagliflozin to insulin therapy with continued insulin monotherapy. Cost effectiveness was measured by the incremental cost-effectiveness ratio, and effectiveness was quantified based on quality-adjusted life-years (QALYs). According to UK guidelines, future costs and QALYs are discounted by 3.5% per year [46]. The study used the Cardiff Type 1 Diabetes Mellitus model and acquired the baseline characteristics of the modeled population through the DEPICT-1 and DEPICT-2 trial populations. The analysis results show that dapagliflozin 5 mg and 10 mg were associated with an increase in 0.42 and 0.49 QALYs, respectively, at an additional cost of £4240 and £2964 per person, respectively. After adding standard care costs, 78–90% of the simulation results estimated by the incremental cost-effectiveness ratio are less than £20,000/QALY. Therefore, under the cost-effectiveness threshold adopted in the UK, using dapagliflozin as an adjuvant therapy for type 1 diabetes is a cost-effective treatment option.
6 Conclusions
Sodium-glucose cotransporter inhibitors, as a generally well-tolerated adjuvant therapy for insulin, can improve glycemic control in patients with type 1 diabetes and reduce the patient’s total daily insulin dose and weight without increasing the risk of hypoglycemic events. It is an effective choice for patients with poor glycemic control with insulin alone.
7 Expert Opinion
Despite advances in medical technology, the needs of patients with type 1 diabetes, especially young patients with type 1 diabetes, have not been met. Sodium-glucose cotransporter-2 inhibitors and SGLT-1/2 inhibitors, as new oral antihyperglycemic drugs, have unique insulin-lowering mechanisms. Cardiovascular benefits, without increasing the risk of hypoglycemia and reducing body weight, have promoted the widespread use of these drugs in the treatment of patients with type 2 diabetes mellitus [47,48,49]. Recently, a number of large-scale, multicenter, phase III clinical trials of dapagliflozin, empagliflozin, and sotagliflozin as adjuvant therapy in patients with type 1 diabetes have been released, laying the foundation for adjuvant treatment with SGLT inhibitors in type 1 diabetes. Based on the results of phase III clinical trials (DEPICT-1 and DEPICT-2), the European Medicines Agency approved dapagliflozin as an adjuvant therapy to insulin for patients with type 1 diabetes who have poor blood glucose control with the optimal dose of insulin alone (body mass index ≥ 27 kg/m2).
Sodium-glucose cotransporter inhibitors bring additional benefits to people with type 1 diabetes, including weight loss. In patients with type 2 diabetes, SGLT inhibitors confer distinct cardiovascular and renal benefits, although these benefits have not been identified in patients with type 1 diabetes. However, they also reduced blood pressure (empagliflozin, systolic blood pressure [up to − 3.9 mmHg] and diastolic blood pressure [up to − 2.3 mmHg]) [40] in patients with type 1 diabetes with hypertension and urine albumin-to-creatinine ratio (dapagliflozin 5 mg vs placebo, − 13.3% [95% CI − 37.2, 19.8]) [50].
The problem of SGLT inhibitors increasing the risk of diabetic ketoacidosis in type 1 diabetes has also been recognized and has been considered by the designers of all phase III clinical studies. Both the medical team and the subjects in the clinical trials received guidance for improving the measurement of ketone levels and for avoiding diabetic ketoacidosis. However, the incidence of ketone-related adverse events in the SGLT inhibitor-treated group was still unavoidably higher than that in the placebo group by two to three times. The severity of DKA was dose dependent, and 2.5 mg of empagliflozin did not increase the incidence of DKA compared to placebo (0.8% vs 1.2%); the incidence of DKA with 200 mg of sotagliflozin also did not increase significantly compared to that with the placebo [40, 45]. Higher doses of SGLT inhibitors are associated with a reduction in the patient’s total daily insulin dose (Tables 2, 3, 4). When the total daily insulin dose is insufficient to inhibit the lipolysis of surrounding adipose tissue, ketone production increases to induce DKA. Therefore, clinicians should pay attention to the possibility of DKA development with SGLT inhibitor use in patients with type 1 diabetes, including fully grasping the patient’s ketone levels and previous DKA episodes and reminding patients to regularly test ketone levels during treatment. Patients with a high risk of DKA or a previous history of DKA may not be suitable for treatment with SGLT inhibitors. Based on the diuretic effect of SGLT inhibitors, patients should be reminded to appropriately increase water consumption and keep genitals clean to reduce genital and urinary tract infections. More studies of SGLT inhibitors as adjuvant insulin therapy for type 1 diabetes will further confirm their effectiveness and safety, which will change the current layout of type 1 diabetes treatment.
References
Soleimanpour SA, Stoffers DA. The pancreatic B cell and type 1 diabetes: innocent bystander or active participant? Trends Endocrinol Metab. 2013;24(7):324–31.
Giwa AM, Ahmed R, Omidian Z, et al. Current understandings of the pathogenesis of type 1 diabetes: genetics to environment. World J Diabetes. 2020;11(1):13–25.
Eray Ş, Uçar HN, Çetinkaya F, et al. The relationship between perceived family climate and glycemic control in type 1 diabetes mellitus adolescent patients. J Clin Res Pediatr Endocrinol. 2017;9(3):253–9.
Sharif K, Watad A, Coplan L, et al. Psychological stress and type 1 diabetes mellitus: what is the link? Expert Rev Clin Immunol. 2018;14(12):1801–8.
Sharp SA, Weedon MN, Hagopian WA, et al. Clinical and research uses of genetic risk scores in type 1 diabetes. Curr Opin Genet Dev. 2018;50:96–102.
Chiang JL, Kirkman MS, Laffel LMB, et al. Type 1 diabetes through the life span: a position statement of the American Diabetes Association. Diabetes Care. 2014;37(7):2034–54.
Gomez-Lopera N, Pineda-Trujillo N, Diaz-Valencia P. Correlating the global increase in type 1 diabetes incidence across age groups with national economic prosperity: a systematic review. World J Diabetes. 2019;10(12):560–80.
Barry-Menkhaus SA, Wagner DV, Riley AR. Small interventions for big change: brief strategies for distress and self-management amongst youth with type 1 diabetes. Curr Diab Rep. 2020;20(1):3.
Massengale J. Depression and the adolescent with type 1 diabetes: the covert comorbidity. Issues Ment Health Nurs. 2005;26(2):137–48.
Alemu S, Dessie A, Tsegaw A, et al. Retinopathy in type 1 diabetes mellitus: major differences between rural and urban dwellers in northwest Ethiopia. Diabetes Res Clin Pract. 2015;109(1):191–8.
Vladu M, Clenciu D, Efrem IC, et al. Insulin resistance and chronic kidney disease in patients with type 1 diabetes mellitus. J Nutr Metab. 2017;2017:6425359.
Trento M, Charrier L, Cavallo F, et al. Vision-related quality of life and locus of control in type 1 diabetes: a multicenter observational study. Acta Diabetol. 2019;56(11):1209–16.
Bode BW, Garg SK. The emerging role of adjunctive noninsulin antihyperglycemic therapy in the management of type 1 diabetes. Endocr Pract. 2016;22(2):220–30.
Hediger MA, Rhoads DB. Molecular physiology of sodium-glucose cotransporters. Physiol Rev. 1994;74(4):993–1026.
Ferrannini E. Sodium-glucose co-transporters and their inhibition: clinical physiology. Cell Metab. 2017;26(1):27–38.
Deeks ED, Scheen AJ. Canagliflozin: a review in type 2 diabetes. Drugs. 2017;77(14):1577–92.
Derosa G, Maffioli P. Ertugliflozin: a sodium-glucose cotransporter-2 (SGLT-2) inhibitor for glycemic control in type 2 diabetes. Ther Clin Risk Manag. 2018;14:1637–40.
Chawla G, Chaudhary KK. A complete review of empagliflozin: most specific and potent SGLT2 inhibitor used for the treatment of type 2 diabetes mellitus. Diabetes Metab Syndr. 2019;13(3):2001–8.
Dhillon S. Dapagliflozin: a review in type 2 diabetes. Drugs. 2019;79(10):1135–46.
Bajaj HS, Raz I, Mosenzon O, et al. Cardiovascular and renal benefits of dapagliflozin in patients with short and long-standing type 2 diabetes: analyses from the DECLARE-TIMI 58 trial. Diabetes Obes Metab. 2020;22(7):1122–31.
McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. New Engl J Med. 2019;381(21):1995–2008.
Lapuerta P, Zambrowicz B, Strumph P, et al. Development of sotagliflozin, a dual sodium-dependent glucose transporter 1/2 inhibitor. Diab Vasc Dis Res. 2015;12(2):101–10.
European Medicines Agency. Forxiga: EPAR: medicine overview. 2019. https://www.ema.europa.eu/en/documents/overview/forxiga-epar-medicine-overview_en.pdf. Accessed 11 Mar 2020.
European Medicines Agency. Zynquista 200 mg flm-coated tablets: summary of product characteristics. 2019. https://www.ema.europa.eu/en/documents/overview/zynquista-epar-medicine-overview_en.pdf. Accessed 11 Mar 2020.
Adler AI, Ting S, Dent R, et al. NICE guidance on dapagliflozin with insulin for type 1 diabetes. Lancet Diabetes Endocrinol. 2019;7(10):750–1.
AstraZeneca. Update on US regulatory decision for Farxiga in type-1 diabetes. 2019. https://www.astrazeneca.com/content/astraz/media-centre/press-releases/2019/update-on-us-regulatory-decision-for-farxiga-in-type-1-diabetes-15072019.html. Accessed 11 Mar 2020.
Sanofi. Sanofi: FDA issues complete response letter for Zynquista™ (sotagliflozin). 2019. https://www.sanofi.com/en/media-room/press-releases/2019/2019-03-22-19-15-00. Accessed 11 Mar 2020.
Company ELa. US FDA issues complete response letter for empagliflozin 2.5 mg as adjunct to insulin for adults with type 1 diabetes. 2020. https://investor.lilly.com/news-releases/news-release-details/us-fda-issues-complete-response-letter-empagliflozin-25-mg. Accessed 11 Mar 2020.
Tang W, Leil TA, Johnsson E, et al. Comparison of the pharmacokinetics and pharmacodynamics of dapagliflozin in patients with type 1 versus type 2 diabetes mellitus. Diabetes Obes Metab. 2016;18(3):236–40.
Henry RR, Rosenstock J, Edelman S, et al. Exploring the potential of the SGLT2 inhibitor dapagliflozin in type 1 diabetes: a randomized, double-blind, placebo-controlled pilot study. Diabetes Care. 2015;38(3):412–9.
Biester T, Aschemeier B, Fath M, et al. Effects of dapagliflozin on insulin-requirement, glucose excretion and ß-hydroxybutyrate levels are not related to baseline HbA1c in youth with type 1 diabetes. Diabetes Obes Metab. 2017;19(11):1635–9.
Watada H, Shiramoto M, Ueda S, et al. Pharmacokinetics and pharmacodynamics of dapagliflozin in combination with insulin in Japanese patients with type 1 diabetes. Diabetes Obes Metab. 2019;21(4):876–82.
Busse D, Tang W, Scheerer MF, et al. Comparison of pharmacokinetics and the exposure-response relationship of dapagliflozin between adolescent/young adult and adult patients with type 1 diabetes mellitus. Br J Clin Pharmacol. 2019;85(8):1820–8.
Dandona P, Mathieu C, Phillip M, et al. Efficacy and safety of dapagliflozin in patients with inadequately controlled type 1 diabetes (DEPICT-1): 24 week results from a multicentre, double-blind, phase 3, randomised controlled trial. Lancet Diabetes Endocrinol. 2017;5:864–76.
Mathieu C, Dandona P, Gillard P, et al. Efficacy and safety of dapagliflozin in patients with inadequately controlled type 1 diabetes (the DEPICT-2 study): 24-week results from a randomized controlled trial. Diabetes Care. 2018;41(9):1938–46.
Mathieu C, Dandona P, Phillip M, et al. Glucose variables in type 1 diabetes studies with dapagliflozin: Pooled analysis of continuous glucose monitoring data from DEPICT-1 and -2. Diabetes Care. 2019;42(6):1081–9.
Dandona P, Mathieu C, Phillip M, et al. Efficacy and safety of dapagliflozin in patients with inadequately controlled type 1 diabetes: the DEPICT-1 52-week study. Diabetes Care. 2018;41(12):2552–9.
Paik J, Blair HA. Dapagliflozin: a review in type 1 diabetes. Drugs. 2019;79:1877–84.
Araki E, Watada H, Uchigata Y, et al. Efficacy and safety of dapagliflozin in Japanese patients with inadequately controlled type 1 diabetes (DEPICT-5): 52-week results from a randomized, open-label, phase III clinical trial. Diabetes Obes Metab. 2020;22(4):540–8.
Rosenstock J, Marquard J, Laffel LM, et al. Empagliflozin as adjunctive to insulin therapy in type 1 diabetes: the EASE trials. Diabetes Care. 2018;41(12):2560–9.
Garg SK, Henry RR, Banks P, et al. Effects of sotagliflozin added to insulin in patients with type 1 diabetes. New Engl J Med. 2017;377(24):2337–48.
Buse JB, Garg SK, Rosenstock J, et al. Sotagliflozin in combination with optimized insulin therapy in adults with type 1 diabetes: the North American Intandem1 study. Diabetes Care. 2018;41(9):1970–80.
Danne T, Cariou B, Banks P, et al. Hba1c and hypoglycemia reductions at 24 and 52 weeks with sotagliflozin in combination with insulin in adults with type 1 diabetes: the European Intandem2 study. Diabetes Care. 2018;41(9):1981–90.
Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. New Engl J Med. 2019;380(4):347–57.
Musso G, Gambino R, Cassader M, et al. Efficacy and safety of dual SGLT 1/2 inhibitor sotagliflozin in type 1 diabetes: meta-analysis of randomised controlled trials. BMJ. 2019;365:I1328.
Bennett H, Tank A, Evans M, et al. Cost-effectiveness of dapagliflozin as an adjunct to insulin for the treatment of type 1 diabetes mellitus in the United Kingdom. Diabetes Obes Metab. 2020;22(7):1047–55.
Avgerinos I, Liakos A, Tsapas A, et al. Cardiovascular risk reduction in type 2 diabetes: therapeutic potential of dapagliflozin. Diabetes Metab Syndr Obes. 2019;12:2549–57.
Tanaka A, Shimabukuro M, Machii N, et al. Effect of empagliflozin on endothelial function in patients with type 2 diabetes and cardiovascular disease: Results from the multicenter, randomized, placebo-controlled, double-blind EMBLEM trial. Diabetes Care. 2019;42(10):e159–61.
Weira MR, McCullough PA, Buse JB, et al. Renal and cardiovascular effects of sodium glucose co-transporter 2 inhibitors in patients with type 2 diabetes and chronic kidney disease: perspectives on the canagliflozin and renal events in diabetes with established nephropathy clinical evaluation trial results. Am J Nephrol. 2020;51(4):276–88.
Edelman S, Jendle J, Dandona P, et al. Effect of adding dapagliflozin as an adjunct to insulin on urinary albumin-to-creatinine ratio over 52 weeks in adults with type 1 diabetes [abstract no. TH-PO1156 plus poster]. ASN Kidney Week; 2018, San Diego (CA).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received to prepare this manuscript.
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Li, N., Chen, R. & Liu, K. Sodium-Glucose Cotransporter Inhibitors for the Treatment of Type 1 Diabetes Mellitus. Clin Drug Investig 40, 991–1000 (2020). https://doi.org/10.1007/s40261-020-00949-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-020-00949-9