Abstract
Inherited retinal diseases (IRDs) comprise a clinically and genetically heterogeneous group of disorders that can ultimately result in photoreceptor dysfunction/death and vision loss. With over 270 genes known to be involved in IRDs, translation of treatment strategies into clinical applications has been historically difficult. However, in recent years there have been significant advances in basic research findings as well as translational studies, culminating in an increasing number of clinical trials with the ultimate goal of reducing vision loss and associated morbidities. The recent approval of Luxturna® (voretigene neparvovec-rzyl) for Leber congenital amaurosis type 2 (LCA2) prompts a review of the current clinical trials for IRDs, with a particular focus on the importance of adeno-associated virus (AAV)-based gene therapies. The present article reviews the current state of AAV use in gene therapy clinical trials for IRDs, with a brief background on AAV and the reasons behind its dominance in ocular gene therapy. It will also discuss pre-clinical progress in AAV-based therapies aimed at treating other ocular conditions that can have hereditable links, and what alternative technologies are progressing in the same therapeutic space.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The safety of adeno-associated virus (AAV)-based gene therapies for inherited ocular conditions has now been substantially validated by several clinical trials. |
Recent improvements in clinical trial design and AAV technologies are providing further encouragement towards the efficacy of these therapies. |
There is increasing support for ‘non-traditional’ AAV therapies and new technologies such as antisense oligonucleotides as alternative treatment strategies. |
1 Adeno-Associated Virus (AAV)-Based Retinal Gene Therapy: Long Time Coming
The eye has several advantages as a target for the use of molecular therapies such as viral vector-based gene therapy: (1) the retina is relatively immune-privileged (due to tight junctions of the blood–retina barrier [1]), thus minimising any systemic inflammatory response from the introduction of a foreign antigen [2]; (2) small amounts of treatment vector are needed to achieve ‘therapeutic response’ and vectors are essentially quarantined from systemic circulation [3]; (3) the retina is readily accessible by surgery and vectors can be delivered close to target cells [4] and (4) there is the ability to non-invasively monitor disease progression in terms of both retinal structure and physiology [5]. Furthermore, all retinal neurons are post-mitotic [6], reducing the likelihood of dilution or progressive loss of the expression of targeted therapeutic agent [7]. However, the success of a retinal gene therapy approach is primarily dependent on how efficiently, and specifically, the selected technology to deliver the therapeutic construct can target the retinal cell of interest.
The use of viral vectors to transfer functional genes into host cells to correct endogenous dysfunctional genes has significantly progressed over the last 30 years. Initial use of recombinant viral vectors, such as those derived from retroviruses, lentiviruses and adenoviruses, showed efficient gene delivery; however, safety concerns have resulted in the predominance of adeno-associated virus (AAV) as the current therapeutic vector of choice [8]. The inherent properties of AAV, and its malleability for genetic modification and engineering, positions it as a useful platform for gene therapy. AAV has many attributes suited to ocular gene therapy; it is non-pathogenic, confers a relatively low immunogenic response [9] in privileged areas such as the eye and brain, different tissue and cell tropism can be modified by careful selection of serotype [10, 11] and the vector is able to sustain long-term transgene expression [8]. Its ability to replicate is dependent upon co-infection with a helper virus, such as adenovirus, otherwise it remains as a non-integrating, nuclear episome in non-dividing cells or integrates into the host genome at the specific AAVS1 site on chromosome 19 [12,13,14]. Since its initial identification in 1965 [15], an increasing number of AAV serotypes and variants have been identified, varying in their tissue tropism and transduction efficiencies [16,17,18,19]. The AAV’s simple cellular and molecular structure belies its significant functional versatility and potential to transform the gene therapy field.
The first attempts of in vivo transduction of mouse and primate retinas [12, 20] and gene replacement therapy in mouse models of inherited retinal diseases (IRDs) [21, 22] were achieved almost three decades ago using the AAV2/2 serotype. The subsequent studies using AAV2/2 formed the basis for the first ocular gene therapy clinical trials [23,24,25]. However, the shortcomings of AAV2/2 were soon evident, such as its limited cellular tropism and the widespread presence of neutralising antibodies to AAV2/2 in the wider population [26]. As new AAV serotypes were being reported, they were used to generate recombinant vectors using the AAV2 genome and capsids from these different serotypes; for example, AAV2/1 (AAV2 genome with AAV1 capsid) [27, 28]. There are now more than 100 AAV serotypes identified from human and non-human primates [29]. Also, in addition to natural AAV variants, a significant amount of research has concentrated on altering AAV’s transduction efficiency by targeted mutagenesis of the capsid coding genes, or by library approaches, allowing for selective screening of novel capsids [17]. Thus, significant advances can still be made through basic research concentrating on atomic scale details of AAV capsid's structure and function. The continual development and testing of new genetically engineered AAVs will enable optimisation of gene delivery efficiencies, either by adjusting the delivery method to suit specific disorders, such as using multiple AAVs for large gene delivery [30, 31], or by simply improving cell targeting and transduction levels by developing novel capsids [17].
The growing evidence from pre-clinical studies using AAV-based approaches to treat retinal disorders suggests that combining the wide spectrum of disease targets with the suitability of AAV for developing retinal therapeutics is effective. Since the recent market approval from the US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) for an AAV2/2-based therapy for the inherited retinal condition Leber congenital amaurosis type 2 (LCA2, caused by mutations in the RPE65 gene; voretigene neparvovec-rzyl, trade name: Luxturna®), there has been a steep increase in the development, testing and launching of new trials specifically for retinal disorders [32]. There are 43 ongoing or completed clinical trials that are using or have used AAV delivery systems as a means of correcting genetic faults in inherited retinal degeneration (IRDs; ClinicalTrials.gov; Table 1, Supplementary Table 1, see Electronic Supplementary Material [ESM]). Another five clinical trials (three ongoing and two completed) are also using or have used AAV to deliver therapeutics for age-related macular degeneration (reviewed in [32]) and future trials for glaucoma are likely [33]. This highlights how far retinal AAV gene therapy research has come. This review will provide an overview of the available results for the AAV-based clinical trials for IRDs with a focus on their selected AAV serotype. It will also discuss some of the latest developments using AAV for what classically have not been thought of as IRDs, yet can have heritable risk factors amenable to gene therapy, such as Leber Hereditary Optic Neuropathy (LHON) and paediatric glaucoma, and the emergence of antisense oligonucleotide technology as a potential alternative to AAV-based therapies.
2 AAV-Based Gene Therapy for Inherited Retinal Diseases (IRDs): Clinical Trials Update
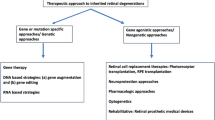
IRDs comprise a clinically and genetically heterogeneous group of disorders that result in the degeneration of the outer retina and progressive visual impairment. Over the past three decades, investigation into the underlying molecular causes have identified over 270 genes associated with inherited vision loss and blindness in one or more clinical subtypes of IRD [184]. The heterogeneous presentation of these conditions, both clinically and genetically, has until now made it difficult to link their pathophysiology with the underlying genetic lesion. It is only advances in genetic screening, along with better clinical measurements, that have allowed stratification and subtype classification [34]. This knowledge has enabled clinicians and researchers to identify genetic targets and start the development and implementation of gene replacement treatment platforms. Whilst many forms exhibit complex aetiology, IRDs are largely monogenic and typically progressive, exhibiting a wide range of presenting age and variability in visual disturbance. Their inheritance patterns follow Mendelian inheritance of autosomal dominant (AD), autosomal recessive (AR), X-linked (XL) or mitochondrial patterns [35]. Furthermore, even when the same mutation is identified, the age of onset and the severity of disease manifestation can vary amongst family members, strongly suggesting involvement of other complex factors [36]. With the provision of a wide scope of potential treatments for different types of IRDs, the eventual choice of therapy will depend on many factors, including the genetic target, the type of inheritance, the time-course of disease, the severity of retinal degeneration and the availability of relevant technologies. AAV-based gene therapy has taken the lead in the last decade, with an ever-growing number of pre-clinical studies in animal models and clinical trials providing encouraging results [37].
2.1 AAV2/2-Based Clinical Trials
AAV2/2 was the first and most widely tested serotype in the retina as it was shown to be capable of targeting both retinal pigment epithelium (RPE) and some photoreceptor cells after subretinal delivery in mice [12, 38], rats [39] and primates [20]. Subsequently, it was the vector of choice in the first studies investigating gene replacement therapy in animal models of IRD [22, 23, 40], and paved the way for future clinical application of AAV-based gene therapy—the vast majority of completed or active AAV-based clinical trials for IRDs have used AAV2/2 (Table 1). These include most of the trials for LCA2 (human retinal pigment epithelium-specific 65 kDa protein [RPE65] deficiency) and Leber Hereditary Optic Neuropathy (LHON), all of the choroideremia trials, and one trial for retinitis pigmentosa (RP) caused by mutations in the MERTK (mer proto-oncogene, tyrosine kinase) gene. Because each of these conditions affect different cell types in the retina, the design of each trial had to take into consideration not only AAV2/2’s retinal tropism, but also the promoter selection and route of vector delivery. The choroideremia and some of the LCA2 trials opted for ubiquitous promoters such as the hybrid cytomegalovirus early enhancer/chicken b-actin (CAG) promoter (choroideremia) or the human cytomegalovirus (CMV) promoter (LCA2). Cell-specific promoters were also used and include the human RPE65 promoter (LCA2) and the RPE-specific human VMD2 (vitelliform macular dystrophy-2) promoter (MERTK-related RP). The choice of delivery route for all trials was selected primarily according to the target cell: RPE and photoreceptors for LCA2, choroideremia and MERTK-related RP, and retinal ganglion cells (RGCs) for LHON. Subretinal delivery is still the most efficient route for AAVs to target RPE and photoreceptors, as in the adult eye most serotypes cannot reach the outer nuclear layer from the vitreous due to the physical barrier created by the inner limiting membrane [41, 42]. However, in adult eyes, especially in rodents, intravitreal AAV2/2 injections are an efficient way of targeting RGCs [10, 33, 43, 44]. The results of the different AAV2/2-based trials are discussed below.
2.1.1 Targeting the Retinal Pigment Epithelium (RPE)—the LCA2 and MERTK Trials
Both LCA2 and MERTK-related RP are conditions that directly affect the RPE cells given the cell-specific expression of RPE65 and MERTK. The first and most successful (to date) AAV-based clinical trials for a retinal condition were for LCA2, an autosomal recessive disorder caused by mutations in the RPE65 gene [45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62]. At a cellular level, RPE65 produces retinoid isomerohydrolase, an enzyme involved in RPE-mediated metabolism of chromophore recycling after phototransduction [63, 64]. The MERTK gene encodes a transmembrane receptor of tyrosine kinases and is found in phagocytic cells such as RPE and macrophages. In RPE cells, MERTK plays an essential role in the renewal of outer segments (OS) of the photoreceptor. Given AAV2/2’s tropism for RPE cells, it was the selected vector in several pre-clinical studies showing that AAV-based subretinal gene therapy in mouse, rat and dog models of RPE65 and MERTK deficiency was capable of restoring visual function [23, 24, 65,66,67,68], paving the way for the first set of gene therapy clinical trials for IRDs.
The initial results from the LCA2 trials were first published in 2008 [45,46,47] and several follow-up studies have now attested to the safety and long-term follow up of this treatment [69,70,71]. However, the reported treatment efficacy between the LCA2 trials has been variable, a discrepancy that can be attributed to differences in construct design, dose volumes and concentration, and outcome measures of visual improvement [72]. The most widely used measure of visual function used in these trials was the best-corrected visual acuity (BCVA) measure, although some trials also reported on retinal thickness, full-field light sensitivity threshold (FST) testing, mobility testing, kinetic visual field, and/or pupillary light reflex. Wang and colleagues [72] recently conducted a systematic review and meta-analysis of the compiled BCVA results from the long-term follow-up (up to 3 years) of the different LCA2-RPE65 clinical trials. Pooling of treated eyes compared with untreated eyes shows that improvement in BCVA is only significant at the 1-year follow-up. At the 2- or 3-years follow-up, the BVCA improvement in the treated versus untreated eyes was no longer significant. This finding is in agreement with some reports showing that the rate of degeneration remains unabated even after treatment delivery [55]. However, a pooled analysis of treated eyes across the different LCA-RPE6 trials can be challenging as considerable design differences exist between the trials. Patient selection (age, mutation, variable baseline visual function), vector design (serotype, promoter, regulatory elements), doses, number of injections, retinal area covered and technical/surgical procedural differences can all influence the visual outcome measures.
When analysed in isolation, the LCA-RPE65 trials conducted at the Children’s Hospital of Philadelphia/Spark Therapeutics provided further validation of their treatment, including follow-up trials such as treating the contralateral untreated eye [54, 59], and measurements of visual cortex activity in treated patients [74]. It is also the only group that progressed to a randomised, controlled, open-label phase III trial [62] and FDA/EMA approval for this treatment, now commercialised under the trademark Luxturna®. Indeed, a recent study by Maguire et al. (2019), reporting on the results from their phase I and III trials, showed that the improvements seen early on in the multi-luminance mobility test and FST were maintained up to 4 years. They also report that treated patients were able to maintain a stable BVCA up to the 4-years follow-up, suggesting a halt in disease progression over time [75]. There are currently five LCA-RPE65 trials that are still active or recruiting, including long-term follow-ups. Therefore, we will continue to learn what this ground-breaking approach can deliver to LCA2 patients in the future.
Similarly, the MERTK phase I trial also showed that delivery of their AAV2/2-VMD2-hMERTK agent was well tolerated and caused no adverse events up to the 2-year follow-up [73]. Visual acuity improvement was, however, very mild and only persisted in two out of the six treated eyes, but with one of the two eyes showing a decline from the 1-year follow-up onwards [73].
2.1.2 The Choroideremia Trials—Targeting RPE and Photoreceptors
The second IRD condition to undergo a series of clinical trials using AAV2/2 was choroideremia, a rare type of inherited X-linked retinal disorder that largely affects men due to random X chromosome inactivation [76]. Affected individuals present with progressive vision loss symptoms starting with loss of night vision in early childhood, followed by increasing loss of peripheral vision [77, 78]. It is caused by mutations in the CHM gene [79], which encodes for the Rab escort protein-1 (REP-1) protein found throughout the body [80]. REP-1 is an essential component of the complex system of intracellular trafficking [80] and its absence usually leads to degeneration of the choroid, RPE and photoreceptors. However, the pathophysiological mechanisms behind this degeneration are still under debate [80,81,82,83]. The success of the LCA2 trials, combined with the relative ease of genetic diagnosis of choroideremia patients, slow progression of the clinical phenotype [78] and small size of the CHM gene [84] provided encouragement for researchers and clinicians to pursue a gene therapy treatment approach. The confirmed safety of AAV2/2 for human use in the retina, combined with its capacity for targeting both RPE and photoreceptors, made this serotype the obvious choice for the choroideremia studies.
The first-in-human clinical trial for choroideremia (NCT01461213) was based in Oxford and used a therapeutic construct containing the human CHM gene driven by the chicken β-actin (CBA) promoter and a Woodchuck hepatitis virus post-translational regulatory element (WPRE) downstream of CHM. The results have been reported at 6 months [85], 3.5 years [86] and 5 years [87] after treatment. Out of the six treated patients, two patients reported significant improvement in their baseline BCVA based on the Early Treatment Diabetic Retinopathy Study (ETDRS) letters that was sustained long term (5 years after treatment) [87]. From the remaining four patients, three were able to maintain their BCVA up to 5 years post-treatment [87]. What is interesting in the data reported for this initial group of patients is that the level of visual improvement directly correlated to the vector dose received. In contrast to previous trials, this trial used post-injection fundus imaging to calculate the treated area and therefore adjust the actual dose received per patient based on the size of the treated area [84]. This is a potentially more accurate approach since other trials tend to report only the injected dose independent of the subretinal area treated. Corroborating this approach, the results showed that the best reported visual improvement was seen in the two patients who received the highest dose of vector per mm2 of treated retina. These patients received 13.2 and 8.1E9 genome particles (gp)/mm2 of retina, respectively, while the three patients that maintained their baseline acuity ranged from 1.2 to 5.6E9, and the sixth patient, who had the worst reported outcome, only received a dose of 0.7E9 gp/mm2 due to surgical complications that caused a permanent retinal thinning [85, 86]. The second group of eight patients received a higher dose of vector at 1E11 gp and significant visual acuity improvement from baseline was reported in seven out of the eight patients at the 2-years trial endpoint follow-up [87]. The one patient from the high-dose group that reported no improvement experienced significant intraocular inflammation 2 weeks after treatment, which was attributed to the vector. Analysed as a group, the results from the Oxford trial show that the median visual improvement by ETDRS in the treated eyes was 5.5 letters above baseline at the 2-years follow-up [87].
Unlike the LCA2 trials, where direct comparisons between trials is challenging due to vector, construct and dose differences, all but one of the choroideremia trials used the exact same therapeutic agent developed by the Oxford team and at the same dose (Table 1). These trials recruited six patients each and the 12-months or 2-years follow-up results show that two to three of the treated eyes in each trial showed improved BCVA [88,89,90]. Interestingly, in the trial conducted in Germany (THOR, ClinicalTrials.gov identifier NCT02671539) [88], a significant improvement of visual acuity in the treated eye was observed at the 3-months follow-up in four out of six patients. This, however, declined at the 12-months follow-up to two out of six, but the minor changes in the other two patients indicate the maintenance of their baseline visual acuity. Furthermore, there was a shift in some patients of their preferred retinal locus used for fixation towards the treated area [88]. Overall in these trials, visual acuity in the untreated eyes showed a fairly stable progression but areas of preserved RPE cells appeared to decline at a similar rate between treated and untreated eyes [90]. Despite a lack of significant differences in retinal sensitivity, there was a trend towards improvement in the treated eyes [88,89,90]. The remaining trial, conducted by Spark Therapeutics (NCT02341807), is the only one that uses a different therapeutic construct. In this trial, the AAV2/2 construct incorporates the same CAG promoter, but not the WPRE used to increase gene expression present in the other trials [91].
2.1.3 The LHON Trials—Targeting Retinal Ganglion Cells
The third group of AAV2/2-based gene therapy clinical trials were for a retinal condition called Leber Hereditary Optic Neuropathy (LHON), an inherited mitochondrial disorder that is characterised by subacute central vision loss in one eye shortly followed by visual loss in the second eye, usually in the second to third decades of life [92]. The majority of mutations that cause LHON are present in mitochondrial genes involved in the mitochondrial respiratory chain and energy production [93]. In particular, mutations in the NADH dehydrogenase subunit 4 complex I (ND4) gene account for 60% of LHON cases worldwide [93]. Despite disease-causing mutations being present in genes expressed in all mitochondria, in LHON patients the disease phenotype is restricted to the loss of RGCs and degeneration of the optic nerve [92]. Different from LCA2 and choroideremia, which affect the photoreceptors and/or the RPE cells, a gene therapy approach for LHON must target the RGCs and, more specifically, deliver the therapeutic construct into the mitochondria. For this to occur successfully, gene therapy for LHON had some significant and unique challenges to overcome. First, as the target cells are the RGCs, the ideal delivery route is intravitreal because subretinal delivery of AAV has shown little to no RGC targeting in macaque eyes [94]. RGC targeting in macaques was slightly improved when AAV2/2 was delivered intravitreally [43]. Several studies have attempted, with some success, to improve intravitreal RGC transduction in non-human primates by surgically removing the inner limiting membrane [95, 96] or the vitreous [97], or by applying an electrical current [98]. Despite the poor RGC transduction rate in non-human primate retinas, AAV2/2 has become the vector of choice for RGC targeting based on successful transduction in the rodent retina [10]. The second challenge to overcome was that once in the RGCs, the AAV-delivered gene needs to reach the mitochondria. An elegant solution was provided by Guy and colleagues [99] by creating a synthetic ND4 subunit that allowed for allotropic expression plus the addition of a mitochondrial targeting sequence that provided effective trafficking to the mitochondria. This novel approach was validated in an LHON animal model [100] and was quickly moved towards clinical trials. Two groups have led the effort for the AAV2/2 LHON trials: the Huazhong University of Science and Technology team and the GenSight Biologics team. A third team based in the USA is behind the only trial currently recruiting, but as this trial uses a modified AAV2tYF capsid, it will be discussed in a separate section.
The results from both the GenSight and Huazhong University trials [101,102,103] were conducted in patients carrying the ND4-G11778A mutation and used a CMV promoter to drive gene expression. The Huazhong University trial injected a total of nine patients, where seven received a 1E10 gp dose and two, who were under 12 years of age at treatment, received a lower dose of 5E9 gp due to safety concerns. The GenSight trial used four different doses: 9E9, 3E10, 9E10 and 1.8E11 gp. No ocular adverse events were reported in the Huazhong University trial up to 36 months post-treatment [101], but quite a few treatment-emergent adverse events (TEAEs) were reported for the GenSight trial at 96 weeks post-treatment, especially in the higher dose cohorts [102]. They reported 96 TEAEs (40 systemic and 56 ocular), but 96% of these were considered mild. Of the ocular TEAEs, 61% were considered treatment-related and the most frequent type of event was intraocular inflammation. All ocular events resolved spontaneously or after appropriate treatment. The discrepancy in the reporting of ocular adverse events between these two trials is not unexpected as the higher dose used in the Huazhong University trial is very close to the lower dose administered in the GenSight trial. However, further analysis on the GenSight trial assessed if there was an association between an immune response and the intraocular inflammation reported after treatment [104]. They calculated a composite ocular inflammation score (OIS) to quantify the systemic immune response and showed that neither were associated with the administered dose, thus suggesting that intravitreal administration of AAV2/2-ND4 in LHON patients was safe [104]. In relation to treatment efficacy, both trials reported around half of the treated eyes showed significant improvement in BCVA compared with baseline. The Huazhong University trial also showed improvement in the visual field index in five out of nine treated eyes but no changes at 36 months on visual evoked potentials (VEPs; measure of optic nerve function) and thickness of the retinal nerve fibre layer. The results of the remaining ongoing trials by both groups, especially the two more recent trials that have recruited at least 90 patients each, will be eagerly awaited and hopefully provide more informative data regarding a treatment for LHON.
The group of LHON trials has included some of the most recent trials that have opted for a ubiquitous promoter such as CMV, where other trials have started to significantly shift towards the use of cell-specific promoters (Table 1). For example, from all trials started from 2017 (10 years from the start of the first LCA2 trials) onwards, 72% are using cell-specific promoters while only 4 out of the 14 trials are using ubiquitous ones. Within the LHON trials, the non-cell-specific nature of the CMV promoter is likely less of an issue due to the combination of an intravitreal delivery method that targets the RGCs and the presence of a mitochondrial targeting sequence providing effective trafficking to the mitochondria. However, high expression levels generated by a CMV promoter could potentially become toxic. Furthermore, it has been reported in other systems, including liver [105], muscle [106] and parts of the central nervous system [107, 108], that the CMV promoter can be silenced over time. This seems to be more the case in rapidly proliferating cells and stem cells, whereas in non-proliferating cells CMV-driven expression is much more stable. In the post-mitotic non-proliferative retina, CMV silencing has not yet been reported and long-term stable expression for up to 3 years has been shown in the canine retina [25]. Interestingly, however, some form of gene silencing may sometimes be useful because, dependent on the nature of the introduced transgene, chronic expression of a molecule—especially one that is secreted—can result in altered cell morphology [109] or altered expression of endogenous genes [110], with potential functional consequences.
2.1.4 Mutating AAV2/2—the AAV2tYF-Based Clinical Trials
In parallel to the discovery and development of novel AAV serotypes, further research into the biology of AAV vectors has allowed for targeted modifications of existing serotypes to improve tropism or efficiency. In 2008, Zhong and colleagues reported that mutating surface-exposed tyrosine residues on the AAV2 capsid reduced capsid ubiquitination and therefore allowed for increased transduction in vitro and in vivo [111]. This was further refined in a 2011 study by Petrs-Silva and colleagues, who tested the efficiency of combining multiple tyrosine mutant AAV2 vectors in transducing retinal cells [112]. They reported that a triple mutant vector (Y444,500,730F–AAV2tYF) was the most efficient at targeting RPE and photoreceptors after subretinal delivery [112]. The triple vector was also better than AAV2/2 and the other mutants at targeting RGCs and inner nuclear layer neurons after intravitreal delivery [112]. Furthermore, the addition of modified promoters may provide greater selectivity for RGCs after intravitreal delivery [113].
Based on the safety profile data for AAV2/2 and the improved tropism of AAV2tYF shown in pre-clinical studies, the use of the modified AAV2tYF vector in new clinical trials was not unexpected. There are currently five active trials for IRD conditions with AAV2tYF-based therapeutic delivery (Table 1). These include trials for LHON, X-linked RP, X-linked retinoschisis (RS) and achromatopsia (ACHM). However, results have only been reported so far for the US-based LHON trial [114, 115]. Similar to the other LHON trials, the delivery was intravitreal to target RGCs but they used a CAG promoter instead of CMV. Visual acuity improvement (at or above baseline) in the treated eye was reported mostly in patients (4/6) with acute bilateral visual loss (< 12 months’ onset) while bilateral chronic vision loss patients (≥ 12 months in one eye and at least 6 months in the other eye) only saw improvements in one of six treated eyes [115]. Furthermore, in treated eyes the baseline thickness of the retinal nerve fibre layer (RNFL) was maintained at 12 months while the untreated eyes showed a reduction in thickness over time [115]. This is a potentially significant result as none of the AAV2/2-based trials had shown improvement in RNFL thickness. The visual acuity results seen in this trial are similar to the ones reported in the other AAV2/2-based trials, where half of the treated patients saw improvements in their visual acuity after treatment. However, the difference in outcomes in the AAVtYF trial between the acute and chronic patients does raise the question concerning an optimal window for treatment in LHON. The remaining AAV2tYF trials are all sponsored by Applied Genetic Technologies Corp. and have not yet reported results. As clinical trials for these same conditions are also ongoing using AAV2/8 and AAV2/5, it will be interesting to compare results once they become available.
2.2 AAV2/4 and AAV2/5-Based Clinical Trials
Both AAV4 and AAV5 were described soon after AAV2 [116]. Subsequent testing in the mouse, canine and primate retinas following subretinal injections showed that AAV2/5 was capable of transducing RPE and photoreceptor cells with higher tropism and efficiency compared with AAV2/2 [117, 118], while AAV2/4 showed improved RPE cell transduction [118]. The RPE specificity of AAV2/4 and long-term expression in primate retinas [118, 119] led to studies investigating the use of this vector for the delivery of RPE65 to a LCA2 canine model [66, 67], providing the pre-clinical validation of an AAV2/4-based clinical trial for LCA2. The published results for this trial show that after treatment, visual acuity improvement was seen in a third of the treated eyes (all within the higher dose cohort) and the overall mean visual acuity in the treated eyes remained stable, while the untreated eye saw a decline in function [61].
The remaining trials are all AAV2/5-based and include an optimised vector for LCA2-RPE65 [120] led by the UK group behind one of the first LCA2 trials, for RP caused by mutations in the PDE6B gene and for X-linked RP caused by mutations in the RPGR gene. No data has been reported for these trials yet but will in the future provide an interesting comparison of vector efficiencies, especially for LCA2 and RP-RPGR.
2.2.1 The Gene Editing AAV2/5 Trial
Genome editing is at the forefront of precision medicine today, and when married with advances in AAV efficiency, specificity and deliverance, holds great promise for many inherited retinal disorders. This is especially relevant in conditions where the traditional gene replacement therapy will not work, such as autosomal inherited and mutations in genes too large to fit into an AAV vector. Genome editing is possible due to the action of targeted nucleases, which create site-specific double-strand breaks in the genome, and their advantage lies in the fact that they offer a permanent and precise in situ correction of genetic mutations causative of a disease. Several methods of genome editing have been developed and used in pre-clinical proof-of-principle studies, including meganucleases, zinc finger nucleases (ZFNs), transcription activator-like effector-based nucleases (TALEN) and the clustered regularly interspaced short palindromic repeats (CRISPR/Cas9) system [121]. Recently, CRISPR/Cas9 has emerged as the preferred system due to its flexibility and user-friendly design platform. While in the other systems the site recognition is mediated by the nuclease protein itself, in the CRISPR/Cas9 system this is done by a guide RNA (gRNA), significantly reducing the costs, complexity and time needed to design it [121]. CRISPR/Cas genome editing in the retina has been a growing area recently, with great potential for new treatment options [reviewed in 122].
The genome editing company Editas has taken advantage of this technology and launched in early 2019 the first genome editing clinical trial (NCT03872479, EDIT-101, also known as AGN-151587) combining CRISPR/Cas9 and AAV technologies to correct the IVS26 mutation (c.2991+1655A>G in intron 26) in the CEP290 gene that causes Leber Congenital Amaurosis type 10 (LCA10). The EDIT-101 therapeutic uses an AAV2/5 vector carrying two gRNA to recognise the mutation site and the Cas9 enzyme under the rhodopsin kinase promoter, limiting its expression to the targeted photoreceptor cells [123]. The results from this trial will be eagerly anticipated by the gene therapy field. A CRISPR/Cas9-based approach has the potential to treat inherited retinal conditions where the limitations of the AAV platform have hindered the development of treatment options. However, the mutation-specific design of a CRISPR/Cas9-based treatment does mean that, unlike traditional gene therapy treatments that work for all patients within a specific gene-affected condition, individual products will have to be developed for each different mutation within the same gene.
2.3 AAV2/8-Based Clinical Trials
AAV8 was isolated from non-human primates in 2002 and AAV2/8 vectors were shown to have up to 100-fold higher transduction capacity compared with other known capsids [124], especially for liver [125] and muscle cells [126]. In the retina, AAV2/8 also proved to be a more efficient vector compared with AAV2/2 and AAV2/5; it provided both faster onset and stronger transgene expression, especially in photoreceptors [127, 128]. From this point onwards, several pre-clinical gene therapy studies for IRDs started to use AAV2/8 in lieu of other serotypes and from 2015 onwards several clinical trials for IRDs using AAV2/8 vectors commenced (Table 1). There are currently six trials using AAV2/8: four for achromatopsia (CNGA3 and CNGB3 mutations), one for X-linked RPGR-RP and one for X-linked retinoschisis. All three conditions are recessive conditions due to mutations in genes affecting photoreceptors specifically. Thus, in contrast to the initial AAV2/2 trials, the selection of the AAV2/8 vector with stronger photoreceptor tropism was, therefore, more appropriate. These conditions do, however, have some crucial differences between them that was reflected in the design of each trial.
The AAV2/8 RPGR trial is led by the Oxford/NightStar team behind the choroideremia trials, and is the trial that has tested the highest number of doses, ranging from 5E9 to 4E11 gp. Similar to what they reported in the choroideremia trial, the dose received by each patient varied slightly as it was adjusted by the injection volume [129]. In the 6 months follow-up, Cehajic-Kapetanovic and colleagues [129] reported that visual acuity remained stable and similar to baseline in the treated eyes. This is not unexpected, as this study is only 6 months after treatment and visual acuity in the untreated eye has remained stable. Visual function gains compared with baseline by microperimetry measurement was variable and seen in around a third of treated eyes. Although the delivery route used in this study was subretinal, they reported mild inflammatory responses in eyes treated with higher vector doses (> 1E11 gp), all of which were resolved after oral treatment. It remains to be seen if a connection between visual gain and post-treatment inflammation will be present in the later follow-up studies and whether or not long-term improvement might be affected, especially because visual function improvement above baseline was not observed after gene therapy in a RPGR-deficient animal model [130].
Achromatopsia became a potential candidate for gene therapy clinical trials following the very successful rescue of cone-mediated vision after AAV-based gene therapy in several animal models of achromatopsia [131,132,133,134,135,136,137]. Different from the other outer retinal IRDs targeted so far, achromatopsia affects only the cone photoreceptors, with patients suffering from birth from absent colour vision, poor visual acuity and photophobia [138]. There are six genes that have been associated with achromatopsia and there are six clinical trials ongoing for two of the most common genes affected (CNGA3 and CNGB3; Table 1). However, data for only one of the trials (AAV2/8-based for CNGA3, NCT02610582) has been reported. All trials have opted to use cone-specific promoters such as the human cone arrestin promoter (hCARp) or promoters based on the red or green opsin promoter regions (PR1.7 and hG1.7p). The 12-months follow-up results from the AAV2/8-CNGA3 trial showed that treatment was well tolerated and that both visual acuity and contrast sensitivity was improved [139]. Interestingly, the eyes that received the lower dose showed better visual improvement compared with the eyes that received the higher doses. Further studies and data from the other trials might clarify whether this effect was due to the lower dose eyes having worse acuity and contrast sensitivity at baseline and, therefore, more room for improvement, or if the higher doses could have a detrimental effect on cone function. The reporting of significant improvements in half of the treated eyes in colour vision-specific tests provides encouragement for an AAV-based gene therapy treatment for achromatopsia [139]. However, achromatopsia is usually considered a fairly stable condition where patients do not experience a progressive loss of vision as the symptoms are present from birth. Under these circumstances, it is questionable whether a gene therapy treatment, and the associated risks, is necessary for these patients. Furthermore, since they have not possessed colour and high acuity vision since birth, experts are also in doubt whether the necessary, mature connections within the visual cortex for colour and high acuity vision have developed and if such connections can be established at a later stage of life.
The AAV2/8-based clinical trial for X-linked retinoschisis (XLRS) differs significantly from the achromatopsia and RPGR trials as XLRS patients have an extremely fragile retina due to the presence of schisis cavities (structural retinal lamellar separations) that are characteristic of this condition. Despite being a condition that affects photoreceptors directly, the fragile nature of the retina does not safely support subretinal delivery of a therapeutic. Successful restoration of the retinal architecture and closure of schisis cavities in a mouse model of XLRS was achieved after intravitreal delivery of an AAV2/8-RS1 vector [140] and provided encouragement that this approach could benefit patients. Unlike the results reported in the intravitreal AAV2/2 LHON trial by GenSight (discussed in the AAV2/2 section), an increase in ocular inflammation and antibodies against AAV2/8 after intravitreal AAV2/8-RS1 delivery was dose-dependent, but both were resolved by oral and topical corticosteroid treatment within 4–6 weeks. Visual acuity improvements at the 18-months follow-up was not considered significant due to the high testing variability for XLRS patients, and neither were any improvements seen in retinal sensitivity, electroretinogram or optical coherence tomography [141]. It is clear that intravitreal delivery of AAV-based therapeutics is possible albeit post-operative care needs to be in place to manage inflammation. However, the correlation between ocular inflammation events and treatment efficacy is still unclear and could potentially compromise the clinical application of intravitreally delivered AAV-based therapeutics.
3 Delivering Inserts for All Occasions—the Multipurpose Use of AAVs
Hundreds of genes have been implicated in IRDs, thus making specific gene therapy for each individual gene mutation an enormous task, from the labour-intensive lab research, to clinical testing, to regulatory approval for each one. Furthermore, the majority of gene therapy studies and clinical trials for IRDs have targeted genes involved in autosomal recessive disorders (i.e. those that create null genotypes); thus, replacing the gene to produce a functional protein can potentially be a straightforward approach. In contrast, other types of inheritance, such as autosomal dominant or gain of function, can create other challenges that limit the development of therapies using the AAV platform. Importantly, the use of AAV is not limited to direct replacement or correction of a disease-causing gene [142]. It can also be used to augment downstream processes and pathways, which may be beneficial for more eye diseases, including glaucoma, autosomal dominant optic atrophy, macular degeneration, retinal ischaemia and optic neuritis, providing an even broader range of potential therapeutic uses in ophthalmology. Thus, gene therapies that target a larger population of causative agents are very appealing, such as inducing and over-expressing neuroprotective factors [3, 143,144,145,146,147,148] and in experimental strategies that focus on novel, potentially therapeutic, optogenetic technologies [149, 150].
Glaucoma is a heterogeneous group of conditions characterised by progressive death of RGCs and associated visual field loss, sometimes leading to blindness in the most severe cases. While increased intraocular pressure is an important risk factor [151], and most current pharmacological or surgical strategies are aimed at pressure reduction, hereditable factors are also important in a proportion of the population. In paediatric glaucoma, for example, a number of candidate genes have been identified [152, 153]. For these individuals, additional neuroprotective strategies should be explored to further reduce the rate of RGC death and visual field loss [154]. Gene therapy is an effective tool to transduce RGCs, and AAV2/2-mediated delivery of neurotrophic factors such as brain-derived neurotrophic factor (BDNF) [155, 156] or ciliary neurotrophic factor (CNTF) [157] promote RGC viability in experimental models of glaucoma. A gene therapy protocol that increases expression of both BDNF and its receptor (TrkB) in RGCs is currently in pre-clinical development [146, 158]. Secretion of, for example, BDNF by transduced RGCs can have a beneficial bystander effect on neighbouring non-transduced neurons [159] and also may act indirectly via effects on resident Muller glia, releasing other supporting factors [160]. However, a possible downside to sustained neurotrophin expression in RGCs is the impact that the factors can have in altering the phenotype of, and gene expression in, other retinal neurons [110]. Note here that gene therapy to upregulate appropriate transcription factors such as Brn3b, and hence various downstream signalling pathways, has also been tested [161], as have viral vector approaches that prevent activation of death-related pathways [162].
In a model of retinal ischaemia/reperfusion injury, use of self-complementary AAV2/2 vectors to deliver the enzyme C3 transferase, which inactivates Rho GTPases to reduce apoptosis and enhance cytoskeletal stability, resulted in RGC protection [163]. In another study, using the experimental autoimmune encephalomyelitis (EAE) model of multiple sclerosis (MS), AAV2/2 was used to deliver either nuclear factor (erythroid derived)-like 2 (NRF2) or Sirtuin 1 (SRT1) to RGCs—both factors known to have beneficial anti-inflammatory effects and to be associated with anti-apoptotic and anti-oxidant effects [164]. Reduced RGC loss was seen but neither vector was able to reduce optic nerve inflammation or demyelination. On the other hand, using a similar EAE model in mice, intraocular delivery of AAV2/2 encoding a mutant phosphorylation-resistant version of collapsing response mediator protein 2 (CRMP2) not only protected RGCs and axon integrity, but also maintained axonal transport and preserved myelin in the optic nerve during active neuroinflammation [165, 166]. CRMP2 regulates tubulin dynamics, interacts with motor proteins kinesin and dynamin, and is important in the growth, maintenance and repair of neuronal processes. CRMP2 activity is inhibited when phosphorylated, resulting in destabilisation of cytoskeletal proteins, reduced growth, degeneration of axons and disruption of axonal transport systems. It is of interest that the same AAV2/2 vector protects RGCs and myelin after partial optic nerve trauma [147], and could be useful in glaucoma, given that there is evidence of disrupted axonal transport and breakdown of microtubules in RGC axons that precedes RGC loss [167, 168].
4 Antisense Oligonucleotides (ASO), the Anti-AAV?
In recent years, one technology has been gaining ground and started to offer an alternative approach to AAV-based therapies for IRDs. ASOs are short synthetic and single-stranded nucleic acid sequences that bind to selected sequences of mRNA and manipulate gene expression by targeting a pathogenic mutation or splicing defects [169]. In contrast to AAV-based constructs, the size of the gene is not a limitation when designing ASO-based therapies [169]. The first generation of ASOs inhibited gene expression by degrading the target mRNA through RNase-H-mediated cleavage. This generation appeared after chemical modifications that improved their binding affinity and increased the resistance of ASOs to nucleases, and include the phosphorothioate backbone (PS) class, which has the ability to interfere with splicing but is highly toxic [170,171,172]. The second generation of ASOs was a result of further modification that reduced toxicity and improved target specificity [173, 174]. Several ASOs have been approved by the FDA and include eteplirsen and golodirsen for Duchenne muscular dystrophy, fomivirsen for cytomegalovirus retinitis, milasen for Batten disease, mipomersen for homozygous familial hypercholesterolaemia and nusinersen for spinal muscular atrophy.
Similar to Luxturna, which was the first-ever FDA-approved gene therapy, the first antisense oligonucleotide therapy was approved for an ocular condition. The drug was called fomivirsen and used for the treatment of cytomegalovirus retinitis in immuno-compromised patients [175]. More recent studies have successfully applied ASO technology to treat IRDs, including conditions where traditional AAV-based gene therapy approaches would be limited. These include large genes such as ABCA4, CEP290 and some Usher genes, and dominant RP (reviewed in [176]). In contrast to AAV gene replacement, ASO can be used to treat vision loss in Stargardt disease due to deep intronic mutations in the ABCA4 gene [177] and effectively provide in vitro allele-specific knock-down of the mutant allele causing a dominant negative effect in NR2E3-associated autosomal dominant RP [178]. Furthermore, a study evaluating ASOs targeting the ATAXIN-7 gene as a treatment strategy for spinocerebellar ataxia type 7 (SCA7; an autosomal dominant neurodegenerative disorder characterised by cerebellar and retinal degeneration) showed improved visual function, retinal histopathology and retinal gene expression in a mouse model of SCA7, suggesting that ASOs targeting ATAXIN-7 might represent a viable treatment for SCA7 retinal degeneration [179]. Pre-clinical studies testing ASOs for LCA10 caused by mutations in CEP290 [180] and Usher 2A-associated RP [181] have shown the most promising results to date, allowing for the advancement of these treatments towards clinical trials (NCT03780257, NCT03140969). The ASO-based therapeutic approach remains an exciting alternative to viral-based gene therapies and future developments in this field are expected to continue to grow.
5 Concluding Remarks
Despite the promising success of the recent LCA2 trials, which ultimately led to the approval of the first ocular gene therapy drug Luxturna®, the translation of retinal gene therapy from lab bench to bedside is still an ongoing process where both sides need to evolve in an interdependent manner. It is essential that to advance the next generation of breakthrough retinal trials, improvements from both basic and clinical research should come together; a thorough understanding of the molecular mechanisms of degeneration needs to marry with a thorough clinical characterisation of the disease process. The increase in clinical trials evaluating the natural history of different ocular conditions, the growing availability and technological advancements in the study of animal models of disease and development of innovative human disease models such as retinal organoids that can bridge some of the limitations of animal model study, are all encouraging developments in the ocular translational field.
Huge strides are also being made in generating better AAV vectors with a focus on human clinical translation. The development of novel capsids and an increased assessment in non-human primates (NHP) of these novel serotypes can help underscore the differences in AAV transduction between mice and primates, helping consolidate the importance of careful evaluation of therapeutic vectors in NHPs prior to clinical trials. Furthermore, NHP studies are crucial in advancing our understanding of potential adverse immune responses to AAV-based therapeutics. One of the prized properties of AAV vectors is the minimal stimulation of the host immune system, and whilst minimal, it is not negligible as inflammation/toxicity responses have recently been attributed to AAV-cis regulatory sequences [182]. Studies looking into different genetic modification of wild-type AAV antigenic epitopes that can produce synthetic variants capable of evading neutralising antibodies without sacrificing production, transduction efficiency or tissue tropism will be extremely valuable towards improving future AAV-based therapeutics [183].
The versatility of AAVs has allowed the gene therapy, and in particular, the ocular gene therapy field to grow exponentially in the last decade and provide hope for the development of a cure for a myriad of conditions that until recently were thought to be incurable. Further developments in capsid and vector engineering, in-depth understanding of vector and host interactions, and growing clinical knowledge of vision loss conditions will continue to come together to provide clinicians and researchers with the tools necessary to advance these innovative treatments forward.
References
Diaz-Coranguez M, Ramos C, Antonetti DA. The inner blood-retinal barrier: cellular basis and development. Vis Res. 2017;139:123–37.
Bennett J. Immune response following intraocular delivery of recombinant viral vectors. Gene Ther. 2003;10(11):977–82.
Hellstrom M, Harvey AR. Retinal ganglion cell gene therapy and visual system repair. Curr Gene Ther. 2011;11(2):116–31.
Ochakovski GA, Bartz-Schmidt KU, Fischer MD. Retinal gene therapy: surgical vector delivery in the translation to clinical trials. Front Neurosci. 2017;11:174.
Jolly JK, Bridge H, MacLaren RE. Outcome measures used in ocular gene therapy trials: a scoping review of current practice. Front Pharmacol. 2019;10:1076.
Hu M, Easter SS. Retinal neurogenesis: the formation of the initial central patch of postmitotic cells. Dev Biol. 1999;207(2):309–21.
Surace EM, Auricchio A. Versatility of AAV vectors for retinal gene transfer. Vis Res. 2008;48(3):353–9.
Wang D, Tai PWL, Gao G. Adeno-associated virus vector as a platform for gene therapy delivery. Nat Rev Drug Discov. 2019;18(5):358–78.
Verdera HC, Kuranda K, Mingozzi F. AAV vector immunogenicity in humans: a long journey to successful gene transfer. Mol Ther. 2020;28(3):723–46.
Hellstrom M, et al. Cellular tropism and transduction properties of seven adeno-associated viral vector serotypes in adult retina after intravitreal injection. Gene Ther. 2009;16(4):521–32.
Ling C, et al. Development of optimized AAV serotype vectors for high-efficiency transduction at further reduced doses. Hum Gene Ther Methods. 2016;27(4):143–9.
Ali RR, et al. Gene transfer into the mouse retina mediated by an adeno-associated viral vector. Hum Mol Genet. 1996;5(5):591–4.
Flotte TR, Berns KI. Adeno-associated virus: a ubiquitous commensal of mammals. Hum Gene Ther. 2005;16(4):401–7.
Flotte TR, Afione SA, Zeitlin PL. Adeno-associated virus vector gene expression occurs in nondividing cells in the absence of vector DNA integration. Am J Respir Cell Mol Biol. 1994;11(5):517–21.
Atchison RW, Casto BC, Hammon WM. Adenovirus-associated defective virus particles. Science. 1965;149(3685):754–6.
Zinn E, Vandenberghe LH. Adeno-associated virus: fit to serve. Curr Opin Virol. 2014;8:90–7.
Li C, Samulski RJ. Engineering adeno-associated virus vectors for gene therapy. Nat Rev Genet. 2020;21(4):255–72.
Hudry E, Vandenberghe LH. Therapeutic AAV gene transfer to the nervous system: a clinical reality. Neuron. 2019;101(5):839–62.
Bedbrook CN, Deverman BE, Gradinaru V. Viral strategies for targeting the central and peripheral nervous systems. Annu Rev Neurosci. 2018;41:323–48.
Bennett J, et al. Stable transgene expression in rod photoreceptors after recombinant adeno-associated virus-mediated gene transfer to monkey retina. Proc Natl Acad Sci USA. 1999;96(17):9920–5.
Bennett J, et al. Photoreceptor cell rescue in retinal degeneration (rd) mice by in vivo gene therapy. Nat Med. 1996;2(6):649–54.
Jomary C, et al. Rescue of photoreceptor function by AAV-mediated gene transfer in a mouse model of inherited retinal degeneration. Gene Ther. 1997;4(7):683–90.
Acland GM, et al. Gene therapy restores vision in a canine model of childhood blindness. Nat Genet. 2001;28(1):92–5.
Narfstrom K, et al. Functional and structural recovery of the retina after gene therapy in the RPE65 null mutation dog. Investig Ophthalmol Vis Sci. 2003;44(4):1663–72.
Acland GM, et al. Long-term restoration of rod and cone vision by single dose rAAV-mediated gene transfer to the retina in a canine model of childhood blindness. Mol Ther. 2005;12(6):1072–82.
Erles K, Sebokova P, Schlehofer JR. Update on the prevalence of serum antibodies (IgG and IgM) to adeno-associated virus (AAV). J Med Virol. 1999;59(3):406–11.
Zolotukhin S, et al. Production and purification of serotype 1, 2, and 5 recombinant adeno-associated viral vectors. Methods. 2002;28(2):158–67.
Rabinowitz JE, et al. Cross-packaging of a single adeno-associated virus (AAV) type 2 vector genome into multiple AAV serotypes enables transduction with broad specificity. J Virol. 2002;76(2):791–801.
Gao G, Vandenberghe LH, Wilson JM. New recombinant serotypes of AAV vectors. Curr Gene Ther. 2005;5(3):285–97.
Carvalho LS, et al. Evaluating efficiencies of dual AAV approaches for retinal targeting. Front Neurosci. 2017;11:503.
Maddalena A, et al. Triple vectors expand AAV transfer capacity in the retina. Mol Ther. 2018;26(2):524–41.
Lee JH, et al. Gene therapy for visual loss: opportunities and concerns. Prog Retin Eye Res. 2019;68:31–53.
Khatib TZ, Martin KR. Neuroprotection in glaucoma: towards clinical trials and precision medicine. Curr Eye Res. 2020;45(3):327–38.
Duncan JL, et al. Inherited retinal degenerations: current landscape and knowledge gaps. Transl Vis Sci Technol. 2018;7(4):6.
Berger W, Kloeckener-Gruissem B, Neidhardt J. The molecular basis of human retinal and vitreoretinal diseases. Prog Retin Eye Res. 2010;29(5):335–75.
Talib M, et al. Clinical and genetic characteristics of male patients with RPGR-associated retinal dystrophies: a long-term follow-up study. Retina. 2019;39(6):1186–99.
Carvalho LS, Vandenberghe LH. Promising and delivering gene therapies for vision loss. Vis Res. 2015;111(Pt B):124–33.
Bennett J, et al. Real-time, noninvasive in vivo assessment of adeno-associated virus-mediated retinal transduction. Investig Ophthalmol Vis Sci. 1997;38(13):2857–63.
Rolling F, et al. Evaluation of adeno-associated virus-mediated gene transfer into the rat retina by clinical fluorescence photography. Hum Gene Ther. 1999;10(4):641–8.
Ali RR, et al. Restoration of photoreceptor ultrastructure and function in retinal degeneration slow mice by gene therapy. Nat Genet. 2000;25(3):306–10.
Dalkara D, et al. Inner limiting membrane barriers to AAV-mediated retinal transduction from the vitreous. Mol Ther. 2009;17(12):2096–102.
Harvey AR, et al. Intravitreal injection of adeno-associated viral vectors results in the transduction of different types of retinal neurons in neonatal and adult rats: a comparison with lentiviral vectors. Mol Cell Neurosci. 2002;21(1):141–57.
Yin L, et al. Intravitreal injection of AAV2 transduces macaque inner retina. Investig Ophthalmol Vis Sci. 2011;52(5):2775–83.
Yu H, et al. Longterm reversal of severe visual loss by mitochondrial gene transfer in a mouse model of Leber hereditary optic neuropathy. Sci Rep. 2018;8(1):5587.
Bainbridge JW, et al. Effect of gene therapy on visual function in Leber’s congenital amaurosis. N Engl J Med. 2008;358(21):2231–9.
Hauswirth WW, et al. Treatment of Leber congenital amaurosis due to RPE65 mutations by ocular subretinal injection of adeno-associated virus gene vector: short-term results of a phase I trial. Hum Gene Ther. 2008;19(10):979–90.
Maguire AM, et al. Safety and efficacy of gene transfer for Leber’s congenital amaurosis. N Engl J Med. 2008;358(21):2240–8.
Cideciyan AV, et al. Human gene therapy for RPE65 isomerase deficiency activates the retinoid cycle of vision but with slow rod kinetics. Proc Natl Acad Sci USA. 2008;105(39):15112–7.
Narfstrom K, et al. Morphological aspects related to long-term functional improvement of the retina in the 4 years following rAAV-mediated gene transfer in the RPE65 null mutation dog. Adv Exp Med Biol. 2008;613:139–46.
Cideciyan AV, et al. Human RPE65 gene therapy for Leber congenital amaurosis: persistence of early visual improvements and safety at 1 year. Hum Gene Ther. 2009;20(9):999–1004.
Maguire AM, et al. Age-dependent effects of RPE65 gene therapy for Lebers congenital amaurosis: a phase 1 dose-escalation trial. Lancet. 2009;374(9701):1597–605.
Simonelli F, et al. Gene therapy for Leber’s congenital amaurosis is safe and effective through 1.5 years after vector administration. Mol Ther. 2010;18(3):643–50.
Jacobson SG, et al. Gene therapy for Leber congenital amaurosis caused by RPE65 mutations: safety and efficacy in 15 children and adults followed up to 3 years. Arch Ophthalmol. 2012;130(1):9–24.
Bennett J, et al. AAV2 gene therapy readministration in three adults with congenital blindness. Sci Transl Med. 2012;4(120):120ra15.
Cideciyan AV, et al. Human retinal gene therapy for Leber congenital amaurosis shows advancing retinal degeneration despite enduring visual improvement. Proc Natl Acad Sci USA. 2013;110(6):E517–25.
Testa F, et al. Three-year follow-up after unilateral subretinal delivery of adeno-associated virus in patients with Leber congenital Amaurosis type 2. Ophthalmology. 2013;120(6):1283–91.
Bainbridge JW, et al. Long-term effect of gene therapy on Leber’s congenital amaurosis. N Engl J Med. 2015;372(20):1887–97.
Pierce EA, Bennett J. The status of RPE65 gene therapy trials: safety and efficacy. Cold Spring Harb Perspect Med. 2015;5(9):a017285.
Bennett J, et al. Safety and durability of effect of contralateral-eye administration of AAV2 gene therapy in patients with childhood-onset blindness caused by RPE65 mutations: a follow-on phase 1 trial. Lancet. 2016;388(10045):661–72.
Weleber RG, et al. Results at 2 years after gene therapy for RPE65-deficient Leber congenital amaurosis and severe early-childhood-onset retinal dystrophy. Ophthalmology. 2016;123(7):1606–20.
Le Meur, G., et al., Safety and long-term efficacy of AAV4 gene therapy in patients with RPE65 Leber congenital amaurosis. Mol Ther. 2017.
Russell S, et al. Efficacy and safety of voretigene neparvovec (AAV2-hRPE65v2) in patients with RPE65-mediated inherited retinal dystrophy: a randomised, controlled, open-label, phase 3 trial. Lancet. 2017;390(10097):849–60.
Redmond TM, et al. Rpe65 is necessary for production of 11-cis-vitamin A in the retinal visual cycle. Nat Genet. 1998;20(4):344–51.
Redmond TM, et al. Mutation of key residues of RPE65 abolishes its enzymatic role as isomerohydrolase in the visual cycle. Proc Natl Acad Sci USA. 2005;102(38):13658–63.
Bennicelli J, et al. Reversal of blindness in animal models of Leber congenital amaurosis using optimized AAV2-mediated gene transfer. Mol Ther J Am Soc Gene Ther. 2008;16(3):458–65.
Rolling F, et al. Gene therapeutic prospects in early onset of severe retinal dystrophy: restoration of vision in RPE65 Briard dogs using an AAV serotype 4 vector that specifically targets the retinal pigmented epithelium. Bull Mem Acad R Med Belg. 2006;161(10–12):497–508 (discussion 508–9).
Le Meur G, et al. Restoration of vision in RPE65-deficient Briard dogs using an AAV serotype 4 vector that specifically targets the retinal pigmented epithelium. Gene Ther. 2007;14(4):292–303.
Smith AJ, et al. AAV-Mediated gene transfer slows photoreceptor loss in the RCS rat model of retinitis pigmentosa. Mol Ther. 2003;8(2):188–95.
Jacobson SG, et al. Improvement and decline in vision with gene therapy in childhood blindness. N Engl J Med. 2015;372(20):1920–6.
Pennesi ME, et al. Results at 5 years after gene therapy for RPE65-deficient retinal dystrophy. Hum Gene Ther. 2018;29(12):1428–37.
Banin E, et al. Molecular anthropology meets genetic medicine to treat blindness in the North African Jewish population: human gene therapy initiated in Israel. Hum Gene Ther. 2010;21(12):1749–57.
Wang X, et al. The effect of human gene therapy for RPE65-associated Leber’s congenital amaurosis on visual function: a systematic review and meta-analysis. Orphanet J Rare Dis. 2020;15(1):49.
Ghazi NG, et al. Treatment of retinitis pigmentosa due to MERTK mutations by ocular subretinal injection of adeno-associated virus gene vector: results of a phase I trial. Hum Genet. 2016;135(3):327–43.
Ashtari M et al. Plasticity of the human visual system after retinal gene therapy in patients with Leber’s congenital amaurosis. Sci Transl Med 2015;7(296):296ra110.
Maguire AM, et al. Efficacy, safety, and durability of voretigene neparvovec-rzyl in RPE65 mutation-associated inherited retinal dystrophy. Ophthalmology. 2019;126(9):1273–85.
Sorsby A, et al. Choroideremia; clinical and genetic aspects. Br J Ophthalmol. 1952;36(10):547–81.
Khan KN, et al. Clinical and genetic features of choroideremia in childhood. Ophthalmology. 2016;123(10):2158–65.
Moosajee M et al. Clinical utility gene card for: choroideremia. Eur J Hum Genet. 2014;22(4).
Sankila EM, et al. Aberrant splicing of the CHM gene is a significant cause of choroideremia. Nat Genet. 1992;1(2):109–13.
Preising M, Ayuso C. Rab escort protein 1 (REP1) in intracellular traffic: a functional and pathophysiological overview. Ophthal Genet. 2004;25(2):101–10.
Krock BL, Bilotta J, Perkins BD. Noncell-autonomous photoreceptor degeneration in a zebrafish model of choroideremia. Proc Natl Acad Sci USA. 2007;104(11):4600–5.
Morgan JI, et al. High-resolution adaptive optics retinal imaging of cellular structure in choroideremia. Investig Ophthalmol Vis Sci. 2014;55(10):6381–97.
Tolmachova T, et al. Independent degeneration of photoreceptors and retinal pigment epithelium in conditional knockout mouse models of choroideremia. J Clin Investig. 2006;116(2):386–94.
Cremers FP, et al. Cloning of a gene that is rearranged in patients with choroideraemia. Nature. 1990;347(6294):674–7.
MacLaren RE, et al. Retinal gene therapy in patients with choroideremia: initial findings from a phase 1/2 clinical trial. Lancet. 2014;383(9923):1129–37.
Edwards TL, et al. Visual acuity after retinal gene therapy for choroideremia. N Engl J Med. 2016;374(20):1996–8.
Xue K, et al. Beneficial effects on vision in patients undergoing retinal gene therapy for choroideremia. Nat Med. 2018;24(10):1507–12.
Fischer MD, et al. Changes in retinal sensitivity after gene therapy in choroideremia. Retina. 2020;40(1):160–8.
Lam BL, et al. Choroideremia gene therapy phase 2 clinical trial: 24-month results. Am J Ophthalmol. 2019;197:65–73.
Dimopoulos IS, et al. Two-year results after AAV2-mediated gene therapy for choroideremia: the Alberta experience. Am J Ophthalmol. 2018;193:130–42.
Loeb JE, et al. Enhanced expression of transgenes from adeno-associated virus vectors with the woodchuck hepatitis virus posttranscriptional regulatory element: implications for gene therapy. Hum Gene Ther. 1999;10:2295–305.
Jurkute N, et al. Clinical utility gene card for: inherited optic neuropathies including next-generation sequencing-based approaches. Eur J Hum Genet. 2019;27(3):494–502.
Wallace DC, et al. Mitochondrial DNA mutation associated with Leber’s hereditary optic neuropathy. Science. 1988;242(4884):1427–30.
Vandenberghe LH, et al. Dosage thresholds for AAV2 and AAV8 photoreceptor gene therapy in monkey. Sci Trans Med. 2011;3(112):112–9.
Boye SE, et al. Highly efficient delivery of adeno-associated viral vectors to the primate retina. Hum Gen Ther. 2016;27(8):580–97.
Takahashi K, et al. Improved intravitreal AAV-mediated inner retinal gene transduction after surgical internal limiting membrane peeling in cynomolgus monkeys. Mol Ther. 2017;25(1):296–302.
Kizito-Tshitoko T, et al. Vitrectomy before intravitreal injection of AAV2/2 vector promotes efficient transduction of retinal ganglion cells in dogs and nonhuman primates. Hum Gen Ther Methods. 2016;27(3):122–34.
Song H, et al. Trans-ocular electric current in vivo enhances AAV-mediated retinal gene transduction after intravitreal vector administration. Mol Ther Methods Clin Dev. 2019;13:77–85.
Guy J, et al. Rescue of a mitochondrial deficiency causing Leber hereditary optic neuropathy. Ann Neurol. 2002;52(5):534–42.
Cwerman-Thibault H, et al. Nuclear expression of mitochondrial ND4 leads to the protein assembling in complex I and prevents optic atrophy and visual loss. Mol Ther Methods Clin Dev. 2015;2:15003.
Yang S, et al. Long-term outcomes of gene therapy for the treatment of Leber’s hereditary optic neuropathy. EBioMedicine. 2016;10:258–68.
Vignal C, et al. Safety of rAAV2/2-ND4 gene therapy for Leber hereditary optic neuropathy. Ophthalmology. 2018;125(6):945–7.
Zhang Y, et al. Three cases of Leber’s hereditary optic neuropathy with rapid increase in visual acuity after gene therapy. Curr Gene Ther. 2019;19(2):134–8.
Bouquet C, et al. Immune response and intraocular inflammation in patients with Leber hereditary optic neuropathy treated with intravitreal injection of recombinant adeno-associated virus 2 carrying the ND4 gene: a secondary analysis of a phase 1/2 clinical trial. JAMA Ophthalmol. 2019;137(4):399–406.
Xu L, et al. CMV-β-actin promoter directs higher expression from an adeno-associated viral vector in the liver than the cytomegalovirus or elongation factor 1α promoter and results in therapeutic levels of human factor X in mice. Hum Gene Ther. 2001;12:563–73.
Brooks AR, et al. Transcriptional silencing is associated with extensive methylation of the CMV promoter following adenoviral gene delivery to muscle. J Gene Med. 2004;6(4):395–404.
Nieuwenhuis B, et al. Optimization of adeno-associated viral vector-mediated transduction of the corticospinal tract: comparison of four promoters. Gene Ther. 2020. https://doi.org/10.1038/s41434-020-0169-1.
Paterna JC, et al. Influence of promoter and WHV post-transcriptional regulatory element on AAV-mediated transgene expression in the rat brain. Gene Ther. 2000;7:1304–11.
Rodger J, et al. Long-term gene therapy causes transgene-specific changes in the morphology of regenerating retinal ganglion cells. PLoS ONE. 2012;7(2):e31061.
LeVaillant CJ, et al. Significant changes in endogenous retinal gene expression assessed 1 year after a single intraocular injection of AAV-CNTF or AAV-BDNF. Mol Ther Methods Clin Dev. 2016;3:16078.
Zhong L, et al. Next generation of adeno-associated virus 2 vectors: point mutations in tyrosines lead to high-efficiency transduction at lower doses. Proc Natl Acad Sci USA. 2008;105(22):7827–32.
Petrs-Silva H, et al. Novel properties of tyrosine-mutant AAV2 vectors in the mouse retina. Mol Ther. 2011;19(2):293–301.
Hanlon KS, et al. A novel retinal ganglion cell promoter for utility in AAV vectors. Front Neurosci. 2017;11:521.
Feuer WJ, et al. Gene therapy for Leber hereditary optic neuropathy: initial results. Ophthalmology. 2016;123(3):558–70.
Guy J, et al. Gene therapy for Leber hereditary optic neuropathy: low- and medium-dose visual results. Ophthalmology. 2017;124(11):1621–34.
Rutledge EA, Halbert CL, Russell DW. Infectious clones and vectors derived from adeno-associated virus (AAV) serotypes other than AAV type 2. J Virol. 1998;72(1):309–19.
Auricchio A, et al. Exchange of surface proteins impacts on viral vector cellular specificity and transduction characteristics: the retina as a model. Hum Mol Genet. 2001;10(26):3075–81.
Weber M, et al. Recombinant adeno-associated virus serotype 4 mediates unique and exclusive long-term transduction of retinal pigmented epithelium in rat, dog, and nonhuman primate after subretinal delivery. Mol Ther. 2003;7(6):774–81.
Stieger K, et al. Long-term doxycycline-regulated transgene expression in the retina of nonhuman primates following subretinal injection of recombinant AAV vectors. Mol Ther. 2006;13(5):967–75.
Georgiadis A, et al. Correction: Development of an optimized AAV2/5 gene therapy vector for Leber congenital amaurosis owing to defects in RPE65. Gene Ther. 2018;25(6):450.
Gaj T, et al. Genome-editing technologies: principles and applications. Cold Spring Harbor Perspect Biol. 2016;8(12):a023754.
Benati D, et al. Gene editing prospects for treating inherited retinal diseases. J Med Genet. 2020;57:437–44.
First CRISPR therapy dosed. Nat Biotechnol. 2020;38(4):382.
Gao GP, et al. Novel adeno-associated viruses from rhesus monkeys as vectors for human gene therapy. Proc Natl Acad Sci USA. 2002;99(18):11854–9.
Conlon TJ, et al. Efficient hepatic delivery and expression from a recombinant adeno-associated virus 8 pseudotyped alpha1-antitrypsin vector. Mol Ther. 2005;12(5):867–75.
Louboutin JP, Wang L, Wilson JM. Gene transfer into skeletal muscle using novel AAV serotypes. J Gene Med. 2005;7(4):442–51.
Natkunarajah M, et al. Assessment of ocular transduction using single-stranded and self-complementary recombinant adeno-associated virus serotype 2/8. Gene Ther. 2008;15(6):463–7.
Allocca M, et al. Novel adeno-associated virus serotypes efficiently transduce murine photoreceptors. J Virol. 2007;81(20):11372–80.
Cehajic-Kapetanovic J, et al. Initial results from a first-in-human gene therapy trial on X-linked retinitis pigmentosa caused by mutations in RPGR. Nat Med. 2020;26(3):354–9.
Deng WT, et al. Stability and safety of an AAV vector for treating RPGR-ORF15 X-linked retinitis pigmentosa. Hum Gene Ther. 2015;26(9):593–602.
Alexander JJ, et al. Restoration of cone vision in a mouse model of achromatopsia. Nat Med. 2007;13(6):685–7.
Pang JJ, et al. Achromatopsia as a potential candidate for gene therapy. Adv Exp Med Biol. 2010;664:639–46.
Michalakis S, et al. Restoration of cone vision in the CNGA3-/- mouse model of congenital complete lack of cone photoreceptor function. Mol Ther. 2010;18(12):2057–63.
Komaromy AM, et al. Gene therapy rescues cone function in congenital achromatopsia. Hum Mol Genet. 2010;19(13):2581–93.
Carvalho LS, et al. Long-term and age-dependent restoration of visual function in a mouse model of CNGB3-associated achromatopsia following gene therapy. Hum Mol Genet. 2011;20(16):3161–75.
Michalakis S, et al. Gene therapy restores missing cone-mediated vision in the CNGA3-/- mouse model of achromatopsia. Adv Exp Med Biol. 2012;723:183–9.
Pang JJ, et al. AAV-mediated cone rescue in a naturally occurring mouse model of CNGA3-achromatopsia. PLoS One. 2012;7(4):e35250.
Thiadens AA, et al. Genetic etiology and clinical consequences of complete and incomplete achromatopsia. Ophthalmology. 2009;116(10):1984–9.
Fischer MD et al. Safety and vision outcomes of subretinal gene therapy targeting cone photoreceptors in achromatopsia: a nonrandomized controlled trial. JAMA Ophthalmol. 2020.
Bush RA, et al. Preclinical dose-escalation study of intravitreal AAV-RS1 gene therapy in a mouse model of X-linked retinoschisis: dose-dependent expression and improved retinal structure and function. Hum Gene Ther. 2016;27(5):376–89.
Cukras C, et al. Retinal AAV8-RS1 gene therapy for X-linked retinoschisis: initial findings from a phase I/IIa trial by intravitreal delivery. Mol Ther. 2018;26(9):2282–94.
Ramlogan-Steel CA, et al. Gene therapy and the adeno-associated virus in the treatment of genetic and acquired ophthalmic diseases in humans: trials, future directions and safety considerations. Clin Exp Ophthalmol. 2019;47(4):521–36.
Wubben TJ, et al. Retinal neuroprotection: overcoming the translational roadblocks. Am J Ophthalmol. 2018;192:15–22.
Wubben TJ, Zacks DN, Besirli CG. Retinal neuroprotection: current strategies and future directions. Curr Opin Ophthalmol. 2019;30(3):199–205.
Yungher BJ, Ribeiro M, Park KK. Regenerative responses and axon pathfinding of retinal ganglion cells in chronically injured mice. Investig Ophthalmol Vis Sci. 2017;58(3):1743–50.
Osborne A, et al. Design of a novel gene therapy construct to achieve sustained brain-derived neurotrophic factor signaling in neurons. Hum Gene Ther. 2018;29(7):828–41.
Chiha W, et al. Intravitreal application of AAV-BDNF or mutant AAV-CRMP2 protects retinal ganglion cells and stabilizes axons and myelin after partial optic nerve injury. Exp Neurol. 2020;326:113167.
Zaninello M, et al. Inhibition of autophagy curtails visual loss in a model of autosomal dominant optic atrophy. Nat Commun. 2020;11(1):4029.
Scholl HP, et al. Emerging therapies for inherited retinal degeneration. Sci Transl Med. 2016;8(368):368rv6.
Lu Q, et al. Comparison of AAV-mediated optogenetic vision restoration between retinal ganglion cell expression and ON bipolar cell targeting. Mol Ther Methods Clin Dev. 2020;18:15–23.
Friedman DS, et al. An evidence-based assessment of risk factors for the progression of ocular hypertension and glaucoma. Am J Ophthalmol. 2004;138(3 Suppl):S19–31.
Ling C, et al. Updates on the molecular genetics of primary congenital glaucoma (Review). Exp Ther Med. 2020;20(2):968–77.
Gauthier AC. Childhood glaucoma genes and phenotypes: Focus on FOXC1 mutations causing anterior segment dysgenesis and hearing loss. Exp Eye Res. 2020;190:107893.
Almasieh M, Levin LA. Neuroprotection in Glaucoma: Animal Models and Clinical Trials. Annu Rev Vis Sci. 2017;3:91–120.
Martin KR, et al. Gene therapy with brain-derived neurotrophic factor as a protection: retinal ganglion cells in a rat glaucoma model. Invest Ophthalmol Vis Sci. 2003;44(10):4357–65.
Ren R, et al. Long-term rescue of rat retinal ganglion cells and visual function by AAV-mediated BDNF expression after acute elevation of intraocular pressure. Invest Ophthalmol Vis Sci. 2012;53(2):1003–11.
Pease ME, et al. Effect of CNTF on retinal ganglion cell survival in experimental glaucoma. Invest Ophthalmol Vis Sci. 2009;50(5):2194–200.
Osborne A, et al. Neuroprotection of retinal ganglion cells by a novel gene therapy construct that achieves sustained enhancement of brain-derived neurotrophic factor/tropomyosin-related kinase receptor-B signaling. Cell Death Dis. 2018;9(10):1007.
Leaver SG, et al. AAV-mediated expression of CNTF promotes long-term survival and regeneration of adult rat retinal ganglion cells. Gene Ther. 2006;13(18):1328–41.
Kimura A et al. Neuroprotection, growth factors and BDNF-TrkB signalling in retinal degeneration. Int J Mol Sci. 2016;17(9).
Phatak NR, Stankowska DL, Krishnamoorthy RR. Bcl-2, Bcl-xL, and p-AKT are involved in neuroprotective effects of transcription factor Brn3b in an ocular hypertension rat model of glaucoma. Mol Vis. 2016;22:1048–61.
McKinnon SJ, et al. Baculoviral IAP repeat-containing-4 protects optic nerve axons in a rat glaucoma model. Mol Ther. 2002;5:780–7.
Tan J, et al. scAAV2-mediated C3 transferase gene therapy in a rat model with retinal ischemia/reperfusion injuries. Mol Ther Methods Clin Dev. 2020;17:894–903.
McDougald DS, et al. SIRT1 and NRF2 gene transfer mediate distinct neuroprotective effects upon retinal ganglion cell survival and function in experimental optic neuritis. Investig Ophthalmol Vis Sci. 2018;59(3):1212–20.
Petratos S, et al. Limiting multiple sclerosis related axonopathy by blocking Nogo receptor and CRMP-2 phosphorylation. Brain. 2012;135(Pt 2):1794–818.
Lee JY, et al. Limiting neuronal nogo receptor signaling during experimental autoimmune encephalomyelitis preserves axonal transport and abrogates inflammatory demyelination. J Neurosci. 2019;39(28):5562–80.
Fortune B, et al. Onset and progression of peripapillary retinal nerve fiber layer (RNFL) retardance changes occur earlier than RNFL thickness changes in experimental glaucoma. Investig Ophthalmol Vis Sci. 2013;54(8):5653–61.
Pease ME, et al. Obstructed axonal transport of BDNF and its receptor TrkB in experimental glaucoma. Investig Ophthalmol Vis Sci. 2000;41(3):764–74.
Goyal N, Narayanaswami P. Making sense of antisense oligonucleotides: a narrative review. Muscle Nerve. 2018;57(3):356–70.
Disterer P, et al. Development of therapeutic splice-switching oligonucleotides. Hum Gene Ther. 2014;25(7):587–98.
Chan JH, Lim S, Wong WS. Antisense oligonucleotides: from design to therapeutic application. Clin Exp Pharmacol Physiol. 2006;33(5–6):533–40.
Hammond SM, Wood MJ. Genetic therapies for RNA mis-splicing diseases. Trends Genet. 2011;27(5):196–205.
Monia BP, et al. Evaluation of 2′-modified oligonucleotides containing 2′-deoxy gaps as antisense inhibitors of gene expression. J Biol Chem. 1993;268(19):14514–22.
Sardone V et al. Antisense oligonucleotide-based therapy for neuromuscular disease. Molecules. 2017;22(4).
Temsamani J, Pari GS, Guinot P. Antisense approach for the treatment of cytomegalovirus infection. Expert Opin Investig Drugs. 1997;6(9):1157–67.
Vazquez-Dominguez I, Garanto A, Collin RWJ. Molecular therapies for inherited retinal diseases-current standing, opportunities and challenges. Genes (Basel). 2019;10(9).
Garanto A et al. Antisense oligonucleotide screening to optimize the rescue of the splicing defect caused by the recurrent deep-intronic ABCA4 variant c.4539+2001G>A in Stargardt disease. Genes (Basel). 2019;10(6).
Naessens S et al. Antisense oligonucleotide-based downregulation of the G56R pathogenic variant causing NR2E3-associated autosomal dominant retinitis pigmentosa. Genes (Basel). 2019;10(5).
Niu C et al. Antisense oligonucleotides targeting mutant Ataxin-7 restore visual function in a mouse model of spinocerebellar ataxia type 7. Sci Transl Med. 2018;10(465).
Dulla K, et al. Splice-modulating Oligonucleotide QR-110 restores CEP290 mRNA and function in human c2991+1655A>G LCA10 models. Mol Ther Nucleic Acids. 2018;12:730–40.
Slijkerman RW, et al. Antisense oligonucleotide-based splice correction for USH2A-associated retinal degeneration caused by a frequent deep-intronic mutation. Mol Ther Nucleic Acids. 2016;5(10):e381.
Xiong W, et al. AAV cis-regulatory sequences are correlated with ocular toxicity. Proc Natl Acad Sci USA. 2019;116(12):5785–94.
Nidetz NF, et al. Adeno-associated viral vector-mediated immune responses: understanding barriers to gene delivery. Pharmacol Ther. 2020;207:107453.
Retnet: Genes and mapped loci causing retinal diseases. https://sph.uth.edu/retnet/disease.htm. Accessed 21 Oct 2020.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was funded by the Lions Eye Institute (LEI), Usher 1F Collaborative and Genetics Cures Australia.
Conflict of interest
The authors declare that this review was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Authors contributions
LSC wrote the first draft of the manuscript; ARH, PFC and HB wrote sections of the manuscript and drafted the tables and all authors contributed to manuscript revision and approval of the submitted version.
Ethics approval
N/A.
Consent to participate
N/A.
Consent for publication
N/A.
Availability of data and material
N/A.
Code availability
N/A.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Fuller-Carter, P.I., Basiri, H., Harvey, A.R. et al. Focused Update on AAV-Based Gene Therapy Clinical Trials for Inherited Retinal Degeneration. BioDrugs 34, 763–781 (2020). https://doi.org/10.1007/s40259-020-00453-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40259-020-00453-8