Abstract
Introduction
The escalating burden of catastrophic health expenditure (CHE) poses a significant threat to individuals and households in India, where out-of-pocket expenditure (OOP) constitutes a substantial portion of healthcare financing. With rising OOP in India, a proper measurement to track and monitor CHE due to health expenditure is of utmost important. This study focuses on synthesizing findings, understanding measurement variations, and estimating the pooled incidence of CHE by health services, reported diseases, and survey types.
Method
Following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, a thorough search strategy was employed across multiple databases, between 2010 and 2023. Inclusion criteria encompassed observational or interventional studies reporting CHE incidence, while exclusion criteria screened out studies with unclear definitions, pharmacy revenue-based spending, or non-representative health facility surveys. A meta-analysis, utilizing a random-effects model, assessed the pooled CHE incidence. Sensitivity analysis and subgroup analyses were conducted to explore heterogeneity.
Results
Out of 501 initially relevant articles, 36 studies met inclusion criteria. The review identified significant variations in CHE measurements, with incidence ranging from 5.1% to 69.9%. Meta-analysis indicated the estimated incidence of CHE at a 10% threshold is 0.30 [0.25–0.35], indicating a significant prevalence of financial hardship due to health expenses. The pooled incidence is estimated by considering different sub-groups. No statistical differences were found between inpatient and outpatient CHE. However, disease-specific estimates were significantly higher (52%) compared to combined diseases (21%). Notably, surveys focusing on health reported higher CHE (33%) than consumption surveys (14%).
Discussion
The study highlights the intricate challenges in measuring CHE, emphasizing variations in recall periods, components considered in out-of-pocket expenditure, and diverse methods for defining capacity to pay. Notably, the findings underscore the need for standardized definitions and measurements across studies. The lack of uniformity in reporting exacerbates the challenge of comparing and comprehensively understanding the financial burden on households.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The meta-analysis revealed an overall incidence of catastrophic health expenditure (CHE) of 30% at a 10% threshold in India, indicating a significant portion of the population faces financial hardship due to healthcare costs. |
The study found no statistical difference in the incidence of CHE between inpatient and outpatient healthcare services, suggesting that both types of healthcare needs contribute similarly to financial strain on households. |
Disease-specific CHE estimates were significantly higher, at 52%, compared to 21% for combined diseases, pointing to the increased financial burden associated with specific health conditions. |
Surveys focused on health reported a higher incidence of CHE (33%) compared to consumption surveys (14%), indicating that the methodology and focus of surveys influence the reported prevalence of financial hardship. |
The review underscores the challenges in measuring CHE due to variations in recall periods, out-of-pocket expenditure components, and definitions of capacity to pay, highlighting the necessity for standardized definitions and measurements across studies to accurately assess and compare the financial impact of healthcare on households. |
1 Introduction
The fundamental goal of any healthcare system is to provide quality care to the citizens and to ensure that they are protected from disproportionate health expenditure [1]. However, several hurdles remain in the way of achieving this objective. Out-of-pocket expenditure is one of the mounting challenges, and serves as the primary source of healthcare financing in low- and middle-income countries [2]. Health expenditures that require households to reduce spending on basic necessities are termed “catastrophic expenditures” [3]. The effect of such health expenditure on households in developing countries can be devastating. Subsequently, there is a growing interest in the incidence of catastrophic expenditure and their effect on individuals, households and communities in India. However, it is difficult to compare the findings of these studies because of the wide variation in the measurement of health expenditures, methodologies and thresholds employed to measure catastrophic expenditure.
While the proportion of healthcare expenses covered directly by patients at the point of care, known as out-of-pocket payments, has been decreasing on a global scale, the out-of-pocket expenditure as a percentage of income has not shown a corresponding decline [4]. In 2019, over 930 million people experienced financial hardship across the world while obtaining healthcare. Due to the inadequate quality of care, frequent absenteeism among staff, and equipment shortages in public health facilities in India [5], out-of-pocket expenditure has risen significantly, comprising around 64% of total healthcare financing. Consequently, private practitioners have emerged as the primary healthcare providers for the poor, particularly in rural regions [5]. As countries across the globe ambitiously stride towards universal health coverage (UHC), a thorough understanding of health burden is necessary for an effective and efficient monitoring and policy interventions. Numerous studies have made attempts to study the burden of disease in terms of CHE in India. Evidence indicates that such estimation is sensitive to the methods and definitions of OOPE and CHE, which, as a result, may vary significantly across the studies [6]. Previous systematic reviews have been limited to studying the economic cost of NCDs for India [7] and of the economic impact of diseases on low- and middle-income countries [8]. Therefore, a systematic review that solely focuses on understating financial burden among households in India is much needed. Specifically, this paper endeavours to understand how the incidence of catastrophic health expenditure is measured across the studies. The review also strives to estimate the pooled incidence of catastrophic health expenditure by type of health services, reported disease and type of surveys employed.
2 Method
2.1 Search Strategy
The team consisting of three members (independent researchers) including the author prepared the search strategy following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. Searches were conducted in PubMed, Google Scholar, Science Direct, SCOPUS, Web of Sciences, JSTOR and EconPapers. The key terms used for search strategy included (although not restricted to) a combination of the following terms “Health cost”, “Health expenditure”, “Financial Burden of Health” “Health spending” “Catastrophic expenditure”, “Impoverishment”. Detailed search terms are given in the Appendix. The literature search was conducted during April–May 2023 and involved reviewing of the abstracts by all the members of the team. Studies that were approved by two researchers were considered for full paper reviews, based on the following inclusion and exclusion criteria. All the members extracted the data independently and read the final list of papers included for review.
2.2 Inclusion Criteria
-
1.
Observational or interventional studies published on India during the period of 2010-2023.
-
2.
Studies reported or published in literature in peer reviewed journals.
-
3.
Publication that reported incidence of catastrophic health expenditure for all individuals and for all ages through a household survey or through a national, regional or state representative health facility survey.
2.3 Exclusion Criteria
-
1.
Publications that have reported health spending based on pharmacy revenue.
-
2.
Disease estimated or loss of economic cost at an aggregate or national level.
-
3.
Publications that reported health spending or economic losses at one or several health facilities that were not representative of the entire community.
-
4.
Unclear reported definitions or samples to measure health expenditure or CHE.
-
5.
Case reports, national reports or state reports. Systematic review papers, commentaries or letters to editor.
All the empirical papers on catastrophic health expenditure in India that were published in peer-reviewed journals are included. Systematic reviews or studies that employed a meta-analysis or were dissertations and working papers are not included. The studies were tabulated in Excel sheets and included the names of the authors, publication year, title, source of data, definitions, sample size, incidence reported, and summary of the findings. In case of studies that did not report proper incidence or sample sizes, the corresponding authors were requested to provide the required tables. The PRISMA diagram for selection of studies is shown in Fig. 1.
2.4 Meta-Analysis
In meta-analysis, before estimating pooled incidence or prevalence we need to decide between two modelling approaches for calculating the summary effect size: the fixed-effects and random-effects models [9]. The fixed-effects model is used when studies share the same population, procedures and conditions, which is often not the case in practice. Effect sizes can vary between studies due to methodological differences, leading to a normal distribution of true effect sizes. The random-effects model accounts for this variability, allowing for differing true effect sizes between studies, while the fixed-effects model assumes no between-study variability by setting the between-study variance to zero [10]. In the present study, a random effects meta-analysis using logit transformation is performed to calculate the combined CHE from various studies. Study heterogeneity was assessed using the I2 statistic. The I2 statistic, which ranges from 0 to 100%, serves as an indicator of the degree of heterogeneity within a dataset. A higher I2 value corresponds to greater heterogeneity. When the I2 is below 40%, it may imply that the level of heterogeneity is not substantial, whereas an I2 exceeding 75% could signal significant heterogeneity [11]. Sensitivity analysis is carried using a method known as leave-one-out analysis. In this analysis, the pooled incidence of CHE is estimated by excluding each study at a time. All analyses were carried out in R version 4.3.0. and used various packages such as metafor and meta.
3 Results
Initial search in all the platforms resulted in a total of 5839 articles of which 1857 articles were found to be duplicated, leaving 3985 articles for further consideration. Of these articles, 3484 articles were not relevant to the research question, leaving about 501 articles for further title screening and abstract screening. Out of the 501 articles, 440 were not relevant to the research question and not related to Indian literature, leaving 67 articles for full review. From these 67 articles, 31 studies were excluded if full-text was not available or it did not address the research question, leaving 36 articles that met the inclusion criteria.
3.1 Characteristics of the Studies Included
A comprehensive review of multiple studies was conducted to provide insights into the extent of financial burden imposed on Indian households due to healthcare costs. The included studies report 77 distinct points, out of which 57 data points reported CHE at the 10% level of threshold while 19 data points employed the 40% definition. Table1A–1C outlines key details of the included studies at 10% CHE stratified by study type, survey years, disease group, and health service settings.
The findings from various studies reveal a noteworthy range of catastrophic health expenditure estimates in India. The studies depict a large variation, ranging from 5.1% to 69.9% depending on the survey design, disease specific and type of health services. Higher reporting of CHE was found to be for disease-specific studies as compared to studies that have reported for an overall disease in households. The majority of the studies included inpatient and outpatient expenditures to calculate CHE. The estimates for different types of health services of CHE varied from 6% to 58% for inpatients, and for outpatients it ranged from 7% to 69.9%. Such wide variation has been observed among disease type and survey type.
3.2 Measuring Out-of-Pocket (OOP) Expenditure
A consistent measurement of out-of-pocket expenditure (OOP) is crucial for assessing the healthcare burden in various studies. The systematic review uncovered variations in how studies defined OOP expenditure, particularly in terms of two key aspects: the recall period and the components considered for inclusion in OOP expenditure.
3.2.1 Recall Period for Reporting OOP
The recall period used to report OOP expenditure for outpatient and inpatient care has shown diversity across the studies. For outpatient expenses, the reported expenditure has varied, with some studies using 15 days, others using 30 days (1 month), and others employing a 365-day (1-year) timeframe. In the case of inpatient care, a consistent recall period of the last year from the date of interview was observed in all the studies. To make the reporting of expenditures uniform, some studies have employed multipliers, especially when they aimed to report a combined figure for both outpatient and inpatient OOP. For instance, studies by Pandey et al. [12], Yadav et al. [13]. Sangar et al. [14], Nanda and Sharma [15] and Mohanty and Dwivedi [16] converted the recall period to a 1-month period for both inpatient and outpatient expenditures before aggregating the figures. In contrast, other studies have annualized the costs to facilitate comparisons [17,18,19,20,21]. In the Longitudinal Aging Study in India (LASI) data, all inpatient and outpatient expenditures were standardized for the 30 days prior to the survey period [22]. Some studies did not explicitly address the adjustment of the recall period for expenditures [23,24,25,26]. However, it becomes evident from the tables in Karan et al. [24] that inpatient yearly expenses were converted into monthly expenditures, and a similar adjustment was made for outpatients. In primary surveys, such as Maurya et al. [31], OOP expenditure was considered directly for a 1-year period. In a tuberculosis (TB) study conducted in Bangalore, medical expenses were collected in the first 2 months and last 2 months of the survey [27].
Extant literature highlights that different studies have adopted varying methods to adjust the reporting period. However, concerns arise when studies multiply or divide reported expenditures to extend or shorten the period, as this assumes that the expenditure will be recurring regularly within households, which may not always be the case. For instance, studies like Lee et al. [17] aggregated outpatient costs into an annual cost, necessitating the assumption that outpatient expenses incurred in a given month will persist throughout the year. Such assumptions may lead to an overestimation of expenditure rather than capturing the actual expenses incurred by most households.
3.2.2 Components to Define OOP
The definition of OOP expenses in the context of healthcare can be divided into two main components: medical expenses and non-medical expenses. However, there is no universally accepted standard for categorizing specific subcomponents within these expense categories. For instance, some studies classify transportation, food and accommodation as non-medical expenses, while others exclude transportation from this category [28]. Additionally, some studies consider food expenses incurred during waiting periods as non-medical [29]. A clear and consistent definition of OOP expenses is crucial for understanding which components were considered by different studies in defining OOP and, consequently, assessing the financial burden and for comparisons.
Several studies have explicitly defined both medical and non-medical expenses within the OOP framework [13, 18, 25, 26, 30,31,32]. However, some studies have not provided a comprehensive definition of OOP or the specific components involved [33, 34]. It's important to note that surveys collecting information on maternal and child-care expenses should address these expenses when calculating OOP. For instance, some studies have considered maternal care expenditure as part of inpatient healthcare costs [16], while others have excluded child-care or maternal-related expenditures [28, 30].
When defining OOP expenses, studies have to account for reimbursement adjustments. Some studies have defined OOP after adjusting for reimbursement of healthcare payments [12,13,14,15, 17, 23, 25, 30, 32, 35], while others have not discussed reimbursement adjustments [18, 26, 34].
When examining primary surveys related to TB patients, both direct and indirect costs are typically aggregated as OOP expenses [27, 29, 31]. However, there are nuances in what costs are included in these calculations. For instance, in the study by Madan et al., certain costs, such as expenses involving food supplements based on medical advice and the cost of accommodation were not counted towards OOP cost [27]. On the other hand Muniyandi et al. broadened the scope and also considered indirect costs of TB as loss of wages due to work absenteeism and the inability to work due to the disease when calculating OOP [29]. Additionally, studies have included caretaker accommodation charges as a component of non-medical expenses [31].
When defining OOP, there are different questions included in the surveys depending upon the survey type, respondent, and number of items included in the survey list [6, 36]. Therefore, studies have to clearly define what components are collected for the survey and what exactly is included in the definition of OOP expenses.
3.3 Variations in Catastrophic Health Expenditure (CHE) Methods (Payment Ability)
Catastrophic measurement involves using health-spending ratios, calculated against specific denominators, as thresholds to determine the extent of catastrophic spending. Most studies employ one of the two main methods to define the denominator for CHE: the capacity to pay (CTP) or the total household expenditure. The common threshold for CTP is 40%, while the total household budget share is set at 10%. However, the way of estimating CTP can vary between studies.
Some studies have approximated the CTP by determining a subsistence expenditure, which, too, differs across studies. When subsistence costs are less than or equal to food expenses, CTP is calculated as the difference between total expenditure and these subsistence costs. However, if subsistence expenses are more than food expenses, CTP is then defined by the difference between total expenditure and the actual food expenses. The criteria for defining what constitutes subsistence expenses also differ. Some studies calculate it based on the poverty line, which can vary significantly. Some studies have defined it as the average food consumption at the 45th and 55th percentiles of total consumption expenditure [22, 33,34,35]. Alternatively, others have defined subsistence expenditure as the median food expenditure [16], with further segmentation for rural and urban areas [37].
When the surveys do not explicitly allow for the calculation of subsistence or food expenditure, studies have used various poverty estimates from different committees to estimate subsistence expenditure. For instance, the study by Pandey and Meltzer [38] used poverty lines from the Rangarajan Expert Group, while Nanda and Sharma [15] employed poverty lines from the Tendulkar committee, multiplied by household sizes, to define subsistence expenditure.
Even when CHE is defined as the share of health spending relative to total household expenditure, studies have not used a consistent cut-off point. Some studies have defined CHE as health expenses equal to or exceeding 10% of total expenditure without discussing other expenses in detail like food, lodging and transportation [12, 14, 30, 34]. Others have defined health expenditure as including expenses like food, lodging and transportation exceeding 10% as CHE [13, 14, 17, 21, 23,24,25,26, 28, 32, 39, 40].
Some studies have adopted alternative methods to measure CHE that deviate from the existing methods. For example, Yadav et al. [13] defined CHE based on consumption by a single person or an average for household with two members. Engelgau et al. [20] defined CHE as a ratio exceeding 30% of health spending and the difference between total household spending and poverty line spending, multiplied by household size. Gupta and Joe [41] employed a multidimensional approach, using five different criteria to define CHE.
3.4 Meta-Analysis
Meta-analysis for incidence of CHE estimates has been depicted in Fig. 2 as a forest plot. The incidence of CHE estimated at the 10% level of threshold is 0.30 [0.25-0.35]. I2 at the bottom of the graphs denotes the heterogeneity. In the analysis, I2 was found to be 100%, indicating heterogeneity across the studies. In cases where heterogeneity is identified, suggesting unaccounted variations among study estimates, one of the methods employed to elucidate this heterogeneity is conducting subgroup analysis. Studies were stratified into groups of health services, diseases groups, and surveys used to estimate CHE. The incidence of CHE based on each stratification are discussed in detail below.
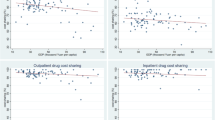
No significant differences were observed in the combined estimates of CHE incidence across different healthcare services. Figure 3 shows the pooled incidence by health services considered for both (inpatient and outpatients), inpatient only and outpatient only. The overall pooled incidence of CHE varied from 0.25 to 0.44, with an estimated total value of 0.35, while for inpatients it is 0.35 [0.22–0.47] and for outpatient 0.34 [0.18–0.50]. The nonexistence of a statistical difference by health services might be due to differences in the recall period and converting the recall period for uniformity. For example, in the review it was found that the majority of the studies adjusted the annual inpatient cost to a monthly cost while outpatient cost (reported to 15 days) was converted into a monthly cost. When converting an outpatient cost into monthly or yearly expenses, it is assumed that that there will be a recurrence of the same expenditure for every month or every 2 weeks. Such an occurrence in real-life situations is less likely.
Estimates of the pooled CHE for different disease groups are presented in Fig. 4, CHEs for specific disease group are higher than the estimates of CHEs for combined diseases. The pooled incidence for specific diseases was found to be 0.52 [0.46, 0.58], while for combined disease it was found to be 0.21 [0.17, 0.25]. Here a statistical difference was found between two subgroups at the 5% level of significance.
To account for CHE by type of survey, the studies have been categorised into three different types of surveys. Firstly, the surveys focused on health and its aspects—health surveys. Secondly, health expenditure was investigated as a part of household schedule called consumption surveys. Thirdly, there were primary surveys. A statistical difference was found between pooled estimates of these three surveys types. The pooled estimates surveyed by a consumption survey are found to be less, 0.14 [0.12, 0.16] as compared to health surveys, 0.33 [0.27, 0.39] and primary surveys, 0.30 [00, 0.86]. As pointed out by Raban et al., estimates of CHE differ by the type of survey, estimates of CHE from a health survey are more likely to report a higher incidence of CHE as compared to consumption surveys. Such differences might be due to the number of detailed questions covered by the health surveys [6].
Sensitivity analysis (see Online Supplementary Material (OSM) Fig. 1S), in which the meta-analysis was iteratively performed with the exclusion of each study, revealed that no single study had an impact greater than 1% on the overall estimate of the incidence of CHE (Fig. 5).
4 Discussion
Catastrophic health expenditure is a critical metric for assessing the financial safeguards offered by healthcare systems worldwide, and it has been quantified using diverse survey tools [6]. This metric, which signifies expenses surpassing a specific portion of a household's total consumption or income, has gained substantial prominence, culminating in its inclusion as indicator 3.8.2 in the UN Sustainable Development Goals. The present study reviewed the measurement of CHE and quantified the CHE through a meta-analysis for India. It was found that about one-third of households affected by disease have incurred catastrophic expenditure (at 10% of total household expenditure). Analysis by Xu et al. [42] estimates a range of 0–10% of CHE across the countries, while Heijink et al. [36] using a the World Health Survey has estimated a range between 0.6 and 30%. Pooled analysis from African countries indicated that one in six households have faced financial difficulty seeking health care [43].
As in the sub-Saharan context [43], it was found that the incidence of CHE is high among studies that have reported CHE for a particular or group of disease. Nevertheless, comparatively fewer studies offered separate disease estimates for CHE, so further population-wide studies sensitive to this distinction are warranted.
Studies in India have shown that CHE is more prevalent among inpatients than outpatients, as highlighted by Yadav et al. [32]. In contrast, this meta-analysis did not reveal significant disparities in CHE rates among outpatients, inpatients, and cases where both settings were considered in CHE calculations. A noteworthy issue arises from the various multipliers used when reporting total, outpatient and inpatient expenditures in these studies. These multipliers can lead to discrepancies, potentially resulting in under-reporting or over-reporting of health expenses, as reported by Raban et al. [6]. For instance, in the context of outpatient expenses, a shorter recall period was consistently employed in all Indian surveys. It is important to note that shorter recall periods are associated with less recall error, as suggested by Clarke et al. [44]. However, the combination of shorter recall periods and the use of multipliers for outpatient expense adjustment may result in an overestimation of health expenses across the studies. As noted by Engelau et al. [20], it is improbable that households reporting health spending in the last 2 weeks will follow the same expenditure pattern in the next 2 weeks, or maintain a consistent pattern throughout the year.
As pointed out by Lu et al. [45] and Xu et al. [42], estimates of household spending on healthcare are sensitive to survey instruments. The present study also revealed a variation of such sensitivity through pooled CHE estimates by type of survey. In India, for health estimates two types of surveys were used, one is consumption and expenditure surveys, which do not have a detailed question on health expenditure, and others are health surveys. While the health surveys have an intense focus on health, they might result in higher estimates of health expenditure and lower estimates of other expenditure [6, 42], consequently we might observe higher CHE estimates from health surveys as compared to consumption surveys. The findings of the study are supported by a validation survey carried out by Raban et al. [6] on various Indian surveys, which discovered that comprehensive health surveys tend to report higher health expenditures.
The meta-analysis results, which highlight a significant incidence of CHE at 0.30 [0.25–0.35], raise important concerns about the financial burden of healthcare on households, particularly in the context of OOP spending and the lack of health coverage in India. Despite efforts to improve health insurance coverage, a large segment of the Indian population still pays for health services directly from their own pockets. This situation forces many into financial hardship when faced with serious health issues, as indicated by the high incidence of CHE. The meta-analysis results illustrate the urgent need for expanded and more effective health coverage in India [46]. The high levels of OOP spending and the significant incidence of CHE indicate that many are left without adequate financial protection against unexpected health crises. Enhancing health insurance coverage, in terms of both reach and depth, could mitigate the impact of OOP spending and reduce the incidence of CHE.
This study provides important evidence for discussions on policy and health financing reforms by demonstrating that a substantial portion of people experience financial burden, even though the Government of India has implemented a social insurance scheme through the Ayushman Bharat programme and Rashtriya Swasthya Bima Yojana (RSBY). Policies aimed at increasing coverage should particularly focus on the most vulnerable populations and those facing high-cost diseases. As highlighted by Yadav et al. [32], the national insurance scheme only covers inpatients. The pooled estimates suggest no difference in financial burden for inpatient and outpatient care, components towards outpatient departments (OPDs) must be added to national insurance schemes. The study findings also highlight the need for uniformity in OOP measurements across the studies such as deduction of insurances, cost of accommodation, and other charges; a standard adaption of health spending measurements will standardise definitions of CHE.
This study is not without some limitations. The pooled CHE estimate is mostly based on surveys which often do not capture people who are unable to access healthcare due to financial constraints and may be reporting lesser expenses or zero. With such limitations across the survey based CHE estimates, the pooled estimates performed in this may not represent a true CHE estimate. In the absence of many studies on CHE at a 40% threshold, pooled estimates from this threshold were not reported. Estimates from CHE at 40% and compared with the 10% threshold definition could have been greater exercise in understanding variation in CHE due to measurements of CHE. Third, India has limited national surveys and all the studies reported here are mostly based on these four to five national surveys across the time period. Thus, there may be a bias in the estimates as studies mostly used the same surveys in CHE estimations.
References
Bredenkamp C, Mendola M, Gragnolati M. Catastrophic and impoverishing effects of health expenditure: new evidence from the Western Balkans. Health Policy Plan. 2011;26:349–56. https://doi.org/10.1093/heapol/czq070.
Joe W. Distressed financing of household out-of-pocket health care payments in India: incidence and correlates. Health Policy Plan. 2015;30:728–41. https://doi.org/10.1093/heapol/czu050.
Xu K, Evans DB, Kawabata K, Zeramdini R, Klavus J, Murray CJL. Household catastrophic health expenditure: a multicountry analysis. Lancet. 2003;362:111–7. https://doi.org/10.1016/S0140-6736(03)13861-5.
Wagstaff A, Flores G, Hsu J, Smitz MF, Chepynoga K, Buisman LR, et al. Progress on catastrophic health spending in 133 countries: a retrospective observational study. Lancet Glob Heal. 2018;6:e169–79. https://doi.org/10.1016/S2214-109X(17)30429-1.
Nandi A, Ashok A, Laxminarayan R. The socioeconomic and institutional determinants of participation in India’s health insurance scheme for the poor. PLoS ONE. 2013. https://doi.org/10.1371/journal.pone.0066296.
Raban MZ, Dandona R, Dandona L. Variations in catastrophic health expenditure estimates from household surveys in India. Bull World Health Organ. 2013;91:726–35. https://doi.org/10.2471/BLT.12.113100.
Shukla V, Arora R. The economic cost of rising non-communicable diseases in India: a systematic literature review of methods and estimates. Appl Health Econ Health Policy. 2023. https://doi.org/10.1007/s40258-023-00822-8.
Alam K, Mahal A. Economic impacts of health shocks on households in low and middle income countries: a review of the literature. Global Health. 2014. https://doi.org/10.1186/1744-8603-10-21.
Harrer M, Cuijpers P, Furukawa TA, Ebert DD. Doing meta-analysis with R. 2021.https://doi.org/10.1201/9781003107347
Wang N. How to conduct a meta-analysis of proportions in R: a comprehensive tutorial. John Jay Coll Crim Justice. 2016. p. 1–63.
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58. https://doi.org/10.1002/sim.1186.
Pandey A, Ploubidis GB, Clarke L, Dandona L. Trends in catastrophic health expenditure in India: 1993 to 2014. Bull World Health Organ. 2018;96:18–28. https://doi.org/10.2471/BLT.17.191759.
Yadav J, Menon GR, John D. Disease-specific out-of-pocket payments, catastrophic health expenditure and impoverishment effects in India: an analysis of national health survey data. Appl Health Econ Health Policy. 2021;19:769–82. https://doi.org/10.1007/s40258-021-00641-9.
Sangar S, Dutt V, Thakur R. Economic burden, impoverishment, and coping mechanisms associated with out-of-pocket health expenditure in India: a disaggregated analysis at the state level. Int J Health Plann Manage. 2019;34:e301–13. https://doi.org/10.1002/hpm.2649.
Nanda M, Sharma R. A comprehensive examination of the economic impact of out-of-pocket health expenditures in India. Health Policy Plan. 2023;38:926–38. https://doi.org/10.1093/heapol/czad050.
Mohanty SK, Dwivedi LK. Addressing data and methodological limitations in estimating catastrophic health spending and impoverishment in India, 2004–18. Int J Equity Health. 2021;20:1–18. https://doi.org/10.1186/s12939-021-01421-6.
Lee THJ, Saran I, Rao KD. Ageing in India: financial hardship from health expenditures. Int J Health Plan Manag. 2018;33:414–25. https://doi.org/10.1002/hpm.2478.
Tripathy JP, Jagnoor J, Prasad BM, Ivers R. Cost of injury care in India: cross-sectional analysis of National Sample Survey 2014. Inj Prev. 2018;24:116–22. https://doi.org/10.1136/injuryprev-2017-042318.
Mahal A, Karan A, Engelgau M. The economic implications of non-communicable disease for India. 2010.
Engelgau MM, Karan A, Mahal A. The economic impact of non-communicable diseases on households in India. Glob Health. 2012;8:9–12. https://doi.org/10.1186/1744-8603-8-9.
Yadav J, John D, Allarakha S, Menon GR. Rising healthcare expenditure on tuberculosis: can India achieve the End TB goal? Trop Med Int Health. 2021;26:1256–75. https://doi.org/10.1111/tmi.13648.
Mohanty SK, Sahoo U, Rashmi R. Old-age dependency and catastrophic health expenditure: evidence from Longitudinal Ageing Study in India. Int J Health Plan Manag. 2022;37:3148–71. https://doi.org/10.1002/hpm.3546.
Rajasulochana SR, Kar SS. Economic burden associated with stroke in India: insights from national sample survey 2017–18. Expert Rev Pharmacoecon Outcomes Res. 2021;00:1–9. https://doi.org/10.1080/14737167.2021.1941883.
Karan A, Farooqui HH, Hussain S, Hussain MA, Selvaraj S, Mathur MR. Multimorbidity, healthcare use and catastrophic health expenditure by households in India: a cross-section analysis of self-reported morbidity from national sample survey data 2017–18. BMC Health Serv Res. 2022;22:1–12. https://doi.org/10.1186/s12913-022-08509-x.
Verma VR, Kumar P, Dash U. Assessing the household economic burden of non-communicable diseases in India: evidence from repeated cross-sectional surveys. BMC Public Health. 2021;21:1–22. https://doi.org/10.1186/s12889-021-10828-3.
Sriram S, Albadrani M. A study of catastrophic health expenditures in India—evidence from nationally representative survey data: 2014–2018. F1000Research 2022;11:2014–8. https://doi.org/10.12688/f1000research.75808.1.
Madan J, Lönnroth K, Laokri S, Squire SB. What can dissaving tell us about catastrophic costs? Linear and logistic regression analysis of the relationship between patient costs and financial coping strategies adopted by tuberculosis patients in Bangladesh, Tanzania and Bangalore, India. BMC Health Serv Res. 2015;15:1–8. https://doi.org/10.1186/s12913-015-1138-z.
Behera S, Pradhan J. Uneven economic burden of noncommunicable diseases among Indian households: a comparative analysis. PLoS ONE. 2021;16:1–17. https://doi.org/10.1371/journal.pone.0260628.
Muniyandi M, Thomas BE, Karikalan N, Kannan T, Rajendran K, Saravanan B, et al. Association of tuberculosis with household catastrophic expenditure in South India. JAMA Netw Open. 2020;3:1–11. https://doi.org/10.1001/jamanetworkopen.2019.20973.
Kastor A, Mohanty SK. Disease-specific out-of-pocket and catastrophic health expenditure on hospitalization in India: do Indian households face distress health financing? PLoS ONE. 2018;13:1–18. https://doi.org/10.1371/journal.pone.0196106.
Maurya PK, Murali S, Jayaseelan V, Thulasingam M, Pandjatcharam J. Economic burden of cancer treatment in a region in South India: a cross sectional analytical study. Asian Pacific J Cancer Prev. 2021;22:3755–62. https://doi.org/10.31557/APJCP.2021.22.12.3755.
Yadav J, Menon G, Agarwal A, John D. Burden of injuries and its associated hospitalization expenditure in India. Int J Inj Contr Saf Promot. 2021;28:153–61. https://doi.org/10.1080/17457300.2021.1879163.
Mohanty SK, Agrawal NK, Mahapatra B, Choudhury D, Tuladhar S, Holmgren EV. Multidimensional poverty and catastrophic health spending in the mountainous regions of Myanmar, Nepal and India. Int J Equity Health. 2017;16:1–13. https://doi.org/10.1186/s12939-016-0514-6.
Dwivedi R, Pradhan J, Athe R. Measuring catastrophe in paying for healthcare: a comparative methodological approach by using National Sample Survey. India Int J Health Plan Manag. 2021;36:1887–915. https://doi.org/10.1002/hpm.3272.
Kumar K, Singh A, Kumar S, Ram F, Singh A, Ram U, et al. Socio-economic differentials in impoverishment effects of out-of-pocket health expenditure in China and India: evidence from WHO SAGE. PLoS ONE. 2015;10:1–19. https://doi.org/10.1371/journal.pone.0135051.
Heijink R, Xu K, Saksana P, Evans D. Validity and Comparability of out-of- pocket health expenditure from household surveys: a review of the literature and current survey instruments. WHO Discuss Pap 2011. p. 1–30.
Mohanty SK, Kim R, Khan PK, Subramanian SV. Geographic variation in household and catastrophic health spending in India: assessing the relative importance of villages, districts, and states, 2011–2012. Milbank Q. 2018;96:167–206. https://doi.org/10.1111/1468-0009.12315.
Pandey KR, Meltzer DO. Financial burden and impoverishment due to cardiovascular medications in low and middle income countries: an illustration from India. PLoS ONE. 2016;11:1–19. https://doi.org/10.1371/journal.pone.0155293.
Yadav J, Allarakha S, Menon GR, John D, Nair S. Socioeconomic impact of hospitalization expenditure for treatment of noncommunicable diseases in India: a repeated cross-sectional analysis of national sample survey data, 2004 to 2018. Value Heal Reg Issues. 2021;24:199–213. https://doi.org/10.1016/j.vhri.2020.12.010.
Karan A, Selvaraj S, Mahal A. Moving to universal coverage? Trends in the burden of out-of-pocket payments for health care across social groups in India, 1999–2000 to 2011–12. PLoS ONE. 2014;9:1999–2000. https://doi.org/10.1371/journal.pone.0105162.
Gupta I, Joe W. Refining estimates of catastrophic healthcare expenditure: an application in the Indian context. Int J Health Care Finance Econ. 2013;13:157–72. https://doi.org/10.1007/s10754-013-9125-6.
Xu K, Ravndal F, Evans DB, Carrin G. Assessing the reliability of household expenditure data: results of the World Health Survey. Health Policy (New York). 2009;91:297–305. https://doi.org/10.1016/j.healthpol.2009.01.002.
Eze P, Lawani LO, Agu UJ, Acharya Y. Catastrophic health expenditure in sub-Saharan Africa: systematic review and meta-analysis. Bull World Health Organ. 2022;100:337-351J. https://doi.org/10.2471/BLT.21.287673.
Clarke PM, Fiebig DG, Gerdtham UG. Optimal recall length in survey design. J Health Econ. 2008;27:1275–84. https://doi.org/10.1016/j.jhealeco.2008.05.012.
Lu C, Chin B, Li G, Murray CJL. Limitations of methods for measuring out-of-pocket and catastrophic private health expenditures. Bull World Health Organ. 2009;87:238–44. https://doi.org/10.2471/BLT.08.054379.
Kalita A, Carton-Rossen N, Joseph L, Chhetri D, Patel V. The barriers to universal health coverage in India and the strategies to address them: a key informant study. Ann Glob Heal. 2023;89:69. https://doi.org/10.5334/aogh.4120.
Acknowledgements
The team mentioned in the Methods section consists of three independent reviewers, Umenthla Srikanth Reddy, Adrita Banerjee, and Tapasya Raj, who extracted papers and data from the selected papers. The authors acknowledge the contribution of Adrita Banerjee, Tapasya Raj and Shreya Singh in editing the manuscript and providing valuable feedback. The author also acknowledges the journal editor for meticulously reviewing the manuscript, as well as the anonymous reviewers for their valuable suggestions and feedback.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding has been received for the study; the paper is a part of PhD thesis.
Conflict of interest
The author declares no competing interests.
Ethics statement
Ethical approval for this type of study is not required by our institute.
Consent for publication
Not applicable.
Consent to participate
Not applicable.
Reflexivity statement
The author is a PhD student, this work is a part of his thesis. The author has an understanding and experience of health financing in India.
Availability of data and materials
Available upon request.
Code availability
Available upon request.
Author contributions
USR has conceptualised and designed the work. USR has collected the data and did analysis. Interpretation of the results were done by USR under the guidance of Prof. K.S. James (PhD supervisor). All the results were discussed with USR’s supervisor. The paper was drafted by USR. The critical revision was done by USR.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Reddy, U.S. Measurement of Catastrophic Health Expenditure in India: A Systematic Review and Meta-Analysis. Appl Health Econ Health Policy 22, 471–483 (2024). https://doi.org/10.1007/s40258-024-00885-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-024-00885-1