Abstract
Actinic keratoses (AKs) are atypical, precancerous proliferations of keratinocytes that develop because of chronic exposure to ultraviolet (UV) radiation. Treatment of AK can be lesion-directed or field-directed. Field cancerization theory postulates that the skin surrounding AK is also at increased risk for possible malignant transformation since it has been exposed to the same chronic UV light. Field-directed therapies thus have the potential to address subclinical damage, reduce AK recurrence rates, and potentially reduce the risk of squamous cell carcinoma (SCC) development. Published clinical studies have found lesion clearance rates ranging from 81 to 91% for photodynamic therapy (PDT) with either aminolevulinic acid (ALA) or methylaminolevulinate (MAL). Clinical studies have also been published on various topical treatments. Complete clinical clearance (CCC) was significantly higher in patients treated with a combination of 5-fluorouracil and salicylic acid (5-FU–SA) than in the vehicle group across multiple studies, and CCC ranged between 46 and 48% following treatment with imiquimod. Additionally, treatment with diclofenac sodium (DFS) found reduction in lesion sizes to range from 67 to 75%. Reported results have been similar for another non-steroidal anti-inflammatory drug (NSAID), piroxicam, which has more cyclooxygenase (COX)-1 activity than DFS. Active treatments with ingenol mebutate were also significantly more effective than vehicle at clearing AK lesions. All treatments resulted in mild, localized skin reactions. PDT using conventional light sources was associated with increased severity of pain and/or discomfort, while PDT using daylight as the light source was associated with less pain and occasionally no pain at all. Though no widely accepted algorithm for the treatment of AKs exists, field-directed therapy can be particularly useful for treating photo-exposed areas containing multiple AKs. Additional research with more direct comparisons between these field-directed therapies will help clinicians determine the best therapeutic approach. Here, we provide a balanced and comprehensive narrative review of the literature, considering both light-based and topical therapies with a focus on their field-therapy aspects, and propose a therapeutic algorithm for selecting an appropriate treatment in the clinical setting.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The important role of field-directed therapies in the treatment of actinic keratoses (AKs) is becoming ever clearer given the need to address subclinical damage, reduce AK recurrence rates, and potentially reduce the risk of squamous cell carcinoma (SCC) development. |
Currently, no widely accepted algorithm exists for the treatment of AK in the USA, though the evidence leans towards field-directed treatment of photo-exposed areas containing multiple AKs. |
Deciding between the various light-based and topical therapies requires an understanding of the outcomes, adverse effects, and costs of each therapy and how those relate to the patient preferences. |
1 Introduction
The emerging science of field cancerization is changing the paradigm for treating cutaneous malignancies by targeting entire skin regions. The concept was first proposed by Slaughter et al. in 1953 to describe histologically abnormal tissue surrounding primary oral squamous cell carcinoma (SCC) and to explain the development of multiple primary tumors and locally recurrent cancers within the field. Since that time, modern molecular techniques have established a genetic basis for this model in various types of cancers, including cutaneous malignancies. The field begins from a singular cell, which accumulates genetic mutations after carcinogen exposure and subsequently divides to create a field of monoclonal premalignant cells. Eventually, transformative events may occur, resulting in cells with invasive and metastatic properties, thus forming a carcinoma. In terms of cutaneous malignancies, ultraviolet (UV) radiation (UVA/UVB) is the most common source of carcinogenesis. The concept of field cancerization suggests that, because the skin surrounding cutaneous malignancies has been exposed to the same chronic UV light as the initial lesion, it is at increased risk for genetic abnormalities and thus possible malignant transformation.
Actinic keratoses (AKs) are intraepithelial atypical proliferations of keratinocytes that are generally regarded as precancerous and typically develop because of chronic exposure to UV radiation. The prevalence of AKs was estimated to be 40 million in the USA in 2004 [1]. In Australia, 11–40% of white people were estimated to have AKs in 1989 [2]. The visible clinical lesions are the initial manifestation of a multi-step carcinogenesis process or disease continuum that can progress from initial subclinical keratinocyte dysplasia into invasive SCC. Field cancerization develops because UV light causes neoplastic changes across the entire sun-exposed field of skin. Thus, areas of subclinical, or non-visible, sun damage in the periphery of visible AKs contain the same genetic changes as those found in the lesions themselves and are known as areas of field cancerization. Within the cancerous field, all stages of AKs may coexist, including individual UV-damaged keratinocytes, subclinical (non-visible, non-palpable) lesions, early clinical lesions, late clinical lesions, and possibly eventually invasive SCCs.
The consequence of this pathophysiology is that the treatment of cutaneous malignancies should focus not only on the tumor but also on the field from which it developed. In terms of AKs, this means that all lesions on the entire sun-exposed field should be targeted and eliminated to provide long-term disease remission and prevent disease recurrence. This concept provides a rationale for field therapy, in which the entire field, rather than individual lesions, is treated. The goals of field therapy are to eliminate clinically visible as well as subclinical lesions and to prevent the development of invasive SCC.
Although broadly applied and effective in clearing visible AKs, lesion-directed therapies such as cryotherapy do not address field cancerization and can lead to high recurrence rates. Field-directed therapies address subclinical damage, reduce AK recurrence rates, and potentially reduce the risk of SCC development [3, 4]. Emerging preclinical evidence indicates that field-directed therapy may have preventive effects and delay recurrence of non-melanoma skin cancers (NMSCs). Thus, field therapy for specialized patient groups, including organ transplant recipients (OTRs) and individuals with a history of chronic sun exposure, are promising developments, as these therapies may confer a preventive potential.
The purpose of this article is to discuss the range of field-directed therapies that are currently available, including photodynamic therapy (PDT) with aminolevulinic acid (ALA) or methylaminolevulinate (MAL), and various topical therapies such as 5-fluorouracil (5-FU) cream (5, 1, 0.5%), imiquimod cream (5, 3.75, 2.5%), diclofenac 3% gel, piroxicam gel (1 and 0.8%), and ingenol mebutate gel (5 and 3.75%). We examine the literature and critically evaluate the role of these treatments as field-directed therapies.
2 Light-Based Minimally Invasive Field Cancerization Therapies
PDT involves the topical application of the precursor molecules ALA or its derivatives (i.e., MAL), which are enzymatically converted through the heme pathway into the active endogenous photosensitizer protoporphyrin IX (PpIX). When an appropriate light source illuminates PpIX, it generates reactive oxygen species (ROS) such as highly cytotoxic singlet oxygen. Cell death follows, driven by direct ROS damage to cell membranes and lipid peroxidation. A reactive inflammatory response is also involved. PpIX preferentially accumulates in pre-malignant and malignant cells, likely due to both enhanced cellular uptake of the precursor molecules and increased heme pathway enzymatic activity. PpIX has several absorption peaks in the visible spectrum, and the 410 nm (blue light) and 635 nm (red light) wavelengths have been broadly applied and received US FDA approval to activate the photodynamic effect. As pre-malignant cells concentrate PpIX even when not clinically visible, PDT represents a field therapy for AKs since an entire area of actinically damaged skin can be treated [5,6,7,8,9].
2.1 Efficacy and Outcomes
The FDA approved PDT with ALA photosensitization and blue light for the treatment of AK in September 2000 [10, 11]. FDA approval for ALA photosensitization and red light followed in 2016 [12, 13]. Initial phase II/phase III trials by Jeffes et al. [14] on face and scalp AKs demonstrated 66% clearance of individual AKs at 8 weeks. A phase III trial by Piacquadio et al. [15] demonstrated individual AK lesion clearance of 83% at 8 weeks, with 66% of patients experiencing complete response rates, that is, 100% AK clearance (Table 1). Both trials gave a second treatment for persistent AKs, finding 85% clearance at 16 weeks and 91% clearance at 12 weeks, respectively. Further studies have investigated PDT with ALA or MAL compared with PDT plus placebo, most recently a double-blind, placebo-controlled multicenter randomized controlled trial (RCT) in 2016 that used red light [12]. These studies have found lesion complete clearance rates of 81–99% for PDT–ALA/–MAL versus 22–37.1% for PDT plus placebo after a maximum of two treatments [12, 16, 17]. Jerjes et al. [18] conducted a longer-term follow-up retrospective evaluation of outcome study in 62 patients at a large tertiary center in the UK. At 3-year follow-up, 96.8% of patients and 98.3% of lesions had complete response.
PDT field therapy has been shown to help prevent AK development. For facial AK, PDT with ALA delayed the development of new AKs by 6 months compared with control [19]. Though not a primary outcome of the 2016 study by Reinhold et al. [12], they did note that—while one patient in the placebo group displayed a new lesion after PDT—no patients in the PDT–ALA group developed new lesions despite the group being twice as large. The ability to reduce the incidence of new AKs may be particularly useful in immunocompromised patients who are at increased risk for new AKs and malignant transformation [20]. Wennberg et al. [20] found that PDT–MAL resulted in a 46% reduction in new AKs at 3 months in transplant patients receiving immunosuppressive therapy. In a longer study, 62% of areas receiving PDT were free from new lesions compared with 35% in control areas 12 months after PDT with MAL in renal transplant patients [21].
Both lesion-targeted PDT and field therapy PDT have been shown to have good outcomes in secondary endpoints. In the early pivotal studies by Jeffes [10], investigators assessed cosmetic results and rated 92% of lesions as appearing “good” or “excellent” after treatment. That same year, investigators in a study by Szeimes et al. [22] graded 96% of cosmetic outcomes for patients treated with PDT as “good” or “excellent” versus 81% for patients treated with cryotherapy. In a comparison study against topical diclofenac, PDT–MAL had significantly greater investigator-reported cosmetic outcomes and never resulted in scarring or pigmentation changes [23].
Daylight is among the light sources that can activate the FDA-approved photosensitizers ALA and MAL. Three split-face/scalp studies, also called intra-individual studies, investigated the efficacy of daylight PDT (d-PDT) compared with conventional PDT (c-PDT) for lesion-targeted treatment. In Italy, Fargnoli et al. [24] showed that d-PDT with MAL had equivalent results to c-PDT with MAL for AK grade I but was not as effective as c-PDT with MAL for AK grades II and III. Two phase III multicenter RCTs demonstrated non-inferiority of d-PDT compared with c-PDT. In the Australian trial, 89.2% of mild AKs treated with d-PDT with MAL had resolved versus 92.8% treated with c-PDT at 12 weeks [25]. In the European trial, 70% of mild AKs treated with d-PDT with MAL had resolved versus 74% treated with c-PDT at 12 weeks [26]. Furthermore, non-inferiority of d-PDT compared with c-PDT for the prevention of new lesions was recently demonstrated. In a split-face/scalp study, there was no statistically significant difference in the development of new lesions at any follow-up point between the d-PDT and c-PDT sides [27]. Interestingly, in two studies of d-PDT, efficacy was maintained regardless of sunny or cloudy weather conditions [26, 27].
2.2 Patient Satisfaction and Preference
We found two surveys of patient satisfaction in the literature. A 2011 telephone survey of Australian patients receiving lesion-targeted therapy found 50% thought PDT–MAL was very effective, and 66% stated they would recommend the therapy. All these patients had previously received cryotherapy for earlier AKs, and patients reported equivalent recovery times [28]. An earlier mailer survey to patients of a hospital in Michigan found patients reported a faster recovery time than with cryotherapy and surgical excision. In this survey, patients had equal preference for PDT, cryotherapy, and trichloroacetic acid destruction and preferred PDT over 5-FU and imiquimod [29]. In an early trial, 98% of patients reported their outcome with PDT as “better than” or “equal to” their results from previous treatments with cryotherapy or 5-FU [22]. Additionally, patients have reported satisfaction with PDT over other therapies such as diclofenac [23]. In a study looking at antihistamine use for side effect prophylaxis, 77.8% of those receiving standard PDT–ALA reported feeling “extremely satisfied” on day 30. On day 180, that number had decreased to 62.5%, with 25% being “slightly satisfied” [30]. Satisfaction is also high with d-PDT. In the European split-face intra-patient trial comparing d-PDT with c-PDT, 64.8% of patients reported being “very satisfied” with the d-PDT treatment side compared with only 18.9% for the c-PDT side [26].
Patient-reported satisfaction with cosmetic outcomes with PDT therapy has been positive. Recently, Tanaka et al. [31] found 83% of patients indicated excellent cosmetic outcome. Of note, despite 88% of patients treated with PDT at a UK tertiary hospital reporting “excellent” cosmetic outcomes, data as of 2015 showed only 15–20% of patients elected PDT over topical or surgical therapies [18]. See Table 2 for a summary of patient satisfaction with PDT.
2.3 Adverse Effects
Pain during the procedure is the primary adverse effect of conventional PDT with ALA or MAL, whether for lesion-targeted therapy or field therapy (Table 3). In the telephone survey by Tran et al. [28], 58% of patients reported severe pain during PTD–MAL illumination, and 42% reported moderate pain. Additionally, 20% of patients required nerve block for pain to continue therapy [28]. A study of 14 patients found that six (43%) required an intermission in the therapy session because of severe pain [32].
Pain reduction approaches can be categorized as pain mitigation or pain control. Pain mitigation approaches optimize treatment variables to minimize pain. Multiple studies have investigated the relative pain caused by various photosensitizers. Six studies found PDT–ALA to be more painful than PDT–MAL [33,34,35,36,37]. In the most striking result, 14% of patients reported severe pain with PDT–MAL compared with 54% with PDT–ALA [33]. At least three of the studies identified showed no statistical difference in pain between ALA and MAL photosensitizers [32, 38, 39]. A study using d-PDT examined pain when using a nano-emulsified preparation of ALA (BF-200 ALA) and found no statistically significant difference between MAL and BF-200 ALA [40]. One complicating factor regarding photosensitizers is the lack of standardized incubation time, with ALA generally receiving a longer incubation time than MAL in the cited studies. Martin [41] attempted to elucidate the incubation question and found that, for ALA, a 15-min incubation time resulted in significantly less pain reported than a 75-min incubation time.
Alternative light sources have also been investigated for pain mitigation. A large study looked at four different light sources used across 688 separate treatments for 483 unique lesions and reported the percentage of treatments for each light source that caused severe pain: xenon (2%), metal halide (16%), halogen (16%), and laser (21%) [42]. d-PDT has received attention because of several studies that reported no pain for many of the patients receiving the treatment, including 17 of 18 patients in a 2012 Swiss study [43]. Three studies investigated d-PDT–MAL compared with c-PDT–MAL and found pain reductions on the 10-point visual analog scale (VAS) of 4.7, 4.9, and 2.2 [24, 25, 44]. Neittaanmäki-Perttu et al. [45] also found that d-PDT–MAL resulted in less pain than c-PDT–MAL. A comparison of light sources is complicated by the lack of standardized irradiation strengths. In one study, low-irradiance c-PDT (7 mW/cm2) delivered over a longer period was shown to be less painful than high-irradiance c-PDT (80 mW/cm2), with similar clearance rates [46].
While pain mitigation approaches have strong potential, especially daylight and low-irradiance/long-exposure protocols, strategies for controlling pain are associated with c-PDT. A review by Ang et al. [47] identified published studies on the following pain-control techniques: nerve block, oral analgesia, intravenous analgesia, subcutaneous infiltration analgesia, inhaled analgesia, cold air, and cold water spray. All four studies of nerve block for pain control during c-PDT found patients given nerve block reported low pain scores [48,49,50,51].
Localized side effects are prominent in PDT regardless of pain reduction. A study of 22 patients receiving one treatment of c-DPT–ALA to the complete face found various side effects in the following percentages of patients: erythema 100%, burning 90.9%, edema 90.9%, itching 86.4%, scaling 81.8%, pustules 59.1%, hypo/hyper-pigmentation 0% [39]. Alternatively, Jerjes et al. [18] found 4.8% of patients in their study had hypoesthesia and 6.5% had hypopigmentation. d-PDT evoked less severe local skin reactions than c-PDT, with statistically significant reductions in erythema (86 vs. 97%), pustular eruption (6 vs. 17%), and crusting (74 vs. 83%) [24].
Gholam et al. [39] pursued a holistic view of the adverse effects of PDT by examining patients’ quality of life as represented by the Dermatology Life Quality Index (DQLI). DLQI score increased from baseline pretreatment (1.6) to a high immediately post-treatment (7.3) and declined steadily (4.4 on day 14), eventually settling better than pre-treatment (0.1 at 4 weeks). A trial of antihistamine prophylaxis for localized adverse effects of PDT measured lifestyle disruption and found no statistical difference between groups. In the antihistamine group, 11.1% of patients reported moderate or severe lifestyle disruption on day 7 versus 20% for PDT without antihistamine. Notably, on day 30, no patients in either group reported “moderate” or “severe” lifestyle disruption [30].
2.4 Cost
Kirby et al. [52] estimated average annual patient costs based on utilization for various therapies for AK: ingenol mebutate $US847, imiquimod $US823, PDT with ALA or MAL $US532, diclofenac $US414, 5-FU $US311, cryotherapy for > 15 lesions $US299 (cryotherapy for one lesion $US129). Multiple studies have directly compared c-PDT and specific topical therapies, with somewhat conflicting results. Over 1 year, imiquimod was £174 less costly than PDT–MAL therapy from the perspective of the UK National Health Service, although PDT resulted in an additional 0.005 quality-adjusted life-years (QALYs) gained. The incremental cost-effectiveness ratio (ICER) for PDT–MAL versus imiquimod was £34,576 [53]. Imiquimod and PDT–MAL both generated higher total costs than diclofenac [54]. Conversely, a cost-effectiveness analysis found a higher per-patient cost for PDT–MAL but a lower cost per patient with complete response than for diclofenac at both 2 and 12 months. PDT had a significantly better lesion complete clearance rate of 85.9 versus 51.8% for diclofenac; thus, PDT–MAL was more expensive but was also more cost effective [55]. Using data from Finland, Soini et al. [56] investigated PDT–MAL compared with cryosurgery, imiquimod, diclofenac, and ingenol mebutate. PDT–MAL was the most effective treatment but cost more than all other treatments, with an ICER of €82,706 versus ingenol mebutate, which was the most cost-effective treatment. See Table 4 for a summary of costs.
It may be useful to note that major policies in the USA preferentially reimburse procedural therapies above pharmacologic treatments, tending to favor cryotherapy over PDT [57]. Most economic studies do not include costs of adverse effects or recurrence. Importantly, the preventive aspect of PDT field therapy has not yet been included in the economic cost-effectiveness literature.
3 Topical Therapies
3.1 5-Fluorouracil
Field-directed therapy with topical 5-FU is a common modality for AKs because of its well-understood mechanism and efficacy (Table 5). This anti-metabolic drug inhibits thymidylate synthetase, an enzyme required for DNA synthesis, preventing cell proliferation and resulting in cell death [58]. Considered a gold standard for topical treatment of AKs, 5-FU is available in creams and solutions of 0.5, 1, 2 and 5%. Destruction of lesions results in inflammation following treatment, with possible local skin reactions including erythema, blistering, scabbing, and itching on treatment sites. Studies have found a combination of 0.5% 5-FU and 10% salicylic acid (5-FU–SA) to be associated with greater efficacy and fewer adverse effects in the management of AKs. 5-FU–SA should be applied once daily for up to 12 weeks, with responses noticeable 4–8 weeks following treatment [58]. Szeimies et al. [59] showed that 5-FU–SA treatment led to a 70% decrease in the mean number of lesions and a 90% decrease in the mean size of AKs. A 2017 study found that complete clinical clearance (CCC) was significantly higher (p = 0.0006) in patients treated with 5-FU–SA than in patients receiving vehicle (49.5 vs. 18.2%, respectively) [60]. Similar studies by Stockfleth and colleagues [60,61,62] found significantly more lesions cleared with 5-FU–SA than with vehicle (74.5 vs. 35.5%; p < 0.001), and 85.8% of the lesions did not recur in the 5-FU–SA group. In these same three randomized, double-blind, vehicle-controlled studies, mild to moderate treatment-emergent adverse events were more common with 5-FU than with a vehicle gel but did not lead to therapy discontinuation. Treatment tolerability was rated as “very good” or “good” in 87% of patients, making 5-FU–SA a favorable option for long-term management of AKs [59].
3.2 Diclofenac Sodium
Diclofenac sodium (DFS) is a nonsteroidal anti-inflammatory drug (NSAID) that targets AKs through the induction of apoptosis and the inhibition of angiogenesis. It inhibits both cyclooxygenase (COX)-2, of which AKs have increased activity, and the upregulation of the arachidonic acid cascade, preventing the production of prostaglandins and thus the formation of UV-induced skin cancers [63]. Its common application includes diclofenac 3 in 2.5% hyaluronic acid gel applied twice daily for 60–90 days. In one study, 41% of patients experienced CCC following 16 weeks of treatment [64]. In another study, DFS resulted in reduction of lesion size by 64.7% compared with 34.3% in the vehicle group [65]. Additionally, a significantly higher proportion of patients treated with DFS had a total lesion number score (TLNS) of 0 compared with the vehicle group (50 vs. 20%; p < 0.001) [66]. This treatment regimen appears to be better tolerated than once-daily application of 5-FU–SA, with patients expressing significant satisfaction and reporting fewer adverse effects [61]. In two different studies, patients observed no significant side effects and reported treatment to be well tolerated [65, 66]. Another study showed adverse effects to be limited to mild erythema and mild–moderate swelling of treated areas [64]. Similarly, one study reported that only 24% of patients experienced irritant-type contact dermatitis confined to the treatment site [67]. Despite being better tolerated, DFS is less effective than 5-FU–SA, with the latter demonstrating higher histological and clinical clearance rates [61]. See Table 6 for a summary.
3.3 Piroxicam
Piroxicam is an NSAID that has received attention as an alternative to diclofenac for both lesional and field-directed AK therapy (Table 7). Piroxicam appears to have more potent COX-1 inhibitory action than diclofenac [68]. It is hypothesized that the synergistic co-treatment of COX-1 and COX-2 results in a significant inhibition of vascular epidermal growth factor (VEGF), a growth factor important in tumor proliferation [69]. In a study in 2010 [70], ten patients (31 lesions) applied a preparation of piroxicam 1% gel twice daily for 12 weeks. Complete response was observed in 15 lesions (48%) [70]. More recent studies have used a novel topical preparation that includes both piroxicam 0.8% and a 50 + sun protection factor (SPF) sunscreen. Puviani et al. [71] reported a 55% reduction in the number of AKs in areas treated twice daily for 12 weeks. The use of a piroxicam plus sunscreen preparation limits the ability to make direct comparisons between piroxicam and other topical treatments such as diclofenac. However, it is worth noting that daily application of a separate sunscreen product is a component of the treatment regimen in many topical studies. A treatment plus sunscreen preparation may be particularly useful when treating OTRs, a population for whom treating existing field-cancerization and preventing additional photodamage are both essential. In a case series of ten OTR patients treated for 16 weeks with a piroxicam plus sunscreen preparation, three patients (30%) experienced complete clearance, and an additional four patients (40%) had marked (≥ 75% lesion count reduction) improvement in their overall AK lesion count [72]. In the 2010 study by Campione et al. [70], adverse effects included pruritus (25% of patients), mild erythema (25%), dry skin (10%), and rash (2%); none of these required treatment suspension.
3.4 Imiquimod
Imiquimod, of the imidazoquinoline family, is a synthetic nucleoside analog that activates Toll-like receptors (TLRs)-7/8, resulting in the activation of the innate immune response and enhancement of interferon (IFN), tumor necrosis factor (TNF), and interleukins (IL)-1 and -12, which then results in an acquired immune response [73]. Specifically, topical imiquimod induces IFNα within AK lesions, triggering both innate and adaptive immune responses [74]. Its common application includes 2.5, 3.75 and 5% creams. In one study, patients applied imiquimod 5% three times weekly for 16 weeks; 48.3% of patients reported CCC and 64.0% reported partial clearance (PC) compared with vehicle-treated patients (7.2 and 13.6%, respectively; p < 0.001) [75]. In another study, 46% of patients experienced CCC, and 35% experienced PC [76]. When response rates were linked to adverse events, a significant trend (p = 0.001) was found, showing a higher percentage of adverse events in the CCC group than in the PC group (74 vs. 39%, respectively) [76]. In a different study, application site reactions were reported by 38.8% of patients (p < 0.001), fever by 2.9% (p = 0.04), and postoperative pain by 3.7% (p = 0.03) [75]. Local erythema has also been reported as an adverse side effect [77]. Overall, imiquimod was well tolerated and led to few treatment-related discontinuations [78, 79], but satisfaction was only 55–60% in imiquimod-treated patients [76]. A pharmacoeconomic analysis of management of AKs assumed standard costs of procedures and office visits and two treatment courses and found imiquimod to be the most expensive treatment compared with 5-FU, DFS, and PDT–ALA [80]. The total cost for each was $US725.17 for PDT–ALA, $US845.07 for diclofenac, $US942.13 for 5-FU, and $US1473.39 for imiquimod, with costs of imiquimod and DFS increasing because of lower efficacy and the need for additional treatments to reach 100% clearance [80]. See Table 8 for a summary of imiquimod efficacy and adverse effects.
3.5 Ingenol Mebutate
Ingenol mebutate (IM) acts as a protein kinase C (PKC) agonist, stimulating neutrophil-mediated antibody-dependent cellular cytotoxicity and activating necrosis of dysplastic AKs [81]. Approved in 2012 by the FDA for the treatment of AKs, IM is commonly used in gels of 0.015, 0.025 and 0.05% (Table 9). A study assessing the efficacy of IM 0.015% applied once daily for 3 consecutive days observed CCC in 46.7% of patients versus 18.4% in the vehicle group (p < 0.001) [82]. Similarly, a study measuring short-term clearance rates of AKs at week 11 found CCC to be higher in the IM group (60.5%) than in the vehicle group (49.4%) [83]. Another study using IM 0.025% and IM 0.05% gel found that both active treatments were significantly more effective than the vehicle at clearing AK lesions [84]. IM appears to be generally well tolerated, with one study stating that 90% of patients reported a “good” or “excellent” treatment experience [85]. Adverse effects tend to be limited to transient local skin responses, such as erythema, crusting, and flaking, with no evidence of treatment-related scarring [84]. A study comparing the cost of DFS versus IM in the treatment of AKs over a period of 12 months, with costs defined as the cost of treatment and the direct costs of the first consultation with the dermatologist, found IM to be more expensive than DFS [86]. Patients treated with IM also reported an overall lower quality of life than those treated with DFS (469.5 vs. 478 QALYs), although statistical analysis showed this to be non-significant [86]. Thus, treatment with IM is associated with higher treatment costs than, but the same efficacy as, DFS.
4 Conclusion
There is no widely accepted algorithm for the treatment of AKs and the management of generalized actinic skin damage. Treatment comprises a variety of lesion-directed or field-directed therapies, or a combination of both, in conjunction with additional therapies tailored to patient needs. Determining the appropriate treatment of AK should be individualized to account for both lesion-related (morphology, duration) and patient-related factors (age, immune status, cosmesis, pain tolerance). Factors related to the treatment modalities, including clearance rates, treatment duration, tolerability profiles, adherence rates, and costs, all need to be considered when selecting a treatment. Some therapies may be more appropriate than others for certain anatomical sites. In general, therapies with shorter and simpler treatment courses and temporary mild-to-moderate skin reactions are associated with better adherence than are treatments with longer courses.
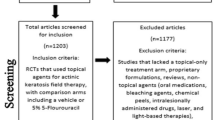
We propose the therapeutic algorithm shown in Fig. 1 for selecting an appropriate treatment in the evaluation of a patient with AK in the clinical setting. One must first consider whether a lesion-directed therapy or field-directed approach is more suitable. The authors recommend lesion-directed therapies, such as cryotherapy, for patients with few well-defined lesions. Field-directed therapy is recommended for any surface with multiple (more than four to eight) AKs, for example, the face, scalp, forearm, etc., with the appropriateness of field-directed therapy increasing further when the AKs occur in photo-exposed areas and the patient has a history of significant sun exposure, recurrent AKs, history of chronic immunosuppression, and history of NMSC [4]. In the near-term, it is likely that field-directed therapy will become the best practice for high-risk patients such as OTRs [20, 21].
Once the decision to pursue field-directed therapy is made, deciding between PDT and topical therapy requires consideration of multiple patient- and clinician-related factors. The advantages of PDT are that the procedure can be performed within 1 day by a physician in an office-based setting, has high cure rates and excellent cosmetic results after one to two sessions, and has a shorter period of therapy-induced inflammation than long-term application of topical therapies such as imiquimod, 5-FU, diclofenac, or piroxicam [10,11,12, 16,17,18, 22, 23, 60,61,62, 70, 76, 78, 79, 84]. PDT is generally more successful than topical therapy when adherence by the patient is in question, especially given the months-long daily application required by some topicals [23]. Poor results after previous attempts at treatment with topicals is another reason to consider PDT [18]. Additionally, patient-reported satisfaction seems to support somewhat of a patient preference for PDT over topical therapy [22, 23, 29]. One disadvantage of PDT is pain during illumination, although more widespread adoptions of “slow” or “fractionated” PDT and d-PDT may ameliorate this concern [24, 25, 28, 32, 41, 43,44,45]. PDT is therefore an appropriate treatment option for patients with multiple AKs because of its high response rate, limited downtime, and excellent aesthetic outcome.
Current reimbursement policies can sometimes dissuade the clinician from using PDT [57]. In the authors’ experience, procedure-based reimbursement for cryotherapy can be equivalent to, and even better than PDT, despite the greater time required by the clinician and/or support staff for PDT. Similarly, topical field therapy places less demand on the clinician’s time than PDT as the topical treatment is applied by the patient at home. Furthermore, the existence in the literature of many different PDT regimens, most of which are not FDA approved, including d-PDT, can make it difficult for a clinician without previous experience to start using PDT [10, 12, 14,15,16,17,18,19,20,21,22,23,24,25,26, 87]. More large, high-quality studies comparing modalities of PDT will be helpful.
Topical therapies are a non-procedural form of field cancerization therapy. Several topical therapies are available for the treatment of AKs, including 5-FU cream (5%, 1%, 0.5%), imiquimod 5% cream (5% and 3.75%), diclofenac 3% gel, piroxicam 1% gel, and IM gel (5% and 3.75%). Studies have shown similar efficacy for these topicals, but their associated adverse events and cosmetic outcomes differ. Topical therapies in preparations that include sunscreen are advantageous given the importance of regular sunscreen use in AK management [88,89,90]. Disadvantages of topical field-directed therapies include a more prolonged treatment course (up to 16 weeks) and adverse effects such as photosensitivity, which reduces patients’ ability to tolerate treatment. These disadvantages can decrease patient adherence and ultimately result in suboptimal effectiveness. Better adherence in a real-world setting would be expected for IM given the shorter treatment duration and transient local skin reactions. Further research with more direct comparisons between these procedural and non-procedural field-directed therapies are necessary to determine the best therapeutic approach.
References
Siegel JA, Korgavkar K, Weinstock MA. Current perspective on actinic keratosis: a review. Br J Dermatol. 2017;177:350–8.
Marks R, Jolley D, Dorevitch AP, Selwood TS. The incidence of non-melanocytic skin cancers in an Australian population: results of a five-year prospective study. Med J Aust. 1989;150:475–8.
Calzavara-Pinton P, Venturini M, Sala R. Photodynamic therapy: update 2006. Part 2: Clinical results. J Eur Acad Dermatol Venereol. 2006;2007(21):439–51.
Dodds A, Chia A, Shumack S. Actinic keratosis: rationale and management. Dermatol Ther (Heidelb). 2014;4:11–31.
Dougherty TJ, Kaufman JE, Goldfarb A, Weishaupt KR, Boyle D, Mittleman A. Photoradiation therapy for the treatment of malignant tumors. Cancer Res. 1978;38(8):2628–35.
Kennedy JC, Pottier RH. Endogenous protoporphyrin IX, a clinically useful photosensitizer for photodynamic therapy. J Photochem Photobiol B. 1992;14(4):27592.
Brancaleon L, Moseley H. Laser and non-laser light sources for photodynamic therapy. Lasers Med Sci. 2002;17:173–86.
Babilas P, Landthaler M, Szeimies R. Photodynamic therapy in dermatology. Eur J Dermatol. 2006;16:340.
Juzeniene A. Photodynamic therapy at the cellular level: the principles of 5-aminolevulinic acid photodynamic therapy. Trivandrum: Research Signpost; 2007. p. 115–40.
Jeffes E. Levulan: the first approved topical photosensitizer for the treatment of actinic keratosis. J Dermatol Treat. 2002;13:s23.
Kelty CJ, Brown NJ, Reed MWR, Ackroyd R. The use of 5-aminolaevulinic acid as a photosensitiser in photodynamic therapy and photodiagnosis. Photochem Photobiol Sci. 2002;1:158–68.
Reinhold U, Dirschka T, Ostendorf R, Aschoff R, Berking C, Philipp-Dormston WG, et al. A randomized, double-blind, phase III, multicentre study to evaluate the safety and efficacy of BF-200 ALA (Ameluz®) vs. placebo in the field-directed treatment of mild-to-moderate actinic keratosis with photodynamic therapy (PDT) when using the BF-RhodoLED® lamp. Br J Dermatol. 2016;175:696–705.
Center for Drug Evaluation and Research. Approval package for application number: 208081Orig1s000. 5 October 2016.
Jeffes EW, McCullough JL, Weinstein GD, Kaplan R, Glazer SD, Taylor JR. Photodynamic therapy of actinic keratoses with topical aminolevulinic acid hydrochloride and fluorescent blue light. J Am Acad Dermatol. 2001;45:96–104.
Piacquadio DF, Chen DM, Farber HF, Fowler JF, Glazer SD, Goodman JJ, et al. Photodynamic therapy with aminolevulinic acid topical solution and visible blue light in the treatment of multiple actinic keratoses of the face and scalp: investigator-blinded, phase 3, multicenter trials. Arch Dermatol. 2004;140:41.
Szeimies RM, Radny P, Sebastian M, Borrosch F, Dirschka T, Krahn-Senftleben G, et al. Photodynamic therapy with BF-200 ALA for the treatment of actinic keratosis: results of a prospective, randomized, double-blind, placebo-controlled phase III study. Br J Dermatol. 2010;163:386–94.
Dirschka T, Radny P, Dominicus R, Mensing H, Brüning H, Jenne L, et al. Photodynamic therapy with BF-200 ALA for the treatment of actinic keratosis: results of a multicentre, randomized, observer-blind phase III study in comparison with a registered methyl-5-aminolaevulinate cream and placebo. Br J Dermatol. 2012;166:137–46.
Jerjes W, Hamdoon Z, Abdulkareem AA, Hopper C. Photodynamic therapy in the management of actinic keratosis: Retrospective evaluation of outcome. Photodiagn Photodyn Ther. 2017;17:200–4.
Apalla Z, Sotiriou E, Chovarda E, Lefaki I, Devliotou-Panagiotidou D, Ioannides D. Skin cancer: preventive photodynamic therapy in patients with face and scalp cancerization. A randomized placebo-controlled study. Br J Dermatol. 2010;162:171–5.
Wennberg A, Stenquist B, Stockfleth E, Keohane S, Lear JT, Jemec G, et al. Photodynamic therapy with methyl aminolevulinate for prevention of new skin lesions in transplant recipients: a randomized study. Transplantation. 2008;86:423–9.
Wulf HC, Pavel S, Stender I, Ahb Bakker-Wensveen C. Topical photodynamic therapy for prevention of new skin lesions in renal transplant recipients. Acta Derm Venereol. 2006;86:25–8.
Szeimies RM, Karrer S, Radakovic-Fijan S, Tanew A, Calzavara-Pinton P, Zane C, et al. Photodynamic therapy using topical methyl 5-aminolevulinate compared with cryotherapy for actinic keratosis: a prospective, randomized study. J Am Acad Dermatol. 2002;47:258–62.
Zane C, Capezzera R, Sala R, Venturini M, Calzavara-Pinton P. Clinical and echographic analysis of photodynamic therapy using methylaminolevulinate as sensitizer in the treatment of photodamaged facial skin. Lasers Surg Med. 2007;39:203–9.
Fargnoli MC, Piccioni A, Neri L, Tambone S, Pellegrini C, Peris K. Conventional vs. daylight methyl aminolevulinate photodynamic therapy for actinic keratosis of the face and scalp: an intra-patient, prospective, comparison study in Italy. J Eur Acad Dermatol Venereol. 2015;29:1926–32.
Rubel DM, Spelman L, Murrell DF, See JA, Hewitt D, Foley P, et al. Daylight photodynamic therapy with methyl aminolevulinate cream as a convenient, similarly effective, nearly painless alternative to conventional photodynamic therapy in actinic keratosis treatment: a randomized controlled trial. Br J Dermatol. 2014;171:1164–71.
Lacour J, Ulrich C, Gilaberte Y, Von Felbert V, Basset-Seguin N, Dreno B, et al. Daylight photodynamic therapy with methyl aminolevulinate cream is effective and nearly painless in treating actinic keratoses: a randomised, investigator-blinded, controlled, phase III study throughout Europe. J Eur Acad Dermatol Venereol. 2015;29:2342–8.
Sotiriou E, Apalla Z, Vrani F, Lazaridou E, Vakirlis E, Lallas A, et al. Daylight photodynamic therapy vs. Conventional photodynamic therapy as skin cancer preventive treatment in patients with face and scalp cancerization: an intra-individual comparison study. J Eur Acad Dermatol Venereol. 2017;31:1303–7.
Tran DT, Salmon R. Field treatment of facial and scalp actinic keratoses with photodynamic therapy: survey of patient perceptions of treatment satisfaction and outcomes. Australas J Dermatol. 2011;52:195–201.
Tierney EP, Eide MJ, Jacobsen G, Ozog D. Photodynamic therapy for actinic keratoses: survey of patient perceptions of treatment satisfaction and outcomes. J Cos Laser Therapy. 2008;10:81–6.
Vanaman Wilson MJ, Jones IT, Wu DC, Goldman MP. A randomized, double-blind, placebo-controlled clinical trial evaluating the role of systemic antihistamine therapy for the reduction of adverse effects associated with topical 5-aminolevulinic acid photodynamic therapy. Lasers Surg Med. 2017;49:738–42.
Tanaka N, Ohata C, Ishii N, Imamura K, Ueda A, Furumura M, et al. Comparative study for the effect of photodynamic therapy, imiquimod immunotherapy and combination of both therapies on 40 lesions of actinic keratosis in Japanese patients. J Dermatol. 2013;40:962–7.
Yazdanyar S, Zarchi K, Jemec GBE. Pain during topical photodynamic therapy—comparing methyl aminolevulinate (Metvix®) to aminolaevulinic acid (Ameluz®); an intra-individual clinical study. Photodiagnosis Photodyn Ther. 2017;20:6–9.
Kasche A, Luderchmidt S, Ring J, Hein R. Photodynamic therapy induces less pain in patients treated with methyl aminolevulinate compared to aminolevulinic acid. J Drugs Dermatol. 2006;5(4):353–6.
Moloney FJ, Collins P. Randomized, double-blind, prospective study to compare topical 5-aminolaevulinic acid methylester with topical 5-aminolaevulinic acid photodynamic therapy for extensive scalp actinic keratosis. Br J Dermatol. 2007;157:87–91.
Steinbauer JM, Schreml S, Babilas P, Zeman F, Karrer S, Landthaler M, et al. Topical photodynamic therapy with porphyrin precursors-assessment of treatment-associated pain in a retrospective study. Photochem Photobiol Sci. 2009;8:1111–6.
Arits A, Weert VD, Nelemans PJ, Kelleners-Smeets N. Pain during topical photodynamic therapy: uncomfortable and unpredictable. J Eur Acad Dermatol Venereol. 2010;24:1452–7.
Gaál M, Otrosinka S, Baltás E, Ocsai H, Oláh J, Kemény L, et al. Photodynamic therapy of non-melanoma skin cancer with methyl aminolaevulinate is associated with less pain than with aminolaevulinic acid. Acta Derm Venereol. 2012;92:173–5.
Ibbotson SH, Valentine R, Hearn R. Is the pain of topical photodynamic therapy with methyl aminolevulinate any different from that with 5-aminolaevulinic acid? Photodermatol Photoimmunol Photomed. 2012;28:272–3.
Gholam P, Kroehl V, Enk AH. Dermatology life quality index and side effects after topical photodynamic therapy of actinic keratosis. Dermatology. 2013;226:253–9.
Neittaanmäki-Perttu N, Karppinen TT, Grönroos M, Tani TT, Snellman E. Daylight photodynamic therapy for actinic keratoses: a randomized double-blinded nonsponsored prospective study comparing 5-aminolaevulinic acid nanoemulsion (BF-200) with methyl-5-aminolaevulinate. Br J Dermatol. 2014;171:1172–80.
Martin GM. In-office painless aminolevulinic acid photodynamic therapy: a proof of concept study and clinical experience in more than 100 patients. J Clin Aesthetic Dermatol. 2016;9:19.
Clark C, Bryden A, Dawe R, Moseley H, Ferguson J, Ibbotson SH. Topical 5-aminolaevulinic acid photodynamic therapy for cutaneous lesions: outcome and comparison of light sources. Photodermatol Photoimmunol Photomed. 2003;19:134–41.
Braathen LR. Daylight photodynamic therapy in private practice in Switzerland: gain without pain. Acta Derm Venereol. 2012;92:652.
Wiegell SR, Haedersdal M, Philipsen PA, Eriksen P, Enk CD, Wulf HC. Continuous activation of PpIX by daylight is as effective as and less painful than conventional photodynamic therapy for actinic keratoses; a randomized, controlled, single-blinded study. Br J Dermatol. 2008;158:740–6.
Neittaanmäki-Perttu N, Grönroos M, Karppinen T, Snellman E, Rissanen P. Photodynamic therapy for actinic keratoses: a randomized prospective non-sponsored cost-effectiveness study of daylight-mediated treatment compared with light-emitting diode treatment. Acta Derm Venereol. 2016;96:241.
Ibbotson SH, Ferguson J. Ambulatory photodynamic therapy using low irradiance inorganic light-emitting diodes for the treatment of non-melanoma skin cancer: an open study. Photodermatol Photoimmunol Photomed. 2012;28:235–9.
Ang JM, Riaz IB, Kamal MU, Parah G, Zeitouni NC. Photodynamic therapy and pain: a systematic review. Photodiagn Photodyn Ther. 2017;19:308–44.
Paoli J, Halldin C, Ericson MB, Wennberg A. Nerve blocks provide effective pain relief during topical photodynamic therapy for extensive facial actinic keratoses. Clin Exp Dermatol. 2008;33:559–64.
Halldin CB, Paoli J, Sandberg C, Gonzalez H, Wennberg AM. Nerve blocks enable adequate pain relief during topical photodynamic therapy of field cancerization on the forehead and scalp. Br J Dermatol. 2009;160:795–800.
Serra-Guillen C, Hueso L, Nagore E, Vila M, Llombart B, Requena Caballero C, et al. Comparative study between cold air analgesia and supraorbital and supratrochlear nerve block for the management of pain during photodynamic therapy for actinic keratoses of the frontotemporal zone. Br J Dermatol. 2009;161:353–6.
Klein A, Karrer S, Horner C, Werner A, Heinlin J, Zeman F, et al. Comparing cold-air analgesia, systemically administered analgesia and scalp nerve blocks for pain management during photodynamic therapy for actinic keratosis of the scalp presenting as field cancerization: a randomized controlled trial. Br J Dermatol. 2015;173:192–200.
Kirby JS, Delikat A, Leslie D, Miller JJ. Bundled payment models for actinic keratosis management. JAMA Dermatol. 2016;152:789–97.
Wilson E. Cost effectiveness of imiquimod 5% cream compared with methyl aminolevulinate-based photodynamic therapy in the treatment of non-hyperkeratotic, non-hypertrophic actinic (Solar) Keratoses a decision tree model. Pharmacoeconomics. 2010;28:1055–64.
Colombo GL, Chimenti S, Di Matteo S, Fargnoli MC, Frascione P, Silipo V, et al. Cost-effectiveness analysis of topical treatments for actinic keratosis in the perspective of the Italian health care system. Giornale italiano di dermatologia e venereologia : organo ufficiale, Società italiana di dermatologia e sifilografia. 2010;145:573.
Zane C, Facchinetti E, Rossi MT, Specchia C, Calzavara-Pinton PG. A randomized clinical trial of photodynamic therapy with methyl aminolaevulinate vs. diclofenac 3% plus hyaluronic acid gel for the treatment of multiple actinic keratoses of the face and scalp. Br J Dermatol. 2014;170:1143–50.
Soini E, Hallinen T, Sokka A, Saarinen K. Cost-utility of first-line actinic keratosis treatments in Finland. Adv Ther. 2015;32:455–76.
Vale S, Hill D, Feldman S. Pharmacoeconomic considerations in treating actinic keratosis: an update. Pharmacoeconomics. 2017;35:177–90.
de Berker D, McGregor JM, Hughes BR. Guidelines for the management of actinic keratoses. Br J Dermatol. 2007;156:222–30.
Szeimies R, Dirschka T, Prechtl A, Melzer A. Efficacy of low-dose 5-fluorouracil/salicylic acid in actinic keratoses in relation to treatment duration. JDDG Journal der Deutschen Dermatologischen Gesellschaft. 2015;13:430–8.
Stockfleth E, von Kiedrowski R, Dominicus R, Ryan J, Ellery A, Falques M, et al. Efficacy and safety of 5-fluorouracil 0.5%/salicylic acid 10% in the field-directed treatment of actinic keratosis: a phase III, randomized, double-blind, vehicle-controlled trial. Dermatol Ther (Heidelb). 2011;7:81–96.
Stockfleth E, Kerl H, Zwingers T, Willers C. Low-dose 5-fluorouracil in combination with salicylic acid as a new lesion-directed option to treat topically actinic keratoses: histological and clinical study results. Br J Dermatol. 2011;165:1101–8.
Stockfleth E, Zwingers T, Willers C. Recurrence rates and patient assessed outcomes of 0.5% 5-fluorouracil in combination with salicylic acid treating actinic keratoses. Eur J Dermatol. 2012;22:370–4.
Berman B, Villa AM, Ramirez CC. Mechanisms of action of new treatment modalities for actinic keratosis. J Drugs Dermatol. 2006;5:167–73.
Ulrich C, Johannsen A, Röwert-Huber J, Ulrich M, Sterry W, Stockfleth E. Results of a randomized, placebo-controlled safety and efficacy study of topical diclofenac 3% gel in organ transplant patients with multiple actinic keratoses. Eur J Dermatol. 2010;20:482–8.
Iraji F, Asilian A, Amir HS, Safavai A. Efficacy of 3% diclofenac gel for the treatment of actinic keratoses: a randomized, double-blind, placebo controlled study. Indian J Dermatol Venereol Leprol. 2006;72:346–9.
Wolf JE, Taylor JR, Tschen E, Kang S. Topical 3.0% diclofenac in 2.5% hyaluronan gel in the treatment of actinic keratoses. Int J Dermatol. 2001;40:709–13.
Rivers JK, McLean DI. An open study to assess the efficacy and safety of topical 3% diclofenac in a 2.5% hyaluronic acid gel for the treatment of actinic keratoses. Arch Dermatol. 1997;133:1239–42.
Hawkey CJ. COX-1 and COX-2 inhibitors. Best Pract Res Clin Gastroenterol. 2001;15:801–20.
Campione E, Paternò EJ, Candi E, Falconi M, Costanza G, Diluvio L, et al. The relevance of piroxicam for the prevention and treatment of nonmelanoma skin cancer and its precursors. Drug Des Devel Ther. 2015;9:5843–50.
Campione E, Diluvio L, Paternò EJ, Chimenti S. Topical treatment of actinic keratoses with piroxicam 1% gel: a preliminary open-label study utilizing a new clinical score. Am J Clin Dermatol. 2010;11(1):45–50.
Puviani M, Galloni C, Marchetti S. Efficacy of a film-forming medical device containing sunscreen (50 +) and piroxicam 0.8% in actinic keratosis and field cancerization: a multicenter, assessor-blinded, 3 month trial. Curr Med Res Opin. 2017;33(7):1255–9.
Garofalo C, Ventura A, Mazzilli S. Treatment of multiple actinic keratosis and field of cancerization with topical piroxicam 0.8% and Sunscreen 50 + in organ transplant recipients: a series of 10 cases. Case Rep Dermatol. 2017;9(3):211–6.
Urosevic M, Maier T, Benninghoff B, Slade H, Burg G, Dummer R. Mechanisms underlying imiquimod-induced regression of basal cell carcinoma in vivo. Arch Dermatol. 2003;139:1325–32.
Khanna R, Bakshi A, Amir Y, Goldenberg G. Patient satisfaction and reported outcomes on the management of actinic keratosis. Clin Cosmet Investig Dermatol. 2017;10:179–84.
Korman N, Moy R, Ling M. Dosing with 5% imiquimod cream 3 times per week for the treatment of actinic keratosis: results of two phase 3, randomized, double-blind, parallel-group, vehicle-controlled trials. Arch Dermatol. 2005;141:467–73.
Waalboer-Spuij R, Holterhues C, van Hattem S, Schuttelaar MLA, Gaastra MTW, Kuijpers DIM, et al. Patient perception of imiquimod treatment for actinic keratosis and superficial basal cell carcinoma in 202 patients. Dermatology. 2015;231:56–62.
Hanke CW, Beer KR, Stockfleth E, Wu J, Rosen T, Levy S. Imiquimod 2.5% and 3.75% for the treatment of actinic keratoses: results of two placebo-controlled studies of daily application to the face and balding scalp for two 3-week cycles. J Am Acad Dermatol. 2010;62:573–81.
Swanson N, Abramovits W, Berman B, Kulp J, Rigel DS, Levy S. Imiquimod 2.5% and 3.75% for the treatment of actinic keratoses: results of two placebo-controlled studies of daily application to the face and balding scalp for two 2-week cycles. J Am Acad Dermatol. 2010;62:582–90.
Swanson N, Smith CC, Kaur M, Goldenberg G. Imiquimod 2.5% and 3.75% for the treatment of actinic keratoses: two phase 3 multicenter, randomized, double-blind, placebo-controlled studies. J Drugs Dermatol. 2013;12:1278–82.
Gold MH. Pharmacoeconomic analysis of the treatment of multiple actinic keratoses. J Drugs Dermatol 2008;7(1):23–5.
Aditya S, Gupta S. Ingenol mebutate: a novel topical drug for actinic keratosis. Indian Dermatol Online J. 2013;4:246–9.
Garbe C, Basset-Seguin N, Poulin Y, Larsson T, Østerdal ML, Venkata R, et al. Efficacy and safety of follow-up field treatment of actinic keratosis with ingenol mebutate 0.015% gel: a randomized, controlled 12-month study. Br J Dermatol. 2016;174:505–13.
Berman B, Goldenberg G, Hanke CW, Tyring SK, Werschler WP, Knudsen KM, et al. Efficacy and safety of ingenol mebutate 0.015% gel 3 weeks after cryosurgery of actinic keratosis: 11-Week results. Journal of Drugs. Dermatology. 2014;13:154–60.
Anderson L, Schmieder GJ, Werschler WP, Tschen EH, Ling MR, Stough DB, et al. Randomized, double-blind, double-dummy, vehicle-controlled study of ingenol mebutate gel 0.025 and 0.05% for actinic keratosis. J Am Acad Dermatol. 2009;60:934–43.
Schaefer D. Survey of patient satisfaction with ingenol mebutate gel treatment of actinic keratosis from a community dermatology practice. J Am Acad Dermatol. 2015;72:AB193.
Nisticò S, Torchia V, Gliozzi M, Bottoni U, Del Duca E, Muscoli C. Pharmacoeconomy of drugs used in the treatment of actinic keratoses. Int J Immunopathol Pharmacol. 2016;29:796–804.
Sotiriou E, Apalla Z, Vrani F, Lazaridou E, Vakirlis E, Lallas A, et al. Daylight photodynamic therapy vs. Conventional photodynamic therapy as skin cancer preventive treatment in patients with face and scalp cancerization: an intra-individual comparison study. J Eur Acad Dermatol Venereol. 2017;31:1303–7.
Thompson SC, Jolley D, Marks R. Reduction of solar keratoses by regular sunscreen use. N Engl J Med. 1993;329(16):1147–51.
Naylor MF, Boyd A, Smith DW, Cameron GS. High sun protection factor sunscreens in the suppression of actinic neoplasia. Arch Dermatol. 1995;131(2):170–5.
Ulrich C, Jürgensen JS, Degen A. Prevention of non-melanoma skin cancer in organ transplant patients by regular use of a sunscreen: a 24 months, prospective, case-control study. Br J Dermatol. 2009;161(Suppl 3):78–84.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
Nathan Jetter, Neha Chandan, Stephanie Wang, and Maria Tsoukas have no potential conflicts of interest related to this manuscript.
Rights and permissions
About this article
Cite this article
Jetter, N., Chandan, N., Wang, S. et al. Field Cancerization Therapies for Management of Actinic Keratosis: A Narrative Review. Am J Clin Dermatol 19, 543–557 (2018). https://doi.org/10.1007/s40257-018-0348-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-018-0348-7