Abstract
Secukinumab (Cosentyx™) is a fully human monoclonal immunoglobulin G1κ antibody targeting human interleukin-17A, an important cytokine in the pathogenesis of psoriasis. Secukinumab, as well as being first in its drug class, is the first biologic treatment to be approved in the EU for the first-line systemic treatment of moderate to severe plaque psoriasis. This article reviews the pharmacologic properties of secukinumab and its clinical efficacy and tolerability in adult patients with moderate to severe plaque psoriasis. In clinical trials, subcutaneous secukinumab was more effective than placebo, etanercept and ustekinumab at improving both psoriasis symptoms (with high skin clearance) and health-related quality of life. Moreover, secukinumab was more effective than placebo in the difficult-to-treat palmoplantar and nail psoriasis populations. Secukinumab was generally well tolerated, with low immunogenicity. Longer-term, efficacy was sustained and secukinumab remained well tolerated. Subcutaneous secukinumab is an effective and generally well tolerated first-line treatment for moderate to severe plaque psoriasis, and is a useful addition to the treatment options for this disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
First-in-class fully human monoclonal immunoglobulin G1κ antibody targeting human interleukin-17A. |
First biologic therapy approved in the EU for first-line systemic treatment of moderate to severe plaque psoriasis. |
More effective than placebo, etanercept and ustekinumab at improving both psoriasis symptoms (with high skin clearance) and health-related quality of life in patients with moderate to severe plaque psoriasis. |
More effective than placebo at improving psoriasis symptoms in patients with palmoplantar or nail psoriasis. |
Generally well tolerated with low immunogenicity; the most common adverse event was nasopharyngitis. |
1 Introduction
Plaque psoriasis, a chronic inflammatory disease, affects 1–3 % of the general population and is often associated with comorbidities (e.g. psoriatic arthritis, inflammatory bowel disease, and cardio-metabolic disorders) [1]. While conventional immunosuppressant drugs are available for use as systemic therapies, these often have tolerability issues [2]. Targeted biologic therapies (which are generally better tolerated and can be taken for longer periods) have thus become available [2]. These include tumor necrosis factor (TNF) inhibitors (e.g. etanercept) and other anti-cytokine agents [e.g. ustekinumab, an anti-interleukin (IL)-12/IL-23 agent] [2].
Patient satisfaction with their psoriasis treatment is typically low, with only 25 % of patients with psoriasis indicating complete satisfaction and 50 and 20 % indicating moderate or slight satisfaction; this often leads to poor compliance [3]. Moreover, the available biologic therapies are not without issues; for example, anti-TNF therapy has several contraindications [such as congestive heart failure (NYHA grade III or IV) or demyelinating diseases [3]]. Thus, drugs are being developed which target other components of the immune system, and there is always a need for higher specificity, greater long-term efficacy, and greater tolerability [2].
IL-17A is an important cytokine in the pathogenesis of psoriasis, and several drugs are either available or in development that target IL-17 and its pathway [2]. Psoriatic plaques contain elevated levels of IL-17A [4, 5]. The IL-17 receptor (expressed on various cell types, including keratinocytes) is also upregulated in psoriatic lesional skin; interaction between IL-17A and the IL-17 receptor leads to the release of proinflammatory cytokines and chemokines and mediators of tissue damage [4–6].
Secukinumab (Cosentyx™), a fully human monoclonal immunoglobulin (Ig)G1κ antibody, is a human IL-17A antagonist [4, 6]. Of the three key cytokine targets in psoriasis (IL-17A, IL-23 and TNFα), IL-17A is the target that acts most proximally to the keratinocyte, and may thus be associated with a lower potential for broad immune suppression than biologic therapies targeting the other two cytokines [5]. This article reviews the pharmacologic properties of secukinumab and its clinical efficacy and tolerability in adult patients with moderate to severe plaque psoriasis.
2 Pharmacodynamic Properties of Secukinumab
Secukinumab is a fully human IgG1κ monoclonal antibody [4, 6]. It selectively binds to IL-17A, inhibiting its interaction with the IL-17 receptor, thus inhibiting its downstream effects on keratinocytes [4, 6]. Upon treatment, clinically relevant levels of secukinumab reach the skin, reducing local inflammatory markers and reducing erythema, induration and desquamation [4].
Following secukinumab treatment in patients with plaque psoriasis, serum levels of total IL-17A (which includes both free and secukinumab-bound IL-17A) were initially increased at weeks 4 and 12 [4, 6], followed by a slow decrease, potentially as a result of reduced clearance of secukinumab-bound IL-17A [4]. This indicates that secukinumab selectively binds to free IL-17A, which plays a key role in plaque psoriasis [4].
Clinical improvements in studies involving patients with plaque psoriasis receiving secukinumab were paralleled by cellular, histologic and molecular changes in psoriatic skin [e.g. reduced epithelial thickness, reduced parakeratosis, decreased keratinocyte proliferation, decreased inflammatory cytokine and chemokine levels, decreased CD3+ T cell levels, and decreases in other innate skin-residing immune cell populations, such as myeloperoxidase-positive (dermal) neutrophils] [4, 6–10]. Responses to global T-cell activation remained unaffected by secukinumab treatment [9].
Secukinumab has been shown to decrease beta-defensin 2 levels in the serum and lesional skin [11], and high-sensitivity C-reactive protein (hsCRP) levels in the serum [12, 13], in patients with moderate to severe plaque psoriasis; both are indicators of inflammation, and high hsCRP levels are indicative of an increased risk of cardiovascular disease. Secukinumab has a neutral lipid profile; it is not associated with changes in total cholesterol, high- or low-density lipoprotein cholesterol, or triglyceride levels in patients with moderate to severe plaque psoriasis [14].
Secukinumab recipients should not receive live vaccines [4, 6]. While non-live vaccinations during secukinumab treatment may not elicit a sufficient immune response to prevent the disease [6], secukinumab recipients may receive these vaccinations [4, 6]. An adequate antibody response to vaccination with meningococcal and influenza vaccines (both non-US-approved formulations [6]) was observed in a similar proportion of healthy volunteers receiving a single secukinumab 150 mg dose (2 weeks before vaccination) to that of healthy volunteers who were not administered secukinumab [4, 6, 15].
3 Pharmacokinetic Properties of Secukinumab
Subcutaneous secukinumab 25–300 mg exhibited dose-proportional pharmacokinetics in patients with psoriasis [4, 6]. The bioavailability of subcutaneous secukinumab 150 or 300 mg was 55–77 %, and the maximum serum concentration was reached by ≈6 days post dose [4, 6]. Steady-state concentrations were reached after 20–24 weeks [4, 6] when the recommended regimen was followed. Secukinumab concentration was a significant predictor of therapeutic response in phase III trials (p < 0.001) [16].
After a single subcutaneous dose of secukinumab 300 mg, the secukinumab concentration in interstitial fluid in lesional and non-lesional skin was 27–40 % of that in serum at 1 and 2 weeks in patients with plaque psoriasis [6]. Secukinumab distribution to peripheral compartments is limited; intravenous secukinumab had a mean volume of distribution of 7.1–8.6 L in patients with plaque psoriasis [4, 6].
Secukinumab elimination occurs via intracellular catabolism following fluid-phase or receptor-mediated endocytosis [4], consistent with it being a human IgG1κ monoclonal antibody [6]. A population pharmacokinetic analysis estimated a mean systemic clearance of 0.19 L/day (range across several studies 0.13–0.36 L/day [4, 6]) and a mean elimination half-life of 27 days (range across studies 18–46 days [4, 6]) in patients with plaque psoriasis [4].
The clearance and volume of distribution of secukinumab increase as bodyweight increases [6].
No drug interaction trials have been conducted with secukinumab [4, 6]. While there has been no report of a role for IL-17A in the expression of cytochrome P450 (CYP) enzymes, certain cytokines have been associated with the suppression of CYP enzyme formation [4, 6].
4 Therapeutic Efficacy of Secukinumab
While data from phase II trials investigating the efficacy of secukinumab in patients with moderate to severe plaque psoriasis are available [17, 18], this section focuses on data from phase III trials.
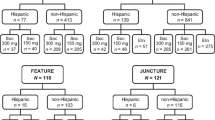
The 12-week efficacy of subcutaneous secukinumab 150 and 300 mg in adult patients with moderate to severe plaque psoriasis (poorly controlled by other treatments) was investigated in four randomized, double-blind, multicenter, placebo-controlled, phase III trials [19–21]; one trial (FIXTURE) also included a subcutaneous etanercept treatment arm [19]. Two of these trials (ERASURE and FIXTURE) used a reconstituted secukinumab powder solution administered by health professionals [19]; the other two used self-administered secukinumab via pre-filled syringe (FEATURE) [20] or autoinjector pen (JUNCTURE) [21]. An additional randomized, double-blind, multicenter, phase IIIb trial (CLEAR) investigated the efficacy of subcutaneous secukinumab 300 mg versus subcutaneous ustekinumab in patients with moderate to severe plaque psoriasis poorly controlled by other treatments [22], and two ongoing randomized, double-blind, placebo-controlled, phase IIIb trials investigated the efficacy of subcutaneous secukinumab 150 or 300 mg versus placebo in patients with moderate to severe palmoplantar psoriasis [palmoplantar Investigator’s Global Assessment (ppIGA) score >3] (GESTURE) [23] or moderate to severe psoriasis with significant nail involvement [fingernail Nail Psoriasis Severity Index (NAPSI) score ≥16 and ≥4 fingernails involved] (TRANSFIGURE) [24].
Secukinumab recipients received weekly injections on weeks 0, 1, 2, 3, and 4, and then once every 4 weeks for a total study period of 52 weeks [19–22]. Etanercept recipients received etanercept 50 mg twice weekly for 12 weeks and then once weekly for a total of 52 weeks [19]. Ustekinumab recipients were treated as per label instructions for a total of 52 weeks [22]. Patients in ERASURE, FIXTURE, FEATURE and JUNCTURE had the option to enter long-term extension studies at completion of the initial study [19–21]. Placebo recipients in ERASURE and FIXTURE who did not show a reduction of 75 % from baseline in Psoriasis Area and Severity Index (PASI) score (PASI 75) by week 12 were re-randomized to treatment with secukinumab 150 or 300 mg for the maintenance period, but are not included in the reported analyses for these treatment arms [19].
The co-primary endpoints for the four phase III trials were the proportion of patients who achieved a PASI 75 response and the proportion of patients who achieved a modified (2011) investigator’s global assessment (IGAmod2011) of 0 or 1 and an improvement of ≥2 from baseline on the IGAmod2011 at 12 weeks [19–21]. The primary endpoint for the phase IIIb CLEAR study was the proportion of patients who achieved a PASI 90 response at 16 weeks [22]. The primary endpoint for the phase IIIb GESTURE study was ppIGA response rate at 16 weeks (response was defined as a ppIGA score of 0 or 1) [23], and for the phase IIIb TRANSFIGURE study was the percentage change from baseline in NAPSI score at 16 weeks [24].
Baseline characteristics did not significantly differ between treatment groups [19–22]. Approximately half to two-thirds of patients had undergone previous systemic treatment [19–22], and, where reported, 15–23 % of patients had psoriatic arthritis [19, 21, 22].
4.1 Shorter-Term Treatment
Subcutaneous secukinumab 150 or 300 mg for 12 or 16 weeks was more effective than placebo, subcutaneous etanercept, or subcutaneous ustekinumab in patients with moderate to severe plaque psoriasis [19–22]. After 12 weeks’ treatment, the proportions of secukinumab 150 and 300 mg recipients with a PASI 75 response and with an IGAmod2011 response (co-primary endpoints [19–21]) were both significantly greater than that of placebo [19–21] and etanercept [19] recipients (all p < 0.001; Table 1).
After 16 weeks’ treatment, the proportion of secukinumab 300 mg recipients with a PASI 90 response (primary endpoint) was significantly greater than that of ustekinumab recipients (p < 0.0001; Fig. 1) [22].
Efficacy of subcutaneous secukinumab 300 mg versus subcutaneous ustekinumab (dosage as per label) in patients with moderate to severe plaque psoriasis [22]. Proportion of patients exhibiting a PASI 90 (primary endpoint) or PASI 100 response (a reduction of ≥90 or ≥100 % from baseline PASI score, respectively) at 16 weeks. PASI Psoriasis Area and Severity Index. *p < 0.0001 versus ustekinumab
Moreover, at 12 weeks, significantly greater proportions of secukinumab 150 and 300 mg recipients had a PASI 90 response than placebo [19–21] and etanercept [19] recipients (Table 1). Secukinumab 300 mg was significantly more effective than placebo with respect to PASI 100 response in all three studies analyzing this outcome, while secukinumab 150 mg was only significantly better in two of the three studies (Table 1) [19–21]. Secukinumab 300 mg was associated with a significantly greater PASI 100 response rate than ustekinumab at 16 weeks (Fig. 1), as well as significantly greater PASI 75 (93.1 vs. 82.7 %; p = 0.0001) and IGAmod2011 (82.9 vs. 67.5 %; p < 0.0001) response rates [22].
Secukinumab treatment was associated with a significantly faster response than etanercept [19]. In FIXTURE, the median time to a 50 % reduction from baseline in mean PASI score was 3.9 and 3.0 weeks for secukinumab 150 and 300 mg versus 7.0 weeks for etanercept (both p < 0.001) [19]. In FEATURE and JUNCTURE, a 50 % reduction from baseline in mean PASI score was achieved by week 3 in secukinumab 300 mg recipients and by week 4 in secukinumab 150 mg recipients [20, 21].
In the CLEAR study, a PASI 75 response was achieved at week 4 by 50.0 % of secukinumab and 20.6 % of ustekinumab recipients (p < 0.0001) [22].
Subgroup analyses of data from ERASURE [25, 26] and FIXTURE [27] indicate that secukinumab was effective regardless of exposure to (or response to) previous biologic therapy [25] or presence of comorbid psoriatic arthritis [26, 27].
Secukinumab was significantly more effective than placebo (p < 0.001) [19], etanercept (p < 0.05) [19] and ustekinumab (p < 0.05) [22] with regard to change from baseline in itching, pain, and scaling scores.
Secukinumab had a positive effect on health-related quality of life (HR-QOL) [19, 22]. While baseline Dermatology Life Quality Index (DLQI) scores were approximately equal across treatment groups in FIXTURE and ERASURE (range 12.0–13.9), the proportions of patients at week 12 with a DLQI score of 0 or 1 (indicating no impact of the disease on their quality of life) were significantly (p < 0.001) higher with secukinumab 150 and 300 mg than with placebo in ERASURE (46.1 and 58.8 vs. 10.3 %), and etanercept and placebo in FIXTURE (50.6 and 56.7 vs. 34.5 and 6.6 %, respectively) [19]. Moreover, the proportions of patients at week 16 with a DLQI score of 0 or 1 in the CLEAR study were significantly higher with secukinumab than with ustekinumab (71.9 vs. 57.4 %; p < 0.0001) [22].
In the studies where patients self-administered secukinumab, the usability of the pre-filled syringe [20] and that of the autoinjector pen [21] were both rated as high.
4.1.1 In Palmoplantar and Nail Psoriasis
Secukinumab 150 and 300 mg were both significantly more effective than placebo in patients with palmoplantar [23] or nail psoriasis [24].
In patients with palmoplantar psoriasis in the GESTURE study (n = 205), a ppIGA 0 or 1 response was achieved at week 16 (primary endpoint) by 22.1 and 33.3 versus 1.5 %, respectively (p < 0.001) [23]. The change from baseline in palmoplantar Psoriasis Area and Severity Index (ppPASI) score was −35.3 and −54.6 versus −4.1 %, respectively (p < 0.001) [23].
In patients with nail psoriasis in the TRANSFIGURE study (n = 198), the change from baseline in NAPSI score at week 16 (primary endpoint) was −37.9 and −45.3 versus −10.8 % (p < 0.0001) in secukinumab 150 and 300 mg versus placebo recipients [24]. PASI 75 response rates (77.0 and 87.1 vs. 5.1 %; p < 0.0001), PASI 90 response rates (54.0 and 72.5 vs. 1.7 %; p-value not reported) and IGAmod2011 response rates (68.3 and 74.0 vs. 3.1 %; p < 0.0001) were also significantly higher in secukinumab recipients [24].
4.2 Longer-Term Treatment
In the maintenance period of ERASURE and FIXTURE, response rates (PASI 75 and IGAmod2011) increased to week 16, then stabilized [19]. Of the patients in ERASURE and FIXTURE who showed an initial response after 12 weeks, most maintained that response to week 52. The rates of maintenance of PASI 75 response were 72.4 and 80.5 % of secukinumab 150 and 300 mg recipients in ERASURE and 82.2 and 84.3 versus 72.5 % of secukinumab 150 and 300 mg versus etanercept recipients (p < 0.01 and 0.001, respectively) in FIXTURE. Corresponding IGAmod2011 response maintenance rates were 59.2 and 74.4 % in ERASURE and 67.7 and 79.7 versus 56.8 % (p < 0.01 and 0.001, respectively) in FIXTURE.
HR-QOL responses were sustained throughout the 52-week maintenance period of ERASURE and FIXTURE [19]. At week 52, the proportions of patients with a DLQI score of 0 or 1 were 48.6 and 66.3 % of secukinumab 150 and 300 mg recipients in ERASURE and 56.2 and 69.7 versus 46.9 % of secukinumab 150 and 300 mg versus etanercept recipients in FIXTURE.
Secukinumab 150 or 300 mg recipients in ERASURE and FIXTURE who were PASI 75 responders at week 52 were re-randomized to continue treatment with the same dosage of secukinumab or to switch to placebo, for continued treatment or until relapse [28]. A total of 73 and 87 % of secukinumab 150 and 300 mg recipients reached week 104 without relapsing, compared with 13 and 16 % of patients who had switched from secukinumab 150 and 300 mg, respectively, to placebo. Of those who relapsed in the secukinumab 300 mg to placebo switch group, 70 % had achieved a PASI 90 response 12 weeks after re-treatment [28].
The long-term maintenance dosing regimen was further assessed in another long-term trial (SCULPTURE), where fixed-interval dosing was found to be more effective in maintaining disease control than the retreatment-as-needed regimen [29]. A total of 966 patients with moderate to severe plaque psoriasis were randomized to secukinumab 150 or 300 mg, once weekly for 4 weeks and then a single dose at week 8; at week 12, PASI 75 responders were further randomized to continue secukinumab at the same dose either every 4 weeks (starting week 12) or as needed (retreatment upon start of relapse) for a total of 52 weeks. The noninferiority of as-needed treatment to the fixed-interval regimen (primary endpoint) was not established at either dosage. The PASI 75 response maintenance rate at week 52 in recipients of secukinumab 150 mg was 52.4 % (retreatment-as-needed) versus 62.1 % (fixed-interval) and in recipients of secukinumab 300 mg was 67.7 versus 78.2 %.
Partial responders to secukinumab treatment may achieve an improved response with continued treatment [30]. Partial responders (PASI 50 but not PASI 75 response) at 12 weeks in the SCULPTURE study (n = 43) were enrolled in the STATURE trial, where they were randomized to treatment with subcutaneous secukinumab 300 mg (weeks 0 and 4) or intravenous secukinumab 10 mg/kg (weeks 0, 2 and 4). The trial’s primary objective was not met, as significance was not achieved in both coprimary endpoints. After 8 weeks, a PASI 75 response was observed in 66.7 versus 90.5 % of subcutaneous versus intravenous recipients, respectively (co-primary endpoint; not significant), and an IGAmod2011 response was observed in 33.3 versus 66.7 % of patients, respectively (co-primary endpoint; p = 0.0332).
5 Tolerability of Secukinumab
Secukinumab is generally well tolerated in patients with moderate to severe plaque psoriasis [4, 6, 19–22, 29]. Adverse events occurred in 57.6–63.9 % of secukinumab 150 mg [19–21], 50.8–70.0 % of secukinumab 300 mg [19–22], 47.0–54.1 % of placebo [19–21], 57.6 % of etanercept [19] and 58.3 % of ustekinumab [22] recipients during the initial, 12- [19–21] or 16-week [22] period of phase III or IIIb trials. The most common adverse events with secukinumab were upper respiratory tract infections (most often nasopharyngitis) (Fig. 2) [4, 6]. Most adverse events were of mild to moderate severity [4].
Twelve-week tolerability of subcutaneous secukinumab 150 and 300 mg in patients with moderate to severe plaque psoriasis [6]. Adverse events occurring in ≥1 % of patients and more frequently with secukinumab than placebo in a pooled analysis of four phase III trials. PL placebo, SEC secukinumab, URTI upper respiratory tract infection not otherwise specified
Over the entire study period (52 weeks) in ERASURE and FIXTURE, the rates of adverse events were 236.4–269.5 and 245.5–252.0 per 100 patient-years with secukinumab 150 and 300 mg versus 323.0–329.7 per 100 patient-years with placebo and 243.4 per 100 patient-years with etanercept [19]. No new or unexpected tolerability findings occurred during the 1-year extension (total 2 years’ treatment) of the ERASURE and FIXTURE trials [28].
Where reported, no treatment-related deaths occurred during the treatment periods of the studies [19–22, 29]. Non-fatal serious adverse events occurred in 0–5 % of secukinumab 150 or 300 mg recipients [19–22], 2 % of placebo recipients [19–21], 1 % of etanercept recipients [19] and 3 % of ustekinumab recipients [22]. The rates of serious adverse events over 52 weeks’ treatment were 6.0–6.8, 7.4–8.3 and 7.0 per 100 patient-years in secukinumab, placebo and etanercept recipients, respectively [19].
A total of 0–2 % of secukinumab 150 or 300 mg [19, 21, 22] versus 1–2 % of placebo recipients [19, 21], 2 % of etanercept recipients [19] and 1 % of ustekinumab recipients [22] discontinued treatment as a result of adverse events during the initial 12- [19, 21] or 16-week [22] study period. During the following 40 weeks in the maintenance period of ERASURE and FIXTURE, 1–5 % of secukinumab 150 or 300 mg and 2 % of etanercept recipients discontinued as a result of adverse events [19].
In a pooled analysis of 10 phase II and III trials, infection rates in secukinumab 150 and 300 mg versus placebo recipients were 26.9 and 25.8 versus 20.6 %, respectively, during the initial 12-week period (n = 1174, 1173 and 793) and 85.3 and 91.1 versus 101.9 per 100 patient-years during the entire treatment period (52 weeks) [n = 1395, 1410, and 793] [31]. Corresponding rates for etanercept in FIXTURE were 25.7 % (n = 323) and 93.7 per 100 patient-years (n = 323). Serious infections were rare in all groups (0–0.3 % at 12 weeks and 0.99–1.37 per 100 patient-years over 52 weeks, respectively). No serious opportunistic infections, reactivation of latent tuberculosis or viral hepatitis infection, or disseminated or CNS herpes infection occurred [31]. However, secukinumab should not be given to patients with active tuberculosis [4, 6].
The incidence of some infection types may be dosage-dependent [6]. Consistent with the assumed role of IL-17A in immune response against Candida mucocutaneous infections, the incidence of these infections was higher in secukinumab 300 mg recipients than in secukinumab 150 mg, placebo and etanercept recipients (3.55 vs. 1.85, 1.00 and 1.37 per 100 patient-years, respectively) [31]. All Candida-related adverse events in secukinumab recipients were mild to moderate (non-serious), were self-resolving or responded to standard antifungal therapy, and did not lead to drug discontinuation; two etanercept recipients had severe Candida-related adverse events [31].
Neutropenia was more common with secukinumab than placebo in clinical trials; however most cases were transient, mild, reversible, and not temporally associated with infections, and no serious cases were reported [4, 6, 32]. The incidence of newly occurring or worsening grades 1, 2, 3, and 4 neutropenia in 2877 secukinumab (either dosage) recipients was 6.5, 1.5, 0.2 and 0 %, in 793 placebo recipients was 2.3, 0.3, 0.1 and 0 %, and in 323 etanercept recipients was 9.4, 3.2, 0, and 0.3 %, after 12 weeks in a pooled analysis of ten phase II and III trials [32]. After 52 weeks, the corresponding incidences were 10.1, 2.5, 0.5 and 0 % (n = 3430), 2.6, 0.3, 0.1 and 0 % (n = 793), and 17.1, 6.0, 0, and 0.3 % (n = 323) [32].
Some cases of anaphylaxis and urticaria were observed in secukinumab recipients in clinical trials [4, 6]. Pooled analyses indicate that there is no increased risk for malignancies [33] or major adverse cardiovascular events [34] with secukinumab treatment.
Some cases of exacerbation of Crohn’s disease (in some cases serious) were observed in secukinumab and placebo recipients in clinical trials [4, 6]. The incidence of Crohn’s disease and ulcerative colitis during the 52-week treatment period was 0.11 and 0.15 per 100 patient-years, respectively, in secukinumab recipients (n = 3430) in 10 phase II and III trials; differences between secukinumab recipients and those receiving placebo or etanercept were not considered to be clinically meaningful [35].
Of 2842 patients treated with secukinumab for up to 52 weeks, 0.4 % developed anti-secukinumab antibodies, of which less than half were neutralizing [36]. Neutralizing antibodies were not associated with a loss of efficacy or with pharmacokinetic abnormalities.
6 Dosage and Administration
Subcutaneous secukinumab is indicated for the treatment of adults with moderate to severe plaque psoriasis who are candidates for systemic therapy (in the US [6] and EU [4]) or phototherapy (in the US [6]). Three secukinumab presentations exist: lyophilized powder for reconstitution, pre-filled syringe and autoinjector pen [4, 6].
The recommended dosage is secukinumab 300 mg administered subcutaneously at weeks 0, 1, 2, 3, and 4, followed by 300 mg every 4 weeks [4, 6]. A dosage of 150 mg (administered at the same frequency as above) may be acceptable for some patients [6]. If no response occurs by 16 weeks of treatment, secukinumab discontinuation should be considered; however, patients with an initial partial response may improve with subsequent treatment beyond 16 weeks [4].
Local prescribing information should be consulted for further, detailed information, including contraindications, precautions, drug interactions, and use in special patient populations.
7 Current Status of Secukinumab in Moderate to Severe Plaque Psoriasis
US guidelines published before the approval of secukinumab list several systemic treatments that can be used as first-line therapy for plaque psoriasis, including oral drugs (e.g. methotrexate sodium) and biologic treatment (e.g. etanercept or ustekinumab) [37]. However, European guidelines published before secukinumab approval recommend that systemic biologic treatment should only be used if conventional systemic therapy or phototherapy was not effective [3]. Secukinumab, as well as being first in its class of anti-IL-17 drugs [7], is thus the first biologic treatment in the EU to be approved for first-line systemic treatment of moderate to severe plaque psoriasis.
In clinical trials, subcutaneous secukinumab was more effective than placebo, etanercept and ustekinumab at improving both psoriasis symptoms (with high skin clearance) and HR-QOL (Sect. 4). Moreover, secukinumab was more effective than placebo in studies specifically investigating efficacy in the difficult-to-treat palmoplantar and nail psoriasis populations. Studies specifically investigating drug efficacy in these populations are rare, and treatment options for these patients are limited [38]. Secukinumab was generally well tolerated, with low immunogenicity (Sect. 5). Longer-term, efficacy was sustained and secukinumab remained well tolerated. Secukinumab has also shown promising results for the treatment of psoriatic arthritis and ankylosing spondylitis [39]; however, it is not currently approved for these indications.
In conclusion, subcutaneous secukinumab is an effective and generally well tolerated first-line systemic treatment for moderate to severe plaque psoriasis, and is a useful addition to the treatment options for this disease.
Data selection sources:
Relevant medical literature (including published and unpublished data) on secukinumab was identified by searching databases including MEDLINE (from 1946) and EMBASE (from 1996) (searches last updated 26 June 2015), bibliographies from published literature, clinical trial registries/databases and websites. Additional information was also requested from the company developing the drug.
Search terms: Secukinumab, AIN-457, KB-03303A, Cosentyx, psoriasis.
Study selection: Studies in patients with psoriasis who received secukinumab. When available, large, well designed, comparative trials with appropriate statistical methodology were preferred. Relevant pharmacodynamic and pharmacokinetic data are also included.
References
Gisondi P, Dalle Vedove C, Girolomoni G. Efficacy and safety of secukinumab in chronic plaque psoriasis and psoriatic arthritis therapy. Dermatol Ther. 2014;4(1):1–9.
Adami S, Cavani A, Rossi F, et al. The role of interleukin-17A in psoriatic disease. BioDrugs. 2014;28(6):487–97.
Pathirana D, Ormerod AD, Saiag P, et al. European S3-guidelines on the systemic treatment of psoriasis vulgaris. J Eur Acad Dermatol Venereol. 2009;23(Suppl. 2):1–70.
Novartis Europharm Limited. Cosentyx™ (secukinumab subcutaneous injection): EU summary of product characteristics. 2015. http://www.ema.europa.eu. Accessed 18 Jun 2015.
Lynde CW, Poulin Y, Vender R, et al. Interleukin 17A: toward a new understanding of psoriasis pathogenesis. J Am Acad Dermatol. 2014;71(1):141–50.
Novartis Pharmaceuticals Corporation. Cosentyx™ (secukinumab subcutaneous injection): US prescribing information. 2015. http://www.pharma.us.novartis.com. Accessed 18 Jun 2015.
Novartis Pharmaceuticals Corporation. Advisory Committee briefing materials: secukinumab. 2014. www.fda.gov. Accessed 18 Jun 2015.
Kolbinger F, Bruin G, Valentin MA, et al. Secukinumab treatment rapidly leads to positive proteomic and transcriptional changes in psoriatic skin [abstract no. P1656]. In: 23rd congress of the European Academy of Dermatology and Venereology. 2014.
Krueger J, Wharton K, Fuentes-Duculan J, et al. Secukinumab reverses disease-defining psoriasis histopathology while retaining full T-cell activation potential [abstract no. P43]. Br J Dermatol. 2014;171:e140.
Reich K, Papp KA, Matheson RT, et al. Evidence that a neutrophil-keratinocyte crosstalk is an early target of IL-17A inhibition in psoriasis. Exp Dermatol. 2015. doi:10.1111/exd.12710.
Bruin G, Dragatin C, Aigner B, et al. Secukinumab, a novel anti-IL-17A antibody, can be quantified in skin after a single dose by dermal open flow microperfusion (dOFM) [abstract]. J Dtsch Dermatol Ges. 2014;12(Suppl 1):15.
Gottlieb A, Sigurgeirsson B, Blauvelt A, et al. Secukinumab reduces hsCRP levels in subjects with moderate-to-severe plaque psoriasis and concomitant psoriatic arthritis: a sub-analysis from the phase 3 ERASURE study [abstract no. AB0738]. Ann Rheum Dis. 2014;73(Suppl 2):1047.
Strober B, Guettner A, Sigurgeirrson B, et al. Secukinumab reduces C-reactive protein levels in patients with moderate to severe plaque psoriasis: result of a regimen-finding study [abstract no. P6395]. J Am Acad Dermatol. 2013;68(4 Suppl 1):AB212.
Mrowietz U, Qureshi A, Escrig C. Secukinumab treatment shows a neutral effect on the lipid profile of patients with moderate to severe plaque psoriasis: results from a randomized, double-blind, placebo-controlled, phase II study [abstract no. P6871]. J Am Acad Dermatol. 2013;68(4 Suppl 1):AB212.
Chioato A, Noseda E, Stevens M, et al. Treatment with the interleukin-17A-blocking antibody secukinumab does not interfere with the efficacy of influenza and meningococcal vaccinations in healthy subjects: results of an open-label, parallel-group, randomized single-center study. Clin Vaccine Immunol. 2012;19(10):1597–602.
US FDA. Dermatologic and Ophthalmic Drugs Advisory Committee Meeting background package for BLA 125504 Cosentyx (secukinumab). 2014. http://www.fda.gov. Accessed 18 Jun 2015.
Rich P, Sigurgeirsson B, Thaci D, et al. Secukinumab induction and maintenance therapy in moderate-to-severe plaque psoriasis: a randomized, double-blind, placebo-controlled, phase II regimen-finding study. Br J Dermatol. 2013;168(2):402–11.
Papp KA, Langley RG, Sigurgeirsson B, et al. Efficacy and safety of secukinumab in the treatment of moderate-to-severe plaque psoriasis: a randomized, double-blind, placebo-controlled phase II dose-ranging study. Br J Dermatol. 2013;168(2):412–21.
Langley RG, Elewski BE, Lebwohl M, et al. Secukinumab in plaque psoriasis—results of two phase 3 trials. N Engl J Med. 2014;371(4):326–38.
Blauvelt A, Prinz JC, Gottlieb AB, et al. Secukinumab administration by pre-filled syringe: efficacy, safety and usability results from a randomized controlled trial in psoriasis (FEATURE). Br J Dermatol. 2014;172(2):484–93.
Paul C, Lacour JP, Tedremets L, et al. Efficacy, safety and usability of secukinumab administration by autoinjector/pen in psoriasis: a randomized, controlled trial (JUNCTURE). J Eur Acad Dermatol Venereol. 2014;29(6):1082–90.
Thaci D, Blauvelt A, Reich K, et al. Secukinumab is superior to ustekinumab in clearing skin of subjects with moderate to severe plaque psoriasis: CLEAR, a randomized controlled trial. J Am Acad Dermatol. 2015. doi:10.1016/j.jaad.2015.05.013.
Gottlieb A, Sullivan J, van Doorn M, et al. Secukinumab efficacy and safety in subjects with moderate to severe palmoplantar psoriasis in a phase 3b study (GESTURE) [abstract no. FC24-07]. In: 23rd World Congress of Dermatology. 2015.
Reich K, Sullivan J, Arenberger P, et al. Secukinumab is effective in subjects with nail psoriasis: 16 week results from the TRANSFIGURE study [abstract]. In: 23rd World Congress of Dermatology. 2015.
Papp K, Karpov A, Papavassilis C, et al. Secukinumab efficacy in relationship with response to previous biologic psoriasis therapy: a subanalysis from the ERASURE Study [abstract no. P8011]. J Am Acad Dermatol. 2014;70(5 Suppl 1):AB186.
Blauvelt A, Gottlieb A, Sigurgeirsson B, et al. Secukinumab efficacy in subjects with moderate-to-severe plaque psoriasis and concomitant psoriatic arthritis: a subanalysis of the ERASURE study [abstract no. P8033]. J Am Acad Dermatol. 2014;70(5 Suppl 1):AB2.
Philipp S, Papavassilis C, Notter M, et al. Secukinumab effect on functional ability in subjects with moderate to severe plaque psoriasis and psoriatic arthritis: a subanalysis from the FIXTURE study [abstract no. P8098]. J Am Acad Dermatol. 2014;70:AB185.
Blauvelt A, Szepietowski J, Sigurgeirrson B, et al. Secukinumab treatment maintains efficacy in moderate to severe plaque psoriasis through second year of treatment: a randomized extension of the ERASURE and FIXTURE studies [abstract]. In: 73rd annual meeting of the American Academy of Dermatology. 2015.
Mrowietz U, Leonardi CL, Girolomoni G, et al. Secukinumab retreatment-as-needed versus fixed-interval maintenance regimen for moderate to severe plaque psoriasis: A randomized, double-blind, noninferiority trial (SCULPTURE). J Am Acad Dermatol. 2015;73(1):27–36 e1.
Thaci D, Humeniuk J, Frambach Y, et al. Secukinumab in psoriasis: randomized, controlled phase 3 trial results assessing the potential to improve treatment response in partial responders (STATURE). Br J Dermatol. 2015. doi:10.1111/bjd.13814.
Tsai T, Blauvelt A, Karpov A, et al. Evaluation of infections with secukinumab in a pooled analysis of 10 clinical studies of moderate-to-severe plaque psoriasis [abstract no. 193]. J Invest Dermatol. 2014;134:S33.
Griffiths C, Guettner A, Prinz J, et al. Secukinumab safety in subjects with moderate to severe plaque psoriasis: a pooled analysis of neutropenia from 10 clinical studies [abstract no. P8266]. J Am Acad Dermatol. 2014;70(5 Suppl 1):AB188.
Van De Kerkhof P, Strober B, Karpov A, et al. Evaluation of malignancy risk with secukinumab treatment in a pooled analysis of 10 clinical studies of moderate-to-severe plaque psoriasis up to 52 weeks [abstract no. 194]. J Invest Dermatol. 2014;134:S33.
Craig L, Nehal M, Mark L, et al. Incidence of major adverse cardiovascular events with secukinumab: a pooled analysis of data from 10 phase 2 and 3 clinical trials in psoriasis [abstract no. T.106]. In: Federation of Clinical Immunology Societies Annual Meeting. 2014.
Ward N, Guettner A, Sands B, et al. Secukinumab safety and tolerability in subjects with moderate to severe plaque psoriasis: a pooled subgroup analysis of 10 clinical studies evaluating exacerbation of Crohn’s disease [abstract no. P8233]. J Am Acad Dermatol. 2014;70(5 Suppl 1):AB188.
Reich K, Blauvelt A, Armstrong A, et al. Secukinumab, a novel Anti-IL-17A antibody, exhibits low immunogenicity in clinical trials and human in vitro assays [abstract no. 1320]. In: 73rd annual meeting of the American Academy of Dermatology. 2015.
Hsu S, Papp KA, Lebwohl MG, et al. Consensus guidelines for the management of plaque psoriasis. Arch Dermatol. 2012;148(1):95–102.
Handa S. Newer trends in the management of psoriasis at difficult to treat locations: scalp, palmoplantar disease and nails. Indian J Dermatol Venereol Leprol. 2010;76(6):634–44.
Sanford M, McKeage K. Secukinumab: first global approval. Drugs. 2015;75(3):329–38.
Disclosure
The preparation of this review was not supported by any external funding. Karly P. Garnock-Jones is a salaried employee of Adis/Springer. During the peer review process, the manufacturer of the agent under review was offered an opportunity to comment on this article. Changes resulting from comments received were made by the author on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Additional information
The manuscript was reviewed by: S. Chimenti, Department of Dermatology, University of Rome, Rome, Italy; C. Leonardi, Department of Dermatology, Saint Louis University School of Medicine, St. Louis, MO, USA; A. Ormerod, Department of Dermatology, University of Aberdeen, Aberdeen, Scotland; F. Rossi, Department of Experimental Medicine, Second University of Naples, Naples, Italy.
Rights and permissions
About this article
Cite this article
Garnock-Jones, K.P. Secukinumab: A Review in Moderate to Severe Plaque Psoriasis. Am J Clin Dermatol 16, 323–330 (2015). https://doi.org/10.1007/s40257-015-0143-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-015-0143-7