Abstract
Amiodarone is an effective antiarrhythmic medication frequently used in practice for both ventricular and atrial arrhythmias. Though classified as a class III antiarrhythmic, it affects all phases of the cardiac action potential. However, the drug has several side effects, including thyroid abnormalities, pulmonary fibrosis, and transaminitis, for which routine monitoring is recommended. It also interacts with several medications, such as warfarin, simvastatin, and atorvastatin, and many HIV antiretroviral medications. Given the common use of this medication in medical practice, it is vital that clinicians understand the indications, contraindications, dosing, side effects, and interactions of this medication. A thorough understanding of these topics is essential for clinicians to ensure safe and effective use of amiodarone.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Though classified as a class III antiarrhythmic, amiodarone affects all phases of the cardiac action potential. |
Amiodarone has several side effects, including thyroid abnormalities, pulmonary fibrosis, and transaminitis, for which routine monitoring is recommended. |
Amiodarone interacts with several commonly used medications, such as warfarin, simvastatin, and atorvastatin, and many HIV antiretroviral medications. |
1 Introduction
Amiodarone is a class III antiarrhythmic medication that is commonly used for the treatment of atrial arrhythmias and ventricular arrhythmias (VAs) [1]. It is an effective antiarrhythmic medication, but long-term therapy can result in a wide variety of side effects affecting several organ systems, some of which can be life threatening [2]. Some of these can be avoided with judicious use of this agent, adjustment to an appropriate dose, and monitoring for adverse side effects. The purpose of this article is to provide a comprehensive review of this commonly used medication, the mechanisms of action, appropriate dosing, common medication interactions, and necessary monitoring or surveillance. The management of adverse effects is also discussed.
2 Mechanism of Action
Amiodarone has several mechanisms of action (Fig. 1). The Vaughan Williams classification system imperfectly classifies the medication as a class III antiarrhythmic because of its predominant potassium channel blockade that increases the cardiac action potential duration [3]. Amiodarone inhibits potassium efflux through IKr, or rapid delayed rectifier channel, during phase III of the action potential. The medication also has class I antiarrhythmic properties via inhibition of sodium channels during phase 0 of the cardiac action potential [4, 5]. In addition, it results in noncompetitive β-receptor blockade (class II antiarrhythmic activity) and L-type (slow) calcium channel blockade (class IV antiarrhythmic activity) [4, 5]. During loading, the acute effects of intravenous amiodarone are predominantly sodium-channel, β-receptor, and calcium channel blockade [4, 5]. The class III effect is seen after completion of the loading dose because of increased levels of the active metabolite, desethylamiodarone [4, 5].
The mechanism of action of amiodarone. A depiction of a normal (black) and post-amiodarone (green) action potentials. Amiodarone inhibits sodium (Na), slightly prolonging phase 0 of the action potential. It inhibits L-type calcium channels (ICaL) and inhibits rectifier potassium channels (IKr), prolonging phase 2 and 3 of the action potential, leading to a prolongation of the QTc
3 Pharmacokinetic Properties
Amiodarone has an oral bioavailability of 30–50%, and the rate and extent of amiodarone absorption are increased when taken with food. When taken with a diet rich in fat, the absorption is enhanced by 2.4- to 3.8-fold compared with the fasting state [6, 7]. Therefore, we recommend that amiodarone should be taken with meals. Amiodarone is metabolized in the liver to desethylamiodarone [5]. During loading, it goes through three phases of distribution: (1) central or vascular distribution occurs over approximately 24 h, (2) peripheral or solid organ distribution occurs over the next 7 days, and (3) deep or fat tissue distribution occurs over the subsequent 4 weeks. The full antiarrhythmic effect of amiodarone for VA plateaus after 10 weeks of therapy [5]. The amount of time the medication persists in the body is dependent on the fat content and prior concentration. Amiodarone leaves the body in the reverse order of distribution, which can take several weeks, with a half-life of 50–60 days [8].
The long half-life of amiodarone means that if it is withheld for a short period of time (up to 1 month) during long-term maintenance therapy, replacement therapy is not necessary. After amiodarone is discontinued, it may continue to have an effect for up to 3 months because of the prolonged half-life [8, 9]. Therefore, it is reasonable to withhold amiodarone if severe toxicity is suspected and confirmatory testing is performed; however, clinicians should be aware that it may take months for amiodarone to clear the body.
4 Indications and Data Supporting Use
4.1 Ventricular Arrhythmias
4.1.1 Ventricular Fibrillation, Ventricular Tachycardia, and Cardiac Arrest
The ARREST trial showed that, among patients with out-of-hospital cardiac arrest due to ventricular fibrillation (VF), those receiving amiodarone (n = 246) had a higher rate of survival to admission than those receiving placebo (n = 258) (44 vs. 34%; p = 0.03) [10]. Subsequently, the ALIVE trial showed amiodarone (n = 180) increased survival as compared with lidocaine (n = 167) in out-of-hospital cardiac arrest due to shock-resistant VF (22.8 vs. 12.0%; p = 0.009) [11]. A major limitation of this trial was the small number of participants and the lack of a placebo group. However, more recently, a large randomized, double-blinded study assessed the efficacy of amiodarone (n = 974), lidocaine (n = 993), or placebo (n = 1059) in out-of-hospital cardiac arrest from VF or ventricular tachycardia (VT) that was refractory to shock therapy. While there was no difference in outcomes between the groups in the overall population, amiodarone demonstrated a survival benefit compared with placebo in the witnessed arrest subgroup [12]. Amiodarone remains a commonly used first-line agent for VF (whether refractory to shock therapy or not) and is the only antiarrhythmic medication recommended by the American Heart Association for the Advanced Cardiovascular Life Support algorithm (class IA recommendation) [13]. Though the survival benefits of amiodarone were limited in the more recent study from Kudenchuk et al. [12], we recommend administering intravenous amiodarone to all patients with VF and cardiac arrest given the signals of benefit seen in witnessed arrest cases. Information as to whether the arrest was witnessed may not be immediately available, and amiodarone administration in this situation did not have major signals of harm.
4.1.2 Hemodynamically Tolerated Ventricular Tachycardia
Until recently, only small studies had compared the efficacy of the different antiarrhythmics for acute termination and safety in the setting of hemodynamically tolerated VT [14, 15]. A recent randomized controlled trial in 62 patients demonstrated the superiority of procainamide over amiodarone in both acute termination of VT and safety [16]. Nonetheless, given the familiarity of most physicians with amiodarone, it is still widely used in this clinical setting. Additionally, procainamide cannot be used as a long-term oral medication in the USA. Data on electrical cardioversion for hemodynamically unstable VT are reviewed in Sect. 4.1.1. In patients with hemodynamically stable VT, antiarrhythmics are usually tried first, and cardioversion is performed if there are signs of poor perfusion or new hemodynamic instability [13, 17]. No data have been published on which antiarrhythmics aid electrical cardioversion of hemodynamically stable VT.
4.1.3 Prevention of Recurrent Ventricular Tachycardia and Implantable Cardioverter Defibrillator Shocks
Amiodarone is also the first-line therapy for patients receiving appropriate implantable cardioverter defibrillator (ICD) shocks for VA. In a comparison of β-blockers versus sotalol versus amiodarone plus β-blockers in 412 patients with spontaneous or inducible VAs in patients with ICDs, the latter combination resulted in the lowest risk of appropriate shocks, albeit at a higher risk of drug-related adverse events [18]. No randomized comparison of amiodarone and mexiletine has been undertaken in this clinical setting.
Recently, catheter ablation of VA has also emerged as an important tool in the management of patients receiving ICD shocks. In a comparison of escalation of antiarrhythmic therapy (n = 127) versus catheter ablation (n = 132) in patients with ischemic cardiomyopathy and VA, catheter ablation resulted in a lower rate of recurrent VA and ICD shocks [19]. The drug-escalation protocol consisted of adding amiodarone in naïve patients and increasing the dose in patients receiving lower doses of amiodarone. Interestingly, there was no difference in outcomes for patients who were not receiving amiodarone therapy at baseline. Thus, the benefit of catheter ablation over amiodarone in patients with ischemic cardiomyopathy who are amiodarone naïve or those with nonischemic cardiomyopathy is unclear. This was also demonstrated in the SCD-HeFT trial (n = 2521), in which amiodarone showed no difference when compared with placebo in reducing mortality in symptomatic patients with a left ventricular ejection fraction < 35% [20].
Patients with cardiomyopathy who have met criteria for an ICD but have not had a prior episode of VT gain no added benefit from “prophylactic” amiodarone.
4.2 Atrial Fibrillation
4.2.1 Acute Cardioversion
Patients who are hemodynamically stable but symptomatic from atrial fibrillation (i.e., left ventricular dysfunction, syncope, or palpitations) can receive acute cardioversion with amiodarone as an adjunct to or in place of electrical cardioversion [21]. Though electrical cardioversion has a reported success rate of 70–90%, some patients may not wish to undergo electrical cardioversion, preferring pharmacologic cardioversion [22]. The efficacy of amiodarone alone in acute cardioversion of atrial fibrillation is 35–65% [22]. Amiodarone is also efficacious in maintaining sinus rhythm after electrical cardioversion, though no more so than other antiarrhythmics [23]. However, unlike propafenone or flecainide, amiodarone may be used in older patients who may have concomitant ischemic heart disease.
4.2.2 Recurrent Atrial Fibrillation Prophylaxis
For patients with left ventricular dysfunction and heart failure who are hemodynamically stable, amiodarone is less effective than catheter ablation for cardioversion of atrial fibrillation. An open-label, parallel-group, multicenter, randomized, controlled trial reported that 70% of patients who received catheter ablation (n = 102) versus 34% of patients receiving amiodarone alone (n = 101) did not have recurrence of atrial fibrillation at 2-year follow-up [24]. Notably, patients who were receiving low-dose amiodarone (< 200 mg daily) continued amiodarone for 12 weeks after the ablation procedure, whereas patients receiving amiodarone ≥ 200 mg daily were not included in the trial. Maintenance dosing is initiated at 400 mg every 8–12 h for 1–2 weeks, followed by 200–400 mg once daily [13]. Dosing can be decreased for women and those with lower body weights to prevent significant drug toxicity, including preventing the need for pacemaker insertion [25].
4.2.3 Rhythm Control after Cardioversion
For patients with severe left ventricular dysfunction and heart failure, or those who are hemodynamically unstable, amiodarone may be used to slow a rapid ventricular response [21]. For patients with symptomatic atrial fibrillation who are not candidates for atrial fibrillation catheter ablation, medical management with amiodarone may be considered. A pooled meta-analysis of the AFFIRM and AF-CHF trials (n = 3307) showed freedom from atrial fibrillation was 84% and 45% at 1 and 5 years, respectively [26]. Interestingly, a 2009 meta-analysis (n = 673) showed that amiodarone was more effective than placebo or β-blockers at achieving sinus rhythm (21.3 vs. 9.2 per 100 patient-years in sinus rhythm) and that it did not increase long-term mortality (4.7 vs. 3.9 per 100 patient-years) [27]. Given the possibility of cardioversion to sinus rhythm, amiodarone should be used when cardioversion and the associated risk of thromboembolism would be acceptable or has been minimized by therapeutic anticoagulation for 3 weeks or the patient has been in atrial fibrillation for < 48 h [21].
4.3 Other Supraventricular Tachyarrhythmias
Stable patients with rate-controlled atrial flutter or cardioverted atrioventricular nodal re-entrant tachycardia, atrial tachycardia, or atrioventricular re-entrant tachycardia should be referred for catheter ablation rather than placed on long-term amiodarone because of the high cure rates with catheter ablation [28]. However, amiodarone has been found to be efficacious in critically ill or severely comorbid patients (n = 33) with atrial tachyarrhythmias who are otherwise precluded from catheter ablation candidacy [29].
5 Dosing
5.1 Ventricular Arrhythmias
For patients experiencing VF or hemodynamically unstable VT, a loading is initiated with intravenous or intraosseous amiodarone for faster onset of action than with oral amiodarone (150–300 mg intravenous or intraosseous bolus per American Heart Association guidelines for Advanced Cardiovascular Life Support), followed by a continuous infusion of 1 mg/min for 6 h; then 0.5 mg/min for at least 18 h [13, 21]. For hemodynamically stable patients, the loading for VA is initiated with intravenous amiodarone for better bioavailability: 150 mg intravenous bolus, followed by 1 mg/min for 6 h; followed by 0.5 mg/min for 18 h or until switched to oral therapy (as described above) [13]. No dose adjustment is required for renal impairment. No specific guidelines exist for hepatic impairment; however, given the intermediate first-pass extraction through the liver, treatment may be initiated at a low-normal dose, with low maintenance dosing [30].
Converting patients from intravenous amiodarone to oral amiodarone depends on the period of time for which the patient received the intravenous infusion. If the intravenous infusion was continued for < 1 week, the initial oral dose should be 800–1600 mg per day. If the intravenous infusion was continued for 1–3 weeks, the initial oral dose should be 600–800 mg per day. Finally, if the intravenous infusion was continued for > 3 weeks, then the initial oral dose should be 400 mg daily. Dosing adjustments should be considered in patients with hepatic dysfunction but is not necessary in patients with renal dysfunction. Overlapping intravenous and oral amiodarone does not decrease the rate of early tachyarrhythmia recurrence [31].
5.2 Atrial Arrhythmias
Similar loading strategies and dosages can be used for both atrial arrhythmias and VAs. When amiodarone is used for rhythm control in atrial fibrillation, typical dosing is 200 mg daily, but 100 mg daily could be considered for elderly patients [32].
6 Drug Interactions
6.1 Cardiac Medications
Amiodarone use with class 1a antiarrhythmic medications (quinidine, procainamide, and disopyramide) is contraindicated because of dose-independent QTc prolongation [33]. Amiodarone should also not be used with other Vaughan William class III agents because of the risk of significant QTc prolongation. When prescribed in combination with β-blockers or calcium channel blockers, amiodarone may further increase the risk of bradycardia because of sinus nodal or atrioventricular nodal blockade [34]. Therefore, amiodarone and β-blocker dual therapy should be used cautiously. The combined use of digoxin and amiodarone can increase serum concentrations of digoxin because of inhibition of gastrointestinal p-glycoprotein, putting patients at risk for digoxin toxicity [35,36,37]. Though flecainide and amiodarone are clinically rarely used together, dosing of flecainide should be adjusted when concurrently using amiodarone. Given the hepatic metabolism of flecainide via cytochrome P450 (CYP)-2D6 inhibition, flecainide dosing should be decreased by 50% when used in combination with amiodarone, though one study found that flecainide levels were increased by 30% in patients receiving amiodarone [38]. Because of amiodarone-mediated inhibition of CYP3A4, both simvastatin and atorvastatin concentrations can be increased when used in combination with amiodarone [39]. This interaction could potentiate the risk of myopathy, including rhabdomyolysis. The currently recommended dose of simvastatin is 20 mg if used concomitantly with amiodarone [40]. Pravastatin may be considered in lieu of simvastatin or atorvastatin as its blood concentration has not been shown to be altered by concurrent amiodarone use [39]. Amiodarone potentiates the anticoagulation effect and plasma concentration of warfarin via inhibition of the S-isomer of warfarin (the more potent enantiomer) and CYP2C9 and CYP3A4, requiring closer monitoring of the international normalized ratio [41]. If amiodarone is started while a patient is receiving warfarin, a dose reduction of warfarin by approximately 30–50% is usually required [42].
6.2 Noncardiac Medications
Amiodarone in combination with other QTc-prolonging medications can result in the R-on-T phenomenon and is therefore a risk category X (avoid combination) [43]. Cholestyramine and other bile acid sequestrants can decrease the bioavailability of amiodarone so therapy modification should be considered [44]. Amiodarone can increase the concentration of doxorubicin by inhibiting CYP2D6, CYP3A4, and p-glycoprotein, which requires closer monitoring of these patients [45]. Fosphenytoin, lopinavir/ritonavir, and ivabradine are other medications that can prolong the QTc in combination with amiodarone and should therefore be used with caution [46,47,48]. Both indinavir and ritonavir can increase the concentration of amiodarone and are combination class X [46, 49]. Similarly, amiodarone should also not be combined with ledipasvir/sofosbuvir because of the risk of severe and rare but fatal bradycardia [50].
7 Toxicities/Side Effects
The adverse reactions of amiodarone include both life-threatening effects leading to black box warnings and common side effects (Table 1). Common intolerances include nausea, vomiting, and taste disturbances, which can be minimized by dividing into twice-daily doses [51,52,53]. Serious black box warnings include hepatotoxicity and pulmonary dysfunction.
7.1 Thyroid
Amiodarone can cause mild alterations in thyroid hormones, including decreased serum T2, increased serum T4, and reversed T3 levels, and either normal or slight elevations in thyroid-stimulating hormone, likely because of interference with the iodothyronine deiodinases, which metabolize thyroid hormones [54]. In a large meta-analysis of placebo-controlled trials of amiodarone, the relative risk of thyroid toxic events was about 4.4 [55]. Amiodarone-induced hypothyroidism (AIH) is thought to occur because of the large amount of iodine released from amiodarone, which inhibits thyroid hormone synthesis, termed the Wolff–Chaikoff effect. This is usually a temporary effect until the thyroid “escapes” and usual synthesis of T4 occurs. However, AIH occurs when the body does not “escape” or is more susceptible to the inhibitory effect of iodine on hormonal synthesis. AIH is expected to resolve 2–4 months after drug cessation, which correlates with the half-life of amiodarone. Patients with persistent hypothyroidism usually have underlying autoimmune thyroid disease [54]. Hypothyroidism may develop as rapidly as 2 weeks and as late as 39 months, and complications can be as serious as myxedema coma. On the opposite end of the spectrum, there are two types of amiodarone-induced thyrotoxicosis (AIT): type I (excessive iodine-induced hormone synthesis and release in patients with abnormal thyroid glands) and type II (destructive thyroiditis usually in patients without underlying thyroid disease) [54, 56].
7.2 Lung
Pulmonary toxicity from amiodarone most commonly presents as interstitial lung disease or hypersensitivity syndrome (relative risk 1.77 compared with placebo), although acute respiratory distress syndrome, pulmonary nodules/masses, or pleural effusions have also been reported [55, 57,58,59,60,61]. Pulmonary complications, including fibrosis and hypersensitivity, have been reported in studies as occurring in about 1–2% of patients receiving amiodarone [62, 63]. This pulmonary toxicity is fatal approximately 10% of the time [57]. High-resolution computerized tomography scans of the lungs can be performed at that time to check for evidence of hypersensitivity pneumonitis but is not recommended for routine monitoring [64]. Amiodarone should be used cautiously in patients with preexisting pulmonary disease (e.g., severe asthma, chronic obstructive pulmonary disease) or those requiring oxygen therapy, as they are at higher risk of pulmonary toxicity [57, 65].
7.3 Liver
Hepatotoxicity typically manifests as mild transaminitis in approximately 0.5–1% of cases, but fatal hepatic failure has occurred in a few cases [63, 66]. The relative risk of developing hepatotoxicity compared with placebo is approximately 2.3 according to a recent meta-analysis [55].
7.4 Heart
Significant heart block or sinus bradycardia is seen in 2–5% of patients (relative risk 1.9), along with QTc prolongation, although this is generally not associated with arrhythmias [55, 63].
7.5 Eye
Epithelial keratopathy, or corneal microdeposits, can occur in up to 90% of the cases according to the literature. Light sensitivity and optic neuropathy are less common [67].
7.6 Skin
Phototoxic and photoallergic reactions have been reported in 25–75% of patients, as has hyperpigmentation, affecting 4–9% of patients (overall relative risk 1.99) [55, 68].
7.7 Pregnancy
Amiodarone, listed as a class D drug during pregnancy, is associated with cardiac, endocrine, and neurodevelopmental anomalies and should only be used as a drug of last resort [69]. In breastfeeding mothers, amiodarone should be avoided or breastfeeding should be stopped to decrease the risk of newborn hypothyroidism [69].
8 Monitoring and Treatment of Side Effects
8.1 Thyroid
Thyroid function should be monitored via TSH and free T4 every 6 months [54, 64]. If hypothyroidism occurs, levothyroxine should be administered [56]. Hypothyroidism can persist for 8 months after amiodarone is discontinued [54]. In patients with VT and hypothyroidism as the only toxicity, amiodarone should not be discontinued because amiodarone has increased efficacy compared with many other antiarrhythmics, and levothyroxine is a generally well-tolerated drug. Rather, hypothyroidism should be treated while amiodarone is continued. In patients with atrial fibrillation or other supraventricular tachyarrhythmias, amiodarone should be withheld if the patient is a candidate for other antiarrhythmics such as propafenone, sotalol, dofetilide, or flecainide to prevent polypharmacy.
In the setting of hyperthyroidism due to type I AIT, another agent should be started in lieu of amiodarone, methimazole 40–80 mg daily or propylthiouracil 400–800 mg daily should be initiated, amiodarone should be stopped, and alternative therapy should be initiated. In type II AIT, amiodarone can be continued initially and prednisone 40–60 mg daily should be prescribed [56]. If there is no improvement in thyroid function within 1–2 months, then amiodarone should be withheld and alternative therapy initiated. Frequently, type II AIT subsequently results in hypothyroidism, which can be treated with levothyroxine [56].
Patients who develop thyroid toxicities should be referred to an endocrinologist [64]. Whether hypo- or hyperthyroidism, decisions about continuing or withholding amiodarone require discussion with the patient about the risks and benefits of the treatment options and effects on quality of life and subsequent shared decision making.
8.2 Lung
Baseline testing should include pulmonary function tests (PFTs), including lung diffusing capacity of carbon monoxide (DLCO) and a chest radiograph [70]. PFTs with DLCO can be repeated if there is clinical suspicion for pulmonary toxicity, as serial monitoring has not shown clear benefit [64]. However, it is recommended to repeat chest X-ray films annually [64]. If there is evidence of pulmonary toxicity, then amiodarone should be promptly discontinued and the patient referred to a pulmonologist; initiation of prednisone 40–60 mg daily is recommended [64].
8.3 Liver
Clinicians should order baseline and repeat testing of liver function every 6 months because of the potential for hepatic dysfunction. Screening liver function tests should include aspartate aminotransferase (AST) and alanine aminotransferase (ALT). AST or ALT elevation greater than two times the upper limit of normal should prompt either dose reduction of amiodarone or a change in agent [64].
8.4 Heart
The cardiac system should be monitored for QTc prolongation and bradycardia with an electrocardiogram before starting the medication and annually thereafter [64]. In asymptomatic bradycardia, we recommend maintaining the dose if the heart rate remains above 40 beats per minute (bpm). However, if heart rates drop below 40 bpm, a dose reduction of 50% followed by monitoring for breakthrough tachyarrhythmias and improved sinus heart rate (via 14- or 30-day event monitor) is recommended. If the patient develops symptomatic bradycardia, amiodarone should be decreased by 50% or withheld completely. If intolerable tachyarrhythmias occur, placement of a pacemaker should be considered for patients with supraventricular tachycardias or an ICD considered in patients with VT.
8.5 Eye
A baseline and annual ophthalmologic exam, including slit-lamp evaluation, should be performed to evaluate for corneal deposits and optical nerve neuropathies [64, 67]. Corneal microdeposits rarely impact on vision and therefore do not necessitate a decreased dose or cessation of amiodarone. Prescribers should promptly refer the patient to an ophthalmologist for any changes in visual acuity while patients are receiving amiodarone [64]. We recommend immediate discontinuation of amiodarone if optical nerve neuropathy is diagnosed.
8.6 Skin
The integumentary system should be monitored via annual physical exam. If photosensitivity occurs, the patient should be encouraged to avoid sunlight (particularly immediately after the dose is taken) and use sunscreen [68]. Photosensitivity alone does not necessitate a change in dose or cessation of amiodarone if these precautions are taken.
8.7 Alternatives to Amiodarone
In situations where amiodarone needs to be stopped, or the reduced dose is ineffective, alternative antiarrhythmics should be considered [13]. For VA, mexiletine or sotalol are options [13]. Rarely, quinidine and procainamide can be used, though these have a very high risk of Torsades [13]. For atrial arrhythmias, in the absence of coronary artery disease or heart failure, class 1c agents can be used [21]. Dronedarone can also be used in patients with structurally normal hearts [21]. The next line of agents includes sotalol or dofetilide if renal function is satisfactory and QTc is not prolonged at baseline [21].
9 Need for an Outpatient Monitoring Tool
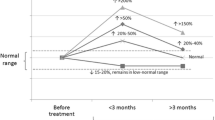
Several studies have demonstrated that adherence to appropriate monitoring of amiodarone is poor [71,72,73]. One proposed solution for improved surveillance while receiving amiodarone is pharmacist-led amiodarone monitoring services, which have been beneficial in increasing screening compliance in retrospective cohort and longitudinal studies [74]. Figure 2 shows the protocol used at Loma Linda University Medical Center as an example.
Sample amiodarone safety monitoring protocol. ALT alanine aminotransferase, AST aspartate aminotransferase, CMP comprehensive metabolic panel, CXR chest X-ray, DLCO lung diffusing capacity of carbon monoxide, ECG electrocardiogram, GI gastrointestinal, INR international normalization ratio, Mg magnesium, PT prothrombin time, SCr serum creatinine, TSH thyroid-stimulating hormone
10 Need for Informed Consent
Given the significant side effects possible with amiodarone, clinicians should explicitly document discussion of all possible side effects. Shared decision making is essential in increasing adherence to medications and prompt recognition of any adverse drug reaction. While formal informed consent is not necessary, it may be considered.
11 Conclusion
Although amiodarone has an important role in the armamentarium of experienced clinicians, it should be used judiciously and only in patients who are likely to receive proper follow-up. The ability to treat life-threatening arrhythmias makes this medication valuable in certain situations. However, the potentially fatal toxicities of long-term use of amiodarone require vigilant monitoring and a low threshold for dose reduction or change in agent whenever appropriate.
References
Williams EMV. A classification of antiarrhythmic actions reassessed after a decade of new drugs. J Clin Pharmacol. 1984;24:129–47.
Haverkamp W, Israel C, Parwani A. Klinische Besonderheiten der Therapie mit Amiodaron. Herzschr Elektrophys. 2017;28:307–16.
Vaughan Williams EM. Classification of antidysrhythmic drugs. Pharmacol Ther B. 1975;1:115–38.
Kodama I, Kamiya K, Toyama J. Cellular electropharmacology of amiodarone. Cardiovasc Res. 1997;35:13–29.
Mitchell LB, Wyse DG, Gillis AM, Duff HJ. Electropharmacology of amiodarone therapy initiation. Time courses of onset of electrophysiologic and antiarrhythmic effects. Circulation. 1989;80:34–42.
Shayeganpour A, Jun AS, Brocks DR. Pharmacokinetics of Amiodarone in hyperlipidemic and simulated high fat-meal rat models. Biopharm Drug Dispos. 2005;26:249–57.
Meng X, Mojaverian P, Doedée M, Lin E, Weinryb I, Chiang ST, et al. Bioavailability of amiodarone tablets administered with and without food in healthy subjects. Am J Cardiol. 2001;87:432–5.
Holt DW, Tucker GT, Jackson PR, Storey GCA. Amiodarone pharmacokinetics. Am Heart J. 1983;106:840–7.
Freedman MD, Somberg JC. Pharmacology and Pharmacokinetics of Amiodarone. J Clin Pharmacol. 1991;31:1061–9.
Kudenchuk PJ, Doherty AM, Murray WA. Amiodarone for resuscitation after out-of-hospital cardiac arrest due to ventricular fibrillation. N Engl J Med. 1999;8.
Dorian P, Cass D, Schwartz B, Cooper R, Gelaznikas R, Barr A. Amiodarone as compared with lidocaine for shock-resistant ventricular fibrillation. N Engl J Med. 2002;346:884–90.
Kudenchuk PJ, Brown SP, Daya M, Rea T, Nichol G, Morrison LJ, et al. Amiodarone, lidocaine, or placebo in out-of-hospital cardiac arrest. N Engl J Med. 2016;374:1711–22.
Al-Khatib Sana M, Stevenson William G, Ackerman Michael J, Bryant William J, Callans David J, Curtis Anne B, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Circulation. 2018;138:e272–391.
Marill KA, deSouza IS, Nishijima DK, Senecal EL, Setnik GS, Stair TO, et al. Amiodarone or procainamide for the termination of sustained stable ventricular tachycardia: an historical multicenter comparison. Acad Emerg Med. 2010;17:297–306.
Tomlinson DR, Cherian P, Betts TR, Bashir Y. Intravenous amiodarone for the pharmacological termination of haemodynamically-tolerated sustained ventricular tachycardia: is bolus dose amiodarone an appropriate first-line treatment? Emerg Med J. 2008;25:15.
Ortiz M, Martín A, Arribas F, Coll-Vinent B, del Arco C, Peinado R, et al. Randomized comparison of intravenous procainamide vs. intravenous amiodarone for the acute treatment of tolerated wide QRS tachycardia: the PROCAMIO study. Eur Heart J. 2016;ehw230.
Panchal Ashish R, Berg Katherine M, Kudenchuk Peter J, Marina Del Rios, Hirsch Karen G, Link Mark S, et al. American Heart Association Focused Update on advanced cardiovascular life support use of antiarrhythmic drugs during and immediately after cardiac arrest: an update to the american heart association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2018;2018(138):e740–9.
Connolly SJ, Dorian P, Roberts RS, Gent M, Bailin S, Fain ES, et al. Comparison of β-blockers, amiodarone plus β-Blockers, or sotalol for prevention of shocks from implantable cardioverter defibrillators: the OPTIC study: a randomized trial. JAMA. 2006;295:165–71.
Sapp JL, Wells GA, Parkash R, Stevenson WG, Blier L, Sarrazin J-F, et al. Ventricular tachycardia ablation versus escalation of antiarrhythmic drugs. N Engl J Med. 2016;375:111–21.
Bardy GH, Boineau R, Johnson G, Davidson-Ray LD, Ip JH. Amiodarone or an implantable cardioverter–defibrillator for congestive heart failure. N Engl J Med. 2005;13.
January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC, et al. AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American college of Cardiology/American heart association task force on clinical practice guidelines and the heart rhythm society in collaboration with the society of thoracic surgeons. Circulation. 2019;2019:140.
Chevalier P, Durand-Dubief A, Burri H, Cucherat M, Kirkorian G, Touboul P. Amiodarone versus placebo and class ic drugs for cardioversion of recent-onset atrial fibrillation: a meta-analysis. J Am Coll Cardiol. 2003;41:255–62.
Gwag HB, Chun KJ, Hwang JK, Park S-J, Kim JS, Park K-M, et al. Which antiarrhythmic drug to choose after electrical cardioversion: A study on non-valvular atrial fibrillation patients. PLoS One [Internet]. 2018 [cited 2020 Jan 30];13. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5963785/.
Di Biase L, Mohanty P, Mohanty S, Santangeli P, Trivedi C, Lakkireddy D, et al. Ablation versus amiodarone for treatment of persistent atrial fibrillation in patients with congestive heart failure and an implanted device. Circulation. 2016;133:1637–44.
Essebag V, Reynolds MR, Hadjis T, Lemery R, Olshansky B, Buxton AE, et al. Sex differences in the relationship between amiodarone use and the need for permanent pacing in patients with atrial fibrillation. Arch Intern Med. 2007;167:1648–53.
Cadrin-Tourigny J, Wyse DG, Roy D, Blondeau L, Levesque S, Talajic M, et al. Efficacy of amiodarone in patients with atrial fibrillation with and without left ventricular dysfunction: a pooled analysis of AFFIRM and AF-CHF trials. J Cardiovasc Electrophysiol. 2014;25:1306–13.
Doyle JF, Ho KM. Benefits and risks of long-term amiodarone therapy for persistent atrial fibrillation: a meta-analysis. Mayo Clin Proc. 2009;84:234–42.
Brugada J, Katritsis DG, Arbelo E, Arribas F, Bax JJ, Blomström-Lundqvist C, et al. 2019 ESC Guidelines for the management of patients with supraventricular tachycardiaThe Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC)Developed in collaboration with the Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J [Internet]. [cited 2020 Jan 30]; Available from: https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehz467/5556821.
Clemo HF, Wood MA, Gilligan DM, Ellenbogen KA. Intravenous amiodarone for acute heart rate control in the critically ill patient with atrial tachyarrhythmias. Am J Cardiol. 1998;81:594–8.
Lewis JH, Stine JG. Review article: prescribing medications in patients with cirrhosis—a practical guide. Aliment Pharmacol Ther. 2013;37:1132–56.
Arnouk S, Aberle C, Altshuler D, Merchan C, Piper GL, Papadopoulos J. Clinical effects of intravenous to oral amiodarone transition strategies in critically ill adult patients. J Clin Pharm Ther. 2019;44:693–700.
Sandler M. Amiodarone dosage in older patients with atrial fibrillation: an open, multi-centre study. Curr Med Res Opin. 1992;13:31–6.
Antonelli D, Atar S, Freedberg NA, Rosenfeld T. Torsade de pointes in patients on chronic amiodarone treatment: contributing factors and drug interactions. Isr Med Assoc J. 2005;7:3.
Hauser TH, Pinto DS, Josephson ME, Zimetbaum P. Safety and feasibility of a clinical pathway for the outpatient initiation of antiarrhythmic medications in patients with atrial fibrillation or atrial flutter. Am J Cardiol. 2003;91:1437–41.
Nademanee K, Kannan R, Hendrickson J, Ookhtens M, Kay I, Singh BN. Amiodarone-digoxin interaction: clinical significance, time course of development, potential pharmacokinetic mechanisms and therapeutic implications. J Am Coll Cardiol. 1984;4:111–6.
Robinson K, Johnston A, Walker S, Mulrow JP, McKenna WJ, Holt DW. The digoxin-amiodarone interaction. Cardiovasc Drug Ther. 1989;3:25–8.
Fenner K, Troutman M, Kempshall S, Cook J, Ware J, Smith D, et al. Drug–drug interactions mediated through P-glycoprotein: clinical relevance and in vitro–in vivo correlation using digoxin as a probe drug. Clin Pharmacol Ther. 2009;85:173–81.
Shea P, Lal R, Kim SS, Schechtman K, Ruffy R. Flecainide and amiodarone interaction. J Am Coll Cardiol. 1986;7:1127–30.
Becquemont L, Neuvonen M, Verstuyft C, Jaillon P, Letierce A, Neuvonen PJ, et al. Amiodarone interacts with simvastatin but not with pravastatin disposition kinetics. Clin Pharmacol Ther. 2007;81:679–84.
Research C for DE and. FDA Drug Safety Communication: Revised dose limitation for Zocor (simvastatin) when taken with amiodarone. FDA [Internet]. 2018 [cited 2019 Jun 7]; Available from: http://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-revised-dose-limitation-zocor-simvastatin-when-taken-amiodarone.
O’Reilly RA, Trager WF, Rettie AE, Goulart DA. Interaction of amiodarone with racemic warfarin and its separated enantiomorphs in humans. Clin Pharmacol Ther. 1987;42:290–4.
Holm J, Lindh JD, Andersson ML, Mannheimer B. The effect of amiodarone on warfarin anticoagulation: a register-based nationwide cohort study involving the Swedish population. J Thromb Haemost. 2017;15:446–53.
Wei A, Peng J, Gu Z, Li J. QTc prolongation and torsades de pointes due to a coadministration of fluoxetine and amiodarone in a patient with implantable cardioverter–defibrillator: case report and review of the literature. Medicine. 2017;96:e9071.
Nitsch J, Lüderitz B. Beschleunigte elimination von amiodaron durch Colestyramin*. Dtsch Med Wochenschr. 1986;111:1241–4.
Chauffert B, Martin M, Hammann A, Michel MF, Martin F. Amiodarone-induced enhancement of doxorubicin and 4′-Deoxydoxorubicin cytotoxicity to rat colon cancer cells in vitro and in vivo. Cancer Res. 1986;46:825–30.
Crouch MA, Limon L, Cassano AT. clinical relevance and management of drug-related QT interval prolongation. Pharmacotherapy. 2003;23:881–908.
Rushworth GF, Lambrakis P, Leslie SJ. Ivabradine: a new rate-limiting therapy for coronary artery disease and heart failure. Ther Adv Drug Saf. 2011;2:19–28.
Nolan PE, Marcus FI, Hoyer GL, Bliss M, Gear K. Pharmacokinetic interaction between intravenous phenytoin and amiodarone in healthy volunteers. Clin Pharmacol Ther. 1989;46:43–9.
Antiretroviral therapy increases serum concentrations of amiodarone. Ann Pharmacother. 1999;33:645–6
Research C for DE and. FDA Drug Safety Communication: FDA warns of serious slowing of the heart rate when antiarrhythmic drug amiodarone is used with hepatitis C treatments containing sofosbuvir (Harvoni) or Sovaldi in combination with another Direct Acting Antiviral drug. FDA [Internet]. 2019 [cited 2019 May 24]; Available from: http://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-warns-serious-slowing-heart-rate-when-antiarrhythmic-drug.
CORDARONE® (amiodarone HCl) Dosage and Administration | Pfizer Medical Information - US [Internet]. [cited 2019 Jun 8]. Available from: https://www.pfizermedicalinformation.com/en-us/cordarone/dosage-admin.
Dosing | NEXTERONE (amiodarone HCl) [Internet]. [cited 2019 Jun 8]. Available from: http://www.nexterone.com/dosing.html.
NEXTERONE (amiodarone HCI) Premixed Injection [Internet]. [cited 2019 Jun 8]. Available from: http://www.nexterone.com/about_nexterone.html.
Trohman RG, Sharma PS, McAninch EA, Bianco AC. Amiodarone and thyroid physiology, pathophysiology, diagnosis and management. Trends Cardiovasc Med. 2019;29:285–95.
Ruzieh M, Moroi MK, Aboujamous NM, Ghahramani M, Naccarelli GV, Mandrola J, et al. Meta-analysis comparing the relative risk of adverse events for amiodarone versus placebo. Am J Cardiol. 2019;124:1889–93.
Basaria S, Cooper DS. Amiodarone and the thyroid. Am J Cardiol. 2005;118:706–14.
Papiris SA, Triantafillidou C, Kolilekas L, Markoulaki D, Manali ED. Amiodarone. Drug Saf. 2010;33:539–58.
Kumar S, Bangalore S, Kumari R, Grosu H, Jean R. Amiodarone-induced acute respiratory distress syndrome masquerading as acute heart failure. J Emerg Med. 2012;43:e311–4.
Azzam I, Tov N, Elias N, Naschitz JE. Amiodarone toxicity presenting as pulmonary mass and peripheral neuropathy: the continuing diagnostic challenge. Postgrad Med J. 2006;82:73–5.
Rodrı́guez-Garcı́a JL, Garcı́a-Nieto JC, Ballesta F, Prieto E, Villanueva MA, Gallardo J. Pulmonary mass and multiple lung nodules mimicking a lung neoplasm as amiodarone-induced pulmonary toxicity. Eur J Intern Med. 2001;12:372–6.
Gonzalez-Rothi RJ, Hannan SE, Hood CI, Franzini DA. Amiodarone pulmonary toxicity presenting as bilateral exudative pleural effusions. Chest. 1987;92:179–82.
Singh SN, Fletcher RD, Fisher SG, Singh BN, Lewis HD, Deedwania PC, et al. Amiodarone in patients with congestive heart failure and asymptomatic ventricular arrhythmia. N Engl J Med. 1995;333:77–82.
Connolly Stuart J. Evidence-based analysis of amiodarone efficacy and safety. Circulation. 1999;100:2025–34.
Goldschlager N, Epstein AE, Naccarelli GV, Olshansky B, Singh B, Collard HR, et al. A practical guide for clinicians who treat patients with amiodarone: 2007. Heart Rhythm. 2007;4:1250–9.
Wolkove N, Baltzan M. Amiodarone pulmonary toxicity. J Thorac Dis. 2009;16:6.
Gayam V, Khalid M, Dahal S, Garlapati P, Gill A, Alex R, et al. Fatal acute liver failure with intravenous amiodarone: a case report and literature review. Gastroenterol Res. 2018;11:62–3.
Passman RS, Bennett CL, Purpura JM, Kapur R, Johnson LN, Raisch DW, et al. Amiodarone-associated optic neuropathy: a critical review. Am J Med. 2012;125:447–53.
Jaworski K, Walecka I, Rudnicka L, Gnatowski M, Kosior DA. Cutaneous adverse reactions of amiodarone. Med Sci Monit. 2014;20:2369–72.
Tan HL, Lie KI. Treatment of tachyarrhythmias during pregnancy and lactation. Eur Heart J. 2001;22:458–64.
Gleadhill IC, Wise RA, Schonfeld SA, Scott PP, Guarnieri T, Levine JH, et al. Serial lung function testing in patients treated with amiodarone: a prospective study. Am J Med. 1989;86:4–10.
Lavon O, Goldman R. Adherence to monitoring guidelines of amiodarone adverse reactions. Health Serv Res Manag Epidemiol. 2019;6:233339281984463.
Bickford CL, Spencer AP. Adherence to the NASPE guideline for amiodarone monitoring at a medical university. JMCP. 2006;12:254–9.
Burgess C, Blaikie A, Ingham T, Robinson G, Narasimhan S. Monitoring the use of amiodarone: compliance with guidelines. Intern Med J. 2006;36:289–93.
Dixon DL, Dunn SP, Kelly MS, McLlarky TR, Brown RE. Effectiveness of pharmacist-led amiodarone monitoring services on improving adherence to amiodarone monitoring recommendations: a systematic review. Pharmacotherapy. 2016;36:230–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the preparation of this manuscript.
Conflicts of interest
David Hamilton Sr., Shuktika Nandkeolyar, Howard Lan, Pooja Desai, Jonathan Evans, Christopher Hauschild, Dimpa Choksi, Islam Abudayyeh, Tahmeed Contractor, and Anthony Hilliard have no potential conflicts of interest that might be relevant to the contents of this manuscript.
Rights and permissions
About this article
Cite this article
Hamilton, D., Nandkeolyar, S., Lan, H. et al. Amiodarone: A Comprehensive Guide for Clinicians. Am J Cardiovasc Drugs 20, 549–558 (2020). https://doi.org/10.1007/s40256-020-00401-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40256-020-00401-5