Abstract
Objectives
In recent years, new hypoglycaemic drugs that affect the incretin system have become increasingly popular in the treatment of type 2 diabetes mellitus (T2DM): glucagon-like receptor 1 agonists (GLP1RAs), dipeptidyl peptidase 4 inhibitors (DPP4is) and the recently developed dual glucagon-like receptor 1 agonist and glucose-dependent insulinotropic polypeptide (tirzepatide). Their main role of these drugs is to normalise blood glucose levels. In addition, GLP1RAs are approved for the treatment of excessive body weight. The efficacy of drugs affecting the incretin system is well described in the literature, however, there are still only few reports about their safety. This review aims to summarize the results of current research and meta-analyses on risk of acute pancreatitis (AP) during incretin-affecting drugs treatment.
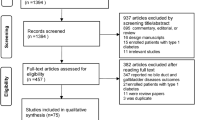
Methods
A narrative review was performed using present literature in an attempt to identify the relationship between AP and incretin-affecting drugs. The following keywords were used: acute pancreatitis, glucagon-like receptor 1 agonists, dipeptidyl peptidase 4 inhibitors and tirzepatide.
Results
It was demonstrated that the use of DPP4is is safe for the majority of patients with T2DM, whereas a risk of AP should be noted in case of GLP1RAs therapy. To date, most studies found no significant association between tirzepatide therapy and the increased risk of AP.
Conclusion
The majority of studies have shown that DPP4is, GLP1RAs and tirzepatide are effective and safe in most T2DM patients. However, the follow-up time for patients treated with tirzepatide is short, therefore more studies are required to confirm the safety of this drug.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, new hypoglycaemic drugs which affect the incretin system have gained increasing popularity in the treatment of type 2 diabetes mellitus (T2DM). Currently, two groups of incretin-based agents are available: glucagon-like peptide 1 receptor agonists (GLP1RAs), e.g. liraglutide and semaglutide, and dipeptidyl peptidase 4 inhibitors (DPP4is), e.g. sitagliptin and linagliptin. In addition to their beneficial effects on the body’s carbohydrate metabolism, they also show protective effects on the cardiovascular system and kidneys [1]. Besides GLP1RAs and DPP4is, tirzepatide (dual agonist of glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP) were approved in 2020 for the treatment of T2DM [2].
T2DM and obesity, due to their growing prevalence, have been recognised as epidemics by the World Health Organisation (WHO) [3]. T2DM accounts for approximately 90–95% of all diabetes. T2DM develops gradually and is rarely diagnosed at an early stage. The risk of developing T2DM is higher in people with obesity, hypertension, dyslipidemia and low physical activity. T2DM is diagnosed when the fasting plasma glucose level in two different measurements is ≥ 126 mg/dl (7.0 mmol/l) or the 2-hour glucose concentration in the oral glucose tolerance test (OGGT) test is ≥ 200 mg/dl (11.1 mmol/l) or glycated hemoglobin concentration is ≥ 6.5% or random plasma glucose level is ≥ 200 mg/dL (11.1 mmol/L) in patients with symptoms of hyperglycaemia (polyuria, polydipsia, weight loss, dehydration) [4]. Pharmacoterapy should be started when the disease is diagnosed. Treatment begins with the administration of metformin as the first-line drug. If metformin therapy is insufficient (glycated hemoglobin level ≥ 8.5%), a stronger hypoglycaemic drug is required (for example GLP1RAs, tirzepatide, DPP4is). Additionally, a very important element of T2DM treatment is the reduction of excessive body weight [5]. Obesity (body mass index (BMI) ≥ 30 kg/m2) and high waist circumference (≥ 94 cm in men and ≥ 80 cm in women) are also associated with an enhanced risk of cardiovascular diseases and metabolic syndrome [6].
A major long-term complication of T2DM is diabetic kidney disease (DKD), which is the leading cause of chronic kidney disease. However, it has been demonstrated that hyperglycaemia is not the only cause of kidney failure, and a number of pathophysiologic pathways are involved in the development of DKD, including overreactive renin-angiotensin-aldosterone system (RAAS), hemodynamics changes, inflammation, oxidative stress and hypoxia [7]. Diabetes causes changes in the glomeruli, which cause increased permeability of the small blood vessels in the glomeruli. As a result, albumin passes from the blood into the urine, where it appears in larger amounts (albuminuria). This is the first signal of kidney damage in the diabetes. There are several pathomechanisms of albuminuria in T2DM patients. The first is mentioned above excessive activation of the RAAS, which leads to increased levels of angiotensin II. Elevated levels of this hormone increase the risk of albuminuria and nephropathy. Hyperglycaemia also leads to increased glycolysis. End products of glycolysis such as fructose, transforming growth factor β1 (TGF-β1) promote renal cell hypertrophy, and persistent activation of protein kinase C (due to increased glycolysis) contributes to glomerular hyperfiltration Another pathomechanism of DKD is the presence of low-grade inflammation. Inflammatory markers (tumor necrosis factor-α (TNFα), interleukin(IL)-1, IL-6, IL-18) are expressed in the kidneys and lead to albuminuria and are toxic to kidney cells [7].
As in T2DM, GLP1RAs are used frequently in obesity and overweight treatment [8]. While there are numerous studies analysing the effectiveness of new hypoglycaemic drugs, there are still only few reports regarding safety of their use. Meta-analyses on the relationship of GLP1RAs and DPP4is treatment and various adverse effects suggested an increased risk of acute pancreatitis (AP), as well as gastrointestinal ulcer haemorrhage, acute cholangitis, acute cholecystitis, gastroesophageal reflux disease, constipation, diarrhoea, nausea, vomiting, and drug-induced liver injury [1].
AP is a disease characterised by acute inflammation of pancreas. The two most common causes of AP are alcohol consumption and cholelithiasis [9]. In the diagnostic process of AP, it is necessary to correlate sign, symptoms, laboratory tests and imaging tests [10]. At least two out of three criteria must be met to diagnose the disease: epigastric pain, at least a threefold increase in pancreatic enzyme (amylase or lipase) concentration, and changes in imaging studies (ultrasound, CT, MRI) specific to AP. According to the Atlanta (2012) classification, AP can be divided into mild, moderate and severe. Characteristics of AP groups are shown in Table 1 [11]. The treatment of AP is based on fluid resuscitation, analgesia and nutritional intervention. Early fluid resuscitation (within 24 h of onset of symptoms) and nutritional treatment is aimed at avoiding the development of systemic inflammation and reducing complications. Fluid resuscitation is important to increase pancreatic microcirculation and stabilize cardiovascular distress. It is recommended to use Ringer’s lactate for fluid resuscitation in AP [12].
Incretin-affecting drugs
GLP-1 is one of the incretin hormones. It is secreted in the small and large intestine by L cells in response to food ingestion. Together with GIP, it promotes insulin secretion in response to elevated blood glucose levels [13]. The secretion of incretin hormones, and thus insulin, depends on the carbohydrate intake level. The incretin effect has been shown to be significantly reduced or absent in T2DM patients. In contrast, infusions of pharmacological amounts of GLP-1 in these patients resulted in normalisation of fasting blood glucose levels [14].
In addition to increasing insulin secretion, incretin hormones also enhance the feeling of satiety and delay gastric emptying [15]. These hormones trigger responses by binding to specific receptors - GIP and GLP-1, which belong to the G-protein-coupled receptor family. They activate adenylate cyclase and increase intracellular cyclic adenosine monophosphate (cAMP) levels in pancreatic β-cells, thereby stimulating glucose-dependent insulin secretion. Physiologically, GLP-1 and GIP are rapidly degraded by the enzyme dipeptidylpeptidase 4 (DPP4), which acts on peptides by splitting the two NH2-terminal amino acids [16, 17]. In healthy humans, endogenous GIP and GLP-1 exert potent insulinotropic effects, however, in T2DM patients the GIP insulinotropic effect is significantly reduced. Therefore GLP1RAs are an important treatment option for T2DM. These drugs stimulate insulin secretion by pancreatic β-cells mainly in the postprandial period and inhibit glucagon secretion by pancreatic α-cells. Additionally, they activate GLP-1 receptors in the hindbrain and delay gastric emptying, which can cause a faster feeling of satiety and reduced food consumption. This leads to weight loss in T2DM and obese patients. In addition, GLP1RAs therapy is associated with reduced risk of hypoglycaemia [15].
At present, several types of GLP1RAs are used in the T2DM treatment. Liraglutide and lyxisenatide are injected once a day. Exenatide twice a day. Albiglutide, dulaglutide and semaglutide are injected once a week, while oral semaglutide is used once daily [18]. For obesity treatment, the Food and Drug Administration (FDA) has approved only two GLP1RAs: liraglutide and semaglutide [19].
It was demonstrated that GLP1RAs not only have a beneficial effect on carbohydrate metabolism (lowering blood glucose and reducing glycosylated haemoglobin) and weight loss, but also improve blood pressure control [20]. Additionally, these drugs contribute to the reduction of visceral adipose tissue and liver fat [21].
The most commonly reported adverse effects of GLP1RAs are gastrointestinal symptoms, such as diarrhoea, nausea and vomiting. These symptoms usually occur at the start of treatment or after increasing the dose of the drug and resolve spontaneously [22]. Meta-analyses demonstrated that GLP1RAs increase the risk of constipation, upper abdominal pain, gastric ulcer bleeding, acute cholangitis, acute cholecystitis and AP [1, 23].
Another line of incretin-based therapy for T2DM is DPP inhibition. DPP4 is a 110 kDa glycoprotein expressed on the surface of pancreas, kidney, liver and plasma cells [24]. DPP4 is composed of three domains: intracellular, transmembrane and extracellular with a glycosylation rich region, a cysteine rich region and a catalytic region. The activity of DPP4 is determined by its dimerization. Few years ago, a soluble form of DPP4 (sDPP4) has been found in serum, which is involved in the immunoregulation [25]. DPP4 is involved in the rapid metabolism of incretin hormones, including GLP-1 and GIP, which regulates postprandial insulin secretion. Therefore, DPP4 inhibitors (DPP4is) are widely used in the treatment of T2DM. These drugs reduce the activity of DPP4 by approximately 70–90%, which results in prolonged GLP-1 and GIP activity, and thus supports the reduction of blood glucose levels.
DPP4is which have been approved for treatment purposes have different half-life and pharmacokinetic profiles [26]. These drugs are: sitagliptin, vildagliptin, saxagliptin, linagliptin, allogliptin, teneligliptin, anagliptin and trelagliptin [27].
DPP4is have a lower risk of hypoglycaemia and do not have a direct impact on the gastric emptying rate or the feeling of satiety. In addition to their blood glucose-regulating properties, DPP4is have favourable effects on the central nervous system, liver, sleep quality, and inflammation [27]. It was also confirmed that these drugs have a beneficial effect on the lipid profile, reduce blood pressure and exhibit anti-atherosclerotic effects [28]. DPP4is have good tolerability and only few adverse effects, including skin lesions, nasopharyngitis, headache, and upper respiratory tract infections. It was also suggested that DPP4is administration may be associated with increased risk of heart failure, however, a meta-analysis conducted by Scirica et al. did not confirm these observations [29]. In another study Seino et al. showed that sitagliptin-treated patients had an enhanced risk of nasopharyngitis and eczema as opposed to the placebo group [30].
Association between incretin-affecting drugs and the risk of AP
To assess the risk of AP in patients treated with incretin-affecting drugs, numerous studies have been conducted, however, they gave opposite or inconclusive results. Liu et al. observed that the administration of GLP1RAs was associated with the higher AP risk. The group analysed 21,281 reports of gastrointestinal adverse effects during GLP1RAs treatment, including 1,752 (8.23%) cases related to AP. Their study showed that the highest risk of AP occurred with liragutide, followed by semaglutide, dulaglutide, liraglutide and exenatide [19]. In contrast, the meta-analysis of 10 studies involving 8,536 patients conducted by, Li et al. found no association between the use of semaglutide and AP [31]. In another study Tseng et al. analyzed the risk of AP in 13,717 patients with T2DM treated with GLP1RAs for at least 2 months and the same number of healthy controls. It was found that 71 T2DM patients (0.54%) and 66 controls (0.50%) were diagnosed with AP [32]. In similar study Storgaard et al. analyzed the results of three randomized trials (9,347 participants in the control group and 9,353 T2DM patients treated with GLP1RAs for minimum 48 months) and did not confirm the association of AP and GLP1RAs [33]. Similar results were obtained by Singh et al. who also did not find an increased risk of AP when using GLP1RAs. This meta-analysis included 7 studies (55,932 T2DM patients, including 27,948 patients treated with GLP1Ras and 27,984 controls). The follow-up period was over 12 months. In total 180 AP cases were diagnosed (92 cases in the treatment group and 88 in the control group) [34]. Wang et al. also reached the same conclusion in their study. The group analyzed the relationship between the GLP1RAs, DPP4is and sodium-glucose cotransporter-2 inhibitors (SGLT2is) and 91 kinds of digestive diseases. Six studies included in this meta-analysis assessed the risk of AP in patients treated with GLP1RAs. In a group of 20,598 patients from treatment group, 37 cases of AP were diagnosed. 36 cases of AP were found in the control group (20,608 patients) [1].
Wilding et al. demonstrated that AP was an uncommon adverse effect of semaglutide administration (AP was diagnosed in 0.2% of T2DM patients using this drug) [35]. However, the post-marketing pharmacovigilance tracings have shown that semaglutide-induced AP is likely to be a serious adverse event. Therefore, it is recommended to monitor all AP symptoms in patients treated with semaglutide and, if AP is diagnosed, it is recommended to discontinue treatment [36]. It is worth emphasizing that semaglutide may increase pancreatic enzymes (amylase and lipase) serum concentrations, but in a way that does not meet the criteria for the diagnosis of AP [37].
Liraglutide is another drug used in T2DM treatment, but is also currently the important component of pharmacotherapy for overweight and obesity [38]. Analysis of Novo Nordisk clinical study (NCT02730377) which investigated the effect in controlling glycaemia with liraglutide in patients with T2DM showed that the incidence of AP is 1.6 cases per 1,000 patient-years of exposure to liraglutide and this is higher when compared to glimepiride, rosiglitazone, insulin glargine, sitagliptin and exenatide [39]. Likewise Liu et al. showed that liraglutide treatment was associated with the elevated AP risk compared to other GLP1RAs [23]. In contrast Caparrotta et al. do not confirm these observations. The group analyzed the results of seven studies that assessed the incidence of AP after exposure to the previously mentioned GLP1RAs. Only one of the five studies included in the meta-analysis suggested an association between exenatide and AP. However, it should be noted that results of this analysis did not achieve statistical significance [40].
Other drugs from the GLP1RAs group are dulaglutide and albiglutide. During an observation period of 2 months, Nauck et al. did not diagnose any cases of AP in patients treated with dulaglutide at a dose of 0.75 mg and 1.5 mg, as well as in the placebo group. The total number of patients included in the study was 1,098. However, elevated pancreatic enzyme levels were observed in all T2DM patients treated with dulaglutide [41]. In the group of 3,136 patients included in the study by Chin et al., only one patient developed AP. In this study, patients were administered dulaglutide at a dose of 0.75 mg, and the follow-up period was 36 months [42]. In another studies AP was found to be a rare adverse effect of albiglutide treatment [43, 44].
In addition to large scale studies and meta-analyses that assessed the risk of adverse effects of GLP1RAs, results of several case reports have been published. Javed et al., Shahbazi et al. and Khan et al. demonstrated an occurrence of AP during GLP1RAs treatment [38, 45, 46]. AlSaadoun et al. described a case of an overweight patient without T2DM treated with liraglutide in which AP was diagnosed. The author noted that the probable cause of AP was a drug overdose [47]. Dolan et al. reported a similar case.
Currently, more research is needed to determine whether liraglutide used in the treatment of obesity at doses 2.5 times higher than those used in T2DM increases the risk of AP [48]. The American Association of Clinical Endocrinologists and the American College of Endocrinology recommend that GLP1RAs should be used with caution in patients with a history of AP and that treatment should be discontinued if this complication occurs [49].
Several studies have been conducted to evaluate the association of DPP4is and AP. In a study of Yabe et al. no elevated risk of AP during DPP4is treatment was found. In the group of 11,075 Japanese T2DM patients treated with DPP4is, 42 cases of AP were diagnosed (0.46%). The risk of AP with other antidiabetic drugs was similar [50]. The same conclusions were reached in the meta-analysis carried out by Wang et al. In their study, only 15 cases of AP were reported among 23,833 patients using DPP4is, however, the results were not statistically significant [1]. In a large study carried out by Azoulay et al., which included 1,532,513 patients treated with various antidiabetic drugs, it was found that the risk of AP is low during DPP4is treatment [51]. Ueki et al. analyzed the effectiveness and safety of alogliptin in 5,096 T2DM patients. It was observed that only five patients developed AP, but the results were not statistically significant [52]. Meanwhile, the studies by Lee et al. and Tkáč et al. confirmed the relationship between DPP4is administration and increased AP occurrence in T2DM patients [53, 54]. In a study of Lee et al. 56 cases of AP were diagnosed among 10,218 patients treated with DPP4is, which was statistically significant. However, the group noted that as exposure time goes up, AP risk does not tend to increase [53]. Tkáč et al. analyzed the results of three multicentre, randomized, double-blind, placebo-controlled studies to assess the frequency of AP in patients treated with DPP4is. The average duration of the research was 1.5 years. In the group of 18,238 patients 52 cases of AP were diagnosed. There was a significant relative increase in the incidence of AP by 79% compared to the placebo group. Moreover, the absolute increase in the incidence of AP was 0.13%. There are one to two extra cases of AP per 1,000 patients treated with DPP4is [54]. In addition, Sayiner et al. showed that DPP4is can increase blood lipase and amylase levels in patients without AP symptoms. Due to the inconclusive findings, DPP4is should be used with caution in individuals with an increased AP risk [55].
Tirzepatide and the risk of AP
Tirzepatide is a recently developed dual agonist of GLP-1 and GIP approved for the T2DM treatment. It has a higher affinity for GIP than for GLP-1, and has a half-life of 5 days, so it can be administered once a week [56]. Despite the fact that the FDA and the European Medicines Agency (EMA) approved tirzepatide in 2022 for T2DM therapy, the drug is currently undergoing the approval procedure for obesity treatment [2].
The SURPASS-5 clinical trial (NCT04039503) showed that patients treated with tirzepatide in combination with insulin glargine achieved lower glycated haemoglobin and greater weight loss than patients treated only with insulin glargine. The most commonly observed side effects of tirzepatide in this clinical study were nausea, vomiting, diarrhoea and reduced appetite. An increased risk of pancreatitis, cholecystitis, injection site reactions and hypersensitivity reactions was also observed, depending on the dose. It was concluded that tirzepatide therapy carries a low risk of hypoglycaemia [56]. A meta-analysis by Karagiannis et al. including seven studies (6,609 participants) gave similar results. It was observed that tirzepatide significantly reduced glycated haemoglobin and body weight compared to placebo, GLP1RAs and basal insulin [57].
In another study Xie et al. found that tirzepatide, administered at a dose of 15 mg, had the highest rate of adverse effects overall and a higher risk of hypoglycaemia compared to GLP1RAs [58].
A meta-analysis of ten studies conducted by Mishra et al. revealed that gastrointestinal adverse effects were reported by 39.05% of patients treated with the 5 mg of tirzepatide, 45.57% of patients treated with the 10 mg, and 49.25% of patients treated with the 15 mg. In this study, the AP risk was found to be at the level of 0.39% in the 5 mg group, 0.36% in the 10 mg group, and 0.32% in the 15 mg group, which was similar to placebo group. Therefore, it was concluded that tirzepatide therapy is associated with a low risk of this adverse effect regardless of the dose [59]. Similar findings were obtained by Tang et al. Their meta-analysis included six studies involving 6,579 patients (4,410 in the tirzepatide-treated group and 2,054 in the control group). It was demonstrated that there are no significant differences in the incidence of AP in these groups [60].
In another study Frias et al. reported four cases of AP in 1,409 tirzepatide-treated patients, however none of which met the criteria for severe condition [61]. A meta-analysis by Mishra et al. evaluated the impact of tirzepatide on blood lipase levels and noted that the drug significantly increased this enzyme concentration, especially in a dose of 15 mg [59].
Conclusion
GLP1RAs and DPP4is have been increasingly applied in the pharmacotherapy of T2DM and obesity. The majority of studies have shown that DPP4is are effective and safe in most T2DM patients. However, when using GLP1RAs, due to differences in findings, attention should be paid to an AP risk. It was recommended that administration of these drugs should be discontinued if AP has been registered. Special attention should be paid to the patients with a history of AP regardless of ethology or with risk factors for this disease. Given the short follow-up period applied to the patients treated with tirzepatide, further studies are necessary to assess the AP risk during the therapy. A summary of the results of the studies included in this review is presented in Table 2.
References
Wang YW, Lin JH, Yang CS. Meta-analysis of the association between new hypoglycemic agents and digestive diseases. Med (Baltim). 2022;101(34):e30072. https://doi.org/10.1097/MD.0000000000030072.
Vázquez LA, Romera I, Rubio-de Santos M, Escalada J. Glycaemic Control and Weight reduction: a narrative review of New therapies for type 2 diabetes. Diabetes Ther. 2023;14(11):1771–84. https://doi.org/10.1007/s13300-023-01467-5.
Chobot A, Górowska-Kowolik K, Sokołowska M, Jarosz-Chobot P. Obesity and diabetes-not only a simple link between two epidemics. Diabetes Metab Res Rev. 2018;34(7):e3042. https://doi.org/10.1002/dmrr.3042.
American Diabetes Association Professional Practice Committee. 2. Diagnosis and classification of diabetes: standards of Care in Diabetes-2024. Diabetes Care. 2024;47(Suppl 1):S20–42. https://doi.org/10.2337/dc24-S002.
American Diabetes Association Professional Practice Committee. 9. Pharmacologic approaches to Glycemic Treatment: standards of Care in Diabetes-2024. Diabetes Care. 2024;47(Suppl 1):S158–78. https://doi.org/10.2337/dc24-S009.
Lavie CJ, Laddu D, Arena R, Ortega FB, Alpert MA, Kushner RF. Healthy Weight and Obesity Prevention: JACC Health Promotion Series. J Am Coll Cardiol. 2018;72(13):1506–31. https://doi.org/10.1016/j.jacc.2018.08.1037.
Toth-Manikowski S, Atta MG. Diabetic kidney disease: pathophysiology and therapeutic targets. J Diabetes Res. 2015;2015:697010. https://doi.org/10.1155/2015/697010.
Liu Y, Ruan B, Jiang H, Le S, Liu Y, Ao X, et al. The weight-loss effect of GLP-1RAs glucagon-like Peptide-1 receptor agonists in non-diabetic individuals with overweight or obesity: a systematic review with Meta-Analysis and Trial Sequential Analysis of Randomized controlled trials. Am J Clin Nutr. 2023;118(3):614–26. https://doi.org/10.1016/j.ajcnut.2023.04.017.
Roussey B, Calame P, Revel L, Zver T, Konan A, Piton G, et al. Liver spontaneous hypoattenuation on CT is an imaging biomarker of the severity of acute pancreatitis. Diagn Interv Imaging. 2022;103(9):401–7. https://doi.org/10.1016/j.diii.2022.03.008.
Kinoshita H, Zhang J, Ponthisarn A, Sharma M, Binh N, Siam A, et al. Clinical practice guidelines in the diagnosis and management of acute pancreatitis. Med Studies/Studia Medyczne. 2019;35(4):304–11. https://doi.org/10.5114/ms.2019.91248.
Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, et al. Classification of acute pancreatitis–2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62(1):102–11. https://doi.org/10.1136/gutjnl-2012-302779.
Szatmary P, Grammatikopoulos T, Cai W, Huang W, Mukherjee R, Halloran C. et al Acute Pancreatitis: Diagnosis Treat Drugs. 2022;82(12):1251–76. https://doi.org/10.1007/s40265-022-01766-4.
Goodarzi MO, Petrov MS. Diabetes of the exocrine pancreas: implications for Pharmacological Management. Drugs. 2023;83(12):1077–90. https://doi.org/10.1007/s40265-023-01913-5.
Boer GA, Holst JJ. Incretin Hormones and type 2 diabetes-mechanistic insights and therapeutic approaches. Biology (Basel). 2020;9(12):473. https://doi.org/10.3390/biology9120473.
Gumieniczek A, Berecka-Rycerz A. Metabolism and chemical degradation of New Antidiabetic drugs: a review of Analytical approaches for Analysis of Glutides and Gliflozins. Biomedicines. 2023;11(8):2127. https://doi.org/10.3390/biomedicines11082127.
Seino Y, Fukushima M, Yabe D. GIP and GLP-1, the two incretin hormones: similarities and differences. J Diabetes Investig. 2010;1(1–2):8–23. https://doi.org/10.1111/j.2040-1124.2010.00022.x.
Sfairopoulos D, Liatis S, Tigas S, Liberopoulos E. Clinical pharmacology of glucagon-like peptide-1 receptor agonists. Horm (Athens). 2018;17(3):333–50. https://doi.org/10.1007/s42000-018-0038-0.
Popoviciu MS, Păduraru L, Yahya G, Metwally K, Cavalu S. Emerging role of GLP-1 agonists in obesity: a Comprehensive Review of Randomised controlled trials. Int J Mol Sci. 2023;24(13):10449. https://doi.org/10.3390/ijms241310449.
Cesaro A, De Michele G, Fimiani F, Acerbo V, Scherillo G, Signore G, et al. Visceral adipose tissue and residual cardiovascular risk: a pathological link and new therapeutic options. Front Cardiovasc Med. 2023;10:1187735. https://doi.org/10.3389/fcvm.2023.1187735.
Shi FH, Li H, Cui M, Zhang ZL, Gu ZC, Liu XY. Efficacy and safety of once-weekly semaglutide for the treatment of type 2 diabetes: a systematic review and Meta-analysis of Randomized controlled trials. Front Pharmacol. 2018;9:576. https://doi.org/10.3389/fphar.2018.00576.
Liao C, Liang X, Zhang X, Li Y. The effects of GLP-1 receptor agonists on visceral fat and liver ectopic fat in an adult population with or without diabetes and nonalcoholic fatty liver disease: a systematic review and meta-analysis. PLoS ONE. 2023;18(8):e0289616. https://doi.org/10.1371/journal.pone.0289616.
Nauck MA, Quast DR, Wefers J, Meier JJ. GLP-1 receptor agonists in the treatment of type 2 diabetes - state-of-the-art. Mol Metab. 2021;46:101102. https://doi.org/10.1016/j.molmet.2020.101102.
Liu L, Chen J, Wang L, Chen C, Chen L. Association between different GLP-1 receptor agonists and gastrointestinal adverse reactions: a real-world disproportionality study based on FDA adverse event reporting system database. Front Endocrinol (Lausanne). 2022;13:1043789. https://doi.org/10.3389/fendo.2022.1043789.
El-Arabey AA, Zhang H, Abdalla M, Al-Shouli ST, Alkhalil SS, Liu Y. Metformin as a promising target for DPP4 expression: computational modeling and experimental validation. Med Oncol. 2023;40(10):277. https://doi.org/10.1007/s12032-023-02140-4.
Chen SY, Kong XQ, Zhang KF, Luo S, Wang F, Zhang JJ. DPP4 as a potential candidate in Cardiovascular Disease. J Inflamm Res. 2022;15:5457–69. https://doi.org/10.2147/JIR.S380285.
Deacon CF. Dipeptidyl peptidase 4 inhibitors in the treatment of type 2 diabetes mellitus. Nat Rev Endocrinol. 2020;16(11):642–53. https://doi.org/10.1038/s41574-020-0399-8.
Röhrborn D, Wronkowitz N, Eckel J. DPP4 in diabetes. Front Immunol. 2015;6:386. https://doi.org/10.3389/fimmu.2015.0038.
Bernardini F, Nusca A, Coletti F, La Porta Y, Piscione M, Vespasiano F, et al. Incretins-based therapies and their Cardiovascular effects: New Game-Changers for the management of patients with diabetes and Cardiovascular Disease. Pharmaceutics. 2023;15(7):1858. https://doi.org/10.3390/pharmaceutics15071858.
Scirica BM, Im K, Murphy SA, Kuder JF, Rodriguez DA, Lopes RD, et al. Re-adjudication of the Trial evaluating Cardiovascular outcomes with Sitagliptin (TECOS) with study-level meta-analysis of hospitalization for heart failure from cardiovascular outcomes trials with dipeptidyl peptidase-4 (DPP-4) inhibitors. Clin Cardiol. 2022;45(7):794–801. https://doi.org/10.1002/clc.23844.
Seino Y, Kaku K, Kadowaki T, Okamoto T, Sato A, Shirakawa M, et al. A randomized, placebo-controlled trial to assess the efficacy and safety of sitagliptin in Japanese patients with type 2 diabetes and inadequate glycaemic control on ipragliflozin. Diabetes Obes Metab. 2021;23(6):1342–50. https://doi.org/10.1111/dom.14346.
Li J, He K, Ge J, Li C, Jing Z. Efficacy and safety of the glucagon-like peptide-1 receptor agonist oral semaglutide in patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetes Res Clin Pract. 2021;172:108656. https://doi.org/10.1016/j.diabres.2021.108656.
Tseng CM, Liao WC, Chang CY, Lee CT, Tseng CH, Hsu YC, et al. Incretin-based pharmacotherapy and risk of adverse pancreatic events in the ethnic Chinese with diabetes mellitus: a population-based study in Taiwan. Pancreatology. 2017;17(1):76–82. https://doi.org/10.1016/j.pan.2016.10.003.
Storgaard H, Cold F, Gluud LL, Vilsbøll T, Knop FK. Glucagon-like peptide-1 receptor agonists and risk of acute pancreatitis in patients with type 2 diabetes. Diabetes Obes Metab. 2017;19(6):906–8. https://doi.org/10.1111/dom.12885.
Singh AK, Gangopadhyay KK, Singh R. Risk of acute pancreatitis with incretin-based therapy: a systematic review and updated meta-analysis of cardiovascular outcomes trials. Expert Rev Clin Pharmacol. 2020;13(4):461–8. https://doi.org/10.1080/17512433.2020.1736041.
Wilding JPH, Batterham RL, Calanna S, Davies M, Van Gaal LF, Lingvay I, et al. Once-weekly semaglutide in adults with overweight or obesity. N Engl J Med. 2021;384(11):989–1002. https://doi.org/10.1056/NEJMoa2032183.
Shu Y, He X, Wu P, Liu Y, Ding Y, Zhang Q. Gastrointestinal adverse events associated with semaglutide: a pharmacovigilance study based on FDA adverse event reporting system. Front Public Health. 2022;10:996179. https://doi.org/10.3389/fpubh.2022.996179.
Aroda VR, Erhan U, Jelnes P, Meier JJ, Abildlund MT, Pratley R, et al. Safety and tolerability of semaglutide across the SUSTAIN and PIONEER phase IIIa clinical trial programmes. Diabetes Obes Metab. 2023;25(5):1385–97. https://doi.org/10.1111/dom.14990.
Javed H, Kogilathota Jagirdhar GS, Kashyap R, Vekaria PH. Liraglutide-Induced Pancreatitis: a Case Report and Literature Review. Cureus. 2023;15(4):e38263. https://doi.org/10.7759/cureus.38263.
Jensen TM, Saha K, Steinberg WM. Is there a link between liraglutide and pancreatitis? A post hoc review of pooled and patient-level data from completed liraglutide type 2 diabetes clinical trials. Diabetes Care. 2015;38(6):1058–66. https://doi.org/10.2337/dc13-1210.
Caparrotta TM, Templeton JB, Clay TA, Wild SH, Reynolds RM, Webb DJ, et al. Glucagon-like peptide 1 receptor agonist (GLP1RA) exposure and outcomes in type 2 diabetes: a systematic review of Population-based Observational studies. Diabetes Ther. 2021;12(4):969–89. https://doi.org/10.1007/s13300-021-01021-1.
Nauck M, Weinstock RS, Umpierrez GE, Guerci B, Skrivanek Z, Milicevic Z. Efficacy and safety of dulaglutide versus sitagliptin after 52 weeks in type 2 diabetes in a randomized controlled trial (AWARD-5). Diabetes Care. 2014;37(8):2149–58. https://doi.org/10.2337/dc13-2761.
Chin R, Nagaoka S, Nakasawa H, Tanaka Y, Inagaki N. Safety and effectiveness of dulaglutide 0.75 mg in Japanese patients with type 2 diabetes in real-world clinical practice: 36 month post-marketing observational study. J Diabetes Investig. 2023;14(2):247–58. https://doi.org/10.1111/jdi.13932.
Al-Kawas F, Anderson MA, Enns R, Wilson TH, Johnson S, Mallory JM, PANCREATIC SAFETY IN STUDIES OF THE GLUCAGON-LIKE PEPTIDE-1 RECEPTOR AGONIST ALBIGLUTIDE. Endocr Pract. 2019;25(7):698–716. https://doi.org/10.4158/EP-2018-0507.
Hernandez AF, Green JB, Janmohamed S, D’Agostino RB, Sr, Granger CB, Jones NP, et al. Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease (harmony outcomes): a double-blind, randomised placebo-controlled trial. Lancet. 2018;392(10157):1519–29. https://doi.org/10.1016/S0140-6736(18)32261-X.
Shahbazi M, Qudsiya Z, Fahel A, Amini A, Tanoli T. First reported case of Dulaglutide-Induced Acute Pancreatitis with normal serum lipase level. Cureus. 2023;15(6):e40576. https://doi.org/10.7759/cureus.40576.
Khan AB, Shah A, Ahmad S, Khan MI, Amir A. Dulaglutide (Trulicity)-Induced Acute Pancreatitis: a Case Report. Cureus. 2023;15(5):e38630. https://doi.org/10.7759/cureus.38630.
AlSaadoun AR, AlSaadoun TR, Al Ghumlas AK. Liraglutide Overdose-Induced Acute Pancreatitis. Cureus. 2022;14(1):e21616. https://doi.org/10.7759/cureus.21616.
Dolan RD, Bazarbashi AN, Lo A, Smith BN. Liraglutide-Induced Hemorrhagic Pancreatitis in a nondiabetic patient. ACG Case Rep J. 2020;7(5):e00380. https://doi.org/10.14309/crj.0000000000000380.
Garber AJ, Handelsman Y, Grunberger G, Einhorn D, Abrahamson MJ, Barzilay JI, CONSENSUS STATEMENT BY THE AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS AND AMERICAN COLLEGE OF ENDOCRINOLOGY ON THE COMPREHENSIVE TYPE, et al. 2 DIABETES MANAGEMENT ALGORITHM– 2020 EXECUTIVE SUMMARY. Endocr Pract. 2020;26(1):107–39. https://doi.org/10.4158/CS-2019-0472.
Yabe D, Kuwata H, Kaneko M, Ito C, Nishikino R, Murorani K, et al. Use of the Japanese health insurance claims database to assess the risk of acute pancreatitis in patients with diabetes: comparison of DPP-4 inhibitors with other oral antidiabetic drugs. Diabetes Obes Metab. 2015;17(4):430–4. https://doi.org/10.1111/dom.12381.
Azoulay L, Filion KB, Platt RW, Dahl M, Dormuth CR, Clemens KK, et al. Association between Incretin-based drugs and the risk of Acute Pancreatitis. JAMA Intern Med. 2016;176(10):1464–73. https://doi.org/10.1001/jamainternmed.2016.1522.
Ueki K, Tanizawa Y, Nakamura J, Yamada Y, Inagaki N, Watada H, et al. Long-term safety and efficacy of alogliptin, a DPP-4 inhibitor, in patients with type 2 diabetes: a 3-year prospective, controlled, observational study (J-BRAND Registry). BMJ Open Diabetes Res Care. 2021;9(1):e001787. https://doi.org/10.1136/bmjdrc-2020-001787.
Lee M, Sun J, Han M, Cho Y, Lee JY, Nam CM, et al. Nationwide trends in Pancreatitis and Pancreatic Cancer Risk among patients with newly diagnosed type 2 diabetes receiving Dipeptidyl Peptidase 4 inhibitors. Diabetes Care. 2019;42(11):2057–64. https://doi.org/10.2337/dc18-2195.
Tkáč I, Raz I. Combined analysis of three large interventional trials with gliptins indicates increased incidence of Acute Pancreatitis in patients with type 2 diabetes. Diabetes Care. 2017;40(2):284–6. https://doi.org/10.2337/dc15-1707.
Sayiner ZA, Inan Demiroğlu G, Akarsu E, Araz M. The relationship between Dipeptidyl Peptidase-4 inhibitor usage and Asymptomatic Amylase Lipase Increment in type 2 diabetes Mellitus patients. Turk J Pharm Sci. 2020;17(1):68–73. https://doi.org/10.4274/tjps.galenos.2018.83788.
Dahl D, Onishi Y, Norwood P, Huh R, Bray R, Patel H, et al. Effect of Subcutaneous Tirzepatide vs Placebo added to titrated insulin glargine on Glycemic Control in patients with type 2 diabetes: the SURPASS-5 Randomized Clinical Trial. JAMA. 2022;327(6):534–45. https://doi.org/10.1001/jama.2022.0078.
Karagiannis T, Avgerinos I, Liakos A, Del Prato S, Matthews DR, Tsapas A, et al. Management of type 2 diabetes with the dual GIP/GLP-1 receptor agonist tirzepatide: a systematic review and meta-analysis. Diabetologia. 2022;65(8):1251–61. https://doi.org/10.1007/s00125-022-05715-4.
Xie Z, Hu J, Gu H, Li M, Chen J. Comparison of the efficacy and safety of 10 glucagon-like peptide-1 receptor agonists as add-on to metformin in patients with type 2 diabetes: a systematic review. Front Endocrinol (Lausanne). 2023;14:1244432. https://doi.org/10.3389/fendo.2023.1244432.
Mishra R, Raj R, Elshimy G, Zapata I, Kannan L, Majety P, et al. Adverse events related to Tirzepatide. J Endocr Soc. 2023;7(4):bvad016. https://doi.org/10.1210/jendso/bvad016.
Tang Y, Zhang L, Zeng Y, Wang X, Zhang M. Efficacy and safety of tirzepatide in patients with type 2 diabetes: a systematic review and meta-analysis. Front Pharmacol. 2022;13:1016639. https://doi.org/10.3389/fphar.2022.1016639.
Frías JP, Davies MJ, Rosenstock J, Pérez Manghi FC, Fernández Landó L, Bergman BK, et al. Tirzepatide versus Semaglutide once Weekly in patients with type 2 diabetes. N Engl J Med. 2021;385(6):503–15. https://doi.org/10.1056/NEJMoa2107519.
Author information
Authors and Affiliations
Contributions
All authors contributed to conceptualization, review and editing of the manuscript. All authors approved the final manuscript for submission.
Ethics declarations
Conflict of interest
None.
Financial interests
The authors declare they have no financial interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Czaplicka, A., Kaleta, B. The effect of incretin-based drugs on the riks of acute pancreatitis: a review. J Diabetes Metab Disord 23, 487–495 (2024). https://doi.org/10.1007/s40200-024-01430-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-024-01430-6