Abstract
This paper summarises the increasing epidemiological and experimental evidence of the causal link between exposure to high concentrations of welding fume exposure for prolonged periods of time and the subsequent development of pulmonary fibrosis in a relatively small number of people. It is not yet clear which components of welding fume or gases are the cause, but the most likely culprits are the soluble transition metals which may cause the formation of free radicals. The most likely work scenario leading to pulmonary fibrosis due to welding fume is of high fume exposure, without effective local extraction and respiratory protection, in confined spaces for long periods of time. Avoidance of high exposures for long periods of time is required to prevent this condition. For clarity, the term “pulmonary fibrosis due to prolonged exposure to welding fume at high concentration” is suggested when there is shown to be a causal link in an individual, and we recommend that the terms siderofibrosis and arc welder’s lung are abandoned.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The purpose of this document is to provide an up-to-date review of the epidemiological and experimental evidence linking prolonged steel welding fume exposure at high concentration and the subsequent development of pulmonary fibrosis. A previous paper in Welding in the World [1] has reviewed the evidence for airway disease in welders, the general nature of welding fume and provided generic guidance on the control of fume [Box 1] and complements this paper.
Box 1. Recommendations from Commission VIII on control of fume and the prevention of airways disease in welders [1]
• Systems of work are employed that will minimise the fume and gas exposure of the welder and others in the workplace, and, if possible, welding in confined spaces is avoided if technically feasible; |
• Welding processes and procedures that produce lower amounts of fume emissions are used wherever possible; |
• Surface coatings are removed prior to welding; |
• The welders keep their head out of the welding plume; |
• Local exhaust ventilation is used when arc welding in order to keep the level of fume exposure as low as reasonably practicable and at least to national standards. Local exhaust ventilation reduces background levels of fume and protects others in the workplace. It is always desirable and may be needed even if an air-fed helmet is used to reduce levels to acceptable standards; |
• Local exhaust ventilation is placed in close proximity to the workpiece when welding and grinding, including when undertaking TIG welding; |
• Local exhaust ventilation is continued after the completion of the welding to clear the remaining welding fume and gas; |
• The welder uses an improved helmet (a helmet with an apron to reduce fume and gases from getting under the helmet), rather than a standard helmet as a minimum but ideally uses a purified air-fed helmet; |
• The welder uses a technique of counting to five at the end of the welding process before lifting an air-fed helmet to allow the fume levels to reduce before breathing ambient air containing welding fume. This technique is not appropriate for standard or improved helmets; |
• If the welder needs to do any grinding in the area, local exhaust ventilation and a suitable dust mask are used; |
• Welders are strongly advised not to smoke as this exposure acts with welding fume to cause more damage than would be the case with welding fume or smoking alone. |
Once we have defined some terms commonly used to describe pulmonary fibrosis in welders, we will go through the historical background and describe the experimental, radiological and clinical evidence currently available. We will describe a typical case of pulmonary fibrosis due to welding fume and provide guidelines regarding appropriate clinical investigation and occupational management. Finally, we suggest key topics for further research and areas needing the development of international consensus.
Excluded from this review are the medical causes of pulmonary fibrosis and pulmonary conditions following exposure in welders to short-duration very high-dose exposures to welding fume and gases; aluminium; tungsten and cobalt; and asbestos and crystalline silica.
1.1 Definitions
Pneumoconiosis is a medical condition caused by dust in the lungs, for instance, as evidenced by X-ray, computerised tomography (CT) scan or histology, and may be for example due to exposure to silica, mixed dusts, metals [2–4], or organic matter. It is modulated by host factors such as genetics, the immune response and smoking [5].
Pneumoconiosis due to welding fume includes the following terms:
-
Siderosis which is evidence of iron in the lung on a chest X-ray or histology without fibrosis;
-
Siderofibrosis which is the development of fibrosis within the lungs as a result of exposure to iron as evidenced by histology;
-
Pulmonary fibrosis due to welding fume where there is histological proof of fibrosis that is thought to be due to welding fumes or gases (but not necessarily due to iron).
Whilst siderosis is common, amounting to a significant percentage of the workforce in many studies, particularly in older workers, the development of symptomatic pulmonary fibrosis due to welding fume is very rare, in the order of 200 cases reported in the world medical literature over the last 75 years.
In the past, the term “arc welder’s lung” was used in a non-specific way and has been used to describe welders with pulmonary fibrosis but could also cover non-fibrotic responses of the lung to welding fume.
2 Historical background
Following the introduction of welding technology, it became apparent that some arc welders who weld steels developed abnormal chest X-rays due to the iron content of the fumes [6]. Debate followed about whether iron from welding fume might result in pulmonary fibrosis [7–9], and by the early 1960s, the conclusion in the UK [10] and by some in the USA [11] was that this was unlikely to be the case. Subsequent mortality studies have not shown an increased rate of death from either pneumoconiosis or pulmonary fibrosis in welders [12–17].
Nevertheless, there has been long standing concern in Germany [18, 19], Japan [20, 21], Eastern Europe [22, 23] and by some in the USA [24–27] that some compounds in the fumes and gases might cause pulmonary fibrosis with high cumulative exposures.
Recently, the German government has prescribed pulmonary fibrosis due to prolonged exposure to welding fume at high concentration as an industrial disease [28], and this action prompted us to review the evidence and write this review.
3 The evidence that welding fume can cause pulmonary fibrosis
3.1 Experimental evidence
Many animal studies of welding fume exposure have been undertaken using both direct instillation of welding fume into the lungs of rodents [29–34], inhalation studies using fresh welding fume [29, 35–41] and in vitro studies of rodent macrophages [42, 43].
Once deposited within the lungs, the insoluble fraction, the “spinels” comprising complex iron-manganese oxides, will remain until removed by phagocytosis or expectoration, but the soluble fraction will dissolve in the macrophages and alveolar tissues and will steadily be carried out of the lungs in the blood and lymphatics. Soluble metals in welding fume include chromium and nickel in stainless steel and manganese that is not bound into spinels in mild steel. It is thought that the most reactive part of the fume is the soluble fraction [42], which may cause free-radical production within the tissues of the alveolus. Manual metal arc (MMA) welding gives rise to a greater amount of soluble fume than metal inert gas or metal active gas welding (MIG/MAG) [33]. Whilst fume contains silicates, these are amorphous and not crystalline and therefore do not pose a risk of fibrosis.
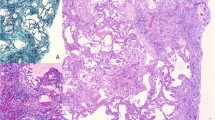
Following sacrifice of experimental animals exposed to welding fume, it is possible to show the sequence of events in the alveoli and bronchioles [44, 45]. These changes are similar to those found in humans with pulmonary fibrosis due to welding fume and are more marked with exposure to stainless steel than mild steel welding fume [31, 33, 37, 41, 46] and more marked in MMA than MIG/MAG [33]. Initially, welding fume deposits in the alveoli and bronchioles and is phagocytosed by macrophages and after a few days by polymorphonuclear cells. Such cells may move up into the bronchi to be expectorated once they have reached the top of the mucociliary escalator. Macrophages may accumulate in the alveoli as a result of persistent levels of welding fume exposure. As the macrophages become overwhelmed by fume, more macrophages are recruited to ingest the fume, some of which pass into the tissue of the alveoli and the interstitial tissue and some of which die in the alveolar air space. Some of the welding fume and macrophages pass into the lymphatic system to be removed from the alveolar interstitial tissue. Deposits of macrophages and welding fume particles increase around the bronchioles and arterioles. With time, fibrosis may develop within these deposits, which may distort the adjacent bronchioles, either leading to narrowing of the small airways or a traction dilatation. The lung demonstrates patchy areas of fibrosis. Areas of emphysema may develop in the peribronchial areas partly as a result of traction on the alveoli from adjacent areas of fibrosis. The ability of the lung to recover and the risk of development of pulmonary fibrosis depend on the cumulative exposure to fume, that is, the product of dose and duration [45, 47].
3.2 Radiological evidence
Several studies have described the radiological investigation of welders’ chests including chest X-ray and CT. The chances of developing radiological evidence of siderosis gradually increase with duration of exposure, lower exposure showing a delayed onset of the condition [48, 49].
Studies of CT scans of welders recruited from the workplace show changes of poorly defined centrilobular micronodules and branching linear structures [50, 51]. These changes reflect iron deposition in the airways but do not reflect changes within the tissue of the lung (unlike silicosis and coal worker’s pneumoconiosis). Welders who have been referred for CT as a result of positive chest X-rays taken during health surveillance programmes show similar changes with the addition of occasional ground-glass opacities [52], occasional mild fibrotic changes and emphysema [53]. In the radiology literature, symptomatic welders who have been referred for clinical assessment, however, show the addition of the following: emphysema in smokers, “ground-glass opacities”; features of usual interstitial pneumonia such as “honeycombing”; and conglomeration and bronchiectasis [54, 55]. There is no histology reported in these papers.
3.3 Histological evidence
In total, there are over 200 cases of histologically proven pulmonary fibrosis thought to be due to welding of steels in the world medical literature over the last 75 years.
Individual case reports can be classified into three groups: those where pulmonary fibrosis was related to welding fume exposure [56–74], those where it was related to an occupational exposure other than welding fume and those where there is most probably a clinical reason for the pulmonary fibrosis. Finally, in some pathology samples, no or minimal fibrosis was found [8, 75–77]. There are additional occasional reports of localised collections of welding fume within the lung tissue and the development of conglomeration/progressive massive fibrosis [78–81].
One of the difficulties with these historical case reports is that the classification of pulmonary fibrosis has changed significantly over the years and therefore it is difficult to know, without thorough multidisciplinary retrospective review of the cases using modern criteria and methods, whether they all represent pulmonary fibrosis due to welding fumes or whether some of them are in fact pulmonary fibrosis in a person who happens to be a welder but where there is no causal connection between the occupation and condition.
Several case series of welders with histologically proven pulmonary fibrosis have been published [8, 19, 22, 26, 27, 76, 77, 82–94], the most detailed of which is a series of 15 welders by Buerke et al. [95]. Buerke et al. came to the same conclusion as others that the cases were related to high exposure to welding fume for a prolonged period of time. Cumulative exposure estimates in the study by Buerke et al. ranged from 115 to 4350 mg years m−3 with a median exposure estimate of 221 mg years m−3. All were MMA welders, but some also undertook MIG, MAG or tungsten inert gas (TIG) welding. The majority undertook confined space welding. Only five were exposed to chromium and seven to aluminium. Five were non-smokers.
In contrast to the radiological papers, honeycombing is not mentioned in any of the case reports or series with histology. Many papers include comments about associated emphysema in addition to the fibrosis, either clinical [26], radiological [57, 74, 80] or pathological [56, 58, 60, 73], but emphysema may be more related to the effects of cigarette smoke than welding exposure [96].
Some papers describe iron overload as a result of the high cumulative exposure to iron fumes [53, 65, 67, 80, 94], and there are several case reports of cor pulmonale (right heart failure) [27, 57, 63, 95].
3.3.1 Pathological grading of pulmonary fibrosis due to welding fume
A proposed pathology grading has been suggested by Müller and Verhoff [91]:
-
Mild pulmonary fibrosis due to welding fume shows alveolar and interstitial macrophages but has no fibrosis in the dust deposits.
-
Moderate pulmonary fibrosis due to welding fume demonstrates an increased number of macrophages with significant fibrosis in the dust deposits.
-
Severe pulmonary fibrosis due to welding fume shows heavy fume deposits, chronic fibrosis with focal accentuation and a close association between fibrosis and deposits.
Buerke et al. [93] indicated that welders with severe disease had a cumulative exposure level in the order of 200 mg years m−3 and welders with moderate disease of 115 mg years m−3.
4 Pulmonary fibrosis in welders
Pulmonary fibrosis in welders is not necessarily due to exposure to welding fume or gases as welders are also subject to clinical conditions unrelated to workplace exposures. The most common clinical condition is idiopathic pulmonary fibrosis (IPF).
Epidemiological research has shown that IPF and usual interstitial pneumonia (UIP), the most common histological pattern seen in IPF, are significantly more common in persons exposed to metal dust but are not more common in welders than controls [97–102]. Furthermore, the case series and case reports of welders with pulmonary fibrosis in the literature where there is histology contain no definite cases and only one case suggestive of IPF [24]. The two case reports of IPF in a welder both had only a radiological diagnosis and no histology [54, 103]. Therefore, a welder who has a diagnosis of IPF/UIP can be reassured that it was not the welding fume that caused the condition.
In contrast, desquamative interstitial pneumonia (DIP) and respiratory bronchiolitis lie on a continuum and share many features with the histology described in individual case reports and case series of welders [81, 83, 85]. These conditions, particularly DIP, have been linked with particle exposure including welding in some studies [104–106]. Given the changes in classification of the clinical conditions, it is now appropriate to review the link with welding fume for welders with pulmonary fibrosis to ascertain whether fibrosis due to welding fume is a separate condition to this continuum or whether in fact these are the same condition [96].
Finally, a few cases of pulmonary fibrosis in welders in the literature are related to exposure to crystalline silica in addition to welding fume [24, 59, 76, 77, 89] or asbestos [82, 85, 89, 107, 108]. Without formal assessment of these compounds within the areas of fibrosis, it is not possible to make the diagnosis and it is easy to miss the diagnosis if there is not a separate mineralogical analysis.
5 Assessment of the welder with pulmonary fibrosis
The assessment of a welder who is suspected of having pulmonary fibrosis should be undertaken by a multidisciplinary team experienced in both interstitial lung disorders and pneumoconiosis. The assessment should be undertaken to national guidelines and will normally include clinical history; examination; spirometry; carbon monoxide transfer factor; transferrin, an exposure assessment by an occupational hygienist or occupational physician and CT of the chest.
Lung biopsy is a highly invasive intervention and should not be undertaken to confirm the diagnosis of pulmonary fibrosis due to welding fume unless there are sound clinical reasons for undertaking the procedure and the risks are significantly outweighed by the benefits. Ideally, an open lung biopsy rather than a transbronchial biopsy is required, but the decision should be dictated by the clinical situation and access to appropriate expert advice. If a lung biopsy is clinically indicated, histological analysis should be supplemented by mineralogical assessment of lung tissue to assess welding fume, iron, silica and asbestos.
The welder will need clinical follow-up, as the diagnosis may need to be revised in the light of changes in the health of the welder with time.
Occupational management will depend on many factors but may require the removal of the welder from exposure, or at the very least, scrupulous use of effective local extraction together with a powered air-purifying respirator to limit the exposure to welding fume to less than 1 mg m−3. A formal assessment of the other members of the workforce should automatically be undertaken by the occupational health/occupational hygiene team and a full review of the control of fume within the workplace and action taken to reduce the exposure levels to at least national standards by management and the occupational hygienist.
5.1 A typical case of pulmonary fibrosis due to steel welding fume
The typical clinical history for a case of pulmonary fibrosis due to welding fume will be as follows. The welder may complain of dyspnoea (shortness of breath) and less frequently a cough or may be a symptom-free welder with an abnormal chest X-ray. They may or may not be a smoker. Exposure assessment would be expected to find that the welder was exposed to high levels of fume, for a significant duration, often in confined spaces without using effective extraction or respiratory protection. On examination, the clinician will very rarely find evidence of clubbing but may find crackles at the bases. Spirometry may be abnormal and may demonstrate obstructive, restrictive or mixed changes. The residual volume is likely to be raised. Transfer factor may be significantly reduced. Chest X-ray findings do not correlate with clinical findings but may occasionally demonstrate conglomeration or progressive massive fibrosis or evidence of pneumoconiosis related to iron exposure. High-resolution CT scans may show ground-glass opacities in symptomatic welders, but such changes are not usually found in asymptomatic welders. Histology of the lung, should it be undertaken, shows alveolar and interstitial macrophages and pulmonary fibrosis, as described above. Areas of patchy pulmonary fibrosis are strongly correlated with welding fume deposition on mineralogical analysis of the histological specimen, but there is no evidence of the presence of crystalline silica or asbestos. Once the welder is withdrawn from exposure, the condition does not, as a rule, progress in simple fibrosis due to welding fume.
6 Further research
Several areas of further work are required on this topic:
6.1 How do we best define and diagnose pulmonary fibrosis from welding fume and how do we distinguish it from other occupational and clinical causes?
There is a need for further international discussion regarding the existence of pulmonary fibrosis due to welding fume as a diagnosis with the development of consensus on the appropriate case definitions and distinguishing features of clinical and occupational causes of pulmonary fibrosis in relation to welding fume. The logical starting point would be the current German model [28]. Given the rarity of the condition and the difficulties in making the diagnosis, it may be that international reference histopathology laboratories dealing in pulmonary fibrosis could be established that could lead in both histological and mineralogical assessment and research in this area.
6.2 What is the aetiology of pulmonary fibrosis in welders?
There are many potential agents that could cause pulmonary fibrosis in welders including components of the fume (complex spinels of iron manganese oxides, soluble hexavalent chromium, titanium or manganese compounds) and gases (oxides of nitrogen, ozone) [49]. Other than hexavalent chromium, it is far from clear what the most likely cause of pulmonary fibrosis in welders might be, but hexavalent chromium does not explain all of the cases. It is not likely to be the iron-manganese oxide spinel which may simply be a marker of exposure. It is most likely to be a soluble element of the fume. It has been suggested that one component of the gases, particularly oxides of nitrogen, may play a part; however, this would not explain the close relationship with particles in the lungs and surrounding fibrosis and exposure to nitrogen dioxide results in a different clinical presentation of disease and pathology, namely bronchiolitis obliterans. Only one case in the literature is of this histological pattern [68]. Further research on the material science of the fume and gases itself rather than concentrating on purely the elemental composition of fume is likely to be rewarding. Such research needs to consider the potential synergistic effects of both the fumes and the gases produced in welding and the changes in the fume oxidation state and surface charge with time.
6.3 What is the interaction of welding fume and host factors such as smoking in the generation of pulmonary fibrosis?
With regards to host factors, firstly there is likely to be a synergistic effect of smoking and welding fume in the genesis of pulmonary fibrosis. Smoking is a significant risk factor for pulmonary fibrosis and is a very common habit among welders. Secondly, if emphysema is present in addition to pulmonary fibrosis, is this related to smoking or welding fume, or is there an interaction between the two? It is thought unlikely that genetics will turn out to be a major component, but with the current rapid progress in our understanding of the interaction between genes and occupational exposures in the genesis of occupational disease, it is wise to keep an open mind about this.
6.4 Does pulmonary fibrosis due to welding fume increase the subsequent risk of infection?
Many of the case reports and case series make mention of tuberculosis (TB) [22, 24, 26, 48, 50, 52, 56, 66, 76, 77, 82, 109, 110] although early commentators thought that there was no link between pulmonary fibrosis due to welding fume and the subsequent development of TB [24]. Given that other forms of pulmonary fibrosis due to occupational exposures such as silicosis are associated with TB and that there is an adverse effect of welding fume on macrophage function, it would not be a surprise if pulmonary fibrosis due to welding fume increased the risk of reactivation of latent tuberculosis. Whether this might be related to pulmonary fibrosis or macrophage dysfunction is worth investigating.
It is well recognised that pneumonia is more common in welders [111], half of the cases being from pneumococcal disease which can also present as meningitis [112]. The risk of pneumonia falls to background levels on cessation of welding fume exposure [113] and therefore cannot be related to underlying pulmonary fibrosis.
6.5 Does pulmonary fibrosis in welders account for the unexplained increased risk of lung cancer?
There is an epidemiological link between welding and lung cancer that remains unexplained [114–116]. Pulmonary fibrosis (including respiratory bronchiolitis), also increases the risk of lung cancer [117, 118] although the link may not be causal. There are very few cases of lung cancer described in the current literature in cases of pulmonary fibrosis due to welding fume [76, 77, 85, 95], but this may be due to lack of follow-up. This warrants further investigation, firstly by following up welders with known pulmonary fibrosis, secondly by formal assessment of lung cancer specimens in welders looking for evidence of fibrosis such as respiratory bronchiolitis in the surrounding non-cancerous tissue and thirdly factoring in lung fibrosis and cumulative exposure estimates to the epidemiological studies on lung cancer and welders.
6.6 Nomenclature
Finally, it is suggested that the term siderofibrosis is abandoned for the sake of consensus and to avoid confusion, as it remains contentious as to whether iron plays any part in the development of fibrosis. Likewise, arc welder’s lung is a non-specific term and should no longer be used. We prefer the descriptive term “pulmonary fibrosis due to prolonged exposure to welding fume at high concentration”.
7 Conclusion
Arc welding of steels is associated with occasional cases of pulmonary fibrosis when the welder is exposed for a significant period of time and at high concentrations. We would like to reinforce the advice already provided to the welding industry on careful control of welding fume to minimise exposure at the workplace, particularly in confined spaces, and strongly reinforce the advice already provided by Commission VIII that welders should not smoke.
References
Cosgrove MP (2015) Arc welding and airway disease. Weld World 59:1–7
Nagelschmidt G (1960) The relation between lung dust and lung pathology in pneumoconiosis. Br J Ind Med 17:247–59
Kelleher P, Pacheco K, Newman LS (2000) Inorganic dust pneumonias: the metal-related parenchymal disorders. Environ Health Perspect 108(Suppl 4):685–96
Nemery B (1990) Metal toxicity and the respiratory tract. Eur Respir J 3(2):202–19
Yoshida T, Ohnuma A, Horiuchi H, Harada T (2011) Pulmonary fibrosis in response to environmental cues and molecular targets involved in its pathogenesis. J Toxicol Pathol 24(1):9–24
Doig AT, McLaughlin AIG.: X-ray appearances of the lungs of electric arc welders. Lancet 1936;i:771–5.
Enzer N, Sander OA (1938) Chronic lung changes in electric arc welders. J Ind Hyg 20:333
Harding HE, McLaughlin AIG, Doig AT (1958) Clinical, radiographic, and pathological studies of the lungs of electric-arc and oxyacetylene welders. Lancet 2(7043):394–9
Harding HE, Grout JL, Davies TA (1947) The experimental production of X-ray shadows in the lungs by inhalation of industrial dusts; iron oxide. Br J Ind Med 4(4):223, 232
Doig AT, Challen PJ (1964) Respiratory hazards in welding. Ann Occup Hyg 7:223–31
Schuler P, Maturana V, Cruze E, Guijon C, Vasquez A, Valenzuela A, Silvar R (1962) Arc welder’s pulmonary siderosis. J Occup Med 4:353–8
Beaumont JJ, Weiss NS (1980) Mortality of welders, shipfitters, and other metal trades workers in boilermakers Local No. 104, AFL-CIO. Am J Epidemiol 112(6):775–86
Sjogren B (1980) A retrospective cohort study of mortality among stainless steel welders. Scand J Work Environ Health 6(3):197–200
Polednak AP (1981) Mortality among welders, including a group exposed to nickel oxides. Arch Environ Health 36(5):235–42
Newhouse ML, Oakes D, Woolley AJ (1985) Mortality of welders and other craftsmen at a shipyard in NE England. Br J Ind Med 42(6):406–10
Moulin JJ, Wild P, Haguenoer JM, Faucon D, De GR, Mur JM, Mereau M, Gary Y, Toamain JP, Birembaut Y (1993) A mortality study among mild steel and stainless steel welders. Br J Ind Med 50(3):234–43
Steenland K (2002) Ten-year update on mortality among mild-steel welders. Scand J Work Environ Health 28(3):163–7
Zober A, Kaduk B, Schaller KH (1983) Lungenfibrose eines Elektroschweißers. Kasuistik und versicherungsrechtlichte Bewertungskriterien [Pulmonary fibrosis in an electric welder—case report and legal criteria]. Zentralbl Arbeitsmed Arbeitsschutz Prophyl Ergonomie 33(4):116–20
Zober A (1981) Symptome und Befunde am bronchopulmonalen System bei Elektroschweißern. 2. Mitteilung: Lungenfibrosen. [Symptoms and findings at the bronchopulmonary system of electric arc welders. II. Communication: pulmonary fibrosis]. Zentralbl Bakteriol Mikrobiol Hyg B 173(1–2):120–48
Sano T (1963) Pathology and pathogenesis of pneumoconiosis. Acta Pathol Jpn 13:77–93
Takigawa T, Kishimoto T, Nabe M, Nishide T, Wang DH, Seki A, Uchida G, Kira S (2002) The current state of workers’ pneumoconiosis in relationship to dusty working environments in Okayama Prefecture. Japan Acta Med Okayama 56(6):303–8
Slepicka J, Kadlec K, Tesar Z, Skoda V, Mirejovsky P (1970) Beitrag zur Problematik der Elektroschweißerpneumokoniose [Problems of electric welder’s pneumoconiosis.]. Int Arch Arbeitsmed 27(3):257–80
Marek K, Starzynski Z (1994) Pneumoconioses in Poland. Int J Occup Med Environ Health 7(1):13–21
Charr R (1953) Respiratory disorders among welders. J Am Med Assoc 152(16):1520–2
Charr R (1954) Nontuberculous pulmonary disease: respiratory disorders among welders. Trans Annu Meet Natl Tuberc Assoc 96(50th Meeting):208–11
Charr R (1955) Respiratory disorders among welders. Am Rev Tuberc 71(6):877–84
Charr R (1956) Pulmonary changes in welders: a report of three cases. Ann Intern Med 44(4):806–12
Bundesministerium für Arbeit und Soziales (BMAS) [Federal Ministry of Labour and Social Affaires]: Wissenschaftliche Begründung zur Berufskrankheit Nummer 4115. Lungenfibrose durch extreme und langjärige Einwirkung von Schweißrauchen und Schweißgasen - (Siderofibrose) [Scientific Rationale of Occupational Disease No. 4115. Lung fibrosis due to extreme prolonged exposure to welding fume and gases]. Bek. des BMAS [Notification of the BMAS] vom 1.September 2006 4-45222-4113. Bundesarbeitsblatt 2006 Oct;35–67
Hicks R, Al-Shamma KJ, Lam HF, Hewitt PJ (1983) An investigation of fibrogenic and other toxic effects of arc-welding fume particles deposited in the rat lung. J Appl Toxicol 3(6):297–306
Kalliomaki PL, Hyvarinen HK, Aitio A, Lakoma EL, Kalliomaki K (1986) Kinetics of the metal components of intratracheally instilled stainless steel welding fume suspensions in rats. Br J Ind Med 43(2):112–9
Antonini JM, Krishna Murthy GG, Rogers RA, Albert R, Ulrich GD, Brain JD (1996) Pneumotoxicity and pulmonary clearance of different welding fumes after intratracheal instillation in the rat. Toxicol Appl Pharmacol 140(1):188–99
Antonini JM, Clarke RW, Krishna Murthy GG, Sreekanthan P, Jenkins N, Eagar TW, Brain JD (1998) Freshly generated stainless steel welding fume induces greater lung inflammation in rats as compared to aged fume. Toxicol Lett 98(1–2):77–86
Antonini JM, Taylor MD, Millecchia L, Bebout AR, Roberts JR (2004) Suppression in lung defense responses after bacterial infection in rats pretreated with different welding fumes. Toxicol Appl Pharmacol 200(3):206–18
McNeilly JD, Jimenez LA, Clay MF, MacNee W, Howe A, Heal MR, Beverland IJ, Donaldson K (2005) Soluble transition metals in welding fumes cause inflammation via activation of NF-kappaB and AP-1. Toxicol Lett 158(2):152–7
Kalliomaki PL, Tuomisaari M, Lakomaa EL, Kalliomaki K, Kivela R (1983) Retention and clearance of stainless steel shieldgas welding fumes in rat lungs. Am Ind Hyg Assoc J 44(9):649–54
Kalliomaki PL, Lakomaa E, Kalliomaki K, Kiilunen M, Kivela R, Vaaranen V (1983) Stainless steel manual metal arc welding fumes in rats. Br J Ind Med 40(2):229–34
Taylor MD, Roberts JR, Leonard SS, Shi X, Antonini JM (2003) Effects of welding fumes of differing composition and solubility on free radical production and acute lung injury and inflammation in rats. Toxicol Sci 75(1):181–91
Antonini JM, Taylor MD, Zimmer AT, Roberts JR (2004) Pulmonary responses to welding fumes: role of metal constituents. J Toxicol Environ Health A 67(3):233–49
Antonini JM, Stone S, Roberts JR, Chen B, Schwegler-Berry D, Afshari AA, Frazer DG (2007) Effect of short-term stainless steel welding fume inhalation exposure on lung inflammation, injury, and defense responses in rats. Toxicol Appl Pharmacol 223(3):234–45
Leonard SS, Chen BT, Stone SG, Schwegler-Berry D, Kenyon AJ, Frazer D, Antonini JM (2010) Comparison of stainless and mild steel welding fumes in generation of reactive oxygen species. Part Fibre Toxicol 7:32
Antonini JM, Roberts JR, Stone S, Chen BT, Schwegler-Berry D, Chapman R, Zeidler-Erdely PC, Andrews RN, Frazer DG (2010) Persistence of deposited metals in the lungs after stainless steel and mild steel welding fume inhalation in rats. Arch Toxicol 6
Antonini JM, Lawryk NJ, Murthy GG, Brain JD (1999) Effect of welding fume solubility on lung macrophage viability and function in vitro. J Toxicol Environ Health A 58(6):343–63
Stern RM, Pigott GH (1983) In vitro RPM fibrogenic potential assay of welding fumes. Environ Health Perspect 51:231–6
Solano-Lopez C, Zeidler-Erdely PC, Hubbs AF, Reynolds SH, Roberts JR, Taylor MD, Young SH, Castranova V, Antonini JM (2006) Welding fume exposure and associated inflammatory and hyperplastic changes in the lungs of tumor susceptible a/j mice. Toxicol Pathol 34(4):364–72
Sung JH, Choi BG, Maeng SH, Kim SJ, Chung YH, Han JH, Song KS, Lee YH, Cho YB, Cho MH, Kim KJ, Hyun JS, Yu IJ (2004) Recovery from welding-fume-exposure-induced lung fibrosis and pulmonary function changes in sprague dawley rats. Toxicol Sci 82(2):608–13
Antonini JM, Roberts JR, Chapman RS, Soukup JM, Ghio AJ, Sriram K (2010) Pulmonary toxicity and extrapulmonary tissue distribution of metals after repeated exposure to different welding fumes. Inhal Toxicol 22(10):805–16
Yu IJ, Song KS, Chang HK, Han JH, Kim KJ, Chung YH, Maeng SH, Park SH, Han KT, Chung KH, Chung HK (2001) Lung fibrosis in Sprague–Dawley rats, induced by exposure to manual metal arc-stainless steel welding fumes. Toxicol Sci 63(1):99–106
Attfield MD, Ross DS (1978) Radiological abnormalities in electric-arc welders. Br J Ind Med 35(2):117–22
Stern RM (1981) Process-dependent risk of delayed health effects for welders. Environ Health Perspect 41:235–53
Ekici A, Bilgili Y, Ekici M, Unal B, Akin A, Erdal H, Arslan M, Kocyigit P (2006) High-resolution computed tomography findings in arc-welders. Turkish Respiratory J 7(2):52–5
Tutkun E, Abusoglu S, Yilmaz H, Gunduzoz M, Evcik E, Ozis TN, Keskinkilic B, Unlu A (2014) Farewell to an old friend: chest X-ray vs high-resolution computed tomography in welders’ lung disease. Clin Respir J 8(2):220–4
Han D, Goo JM, Im JG, Lee KS, Paek DM, Park SH (2000) Thin-section CT findings of arc-welders’ pneumoconiosis. Korean J Radiol 1(2):79–83
Yoshii C, Matsuyama T, Takazawa A, Ito T, Yatera K, Hayashi T, Imanaga T, Kido M (2002) Welder’s pneumoconiosis: diagnostic usefulness of high-resolution computed tomography and ferritin determinations in bronchoalveolar lavage fluid. Intern Med 41(12):1111–7
Akira M (1995) Uncommon pneumoconioses: CT and pathologic findings. Radiology 197(2):403–9
Akira M (2002) High-resolution CT in the evaluation of occupational and environmental disease. Radiol Clin North Am 40(1):43–59
Mann BT, Lecutier ER (1957) Arc-welders' lung. Br Med J 2(5050):921–2
Friede E, Rachow DO (1961) Symptomatic pulmonary disease in arc welders. Ann Intern Med 54:121–7
Angervall L, Hansson G, Rockert H (1960) Pulmonary siderosis in electrical welder. A note on pathological appearances. Acta Pathol Microbiol Scand 49:373–92
Fabre M, Marais M, Ladouch A, Paillas J, Blanchon P (1976) quillard J.: La pneumoconiose des soudeurs a l'arc. Arch Anat Cytol Pathol 24(6):481–5
Guidotti TL, Abraham JL, DeNee PB, Smith JR (1978) Arc welders’ pneumoconiosis: application of advanced scanning electron microscopy. Arch Environ Health 33(3):117–24
Kalliomaki PL, Sutinen S, Kelha V, Lakomaa E, Sortti V, Sutinen S (1979) Amount and distribution of fume contaminants in the lungs of an arc welder post mortem. Br J Ind Med 36(3):224–30
Barth J, Holtmann B, Muller KM (1986) Alveolar-septale Fibrose und systemische Eisenbelastung bei einem Schweißer [Interstitial pulmonary siderofibrosis and increased systemic iron level in an arc welder]. Atemw-Lungenkrkh 7:290–3
Wagner U, Meerbach W, Fischer W, Otto J, Jahn R, Schneider WD (1990) Kasuistischer Beitrag zur Schweißerlunge [A case report of welder’s lung]. Z Erkr Atmungsorgane 174(2):149–54
Steurich F, Feyerabend R (1997) Sidero-Fibrose der Lungen nach jahrzehntelangem Elektroschweißen [Sidero-fibrosis of the lungs after decades of arc welding]. Pneumologie 51(6):545–9
Yamada G, Igarashi T, Sonoda H, Morita S, Suzuki K, Yoshida Y, Abe S (1998) Use of bronchopulmonary lavage for eliminating inhaled fume particles from a patient with arc welder's lung. Intern Med 37(11):962–4
Scharrer E, Bittmann I, Behr J, Nowak D (2003) Siderofibrose, atypische Mykobacteriose und Lungentransplantation bei einem Behälterschweißer [Siderofibrosis, MOTT, and lung transplantation in a worker welding in confined spaces]. Pneumologie 57(1):15–8
Ishida Y, Sera K, Ohta K, Kageshita T (2003) A case of rapid development of arc welder’s lung during the course of a year. Nihon Kokyuki Gakkai Zasshi 41(5):351–5
Mendez JL, Rabatin JT, Cassivi SD (2004) Bilateral pulmonary nodules in a welder with a 90 pack year history of smoking. Chest 996S
Fidan F, Esme H, Unlu M, Acar M, Albayrak R, Dilek FH (2005) Welder’s lung associated with pneumothorax. J Thorac Imaging 20(2):120–2
McCormick LM, Goddard M, Mahadeva R (2008) Pulmonary fibrosis secondary to siderosis causing symptomatic respiratory disease: a case report. J Med Case Rep 2:257
Khalid I, Khalid TJ, Jennings JH (2009) A welder with pneumosiderosis: a case report. Cases J 2:6639
Modrykamien A, Christie H, Farver C, Ashton RW (2009) A 38-year-old welder with dyspnea and iron overload. Chest 136(1):310–3
Roshan R, Guptal M, Kulshrestha R, Menon B, Chhabra SK (2012) Combined pulmonary fibrosis and emphysema in a welder. Monaldi Arch Chest Dis 77(1):26–8
Antonini JM, Roberts JR, Schwegler-Berry D, Mercer RR.: Comparative Microscopic Study of Human and Rat Lungs After Overexposure to Welding Fume. Ann Occup Hyg 2013 Jun 24
Schuler P (1962) Arc welder’s pulmonary siderosis. J Occup Med 4:353–8
Einbrodt HJ, Maass W, Josten HG, Stecher W (1971) Untersuchungen über die Lungenveränderungen bei Elektroschweißern [Studies of pulmonary changes in electric welding workers]. Öffentl Gesundheitswes 33(5):286–99
Irmscher G, Beck B, Ahlendorf W, Anspach M, Konetzke G, Ludwig V, Sturm W (1975) Erfahrungen bei der Begutachtung von fraglichen Lungenfibrosen durch Einwirkung von Schweißrauchen [Experience gathered in assessing doubtful fibrosis of the lung caused by welding fume]. Z Gesamte Hyg 21(7):562–6
Morgan WK (1962) Arc-welders’ lung complicated by conglomeration. Am Rev Respir Dis 85:570–5
Kinoshita M, Hanzawa S, Momiki S, Sasaki K, Hashizume I, Kasamatsu N, Nakamura A, Shirai T, Ozawa T (1997) A case of pneumoconiosis (welder’s lung) suspected to be lung cancer. Nihon Kyobu Shikkan Gakkai Zasshi 35(10):1124–31
Yokoyama T, Aoshima M, Kurakawa E, P J, Kasuga I, Minemura K, Ohyashiki K (2005) A case of arc welder’s lung with ground-glass opacities and progressive massive fibrosis. Nihon Kokyuki Gakkai Zasshi 43(5):302–7
Ji C, Chen G, Cai HR, Meng FQ, Chen YB, Guo LC, Huang JA, Ling CH (2012) An unusual case of Welder’s siderosis with local massive fibrosis: a case report. Chin Med J (Engl ) 125(3):552–4
Morgan KCM, Kerr HD (1963) Pathologic and physiologic studies of welder’s siderosis. Ann Intern Med 55:293–304
Stettler LE, Groth DH, MacKay GR (1977) Identification of stainless steel welding fume particulates in human lung and environmental samples using electron probe microanalysis. Am Ind Hyg Assoc J 38(2):76–82
Burger A, Philippou X.: Electronenmikroskopische Befunde zur Pathogenese der sogenannten Schweißerlunge. [Electron microscopic findings with respect to the pathogenesis of so-called welder's lung]. Berichte Pathologie 1977;104:447.
Stern RM, Pigott GH, Abraham JL (1983) Fibrogenic potential of welding fumes. J Appl Toxicol 3(1):18–30
Morgenroth K, Verhagen-Schröter G (1984) Licht - und electronenmikroskopische Untersuchungen und energiedispersive Röntgenmikroanalyse an Biopsiematerial zur Pathogenese der Schweißerlunge [Light and electron microscopic examination and energy dispersive radiologic microanalysis of biopsy specimens for the pathogenesis of arc-welder’s lung]. Atemw-Lungenkrkh 10:451–6
Stanulla H, Liebetrau G (1984) Die Elektroschweißerlunge [Electric welder’s lung]. Prax Klin Pneumol 38(1):14–8
Funahashi A, Schlueter DP, Pintar K, Bemis EL, Siegesmund KA (1988) Welders' pneumoconiosis: tissue elemental microanalysis by energy dispersive x ray analysis. Br J Ind Med 45(1):14–8
Radenbach D, Nowak D, Jörres R, Magnussen H (1995) Untersuchungsergsergebnisse bei 30 symptomatischen Schweißern [Medical findings in 30 symptomatic welders]. Atemw-Lungenkrkh 21:105–11
Rösler J, Morgenroth K, Müller KM, Woitowitz HJ.: Lungenfibrosen nach langjähriger Einwirkung von Schweißrauchen [Lung fibroses after long-time exposure to welding fumes]. In: Schiele R, Beyer B, Petrovitch A (Hrsg) [eds]: Verh Dtsch Ges Arbeitsmed Umweltmed. [Proceedings of the Annual Assembly of the German Society of Occupational Medicine and Environmental Medicine]. 1995;35:285–8, Rindt-Druck [Rindt-Publishers], Fulda.
Müller KM, Verhoff MA (2000) Graduierung von Sideropneumokoniosen [Gradation of sideropneumoconiosis]. Pneumologie 54(8):315–7
Verhoff MA, Müller KM (2000) Sideroelastose der Pulmonalgefäße nach Schweißrauchexposition [Sideroelastosis of pulmonary vessels after welder dust exposure]. Pathologe 21(3):229–33
Buerke U, Schneider J, Müller KM, Woitowitz HJ (2003) Schweißerlungenfibrose: Begründung fuer die Aufnahme als neue Berufskrankheit [Interstitial pulmonary siderofibrosis: requirements for acceptance as new occupational disease]. Pneumologie 57(1):9–14
Doherty MJ, Healy M, Richardson SG, Fisher NC (2004) Total body iron overload in welder’s siderosis. Occup Environ Med 61(1):82–5
Buerke U, Schneider J, Rosler J, Woitowitz HJ (2002) Interstitial pulmonary fibrosis after severe exposure to welding fumes. Am J Ind Med 41(4):259–68
Cosgrove MP (2015) Pulmonary fibrosis and exposure to steel welding fume. Occup Med (Lond) 65:706--712
Scott J, Johnston I, Britton J (1990) What causes cryptogenic fibrosing alveolitis? A case–control study of environmental exposure to dust. BMJ 301(6759):1015–7
Iwai K, Mori T, Yamada N, Yamaguchi M, Hosoda Y (1994) Idiopathic pulmonary fibrosis. Epidemiologic approaches to occupational exposure. Am J Respir Crit Care Med 150(3):670–5
Baumgartner KB, Samet JM, Coultas DB, Stidley CA, Hunt WC, Colby TV, Waldron JA (2000) Occupational and environmental risk factors for idiopathic pulmonary fibrosis: a multicenter case–control study. Collaborating Centers Am J Epidemiol 152(4):307–15
Miyake Y, Sasaki S, Yokoyama T, Chida K, Azuma A, Suda T, Kudoh S, Sakamoto N, Okamoto K, Kobashi G, Washio M, Inaba Y, Tanaka H (2005) Occupational and environmental factors and idiopathic pulmonary fibrosis in Japan. Ann Occup Hyg 49(3):259–65
Taskar VS, Coultas DB (2006) Is idiopathic pulmonary fibrosis an environmental disease? Proc Am Thorac Soc 3(4):293–8
Pinheiro GA, Antao VC, Wood JM, Wassell JT (2008) Occupational risks for idiopathic pulmonary fibrosis mortality in the United States. Int J Occup Environ Health 14(2):117–23
Fireman EM, Lerman Y, Ben MM, Ganor E, Kramer MR (2007) Redefining idiopathic interstitial lung disease into occupational lung diseases by analysis of chemical composition of inhaled dust particles in induced sputum and/or lung biopsy specimens. Toxicol Ind Health 23(10):607–15
Abraham JL, Hertzberg MA (1981) Inorganic particulates associated with desquamative interstitial pneumonia. Chest 80(1 Suppl):67–70
Nasr MR, Savici D, Tudor L, Abou AD, Newman N, Abraham JL (2006) Inorganic dust exposure causes pulmonary fibrosis in smokers: analysis using light microscopy, scanning electron microscopy, and energy dispersive X-ray spectroscopy. Arch Environ Occup Health 61(2):53–60
Godbert B, Wissler MP, Vignaud JM (2013) Desquamative interstitial pneumonia: an analytic review with an emphasis on aetiology. Eur Respir Rev 22(128):117–23
Monso E, Tura JM, Marsal M, Morell F, Pujadas J, Morera J (1990) Mineralogical microanalysis of idiopathic pulmonary fibrosis. Arch Environ Health 45(3):185–8
Monso E, Tura JM, Pujadas J, Morell F, Ruiz J, Morera J (1991) Lung dust content in idiopathic pulmonary fibrosis: a study with scanning electron microscopy and energy dispersive x ray analysis. Br J Ind Med 48(5):327–31
Sander OA (1944) Further observations on lung changes in electric arc welders. J Ind Hyg Toxicol 26:79–85
Meyer EC, Kratzinger SF, Miller WH (1967) Pulmonary fibrosis in an arc welder. Arch Environ Health 15(4):462–9
Palmer KT, Cosgrove MP (2012) Vaccinating welders against pneumonia. Occup Med (Lond) 62(5):325–30
Wong A, Marrie TJ, Garg S, Kellner JD, Tyrrell GJ (2010) Welders are at increased risk for invasive pneumococcal disease. Int J Infect Dis 14(9):e796–e799
Palmer KT, Poole J, Ayres JG, Mann J, Burge PS, Coggon D (2003) Exposure to metal fume and infectious pneumonia. Am J Epidemiol 157(3):227–33
Kendzia B, Behrens T, Jockel KH, Siemiatycki J, Kromhout H, Vermeulen R, Peters S, Van GR, Olsson A, Bruske I, Wichmann HE, Stucker I, Guida F, Tardon A, Merletti F, Mirabelli D, Richiardi L, Pohlabeln H, Ahrens W, Landi MT, Caporaso N, Consonni D, Zaridze D, Szeszenia-Dabrowska N, Lissowska J, Gustavsson P, Marcus M, Fabianova E, Pearce N, Tse LA, Yu IT, Rudnai P, Bencko V, Janout V, Mates D, Foretova L, Forastiere F, McLaughlin J, Demers P, Bueno-de-Mesquita B, Boffetta P, Schuz J, Straif K, Pesch B, Bruning T (2013) Welding and lung cancer in a pooled analysis of case–control studies. Am J Epidemiol 178(10):1513–25
Ambroise D, Wild P, Moulin JJ (2006) Update of a meta-analysis on lung cancer and welding. Scand J Work Environ Health 32(1):22–31
Moulin JJ (1997) A meta-analysis of epidemiologic studies of lung cancer in welders. Scand J Work Environ Health 23(2):104–13
Yamada Y, Terada J, Tatsumi K, Kono C, Tanno M, Takemura T, Yamaguchi T (2013) Respiratory bronchiolitis and lung carcinoma. Respir Investig 51(3):184–90
Harris JM, Johnston IDA, Rudd R, Newman Taylor AJ, Cullinan P (2010) Cryptogenic fibrosing alveolitis and lung cancer: the BTS study. Thorax 65(1):70–76
Acknowledgements
The authors would like to thank all the members of Commission VIII of the International Institute of Welding and Paul Cullinan for their tremendous support, advice and cooperation in developing and writing this document. We would also like to thank Paul Stevenson and the British Library for their help with undertaking the literature search and obtaining the papers.
Author information
Authors and Affiliations
Corresponding author
Additional information
Recommended for publication by Commission VIII - Health, Safety, and Environment
Rights and permissions
About this article
Cite this article
Cosgrove, M., Zschiesche, W. Arc welding of steels and pulmonary fibrosis. Weld World 60, 191–199 (2016). https://doi.org/10.1007/s40194-015-0283-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40194-015-0283-7