Abstract
Purpose of Review
Von Hippel-Lindau disease is a multiple neoplasia syndrome that encompasses uncommon tumor types including hemangioblatoma, pheochromocytoma, renal cancer, and pancreatic neuroendocrine tumors. The disease is highly variable, and a review of the literature reinforces the need for referral for genetic risk assessment and counseling when a patient has any component tumor.
Recent Findings
Research from registry-based von Hippel-Lindau disease (VHL) populations provides new evidence of the benefits of patient compliance with close surveillance, the significantly younger age of renal cancer compared to the US population, evidence that pregnancy may not trigger new hemangioblastomas, and that the rate of new tumor growth is age and genotype dependent with the highest rates occurring between 30 and 34 years. Testing for somatic mosaicism has not moved from research to the clinical realm despite the known clinical implications for patients. Qualitative research supports observations that patients attribute stories of resilience to their medical experiences, while they also endorse that greater support is needed to help them cope with VHL-related distress.
Summary
The breadth of considerations in risk assessment, genetic testing, and psychosocial issues for VHL patient across the lifespan is described.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Von Hippel-Lindau disease is an autosomal dominant tumor susceptibility condition that affects multiple-organ systems. The disease is pan-ethnic and estimated incidence is 1 in 36,000 worldwide. Von Hippel-Lindau disease (VHL) is highly penetrant with a >90% chance of developing at least one characteristic tumor by age 65: hemangioblastoma (HMB) of the retina, brain, or spine; endolymphatic sac tumor (ELST); pheochromocytoma or paraganglioma (PHEO or PGL); clear cell renal cell carcinoma (ccRCC); and pancreatic neuroendocrine tumor (PNET). Additional features include cystadenomas of the epididymis, broad ligament, and pancreas and cysts of the kidneys and pancreas [1]. Retinal (25–60%) and cerebellar HMB (60–80%) are the most frequent finding in patients with VHL, often developing more than one primary HMB over the course of their lifetime [1, 2].
Positional cloning of the VHL gene in 1993 has permitted definitive establishment of a VHL diagnosis in affected index patients and identification of family members at risk for the disease through genetic testing [3]. The VHL gene is located on chromosome 3p25-26 and is a tumor suppressor gene expressed in all tissues of the body. Biallelic inactivation of the VHL gene is known to be an early driver in both VHL-associated and sporadic ccRCC, and the elucidation of the role of pVHL in tumorigenesis has led to major strides in the development of therapies to treat metastatic disease [4,5,6,7]. Under normoxic conditions, pVHL binds with elongin B, elongin C, Cullin2, and Rbx1, and the complex targets the hypoxia-inducible factors HIF-1α and HIF-2α for ubiquitin-mediated degradation. The HIF-1α and HIF-2α genes, along with HIF-3α, encode the α subunit of the hypoxia-inducible factor (HIF) heterodimer. Loss of pVHL function in renal tumors simulates low tissue oxygen levels or “pseudohypoxia” where HIF-1α and HIF-2α accumulate causing upregulation of many genes involved in tumorigenesis such as vascular endothelial growth factor (pro-angiogenesis), epidermal growth factor receptor (cell-proliferation and survival), and glucose transporter 1 (regulation of glucose uptake) [8•]. Gossage et al. provide a superbly thorough historical review of the VHL gene from cloning to protein function and the landscape of targeted therapy.
Clinical Features
A clinical diagnosis of VHL disease can be made in an individual with a family history of VHL and one VHL component tumor, or when an individual presents with two or more HMB, or one HMB plus RCC, PHEO/PGL, or PNET [1]. These clinical criteria are useful for diagnosing new cases; however, confirmation with genetic testing is highly desirable. Identification of a pathogenic VHL mutation allows for further characterization of the phenotype as a correlation exists between genotype and phenotype (Table 1). Identification of the pathogenic mutation also permits presymptomatic identification of mutation carriers in the family and exonerates non-carriers from unnecessary screening.
The disease has high penetrance with >90% probability of at least one component feature, hence the reliability of establishing a diagnosis when an at-risk member of a VHL family based on clinical grounds alone once a component tumor is detected. However, the disease is also highly variable even within a family, so disease course and severity cannot be accurately or reliably predicted based on mutation type or family history. Penetrance estimates are more useful in counseling presymptomatic mutation carriers in that an explanation of the high likelihood of manifestations of the disease improves patient understanding of the need for surveillance.
The estimated de novo rate in VHL is ∼20%, and such cases pose a diagnostic challenge in two important ways. First, an absence of family history renders an index case to appear as a sporadic presentation and a genetic evaluation may not necessarily be considered, putting a de novo case of VHL at risk of diagnostic delay. Most de novo cases to date have been suspected and diagnosed on the grounds of two or more component tumors, and given that these tumors often present metachronously, a diagnostic delay is highly likely and potentially harmful to the patient. A delay of 3 or more years has been observed when patients are referred for genetic risk assessment after the diagnosis of a second component tumor. A case scenario (that we have seen a few times) is when a patient presents with a PHEO as the first tumor and is not evaluated for VHL, receives treatment and follow-up for the PHEO, and several years later presents with the neurologic symptoms of an HMB. The second challenge in de novo cases is defining whether the patient is truly the first in the family to have VHL, where the mutation arose in the parental egg or sperm or within the first few cell divisions after fertilization or whether one parent is mosaic. In parental mosaicism, both parents may test negative on peripheral blood sampling for their child’s VHL mutation; however, one parent may harbor mosaicism in the germ cells. Mosaicism is known to occur in VHL disease and is estimated to represent at least 5% of cases although this may be under-recognized due to the technical challenges of identifying mosaicism through currently available genetic tests and poses additional challenges to identifying which family members (i.e., parent and siblings) are truly at risk of developing disease manifestations. Additional guidance on genetic risk assessment for subtle or variant presentations is discussed in the next section.
Over 200 VHL mutations have been reported in the literature, and genotype-phenotype correlations are described in Table 1. All genotypes are associated with HMB; however, the risk of ccRCC and PHEO can vary accordingly to genotype. Mutations that severely affect protein function such as deletions, non-sense mutations, and small deletions/insertions are associated with type 1 phenotype with a lower risk of PHEO and high risk of ccRCC. Missense mutations that cause defects in protein structure are also associated with a type 1 phenotype. The majority of type 2 mutations are missense mutations that result in an amino acid substitution on the surface of VHL protein and carry a high risk of PHEO and varying degrees of risk of RCC. Genotype-phenotype correlations are useful from the academic standpoint but cannot be relied upon clinically to dictate surveillance as exceptions have been observed. One case example from our clinic is a three-generation family harboring a partial VHL deletion in the germline with three members diagnosed with PHEO. The predicted phenotype in this family is type 1; however, the PHEO rate in the family is high. Such observations underscore the limited clinical utility of genotype-phenotype correlations and the current consensus that VHL patients should be followed with surveillance of all target organ systems [9, 10].
Genetic Testing Considerations
Patients meeting clinical diagnostic criteria should consider genetic testing, and the likelihood of a mutation is very high, in the range of 95–99% when large rearrangement analysis is included with full gene sequencing [11]. Currently available methodology for VHL gene analysis includes Sanger sequencing and deletion/duplication detection techniques such as array-based comparative genome hybridization (cCGH) or multiplex ligation-dependent probe amplification (MPLA). Next-generation sequencing (NGS) is offered at many commercial laboratories with or without confirmation of pathogenic or likely pathogenic variants with Sanger sequencing. Copy number changes detected on read-depth analysis of NGS data may be confirmed by aCGH or MLPA [12].
Mosaicism is the consequence of a post-zygotic mutation in one cell in an embryo yielding two cell lines: one wild type and one harboring the mutation. The mutated cell line can be present in the soma (somatic mosaicism) or the germ cells (germline or gonadal mosaicism) or both. If the mutation is present in germ cells, offspring are at risk of inheriting the mutation and will be heterozygous for the mutated allele in all of their cells [13]. Mosaicism has been reported in several cases where one parent is found to carry the VHL mutation at low allele frequencies (less than 50%) where the offspring has clinically apparent VHL disease and a heterozygous mutation detectable in peripheral blood [14,15,16]. Low-level somatic mosaicism in VHL may be below the detection threshold of conventional techniques such as Sanger sequencing. NGS technology with high-density coverage may prove a promising way of providing clinical testing for somatic mosaicism [17•]. At the time of this publication, testing for low-level mosaicism is not clinically available for VHL. The ability to do so would have important implications for parents of de novo cases both in recurrence risk counseling and for screening of target organs.
When a mutation is identified, at-risk family members should be offered genetic testing. This includes siblings and parent(s) of the index patient whenever possible. Additionally, offspring should be offered genetic testing in the context of genetic counseling. Unaffected children at any age can undergo mutation-specific testing for a familial pathogenic mutation as screening for early detection of VHL-associated pediatric tumors, such as retinal HMB (and PHEO, particularly in VHL type 2) is appropriate. Mutation-negative children can be spared unnecessary screening. Mutation-positive children can enroll in age-specific surveillance where early detection and monitoring is of paramount importance (Table 2).
Several of the VHL component tumors are uncommon in the general population, such as HMB, PHEO, PGL, and ELST. Phenotypic variability is the norm in VHL rather than the exception, and a confirmed diagnosis of VHL has profound implications for medical management and for at-risk family members. With this in mind, genetic testing should be considered even in subtle presentations such as isolated cases (i.e., one tumor and a negative family history) of HMB, ELST, or PHEO, especially when diagnosed in an individual under 50 years of age (Table 3). Four to 14% of patients with isolated HMB of the brain or spine may have a germline VHL mutation [19,20,21], 39% of patients with isolated ELST [23], and 3% of patients with isolated PHEO [24]. The probability of detecting a mutation increases with bilateral PHEO [26].
PNETs are also uncommon in the general population but are infrequently the initial presenting lesion in patients with VHL, and the probability of a VHL mutation in these cases is quite low [25]. Patients with multifocal disease and a young age of diagnosis (<40 years) should consider evaluation and testing for multiple endocrine neoplasia type 1 as well as VHL.
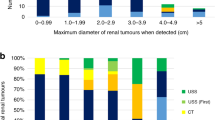
The lifetime risk of kidney and renal pelvis cancer is estimated to be about 1.6% in the US population [27]. Approximately 80% of the cancers are clear cell renal carcinomas (ccRCC). A young age of diagnosis or multifocal or bilateral disease should prompt a consideration of VHL genetic testing. The age of onset of ccRCC in VHL patients can range from 16 to 79 years old with the mean age of onset of 35 or 29 years younger than the general population average of 64 [28•]. Unilateral ccRCC diagnosed under age 40 (with or without a family history) should prompt a referral for formal risk assessment. If no additional VHL stigmata are known in the patient’s medical history or family history, VHL genetic testing can still be considered; however, the yield is likely to be low. Neumann and colleagues identified three (1.6%) mutation carriers in a pooled series of 189 unselected patients with renal cell carcinoma, although it is important to note that further probing into reported family history revealed a positive history of VHL-associated lesions. Two of the three were found to have spinal HMBs, and the third patient had no additional lesions detected on clinical screening despite having a father and daughter clinically affected with VHL [22]. In our clinical experience of 14 patients with isolated unilateral ccRCC and a negative family history (age range 25 to 53; mean age 36.6 years), the uptake of genetic testing is 100% and the VHL positivity rate is zero (unpublished data).
Additional considerations in the setting of isolated PHEO/PGL diagnosed at any age is the option of multigene panel testing to simultaneously analyze other genes known to be associated with this rare tumor type, including FH, MAX, MEN1, NF1, RET, SDHA, SDHAF2, SDHB, SDHC, SDHD, and TMEM127 in addition to VHL. More genes are likely to be identified in the near future, and a recent meta-analysis by Brito et al. found that 11–13% of sporadic cases of PHEO/PGL can be attributed to a germline mutation in one of these genes [29]. Evidence suggests that a multigene panel should be considered for any age of diagnosis of isolated PHEO/PGL with particular attention to pediatric cases as the probability of a germline mutation is very high in this age group, reduces the likelihood of diagnostic delay, and has implications for lifelong surveillance.
An estimated 1–3% of renal cell carcinomas (RCC) are attributable to an underlying hereditary susceptibility, and it should be noted that additional genes can be considered, particularly based on RCC pathology. ccRCCs have been reported in carriers of germline mutations in several inherited susceptibility genes including BAP1, FLCN, MITF, SDHB, SDHC, SDHD, TSC1, and TSC2, while germline mutations in c-MET and FH are associated with papillary type 1 and type 2 RCC, respectively. Thus, a multigene panel may be warranted, in the absence of HMB, PHEO/PGL, or other distinct VHL lesions, for patients presenting with young onset RCC, or bilateral/multifocal disease, or with a positive family history of RCC.
Tumor Detection and Surveillance
Individuals with VHL require surveillance at regular intervals to check for new lesions and monitor for interval tumor growth. Patients should be encouraged to report development of new symptoms so that necessary steps towards intervention can be undertaken in a timely fashion. At least yearly follow-up with a healthcare provider(s) informed in VHL disease ensures optimal and comprehensive medical and psychosocial care. The suggested screening protocol at the Massachusetts General Hospital can be individualized to the patient’s age as well as family history with regard to the youngest age of onset of component tumors within the family (Table 2).
Pregnancy is generally not contraindicated for women with VHL although close monitoring by a multidisciplinary team may be prudent. Some groups advocate for MRI without contrast in the fourth month [18]; however, there is no general consensus and the monitoring practices are likely to be highly variable between clinical centers and providers due to paucity of evidence-based data and different experiences with clinical outcomes of pregnant patients. With regard to the potential of pregnancy as a risk factor for new tumor growth, Binderup et al. performed a retrospective cohort study of 26 male and 26 female VHL mutation carriers in Denmark. Seventeen women completed 30 pregnancies, and the rate of new tumor growth at 1, 3, and 5 years after conception was unchanged compared to the non-pregnant intervals within the same female cohort. Based on their findings, the authors do not recommend heightened tumor surveillance during pregnancy for women with VHL [30•]. Women planning pregnancy should be advised that screening for PHEO prior to establishing a pregnancy is ideal so that an occult PHEO can be assessed and removed if necessary as hypertension is a known risk to the pregnancy [31]. Women with cerebellar HMB may be advised by their team to plan a cesarean section instead of vaginal delivery to decrease the chance of intracranial pressure.
The average age of onset differs for each component tumor with retinal HMB and PHEO being the earliest manifestation; however, the age range for all tumor types is broad and necessitates multisystem monitoring from adolescence onward. Table 4 provides a summary of the average ages of diagnosis and ranges published in the literature for the purpose of emphasizing the range in age; however, this falls short in effectively describing the wide variability of clinical presentations and morbidities across the VHL population. Within our clinic-based population of germline VHL mutation carriers, we follow patients who have been under our care for over a decade with mild presentations, e.g., a 55-year-old (non-mosaic) man with a single, clinically stable HMB and several renal cysts. At the severe end of the spectrum we have several unrelated patients in their 20s with over nine synchronous HMBs and others who have undergone multiple nephron-sparing surgeries for RCC before reaching 40 and may be facing complete nephrectomies in the future. The morbidity is not represented solely by tumor number either, as a solitary tumor positioned in a risky region, such as a brainstem HMB or a ccRCC impinging on the renal vein, poses a significant interventional challenge. The variability and unpredictability of the disease burden the VHL patient with lifelong surveillance and clinicians familiar with this non-linear trajectory should also recognize the long-term psychosocial implications of living with VHL discussed further in the next section.
Parents of children with seemingly de novo cases should be offered full evaluation for subtle signs of VHL disease. If clinical testing for low-level mosaicism becomes available in the future, re-analysis of parents who initially test negative for their offspring’s VHL mutation in peripheral blood lymphocytes could be considered. The potential impact on medical management warrants consideration of parental mosaicism as a possibility. When mosaicism is confirmed in a family member, the disease severity cannot be predicted and is likely to be dependent on the number of organs harboring the mutant allele. However, given that sampling multiple tissues is not feasible, following a system-wide monitoring protocol is prudent.
Compliance with regular monitoring; improved understanding of the natural history and biology of HMB, PHEO, and ccRCC; and advances in surgical techniques have improved patient care. More advances are needed given the cumulative effects of multiple interventions. Patients with high-risk brainstem HMBs and patients with impaired renal function due to repeated interventions need chemopreventative options to stabilize their disease progression. New targeted therapies are on the horizon but are still in the very early stages [6, 33, 34].
Genetic Counseling Across the Lifespan
Current treatment of component tumors is primarily invasive and no preventative treatment is available to slow tumor growth, prevent new tumors, or mitigate the symptoms. Some patients bear a larger burden of HMB or ccRCC, often before their fourth decade of life, and face greater morbidity from the effects of treatment due to repeated interventions or unresectable tumors (such as brainstem HMBs). The relative unpredictability of the course of the disease requires a high degree of compliance with surveillance guidelines so that existing tumors can be monitored and new growths identified, as early detection with ccRCC is crucial and necessary for prevention of metastatic disease. Annual screenings can be associated with cycles of anxiety prior to imaging as patients wait to learn whether their results will show interval growth or new tumor growth [35]. While the screening is lifelong and therefore the uncertainty and burden of screening are chronic, clinicians involved in the care of VHL patients should also be aware of the changing psychosocial needs over time and anticipate issues unique to each major life stage against this backdrop of lifelong uncertainty.
Genetic testing of children at 50% risk for VHL should be offered to parents as early as the first year of life. Children known to carry the familial mutation require early screening of the retina for HMB as well as PHEO. A negative test allows the child to avoid unnecessary retinal exams and plasma or 24-h urine catecholamine collection for PHEO screening. Genetic counselors should be aware of the psychosocial needs of the parents in the setting of genetic testing of minors. The question of timing of genetic testing grows more challenging for parents the longer testing is delayed and the older their child becomes.
Genetics professionals should also keep the age of comprehension and assent in mind when counseling parents and older children regarding genetic testing. In our observations, children who grow up knowing that they have VHL disease fare well, as they know that routine screenings, beginning with annual retinal exams, are par for the course. Children who are old enough to recognize or sense avoidance, reluctance, or anxiety in their parent are more challenging to counsel; it is far more difficult to normalize a situation that does not seem normal and is distressing to the parent(s). Adolescents in particular are at risk of adverse effects if left out of the genetic testing conversation. Adolescents who test positive cannot be protected from this knowledge as age-based screening begins to increase at this age. It is normal for teens to have an evolving sense of self as they negotiate their way between their identity in the context of the protection and security of their family and their identity in the context of their peers. Genetic counselors may need to help parents remember that the trust that their child places in them is of paramount importance and part of maintaining this trust at a crucial time such as genetic testing is to inform them of the purpose of testing in an age-appropriate manner and not to shield them from the information. It is understandably tempting for many parents to request the test in hopes that their teen is negative and inform them of the result afterward however, this scenario is fraught with challenges when an adolescent is unprepared.
At our center, we offer a baseline MRI of the brain in our pediatric population at age 9, due to our clinical experience and published cases of HMB in the cerebellum and cervical spine in preadolescence [32]. Parent/caregivers can access resources such as their healthcare provider or genetic counselor to explore ways to prepare their children for an MRI procedure. The VHL Handbook: Kid’s Edition which is written for this age group and contains illustrations by children and pictures contributed by families with VHL of their children preparing for medical procedures is an excellent resource for families [18]. Parents may wish to review the book ahead of time, or read portions of it with their child, and can also be read by the child independently. Parents may also find the book useful for answering questions that their unaffected children may pose as well about VHL. Resources such as these help lessen a child’s anxiety associated with medical exams and procedures, encourage communication between the child and parent in an age-appropriate way, and promote healthy coping overall.
As teens begin to move into adulthood, they begin to take on more of a primary role in their healthcare. Clinicians should support this transition time by incorporating the adolescent into the annual primary care visit and VHL check-up. Genetic counselors can encourage teens to talk about the social aspects of having a chronic, lifelong condition like VHL (or at least attempt to as teens are not often forthcoming). Checking in with parents and caregivers may help assess the need for further follow-up with social work and counseling. The transition is gradual, and therefore, clinicians should assess the psychosocial needs at regular intervals, such as the annual visit, as this consistency is important to the therapeutic relationship. Evidence suggests that adult patients want to be offered psychosocial support and referrals by their healthcare providers [35, 36] and it is reasonable to begin the process in adolescence. Older teens may find friendship and commonality amongst peers with VHL and other chronic medical problems based on shared identification of medical situations and challenges.
Emerging adulthood has been described by Arnett as a dynamic period between 18 and 25 in which young adults struggle between identifying as a teen versus an adult [37]. Young adults may have unique needs as they consider careers, serious relationships, and the prospect of having their own children. Furthermore, young adults may be torn between reluctance with taking a more independent role in managing their own healthcare while also wanting greater independence overall. A qualitative interview of ten young adults with VHL (five male, five female) showed that the unpredictability of the disease was most worrying; however, each participant identified a key person as a major means of support (mother or spouse) and many felt that their personal medical experiences gave them a better sense of what it meant to be a good friend [38]. The young adults in this pilot study ranged in age of diagnosis of VHL from prenatal (n = 1) to childhood (n = 3) and adolescence (n = 6), and further studies are needed to explore if an earlier age of diagnosis is associated with differing acceptance and coping strategies for VHL-related worry.
We are also observing that young adults are increasingly voicing concern about the insecurity of their financial and medical insurance situation. The concerns are less regarding genetic discrimination and greater regarding employment insecurity and affordability of health insurance. Furthermore, young adults and adults with VHL may be simultaneously managing their own disease while juggling primary caregiving for a loved one with VHL, such as a child, sibling, or parent. The social and medical consequences of financial insecurity cannot be underestimated, and clinicians may need to familiarize themselves with assistance and resources within their institution for the benefit of a segment of their VHL patient populations that are potentially vulnerable medically and financially.
Clinicians should also be aware of the preconception genetic counseling needs of patients with VHL who are contemplating having children. In addition to the option of adoption, gamete donation, or delaying genetic testing until childhood, prospective parents also have the option of prenatal diagnosis or preimplantation genetic diagnosis (PGD) with in vitro fertilization [39]. Patients should also be counseled on the recommendation for children to undergo testing early in life, as a positive test would indicate the need for retinal exams with dilation, and a negative test would rule out the disease and spare them from unnecessary exams. Research on the attitudes and perspectives of patients with VHL, familial adenomatous polyposis, Li-Fraumeni syndrome, and other inherited cancer predisposition syndromes indicates that overall patients do not object to the availability of PGD on ethical grounds and feel that this option should be offered. Many report that they are uncertain or would not be inclined to personally pursue PGD for themselves, which is consistent with our observations in the clinic [40,41,42]. In our experience, most couples planning a family elect to forego PGD and prenatal testing and will undergo presymptomatic testing after the child is born, usually within the child’s first year of life.
Support persons in the family, such as the unaffected parent or spouse, can have significant levels of distress, often not only due to the caregiving role during treatment and recovery but also due to worry over for their affected spouse and affected children. Although this area requires further research in order to improve our overall understanding, clinicians should be mindful of the psychosocial needs of support persons in order to offer for mental health services and community support such as through local caregiving support groups and the VHL Alliance [18].
In summary, a patient can anticipate that living with VHL will involve long stretches of stability without significant symptoms, even when lesions such as CNS HMBs are known clinically on imaging, interrupted with episodes of symptomatic periods as tumors “declare” their presence. For ccRCCs, we rely on imaging and application of the “3-cm rule” in timing surgical intervention, as these lesions are generally asymptomatic. The size-based approach attempts to weigh the need for multiple surgeries over the lifespan against the risk of metastasis in ccRCC greater than 3.8 cm [43]. With respect to the lifelong monitoring required, the unpredictable course, the effects on the patient, and their primary support persons/caregivers, VHL disease follows the course of a chronic disease. Throughout these times, following recommended surveillance is key but may be challenging to adhere to particularly when asymptomatic [44, 45]. For this reason, it is critical that the patient have at least one healthcare provider who is familiar enough with the disease and willing to oversee and coordinate their care and preferably works with an integrated multidisciplinary team that includes expertise in genetic counseling, mental health, surgery, radiation oncology, nephrology, endocrinology, and ophthalmology [18]. Clinicians should also be aware of the changing psychosocial needs of their patients and assess and address the need for further support with referrals to mental health professionals familiar with chronic disease and/or cancer survivorship.
Conclusions
Von Hippel-Lindau syndrome is highly variable, and the rate of new tumor development varies over a patient’s lifespan. The chronicity of the disease is superimposed against a backdrop of the normal developmental stages and life’s milestones that each individual will experience. A VHL family can also be seen as a multigenerational system moving through time where uncertainty and fluctuations in the disease course can cause stress, worry, and anxiety. Clinicians should be aware of both the individual medical and psychosocial needs of the patient. The signs of VHL and other related syndromes can be subtle in an index patient, and a referral to a genetic counselor for formal genetic risk assessment can uncover a diagnosis without delay and provide on-going source of support of the patient and family. Presymptomatic testing in childhood, particularly adolescence, is emotionally distressing for parents, and genetic counselors need to provide anticipatory guidance to both parent(s) and child.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Maher ER, Yates JRW, Harries R, Benjamin C, Harris R, Moore AT, et al. Clinical features and natural history of von Hippel-Lindau disease. QJM. 1990;77(1):1151–63.
Lonser RR, Glenn GM, Walther M, Chew EY, Libutti SK, Linehan WM, et al. von Hippel-Lindau disease. Lancet. 2003;361(9374):2059–67.
Latif F, Tory K, Gnarra J, Yao M, Duh FM, Orcutt ML, et al. Identification of the von Hippel-Lindau disease tumor suppressor gene. Science. 1993;260(5112):1317–20.
Herman JG, Latif F, Weng Y, Lerman MI, Zbar B, Liu S, et al. Silencing of the VHL tumor-suppressor gene by DNA methylation in renal carcinoma. Proc Natl Acad Sci U S A. 1994;91(21):9700–4.
Iliopoulos O, Levy AP, Jiang C, Kaelin Jr WG, Goldberg MA. Negative regulation of hypoxia-inducible genes by the von Hippel-Lindau protein. Proc Natl Acad Sci U S A. 1996;93(20):10595–9.
Schunemann V, Huntoon K, Lonser RR. Personalized medicine for nervous system manifestations of von Hippel-Lindau disease. Frontiers in surgery. 2016;3:39.
van der Mijn JC, Panka DJ, Geissler AK, Verheul HM, Mier JW. Novel drugs that target the metabolic reprogramming in renal cell cancer. Cancer Metab. 2016;4:14.
• Gossage L, Eisen T, Maher ER. VHL, the story of a tumour suppressor gene. Nat Rev Cancer. 2015;15(1):55–64. The authors provide an elegant historical perspective with emphasis on the importance of the VHL gene in the biological understanding of cancer.
Poulsen ML, Budtz-Jorgensen E, Bisgaard ML. Surveillance in von Hippel-Lindau disease (vHL). Clin Genet. 2010;77(1):49–59.
Binderup ML, Budtz-Jorgensen E, Bisgaard ML. Risk of new tumors in von Hippel-Lindau patients depends on age and genotype. Genetics in medicine : official journal of the American College of Medical Genetics. 2016;18(1):89–97.
Stolle C, Glenn G, Zbar B, Humphrey JS, Choyke P, Walther M, et al. Improved detection of germline mutations in the von Hippel-Lindau disease tumor suppressor gene. Hum Mutat. 1998;12(6):417–23.
GeneTests. GeneTests. [12/14/16]. 2016. Available from: genetests.org.
Freed D, Stevens EL, Pevsner J. Somatic mosaicism in the human genome. Genes (Basel). 2014;5(4):1064–94.
Murgia A, Martella M, Vinanzi C, Polli R, Perilongo G, Opocher G. Somatic mosaicism in von Hippel-Lindau disease. Hum Mutat. 2000;15(1):114.
Santarpia L, Sarlis NJ, Santarpia M, Sherman SI, Trimarchi F, Benvenga S. Mosaicism in von Hippel-Lindau disease: an event important to recognize. J Cell Mol Med. 2007;11(6):1408–15.
Sgambati MT, Stolle C, Choyke PL, Walther MM, Zbar B, Linehan WM, et al. Mosaicism in von Hippel-Lindau disease: lessons from kindreds with germline mutations identified in offspring with mosaic parents. Am J Hum Genet. 2000;66(1):84–91.
• Coppin L, Grutzmacher C, Crepin M, Destailleur E, Giraud S, Cardot-Bauters C, et al. VHL mosaicism can be detected by clinical next-generation sequencing and is not restricted to patients with a mild phenotype. European journal of human genetics : EJHG. 2014;22(9):1149–52.The authors are first to demonstrate technical feasibility of detecting VHL mosaicism with next-generation sequencing which holds promise for defining atypical cases in the future.
VHL Alliance. [VHL Alliance Homepage]. 2016. Available from: vhl.org.
Catapano D, Muscarella LA, Guarnieri V, Zelante L, D’Angelo VA, D’Agruma L. Hemangioblastomas of central nervous system: molecular genetic analysis and clinical management. Neurosurgery. 2005;56(6):1215–21. discussion 21
Hes FJ, McKee S, Taphoorn MJ, Rehal P, van Der Luijt RB, McMahon R, et al. Cryptic von Hippel-Lindau disease: germline mutations in patients with haemangioblastoma only. J Med Genet. 2000;37(12):939–43.
Woodward ER, Wall K, Forsyth J, Macdonald F, Maher ER. VHL mutation analysis in patients with isolated central nervous system haemangioblastoma. Brain J Neurol. 2007;130(Pt 3):836–42.
Neumann HP, Bender BU, Berger DP, Laubenberger J, Schultze-Seemann W, Wetterauer U, et al. Prevalence, morphology and biology of renal cell carcinoma in von Hippel-Lindau disease compared to sporadic renal cell carcinoma. J Urol. 1998;160(4):1248–54.
Bausch B, Wellner U, Peyre M, Boedeker CC, Hes FJ, Anglani M, et al. Characterization of endolymphatic sac tumors and von Hippel-Lindau disease in the International Endolymphatic Sac Tumor Registry. Head & neck. 2016;38(Suppl 1):E673–9.
Brauch H, Hoeppner W, Jahnig H, Wohl T, Engelhardt D, Spelsberg F, et al. Sporadic pheochromocytomas are rarely associated with germline mutations in the vhl tumor suppressor gene or the ret protooncogene. J Clin Endocrinol Metab. 1997;82(12):4101–4.
Erlic Z, Ploeckinger U, Cascon A, Hoffmann MM, von Duecker L, Winter A, et al. Systematic comparison of sporadic and syndromic pancreatic islet cell tumors. Endocr Relat Cancer. 2010;17(4):875–83.
Castellano M, Mori L, Giacche M, Agliozzo E, Tosini R, Panarotto A, et al. Genetic mutation screening in an Italian cohort of nonsyndromic pheochromocytoma/paraganglioma patients. Ann N Y Acad Sci. 2006;1073:156–65.
SEER Cancer Stat Fact Sheets [Internet]. [cited 12/14/16]. Available from: seer.cancer.gov.
• Shuch B, Vourganti S, Ricketts CJ, Middleton L, Peterson J, Merino MJ, et al. Defining early-onset kidney cancer: implications for germline and somatic mutation testing and clinical management. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2014;32(5):431–7.The authors provide evidence that the average age of renal cancer diagnosis is significantly younger and provides grounds for using age in identifying which patients should be referred for genetic risk assessment and evaluation.
Brito JP, Asi N, Bancos I, Gionfriddo MR, Zeballos-Palacios CL, Leppin AL, et al. Testing for germline mutations in sporadic pheochromocytoma/paraganglioma: a systematic review. Clin Endocrinol. 2015;82(3):338–45.
• Binderup ML, Budtz-Jorgensen E, Bisgaard ML. New von Hippel-Lindau manifestations develop at the same or decreased rates in pregnancy. Neurology. 2015;85(17):1500–3. The evidence presented in this retrospective study that pregnancy does not necessarilty aggravate tumors can provide clinicians with some reassurance when counseling women with VHL who are planning pregnancy.
Lenders JW. Pheochromocytoma and pregnancy: a deceptive connection. Eur J Endocrinol. 2012;166(2):143–50.
Chittiboina P, Lonser RR. Von Hippel-Lindau disease. Handb Clin Neurol. 2015;132:139–56.
Metelo AM, Noonan HR, Li X, Jin Y, Baker R, Kamentsky L, et al. Pharmacological HIF2alpha inhibition improves VHL disease-associated phenotypes in zebrafish model. J Clin Invest. 2015;125(5):1987–97.
Noonan HR, Metelo AM, Kamei CN, Peterson RT, Drummond IA, Iliopoulos O. Loss of vhl in the zebrafish pronephros recapitulates early stages of human clear cell renal cell carcinoma. Dis Model Mech. 2016;9(8):873–84.
Kasparian NA, Rutstein A, Sansom-Daly UM, Mireskandari S, Tyler J, Duffy J, et al. Through the looking glass: an exploratory study of the lived experiences and unmet needs of families affected by Von Hippel-Lindau disease. European journal of human genetics : EJHG. 2015;23(1):34–40.
Lammens CR, Bleiker EM, Verhoef S, Hes FJ, Ausems MG, Majoor-Krakauer D, et al. Psychosocial impact of Von Hippel-Lindau disease: levels and sources of distress. Clin Genet. 2010;77(5):483–91.
Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. The American psychologist. 2000;55(5):469–80.
Schmidt L. Peering down the rabbit hole: living with von Hippel-Lindau syndrome from the young adult perspective [Masters thesis]. Brandeis Institutional Repository: Brandeis University; 2015.
Rechitsky S, Verlinsky O, Chistokhina A, Sharapova T, Ozen S, Masciangelo C, et al. Preimplantation genetic diagnosis for cancer predisposition. Reprod BioMed Online. 2002;5(2):148–55.
Lammens C, Bleiker E, Aaronson N, Vriends A, Ausems M, Jansweijer M, et al. Attitude towards pre-implantation genetic diagnosis for hereditary cancer. Familial Cancer. 2009;8(4):457–64.
Meister U, Finck C, Stobel-Richter Y, Schmutzer G, Brahler E. Knowledge and attitudes towards preimplantation genetic diagnosis in Germany. Hum Reprod. 2005;20(1):231–8.
Quinn GP, Pal T, Murphy D, Vadaparampil ST, Kumar A. High-risk consumers’ perceptions of preimplantation genetic diagnosis for hereditary cancers: a systematic review and meta-analysis. Genetics in medicine: official journal of the American College of Medical Genetics. 2012;14(2):191–200.
Walther MM, Lubensky IA, Venzon D, Zbar B, Linehan WM. Prevalence of microscopic lesions in grossly normal renal parenchyma from patients with von Hippel-Lindau disease, sporadic renal cell carcinoma and no renal disease: clinical implications. J Urol. 1995;154(6):2010–4. discussion 4-5
Lammens CR, Aaronson NK, Hes FJ, Links TP, Zonnenberg BA, Lenders JW, et al. Compliance with periodic surveillance for Von-Hippel-Lindau disease. Genetics in medicine: official journal of the American College of Medical Genetics. 2011;13(6):519–27.
Rasmussen A, Alonso E, Ochoa A, De Biase I, Familiar I, Yescas P, et al. Uptake of genetic testing and long-term tumor surveillance in von Hippel-Lindau disease. BMC medical genetics. 2010;11:4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares that there is no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Genetic Counseling and Clinical Testing
Rights and permissions
About this article
Cite this article
Chan-Smutko, G. Genetic Counseling in Von Hippel-Lindau Disease: Navigating the Landscape of a Well-Established Syndrome. Curr Genet Med Rep 5, 66–74 (2017). https://doi.org/10.1007/s40142-017-0119-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40142-017-0119-4