Abstract
Purpose of Review
The purpose of this narrative review is to highlight clinically relevant characteristics and rehabilitation interventions for aromatase inhibitor-induced musculoskeletal syndrome (AIMSS).
Recent Findings
AIMSS is a constellation of musculoskeletal symptoms including arthralgias, myalgias, and stiffness resulting from estrogen deprivation. The etiology likely relates to estrogen’s role in pain, immune, and skeletal, cartilaginous modulation. Rehabilitation strategies include medications and supplements, resistance, and aerobic exercises. Majority of the rehabilitation studies evaluated exercise interventions.
Summary
AIMSS continues to be a broadly defined condition. The exact pathophysiology has not yet been discovered. Rehabilitation management is multi-dimensional and future research may consider a biopsychosocial approach. While exercise interventions are the most widely studied, there is a need to identify effective exercise protocols. Future research should also evaluate the effectiveness of occupational therapy interventions specifically for AIMSS populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There are approximately 3.6 million breast cancer survivors, 75% with hormone receptor positive cancers, in the USA and 1.3 million gynecologic cancer survivors[1,2,3]. Aromatase inhibitors (AI) are prescribed as endocrine therapy for cancer treatment to reduce tumor growth and to reduce recurrence[1]. A 5-year treatment with AI reduces the risk of breast cancer recurrence by 18–32%[4]. AI therapy is also administered in select ovarian and uterine cancers[5]. For breast cancer, the American Society of Clinical Oncology updated guidelines from 2018 recommend ten years adjuvant endocrine therapy[6]. The National Comprehensive Cancer Network recommends consideration of hormone therapy in low grade endometrial carcinoma[7] and may be considered in relapsed ovarian and endometrial cancers[8].
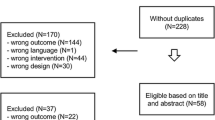
Unfortunately, approximately 33–61% of individuals on aromatase inhibitors develop musculoskeletal and joint symptoms; collectively described as “aromatase inhibitor-induced musculoskeletal syndrome” (AIMSS) or aromatase inhibitor-related arthralgias. In this review, aromatase inhibitors will refer only to anastrozole, letrozole, and exemestane; musculoskeletal and joint sequelae of Tamoxifen were not reviewed. AIMSS leads to treatment cessation, functionally limiting impairments and decreased quality of life[9]. The following narrative review defines aromatase inhibitors, proposed pathophysiology and presents common rehabilitation interventions. PubMed and EBSCO databases were queried with the following Mesh terms ((“Breast Neoplasms”[Mesh]) AND/OR ((“Endometrial Neoplasms”[Mesh]), “Ovarian Neoplasms” [Mesh], “Aromatase Inhibitors/adverse effects”[Mesh]) AND “Rehabilitation”[Mesh].
Defining Aromatase Inhibitor-induced Musculoskeletal Syndrome
Aromatase inhibitors reduce peripherally circulating levels of estrogen in post-menopausal women. The third generation AIs include anastrozole, letrozole, and exemestane. Anastrozole and Letrozole are non-steroid and reversible inhibitors; exemestane is steroidal, irreversible and acts as a false substrate[10].
There are multiple definitions of “AIMSS”. AIMSS typically manifests as arthralgias, muscle weakness, and bone pain[2, 11]. There is no standard definition of AIMSS to our knowledge. AIMSS is also defined by the following five symptoms: arthralgia, myalgia, joint stiffness, tingling, carpal tunnel syndrome[12]. One study utilized a mix of symptoms and signs as presented by Niravath et al.—major criteria as “currently taking AIs therapy, major criteria as joint pain that had emerged or worsened after starting AI therapy, joint pain improves or resolves within 2 weeks of stopping AIs therapy and joint pain returns upon resuming AI’s” and minor criteria: symmetric joint pain, carpal tunnel syndrome, reduced grip strength, morning stiffness, and improvement in symptoms with exercise[13, 14]. In a retrospective study of individuals with gynecologic cancers, AIMSS was defined by arthralgias, stiffness, myalgias, tendon pathology, paresthesias, carpal tunnel syndrome, fatigue, hot flashes, and deep venous thrombosis[5]. Overall, the above definitions include symptoms (arthralgias, myalgias, stiffness, fatigue, paresthesia) and measurable clinical signs (tendon pathology, grip strength, DVT). AIMSS often occurs within 6 weeks of initiating AI therapy [15] (Fig. 1).
Despite the different definitions, joint pain is the most commonly reported symptom[11]. It is currently unknown if AIMSS causes to one primary symptom (i.e., arthralgias) and then subsequently results in myalgias and joint stiffness or whether multiple symptoms arise simultaneously. Regardless, it is known that individuals with other arthritic conditions (rheumatoid arthritis, osteoarthritis) and muscular conditions (fibromyalgia) describe inter-connected symptoms. For AIMSS, among 188 breast cancer participants, the most common sites of joint symptoms were knees, followed by hands/fingers and shoulders[12]. Notably, 60% in this sample experienced 3 or more symptoms. Symptoms peak in the first 4–8 months with 80% of symptoms emerging within 6 months of starting AI therapy [16]. While the diagnosis is clinical and based on patient’s reported symptoms, imaging may confirm underlying musculoskeletal pathology. For example, MRI imaging has demonstrated tenosynovial changes among individuals with AIMSS; these changes were associated with a reduced grip strength [17].
AIMSS has not been as widely reported in gynecologic cancers. It is unclear if this is due to differing indications to start AI therapy, reduced incidence, a lower level of symptom reporting in this population. One retrospective study in this population was identified. Thirty five percent of 146 individuals with gynecologic cancers reported musculoskeletal symptoms during AI therapy[5]. Symptoms were reported within the first 4–6 months of treatment initiation. Similar to breast cancer patients, the most common musculoskeletal symptom was arthralgia (29.5%).
Pathophysiology
The etiology of AIMSS is attributed to estrogen deprivation but the exact pathophysiology has not been identified. Additionally, estrogen receptors may impact cartilage homeostasis and prevent cartilage degeneration but this has been primarily studied in rat models[18, 19]. Studies have identified genetic variants associated with increased pain and arthralgias among those receiving AI therapy. The allele rs4646536 of the CYP27B1 gene and rs6163 of the CYP17A1, VDR are associated with increased symptoms [20, 21]. Furthermore, the number of unfavorable alleles may be associated with greater pain[22]. Estrogen has been shown to modulate pain pathways in the spinal cord[10]. Additionally, individuals with AIMSS may express higher levels of inflammatory biomarkers. A cross-sectional study identified an association between higher levels of vitamin D-binding protein (VDBP), an acute phase reactant, eotaxin, and monocyte chemoattractant protein (MCP-1) and moderate-severe arthralgia[23]. Carpal tunnel syndrome is the most common described neuropathy in AIMSS. The etiology may also be related to estrogen as well. Interestingly, a cross-sectional study identified a higher number of estrogen receptors on the transverse carpal ligament in women aged 50–70 years with carpal tunnel syndrome compared to controls [24].
Risk Factors for Developing AIMSS
Identified risk factors among breast, endometrial, and ovarian cancers for AIMSS include history of Taxane chemotherapy, younger age (less than 55 years old), history of musculoskeletal symptoms, and body mass index (BMI) [5, 12, 16, 25]. The younger age is attributed to an accelerated, abrupt decline in estrogen levels compared to those starting AI therapy further into menopause[26]. Furthermore, a pre-existing history of musculoskeletal symptoms, arthralgias have been associated with higher rates of treatment discontinuation. Approximately one-fourth to one-third of breast cancer patients may experience arthralgias and myalgias prior to AI therapy[2].
Researchers have further assessed the association of body mass index and AIMSS. A BMI of 25 to 30 was associated with a lower risk[25]. The etiology may be attributed to underlying chronic inflammation[27]. Individuals with low or high BMI, less than approximately 20 or higher than 35, respectively have a higher probability to stop AIs[12]. One study identified that individuals with vitamin D levels less than 40 ng/mL developed pain after 3 months of AI therapy (21% vs 53.2%)[22]. The underlying mechanism has not been established and further studies are needed to corroborate this finding.
Researchers have also evaluated if certain aromatase inhibitors increase the risk of AIMSS. Anastrozole is the most commonly prescribed AI in the USA. In a meta-analysis of breast cancer patients, anastrozole was not associated with an elevated risk compared to exemestane and letrozole[25].Whereas, in uterine and ovarian cancers, a multivariate analysis revealed that exemestane was associated with a higher odds ratio of developing musculoskeletal side effects[5].
Importantly, symptom presence is not synonymous with AI discontinuation. A number of factors may drive an individual to discontinue the medication. A multivariate model showed that being bothered by symptoms was significantly associated with treatment cessation. Individuals with receipt of prior chemotherapy, hormone replacement therapy, and on a higher number of mediations were factors associated with “bother”[11].
Measuring Symptom Burden
To the author’s knowledge, there is not a standardized screening or outcome measure to capture AIMSS characteristics, severity, and functional limitations. Despite this, a number of clinical studies have incorporated patient outcome measures pertaining to arthritis and general physical function to assess the syndrome (Table 1). These measures have been used to detect symptoms in cross-sectional studies and as outcome measures in interventional studies. Notably, a study by Swenson et al. identified the Australian/Canadian Osteoarthritis Hand Index (AUSCAN), Western and McMaster Osteoarthritis Index (WOMAC), and Breast Cancer Prevention Trial-Musculoskeletal Symptom (BCPT-MS) to be responsive to AIMSS symptoms over time[2].
A prospective, observational study of breast cancer patients demonstrated a significant increase in symptom burden from baseline to 6 months as measured by the WOMAC, BCPT-MS, and AUSCAN. The QuickDASH score did not significantly change; this may be because a number of questions pertain to shoulder/proximal upper extremity function which may be less impacted in AIMSS[2]. There were no changes on the WOMAC-physical function and PROMIS physical function scales. This could be expected if participants were experiencing hand, dexterity symptoms rather than gait and mobility limitations.
Regarding objective physical function tests, studies have measured grip strength and functional mobility in breast cancer patients. In a prospective study of 292 participants, individuals who reported AIMSS symptoms experienced a 2.5 kPA (about 0.38 lb of force/square inch) decrease in grip strength compared to those on AI therapy without symptoms at 12-months follow-up[12]. Further supporting the association with rate of estrogen loss and symptoms, younger individuals exhibited a greater reduction in grip strength[12]. However, in a prospective study by Swenson et al. of 122 participants, there were no significant changes in objective physical function measures—hand grip and functional mobility at 6 months [2]. The latter did not distinguish physical function outcome measures based on the presence of AIMSS.
Rehabilitation Medicine Interventions
Medications and Supplements
Common treatments to alleviate symptoms include non-steroid anti-inflammatory medications. Other studied interventions include serotonin-norepinephrine receptor inhibitors (SNRIs)[28], bisphosphonates, calcium and vitamin D supplementation[29][30, 31], and complementary therapies such as acupuncture[32, 33] and supplements such as glucosamine-sulfate and chondroitin-sulfate[34]. Among gynecologic cancers, those already on SNRIs and Gabapentin reported a lower level of symptom burden[5].
A randomized controlled study of 299 individuals with breast cancer with joint pain on AI therapy demonstrated statistically significant improved Brief Pain Inventory scores with Duloxetine compared to placebo at 12 weeks [35]. The analysis controlled for baseline pain score, prior receipt of taxane chemotherapy and time from trial registration to the 12-week follow-up assessment. Duloxetine reduced pain by 0.82 points compared to the placebo; notably, a difference by 2 points has been shown to be the minimum clinically important difference for the Brief Pain Inventory [36]. Similarly, WOMAC and M-SACRAH scores in the intervention arm improved compared to the control. Importantly, individuals randomized to Duloxetine reported symptom relief only 2 weeks after starting treatment. While the results were modest and may not be interpreted as clinically significant, it should be noted that eligibility criteria included individuals with an ECOG performance status of 0–2 (higher level of performance status). Additionally, the study appears to have been powered with pain as the primary outcome. Future study designs could compare the effect of duloxetine on those with high vs. low performance status, be powered to assess self-reported changes in physical function, and could evaluate its association with AI therapy adherence.
Interestingly, aromatase inhibitors have been shown to activate TRPA1 ion channels—a channel whose activation is associated with chronic pain[37]. Stimulation of TRPA1 generates a calcium response, increased neuropeptide flow out of the dorsal spinal cord and is also associated with inflammatory neuroedema[38]. Animal models have tested agents such as Gabapentin and Capsaicin to attenuate this neuroinflammatory response in chronic pain conditions [39]. Additionally, TRPA1 ion channels are upregulated in osteoarthritis and rheumatoid arthritis[40]. Gabapentin is particularly appealing given its use in also alleviating menopausal symptoms such as hot flashes—another common symptom among individuals on AI therapy [11]. Based on the above, the relationship between TRPA1 and calcium channel blockers in mitigating AIMSS could be further explored.
While estrogen is needed to activate vitamin D, supplementation has not been consistently shown with a high level of evidence to mitigate AIMSS symptoms[41]. Limitations of these Vitamin D interventions included lack of true randomization, secondary analyses to draw conclusions, and sample bias [26].
Interestingly, one study evaluated the role of diuretics in mitigating AIMSS based on retrospective work which showed lower report of symptoms among those on diuretics for hypertension or heart disease[14]. A phase II study administered a combination of Furosemide 20 mg/Spironolactone 50 mg every other day for 4 weeks to 50 women receiving AI therapy. After weeks, the WOMAC scores improved from 29 to 17 and QuickDASH from 25 to 16. Four participants stopped the diuretic due to morning diuresis. Spironolactone, an aldosterone antagonist, has been proposed as an anti-inflammatory medication in osteoarthritis[42]. Further research in AIMSS with larger, randomized controlled trials is needed to establish effectiveness.
Exercise Interventions
It appears that a majority of rehabilitation studies encompass an exercise intervention. A Cochrane review in 2020 identified low to very low certainty regarding the evidence for exercise compared to standard of care in improving the following outcomes: pain, stiffness, and quality of life. It should be noted that the review included one to four randomized controlled trials (RCTs) per outcome with an analysis of seven RCTs total for the review[43]. In particular, exercise included activities such as tai chi, yoga, and aqua aerobics in addition to aerobic and resistance exercises. Among aerobic interventions, exercise regimens were quite heterogeneous—included Nordic walking, 150-min weekly walking program, calisthenics, and ascending/descending stairs. The intervention lasted anywhere from 6 to 52 weeks. Importantly, adherence to the intervention varied from 8 to 85%. While exercise is a compelling intervention, given the heterogeneity and quality of the studies, it is challenging to identify the most effective exercise regimen from this review.
Another systematic review by Lu et al. identified eight randomized controlled trials[44]. Five out of eight included a walking intervention; two included resistance exercises and one an aquatic regimen. They identified 3 primary outcomes: pain, stiffness, and grip strength. A subgroup analysis demonstrated that exercise improved all three outcomes. It should be noted that this included six, two, and three studies, respectively; however, for pain, heterogeneity was 63%, 0% for stiffness, and 0% for grip strength.
Furthermore, outcome measures selected the above two reviews focused on impairments/symptoms but did not assess functional limitations and activity participation.
One of the most cited trials, The Hormone and Physical Exercise (HOPE trial), evaluated a 12-month aerobic and resistance exercise intervention among individuals receiving AI therapy[45]. It demonstrated that pain improved by 29% in the exercise compared to 3% in the control arm. On average, participants in the intervention arm engaged in 119 min of aerobic exercise (brisk walking) per week. Notably, 120 min of aerobic exercise a week may be more feasible than the 150 min recommended by national exercise guidelines[46]. Furthermore, walking alone may mitigate symptoms[47]. More recently, a sub-analysis of the HOPE trial assessed predictors of exercise adherence[48]. Baseline VO2 was associated with higher levels of aerobic exercise participation; older age and a higher educational level was associated with better in-person attendance rates for supervised resistance exercise training. The positive correlation with older age could be due to the ability to attend classes during working hours. Higher levels of education have been associated with higher rates of exercise participation in cancer and non-cancer studies[49, 50]. Of note, the tested covariates for adherence included “age, education, BMI, years on AIs, baseline physical activity, and marital status”. It did not directly measure comorbid musculoskeletal conditions, current socioeconomic status, competing factors, and attitudes toward exercise.
Future Considerations
The rationale for exercise interventions is largely drawn from the evidence in other arthritic conditions. In rheumatoid arthritis (RA), physical activity may be associated with increased neutrophil migration and improved monocyte, macrophage function. A pilot study evaluating a high intensity exercise program in RA patients demonstrated improved neutrophil migration and reduced toll-like receptor expression but no change in inflammatory marker levels [51]. This is consistent with a systematic review from 2019 which did not identify any association between physical activity and inflammatory marker levels (interleukins, ESR, and CRP) in RA [52]. Notably, the study was not designed to evaluate if these changes in immune cell activity were associated with symptom burden. Additionally, resistance exercise, mixed aerobic, and resistance exercises are associated with increased muscle strength but not flexibility[53]. While there is symptom overlap between RA and AIMSS, as illustrated above, these outcomes have not been as widely studied in AIMSS. The physiology and clinical implication of exercise on the control and progression of AIMSS needs to be further explored.
Role of Occupational Therapy
Because occupational therapy interventions specifically for AIMSS were not identified, the author reviewed evidence for comparable musculoskeletal and rheumatologic conditions. A systematic review assessed the effectiveness of occupational therapy for musculoskeletal conditions of the distal upper extremities. Twenty of the 59 studies were for carpal tunnel syndrome and 7 included rheumatoid and osteoarthritis[54]. There was moderate quality evidence of a strengthening program and low quality of evidence for kinesiotaping in RA[54]. Additionally, there was mixed evidence for splinting in OA. Notably, one study involving mixed hand diagnoses demonstrated greater effectiveness with a biopsychosocial model approach. Compared with a standard inpatient care model for patients with hand-related diagnoses, a nonrandomized comparative study found greater functional improvement and decreased pain. Participants were screened and treated for anxiety and depression, met jointly on a weekly basis with a multidisciplinary treatment team, had a rehabilitation manager, and participated in targeted work-related activities as part of the occupational therapy intervention[55].
Carpal Tunnel Syndrome
Based on the systematic review of 20 studies evaluating OT interventions for carpal tunnel syndrome, there is a moderate level of evidence for manual therapy and mobilization techniques. There is also moderate evidence for splinting. Low level laser therapy has not been found to be an effective treatment; additionally, there is limited evidence of ultrasound compared to placebo[54]. Given the lack of studies in AIMSS, it would be reasonable incorporate manual therapy, mobilization techniques, and splinting for those with carpal tunnel syndrome symptoms. Future studies should evaluate these interventions in this population.
Behavioral Interventions
In 2019, Shelby et al developed a “coping skills training intervention protocol” (CSA-AET) to improve adherence to AI therapies and to improve impact of the symptom burden; additional outcomes include understanding barriers and beliefs about taking AIs. The intervention was delivered by nurses via telephone. Participants also received automated messages for medication reminders and reinforcement of skills to manage symptoms. The content included education, symptom management strategies, and a workbook with the educational content. Educational topics include pain, fatigue, depression, sleep, cognition, and sexual side effects. The results of this behavioral intervention are pending.
Conclusion
Aromatase inhibitor-induced musculoskeletal syndrome is a prevalent condition among individuals with breast and gynecologic cancers. While the etiology is attributed to estrogen deprivation, the pathophysiology has yet to be fully understood. It is especially clinically relevant to mitigate symptom burden to prevent discontinuation of oncologic therapy. Given the heterogeneity of muscular, joint, and nerve-related symptoms, effective medication and rehabilitation interventions will likely have to be tailored to the patient. Moreover, because estrogen deprivation impacts other areas of health (bone, sexual, cognitive), patients may present with a constellation of symptoms in addition to AIMSS impacting daily activities and function[10]. As a result, a biopsychosocial model approach to rehabilitation is particularly compelling to research. There is an immense opportunity for rehabilitation investigators to engage in research to better understand AIMSS and to identify effective treatment regimens.
References
Nyrop KA, Callahan LF, Rini C, Altpeter M, Hackney B, DePue A, et al. Aromatase inhibitor associated arthralgia: the importance of oncology provider-patient communication about side effects and potential management through physical activity. Support Care Cancer. 2016;24:2643–50.
Swenson KK, Nissen MJ, Henly SJ, Maybon L, Pupkes J, Zwicky K, et al. Identification of tools to measure changes in musculoskeletal symptoms and physical functioning in women with breast cancer receiving aromatase inhibitors. Oncol Nurs Forum. 2013;40:549–57.
Institute NC Cancer Stat Facts. https://seer.cancer.gov/statfacts/. Accessed 4/12/2021.
Abe O, Abe R, Enomoto K, et al. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomised trials. Lancet. 2005;365:1687–717.
Bell SG, Dalton L, McNeish BL, Fang F, Henry NL, Kidwell KM, et al. Aromatase inhibitor use, side effects and discontinuation rates in gynecologic oncology patients. Gynecol Oncol. 2020;159:509–14.
Burstein HJ, Lacchetti C, Holly A, et al. Adjuvant endocrine therapy for women with hormone receptor-positive breast cancer: ASCO Clinical Practice Guideline Focused Update. J Clin Oncol. 2018;37:423–38.
Paleari L, Rutigliani M, Siri G, Provinciali N, Colombo N, Decensi A. Aromatase inhibitors as adjuvant treatment for ER/PgR positive stage I endometrial carcinoma: a retrospective cohort study. Int J Mol Sci. 2020;21. https://doi.org/10.3390/ijms21062227.
Colon-Otero G, Zanfagnin V, Hou X, Foster NR, Asmus EJ, Wahner Hendrickson A, et al. Phase II trial of ribociclib and letrozole in patients with relapsed oestrogen receptor-positive ovarian or endometrial cancers. ESMO Open. 2020;5:e000926. https://doi.org/10.1136/esmoopen-2020-000926.
Shelby RA, Dorfman CS, Bosworth HB, Keefe F, Sutton L, Owen L, et al. Testing a behavioral intervention to improve adherence to adjuvant endocrine therapy (AET). Contemp Clin Trials. 2019;76:120–31.
Tenti S, Correale P, Cheleschi S, Fioravanti A, Pirtoli L. Aromatase inhibitors—induced musculoskeletal disorders: current knowledge on clinical and molecular aspects. Int J Mol Sci. 2020;21:1–38.
Wagner LI, Zhao F, Goss PE, Chapman JW, Shepherd LE, Whelan TJ, et al. Patient-reported predictors of early treatment discontinuation: treatment-related symptoms and health-related quality of life among postmenopausal women with primary breast cancer randomized to anastrozole or exemestane on NCIC Clinical Trials Group (CCTG) MA.27 (E1Z03). Breast Cancer Res Treat. 2018;169:537–48.
Lintermans A, Van Asten K, Wildiers H, et al. A prospective assessment of musculoskeletal toxicity and loss of grip strength in breast cancer patients receiving adjuvant aromatase inhibitors and tamoxifen, and relation with BMI. Breast Cancer Res Treat. 2014;146:109–16.
Niravath P. Aromatase inhibitor-induced arthralgia: a review. Ann Oncol. 2013;24:1443–9.
Alhanafy AM, Labeeb A, Khalil A. The role of diuretics in treatment of aromatase inhibitors induced musculoskeletal symptoms in women with non metastatic breast cancer. Asian Pac J Cancer Prev. 2018;19:3525–31.
Henry NL, Giles JT, Ang D, Mohan M, Dadabhoy D, Robarge J, et al. Prospective characterization of musculoskeletal symptoms in early stage breast cancer patients treated with aromatase inhibitors. Breast Cancer Res Treat. 2008;111:365–72.
Egawa C, Hirokaga K, Takao S, Yamagami K, Miyashita M, Baba M, et al. Risk factors for joint symptoms in postmenopausal Japanese breast cancer patients treated with anastrozole: a prospective multicenter cohort study of patient-reported outcomes. Int J Clin Oncol. 2016;21:262–9.
Morales L, Pans S, Verschueren K, van Calster B, Paridaens R, Westhovens R, et al. Prospective study to assess short-term intra-articular and tenosynovial changes in the aromatase inhibitor-associated arthralgia syndrome. J Clin Oncol. 2008;26:3147–52.
Xu X, Li X, Liang Y, Ou Y, Huang J, Xiong J, et al. Estrogen modulates cartilage and subchondral bone remodeling in an ovariectomized rat model of postmenopausal osteoarthritis. Med Sci Monit. 2019;25:3146–53.
Oestergaard S, Sondergaard BC, Hoegh-Andersen P, Henriksen K, Qvist P, Christiansen C, et al. Effects of ovariectomy and estrogen therapy on type II collagen degradation and structural integrity of articular cartilage in rats: implications of the time of initiation. Arthritis Rheum. 2006;54:2441–51.
Garcia-Giralt N, Rodríguez-Sanz M, Prieto-Alhambra D, Servitja S, Torres-del Pliego E, Balcells S, et al. Genetic determinants of aromatase inhibitor-related arthralgia: the B-ABLE cohort study. Breast Cancer Res Treat. 2013;140:385–95.
Rodriguez-Sanz M, Garcia-Giralt N, Prieto-Alhambra D, Servitja S, Balcells S, Pecorelli R, et al. CYP11A1 expression in bone is associated with aromatase inhibitor-related bone loss. J Mol Endocrinol. 2015;55:69–79.
Servitja S, Martos T, Garrigos L, Rodriguez Sanz M, Garcia Giralt N, Prieto Alhambra D, et al. Skeletal adverse effects with aromatase inhibitors in early breast cancer: Evidence to date and clinical guidance. Ther Adv Med Oncol. 2015;7:291–6.
Bauml J, Chen L, Chen J, Boyer J, Kalos M, Li SQ, et al. Arthralgia among women taking aromatase inhibitors: is there a shared inflammatory mechanism with co-morbid fatigue and insomnia? Breast Cancer Res. 2015;17:89.
Toesca A, Pagnotta A, Zumbo A, Sadun R. Estrogen and progesterone receptors in carpal tunnel syndrome. Cell Biol Int. 2008;32:75–9.
Beckwee D, Leysen L, Meuwis K, Adriaenssens N. Prevalence of aromatase inhibitor-induced arthralgia in breast cancer: a systematic review and meta-analysis. Support Care Cancer. 2017;25:1673–86.
Nahm N, Mee S, Marx G. Efficacy of management strategies for aromatase inhibitor-induced arthralgia in breast cancer patients: a systematic review. Asia Pac J Clin Oncol. 2018;14:374–82.
Henry NL, Unger JM, Till C, Schott AF, Crew KD, Lew DL, et al. Association between body mass index and response to duloxetine for aromatase inhibitor-associated musculoskeletal symptoms in SWOG S1202. Cancer. 2019;125:2123–9.
Henry NL, Azzouz F, Desta Z, Li L, Nguyen AT, Lemler S, et al. Predictors of aromatase inhibitor discontinuation as a result of treatment-emergent symptoms in early-stage breast cancer. J Clin Oncol. 2012;30:936–42.
Khan QJ, Reddy PS, Kimler BF, Sharma P, Baxa SE, O’Dea AP, et al. Effect of vitamin D supplementation on serum 25-hydroxy vitamin D levels, joint pain, and fatigue in women starting adjuvant letrozole treatment for breast cancer. Breast Cancer Res Treat. 2010;119:111–8.
Prieto-Alhambra D, Javaid MK, Servitja S, Arden NK, Martinez-García M, Diez-Perez A, et al. Vitamin D threshold to prevent aromatase inhibitor-induced arthralgia: a prospective cohort study. Breast Cancer Res Treat. 2011;125:869–78.
Rastelli AL, Taylor ME, Gao F, Armamento-Villareal R, Jamalabadi-Majidi S, Napoli N, et al. Vitamin D and aromatase inhibitor-induced musculoskeletal symptoms (AIMSS): a phase II, double-blind, placebo-controlled, randomized trial. Breast Cancer Res Treat. 2011;129:107–16.
Hershman DL, Unger JM, Greenlee H, et al Effect of acupuncture vs sham acupuncture or waitlist control on joint pain related to aromatase inhibitors among women with early-stage breast cancer a randomized clinical trial. In: JAMA - J. Am. Med. Assoc. American Medical Association; 2018 pp 167–176
Bao T, Cai L, Giles JT, Gould J, Tarpinian K, Betts K, et al. A dual-center randomized controlled double blind trial assessing the effect of acupuncture in reducing musculoskeletal symptoms in breast cancer patients taking aromatase inhibitors. Breast Cancer Res Treat. 2013;138:167–74.
Greenlee H, Crew KD, Shao T, Kranwinkel G, Kalinsky K, Maurer M, et al. Phase II study of glucosamine with chondroitin on aromatase inhibitor-associated joint symptoms in women with breast cancer. Support Care Cancer. 2013;21:1077–87.
Henry NL, Unger JM, Schott AF, et al Randomized, multicenter, placebo-controlled clinical trial of duloxetine versus placebo for aromatase inhibitor-associated arthralgias in early-stage breast cancer: SWOG S1202. In: J. Clin. Oncol. American Society of Clinical Oncology; 2018pp 326–332
Mease PJ, Spaeth M, Clauw DJ, Arnold LM, Bradley LA, Russell IJ, et al. Estimation of minimum clinically important difference for pain in fibromyalgia. Arthritis Care Res. 2011;63:821–6.
Paulsen CE, Armache JP, Gao Y, Cheng Y, Julius D. Structure of the TRPA1 ion channel suggests regulatory mechanisms. Nature. 2015;520:511–7.
Fusi C, Materazzi S, Benemei S, Coppi E, Trevisan G, Marone IM, et al. Steroidal and non-steroidal third-generation aromatase inhibitors induce pain-like symptoms via TRPA1. Nat Commun. 2014;5:5736. https://doi.org/10.1038/ncomms6736.
Biggs JE, Stemkowski PL, Knaus EE, Chowdhury MA, Ballanyi K, Smith PA. Suppression of network activity in dorsal horn by gabapentin permeation of TRPV1 channels: Implications for drug access to cytoplasmic targets. Neurosci Lett. 2015;584:397–402.
Giorgi S, Nikolaeva-Koleva M, Alarcón-Alarcón D, Butrón L, González-Rodríguez S. Is TRPA1 burning down TRPV1 as druggable target for the treatment of chronic pain? Int J Mol Sci. 2019;20. https://doi.org/10.3390/ijms20122906.
Khan QJ, Kimler BF, Reddy PS, Sharma P, Klemp JR, Nydegger JL, et al. Randomized trial of vitamin D3 to prevent worsening of musculoskeletal symptoms in women with breast cancer receiving adjuvant letrozole. The VITAL trial. Breast Cancer Res Treat. 2017;166:491–500.
Mcmurdo MET, Sumukadas D, Donnan PT, Cvoro V, Rauchhaus P, Argo I, et al. Spironolactone for people age 70 years and older with osteoarthritic knee pain: a proof-of-concept trial. Arthritis Care Res. 2016;68:716–21.
Roberts KE, Rickett K, Feng S, Vagenas D, Woodward NE (2020) Exercise therapies for preventing or treating aromatase inhibitor-induced musculoskeletal symptoms in early breast cancer. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD012988.pub2
Lu G, Zheng J, Zhang L. The effect of exercise on aromatase inhibitor-induced musculoskeletal symptoms in breast cancer survivors :a systematic review and meta-analysis. Support Care Cancer. 2020;28:1587–96.
Irwin ML, Cartmel B, Gross CP, Ercolano E, Li F, Yao X, et al. Randomized exercise trial of aromatase inhibitor-induced arthralgia in breast cancer survivors. J Clin Oncol. 2015;33:1104–11.
Patel AV, Friedenreich CM, Moore SC, et al. American College of Sports Medicine Roundtable report on physical activity, sedentary behavior, and cancer prevention and control. Med Sci Sports Exerc. 2019;51:2391–402.
Nyrop KA, Callahan LF, Cleveland RJ, Arbeeva LL, Hackney BS, Muss HB. Randomized controlled trial of a home-based walking program to reduce moderate to severe aromatase inhibitor-associated arthralgia in breast cancer survivors. Oncologist. 2017;22:1238–49.
Arem H, Sorkin M, Cartmel B, Fiellin M, Capozza S, Harrigan M, et al. Exercise adherence in a randomized trial of exercise on aromatase inhibitor arthralgias in breast cancer survivors: the Hormones and Physical Exercise (HOPE) study. J Cancer Surviv. 2016;10:654–62.
van Waart H, van Harten WH, Buffart LM, Sonke GS, Stuiver MM, Aaronson NK. Why do patients choose (not) to participate in an exercise trial during adjuvant chemotherapy for breast cancer? Psychooncology. 2016;25:964–70.
Shaw BA, Spokane LS. Examining the association between education level and physical activity changes during early old age. J Aging Health. 2008;20:767–87.
Bartlett DB, Willis LH, Slentz CA, Hoselton A, Kelly L, Huebner JL, et al. Ten weeks of high-intensity interval walk training is associated with reduced disease activity and improved innate immune function in older adults with rheumatoid arthritis: a pilot study. Arthritis Res Ther. 2018;20:127. https://doi.org/10.1186/s13075-018-1624-x.
Burghardt RD, Kazim MA, Rüther W, Niemeier A, Strahl A. The impact of physical activity on serum levels of inflammatory markers in rheumatoid arthritis: a systematic literature review. Rheumatol Int. 2019;39:793–804.
Rausch Osthoff AK, Niedermann K, Braun J, Adams J, Brodin N, Dagfinrud H, et al. 2018 EULAR recommendations for physical activity in people with inflammatory arthritis and osteoarthritis. Ann Rheum Dis. 2018;77:1251–60.
Roll SC, Hardison ME. Effectiveness of occupational therapy interventions for adults with musculoskeletal conditions of the forearm, wrist, and hand: a systematic review. Am J Occup Ther. 2017;71:7101180010p1–7101180010p12. https://doi.org/10.5014/ajot.2017.023234.
Harth A, Germann G, Jester A. Evaluating the effectiveness of a patient-oriented hand rehabilitation programme. J Hand Surg Eur Vol. 2008;33:771–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Conflict of Interest
The author declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Cancer Rehabilitation
Rights and permissions
About this article
Cite this article
Oza, S. Aromatase Inhibitor-induced Musculoskeletal Syndrome: a Review of Rehabilitation Interventions. Curr Phys Med Rehabil Rep 9, 119–126 (2021). https://doi.org/10.1007/s40141-021-00318-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40141-021-00318-3