Abstract
Purpose of Review
Enhanced Recovery After Surgery (ERAS) protocols have shown significant success in improving pain scores and postoperative recovery and reducing hospital length of stay. Since the initial application in the colorectal patient population in the late 1990s, ERAS pathways have expanded to include many surgical subspecialties. This review explores the applicability of ERAS and its components in the field of cranial and spinal surgery.
Recent Findings
Only recently have researchers begun to study how to apply ERAS principles to intracranial or spine procedures. To date, robust evidence is lacking. Spine surgery patients benefit from preoperative education and early physical therapy, but how anesthetic or analgesic choice impacts recovery remains unclear. Additionally, there is a dearth of high-quality evidence to support the specific use of ERAS in cranial surgery. One randomized controlled trial, however, indicates that there is value in further study of ERAS care standardization in cranial neurosurgery and that concerns about increased complications may be unfounded. Regardless of adherence to ERAS components, the nature of intracranial surgery carries a high risk for morbidity and neurologic deficit.
Summary
Patients across multiple surgical specialties benefit from ERAS protocols. Early studies suggest many of the components in these protocols can be advantageous in neurosurgery. However, how to tailor them to the neurosurgical patient is still evolving.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction to Enhanced Surgical Recovery
Enhanced Recovery After Surgery (ERAS) describes a comprehensive set of evidence-based, multidisciplinary approaches to preoperative, intraoperative, and postoperative interventions. ERAS pathways strive to minimize perturbations in normal physiology in the perioperative period to decrease hospital length of stay and avoid decreases in patient-reported outcome measures (PROMs), without increasing the rates of readmission or complications. The concept of ERAS was developed in the late 1990s by Dr. Henrik Kehlet, a Danish colorectal surgeon. Although ERAS protocols were first proposed and studied in colorectal surgery [1], many of the principles apply to other surgical fields. Published ERAS protocols are available for colorectal, gynecological, liver, urological, breast reconstruction, pancreatic, bariatric, and head and neck surgery. These protocols are maintained by the ERAS Society guideline groups. At the authors’ institution, ERAS introduction began with colorectal surgery and, over a period of approximately five years, based on the successful results of the initial programs, has expanded to 12 surgical service lines, including spine surgery.
This chapter explores the evidence available for ERAS in neurosurgery, limited to craniotomy and spine surgery.
ERAS’s early primary metric of success was the hospital-centric measurement of hospital length of stay (LOS). More recently, emphasis has been placed on PROMs, validated questionnaires completed by patients that assign a numerical score to the assessed outcome. Many outcomes measured by PROMs relate to quality of life and degree of independence [2], and these are captured by metrics such as the World Health Organization’s Disability Assessment Score [3] (WHODAS). Financial metrics are also critical to the success of ERAS programs in that hospital systems require evidence that the upfront investment in these projects benefits both patient outcomes and the fiscal health of the institution. Quantifying the financial costs and benefits of care standardization programs is difficult and is best accomplished and sustained by involving a multidisciplinary team that includes clinical, revenue cycle, billing and coding, and decision support personnel.
When a hospital-wide ERAS program is implemented systematically and deliberately, the potential exists for dramatic improvements in patient outcomes and hospital expenditures. A recent multi-year audit of ERAS programs at a single institution demonstrated a significant decrease in postoperative hospital length of stay across all programs (1.5 days, p < 0.001), an association with improved 30-day survival (OR 1.04, p = 0.001), and a financial impact of 44% savings (p < 0.001) when ERAS protocols reached high levels (> 80%) of adherence [4].
Components of Enhanced Recovery Protocols
Greenshields and Mythen [2] have described the development of enhanced recovery programs over the past decade and the common components found across surgical disciplines. These components are categorized by time period across the patient’s perioperative journey (Table 1). The overarching goals are to present a well-optimized and educated patient for surgery, perform the least invasive surgical procedure while maintaining normal physiology throughout the perioperative period, and minimize interventions that prevent successful discharge from hospital (e.g., nasogastric tubes, surgical drains, opioid medications, and late nutrition). The overall success of ERAS programs is typically measured by monitoring practitioner adherence to the established protocol, realizing shorter inpatient hospital stays, and not increasing readmissions.
ERAS for Spine Surgery
Key concepts for developing a successful ERAS pathway for spine surgery should focus on pre(peri)operative education and health optimization, limiting the use of long-acting opioids, use of minimally invasive surgical approaches, targeted fluid and hemodynamic management, early physical therapy and mobilization, and appropriate nutrition (Fig. 1).
Few studies have focused specifically on ERAS pathways as they related to spinal surgeries. Staartjes et al. [5] found that standardizing surgical approach and anesthetics shortened the length of the surgical procedure; additionally, time to discharge was lowered, but this was not statistically significant. While trying to adhere to non-opioid analgesics postoperatively, they did not comment on preoperative or intraoperative multimodal analgesia, nor did they comment on the amount of opioids needed postoperatively. The study was also limited to patients in ASA Physical Status 2 or lower, body mass index (BMI) < 33, and patients undergoing minimally invasive surgery. Similarly, Soffin et al. [6] were unable to achieve all the benefits seen in the early ERAS studies. The observed differences between patients assigned to ERAS and “usual care” were limited to time to oral intake, decrease in opioid consumption on postoperative day (POD1), and less pain with physical therapy on POD1. The Quality of Recovery 40 (QoR-40) scores were statistically higher compared with patients receiving “usual care,” but were impacted mostly by reductions in postoperative nausea and vomiting (PONV). By 2–3 weeks, QoR-40 scores were comparable. What does stand out in their study was that significantly more time was spent with the ERAS group on patient education regarding expectations for recovery, pain, physical therapy, nutrition goals, use of non-opioid analgesia and opioids, and the patient’s role in recovery. Additionally, compliance to all enhanced recovery process measures was considerably higher in their ERAS group. This study’s limitations were the small sample size (50 patients) and that the majority of the patients were ASA 1 or 2. Furthermore, the authors failed to define “usual care” for their non-ERAS group.
Multimodal Analgesia
Many ERAS studies focus on multimodal analgesia/anesthesia as a key component of the ERAS pathway, looking to limit the use of long-acting opioids. Approaches studied range from the use of preoperative gabapentinoids and acetaminophen to ketorolac and methadone, total intravenous anesthesia (TIVA) versus combination of volatile and IV anesthetics, lidocaine infusion, ketamine boluses and/or infusions, dexmedetomidine, and postoperative gabapentinoids, among others (Table 2). Data, however, show conflicting or inconclusive results. When multiple pre-emptive non-opioid analgesics are given preoperatively, the effectiveness of individual drugs is uncertain.
Acetaminophen has become one of the most commonly used preoperative analgesics across all surgical services. Hansen et al. [7] compared IV with oral acetaminophen, demonstrating a reduction in total opioid consumption and shorter hospital length of stay (LOS). Mörwald et al. [8], however, were unable to replicate these results. Acetaminophen, with its moderate analgesic effect, may have marked benefit in reducing opioid consumption in the late postoperative phase once acute pain has been mitigated.
In 2006, Hurley et al. [9] showed a decrease in rated pain with gabapentin, and a reduction in opioid consumption over the first 24 h postoperatively, but with an increase in dizziness, sedation, and visual disturbances. More recently, in a meta-analysis of 281 trials[21] examining the use of perioperative gabapentinoids, Verret et al. found a slightly lower pain intensity rating in the first 48 h but deemed that it was not clinically meaningful. Additionally, lower, but not clinically significant, opioid use was observed. A reduction in PONV was offset by a notable increase in dizziness, visual disturbances (with pregabalin), and hospital LOS [21].
Nonetheless, Raja et al. [10] demonstrated that the combination of pregabalin, acetaminophen, and ketorolac led to earlier ambulation and lowered opioid requirements and hospital LOS. However, caution is urged. While ketorolac can lower opioid requirements, Li et al. [20] showed adverse effects on spinal fusion if given for > 2 days or at dose of > / = 120 mg/day. Use of ketorolac should be discussed with the surgeon in advance.
Lidocaine and ketamine have been integrated into ERAS pathways because of long observed benefits for pain management. Systemic lidocaine can have analgesic and anti-inflammatory effects. A meta-analysis [11] of lidocaine use in spine surgery showed overall reduction in pain scores and opioid consumption but did not demonstrate a difference in LOS. Ketamine, an N-methyl-d-aspartate (NMDA) receptor inhibitor, has had proven efficacy for pain reduction. In a Cochrane review [12] of ketamine in 130 studies, given to 8341 patients, used across multiple surgical specialties, the authors concluded that ketamine “probably” reduced postoperative analgesic consumption and lowered pain intensity. They did not comment on LOS but noted that there was a mild reduction in PONV. Recently, however, in the PODCAST study [13], the investigators failed to see a benefit in pain scores or opioid consumption comparing 0.5 mg/kg or 1.0 mg/kg bolus doses of ketamine with placebo. And, while ketamine did not have any notable deliriogenic impact, at increasing doses, patients reported more visual hallucinations and nightmares.
Dexmedetomidine is another agent being considered for use as part of ERAS pathways. It has opioid-sparing properties, can decrease total anesthetic requirements, and contributes to a reduced systemic stress response due to effects on the hypothalamic–pituitary–adrenal axis [14]. Potentially, the reduction in delirium seen in the ICU setting [22] with the use of dexmedetomidine could translate to the operating room. Its use could help reduce and prevent postoperative delirium or cognitive dysfunction, further reducing LOS. One study by Chen et al. [15] demonstrated that patients receiving dexmedetomidine had less of an increase in IL-6 and TNF-alpha levels. In their study, elevated cytokines were associated with a higher incidence of postoperative cognitive dysfunction (POCD). However, in a study by Steiner et al. [16], rates of postoperative delirium/dysfunction did not differ between the dexmedetomidine group and placebo. They also did not see a reduction in the amount of fentanyl used intraoperatively. Similarly, Naik et al. [17] failed to see a decrease in opioid consumption or pain scores with dexmedetomidine use. And, in a study by Bekker et al. [18], while postoperative rise in serum levels of cortisol and IL-10 was attenuated by dexmedetomidine, clinically, the only statistically significant clinical benefit was seen in the QoR-40 score on POD3.
Methadone should be considered for patients with significant neuropathic pain or who have been on opioids chronically. It has multiple beneficial characteristics: It is a potent mu-opioid receptor agonist and an NMDA receptor inhibitor, and it inhibits reuptake of serotonin and norepinephrine. These properties all help control pain, prevent hyperalgesia, and potentially elevate mood, which can affect perceived pain. In a study by Murphy et al. [19], patients who received methadone reported better pain scores in the PACU, and on PODs 1–3 had reduced opioid consumption and overall better satisfaction scores.
Developing an ERAS pathway that applies to all patients undergoing spine surgery has proven challenging. Attempts to translate evidence from early studies on colorectal patients have not produced consistent outcomes. Attempts to develop multimodal anesthetic and pain pathways have also not been as conclusive. Most recently, in a study by Maheswari K et al. [23], patients receiving preoperative acetaminophen, in addition to lidocaine and ketamine infusions intraoperatively, did not show any meaningful clinical benefit in terms of physical recovery (QoR-40) or opioid reduction compared with patients who did not receive the same intra- or preoperative management. Spine surgeries are historically very painful and invasive procedures, on patients who may already have significant physical or neuropathic pain. Developing the appropriate perioperative management pathway for these patients cannot be based solely on pharmacology. It is important to note that ERAS pathways as originally developed have 24 core components. Focusing on only one component will, not surprisingly, lead to mixed results. Studies focusing on preoperative education and health optimization have shown promise [6]. Optimizing surgical techniques by decreasing tissue trauma and decreasing length of surgery is also beneficial [5].
Regarding the analgesic component of an ERAS pathway for neurosurgery, the evidence is unfortunately mixed. The ERAS Society recently released a consensus statement supporting use of acetaminophen, NSAIDs, and gabapentinoids [24]. However, recent evidence that gabapentin is associated with sedation and visual disturbances suggests that it may be best to avoid gabapentinoids in elderly patients, or at least use a lower dose. Given the use of somatosensory evoked potentials and motor evoked potentials in spine surgery, the anesthetic approach is already geared toward IV-based anesthetic. The best combination is debatable. Dexmedetomidine may potentially limit the inflammatory response, allow a reduction in propofol and/or opioid infusions, and provide good hemodynamic stability in elderly patients in whom an increased heart rate or low blood pressure would be detrimental. The evidence to support these benefits is mixed. Ketamine use in some cases has shown considerable reduction in postoperative opioid requirements and pain scores, but other studies showed no significant difference. Given its potential to cause hallucinations and nightmares, it may be best to avoid ketamine in elderly patients to prevent delirium. In chronic pain patients on opioids for extended periods, lidocaine and methadone could help reduce postoperative pain and opioid requirements.
There is also growing evidence and support for the use of regional techniques performed intraoperatively to ameliorate postoperative pain. The use of intrathecal or epidural analgesia, or wound infiltration for pain control has shown reduction in early postoperative opioid use and improved patient satisfaction [24]. Alternatively, others have shown benefits from erector spinae blocks and thoracolumbar interfascial plane (TLIP) blocks for postoperative pain control. Both techniques provide analgesia by blocking the dorsal rami and have shown effective postoperative pain control and a reduction in early postoperative opioid consumption [25]. Furthermore, intraoperative nerve monitoring is not affected, and patients can have a reliable postoperative motor exam. However, because of significant craniocaudal spread, caution should be exercised with the erector spinae block on cervical spine patients as this can block phrenic nerves and contribute to pulmonary compromise. Additionally, Garg et al. [25] note the possibility of using a spinal anesthetic as the primary anesthetic in certain instances. The articles reviewed report better hemodynamic stability, less blood loss, and better patient satisfaction compared with general anesthesia. However, this approach is somewhat limited in its scope, recommended for non-obese patients having procedures shorter than 2 h, minimally invasive spine surgeries, procedures involving no more than 1–2 levels, and below the level of T10. Above T10, this approach may contribute to intercostal paralysis and compromise pulmonary function.
Opioid-sparing techniques have been “in vogue” for a number of years. Multimodal analgesia can lead to significant opioid sparing, specifically in the intraoperative phase. However, the benefits of opioid sparing may not outweigh the challenges of inadequate postoperative analgesia in some patients. Therefore, titration of analgesics based on individual patient needs is important to enhance recovery and improve patient satisfaction [26].
Fluids and Hemodynamic Management
Intraoperative fluid management is another component of ERAS programs. It can significantly impact hemodynamics intraoperatively and play an important role in the postoperative recovery of spine patients. Hypovolemia can lead to hypotension, end-organ hypoperfusion, and ischemia. Conversely, hypervolemia should be avoided because it can contribute to hemodilution, coagulopathy, and increased bleeding, which may increase the need for transfusions of blood products. It can also cause peripheral and/or pulmonary edema. Euvolemia should be maintained to provide optimal blood pressure for spinal cord perfusion. Many parameters together can guide appropriate fluid therapy: lactate levels, stroke volume variation (SVV), urinary output (UOP), and hemodynamics. In a study by Bacchin et al. [27] using an SVV-based protocol to direct fluid therapy, the authors reported that if less crystalloid was given, estimated blood loss was lower, and fewer transfusions were needed. It was also noted that peak lactate levels were lower, and postoperatively patients had less pulmonary congestion seen on chest x-ray, required less oxygen support, had earlier return of bowel function, and were discharged home earlier. Prevention of hypothermia, a streamlined surgical approach/technique, and the use of an antifibrinolytic as part of standard care (when not contraindicated) can reduce blood loss and thus prevent hypovolemia and end-organ hypoperfusion. A meta-analysis by Li et al. [28] showed that antifibrinolytics were able to reduce perioperative blood loss and transfusion requirements in spine surgery, with tranexamic acid (TXA) being the more effective of the agents. Multiple dosing regimens for TXA are in use and vary from 10 to 50 mg/kg bolus, followed by varying infusion rates based on institutional preference.
In addition to fluid management, appropriate blood pressure (BP) management is critical. When there is trauma to the spinal cord or concern for cord compression and potential myelopathy, surgeons may request mean arterial pressure (MAP) goals > 80–85 mmHg. Otherwise, normotension should be the goal. Once euvolemia is achieved, the addition of a vasopressor such as phenylephrine or norepinephrine may be necessary and preferred over additional volume transfusion to achieve desired BP goals. But, if additional volume is warranted, the use of colloid over exclusively using crystalloid may prevent extravascular volume losses and tissue edema, which can compromise perfusion.
Postoperative Care
Postoperatively, adequate pain control and prevention of nausea and vomiting are critical for early discharge from the post anesthesia care unit (PACU) and overall quality of recovery. Opioids should be used judiciously only when necessary to minimize opioid related adverse events. However, if, despite the use of multimodal analgesic approaches, patients continue to have significant postoperative pain hindering recovery and necessitating significant opioid consumption, it is best to seek consultation from your institution’s acute pain service.
Early mobilization with physical therapy and optimal nutrition contribute to good recovery. Malnourished patients have significantly higher postoperative morbidity, mortality, and LOS and increased hospital costs [29,30,31]. Enteral nutrition should be resumed as soon as possible, and high-protein diet is recommended by the American Society for Enhanced Recovery (ASER) in their consensus statement [31]. Reiterating preoperative discussions of goals and expectations facilitates good patient cooperation and ultimately satisfactory outcomes.
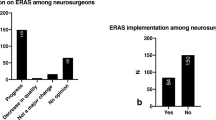
ERAS for Cranial Surgery
Enhanced recovery pathways for cranial neurosurgery have developed slowly in comparison to other surgical specialties. The reasons are unclear, but one factor may be that ERAS protocols typically promote more rapid discharge from hospital, and neurosurgical teams may be reluctant to strive for this goal in a population with a high rate of postoperative complications and morbidity. In many institutions, it is common for all cranial surgery patients to be monitored postoperatively in the intensive care unit, while many of the common components of ERAS (e.g., minimizing tubes and drains, early mobilization) are still relatively novel in critical care units. Independent of the inherent risk of surgical complications, many components of ERAS protocols can be adapted to use in the cranial neurosurgery population.
It should be noted, however, that there is a dearth of high-quality evidence to support the specific use of ERAS in cranial surgery, with significant opportunity to contribute to the body of evidence. In 2016, Hagan et al. published a comprehensive review of enhanced recovery approaches to oncologic craniotomy [32], but much of the evidence they evaluated comes from other surgical populations and its use in cranial surgery was extrapolated. In a similar paper in 2017, Mishra et al. also reviewed the broader literature for ERAS interventions that could be applied to cranial neurosurgery, but, again, they described minimal evidence specific to neurosurgery [33]. Both reviews provide a robust conceptual framework for ERAS in cranial neurosurgery but fail to present specific evidence to inform neurosurgical practice.
One randomized controlled trial has investigated the impact of a care-standardization ERAS protocol in cranial neurosurgery. Wang et al. published a trial of 140 subjects randomized to usual care or a standardized ERAS pathway [34]. This group’s protocol included all the usual components of an ERAS care pathway but interestingly did not include regional analgesia (i.e., scalp blockade) or other maneuvers to minimize long-acting opioid use. The primary endpoint was hospital length of stay, and the ERAS group was discharged significantly sooner (median 4 days) than the usual care group (median 7 days, p < 0.0001) without an increase in readmissions or complications. This relatively small, single-center study indicates that there is potential value in further study of ERAS care standardization in cranial neurosurgical patients, and that concerns about increased complications may be unfounded.
Venkatraghavan et al. describe their experience with an ERAS approach to supratentorial craniotomy surgery in a large series of nearly 200 patients booked for same-day discharge [35]. Successful same-day discharge was achieved in 88% of patients with 2.9% requiring readmission to hospital within 12 h of discharge. The majority of these patients were treated with an awake craniotomy approach (intravenous sedation plus regional anesthesia) rather than general anesthesia, which in the authors’ experience leads to a more rapid return to baseline neurologic status, ambulation, and oral intake, all factors necessary for either same-day discharge from hospital or postoperative care in a lower acuity ward than the ICU. In the extensive experience of the Toronto, Canada, neuroanesthesia group, as well as both of the authors’ institutions, the use of regional anesthesia in the form of scalp blocks for both awake and asleep craniotomy makes a clinically significant difference in the immediate recovery and in-hospital analgesic requirements of patients. This is certainly an area of focus that merits further investigation.
Directions of Future Research
A recent systematic review of ERAS protocols for craniotomy reported just three randomized studies with inconsistent research endpoints other than length of hospital stay; furthermore, there was not a significant difference in LOS [36]. The primary conclusion to be drawn from this review is that the dearth of high-quality randomized evidence to support or refute ERAS management in cranial neurosurgery persists.
Cranial neurosurgery and the perioperative care of these patients are poised to join the myriad other surgical specialties that have embraced the concept of ERAS. Strong evidence exists in many other surgical disciplines that logically can be extrapolated to neurosurgical patients. However, cranial neurosurgery-specific research must be undertaken pragmatically to determine whether ERAS care standardization will have the same direction and magnitude of impact on the outcomes of neurosurgical patients. The work of Wang et al. [8] should be replicated on a larger scale across multiple institutions to inform a definitive answer about the future of ERAS in the complex realm of cranial neurosurgery.
Conclusion
Anesthesiologists play a major role in the development and implementation of ERAS pathways. An optimal ERAS pathway will incorporate multiple components of the health care system to provide clearly defined expectations preoperatively and incorporate evidence-based practice for all aspects of patient care. Unfortunately, robust evidence is lacking; until such evidence becomes available, our quest must continue.
References
Wilmore DW, Kehlet H. Management of patients in fast track surgery. BMJ. 2001;322(7284):473–6.
Greenshields N, Mythen M. Enhanced recovery after surgery. Curr Anesthesiol Rep. 2020;10(1):49–55.
Andrews G, et al. Normative data for the 12 Item WHO Disability Assessment Schedule 2.0. PLOS ONE. 2009;4(12):e8343.
Pickens RC, et al. Impact of multidisciplinary audit of Enhanced Recovery After Surgery (ERAS)® programs at a single institution. World J Surg. 2021;45(1):23–32.
Staartjes VE, Wispelaere MPD, Schröder ML. Improving recovery after elective degenerative spine surgery: 5-year experience with an Enhanced Recovery After Surgery (ERAS) protocol. Neurosurg Focus FOC. 2019;46(4):E7.
Soffin EM, et al. Enhanced recovery after lumbar spine fusion: a randomized controlled trial to assess the quality of patient recovery. Anesthesiology. 2020;133(2):350–63.
Hansen RN, et al. Comparative analysis of length of stay, hospitalization costs, opioid use, and discharge status among spine surgery patients with postoperative pain management including intravenous versus oral acetaminophen. Curr Med Res Opin. 2017;33(5):943–8.
Mörwald EE, et al. Intravenous acetaminophen does not reduce inpatient opioid prescription or opioid-related adverse events among patients undergoing spine surgery. Anesth Analg. 2018;127(5):1221–8.
Hurley R, et al. The analgesic effects of perioperative gabapentin on postoperative pain: a meta-analysis. Reg Anesth Pain Med. 2006;31:237–47.
Raja SD, et al. A prospective randomized study to analyze the efficacy of balanced pre-emptive analgesia in spine surgery. Spine J. 2019;19(4):569–77.
Bi Y, et al. Effect of perioperative intravenous lidocaine for patients undergoing spine surgery: a meta-analysis and systematic review. Medicine. 2020;99(48):e23332–e23332.
Brinck EC, et al. Perioperative intravenous ketamine for acute postoperative pain in adults. Cochrane Database Syst Rev. 2018;12(12):Cd012033.
Avidan MS, et al. Intraoperative ketamine for prevention of postoperative delirium or pain after major surgery in older adults: an international, multicentre, double-blind, randomised clinical trial. Lancet. 2017;390(10091):267–75.
Mo Y, Zimmermann AE. Role of dexmedetomidine for the prevention and treatment of delirium in intensive care unit patients. Ann Pharmacother. 2013;47(6):869–76.
Chen W, et al. The effects of dexmedetomidine on post-operative cognitive dysfunction and inflammatory factors in senile patients. Int J Clin Exp Med. 2015;8(3):4601–5.
Deiner S, et al. Intraoperative infusion of dexmedetomidine for prevention of postoperative delirium and cognitive dysfunction in elderly patients undergoing major elective noncardiac surgery: a randomized clinical trial. JAMA Surg. 2017;152(8):e171505.
Naik BI, et al. The effect of dexmedetomidine on postoperative opioid consumption and pain after major spine surgery. Anesth Analg. 2016;122(5):1646–53.
Bekker A, et al. The effect of intraoperative infusion of dexmedetomidine on the quality of recovery after major spinal surgery. J Neurosurg Anesthesiol. 2013;25(1):16–24.
Murphy GS, et al. Clinical effectiveness and safety of intraoperative methadone in patients undergoing posterior spinal fusion surgery: a randomized, double-blinded, controlled trial. Anesthesiology. 2017;126(5):822–33.
Li J, et al. The effect of ketorolac on thoracolumbar posterolateral fusion: a systematic review and meta-analysis. Clin Spine Surg. 2018;31(2):65–72.
Verret M, et al. Perioperative use of gabapentinoids for the management of postoperative acute pain: a systematic review and meta-analysis. Anesthesiology. 2020;133(2):265–79.
Pandharipande PP, et al. Effect of dexmedetomidine versus lorazepam on outcome in patients with sepsis: an a priori-designed analysis of the MENDS randomized controlled trial. Crit Care. 2010;14(2):R38.
Maheshwari K, et al. Multimodal analgesic regimen for spine surgery: a randomized placebo-controlled trial. Anesthesiology. 2020;132(5):992–1002.
Debono B, et al. Consensus statement for perioperative care in lumbar spinal fusion: Enhanced Recovery After Surgery (ERAS(R)) Society recommendations. Spine J. 2021;21(5):729–752.
Garg B, et al. Regional anesthesia for spine surgery. Clin Spine Surg. 2020.
Shanthanna H, et al. Perioperative opioid administration. Anesthesiology. 2021;134(4):645–59.
Bacchin MR, et al. Goal-directed fluid therapy based on stroke volume variation in patients undergoing major spine surgery in the prone position a cohort study. Spine (Phila Pa 1976). 2016;41(18):E1131-e1137.
Li G, et al. Efficacy of antifibrinolytic agents on surgical bleeding and transfusion requirements in spine surgery: a meta-analysis. Eur Spine J. 2017;26(1):140–54.
Correia MI, Waitzberg DL. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr. 2003;22(3):235–9.
Kassin MT, et al. Risk factors for 30-day hospital readmission among general surgery patients. J Am Coll Surg. 2012;215(3):322–30.
Wischmeyer PE, et al. American Society for Enhanced Recovery and Perioperative Quality Initiative Joint Consensus Statement on nutrition screening and therapy within a surgical enhanced recovery pathway. Anesth Analg. 2018;126(6):1883–95.
Hagan KB, et al. Enhanced recovery after surgery for oncological craniotomies. J Clin Neurosci. 2016;24:10–6.
Mishra RK, et al. Enhanced recovery after surgery: neuroanaesthetic perspective. J Neuroanaesthesiol Crit Care. 2017;04(01):017–22.
Wang Y, et al. Safety and efficacy of a novel neurosurgical Enhanced Recovery After Surgery protocol for elective craniotomy: a prospective randomized controlled trial. Journal of Neurosurgery JNS. 2019;130(5):1680.
Venkatraghavan L, et al. Same-day discharge after craniotomy for supratentorial tumour surgery: a retrospective observational single-centre study. Can J Anaesth. 2016;63(11):1245–57.
Kapoor I, Mahajan C, Prabhakar H. Enhanced Recovery After Surgery (ERAS) for patients undergoing craniotomy: a systematic review. J Neurosurg Anesthesiol. 2021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Roy C. Neeley declares that he has no conflict of interest. Ryan S. Smith declares that she has no conflict of interest. Letha Mathews is a member of the Education Committee for the Society for Neuroscience in Anesthesiology and Critical Care (SNACC).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Neuroanesthesia
Rights and permissions
About this article
Cite this article
Neeley, R.C., Smith, R.S. & Mathews, L. Enhanced Recovery After Neurosurgery. Curr Anesthesiol Rep 11, 298–305 (2021). https://doi.org/10.1007/s40140-021-00478-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-021-00478-x