Abstract
Point-of-care (POC) ultrasonography can be defined as ultrasonography brought to the patient and performed by the provider in real time. Anesthesiologists commonly use this modality to aid regional anesthesia and central vascular access. However, as POC ultrasonography has been further developed, utility of this technology has increased in the areas of hemodynamic monitoring, cardiopulmonary function, and other areas that are relevant for the perioperative physician. This manuscript seeks to provide a review of the literature of point-of-care ultrasound topics that are relevant for the anesthesiologist. These topics will include (I) assessment of preload and fluid responsiveness, (II) assessment of mechanisms of hypotension and shock, (III) evaluation of pulmonary function, (IV) advanced vascular access, and (V) additional areas of POC ultrasound for perioperative improvement. Finally, this manuscript will suggest a novel POC ultrasound curriculum that integrates the components of this review into a comprehensive perioperative ultrasound examination, abbreviated as FORESIGHT (focused, perioperative, risk, evaluation, sonography, involving, gastro-abdominal, hemodynamic, and trans-thoracic ultrasound) exam.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
With recent changes in the medical environment, the concept of anesthesiologists embracing more of a role in perioperative medicine has been widely reported and has even been published as being essential for our specialty to thrive [1]. Continued expansion into a broader role as perioperative physicians will encompass many aspects of the “non-operative” care of the patient undergoing surgery. This new role will also cause anesthesiologists to more frequently face issues involving patient’s cardiac, pulmonary, hemodynamic, and gastrointestinal status in both the preoperative and postoperative arenas.
Early ultrasound devices were large and often confined to imaging laboratories (cardiology, radiology, and obstetrics). With recent advances in ultrasound technology, these devices have become more portable, smaller, cheaper, and usable at the patient’s bedside [2]. Point-of-care (POC) ultrasound (US) refers to the use of portable ultrasonography at the patient’s bedside for diagnostic and therapeutic purposes [3]. Kendall et al. defined the characteristics of POC US examinations as follows: (1) an exam that has a well-defined purpose linked to improving patient outcomes, (2) focused and goal directed, (3) easily learned, (4) quickly performed, and (5) performed at the patient’s bedside [3]. POC US has proven to serve a vital role in the rapid assessment of the patient’s cardiac, pulmonary, hemodynamic, vascular, neurologic, and gastrointestinal status. Several other acute care specialties such as emergency medicine and critical care have also developed point-of-care (POC) ultrasound protocols to help assist the rapid assessment and management of their patients. As anesthesiologists redefine their role as perioperative physicians, they will be faced with similar clinical scenarios as these specialties. Thus, we seek to review the basics of clinical ultrasound and highlight the areas in which this technology may be useful in perioperative care.
Specifically, this chapter will discuss the following areas of POC ultrasound: (1) ultrasound physics and probe selection (2) preload and fluid responsiveness, (3) assessment of cardiac status and mechanisms of shock, (4)assessment of pulmonary status, (5) vascular access, and (6) additional topics. A novel US examination, abbreviated as FORESIGHT study (focused, perioperative, risk, evaluation, sonography, involving, gastro-abdominal, hemodynamic, and trans-thoracic ultrasound), incorporates these topics and has demonstrated to positively impact perioperative patient care [4••] (Fig. 1).
Ultrasound Physics and Probe Selection
Clinical ultrasound systems use transducers of a frequency between 2 and 27 MHz. Image production depends on the strength of the returning ultrasound signal and is directly related to the angle at which the beam strikes the acoustic interface. The ultrasound signal is described by its frequency and wavelength. A smaller wavelength results in a higher frequency, higher the resolution, but decreased penetration. Therefore, higher frequency probes (5–10 MHz) provide better resolution but can be applied only for superficial structures. Low frequency probes (2–5 MHz) provide better penetration but have a lower resolution. Probe selection is based on matching the properties of the ultrasound probe with the particular structure that the provider is trying to insonate. Besides frequency, additional properties of the probe include the footprint (area of which the ultrasound is emitted from) and the probe shape. Common ultrasound probes include the phased array, curved linear, and the linear. The phased array is characterized by a small foot print, a frequency of 3–5 MHz, and produces a wide ultrasound image by sending out pulses of ultrasound that are “stitched” together. The curved linear probe has a large footprint, frequency of 4–7 MHz, and the US waves are emitted (curved) which produces a wide image, making the probe ideal for abdominal examination. In contrast, the linear probe has a frequency of 10–27 MHz which provides the best image resolution and is ideal for superficial structures (Fig. 2).
The different modes of ultrasound utilize specific mechanisms to evaluate either static or dynamic anatomic structures. The standard 2-D image, also known as B-mode (brightness mode), involves sending echo pulses to a structure in which a fraction of the pulse is then reflected and collected by the transducer to produce an image. The amount of pulses received by the transducer directly correlates with the spot brightness of the US image. The fraction of the echo pulse that is reflected is dependent on the structures acoustic impedance. Acoustic gel is used to minimize the difference in acoustic impendence from the probe to the skin. M-mode (motion mode) is a graphic B-mode pattern that is a single screen line of ultrasound signal displayed over time and is used to assess the motion of structures along the ultrasound beam. Doppler ultrasound is a modality that is used to assess direction and intensity of flow. Doppler assesses the change in velocities secondary to the motion of the interested structure (usually blood flow). To optimize accuracy when using this modality, it is important to have the Doppler signal parallel to the direction of flow. With color Doppler, the Doppler echoes are displayed with colors corresponding to flow directed toward or away from the transducer (positive or negative Doppler shift). With continuous wave Doppler, one assesses the summation of velocities of flow along a line of ultrasound signal. Finally, pulse wave Doppler assesses flow velocity in an exact location but with the limitation of only being able to assess a range of velocities.
From each transducer position, the target structure is focused by three major movements: (1) Tilt which is scanning in the left–right direction (used to position structures in the middle of the screen), (2) Angle which is scanning in the anterior–inferior direction, and (3) rotation (clockwise–counterclockwise).
Preload and Fluid Responsiveness
There is evidence that either too little or too much fluid administration during the perioperative period can worsen organ function [5]. Administering the correct amount of fluid is an ongoing challenge due the inability to accurately measure parameters such as cardiac filling pressures. Historically, invasive measures like Central Venous Pressure have been used to estimate a patient’s preload status. It has been shown in numerous studies that CVP is a poor predictor of fluid responsiveness [6]. Certain POC US techniques can aid in optimizing fluid management in the perioperative arena.
Static Parameters for Filling Pressure Estimation
POC US has several non-invasive modalities to help determine the patient’s filling pressures. The diameter of the inferior vena cava (IVC) and its percent collapsibility from a maximal negative inspiratory breath have been shown to correlate to right atrial pressures. To obtain IVC measurements, one places a low frequency probe in the subxiphoid position with a sagittal ultrasound plane (Fig. 3). It is important to note that a spontaneous inspiratory breath will cause a decrease in IVC diameter while a mechanical inspiratory breath will cause an increase in IVC diameter, secondary to the difference in intrathoracic pressures. Specific guidelines for IVC measurements and their corresponding atrial pressures are listed in (Table 1) [7, 8]. Monitoring for collapsibility of the inferior vena cava (IVC) has been shown to be an effective measurement of reduced preload for both spontaneously breathing [9] as well as mechanically ventilated patients [10].
Another modality that helps identify filling pressures of the patient’s cardiovascular system involves the direct measurement of left ventricular end-diastolic area from a parasternal short axis view. Several studies have shown its utility in helping predict preload status in ventilated patients [11–13]. Key reference values from these studies suggest that reduced filling pressures may be present when the left ventricular end-diastolic area (LVEDA) is <8 cm2.
However, similar to central venous pressure, measurements of the IVC or LVEDA are “static” measurements of volume status, individual response is variable, and patients may not respond to fluid boluses as expected [14, 15]. In addition, impaired tissue oxygenation from decreased cardiac output may not be identified by these static parameters [16]. Thus, while these static parameters may be more reliable than traditional markers of hypovolemia such as urine output, they may not always predict fluid responsiveness.
Dynamic Parameters for Fluid Responsiveness
In comparison, dynamic flow parameters are used to identify whether a patient is fluid responsive, which is defined as an increase in stroke volume by 10 % from an intravascular fluid bolus (steep portion of the Frank–Starling curve). Dynamic flow parameters not simply require recording a static measurement but also involve comparing these measurements through several cardiac cycles. This makes it possible to monitor the effects of controlled pressure changes in the thorax created by mechanical ventilation on hemodynamic parameters. Briefly, this cardiopulmonary interaction is based on controlled cyclic inspiration and expiration during mechanical ventilation, which induces a regular change in intrathoracic positive pressure. This cyclic change stresses the filling condition of the heart to a degree that is directly correlated to intravascular volume of the patient. An example of a dynamic parameter that can be used to guide fluid management during controlled ventilation is evaluating the change in IVC diameter utilizing POC US.
Assessment of the IVC diameter change secondary to the mechanical ventilatory cycle has shown to predict fluid responsiveness. Specifically, the inferior vena cava diameter (D) at end-expiration (D min) and at end-inspiration (D max) was measured by echocardiography using a subcostal approach. The distensibility index of the IVC (dIVC) was calculated as the ratio of D max − D min/D min and expressed as a percentage. Measurements were performed at baseline and after a 7 ml/kg volume expansion using a plasma expander. Patients were separated into responders (increase in CI ≥15 %) and non-responders (increase in CI <15 %) [10]. Using a threshold dIVC of 18 %, responders and non-responders were discriminated with 90 % sensitivity and 90 % specificity [10]. Similar studies have been repeated in other settings such as with trauma patients in shock [17].
More intricate methods of using POC ultrasonography to determine volume status include the use of Doppler ultrasonography to measure the area under the flow curve, termed Velocity Time Integral (VTI), for structures that transmit the pulsatile systemic blood flow. For example, once the apical 4-chamber cardiac view is obtained, assessment of the respiratory variation during positive pressure mechanical ventilation of the VTI across the Left Ventricular Outflow Tract (LVOT) has been shown to indicate fluid responsiveness (Fig. 4) [18, 19]. This parameter relies on controlled mechanical ventilation with a uniform positive pressure. In this situation, a greater amount of respiratory variation of the VTI correlates with greater “preload dependence” or a greater increase in cardiac output from a fluid bolus. Across the multitude of studies measuring dynamic indices of fluid responsiveness, the percentage of variation threshold indicating “Fluid Responsive” is almost universally between 15 and 20 %. Feissel et al. found that a respiratory variation of the maximal flow velocity across the aorta of greater than 12 % or the VTI of greater than 20 % was a predictor of fluid responsiveness [20]. The same concepts are the basis for similar measurements performed across the brachial and other peripheral arteries [18, 19, 21].
In spontaneously breathing patients, one cannot use the controlled thorax pressure generation to predict fluid responsive as described above. Monnet et al. used the Passive Leg Raise as a means to determine fluid responsiveness. In their study, the VTI was measured across the aortic outflow using a 5-chamber apical view on TTE. The first measurement was taken with the patient in supine position. The second measurement of VTI was taken 1–3 min following the PLR when the patient had the equilibrated to the corresponding 300–500 ml increase in RV preload from the blood from the lower extremities. They found that an increase in aortic flow of >10 % was predictive of an increase in stroke volume of 15 % (sensitivity 97 %, specificity 94 %) [22]. Lamia et al. and Maizel et al. demonstrated similar findings with the “preload dependent” threshold being defined as a 12 % increase in VTI [23, 24]. This method has been found to be accurate with patients in atrial fibrillation, a condition which can make other dynamic indices, which rely on a regular cardiac rhythm and controlled mechanical ventilation to be erroneous [25, 26]. However, this method cannot be used to determine fluid responsiveness in patients with intra-abdominal hypertension [26].
Cardiac Status and Mechanism of Shock
In addition to the above modalities used to evaluate volume status, POC US has also proven to be critical during the assessment of hemodynamic instability and shock. POC US allows one to investigate the mechanism of injury, as well as cardiac function, causing instability. This section will review the methods commonly used in POC US that address these topics.
FAST (focused assessment with sonography for trauma) POC US exam
The focused assessment with sonography for trauma (FAST) [27] is the most studied example of focused clinical US in trauma care [9]. The purpose of bedside ultrasound in trauma is to rapidly identify free fluid (usually blood) in the peritoneal, retro-peritoneal, pericardial, or pleural spaces. The FAST exam has been shown to reliably detect >200 ml in body cavities. Indications include acute blunt or penetrating torso trauma, trauma in pregnancy, pediatric trauma, and sub acute torso trauma.
To review, the peritoneum is the serous membrane that forms the line of the abdominal cavity and overs most of the intra-abdominal organs. These peritoneal organs include stomach, spleen, liver, pancreas (only tail), parts of the colon, uterus, fallopian tubes, and ovaries. Because of this peritoneum layer, one is able to appreciate the collection of fluids between organs within the peritoneum to those either behind (retro-peritoneal) or below it (infra or sub-peritoneal). Retro-peritoneal structures include kidneys, IVC, aorta, and part of colon. Infra-peritoneal structures include bladder and distal rectum.
Both trauma patients and patients in the perioperative arena may have injuries that will cause significant blood loss but are not apparent on the initial physical exam. Studies have shown that 20–40 % of patients with significant abdominal injuries may initially have a normal physical examination of the abdomen [28, 29]. The FAST exam (Fig. 5) has been shown to be a highly effective tool in the detection of clinically significant hemoperitoneum and hemopericardium in the unstable patient [27, 30–32]. For the perioperative physician, the application of this exam allows one to rapidly determine if hemodynamic instability is secondary to injury of the pericardial and/or peritoneal space resulting in free fluid.
Assessment of Cardiac Function
Trans-thoracic examination of the cardiopulmonary system using bedside POC ultrasound technology has proven to be a reliable tool when compared to formal echocardiography [33]. Assessments of global left ventricular (LV) function, abdominal aorta size, and the presence of pericardial effusion showed a very strong correlation (r ≥ 0.92) between POC ultrasound and formal echocardiography examinations [33]. Similarly, correlation was also shown between right ventricular (RV) function and valvular function (excluding aortic stenosis) (r > 0.81) [33].
Perhaps the most integrated focused POC cardiac exam to date was proposed by Gunst et al. in 2008 with introduction of the “BEAT” (Bedside Echocardiographic Assessment in Trauma) examination. The study demonstrated that a focused cardiac TTE examination correlated well with pulmonary artery catheter (PAC) data regarding cardiac function and volume status [34]. This exam included obtaining a parasternal short axis cardiac view. This view is performed by placing the phased array US probe along the L parasternum at the 3rd rib space with the indicator at the 2–3 o’clock position (Fig. 6). Gunst et al. proposed a focused POC cardiac examination with the mnemonic “BEAT” which aims to assess “Beat” (or Cardiac Index), “Effusion,” “Area” (Ventricular Size/Function), and “Tank” (Preload). Using their approach, cardiac index is determined by quickly calculating Fractional Shortening in the parasternal long axis view (PLAX). The end-diastolic and end-systolic left ventricular areas are traced and software then derives the percent of fractional shortening. The normal values are 25–43 %, and severe dysfunction occurs at <15 % [34]. In general, fractional shortening values correspond to ejection fraction values, which are twice as large. Gunst evaluates the presence of pericardial effusion in the PLAX and then assesses right and left ventricular size in the parasternal short axis view (PSAX). Normal values for left ventricular end-diastolic diameter are 3.9–5.3 cm with severe dilation at >6.2 cm [34]. To correct for individual variability, right ventricular size is evaluated in relation to the Left Ventricle. Moderate right ventricular enlargement corresponds to a Right Ventricular EDA to Left Ventricular EDA ratio of 0.6–1.0. Severe enlargement exists when the ventricular diastolic ratio is >1. This would indicate cor pulmonale and may significantly affect treatment approach [35].
In the “BEAT” exam, intravascular fluid status is determined by calculating the IVC-CI. This calculation is obtained from the subcostal view in M-Mode as well as analyzing the E-to-A Doppler wave pattern across the mitral valve in PLAX view. As discussed in the study publication, these two methods are not without limitations. For example, the patient’s inspiratory effort and restrictive pulmonary disease can affect the former and pre-existing diastolic dysfunction can affect the latter. However, when combined, they may provide a reasonably, reliable, and efficient assessment of preoperative volume status in most patients.
Additional support for bedside TTE has been demonstrated by a study involving 100 consecutive patients with shock. The study showed TTE had an adequate image quality in 99 % of exams performed. It also showed that bedside TTE had a sensitivity and specificity of 100 and 95 %, respectively, for diagnosing a cardiac cause of shock [36]. Finally, the ability to train non-cardiologist to perform and interpret a limited trans-thoracic exam that focused on assessment of left ventricular (LV) function has been demonstrated [37, 38]. Recently, guidelines have been published for POC cardiac ultrasound by non-cardiologists for the intensive care setting [38]. Given the strong similarity of the ICU to the OR, it would seem beneficial that the perioperative physician adopt similar guidelines.
Assessment of Pulmonary Function
Ultrasound assessment of pulmonary function and injury has recently gained significant interest. For the perioperative physician, the ability to rapidly detect pneumothorax, pleural effusion, and severe alveolar–interstitial disease would be of tremendous asset. Ultrasonography has been shown to be more accurate than auscultation or chest radiography for the detection of pleural effusion, consolidation, and alveolar–interstitial syndrome in the critical care setting [39, 40]. In addition, the ability to learn the skill set to detect significant pleural effusion and severe alveolar–interstitial disease has been shown [41, 42].
Examination
Basic concept for lung US is that fluid is present in more dependent areas while gases rise to the top. Therefore, the position of the patient will be important at the time of examination, i.e., supine or lying. The position of probe placement is similar to that of the stethoscope and can be anterior/superior or posterior/inferior for the diagnosis of dependent versus non-dependent pathologies. The probe can be placed transverse (between the 2 ribs) or longitudinally. Longitudinal approach is preferred as the ribs in view provide a landmark. The first step in lung US is to visualize the diaphragm, which is a concave hyper echoic structure and descends with every breath. Another landmark under the diaphragm is the liver on the right and spleen on the left. The curvilinear probe is usually best for visualization of the pleural cavity. The lower frequency of 4–5 MHz does not allow the distinction of visceral and parietal pleura but allows the visualization of lung sliding and air artifacts. Subcostal or abdominal approach can also be used to visualize the pleural cavity trans-diaphragm.
Assessment of Pneumothorax
POC sonography has proven to be a valuable tool for the detection of pneumothorax [43, 44], even when used by recently trained non-experienced personnel [45]. The ultrasound techniques used for this assessment involves the detection of pleural lung sliding. Specifically, ultrasound can identify the movement of the lung across the pleura with respiration, termed lung or pleural sliding. If lung sliding is present, pneumothorax can be ruled out. However, loculated posterior, mediastinal, and apical pneumothoraces can be missed. For a complete examination, the probe must be placed along the anterior, lateral, and posterior intercostal spaces. Observation of lung sliding must include an entire respiratory cycle at each point.
Pleural Effusion
Pleural cavity is highly accessible to ultrasound. Pleural effusion is diagnosed in the dependent area of the lung, i.e., posterior or inferior areas. The fluid is bound inferiorly by the diaphragm and all around by the visceral and parietal pleura. With respiration, the visceral pleural should move toward the parietal pleura leading to a sinusoid sign on M-mode. This method has a specificity of 97 % for the detection of a pleural effusion [46]. Ultrasound is more sensitive and specific than auscultation and CXR and is therefore the method of choice to detect pleural effusion [39, 47]. Effusions over 1 cm are easily detected and have more than 90 %sensitivity and specificity for detection. [39].
Parenchymal Lung Pathologies
Another common utility of POC ultrasound in the assessment of pulmonary function is the evaluation of Ultrasound Lung Comets (ULC), also known as B-Lines (Fig. 7). These ULCs are artifacts of water-thickened interlobular septa. ULCs indicate increased amounts of extravascular pulmonary as in the setting of congestive heart failure. The number of ULCs correlates with extracellular lung water and pulmonary wedge pressure (p < 0.001) [48]. The presence of ULCs in the setting of acute dyspnea correlates with NT-proBNP and the Framingham criteria as a means to distinguish cardiogenic and non-cardiogenic dyspnea (p < 0.001) [49]. For this study, the presence of 9 ULCs was 100 % specific for cardiogenic dyspnea though maximum accuracy was with 4 ULCs (sens. 81 %, spec. 85 %) [49]. While more research is needed to determine the significance of such findings to perioperative risk stratification or medical optimization, the recent literature continues to support the greater utility of POC sonography for the assessment of pulmonary function. Given that this a common perioperative issue, integration of these validated skillsets by the perioperative physician may greatly assist patient care.
Advanced Vascular Access
The use of ultrasound to aid with vascular access has advanced beyond its use for central venous access. Specifically, ultrasound has proven to reliably aid in the placement of difficult intravenous [50, 51] and intra-arterial catheters [52, 53]. The use of ultrasound for peripheral venous access also has shown to significantly increase success rates as well [54]. Regarding central venous access, a recent meta-analysis was conducted to compare an ultrasound guidance technique with anatomical landmark technique and the results showed decreased risks of cannulation failure, arterial puncture, hematoma, and hemithorax with ultrasound [55]. However, it is important to emphasize that good anatomical knowledge and a dynamic hand–eye–probe co-ordination to follow the needle tip are vital for success and avoidance of inadvertent arterial punctures [56]. The use of ultrasound has resulted in some complications related to injury of deeper structures (subclavian or vertebral artery) while inserting Internal jugular central lines. This underlines the importance of formalized training in ultrasound and simulated practice of central line placement, and this has been supported by recent guidelines published on this topic [56].
Additional Areas of Perioperative Improvement with POC Ultrasound
There are additional areas of POC ultrasonography that are relevant to the issues faced by the perioperative physician.
Evaluation of Deep Venous Thrombosis and Pulmonary Embolus
The current standard for evaluation of patient’s with suspicion for deep venous thrombosis (DVT) or pulmonary embolus (PE) often involves CT pulmonary angiography and lower compression ultrasonography. These tests are often performed despite low pre-test probability along with potential delays in diagnosis to perform these studies. (4/5). Recent evidence supports that the use of a focused POC US exam, involving lung ultrasonography for subpleural infarcts, right ventricular dilatation by heart ultrasonography, and deep venous thrombosis by leg vein ultrasonography, can provide a high degree of sensitivity (90 %) and a specificity (86.2 %) for the detection of pulmonary embolus [57].
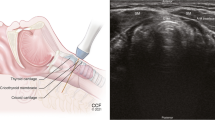
Endotracheal Tube Placement
Recent studies have also shown the utility of ultrasound for verification of successful endotracheal intubation. Data showed a sensitivity and specificity of 100 % for the detection of successful endotracheal intubation vs. esophageal [58]. A recent POC US examination abbreviated as PLUS (Pulmonary tree and Lung expansion Ultrasound Study), which included assessment for tracheal dilation with the endotracheal tube cuff inflation and bilateral pleural lung sliding, demonstrated a high degree of sensitivity and specificity (>93 %) to detect endobronchial vs. tracheal intubations [59].
Gastric Volume Assessment
POC US has also been used to assess for gastric content and volume [60, 61], and a recent grading system based exclusively on qualitative sonographic assessment of the gastric antrum has shown strong correlation with predicted gastric volume [61] (Fig. 8). Perlas et al. reported that the presence of fluid in the antrum identified by ultrasound in the supine and right lateral decubitus positions correlates with a clinically significant amount of gastric contents (180 ± 83 ml). This ability to detect gastric volume via POC ultrasonography may provide a method to assess aspiration risk.
Intracranial Pressure Estimation
POC ultrasonography has been shown to provide rapid assessment of elevated intracranial pressures (ICP) based on the assessment of optic nerve sheath diameter. The optic nerve sheath is contiguous with the dura mater and has a trabeculated arachnoid space through which cerebrospinal fluid circulates. This relationship between the optic nerve sheath diameter (ONSD) and ICP has been well established [62, 63]. The sensitivity for the ultrasonography in detecting elevated intracranial pressure was 100 % [95 % confidence interval (CI) 68–100 %], and specificity was 63 % (95 % CI 50–76 %) [56]. An optic nerve sheath diameter of greater than 5 mm, at a point approximately 2 mm from the retina, suggests elevated ICP (Fig. 9).
Bringing these Modalities to the Perioperative Physician
The above review indicates that POC ultrasound has the capability to help the perioperative physician with far more than central venous access and regional anesthesia. Point-of-care ultrasound has become increasingly vital within critical care medicine [64•], and its positive impact in the perioperative arena is beginning to be shown [65••]. Educational courses for advanced ultrasound have been taught at the Society of Critical Care Medicine, American College of Chest Physicians, and the America College of Surgeons for years. In their role as the perioperative physicians, anesthesiologist may benefit from the use of POC ultrasound throughout the preoperative evaluation, medical management in the operating room, as well as the recovery area.
However, our specialty needs to formulate a standardized comprehensive POC ultrasound curriculum to maximize its potential benefit to patient care. Several education curriculums have been established [4, 66••]. We suggest the development of a comprehensive POC ultrasonography (based on the review described above) to help the anesthesiologist in all aspects of perioperative care. The authors currently have designed such a curriculum, termed FORESIGHT (focused, perioperative, risk, evaluation, sonography, involving, gastro-abdominal, hemodynamic, and trans-thoracic ultrasound) ultrasound examination (Fig. 1). Details of the topics discussed in this curriculum are listed in “Appendix.” Implementation of the curriculum during resident training has shown to be well received and observational results suggest that successful training may positively impact patient care [4••].
Summary
As POC ultrasound becomes more readily available in the operating room the perioperative physician must be ready to use the technology effectively to elevate their level of patient care. The formulation of a structured curriculum and method of education is essential. Further research in this area is needed to consolidate the role of POC ultrasound as an important technique for advancing patient care modality.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Grocott MP, Pearse RM. Perioperative medicine: the future of anaesthesia? Br J Anaesth. 2012;108(5):723–6.
Alpert JS, Mladenovic J, Hellmann DB. Should a hand-carried ultrasound machine become standard equipment for every internist? Am J Med. 2009;122(1):1–3.
Kendall JL, Hoffenberg SR, Smith RS. History of emergency and critical care ultrasound: the evolution of a new imaging paradigm. Crit Care Med. 2007;35(5 Suppl):S126–30.
•• Ramsingh D, R.J., Kain Z, Strom S, Canales C, Alexander B, Capatina A, Ma M, Le K, Cannesson M, Impact assessment of perioperative point of care ultrasound training anesthesiology (Forthcoming 2015). This upcoming publication highlights a perioperative “whole-body” point of care ultrasound curricuium for anesthesiologists and suggests the potential for its postivie clinical impact.
Bundgaard-Nielsen M, et al. Monitoring of peri-operative fluid administration by individualized goal-directed therapy. Acta Anaesthesiol Scand. 2007;51(3):331–40.
Marik PE, Cavallazzi R. Does the central venous pressure predict fluid responsiveness? An updated meta-analysis and a plea for some common sense. Crit Care Med. 2013;41(7):1774–81.
Ommen SR, et al. Assessment of right atrial pressure with 2-dimensional and Doppler echocardiography: a simultaneous catheterization and echocardiographic study. Mayo Clin Proc. 2000;75(1):24–9.
Prekker ME, et al. Point-of-care ultrasound to estimate central venous pressure: a comparison of three techniques. Crit Care Med. 2013;41(3):833–41.
Gillman LM, et al. Clinician performed resuscitative ultrasonography for the initial evaluation and resuscitation of trauma. Scand J Trauma Resusc Emerg Med. 2009;17:34.
Barbier C, et al. Respiratory changes in inferior vena cava diameter are helpful in predicting fluid responsiveness in ventilated septic patients. Intensive Care Med. 2004;30(9):1740–6.
Cannesson M, et al. Prediction of fluid responsiveness using respiratory variations in left ventricular stroke area by transoesophageal echocardiographic automated border detection in mechanically ventilated patients. Crit Care. 2006;10(6):R171.
Scheuren K, et al. Left ventricular end-diastolic area is a measure of cardiac preload in patients with early septic shock. Eur J Anaesthesiol. 2009;26(9):759–65.
Subramaniam B, Talmor D. Echocardiography for management of hypotension in the intensive care unit. Crit Care Med. 2007;35(8 Suppl):S401–7.
Marik PE, Baram M, Vahid B. Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares. Chest. 2008;134(1):172–8.
Gelman S. Venous function and central venous pressure: a physiologic story. Anesthesiology. 2008;108(4):735–48.
Howell MD, et al. Occult hypoperfusion and mortality in patients with suspected infection. Intensive Care Med. 2007;33(11):1892–9.
Sefidbakht S, et al. Sonographic measurement of the inferior vena cava as a predictor of shock in trauma patients. Emerg Radiol. 2007;14(3):181–5.
Broch O, et al. Variation of left ventricular outflow tract velocity and global end-diastolic volume index reliably predict fluid responsiveness in cardiac surgery patients. J Crit Care. 2012;27(3):325e7–13.
Charron C, et al. Echocardiographic measurement of fluid responsiveness. Curr Opin Crit Care. 2006;12(3):249–54.
Feissel M, et al. Respiratory changes in aortic blood velocity as an indicator of fluid responsiveness in ventilated patients with septic shock. Chest. 2001;119(3):867–73.
Monge Garcia MI, Gil Cano A, Diaz Monrove JC. Brachial artery peak velocity variation to predict fluid responsiveness in mechanically ventilated patients. Crit Care. 2009;13(5):R142.
Monnet X, et al. Passive leg raising predicts fluid responsiveness in the critically ill. Crit Care Med. 2006;34(5):1402–7.
Lamia B, et al. Echocardiographic prediction of volume responsiveness in critically ill patients with spontaneously breathing activity. Intensive Care Med. 2007;33(7):1125–32.
Maizel J, et al. Diagnosis of central hypovolemia by using passive leg raising. Intensive Care Med. 2007;33(7):1133–8.
Levitov A, Marik PE. Echocardiographic assessment of preload responsiveness in critically ill patients. Cardiol Res Pract. 2012;2012:819696.
Mahjoub Y, et al. The passive leg-raising maneuver cannot accurately predict fluid responsiveness in patients with intra-abdominal hypertension. Crit Care Med. 2010;38(9):1824–9.
Rozycki GS, et al. A prospective study of surgeon-performed ultrasound as the primary adjuvant modality for injured patient assessment. J Trauma. 1995;39(3):492–8.
Rodriguez A, DuPriest RW Jr, Shatney CH. Recognition of intra-abdominal injury in blunt trauma victims. A prospective study comparing physical examination with peritoneal lavage. Am Surg. 1982;48(9):457–9.
Perry JF Jr, DeMeules JE, Root HD. Diagnostic peritoneal lavage in blunt abdominal trauma. Surg Gynecol Obstet. 1970;131(4):742–4.
Scalea TM, et al. Focused assessment with sonography for trauma (FAST): results from an international consensus conference. J Trauma. 1999;46(3):466–72.
Rose JS. Ultrasound in abdominal trauma. Emerg Med Clin North Am. 2004;22(3):581–599, vii.
Kirkpatrick AW, et al. Prospective evaluation of hand-held focused abdominal sonography for trauma (FAST) in blunt abdominal trauma. Can J Surg. 2005;48(6):453–60.
Andersen GN, et al. Feasibility and reliability of point-of-care pocket-sized echocardiography. Eur J Echocardiogr. 2011;12(9):665–70.
Gunst M, et al. Accuracy of cardiac function and volume status estimates using the bedside echocardiographic assessment in trauma/critical care. J Trauma. 2008;65(3):509–16.
Beaulieu Y. Bedside echocardiography in the assessment of the critically ill. Crit Care Med. 2007;35(5 Suppl):S235–49.
Joseph MX, et al. Transthoracic echocardiography to identify or exclude cardiac cause of shock. Chest. 2004;126(5):1592–7.
Manasia AR, et al. Feasibility and potential clinical utility of goal-directed transthoracic echocardiography performed by noncardiologist intensivists using a small hand-carried device (SonoHeart) in critically ill patients. J Cardiothorac Vasc Anesth. 2005;19(2):155–9.
Mazraeshahi RM, Farmer JC, Porembka DT. A suggested curriculum in echocardiography for critical care physicians. Crit Care Med. 2007;35(8 Suppl):S431–3.
Lichtenstein D, et al. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology. 2004;100(1):9–15.
Vignon P, et al. Quantitative assessment of pleural effusion in critically ill patients by means of ultrasonography. Crit Care Med. 2005;33(8):1757–63.
Bedetti G, et al. Evaluation of ultrasound lung comets by hand-held echocardiography. Cardiovasc Ultrasound. 2006;4:34.
Eibenberger KL, et al. Quantification of pleural effusions: sonography versus radiography. Radiology. 1994;191(3):681–4.
Bouhemad B, et al. Clinical review: bedside lung ultrasound in critical care practice. Crit Care. 2007;11(1):205.
Ueda K, Ahmed W, Ross AF. Intraoperative pneumothorax identified with transthoracic ultrasound. Anesthesiology. 2011;115(3):653–5.
Monti JD, Younggren B, Blankenship R. Ultrasound detection of pneumothorax with minimally trained sonographers: a preliminary study. J Spec Oper Med. 2009;9(1):43–6.
Lichtenstein D, et al. Feasibility and safety of ultrasound-aided thoracentesis in mechanically ventilated patients. Intensive Care Med. 1999;25(9):955–8.
Doust BD, et al. Ultrasonic evaluation of pleural opacities. Radiology. 1975;114(1):135–40.
Agricola E, et al. “Ultrasound comet-tail images”: a marker of pulmonary edema: a comparative study with wedge pressure and extravascular lung water. Chest. 2005;127(5):1690–5.
Gargani L, et al. Ultrasound lung comets for the differential diagnosis of acute cardiogenic dyspnoea: a comparison with natriuretic peptides. Eur J Heart Fail. 2008;10(1):70–7.
Costantino TG, et al. Ultrasonography-guided peripheral intravenous access versus traditional approaches in patients with difficult intravenous access. Ann Emerg Med. 2005;46(5):456–61.
Keyes LE, et al. Ultrasound-guided brachial and basilic vein cannulation in emergency department patients with difficult intravenous access. Ann Emerg Med. 1999;34(6):711–4.
Ashworth A, Arrowsmith JE. Ultrasound-guided arterial cannulation. Eur J Anaesthesiol. 2010;27(3):307.
Shiver S, Blaivas M, Lyon M. A prospective comparison of ultrasound-guided and blindly placed radial arterial catheters. Acad Emerg Med. 2006;13(12):1275–9.
Stolz LA, et al. Ultrasound-guided peripheral venous access: a meta-analysis and systematic review. J Vasc Access. 2015;16(4):321–6.
Wu SY, et al. Real-time two-dimensional ultrasound guidance for central venous cannulation: a meta-analysis. Anesthesiology. 2013;118(2):361–75.
Troianos CA, et al. Special articles: guidelines for performing ultrasound guided vascular cannulation: recommendations of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. Anesth Analg. 2012;114(1):46–72.
Nazerian P, et al. Accuracy of point-of-care multiorgan ultrasonography for the diagnosis of pulmonary embolism. Chest. 2014;145(5):950–7.
Muslu B, et al. Use of sonography for rapid identification of esophageal and tracheal intubations in adult patients. J Ultrasound Med. 2011;30(5):671–6.
Ramsingh D, Haughton FE, Schilling J, Gimenez K, Banh E, Rinehart J, Cannesson M. Auscultation vs. point of care ultrasound to determine endotracheal versus bronchial intubation: a diagnostic accuracy study. Anesthesiology 2015.
Perlas A, et al. Ultrasound assessment of gastric content and volume. Anesthesiology. 2009;111(1):82–9.
Perlas A, et al. Gastric sonography in the fasted surgical patient: a prospective descriptive study. Anesth Analg. 2011;113(1):93–7.
Hansen HC, Helmke K. Validation of the optic nerve sheath response to changing cerebrospinal fluid pressure: ultrasound findings during intrathecal infusion tests. J Neurosurg. 1997;87(1):34–40.
Tayal VS, et al. Emergency department sonographic measurement of optic nerve sheath diameter to detect findings of increased intracranial pressure in adult head injury patients. Ann Emerg Med. 2007;49(4):508–14.
• Manno E et al. Deep impact of ultrasound in the intensive care unit: the “ICU-sound” protocol. Anesthesiology 2012;117(4):801–9. This study demonstrated the use of a comprehensive point of care ultrasound examination upon admission to the intensive care unit results in a high prevalence of unsuspected clinical abnormalities.
•• Botker MT et al. Routine pre-operative focused ultrasonography by anesthesiologists in patients undergoing urgent surgical procedures. Acta Anaesthesiol Scand 2014;58(7):807–14. This study demonstrated that pre-operative focused cardiopulmonary ultrasonography disclosed unexpected pathology in patients undergoing urgent surgical procedures and induced changes in the anesthesia management.
•• Killu K et al. Model point-of-care ultrasound curriculum in an intensive care unit fellowship program and its impact on patient management. Crit Care Res Pract 2014;2014:934796. This study assessed the clinical impact of establishing a Point-of-Care (POC) ultrasound curriculum into an intensive care unit (ICU) fellowship program and was associated with an increase in new diagnosis in about 2/3 and change in management in over 1/3 of ICU patients studied.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Davinder Ramsingh, Sumit Singh, Mike Ross, Wendell Williams, and Maxime Cannesson declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Cardiovascular Anesthesia.
Appendix
Appendix
See Fig. 10.
Rights and permissions
About this article
Cite this article
Ramsingh, D., Singh, S., Ross, M. et al. Review of Point-of-Care (POC) Ultrasound for the 21st Century Perioperative Physician. Curr Anesthesiol Rep 5, 452–464 (2015). https://doi.org/10.1007/s40140-015-0137-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40140-015-0137-2