Abstract
Purpose of Review
In this article, we review the use of hypertonic saline (HTS) for FDA-approved indications, namely treatment of hyponatremia and elevated intracranial pressure (ICP), as well as the routes of administration appropriate for infusion.
Recent Findings
Though society guidelines for treating hyponatremia have not recently changed, new data is emerging that supports the use of bolus-based HTS treatment regimens. HTS is at least as effective as mannitol for lowering elevated ICP from cerebral edema and is also now the preferred hyperosmolar treatment in patients with intracranial hemorrhage (ICH) and traumatic brain injury (TBI). Central venous catheter (CVC) has been recommended in the past for HTS infusions, but emerging data suggest infusion via peripheral intravenous catheters (IV) is likely safe and may be worth avoiding the time intensive and potentially harmful process of placing a CVC.
Summary
HTS infusion via peripheral IV appears to be safe, effective, and more time efficient than infusion via CVC in treating acute hyponatremia and increased ICP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypertonic saline (HTS) is a critical medication used in the hospital setting. Administration of concentrations ranging from 2 to 23% saline are described in the literature as well as continuous or bolus dosing strategies. Historically, infusion via central venous catheter (CVC) has been recommended due to perceived extravasation risk when infused via peripheral intravenous (IV) access. However, emerging data suggests peripheral IV may be a safe and effective option.
HTS is most commonly used for treating symptomatic hyponatremia and elevated intracranial pressure (ICP). Hyponatremia, defined as serum sodium < 136 mEq/L, is the most commonly encountered electrolyte abnormality among patients in the USA, present in an estimated 1.72% of the US population in general [1] and 20–40% of all hospitalized patients [2, 3]. Though many cases are mild and relatively asymptomatic, hyponatremia is independently associated with increased morbidity and mortality both in the inpatient and outpatient setting [1]. Identifying, differentiating, and managing hyponatremia are a crucial skill for a physician caring for the critically ill. Improper management of these conditions can lead to worsening clinical status of the patient and can increase morbidity and mortality. HTS is commonly used in the management of patients with moderate to severe symptoms.
Additionally, HTS has demonstrated utility in the initial management of increased ICP in both the adult and pediatric populations. Increased ICP as the result of cerebral edema, can be caused by a variety of insults such as trauma, epidural/subdural hematoma, intracranial masses, and hydrocephalus.
Hyponatremia
Etiology and Pathophysiology
Establishing the cause of hyponatremia is important to guide treatment. In most cases, hyponatremia is simply a manifestation of a more general hypotonic state, but in two specific conditions, hyponatremia can also occur in isotonic or hypertonic states. In one subset of these isotonic or hypertonic states, a significant excess of lipids or proteins can cause pseudohyponatremia due to the relatively larger plasma volume occupied by these particles. These patients will have a normal plasma osmolality. Hyponatremia with normal or increased osmolality can also occur when other solutes outside of sodium are present in the plasma. This most commonly occurs with hyperglycemia, as significant hyperglycemia can induce an osmotic diuresis resulting in hypertonic hyponatremia [4••].
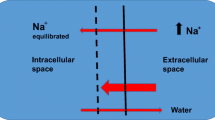
Most cases of hyponatremia are due to hypotonicity. Hypotonic hyponatremia is due to a disorder of water balance with an excess of total body water in relation to extracellular sodium. Decreased extracellular osmolality due to decreased sodium creates an osmotic gradient, causing water influx into cells, creating edema. Cells, especially those in the brain, regulate osmotically active solutes to compensate. As hyponatremia is corrected, the process reverses, though this is much slower than the initial recalibration.
Hypotonic hyponatremia can be further subdivided by underlying etiology into hypovolemic, euvolemic, and hypervolemic states. Hypovolemic hyponatremia results from a loss of solutes from the body. This can be seen with gastrointestinal disease, diuretic therapies, cerebral salt wasting, and mineralocorticoid deficiency. Euvolemic hyponatremia is a result of relative excess of body water, usually due to syndrome of inappropriate antidiuretic hormone (SIADH), glucocorticoid deficiency, hypothyroidism, low solute intake, or primary polydipsia. Hypervolemic hyponatremia is caused by inability of the kidneys to maximally excrete water, caused by heart failure, cirrhosis, acute kidney injury, chronic kidney disease, or nephrotic syndrome [4••].
Clinical Features
The laboratory-defined severity of hyponatremia is divided into mild (Na 130–135 mEq/L), moderate (Na 125–129 mEq/L), and profound (Na < 125 mEq/L), but the specific clinical presentation and timeframe over which hyponatremia develops is most clinically relevant when determining treatment [5••]. Hyponatremia is divided into “acute” and “chronic” based on whether it has been present for more or less than 48 h, which is the average amount of time required for cells to adapt to a hypotonic environment. Mild-moderate symptoms include nausea with or without vomiting, headache, confusion, whereas severe symptoms include cardiorespiratory distress, altered mental status, seizures, obtundation, coma, and death [5••, 6]. These severe manifestations are more likely to occur with less profound hyponatremia in acute cases, due to significant cerebral edema from delayed solute redistribution within the brain. In cases of chronic hyponatremia, the brain is able to equilibrate osmolality leading to less edema and thus less severe clinical manifestations until the sodium has reached a more profound nadir [6]. Any patient with moderate-profound hyponatremia displaying moderate to severe symptoms should undergo immediate sodium correction. Treatment becomes more nuanced with chronic hyponatremia with mild to moderate symptoms.
One of the most feared complications of correcting hyponatremia is osmotic demyelination (ODS), a clinical syndrome defined by worsening neurologic symptoms after a rapid correction of hyponatremia. Symptoms of ODS may include quadriplegia, pseudobulbar palsy, coma, seizures, and death. ODS is most common when patients with chronic hyponatremia undergo rapid correction, as the brain has been equilibrated to a hypotonic serum and is unable to regulate its solutes as rapidly as the serum sodium is being corrected [7]. The true incidence of ODS is unknown, but MRI based studies estimate an incidence of approximately 0.3–1.1%, with higher incidence in high risk groups such as patients receiving liver transplantation [8].
Treatment
The general guiding principles for treatment of hyponatremia were most recently defined in US and European consensus guidelines for hyponatremia [4••, 5••]. Hypertonic saline, specifically 3%, is recommended for treatment of moderate to profound hyponatremia (serum sodium < 130) with moderate to severe symptoms. Both guidelines recommend a bolus-based correction strategy in most cases with either up to three 100-mL boluses of 3% HTS infused over 10 min or two 150-mL boluses infused over 20 min each [4••, 5••]. In the US guidelines, slow continuous infusion of 0.5–2 mL/kg/hr was still recommended for mild-moderate symptoms [4••] versus the European guidelines which advocated for bolus-based correction for anyone with moderate-severe symptoms or anyone with acute hyponatremia displaying a drop of 10 mEq/L from baseline [5••]. A serum sodium increase of 4–6 mEq/L in the first 6 h is recommended, as literature has shown this increase sufficient to reverse the most serious neurologic manifestations of severe hyponatremia without increasing the risk of osmotic demyelination syndrome [9]. The suggested ceiling for sodium increase to reduce risk of ODS is 10 mEq/L in the first 24 h and 8 mEq/L every 24 h thereafter until the sodium reaches 130 mEq/L [5••], which coheres with previous studies showing an increased risk of ODS at rates above than 12 mEq/L/24 h [9]. If sodium correction exceeds the suggested limit, therapeutic re-lowering with desmopressin and serial 3-mL/kg infusions of dextrose 5% in water is recommended [4••].
Since guideline publication, several studies have aimed to further evaluate the bolus-based infusion strategy recommended as well as pros and cons of the slow continuous infusion. In Europe, Ayus et al. evaluated the treatment of hyponatremic encephalopathy with a limited infusion of 500 mL of 3% HTS infused over 6 h. They showed an improvement in neurologic status without osmotic demyelination. However, the rate of correction seen at 24 h was at the upper limit of recommendations (9.8 + / − 1 mEq/L), making this a less ideal strategy in patients where chronicity of hyponatremia is unclear [10].
A study by Garrahy et al. in patients with hyponatremia from SIADH compared prospective data from a bolus protocol to retrospective data from prior continuous infusion protocols. The bolus protocol involved 100-mL bolus of 3% HTS over 15 min, repeated up to two more times to achieve 4–6-mEq/L rise over 6 h, whereas the continuous protocol involved 500 mL of 3% HTS infused at 20 mL/hr, adjusted to achieve a rise of 8–12 mEq/L over the first 24 h. They showed the bolus protocol produced a faster rise in serum sodium and a more favorable neurologic recovery (based on improved Glasgow Coma Scale) initially, but ultimately no difference was seen at 24 h. However, the bolus-based dosing was more likely to overcorrect sodium, requiring dextrose infusions or desmopressin to offset the increase. This occurred more in patients requiring a third bolus, though most patients in the study were only treated with two [11].
More recently, the SALSA randomized controlled trial (RCT) aimed to assess the risk of overcorrection in rapid bolus versus slow continuous HTS infusion, as well as efficacy and safety of proposed regimens [12]. This study was more inclusive than prior studies, focusing on patients with many different causes of hyponatremia, and was one of the first RCTs on this topic. Treatment in the bolus group included one 2 mL/kg 3% bolus for moderate symptoms or two boluses for severe symptoms, and slow continuous included infusions of 0.5 mL/kg/hr for moderate symptoms or 1 mL/kg/hr for severe symptoms with adjustments at 1 and 6 h based on sodium response on repeat labs. Treatment goals were to increase sodium by 5–9 mEq/L and achieve symptom relief in the first 24 h and to increase sodium by 10–17 mEq/L or to > 130 mEq/L and achieve symptom relief in the first 48 h. Overcorrection was also monitored and treated. Both bolus and continuous infusion methods were found to be safe and effective, with no significant difference in overcorrection risk. Bolus infusion was found to have a greater increase in sodium within 1 h and required less therapeutic re-lowering, thus suggesting bolus doses as the preferred treatment as recommended by the current guidelines [12].
Treatment of chronic hyponatremia is more nuanced and depends on the underlying cause and volume status of the patient. Hypertonic saline has a more limited use, as patients with chronic hyponatremia develop severe symptoms less frequently. If severe symptoms develop, bolus-based correction as described above is recommended [4••]. In two specific cases, namely heart failure and cirrhosis, hypertonic saline with possible addition of loop diuretics have shown benefit in cases of profound hyponatremia, regardless of severity of symptoms [4••, 13]. Typically, for other etiologies or mild presentations, etiology specific treatment is more commonly indicated for chronic hyponatremia [14]. The rate of correction for chronic hyponatremia also differs slightly from that of acute hyponatremia and depends on risk factors for ODS. Patients at high risk, including those with a serum sodium concentration < 105 mEq/L, hypokalemia, alcoholism, cirrhosis, and malnutrition, an initial target of 4–6 mEq/L per day is recommended with a maximum daily correction of 8 mEq/L. Patients without these high risk features should be targeted for an initial increase of 4–8 mEq/L in the first 24 h and a subsequent limit of 10 mEq/L per day afterwards [4••].
Elevated Intracranial Pressure
Increased ICP, as a result of cerebral edema, may develop after a variety of insults, such as the disruption of the blood–brain barrier, vascular changes, local inflammation, altered cellular metabolism, or trauma [15••]. ICP can vary with age and monitoring is often unavailable at the time of initial treatment decisions. Normal values are typically < 15 mmHg for adults and older children. ICP values greater than 20 mmHg require treatment in most circumstances, with ICP values > 40 mmHg indicating severe, life-threatening intracranial hypertension [16]. The use of hyperosmolar therapy has been a cornerstone in treating increased ICP for decades. Hyperosmolar agents create an osmotic gradient across the blood–brain barrier which pulls fluid from the interstitial space into the vascular space. Historically mannitol has been used; however, hypertonic saline has emerged as an alternative hyperosmolar agent which may have some advantages over mannitol [16].
Dosing
Hypertonic saline concentrations ranging from 2 to 23.4% and multiple dosing strategies have been described in the literature for the treatment of elevated ICP. Titratable continuous infusions of 3% HTS at an initial rate of 30–50 mL/h can be administered to maintain serum sodium 145–155 mEq/L [19]. While there are many options for bolus dosing, concentrations of 7.5% and 23.4% are frequently used. A bolus of 7.5% saline can be administered at a rate of 2 mL/kg over 20 min [20]. Alternatively, a single 30–60-mL bolus of 23.4% saline can be administered over 2–10 min as needed to treat acute ICP elevations [21].
There is little evidence demonstrating superiority of a specific dose or concentration of HTS by direct comparison. Carter et al. conducted a single center, retrospective study comparing 5% HTS as an alternative to 23.4% for the treatment of ICP and found similar reduction of ICP at 120 min, and faster time to administration due to not needing central venous access. Although this study had a small sample size, they did not see a significant difference in efficacy or adverse events [17]. Busey et al. looked at a single bolus of 23.4% HTS compared to weight-based dosing of 23.4% HTS and found no statistically significant differences in ICP reduction between groups [18]. Similarly, Maguigan et al. looked at bolus versus continuous infusion of 3% HTS in patients with severe traumatic brain injury (TBI) and found no difference between ICP, length of stay, and mortality [19]. A 2022 systematic review noticed greater reductions in ICP amongst studies that utilized lower concentrations of saline (3% or 7.5%) rather than higher concentrations. It should be noted that concentration and dosing strategies were not directly compared in the source studies [22•]. Given the lack of quality evidence demonstrating a superiority of a specific dosing strategy, we suggest adhering to institutional guidelines when administering HTS for elevated ICP.
Treatment
Evidence shows that HTS is helpful in reducing elevated ICP in patients with TBI, subarachnoid hemorrhage (SAH), intracranial hypertension, hepatic encephalopathy, acute ischemic strokes, and bacterial meningitis [15••, 23]. Early and continuous infusion of 3% HTS in patients with cerebrovascular disease might reduce the frequency of ICP crisis and cerebral edema [24, 25]. The evidence is most robust for reduction of ICP in patients with severe TBI [22•, 26,27,28]. Rockswold et al. looked at the effects of a 30-mL bolus of 23.4% HTS on ICP reduction and concluded that hypertonic saline as a single osmotic agent decreases ICP while improving cerebral perfusion pressure (CPP) [27]. Munar et al. administered a 15 min infusion of 7.2% HTS (1.5 mL/kg) in patients with TBI and found a significant reduction in ICP to approximately 30% of the baseline [28]. The most recent systematic review showed an average 44% decrease in ICP over 15 studies, with an average 8 mmHg decrease in ICP when comparing before and after infusion or bolus [22•]. Additionally, there was a correlation between a greater ICP reduction and lower concentrations of HTS [22•].
Neurocritical Care Society (NCS) guidelines were published in 2020 and since then there have been few consistent or meaningful updates to the literature. Guideline authors affirmed that hypertonic saline reduces ICP, but has not been consistently shown to improve neurologic outcomes or mortality in patients with cerebral edema. Due to the low quality of evidence, there were few recommendations on dosing strategies apart from suggesting symptom-based bolus dosing over sodium target-based dosing in patients with cerebral edema due to SAH. Authors also recommended frequent monitoring of serum creatinine in addition to sodium and chloride concentrations to prevent renal injury. They suggested upward limits of 155–160 mEq/L for sodium and 110–115 mEq/L for chloride. They also gave multiple recommendations addressing the use of HTS vs mannitol in treating cerebral edema. However, due to conflicting and often low quality of evidence, the NCS suggests HTS over mannitol only for the indications of cerebral edema in ICH and TBI. The panel felt that the putative advantages of HTS for fluid resuscitation and cerebral perfusion justified this suggestion [15••]. There is insufficient evidence for the NCS to suggest the use of either agent in treating cerebral edema from AIS, hepatic encephalopathy and bacterial meningitis [15••].
There are many theoretical advantages to using HTS over mannitol for the initial management of elevated ICP [15••, 29]. Mannitol is an osmotic diuretic and therefore can lead to volume depletion and hypotension when compared to HTS. This can specifically be consequential in trauma patients where hypovolemia should be avoided to decrease potential secondary brain injury. Several studies have compared the overall ICP reduction of HTS versus mannitol. Mangat et al. conducted a large retrospective study looking at ICP after severe TBI and concluded that HTS use was associated with a significant reduction in daily ICP burden and fewer total intensive care unit days when compared to mannitol [30]. Kochanek et al. conducted a comparative effectiveness study on the effects of HTS and mannitol in children with head trauma and elevated ICP. This study suggested that when ICP was greater than 20 mmHg, HTS outperformed mannitol in ICP reduction [31].
However, evidence suggesting superiority of HTS compared to mannitol is still debated, even amongst systematic reviews. A 2016 meta-analysis found no difference in mortality, ICP, or functional difference between HTS and other hyperosmolar therapies in patients with elevated ICP secondary to TBI [32]. A 2020 Cochrane review concluded both therapies were effective in reducing ICP and that weak evidence suggests HTS is no better than mannitol for improving long term outcomes [26]. Conversely a 2021 systematic review and meta-analysis concluded that HTS has a more sustained effect on lowering ICP and greater benefit in increasing CPP [33].
Overall, evidence supports administering HTS as an alternative to mannitol to reduce ICP and is preferred in TBI and intracranial hemorrhage [15••]. There is a dearth of evidence supporting one concentration or dosing strategy over another. Therefore, providers should adhere to their institutional guidelines when administering HTS. It is recommended that intravenous HTS be used as adjunctive therapy for raised ICP. However, survival benefit or improvement in neurological outcomes has not been well demonstrated [15••, 34].
Route of Administration
Central Line
Hypertonic saline has traditionally been reserved for administration via CVC due to concerns for infusion related adverse events (IRAE’s) such as thrombophlebitis, infusion-related pain, and soft tissue injury from extravasation. Such practices appear to be extrapolated from parenteral nutrition studies rather than data specific to HTS [35]. There is a recent trend challenging this practice for two main reasons. First, guidelines derived from parenteral nutrition administration failed to weigh the inherent risks in placing and maintaining central lines as well as delays that impact care when treating time-sensitive and potentially life-threatening emergencies [36]. Second, there is a growing body of literature demonstrating the relative safety of peripheral HTS infusion [37,38,39,40,41,42,43,44,45].
In a 2015 RCT, authors measured the rate of serious complications resulting from central line placement in either the femoral, subclavian, or internal jugular vein. They found a 3–4% rate of serious complications overall, including symptomatic deep vein thrombosis, mechanical complication (arterial injury, pneumothorax, or hematoma), and central line associated bloodstream infection. In addition, authors noted an average time for insertion of 11.6–12.8 min depending on placement site [36]. The actual time until HTS administration via central line is substantially longer in practice, given the additional time required for consent, setup, and confirmation with imaging. These risks need to be weighed against both the frequency and severity of adverse events resulting from peripheral HTS infusion.
Peripheral Intravenous Catheter
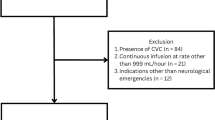
There have been a number of studies exploring the safety of peripheral infusion of HTS in recent years. The overall quality of evidence addressing the topic remains low, with almost all study designs retrospective in nature or prospective without a comparison group. The only controlled trial was not randomized with respect to administration of HTS via peripheral line or central line, but rather to study arms with or without lidocaine co-infusion with HTS [37].
However, the low frequency and minor nature of adverse events consistently reported across studies are enough to call into question the practice of placing a central line for the sole purpose of HTS administration. IRAE frequency ranged in most studies from 0 to 10.7% with saline concentrations as high as 23.4% [37,38,39,40,41,42,43,44,45]. Though there were significant differences in outcome measurements, all reported adverse events were considered minor in severity. These events typically consisted of temporary erythema, pain, and edema at the IV site due to phlebitis or infiltration. There were no episodes of ischemia or permanent tissue damage, and no interventions were required apart from removal of the offending IV [see Table 1]. Many studies reported continuing HTS peripherally through an IV at a different site following infiltration or phlebitis. In all of the studies combined, there was one deep vein thrombosis identified, though authors did not consider this a result of peripheral HTS infusion as it was likely present prior to administration [44].
One study appears to be an outlier, reporting a 47% rate of phlebitis among patients. The notably increased frequency is likely due to authors using Infusion Nursing Society definitions which categorize isolated pain at the infusion site as grade 1 phlebitis. There was no difference in phlebitis rates compared to patients in the control arm of the study who received infusions of medications typically given through peripheral IV catheters [46].
Infusion-related pain is a common complaint as confirmed by a single-center RCT of 106 patients receiving peripheral HTS administration. Patients in the treatment arm received a lidocaine bolus prior to HTS and lidocaine co-infusion with HTS versus the control arm who received equivalent doses of placebo (normal saline) before and during HTS infusion. Pain was reported in 48% of patients in the control arm, though low in severity with a median visual analog scale of 2 out of 10. Pain was reported in 20% of patients in the lidocaine arm with a median visual analog scale of 0 out 10. Patients receiving lidocaine experienced transient dizziness and tinnitus 8% of the time and there were no serious adverse events [37]. It should be noted that this study was not powered to identify or compare rare but serious adverse events associated with intravenous lidocaine. Lidocaine may be considered for reducing the frequent, though minor, pain associated with peripheral HTS infusion.
There are few pediatric studies of HTS administered via peripheral IV; however, the available data suggests a similar low frequency and minor severity of complications as adults. The largest cohort of pediatric patients showed an overall complication rate of 3.8%, none of which required intervention. Short term pain and swelling were the most common complications and there were no reports of tissue injury from extravasation. There was a significantly higher rate of infiltration in pediatric patients receiving continuous infusion (7.6%) compared to those receiving bolus infusions (0.9%). Authors speculated that the frequency of occurrence in continuous infusion is related to the prolonged vascular contact with HTS [45]. In the two additional hospital-based pediatric studies, authors reported zero adverse events out of a total of 98 patients given HTS via peripheral IV [38, 43].
Though IRAE’s are generally reported as relatively infrequent and minor in the literature, safety with peripheral IV administration may be improved by following a few sensible practices. A recently published manuscript described a multi-disciplinary quality improvement project utilizing updated policies, nursing education, and development of electronic medical record order sets. Their policies restricted peripheral hypertonic saline infusion from 18 to 22 gauge IV catheters, placed proximal to the wrist, with less than 48-h dwell time, and prohibited the use of IVs started prior to hospital arrival. They also limited infusion rates to less than 100 ml/hr. Following these interventions, authors recorded an IRAE rate of 2.9% for peripheral hypertonic saline infusion. The three adverse events in their study were minor infusion site reactions that were managed by catheter removal and switching the infusion to a different peripheral IV [41]. While not directly compared, they achieved a lower frequency of adverse events that were also less severe than complications from central line placement reported in the literature [36]. Though the policies followed in the above study may be reasonable, caution should be advised in applying them as rigid requirements, as the evidence at this point does not consistently demonstrate a correlation between peripheral catheter size, location, or infusion rate with IRAE frequency.
Electrolyte abnormalities are reported in up to almost half of patients treated with HTS. Hyperchloremia is the most common abnormality occurring in 39–49% of patients, followed by hypokalemia (25–47%), and hypernatremia (8–22%) [42, 43]. Route of administration is not thought to influence the rate of electrolyte abnormalities. Chemistries should be monitored frequently during and after administration of hypertonic saline and risks from abnormal values should be weighed against the benefit of ongoing administration.
Intraosseous (IO)
When peripheral IV catheter placement is unobtainable, IO administration may be a suitable alternative in life-threatening situations to avoid treatment delays. One case series highlighted five adults with acute brain injury without central or peripheral venous access who received 3% saline through humeral or tibial IOs. There was an expected rise in serum sodium concentration and there were no episodes of infection, soft tissue injury, extravasation, or accidental IO dislodgement [47].
A separate case series described the infusion of 23.4% saline via IO in six patients with suspected impending herniation. All patients had an appropriate elevation in serum sodium concentration following infusion and there were no reported IO-related complications. Only one patient had ICP monitoring available at the time of infusion which demonstrated a reduction from 43 to 28 mmHg [48]. To date, there are no prospective studies reporting the safety and efficacy of IO HTS administration.
Conclusions
Hypertonic saline is an important tool in the care of critically ill patients with acute severe hyponatremia or elevated ICP. Three percent saline is indicated in patients with acute symptomatic hyponatremia and in all patients with moderate to severe symptoms resulting from hyponatremia regardless of chronicity. Boluses are preferred over continuous infusion due to more timely correction of severe symptoms without increased risk of overly rapid correction. Patients with a serum sodium concentration less than 120 mEq/L of greater than 48 h duration are at risk of ODS when undergoing treatment with HTS. Goals for immediate correction should be 4–6 mEq/L with no more than a 10 mEq/L rise in any 24-h period to avoid ODS. Certain patients face a markedly increased risk of ODS, including those with serum sodium concentration less than 105 mEq/L, alcoholism, cirrhosis, hypokalemia, and malnutrition. In this subgroup of patients, initial correction targets should be 4–6 mEq/L per day and not exceed 8 mEq/L in any 24-h period. In addition to hypertonic saline, all patients should undergo diagnostic workup to identify and initiate etiology specific treatment.
Hypertonic saline has been shown to reduce ICP in patients with cerebral edema of various causes. To date, evidence does not show effectiveness for improving neurologic outcomes or reducing mortality. Hypertonic saline may have less risk of causing hypovolemia and hypotension compared to mannitol and is preferred by the NCS for the treatment of elevated ICP stemming from TBI or ICH. Its use is supported as an alternative to mannitol for elevated ICP caused by SAH, acute ischemic stroke, bacterial meningitis, and hepatic encephalopathy. For most indications, there is not enough evidence to recommend a specific concentration or dosing strategy at this time.
Peripheral IV administration may result in minor infusion related pain as well as a low frequency of local infiltration, redness and swelling. These infrequent and minor adverse events should be weighed against the serious complications and treatment delays associated with central line placement. Peripheral IV administration should be utilized if there is no other indication for central line placement. Central line placement may be considered when continuous infusion will be prolonged over several days. IO administration appears safe and effective based on case reports and should be considered in life-threatening situations when IV access is not immediately obtainable. Electrolyte abnormalities are common regardless of route of administration and should be monitored frequently.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Mohan S, Gu S, Parikh A, Radhakrishnan J. Prevalence of hyponatremia and association with mortality: results from NHANES. Am J Med. 2013;126:1127-1137.e1.
Zhang X, Li X-Y. Prevalence of hyponatremia among older inpatients in a general hospital. Eur Geriatr Med. 2020;11:685–92.
Upadhyay A, Jaber BL, Madias NE. Incidence and prevalence of hyponatremia. Am J Med. 2006;119:S30–5.
•• Verbalis JG, Goldsmith SR, Greenberg A, Korzelius C, Schrier RW, Sterns RH, Thompson CJ. Diagnosis, evaluation, and treatment of hyponatremia: expert panel recommendations. Am J Med. 2013;126:S1-42. Most recent American guidelines on treating hyponatremia.
•• Spasovski G, Vanholder R, Allolio B, et al. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Eur J Endocrinol. 2014;170:G1-47. Most recent European guidelines on treating hyponatremia.
Buffington MA, Abreo K. Hyponatremia: a review. J Intensive Care Med. 2016;31:223–36.
Sterns RH, Riggs JE, Schochet SS. Osmotic demyelination syndrome following correction of hyponatremia. N Engl J Med. 1986;314:1535–42.
Lambeck J, Hieber M, DreBing A, Niesen WD. Central pontine myelinosis and osmotic demyelination syndrome. Dtsch Arxtebl Int. 2019;116:600–6.
Sterns RH, Nigwekar SU, Hix JK. The treatment of hyponatremia. Semin Nephrol. 2009;29:282–99.
Ayus JC, Caputo D, Bazerque F, Heguilen R, Gonzalez CD, Moritz ML. Treatment of hyponatremic encephalopathy with a 3% sodium chloride protocol: a case series. Am J Kidney Dis. 2015;65:435–42.
Garrahy A, Dineen R, Hannon AM, Cuesta M, Tormey W, Sherlock M, Thompson CJ. Continuous versus bolus infusion of hypertonic saline in the treatment of symptomatic hyponatremia caused by SIAD. J Clin Endocrinol Metab. 2019;104:3595–602.
Baek SH, Jo YH, Ahn S, Medina-Liabres K, Oh YK, Lee JB, Kim S. Risk of overcorrection in rapid intermittent bolus vs slow continuous infusion therapies of hypertonic saline for patients with symptomatic hyponatremia: The SALSA randomized clinical trial. JAMA Intern Med. 2021;181:81–92.
Sigal SH, Amin A, Chiodo JA, Sanyal A. Management strategies and outcomes for hyponatremia in cirrhosis in the hyponatremia registry. Can J Gatroenterol Hepatol. 2018;2018:1579508.
Hoorn EJ, Spasovski G. Recent developments in the management of acute and chronic hyponatremia. Curr Opin Nephrol Hypertens. 2019;28:424–32.
•• Cook AM, Morgan Jones G, Hawryluk GWJ, et al. Guidelines for the acute treatment of cerebral edema in neurocritical care patients. Neurocrit Care. 2020;32:647–66. Most recent Neurocritical Care Society Guidelines based on an in depth literature review.
Rangel-Castillo L, Gopinath S, Robertson CS. Management of intracranial hypertension. Neurol Clin. 2008;26:521–41.
Carter C, Human T. Efficacy, safety, and timing of 5% sodium chloride compared with 23.4% sodium chloride for osmotic therapy. Ann Pharmacother. 2017;51:625–9.
Busey K, Ferreira J, Aldridge P, Crandall M, Johnson D (2020) Comparison of weight-based dosing versus fixed dosing of 23.4% hypertonic saline for intracranial pressure reduction in patients with severe traumatic brain injury. J Emerg Trauma Shock 13:252
Maguigan KL, Dennis BM, Hamblin SE, Guillamondegui OD. Method of hypertonic saline administration: effects on osmolality in traumatic brain injury patients. J Clin Neurosci. 2017;39:147–50.
Vialet R, Albanèse J, Thomachot L, Antonini F, Bourgouin A, Alliez B, Martin C. Isovolume hypertonic solutes (sodium chloride or mannitol) in the treatment of refractory posttraumatic intracranial hypertension: 2 mL/kg 7.5% saline is more effective than 2 mL/kg 20% mannitol. Crit Care Med. 2003 Jun;31(6):1683–7. https://doi.org/10.1097/01.CCM.0000063268.91710.DF. PMID:12794404.
Kerwin AJ, Schinco MA, Tepas JJ 3rd, Renfro WH, Vitarbo EA, Muehlberger M. The use of 23.4% hypertonic saline for the management of elevated intracranial pressure in patients with severe traumatic brain injury: a pilot study. J Trauma. 2009 Aug;67(2):277–82. https://doi.org/10.1097/TA.0b013e3181acc726. PMID:19667879.
• Mekonnen M, Ong V, Florence TJ, Mozaffari K, Mahgerefteh N, Rana S, Duong C, Plurad DS, Yang I (2022) Hypertonic saline treatment in traumatic brain injury: a systematic review. World Neurosurgery 162:98–110. Most recent meta-analysis on HTS in TBI. This study confirms significant ICP reduction and suggests using lower concentrations for sustained reduction.
Pasarikovski CR, Alotaibi NM, Al-Mufti F, Macdonald RL. Hypertonic saline for increased intracranial pressure after aneurysmal subarachnoid hemorrhage: a systematic review. World Neurosurgery. 2017;105:1–6.
Hauer E-M, Stark D, Staykov D, Steigleder T, Schwab S, Bardutzky J. Early continuous hypertonic saline infusion in patients with severe cerebrovascular disease. Crit Care Med. 2011;39:1766–72.
Wagner I, Hauer E-M, Staykov D, Volbers B, Dörfler A, Schwab S, Bardutzky J. Effects of continuous hypertonic saline infusion on perihemorrhagic edema evolution. Stroke. 2011;42:1540–5.
Chen H, Song Z, Dennis JA. Hypertonic saline versus other intracranial pressure-lowering agents for people with acute traumatic brain injury. Cochrane Database Syst Rev. 2020. https://doi.org/10.1002/14651858.CD010904.pub3.
Rockswold GL, Solid CA, Paredes-Andrade E, Rockswold SB, Jancik JT, Quickel RR. Hypertonic saline and its effect on intracranial pressure, cerebral perfusion pressure, and brain tissue oxygen. Neurosurgery. 2009;65:1035–42.
F Munar AM Ferrer de NADAL M, Poca MA, Pedraza S, Sahuquillo J, Garnacho A, 2000 Cerebral hemodynamic effects of 7.2% hypertonic saline in patients with head injury and raised intracranial pressure J Neurotrauma 17:41–51
Boone M, Oren-Grinberg A, Robinson T, Chen C, Kasper E. Mannitol or hypertonic saline in the setting of traumatic brain injury: what have we learned? Surg Neurol Int. 2015;6:177.
Mangat HS, Chiu Y-L, Gerber LM, Alimi M, Ghajar J, Härtl R. Hypertonic saline reduces cumulative and daily intracranial pressure burdens after severe traumatic brain injury. JNS. 2015;122:202–10.
Kochanek PM, Adelson PD, Rosario BL, et al. Comparison of intracranial pressure measurements before and after hypertonic saline or mannitol treatment in children with severe traumatic brain injury. JAMA Netw Open. 2022;5: e220891.
Berger-Pelleiter E, Émond M, Lauzier F, Shields J-F, Turgeon AF. Hypertonic saline in severe traumatic brain injury: a systematic review and meta-analysis of randomized controlled trials. CJEM. 2016;18:112–20.
Shi J, Tan L, Ye J, Hu L. Hypertonic saline and mannitol in patients with traumatic brain injury: a systematic and meta-analysis. Medicine. 2020;99: e21655.
Strandvik GF. Hypertonic saline in critical care: a review of the literature and guidelines for use in hypotensive states and raised intracranial pressure. Anaesthesia. 2009;64:990–1003.
Mirtallo J, Canada T, Johnson D, Kumpf V, Petersen C, Sacks G, Seres D, Guenter P. Safe practices for parenteral nutrition. JPEN J Parenter Enteral Nutr. 2004;28:S39–70.
Parienti J-J, Mongardon N, Mégarbane B, et al. Intravascular complications of central venous catheterization by insertion site. N Engl J Med. 2015;373:1220–9.
Song Z, Chen S, Zhang Y, Shi X, Zhao N, Liao Z. Lidocaine coinfusion alleviates vascular pain induced by hypertonic saline infusion: a randomized, placebo-controlled trial. BMC Anesthesiol. 2021;21:109.
Brenkert TE, Estrada CM, McMorrow SP, Abramo TJ. Intravenous hypertonic saline use in the pediatric emergency department. Pediatr Emerg Care. 2013;29:71–3.
Dillon RC, Merchan C, Altshuler D, Papadopoulos J. Incidence of adverse events during peripheral administration of sodium chloride 3%. J Intensive Care Med. 2018;33:48–53.
Faiver L, Hensler D, Rush SC, Kashlan O, Williamson CA, Rajajee V. Safety and efficacy of 23.4% sodium chloride administered via peripheral venous access for the treatment of cerebral herniation and intracranial pressure elevation. Neurocrit Care. 2021;35:845–52.
Jannotta GE, Gulek BG, Dempsey JS, Blissitt PA, Sullivan HC, Tran K, Joffe A, Lele AV. Administration of 3% sodium chloride through peripheral intravenous access: development and implementation of a protocol for clinical practice. Worldviews on Evidence-Based Nursing. 2021;18:147–53.
Jones GM, Bode L, Riha H, Erdman MJ. Safety of continuous peripheral infusion of 3% sodium chloride solution in neurocritical care patients. Am J Crit Care. 2017;26:37–42.
Mesghali E, Fitter S, Bahjri K, Moussavi K. Safety of peripheral line administration of 3% hypertonic saline and mannitol in the emergency department. J Emerg Med. 2019;56:431–6.
Perez CA, Figueroa SA. Complication rates of 3% hypertonic saline infusion through peripheral intravenous access. J Neurosci Nurs. 2017;49:191–5.
Pohl CE, Harvey H, Foley J, Lee E, Xu R, O’Brien NF, Coufal NG. Peripheral IV administration of hypertonic saline: single-center retrospective picu study*. Pediatr Crit Care Med. 2022;23:277–85.
Meng L, Nguyen CM, Patel S, Mlynash M, Caulfield AF. Association between continuous peripheral i.v. infusion of 3% sodium chloride injection and phlebitis in adults. Am J Health Syst Pharm. 2018;75:284–91.
Lawson T, Hussein O, Nasir M, Hinduja A, Torbey MT. Intraosseous administration of hypertonic saline in acute brain-injured patients: a prospective case series and literature review. Neurologist. 2019;24:176–9.
Farrokh S, Cho S-M, Lefebvre AT, Zink EK, Schiavi A, Puttgen HA. Use of intraosseous hypertonic saline in critically ill patients. J Vasc Access. 2019;20:427–32.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dangers, J., Enders, M. & Helberg, T. Hypertonic Saline in the Critically Ill: A Review of Indications, Routes, and Dosing. Curr Emerg Hosp Med Rep 11, 95–102 (2023). https://doi.org/10.1007/s40138-023-00267-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40138-023-00267-2