Abstract
Purpose of Review
We aimed to describe bleeding events associated with extracorporeal cardiopulmonary resuscitation (eCPR) using two institutional heparin protocols. In addition, we discuss current barriers to optimal anticoagulation in this critical population.
Recent Findings
Patients initiated on venoarterial membrane oxygenation (VA-ECMO) are at risk of bleeding and thrombosis; both conditions can lead to severe morbidity or mortality. Intravenous heparin is the preferred form of anticoagulation for VA-ECMO. Prior studies have found elevated activated partial thromboplastin time (aPTT) may be an independent risk factor for bleeding; however, many studies lack standardization of bleeding scores and optimal anticoagulation targets.
Summary
All six patients initiated on VA-ECMO experienced at least one bleeding event. Of 71 aPTT levels collected, 44% were within therapeutic range, 18% were subtherapeutic, and 38% were supratherapeutic. There were no obvious correlation between aPTT levels and bleeding. Future studies are needed to evaluate anticoagulation strategies in this population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction/Background
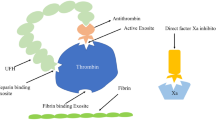
Extracorporeal cardiopulmonary resuscitation (eCPR) using venoarterial extracorporeal membrane oxygenation (VA-ECMO) is increasing throughout the world. Improving survival and favorable neurological outcomes has led to increased use as advanced therapy for out-of-hospital cardiac arrest [1,2,3]. eCPR is appealing because it provides full cardiopulmonary support to patients in cardiopulmonary arrest [4•]. This benefits providers and patients by allowing cessation of external chest compressions, thus reducing trauma, and minimizing stress, in addition to providing time for diagnosis and treatment of the underlying arrest etiology [5, 6]. Initiation of eCPR often includes a loading dose of a preferred anticoagulant upon cannulation and priming. The Extracorporeal Life Support Organization (ELSO) recommends utilizing unfractionated heparin (UFH) at a dose of 50–100 units/kg upon initiation, then following with an intravenous continuous infusion. Anticoagulation strategies are mixed and vary between institutions; however, UFH is most often used [4•, 7•, 8, 9•]. Bleeding events associated with eCPR are a major complication and hemorrhagic complications are well understood to be the most common adverse effects of VA-ECMO, significantly contributing to morbidity and death [10, 11••]. To our knowledge, the existing literature around anticoagulation during eCPR is limited to descriptive practices or procedures to reduce bleeding in patients initiated on VA-ECMO in the emergency department. This study aimed to evaluate heparin anticoagulation and bleeding events in adult patients initiated on VA-ECMO for eCPR in the emergency department after out-of-hospital cardiac arrest.
Methods
This study was a single-center retrospective chart review of all emergency department (ED) eCPR cases from July 2015 through July 2016 at the University of Utah. University of Utah Health is a tertiary academic medical center serving as a safety net hospital for the mountain states region, with over 60,000 emergency department visits annually. Patients were included if they sustained cardiac arrest treated in the ED with resuscitative VA-ECMO. Patients were excluded if they survived less than 24 h, transferred from an outside facility, or cannulated for VA-ECMO in an inpatient intensive care unit or catheterization lab. This study was approved by the University of Utah Institutional Review Board.
The primary endpoint was the percentage of measured activated partial thromboplastin time (aPTT) levels within therapeutic range, according to the institution’s selected heparin protocol. Secondary endpoints were bleeding events on heparin, defined by the Bleeding Academic Research Consortium (BARC) grading, and in hospital mortality.
Data was obtained through electronic medical records (EMR). Information collected included baseline characteristics, heparin protocol ordered, complete blood count, aPTT, bleeding events, and death during hospitalization. Patients were identified as having a bleeding event if they had a decrease in hemoglobin of at least 3 points over 24 h, if they received at least 1 unit of packed red blood cell (PRBC) transfusion, or if a medical note stated there was bleeding requiring medical action. Any bleeding event identified was categorized using BARC definitions.
Due to the retrospective and descriptive nature of this study, sample size calculations and statistical analysis were not performed.
Anticoagulant Titration Management
At our institution, heparin is the most common anticoagulant used during extracorporeal life support (ECLS), including ECMO. During ECMO cannulation, patients are initially given up to 5000 units of heparin as a bolus, then initiated on a heparin drip, managed per protocol.
There are two heparin protocols available at our institution routinely used while patients are on ECMO therapy. One protocol, called the high dose (HD) protocol, targets aPTT goals between 70 and 90 s; the second low dose (LD) protocol targets aPTT goals of 40–60 s. Neither protocol utilizes a bolus on initiation or intermittently for low aPTT levels. Heparin drip rates are titrated up or down by trained nursing staff based on aPTT levels drawn every 6 h.
Results
From July 1, 2015 to June 30, 2016, 7 patients were cannulated for VA-ECMO for ongoing circulatory support due to refractory out-of-hospital cardiac arrest in the ED. A single patient was excluded for ineffectual VA-ECMO cannulation and subsequent death, leaving 6 patients assessed. Demographic characteristics are outlined in Table 1. Of the six patients, median age was 53.5 (± 7) years, 50% were male, and 83% had at least one cardiovascular risk factor.
After initial heparin exposure, all patients were initiated on the LD heparin drip protocol. Three of the six patients were transitioned to the HD heparin protocol at 19, 28, and 64 h, respectively. Patients were deemed hemodynamically stable without evidence of overt bleeding at the time of transition. Three patients were never placed on the HD heparin protocol during VA-ECMO and had no reported thrombosis events during the hospitalization.
Out of 71 aPTT levels collected while patients were on both ECMO and heparin, 44% were within therapeutic range, while 18% were subtherapeutic, and 38% were supratherapeutic, per the ordered heparin protocol (Table 2). Using BARC definitions for bleeding, 13 type 2 and 10 type 3a bleeding events were identified [12, 13••]. Type 2 bleeding was most commonly identified through medical notes containing information regarding cannulation sites with consistent oozing, small hematomas, or persistent gastrointestinal bleeding (GIB). All BARC type 2 bleeding lead to a bleeding assessment by the cardiothoracic and intensive care unit (ICU) teams. Interventions for type 2 bleeding included blood transfusions, holding pressure at cannula sites, or surgical investigation of bleeding sites. BARC type 3a bleeding was identified by a hemoglobin drop of ≥ 3 g/dL and/or blood products administered for hemodynamic stabilization (Table 3).
Among all patients, 32 units of PRBC, 4 units of fresh frozen plasma (FFP), and 3 platelets (PLTs) were administered. Of 26 aPTT levels drawn within 6 h prior to blood transfusions, 88.5% were below 70 s (aPTT 42 ± 11 s), while 11.5% were greater than or equal to 70 s (PTT 122 ± 45). Vasoactive agents were required intermittently in all patients at some point during VA-ECMO therapy. Vasopressin and epinephrine were most commonly utilized to maintain hemodynamic stability. Eight of the 10 BARC type 3 bleeding events required PRBCs and initiation or increased dose of vasoactive agents. APTT levels were recorded at the time a BARC bleeding event was documented shown in Fig. 1. A majority of bleeding events were noted to occur with an aPTT < 70 s.
Discussion and Limitations
In this small observational study, we sought to review bleeding events and the corresponding aPTT levels in patients placed on VA-ECMO in the ED. Out of 6 patients, all patients met at least one BARC definition of bleeding while on VA-ECMO therapy. Most bleeding sources were identified as surgical site or ear, nose, and throat (ENT) related bleeding requiring blood products. Our main finding in our small cohort of patients, bleeding events occurred regardless of the aPTT. This raises the question of whether aPTT levels are reliable in this population or predictive of bleeding, and thus of the validity and utility of targeting therapeutic aPTT levels.
There is a general understanding that exposure of blood through the ECMO circuit results in both inflammatory and pro-thrombotic responses, necessitating the use of systemic anticoagulation. While the causes of bleeding are known to be multifactorial, with platelet activation, von Willebrand factor depletion, and hyperfibrinolysis, the type and intensity of anticoagulation needed has yet to be fully understood [8, 14, 15•, 16]. Likewise, given the multifactorial nature of coagulopathy during mechanical circulatory support, alternative assessments of anticoagulation have been proposed, including D-Dimer and ROTEM [17,18,19,20], with varying results.
The utilization of blood products to maintain hemostasis is commonly used in ECMO. Although ELSO recommends maintaining hemoglobin levels within the normal range of 8–12 g/dL, there is little clinical data to support this practice to be superior. In our observed population, 29 PRBC transfusions occurred while on heparin therapy. In practice, providers may not achieve recommended levels and have to weigh benefits and risks of multiple transfusions. Multiple analysis observing adult ECMO found survivors received less PRBC transfusions and adopting restrictive transfusion practices is reasonable and safe [19, 21]. Although the finding has not been validated prospectively in a large randomized study, the risks of transfusions are known to place patients at risk of transfusion-related complications such as acute lung injury and hemolytic reactions [22, 23].
Overall, bleeding complications reported in the literature occur in over 50% of patients who receive extracorporeal membrane oxygenation therapies (ECMO) [11••, 24••]. The variations in bleeding rates may be contributed by the lack of standard bleeding scores for this population. It is reported that surgical site bleeding at the cannulation site is the most common source of bleeding in ECMO [25, 26]. In our cohort, we found cannulation and ENT-associated sites to be the most common sources of bleeding. While intracranial bleeding is a known complication of ECMO, we did not identify any intracranial hemorrhage (ICH) events in our sample.
Conclusion
Our study, although limited to a small sample size, demonstrated aPTT did not correlate with bleeding events. Forty-four percent of all aPTT levels met the targeted goal range leaving room for improvements in protocol adherence. All patients met at least one BARC bleeding criteria while on VA-ECMO. Although half of our patient population had in hospital death, in no case was it due to uncontrolled or fatal bleeding. This descriptive study suggests the need for larger prospective studies to assess for optimal coagulation targets.
Source of Funding
This study was supported, in part, by the University of Utah Study Design and Biostatistics Center, with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 5UL1TR001067-02 (formerly 8UL1TR000105 and UL1RR025764).
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Dalle Ave AL, Shaw DM, Gardiner D. Extracorporeal membrane oxygenation (ECMO) assisted cardiopulmonary resuscitation or uncontrolled donation after the circulatory determination of death following out-of-hospital refractory cardiac arrest-an ethical analysis of an unresolved clinical dilemma. Resuscitation. 2016;108:87–94.
Lee JJ, Han SJ, Kim HS, Hong KS, Choi HH, Park KT, et al. Out-of-hospital cardiac arrest patients treated with cardiopulmonary resuscitation using extracorporeal membrane oxygenation: focus on survival rate and neurologic outcome. Scand J Trauma Resusc Emerg Med. 2016;24:74.
Choi DH, Kim YJ, Ryoo SM, Sohn CH, Ahn S, Seo DW, et al. Extracorporeal cardiopulmonary resuscitation among patients with out-of-hospital cardiac arrest. Clin Exp Emerg Med. 2016;3(3):132–8.
• Tonna JE, Johnson NJ, Greenwood J, Gaieski DF, Shinar Z, Bellezo JM, et al. Practice characteristics of emergency department extracorporeal cardiopulmonary resuscitation (eCPR) programs in the United States: the current state of the art of emergency department extracorporeal membrane oxygenation (ED ECMO). Resuscitation. 2016;107:38–46. This article is important because it describes the culture and lack of inclusion and exclusion for patients who received VA-ECMO in an emergency department.
Hunziker S, Semmer NK, Tschan F, Schuetz P, Mueller B, Marsch S. Dynamics and association of different acute stress markers with performance during a simulated resuscitation. Resuscitation. 2012;83(5):572–8.
Shin TG, Jo IJ, Sim MS, Song YB, Yang JH, Hahn JY, et al. Two-year survival and neurological outcome of in-hospital cardiac arrest patients rescued by extracorporeal cardiopulmonary resuscitation. Int J Cardiol. 2013;168(4):3424–30.
• Iwashita Y, Yukimitsu M, Matsuduki M, Yamamoto A, Ishikura K, Imai H. Use of a fixed, body weight-unadjusted loading dose of unfractionated heparin for extracorporeal cardiopulmonary resuscitation. J Intensive Care. 2015;3(1):33. This article is important because it describes fixed heparin bolus doses used in ECMO and resulted in fatal bleeding events.
Murphy DA, Hockings LE, Andrews RK, Aubron C, Gardiner EE, Pellegrino VA, et al. Extracorporeal membrane oxygenation-hemostatic complications. Transfus Med Rev. 2015;29(2):90–101.
• Oliver WC. Anticoagulation and coagulation management for ECMO. Semin Cardiothorac Vasc Anesth. 2009;13(3):154–75. This article is important because it provides a review of methods used to monitor anticoagulation in patients with ECMO.
Factora FN, et al. Intracranial hemorrhage surgery on patients on mechanical circulatory support: a case series. J Neurosurg Anesthesiol. 2011;23(1):30–4.
•• Sy E, Sklar MC, Lequier L, Fan E, Kanji HD. Anticoagulation practices and the prevalence of major bleeding, thromboembolic events, and mortality in venoarterial extracorporeal membrane oxygenation: a systematic review and meta-analysis. J Crit Care. 2017;39:87–96. This systematic review is important because it demonstrated optimal targets and strategies for anticoagulation monitoring in VA-ECMO are unclear.
Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123(23):2736–47.
•• Vranckx P, White HD, Huang Z, Mahaffey KW, Armstrong PW, van de Werf F, et al. Validation of BARC bleeding criteria in patients with acute coronary syndromes: the TRACER trial. J Am Coll Cardiol. 2016;67(18):2135–44. This article is significant because it validates the use of BARC bleeding scales for ACS related trials due to its association with death after a cardiac event with higher BARC scores.
Lim JY, Kim JB, Choo SJ, Chung CH, Lee JW, Jung SH. Anticoagulation during extracorporeal membrane oxygenation; nafamostat mesilate versus heparin. Ann Thorac Surg. 2016;102(2):534–9.
• Lamarche Y, Chow B, Bédard A, Johal N, Kaan A, Humphries KH, et al. Thromboembolic events in patients on extracorporeal membrane oxygenation without anticoagulation. Innovations (Phila). 2010;5(6):424–9. This article is significant because the researchers used no anticoagulation in VA-ECMO without increased thromboembolic events.
Da Q, et al. Free hemoglobin increases von Willebrand factor-mediated platelet adhesion in vitro: implications for circulatory devices. Blood. 2015;126(20):2338–41.
Otani T, Sawano H, Natsukawa T, Matsuoka R, Nakashima T, Takahagi M, et al. D-dimer predicts bleeding complication in out-of-hospital cardiac arrest resuscitated with ECMO. Am J Emerg Med. 2018;36(6):1003–8.
Prakash S, et al. Discordance between ROTEM(R) clotting time and conventional tests during unfractionated heparin-based anticoagulation in intensive care patients on extracorporeal membrane oxygenation. Anaesth Intensive Care. 2016;44(1):85–92.
Park HSKaS. Blood transfusion strategies in patients undergoing extracorporeal membrane oxygenation. Koran J Crit Care Med. 2017;21(1):22–8.
Malfertheiner MV, et al. Acquired von Willebrand syndrome in respiratory extracorporeal life support: a systematic review of the literature. Critical Care And Resuscitation: Journal Of The Australasian Academy Of Crit Care Resusc. 2017;19(Suppl 1):45–52.
Omar HR, et al. Plasma free hemoglobin is an independent predictor of mortality among patients on extracorporeal membrane oxygenation support. PLoS One. 2015;10(4):e0124034.
Tekindur S, Yetim M, Kilickaya O. Risk of transfusion-related acute lung injury after blood products transfusions. Am J Emerg Med. 2016;34(8):1674–5.
Zalpuri S, et al. Intensive red blood cell transfusions and risk of alloimmunization. Transfusion. 2014;54(2):278–84.
•• Aubron C, DePuydt J, Belon F, Bailey M, Schmidt M, Sheldrake J, et al. Predictive factors of bleeding events in adults undergoing extracorporeal membrane oxygenation. Ann Intensive Care. 2016;6(1):97. This article is important because it concluded elevated aPTT levels were associated with more bleeding events.
Aubron C, Cheng AC, Pilcher D, Leong T, Magrin G, Cooper DJ, et al. Factors associated with outcomes of patients on extracorporeal membrane oxygenation support: a 5-year cohort study. Crit Care. 2013;17(2):R73.
Bakhtiary F, Keller H, Dogan S, Dzemali O, Oezaslan F, Meininger D, et al. Venoarterial extracorporeal membrane oxygenation for treatment of cardiogenic shock: clinical experiences in 45 adult patients. J Thorac Cardiovasc Surg. 2008;135(2):382–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pharmacology Care
Rights and permissions
About this article
Cite this article
Terry, K., Lonardo, N. & Tonna, J. Anticoagulation Levels and Bleeding After Emergency Department Extracorporeal Cardiopulmonary Resuscitation. Curr Emerg Hosp Med Rep 7, 1–5 (2019). https://doi.org/10.1007/s40138-019-00176-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40138-019-00176-3