Abstract
Sentinel lymph node (SLN) dissection provides a minimally invasive approach for axillary staging in breast cancer and is the standard of care in patients with clinically node-negative disease. In patients with node-positive disease, the traditional approach has been axillary lymph node dissection (ALND). After neoadjuvant chemotherapy, approximately 40 % of patients will be converted from clinically node positive to pathologically node negative raising significant interest in evaluating the role of SLN dissection in this clinical setting. Several clinical trials have evaluated the feasibility and accuracy of SLN dissection after neoadjuvant chemotherapy in patients with node-positive disease including ACOSOG Z1071, SENTINA, and SN FNAC. In these trials, the false negative rate of the procedure has been reported to be >10 % when SLNs are evaluated by hematoxylin and eosin staining. However, there are several factors which have been identified to be associated with improved accuracy including the number of SLNs examined and the use of dual tracer lymphatic mapping. The SN FNAC trial also reported improved accuracy when immunohistochemistry was used in SLN evaluation. Patient selection is an important consideration as those with a low likelihood for residual disease and high likelihood of pathologic complete response are the most likely to benefit from this approach. Although, ALND remains the standard of care in these patients, there may be a selective role for SLN dissection in this setting. An alternative approach targeting removal of the known axillary disease in addition to SLN dissection may improve accuracy and is the focus of current investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical management of the axilla has remained an area of controversy in breast cancer treatment. Axillary surgery primarily provides accurate disease staging with implications regarding prognosis and treatment planning. Sentinel lymph node (SLN) dissection has become the standard approach for patients with clinically node-negative disease as it provides accurate axillary staging with decreased morbidity when compared to axillary lymph node dissection (ALND) [1, 2]. Patients presenting with node-positive disease have traditionally been managed with ALND. In contemporary practice, this paradigm has been challenged by findings from the ACOSOG Z0011 trial in which patients with early stage breast cancer treated with breast conservation and found to have 1–2 positive SLNs did not benefit from completion ALND in terms of overall survival or local–regional recurrence [3•, 4].
Clinicians have also questioned the value of ALND in patients who receive neoadjuvant chemotherapy. Neoadjuvant chemotherapy, initially introduced in the management of patients with locally advanced breast cancer, is increasingly employed in the management of operable breast cancer. Although landmark trials did not demonstrate a survival advantage with this approach as compared to adjuvant chemotherapy, several benefits were realized including—facilitation of breast conservation and improved survival in patients who achieved a pathologic complete response (pCR) in the primary tumor and axillary lymph nodes [5]. Historically, many surgeons performed SLN dissection prior to chemotherapy in patients presenting with clinically node-negative disease. This approach has largely been abandoned since patients who have a positive SLN will be committed to ALND at the completion of chemotherapy. This also means the patient would be subjected to two surgical procedures (SLN dissection before chemotherapy and ALND following chemotherapy) and the opportunity to evaluate pathologic response in the nodes is no longer possible. Several groups have reported that SLN dissection is accurate following chemotherapy in patients who are clinically node negative at presentation [6]. There have been three meta-analyses examining the accuracy in this clinical setting and all have concluded that the procedure is feasible and accurate [7–9].
In patients who present with clinically node-positive disease proven with fine-needle aspiration or core biopsy, up to 40 % will be converted to pathologically node negative with neoadjuvant chemotherapy. These patients are unlikely to benefit from ALND and this has led many investigators to evaluate the utility of SLN dissection in this population. If SLN dissection could replace ALND in patients with a good response to neoadjuvant therapy, they could be spared the morbidity of ALND which includes lymphedema, decreased range of motion about the shoulder and axillary and brachial paresthesias.
This review evaluates the current role of SLN surgery following neoadjuvant chemotherapy in breast cancer patients who present with clinically node-positive disease. The feasibility and accuracy of SLN dissection in this setting will be discussed as well as additional important considerations including nodal disease burden, tumor biology, and multidisciplinary considerations. Lastly, we will describe the targeted axillary dissection, an alternative approach to axillary staging after neoadjuvant therapy that is currently under investigation at our institution.
SLN Dissection After Neoadjuvant Chemotherapy in Node-Positive Breast Cancer: Summary of Findings from Completed Clinical Trials
The primary concerns regarding the use of SLN surgery after neoadjuvant chemotherapy in node-positive breast cancer include the feasibility of the procedure in SLN identification and the accuracy of the procedure. These are described by the SLN identification rate and false negative rate, respectively. Several institutions have evaluated the role of SLN dissection after neoadjuvant chemotherapy in node-positive breast cancer and reported false negative rates ranging from 6 to 25 % [10–16]. A retrospective analysis from the NSABP B-27 trial of 428 patients who underwent SLN dissection in addition to ALND after neoadjuvant chemotherapy found a SLN identification rate of 84.8 % and false negative rate of 10.7 % [17]. This analysis included both clinically node-negative and node-positive patients with no significant difference in the false negative rates between the groups. This suggested a potential role for SLN surgery after neoadjuvant chemotherapy, prompting further investigation.
Recently, three large multicenter prospective trials evaluating the feasibility and accuracy of SLN dissection after chemotherapy in patients who present with clinically node-positive disease have completed accrual and reported results. These trials will be described below and discussed as to how they provide further insight into this clinical question.
Clinical Trials
ACOSOG Z1071
The American College of Surgeons Oncology Group (ACOSOG) Z1071 is a phase II multicenter trial planned to determine the false negative rate of SLN dissection after neoadjuvant chemotherapy in breast cancer patients with node-positive disease at presentation. Eligible patients included those with clinical stage T0–4 N1–2 M0 breast cancer and biopsy-proven axillary disease. All received neoadjuvant chemotherapy followed by SLN dissection and completion ALND. The protocol specified that at least two SLNs should be removed and suggested that dual tracer technique (blue dye and radioisotope) was used to identify the SLNs. SLNs were evaluated by hematoxylin and eosin (H & E) staining and determined to be positive if the metastatic focus was >0.2 mm.
From July 2009 to June 2011, 649 patients with N1 disease completed chemotherapy, SLN dissection and ALND. The SLN identification rate was 92.9 %. Five hundred and twenty-five patients had two or more SLNs identified and were included in the primary endpoint analysis. Among these patients 41 % had an axillary pCR. The primary endpoint was the false negative rate for SLN dissection after neoadjuvant chemotherapy in patients with clinical N1 disease and at least two SLNs examined. The false negative rate was found to be 12.6 % (95 % CI 9.85–16.05 %). Factors affecting the false negative rate included dual tracer technique (10.8 % with dual tracer as compared to 20.3 % with a single agent, p = 0.05) and the number of SLNs examined (31.5 % with one SLN, 21 % with two SLNs, and 9.1 % with three or more SLNs, p = 0.007) [18••].
SENTINA Trial
The SENTinel NeoAdjuvant (SENTINA) study is a four arm prospective multicenter trial evaluating SLN dissection and ALND in breast cancer patients treated with neoadjuvant chemotherapy. In this trial, Arm C included clinically node-positive patients who converted to clinically node negative after neoadjuvant chemotherapy. Eligible patients had clinical N1 or N2 disease which was determined by clinical exam and axillary ultrasound, however, biopsy was not required. The SLN procedure was standardized such that radioisotope was utilized in each case, and the use of blue dye was optional. SLNs were examined by H&E staining.
From September 2009 to May 2012, 592 patients were enrolled in Arm C, and an axillary pCR was achieved in 52.3 % of patients. The SLN identification rate was 80.1 % overall, 87.8 % with dual mapping and 77.4 % with radioisotope alone. The primary endpoint was the false negative rate of SLN dissection after neoadjuvant chemotherapy, which was determined to be 14.2 % (95 % CI 9.9–19.4 %). Multivariate analysis found factors affecting the false negative rate to include the number of SLNs examined (24.3 % with one SLN, 18.5 % with two SLNs, and <10 % with three or more SLNs, p = 0.008) and mapping technique, although the latter was not a statistically significant finding (8.6 % with dual mapping, 16 % with radiocolloid alone, p = 0.145). Only one quarter of patients in Arm C had biopsy-proven nodal disease at presentation, however, there was no difference in accuracy if nodal positivity was defined by biopsy or clinical exam [19••].
SN FNAC
The sentinel node biopsy following neoadjuvant chemotherapy (SN FNAC) study is also a prospective multicenter phase II trial evaluating the accuracy of SLN dissection after neoadjuvant chemotherapy in breast cancer patients with biopsy-proven node-positive disease at presentation. Eligible patients included those with clinical stage T0–3 N1–2 all of whom underwent neoadjuvant chemotherapy followed by SLN dissection and ALND. SLN status was determined first by H&E staining and, if negative, evaluation by immunohistochemistry (IHC) was mandatory. Accrual to this study was closed early after the results of the ACOSOG Z1071 trial were reported given the similarities between the trials.
From March 2009 to December 2012, 145 patients were included in the final analysis. The axillary pCR rate was 34.5 %. The SLN identification rate was 87.6 % overall, 87.5 % if one SLN was identified and 96.8 % if two or more SLNs were identified. In the setting of a technical failure, two-thirds of patients had positive nodes. The overall false negative rate was 8.4 % (95 % CI 2.4–14.4 %). Factors impacting the false negative rate included the number of SLNs examined (18.2 % with one SLN compared to 4.9 % with two or more SLNs, p = 0.076) and the use of dual tracer (5.2 % with dual tracer mapping compared to 16.0 % with one mapping agent, p = 0.190). Interestingly, the false negative rate was 13.3 % when the SLNs were examined by H&E alone. The use of IHC decreased the false negative rate by increasing the detection of isolated tumor cells and micrometastasis [20••].
In these three trials, the false negative rate of SLN dissection after neoadjuvant chemotherapy in patients with clinically node-positive disease at presentation was over 10 %—the generally acceptable threshold established by trials evaluating SLN dissection in the clinically node-negative setting. At first pass, this would suggest that SLN dissection after neoadjuvant chemotherapy should not routinely be performed in the setting of node-positive disease. However, these trials also identified several factors, including operative technique and patient selection, which improved the accuracy of SLN dissection in this setting. Consideration of these factors is important when discussing the application of SLN surgery after neoadjuvant chemotherapy in node-positive patients. The standard of care in current practice remains axillary dissection, although the approach to axillary management in this clinical setting continues to be the focus of ongoing investigation.
Techniques to Improve the False Negative Rate
The number of SLNs examined is an important factor influencing the accuracy of SLN dissection after neoadjuvant chemotherapy in node-positive breast cancer that was noted in each of the major trials. Collectively, they suggest that the false negative rate reaches an acceptable threshold when three or more SLNs are examined. This suggests that in the clinical scenario when 0–2 SLN are identified ALND may still be warranted given the lack of confidence in accurately defining the residual axillary disease burden.
The mapping technique utilized for SLN identification has also been highlighted as an important factor in improving the accuracy of SLN in this setting. Use of dual tracer with blue dye and radioisotope has previously been described to improve the SLN identification rate and false negative rate after neoadjuvant chemotherapy [6]. Although this was not a requirement in any of the major trials, each described improved accuracy with use of dual tracer. This suggests that SLN dissection after neoadjuvant chemotherapy in node-positive patients should only be performed using dual-agent lymphatic mapping.
In 171 patients registered on the Z1071 trial, a clip was placed at the time of the initial biopsy indicating the positive node. When the clipped node was documented to also be one of the SLNs removed, the false negative rate was improved to 6.8 % [21, 22]. Other techniques for marking the involved node such as tattooing with ink have also been described [23]. This finding supports marking the known positive node prior to chemotherapy and confirming removal at the time of surgery to evaluate response as this node effectively also represents a SLN. The current NCCN guidelines recommend placement of a clip marker into an axillary node found to be positive at the time of biopsy [24].
Another consideration is the definition of pathologic node-negative disease in this clinical setting. The Z1071 and SENTINA trials used H&E evaluation of the SLNs, whereas the SN FNAC trial also included IHC analysis and defined a positive SLN to include those with isolated tumor cells and micrometastasis. The false negative rate was lower in the SN FNAC trial when the IHC results were included. In the Z1071 trial, a positive node was defined as disease >0.2 mm. The Z1071 investigators recently reported results of IHC staining on H&E negative SLNs and found that the false negative rate was lowered to 8.7 % when disease <0.2 mm was considered to be a positive node [22]. Whether persistent nodal disease of this size is clinically relevant after neoadjuvant chemotherapy has been debated. A recent meta-analysis of patients with initial node-positive disease reported a significant decrease in the false negative rate from 16 to 8.7 % (p = 0.001) with the addition of IHC after H&E evaluation showed negative findings in the SLN after neoadjuvant chemotherapy [25•]. It is not known if this definition for SLN positivity would have implications on the SENTINA findings.
Considerations in Patient Selection
Nodal Disease Burden
The preoperative nodal disease burden is also an important consideration. Patients with clinical N2 disease represented a minority of patients in the major clinical trials evaluating SLN after neoadjuvant chemotherapy. The Z1071 trial included 38 patients with clinical N2 disease of which 25 had two or more SLNs examined. The pCR rate was 46.1 % in this group. The false negative rate was 0 % as all 14 patients who did not have a pCR were found to have positive SLNs [18••]. These patients were not included in the primary endpoint analysis and with limited experience it is difficult to infer the role and accuracy of SLN dissection in this population.
Patients with significant nodal disease burden on imaging or clinical examination following chemotherapy may not be candidates for SLN surgery after neoadjuvant chemotherapy. In the SENTINA trial, patients with clinically node-positive disease following chemotherapy were treated with axillary lymph node dissection (Arm D). In the Z1071 trial, patients could be registered at the initiation or at the completion of chemotherapy. The trial did not specify any selection criteria for proceeding with SLN surgery based on nodal status after chemotherapy. Ultrasound of the axilla was performed before and after chemotherapy to assess for residual nodal disease. The investigators found that 56.5 % of patients with normal findings by axillary ultrasound had pathologically positive nodes as compared to 71.8 % of those with suspicious nodes by axillary ultrasound after neoadjuvant chemotherapy (p < 0.001). They also describe the false negative rate to improve to 9.8 % if patients with suspicious findings on axillary ultrasound after chemotherapy are excluded from SLN dissection [26].
This suggests axillary ultrasound can be a tool to identify patients with residual disease and who may not be ideal candidates for SLN surgery after neoadjuvant chemotherapy. The utility of SLN dissection in patients with residual clinically node-positive disease following chemotherapy has not been demonstrated and is not warranted.
Tumor Biology
Several studies have demonstrated a significant relationship between approximated biologic subtype and the response to neoadjuvant chemotherapy. Patients with hormone receptor negative disease are most likely to achieve a pCR and those with HER-2-positive disease treated with chemotherapy and trastuzumab have the highest reported axillary pCR rates [27, 28].
The Z1071 investigators reported the overall nodal pCR rate to be 41 %. When they evaluated the axillary pCR rate by tumor subtype, there was a significantly higher rate in triple negative disease (49.4 %) and HER-2-positive disease (64.7 %) as compared to hormone receptor-positive, HER-2-negative disease. Similarly, the burden of residual disease after neoadjuvant chemotherapy correlated with the tumor subtype, with increased residual burden in hormone receptor-positive, HER-2-negative disease as compared to triple negative or HER-2-positive disease [29].
This implies that with an increased likelihood for pCR, patients presenting with triple negative or HER-2-positive breast cancer and low nodal disease burden may be better candidates for SLN surgery after neoadjuvant chemotherapy. However, this has not been demonstrated or specifically evaluated in the previously described clinical trials. At this time, tumor subtype independent of the clinical response to therapy and nodal disease burden is not a factor in clinical decision making regarding SLN surgery after neoadjuvant chemotherapy.
Can We Replace ALND with Adjuvant Radiation in the Setting of a Positive SLN After Neoadjuvant Chemotherapy? Multidisciplinary Considerations
In current practice, patients found to have evidence of residual disease after treatment with neoadjuvant chemotherapy typically do not receive adjuvant chemotherapy. Given this, it is unlikely that SLN surgery after neoadjuvant chemotherapy will have an impact on recommendations regarding the receipt of further systemic therapy.
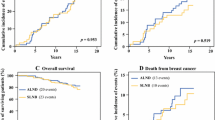
However, residual disease following chemotherapy does have implications regarding adjuvant radiation therapy. Increasingly, the role of radiation therapy in treatment of residual axillary disease is being studied in the clinically node-negative setting. It has been estimated that traditional whole breast radiation tangential fields include a significant portion of the axilla and may have had an impact on the ACOSOG Z0011 findings [30, 31]. The recently reported AMAROS trial evaluated axillary radiation as compared to completion ALND in patients with positive SLNs treated with upfront surgery. The investigators found no difference in local–regional recurrence or survival but did identify a lower incidence of lymphedema in the axillary radiation group [32]. Neither of these studies enrolled patients treated with neoadjuvant chemotherapy.
There are two ongoing clinical trials addressing the role and impact of radiation therapy after neoadjuvant chemotherapy in patients who present with clinically node-positive disease. The ALLIANCE A011202 study is a randomized phase III trial comparing axillary radiation to ALND in patients who present with node-positive disease, are treated with neoadjuvant chemotherapy and have positive SLNs after chemotherapy. All patients receive nodal irradiation to the supraclavicular and internal mammary nodal basins [33].
The NSABP B-51/RTOG 1304 trial is a randomized phase III trial comparing whole breast or chest wall irradiation with regional nodal irradiation versus no regional nodal irradiation in patients who are converted from clinically node positive to pathologically node negative after neoadjuvant chemotherapy. This trial includes axillary staging by ALND, SLN dissection alone, or SLN dissection followed by completion ALND [34]. The primary aim of these studies is to evaluate for invasive breast cancer recurrence-free survival between groups. These trials will be informative in better defining the optimal local–regional approach for these patients with the potential for decreased morbidity.
MDACC Approach: Targeted Axillary Dissection
At the University of Texas MD Anderson Cancer Center, we are currently investigating an alternative approach to management of the axilla in breast cancer patients with node-positive disease treated with neoadjuvant chemotherapy which we have designated as targeted axillary dissection (TAD). This approach is guided by findings of the Z1071 trial in which the accuracy of SLN dissection after neoadjuvant chemotherapy was improved when the clinically positive node was marked with a clip prior to therapy and also found to be a SLN. Targeted axillary dissection is defined as removal of the node proven at diagnosis to have metastatic disease (clipped node) as well as the SLNs [35•].
Our institutional practice is for all breast cancer patients with invasive disease to undergo a staging ultrasound of the breast and regional nodal basins at the time of presentation. Any suspicious appearing nodes are evaluated further with biopsy. For patients with abnormal appearing axillary disease consistent with clinical N1 disease, a clip is placed within the node if the biopsy shows malignancy (Fig. 1). Patients with clinical N2 or N3 disease (matted nodes, internal mammary nodes, infraclavicular, or supraclavicular disease) are not candidates for this approach and will go on to receive ALND, thus no clip is placed. Patients who are appropriate candidates for neoadjuvant chemotherapy will undergo systemic therapy with interval clinical exams and ultrasound to assess response. After completion of neoadjuvant chemotherapy, a localization wire or I-125 radioactive seed is placed into the clipped node for intraoperative guidance. The operative approach to the axilla includes SLN dissection using dual tracer intraoperative lymphatic mapping, excision of the clipped node (via localization) followed by completion axillary dissection. Excision of the clipped node is confirmed by specimen radiograph (Fig. 2). The intent is to determine the correlation between the SLN and the clipped node as well as the false negative rate using a targeted approach removing the node known to harbor malignancy in addition to SLN dissection.
Axillary ultrasound of a patient with a right multifocal invasive ductal carcinoma and ipsilateral axillary lymphadenopathy at presentation and after neoadjuvant chemotherapy; a abnormal appearing axillary lymph node measuring 2.6 × 2.3 × 2.1 cm3, b fine-needle aspiration and placement of marker clip into suspicious node, c mammogram confirming clip in axillary node and clips in right breast marking the multifocal breast cancer, d interval response to therapy in the clipped node measuring 1.8 × 0.6 × 0.5 cm3
Conclusion
Approximately 40 % of breast cancer patients with clinically node-positive disease will achieve an axillary pCR with neoadjuvant chemotherapy and may be spared the morbidity of axillary dissection. Although the current standard practice in this clinical scenario remains axillary dissection, there may be selective patients who would be acceptable candidates for SLN surgery after neoadjuvant chemotherapy—those with clinical N1 disease and a high likelihood for pCR. Technique is also important with the use of dual tracer lymphatic mapping and removal of all SLNs improving the accuracy of the procedure. Placement of a clip at initial biopsy and use of IHC to evaluate the SLNs after chemotherapy have been reported to lower the false negative rates with SLN surgery. Patients who are not candidates include those with poor response to neoadjuvant chemotherapy, clinical N2 or N3 disease, or an inadequate number of SLNs identified at surgery. Ongoing trials are investigating the role of radiation therapy in addressing residual nodal disease and targeted excision of the positive node in addition to SLN dissection for axillary staging.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Krag DN, Anderson SJ, Julian TB, et al. Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node- negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol. 2010;11(10):927–33.
Ashikaga T, Krag DN, Land SR, et al. Morbidity results from the NSABP B-32 trial comparing sentinel lymph node dissection versus axillary dissection. J Surg Oncol. 2010;102(2):111–8.
• Giuliano AE, Hunt KK, Ballman KV, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA 2011;305(6):569–75. Practice changing trial finding no survival advantage to completion axillary dissection for women with early stage breast cancer and 1–2 positive SLNs treated with breast conserving therapy.
Giuliano AE, McCall L, Beitsch P, et al. Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons Oncology Group Z0011 randomized trial. Ann Surg. 2010;252(3):426–32; discussion 32–3.
Rastogi P, Anderson SJ, Bear HD, et al. Preoperative chemotherapy: updates of national surgical adjuvant breast and bowel project protocols B-18 and B-27. J Clin Oncol. 2008;26(5):778–85.
Hunt KK, Yi M, Mittendorf EA, et al. Sentinel lymph node surgery after neoadjuvant chemotherapy is accurate and reduces the need for axillary dissection in breast cancer patients. Ann Surg. 2009;250(4):558–66.
Xing Y, Foy M, Cox DD, Kuerer HM, Hunt KK, Cormier JN. Meta-analysis of sentinel lymph node biopsy after preoperative chemotherapy in patients with breast cancer. Br J Surg. 2006;93(5):539–46.
Kelly AM, Dwamena B, Cronin P, Carlos RC. Breast cancer sentinel node identification and classification after neoadjuvant chemotherapy—systematic review and meta analysis. Acad Radiol. 2009;16(5):551–63.
van Deurzen CH, Vriens BE, Tjan-Heijnen VC, et al. Accuracy of sentinel node biopsy after neoadjuvant chemotherapy in breast cancer patients: a systematic review. Eur J Cancer. 2009;45(18):3124–30.
Newman EA, Sabel MS, Nees AV, et al. Sentinel lymph node biopsy performed after neoadjuvant chemotherapy is accurate in patients with documented node-positive breast cancer at presentation. Ann Surg Oncol. 2007;14(10):2946–52.
Alvarado R, Yi M, Le-Petross H, et al. The role for sentinel lymph node dissection after neoadjuvant chemotherapy in patients who present with node-positive breast cancer. Ann Surg Oncol. 2012;19(10):3177–84.
Lee HD, Ahn SG, Lee SA, Lee HM, Jeong J. Prospective evaluation of the feasibility of sentinel lymph node biopsy in breast cancer patients with negative axillary conversion after neoadjuvant chemotherapy. Cancer Res Treat. 2015;47(1):26–33.
Shen J, Gilcrease MZ, Babiera GV, et al. Feasibility and accuracy of sentinel lymph node biopsy after preoperative chemotherapy in breast cancer patients with documented axillary metastases. Cancer. 2007;109(7):1255–63.
Park S, Park JM, Cho JH, Park HS, Kim SI, Park BW. Sentinel lymph node biopsy after neoadjuvant chemotherapy in patients with cytologically proven node- positive breast cancer at diagnosis. Ann Surg Oncol. 2013;20(9):2858–65.
Classe JM, Bordes V, Campion L, et al. Sentinel lymph node biopsy after neoadjuvant chemotherapy for advanced breast cancer: results of Ganglion Sentinelle et Chimiotherapie Neoadjuvante, a French prospective multicentric study. J Clin Oncol. 2009;27(5):726–32.
Yagata H, Yamauchi H, Tsugawa K, et al. Sentinel node biopsy after neoadjuvant chemotherapy in cytologically proven node-positive breast cancer. Clin Breast Cancer. 2013;13(6):471–7.
Mamounas EP, Brown A, Anderson S, et al. Sentinel node biopsy after neoadjuvant chemotherapy in breast cancer: results from National Surgical Adjuvant Breast and Bowel Project Protocol B-27. J Clin Oncol. 2005;23(12):2694–702.
•• Boughey JC, Suman VJ, Mittendorf EA, et al. Sentinel lymph node surgery after neoadjuvant chemotherapy in patients with node-positive breast cancer: the ACOSOG Z1071 (Alliance) clinical trial. Jama 2013;310(14):1455–61. Trial evaluating the feasibility and accuracy of sentinel lymph node surgery in breast cancer patients with clinically node positive disease treated with neoadjuvant chemotherapy. This study reported an overall false negative rate of 12.6%, however identified several techniques which improved procedural accuracy.
•• Kuehn T, Bauerfeind I, Fehm T, et al. Sentinel-lymph-node biopsy in patients with breast cancer before and after neoadjuvant chemotherapy (SENTINA): a prospective, multicentre cohort study. Lancet Oncol .2013;14(7):609–18. Trial evaluating the timing and accuracy of sentinel lymph node surgery in the setting of neoadjuvant chemotherapy. This study included four treatment arms one of which evaluated the role of sentinel lymph node surgery in patients who converted from clinically node positive to clinically node negative after neoadjuvant chemotherapy. The overall false negative rate in this group was 14.3%.
•• Boileau JF, Poirier B, Basik M, et al. Sentinel node biopsy after neoadjuvant chemotherapy in biopsy-proven node-positive breast cancer: the SN FNAC study. J Clin Oncol. 2015;33(3):258–64. Trial evaluating the feasibility and accuracy of sentinel lymph node surgery after neoadjuvant chemotherapy in node positive breast cancer. The overall false negative rate was 13.3% and improved to 8.4% with the addition of immunohistochemistry to determine sentinel lymph node status.
Boughey J, Suman V, Mittendorf E, et al. Abstract S2-1: the role of sentinel lymph node surgery in patients presenting with node positive breast cancer (T0-T4, N1-2) who receive neoadjuvant chemotherapy—results from the ACOSOG Z1071 trial. Cancer Res. 2012;72(24 Supplement):S2-1.
Boughey JC, Ballman KV, Symmans WF, et al. Methods impacting the false negative rate of sentinel lymph node surgery in patients presenting with node positive breast cancer (T0-T4,N1-2) who receive neoadjuvant chemotherapy—Results from a prospective trial—ACOSOG Z1071 (Alliance). Meeting abstract P2-01-02, San Antonio Breast Cancer Symposium 2014.
Choy N, Lipson J, Porter C, et al. Initial results with preoperative tattooing of biopsied axillary lymph nodes and correlation to sentinel lymph nodes in breast cancer patients. Ann Surg Oncol. 2015;22(2):377–82.
National Comprehensive Cancer Network. Breast Cancer (Version 3.2014). 2014. http://www.nccn.org/professionals/physician_gls/pdf/breast.pdf.
• Fu JF, Chen HL, Yang J, Yi CH, Zheng S. Feasibility and accuracy of sentinel lymph node biopsy in clinically node-positive breast cancer after neoadjuvant chemotherapy: a meta-analysis. PloS One 2014;9(9):e105316. Meta-analysis reviewing the literature regarding sentinel lymph node surgery after neoadjuvant chemotherapy in clinically node-positive breast cancer.
Boughey JC, Ballman KV, Hunt KK, et al. Axillary ultrasound after neoadjuvant chemotherapy and its impact on sentinel lymph node surgery: results from the American College of Surgeons Oncology Group Z1071 Trial (Alliance). J Clin Oncol. 2015. doi:10.1200/JCO.2014.57.8401.
Houssami N, Macaskill P, von Minckwitz G, Marinovich ML, Mamounas E. Meta-analysis of the association of breast cancer subtype and pathologic complete response to neoadjuvant chemotherapy. Eur J Cancer. 2012;48(18):3342–54.
Dominici LS, Negron Gonzalez VM, Buzdar AU, et al. Cytologically proven axillary lymph node metastases are eradicated in patients receiving preoperative chemotherapy with concurrent trastuzumab for HER2-positive breast cancer. Cancer. 2010;116(12):2884–9.
Boughey JC, McCall LM, Ballman KV, et al. Tumor biology correlates with rates of breast-conserving surgery and pathologic complete response after neoadjuvant chemotherapy for breast cancer: findings from the ACOSOG Z1071 (Alliance) Prospective Multicenter Clinical Trial. Ann Surg. 2014;260(4):608–14 discussion 14–6.
Schlembach PJ, Buchholz TA, Ross MI, et al. Relationship of sentinel and axillary level I-II lymph nodes to tangential fields used in breast irradiation. Int J Radiat Oncol Biol Phys. 2001;51(3):671–8.
Haffty BG, Hunt KK, Harris JR, Buchholz TA. Positive sentinel nodes without axillary dissection: implications for the radiation oncologist. J Clin Oncol. 2011;29(34):4479–81.
Donker M, van Tienhoven G, Straver ME, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol. 2014;15(12):1303–10.
Comparison of axillary lymph node dissection with axillary radiation for patients with node-positive breast cancer treated with chemotherapy. 2014. https://clinicaltrials.gov/ct2/show/NCT01901094.
Standard or comprehensive radiation therapy in treating patients with early-stage breast cancer previously treated with chemotherapy and surgery. 2014. https://clinicaltrials.gov/ct2/show/NCT01872975.
• Caudle AS, Yang WT, Mittendorf EA, et al. Selective surgical localization of axillary lymph nodes containing metastases in patients with breast cancer: a prospective feasibility trial. JAMA Surg. 2015;150(2):137–43. Trial describing the feasibility of targeted removal of known axillary metastasis in addition to sentinel lymph nodes in patients with node positive breast cancer treated with neoadjuvant chemotherapy.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Breast Cancer Surgery.
Rights and permissions
About this article
Cite this article
Teshome, M., Hunt, K.K. Sentinel Node Biopsy After Neoadjuvant Chemotherapy in Initial Node-Positive Patients: Why or Why Not?. Curr Surg Rep 3, 12 (2015). https://doi.org/10.1007/s40137-015-0089-y
Published:
DOI: https://doi.org/10.1007/s40137-015-0089-y