Abstract
Purpose of Review
The purpose of this review is to convey to the reader the most recent literature on the association between human papillomavirus (HPV) and sinonasal malignancies.
Recent Findings
In recent years, HPV has been recognized as an etiological factor in sinonasal squamous cell carcinomas (SN-SCCs). Studies find that 28% of SN-SCCs are HPV positive, mostly HPV-16 and -18. Inverted papillomas (IPs), sinonasal benign epithelial neoplasms, have also been associated with HPV and by extension malignant transformation to SCC. Despite repeated detection of HPV in IPs, the association remains controversial. Furthermore, a new unique histological tumor type, HPV-related multiphenotypic sinonasal carcinoma, has been described. Studies indicate that HPV-positive sinonasal malignancies have a decreased mortality compared to HPV-negative tumors, much like other head and neck carcinomas.
Summary
A significant proportion of sinonasal malignancies are caused by HPV. Several subtypes have been found, but further studies on clinical outcome are needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sinonasal malignancies are rare, accounting for < 1% of all malignant tumors and approximately 3 − 5% of all head and neck cancers [1]. Most sinonasal cancers have an epithelial histology, with squamous cell carcinoma (SCC) being the most common. As in SCC of other sites in the head and neck, human papillomavirus (HPV) is a recognized etiological factor [2, 3].
In general, HPV-related tumors are a distinct entity, and the carcinogenic effect of HPV infection on a molecular level has been thoroughly investigated. Even though the molecular patterns in HPV-infected cells that undergo malignant transformation are the same, the pathological and clinical behavior varies from subsite to subsite [4].
Because of the rarity of sinonasal malignancies, the epidemiology, clinical and pathological presentation, overall survival, and treatment outcomes are not completely understood. The purpose of this review is to summarize the current knowledge on HPV-related sinonasal malignancies and present recent discoveries. This review will primarily be based on studies published in 2017 and after, though some classical work on the subject will be included.
The sinonasal space is comprised of the nasal cavity with four paired paranasal sinuses connected via openings to the nasal cavity. The nasal cavity extends from the nasal vestibule to the choana through which it communicates with the nasopharynx. It is the most cephalic part of the upper respiratory tract, and the surface is covered with ciliated pseudostratified epithelium with a secretory component.
Benign Sinonasal Papillomas: The Association to HPV Infection and Malignant Transformation
Sinonasal papilloma is a common benign epithelial neoplasm. It is morphologically classified into three distinct subtypes: exophytic (everted) squamous cell papilloma, inverted papilloma, and oncocytic papilloma. Histologically, sinonasal papillomas are mostly covered by non-keratinized epithelium and display some degree of stromal inflammation, which has been suspected to play a role in the initiation and formation of neoplastic growth [5]. Papillomas often recur, but inverted and oncocytic papillomas are especially prone to undergo malignant transformation; this very rarely happens in exophytic papillomas, which in contrast to the two other types most often are multicentric [6].
Inverted papillomas are the most prevalent subtype, with an annual prevalence of 0.2 − 1.5 cases per 100,000 persons [7•]. Inverted papillomas primarily arise in the lateral nasal wall and can extend into the paranasal sinuses. They exhibit aggressive local growth and a high rate of recurrence of up to 34% [7•]. Lesions can consist of cells with different grades of metaplasia and/or dysplasia, and transformation to SCC has been shown to occur in about 10% of cases [8, 9].
It is estimated that approximately one-third of the papillomas harbor HPV-DNA [6]. The prevalence varies in studies and is 60 − 100% in the exophytic papillomas and 10 − 40% in inverted papillomas. Almost none of the oncocytic papillomas are HPV positive [6, 10, 11]. HPV is suspected to be involved in the pathogenesis of both initiation of papilloma formation and the subsequent malignant transformation [6, 10, 11]. However, there is a lack of extensive homogeneous studies to establish this association, which is why it remains controversial [5].
Sinonasal Squamous Cell Carcinomas
Malignant sinonasal tumors are a histologically diverse group. The most common epithelial types are SCC (60 − 75%), followed by adenocarcinoma (15%), and adenoid cystic carcinoma (10%) [12]. The sinonasal space has the smallest fraction of SCCs in the entire head and neck area. This may be due to many functions of the sinonasal membrane, potentially giving rise to a wider array of neoplasms. Apart from a few extremely rare subtypes, SCCs can be further subdivided by histopathology into keratinizing type, non-keratinizing type, basaloid type, and papillary type. The keratinizing-type SCC (K-SCC) is the most common in the sinonasal space, which is comparable to rates seen in the rest of the upper aerodigestive tract. K-SCC comprise 35 − 50% of the SCCs, while the non-keratinizing-type SCC (NK-SCC) accounts for 15 − 25% [13].
SN-SCC has a 2:1 male predominance, and more than 80% of the patients are older than 55 at the time of diagnosis [13]. Exposure to industrial compounds such as welding fumes, organic solvents, and leather dust has been associated with the development of SN-SCC [14]. The oncogenic mechanism is not fully understood, but it is suspected to be a matter of geno- and/or immunotoxicity. Smoking has also been associated with the risk of developing SN-SCC but has not been found to be as significant driver of carcinogenesis as in other head and neck subsites [13].
The maxillary sinus is the most common affected site (60%), followed by the nasal cavity (25%), and ethmoid sinus (10 − 15%). SN-SCC is rarely found in the frontal and sphenoid sinuses (1 − 2%) [13]. Sinonasal tumors present with unspecific symptoms, e.g., nasal discharge, obstruction or congestion, epistaxis, facial pain, and/or headache. Tumors located in the nasal cavity will often present at an earlier stage due to more obvious symptoms, while paranasal sinus tumors usually exhibit more insidious symptoms, leading to diagnostic delay [15].
In a retrospective study on 537 patients from the American National Cancer Database, Al-Qurayishi et al. found that 33% of patients had T1/T2, while 32% had T3/T4 tumors at the time of diagnosis. Close to 30% of all tumors had nodal involvement; only a few presented with distant metastases [16••]. For staging purposes, SN-SCCs are divided into maxillary sinus tumors and nasoethmoidal tumors. In a study by Ahn et al., the authors found that among 1283 patients from the Surveillance, Epidemiology, and End Results (SEER) database, about 20% of maxillary sinus tumors had nodal involvement at the time of diagnosis compared to about 10% of nasal cavity tumors [17]. This is probably due to the advanced T stage of maxillary tumors and local differences in the drainage pattern of sinonasal compartments, both associated with a poorer prognosis [18]. In a small single-center study on 47 patients with SN-SCC of the nasoethmoidal complex, Janik et al. found that septal and ethmoid tumors more frequently presented as advanced-stage disease. Moreover, lymph node metastases were more prevalent in septal tumors, presumably leading to a worse prognosis [19]. Similar studies on sphenoid and frontal sinus tumors are scarce due to the rarity of these tumors.
Human Papillomavirus
Human papillomavirus (HPV) is a double-stranded DNA virus belonging to a family of more than 200 subtypes (Papillomaviridae) [20]. The virus is known to infect the keratinocytes of epithelial surface cells, and it is the most common sexually transmitted infection worldwide [20].
Infection with low-risk HPV subtypes (e.g., HPV 6, 11, 42, 54, 57, 83) causes benign hyperproliferative lesions as condylomata acuminate, verruca vulgaris, recurrent respiratory papillomas, and probably also exophytic papillomas [21].
For five decades, HPV has been known to be associated with the development of carcinomas. In the early 1980s, two high-risk subtypes, HPV-16 and HPV-18, were isolated in cervical cancer [22]. Today, several high-risk HPV subtypes (e.g., 16, 18, 31, 33, 35, 45, 51, 52, 56, 58, 59) have been identified, though HPV-16 and -18 are still the most prevalent and have the greatest malignant potential. Moreover, recent studies have estimated that approximately 5% of all cancers worldwide are caused by HPV infection [23].
Carcinogenesis
HPV integrates in the host-cell DNA causing alterations in the genome and transcription of proteins. To date, the viral oncogenes E6 and E7 are the most studied. They are overexpressed in cells infected with high-risk HPV and contribute to all six main phenotypic alterations of cancer cells, known as the “hallmarks of cancer” [24•]. Through several mechanisms, they induce carcinogenesis by dysregulation of the cell cycle. E6 inactivates p53, a tumor suppressor that under normal circumstances regulates the cell cycle. E6 induces ubiquitination of p53 which leads to deregulation of the effect of p53 on the cell cycle. Under normal circumstances, p53 would halt cells with damaged DNA at the G1/S regulation point and initiate apoptosis if the damage is irreparable. The second oncoprotein, E7, inhibits the tumor suppressor Rb (retinoblastoma) by phosphorylation. When Rb is inactivated, the transcription factor E2F is translocated into the nucleus, where it interacts with the cell cycle, resulting in cell proliferation [25]. Furthermore, these oncogenes lead to the transcription and overexpression of T-cell-regulating ligands (e.g., PDL1) which allow for immune evasion in HPV-infected cells [26].
In general, malignant neoplasms are often characterized by expression of genes that control cell motility, angiogenesis, and epithelial-mesenchymal transition, leading to an aggressive clinical behavior. Conversely, HPV-induced malignancies predominantly express genes that mediate changes in genes involved in proliferation, making the clinical behavior less aggressive [25].
Detection of HPV
HPV-DNA can be detected in paraffin-embedded tissues either via polymerase chain reaction (PCR), a reproducible and precise technique, or by in situ hybridization (ISH) where virus is directly visualized in the tumor cells, eliminating the risk of false-positive test results from contamination. However, detecting HPV-DNA does not distinguish between latent infection and carcinogenic transcriptionally active infection.
The golden standard for HPV diagnostics is the detection of the HPV oncogenes E6 and E7 mRNA by reverse transcriptase PCR (RT-PCR) or ISH showing excellent sensitivity and specificity, albeit RT-PCR requires fresh-frozen specimens and mRNA deteriorates quickly [27, 28].
In oropharyngeal SCC (OP-SCC), it is recommended to routinely screen for p16 by immunohistochemistry (IHC) as a surrogate marker for infection with transcriptionally active HPV. p16 is a tumor-suppressor protein that is often, but not exclusively, overexpressed in HPV-infected cells because of the degradation of Rb by E7. In SN-SCCs, numerous studies have investigated the role of p16 as a surrogate marker for active HPV infection. However, results diverge both in regards to sensitivity and specificity, resulting in the exclusion of p16 in routine diagnostic in SN-SCC [29, 30•, 31]. Therefore, a combination of approaches remains the preferred detection method in SN-SCC [29, 30•, 31].
The Role of Human Papillomavirus in Sinonasal Malignancies
In 1989, Klemi et al. published the first study proving the presence of HPV in sinonasal papillomas and the virus’ association to malignant transformation to SCC [32]. Subsequently, several studies have detected HPV in de novo and ex-papilloma SN-SCC. So much so, that in 2017, HPV-related sinonasal carcinoma was added to the chapter about tumors in the nasal cavity, paranasal sinuses, and skull base in the updated version of the WHO Classification of Head and Neck Tumors [33].
Studies published after 2017 report very different rates of HPV positivity in SN-SCC, ranging from 20 to 60% [31, 34]. Because of the rarity of sinonasal cancers, studies are generally small, retrospective, single center, and very heterogenous regarding detection methods. In a recent systematic review including 2025 patients, Sjöstedt et al. found HPV positivity in 28% of all SN-SCCs [35••].
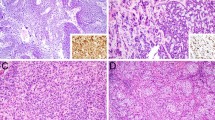
In SN-SCC, HPV-16 is the prevailing subtype, followed by HPV-18, -31, and -33, either alone or in combination with other HPV subtypes [31, 34, 36, 37]. This is comparable to HPV-related tumors of other areas of the head and neck [11]. Beside the most common subtypes, some studies have detected rarer subtypes including, e.g., HPV-39, -45, -56, and -82 (Fig. 1) [34, 37]. Most studies have found HPV-positive SN-SCC to be of non-keratinizing, papillary, or basaloid histology [30•, 36, 38].
Schematic figure of the different HPV subtypes and the mucosal neoplasms they cause. The nasal cavity and paranasal sinuses comprise the sinonasal space where a variety of benign and malignant HPV-positive neoplasms are found. Compared to the HPV-positive neoplasms in the oropharynx and larynx, a wider range of different HPV-related neoplasms and subtypes have been detected in the sinonasal space. LR-HPV, low-risk HPV. HR-HPV, high-risk HPV. HMSC, HPV-related multiphenotypic sinonasal carcinoma. Created with BioRender.com
Patients with HPV-positive SN-SCC are slightly younger than their HPV-negative counterparts [29, 30•, 36, 38]. HPV-positive SN-SCC is evenly distributed between men and women. In contrast, men are twice as likely as women to get HPV-negative SN-SCC [29, 30•, 36,37,38]. Male predominance is also found in HPV-positive OP-SCC [39], emphasizing that HPV-induced SCC is a distinct entity that behaves uniquely according to location and biological and behavioral differences between the sexes.
The most frequent location among HPV-positive SN-SCCs is the nasal cavity (49%) followed by the maxillary (18.8%) and ethmoid sinus (18.8%) [38]. HPV-related SN-SCC in the frontal or sphenoid sinus is equally rare [38, 40]. Compared to HPV-negative SN-SCC, the HPV-positive tumors are generally high-grade and low T stage [31, 36]. Furthermore, in contrast to HPV-related OP-SCC where a high rate of lymph node involvement is found (88%) [41], HPV-positive and -negative SN-SCC exhibit a low rate (< 20%) [30•, 36].
HPV Infection and Malignant Transformation of Inverted Papillomas
Inverted papillomas (IPs) exhibit different degrees of dysplasia and are in the literature usually stratified into nonmalignant, dysplastic, and malignant IPs. Histologically, IPs are characterized by metaplastic squamous cells scattered in the normal respiratory mucosa [42, 43]. Dysplastic and ultimately malignant transformation leads to SN-SCC, most commonly of NK type [44, 45]. The pathogenesis of IP formation and malignant transformation is not fully understood. However, infection with HPV has been suggested to be involved [5].
About 25% of all IPs contain HPV-DNA, a prevalence much higher than that found in nasal polyps (4%) and normal-appearing nasal mucosa (7%) [6, 46, 47•]. Stratified by histopathology, 20% of nonmalignant IPs, 53% of dysplastic IPs, and 24% of malignant IPs are HPV positive [47•]. Several different HPV subtypes have been detected in all histopathological subtypes. HPV-16 and HPV-18 are the prevailing high-risk subtypes associated with an odds ratio for malignant transformation of 8.5 and 23, respectively [7•]. The most frequently occurring low-risk subtypes were HPV-6 and HPV-11, which were not associated with an increased risk of malignant transformation [7•]. Furthermore, a range of rarer subtypes have been detected in both nonmalignant and malignant IPs such as low-risk HPV 42, 54, 57, and 83 and high-risk HPV 39, 51, 52, 56, 58, and 59 [47•]; see Fig. 1.
The association between malignant transformation of IPs and HPV infection has been contested. EGFR mutations have been found in 88% of IPs and 77% of IPs associated with SN-SCC but in none of the SN-SCCs without prior IP. Due to this association, the authors suggest that EGFR mutations are the driving factor for the formation and malignant transformation of IPs [30•, 48, 49]. Furthermore, they do not find EGFR mutations in any of the HPV-positive IPs, indicating that these are two distinct carcinogenic mechanisms that are mutually exclusive [48]. This led the authors to conclude that, based on their findings, HPV is not involved in the malignant transformation of IPs. This is in stark contrast to the bulk of studies emphasizing the role of HPV infection in the formation and malignant transformation of IPs [6, 7•, 46, 47•].
HPV-Related Multiphenotypic Sinonasal Carcinoma
Recently, a new and distinct entity of HPV-related sinonasal carcinoma has been described. It exhibits a wide range of histological features and was therefore named HPV-related multiphenotypic sinonasal carcinoma (HMSC) [50•]. The majority of HMSCs are positive for HPV subtype 33, while the remaining are positive for HPV-16, -35, and -56 [50•] (Fig. 1). All of the examined tumors to date have shown a strong and diffuse p16 positivity.
Contrary to the HPV-related SN-SCC which predominantly resides in the nasal cavity, HMSC is mostly found in the maxillary sinus. The gender distribution is nearly equal between men and women, and the mean age is 54, ranging from 28 to 90 [51]. Most patients present with early-stage disease (T1/T2), and none of the patients has regional lymph node involvement.
More than one-third of all patients have recurrence despite combination treatment with surgery and radiation, though radiotherapy seems to shorten the recurrence interval. To date, no deaths have been registered due to HMSC, but long-term follow-up data is sparse [50•, 51].
Treatment and Prognosis
Regardless of HPV status, if the SN-SCC is resectable, the primary treatment should be surgery, as this carries less morbidity when compared to radiotherapy with or without chemotherapy. In cases of distant metastasis, surgery may still be indicated in instances of tumor bleeding and risk of acute vision loss due to optic-nerve compression. Survival is improved if the tumor is completely removed with negative margins [52]. If possible, endoscopic surgery is equal to an open approach but less invasive, resulting in a shorter postoperative rehabilitation time, and less risk of esthetic consequences and postoperative complications [53], thereby shortening the time to postoperative radiotherapy [54]. In seldom cases when there is extensive invasion of the brain, orbit, cutaneous tissue, or indication for maxillectomy, external approaches are necessary. In most cases, monotreatment with endoscopic resection is possible. Elective neck dissection of T3/T4 tumors without lymph node metastases has been proposed to lower the risk of locoregional recurrence, but evidence is lacking [55].
Patients presenting with advanced disease will often require a multimodal treatment comprised of surgery in combination with radiotherapy, as multimodal treatment has been shown to improve local control and overall survival [56]. The 5-year overall survival for all SN-SCCs is around 50 − 60%. Unfortunately, SN-SCC recurs in 20 − 30% of cases, making it necessary for patients to receive salvage treatment, which leads to higher morbidity rates [57].
Chemotherapy is a possible addition to the aforementioned treatment regimens, either as adjuvant or neoadjuvant therapy. Retrospective studies have shown that induction therapy might raise the chance of complete resection with negative margins, reducing the risk of regional and distant metastases and improving the prognosis [58]. Larger randomized controlled trials are needed to fully establish chemotherapy’s efficacy and safety in treating SN-SCC.
Recent trials on the potential use of immune checkpoint inhibitors (pembrolizumab, nivolumab) for the treatment of head and neck SCC (HNSCC) report improved median survival time and fewer treatment-related adverse events compared to standard treatment [59, 60]. Immunotherapy may be a new and promising treatment, and numerous clinical trials investigating a multitude of different immunotherapeutic targets are underway. In 2021, a systematic review on the use of immunotherapy for HNSCC found as many as 67 ongoing trials [26].
HPV-positive HNSCCs have been found to be more sensitive to radio-, chemo-, and immunotherapy compared to HPV-negative HNSCCs [26, 61]. This has not been shown for the HPV-positive SN-SCCs specifically, though these results are presumably applicable for this subtype as well. The improved treatment response is partly explained by the fact that HPV-negative and HPV-positive SCCs are distinct tumor subtypes that exhibit different genomic and immunologic features [62].
The HPV-positive tumors depend on the host cell’s transcriptional machinery to produce the oncogenes E6 and E7, which are key factors for maintaining the malignant phenotype. Therefore, E6 and E7 have been suggested as specific therapeutic targets. In vitro research shows that inhibiting E6 leads to apoptosis as the function of p53 is reestablished [24•]. However, since E7 is capable of inducing carcinogenesis on its own, inhibition of the common E6/E7 transcriptional promotor region or destruction of the E6/E7 transcripts with interfering RNA seems like more promising options. However, these therapeutic strategies are challenged by the fact that hypoxic conditions in subregions of cancers induce metabolic reprogramming, cancer progression, and therapeutic resistance in in vivo models [62]. Research to overcome these challenges is in progress and may lead to new therapeutic options in HPV-positive SCC in the future.
The incidence of SN-SCC has decreased over the last decades. Nonetheless, overall survival rates remain poor. This is especially true for those with local or distant metastases or locally advanced disease [63]. Conversely, with a survival rate of 67.7% in HPV-positive and 47.6% in HPV-negative SN-SCCs, a recent major meta-analysis cemented that HPV positivity is also a favorable prognostic factor in SN-SCC [64].
Daisuke et al. compared HPV-positive SN-SCCs to EGFR-mutated or EGFR-wild-type HPV-negative SN-SCCs. The 5-year overall survival was 100% in HPV-positive, 47.7% in EGFR-mutated, and 62.1% in EGFR-wild-type HPV-negative cases [40]. HPV-positive SN-SCC yielded the best prognosis, while EGFR-mutated tumors had the worst prognosis. This indicated that the behavior of HPV-related SN-SCCs is less aggressive compared to tumors with a different genotype [40].p16 positivity is correlated to a better prognosis in OP-SCC, even in HPV-negative tumors [65]. This has not been shown for the HPV-related SN-SCCs. In contrast to OP-SCC, where HPV-positive tumors are downstaged, no distinction is made for HPV-negative and HPV-positive SN-SCCs [66]. As SN-SCC are rare, no single center will have sufficient numbers to address the association between improved survival in HPV-positive SN-SCC. Therefore, international collaborations with homogenous treatment regimens would be the ideal course of action for future research.
Conclusion
Sinonasal malignancies are rare and heterogenous. SCC accounts for 60 − 75% of all epithelial sinonasal cancers. HPV is found to play a role in a subgroup of factor SN-SCC. About 28% of SN-SCCs are HPV positive, most frequently HPV-16, though a wide variety of subtypes have been described. HPV-related multiphenotypic sinonasal carcinoma is associated with other subtypes as HPV-33, -35, and -56. Furthermore, HPV has also been suspected to be implicated in the formation and malignant transformation of IPs because of the repeated detection of HPV subtypes in these benign sinonasal neoplasms; however, the association remains controversial. The main treatment of SN-SCC is surgery, which can be combined with radiotherapy in advanced cases for improved local control and survival. Studies indicate that there is an improved overall survival rate for the HPV-positive tumors, but this association needs further investigation to be fully validated. Immunotherapy may provide further treatment options in the future. Furthermore, treatments focusing on intracellular pathways connected to HPV infection may also provide a highly specific treatment option with a low toxicity.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ansa B, Goodman M, Ward K, Kono SA, Owonikoko TK, Higgins K, et al. Paranasal sinus squamous cell carcinoma incidence and survival based on Surveillance, Epidemiology, and End Results data, 1973 to 2009: paranasal SCC SEER analysis. Cancer. 2013;119:2602–10. https://doi.org/10.1002/cncr.28108.
Sjöstedt S, Jensen DH, Jakobsen KK, Grønhøj C, Geneser C, Karnov K, et al. Incidence and survival in sinonasal carcinoma: a Danish population-based, nationwide study from 1980 to 2014. Acta Oncol. 2018;57:1152–8. https://doi.org/10.1080/0284186X.2018.1454603.
Youlden DR, Cramb SM, Peters S, Porceddu SV, Møller H, Fritschi L, et al. International comparisons of the incidence and mortality of sinonasal cancer. Cancer Epidemiol. 2013;37:770–9. https://doi.org/10.1016/j.canep.2013.09.014.
Paver EC, Currie AM, Gupta R, Dahlstrom JE. Human papilloma virus related squamous cell carcinomas of the head and neck: diagnosis, clinical implications and detection of HPV. Pathology (Phila). 2020;52:179–91. https://doi.org/10.1016/j.pathol.2019.10.008.
Wang M. Noel JE Etiology of sinonasal inverted papilloma: a narrative review. World J Otorhinolaryngol - Head Neck Surg. 2017;3:54–8. https://doi.org/10.1016/j.wjorl.2016.11.004.
Syrjänen K, Syrjänen S. Detection of human papillomavirus in sinonasal papillomas: systematic review and meta-analysis: HPV in sinonasal papillomas. Laryngoscope. 2013;123:181–92. https://doi.org/10.1002/lary.23688.
• Ding R, Sun Q, Wang Y. Association between human papilloma virus infection and malignant sinonasal inverted papilloma. Laryngoscope. 2021;131:1200–5. https://doi.org/10.1002/lary.29125. A systematic review and meta-analysis on the association between HPV infection and malignant transformation of inverted papillomas with emphasis on subtype.
Archang M, Chew L, Han AY-K, Sajed D, Vorasubin N, Wang M. Sinonasal papillomas: 10-year retrospective analysis of etiology, epidemiology, and recurrence. Am J Rhinol Allergy 2022;36:827–834. https://doi.org/10.1177/19458924221116441
Li W, Lu H, Zhang H, Sun X, Hu L, Wang D. Squamous cell carcinoma associated with inverted papilloma: recurrence and prognostic factors. Oncol Lett. 2019;19(1):1082–8. https://doi.org/10.3892/ol.2019.11185.
Kraft M, Simmen D, Casas R, Pfaltz M. Significance of human papillomavirus in sinonasal papillomas. J Laryngol Otol 2001;115:(9):709–14. https://doi.org/10.1258/0022215011908955
Beigh A, Rashi R, Junaid S, Khuroo MS, Farook S. Human papilloma virus (HPV) in sinonasal papillomas and squamous cell carcinomas: a PCR-based study of 60 cases. Gulf J Oncolog. 2018;1:37–42.
Mani N, Shah JP. Squamous cell carcinoma and its variants. Advances in oto-rhino-laryngology Adv Otorhinolaryngol. 2020;84:124–36. https://doi.org/10.1159/000457932.
Ferrari M, Taboni S, Carobbio ALC, Emanuelli E, Maroldi R, Bossi P, et al. Sinonasal squamous cell carcinoma, a narrative reappraisal of the current evidence. Cancers. 2021;13:2835. https://doi.org/10.3390/cancers13112835.
d’Errico A, Zajacova J, Cacciatore A, Alfonzo S, Beatrice F, Ricceri F, et al. Exposure to occupational hazards and risk of sinonasal epithelial cancer: results from an extended Italian case–control study. Occup Environ Med. 2021;78:323–9. https://doi.org/10.1136/oemed-2020-106738.
Nguyen ES, Risbud A, Birkenbeuel JL, Murphy LS, Goshtasbi K, Pang JC, et al. Prognostic factors and outcomes of de novo sinonasal squamous cell carcinoma: a systematic review and meta-analysis. Otolaryngol Neck Surg. 2022;166:434–43. https://doi.org/10.1177/01945998211021023.
•• Al-Qurayshi Z, Smith R, Walsh JE. Sinonasal squamous cell carcinoma presentation and outcome: a national perspective. Ann Otol Rhinol Laryngol. 2020;129:1049–55. https://doi.org/10.1177/0003489420929048. A large retrospective study of patients with sinonasal squamous cell carcinoma, histological type, stage at diagnoses and prevalence of HPV infection.
Ahn PH, Mitra N, Alonso-Basanta M, Palmer JN, Adappa ND, O’Malley BW Jr, et al. Risk of lymph node metastasis and recommendations for elective nodal treatment in squamous cell carcinoma of the nasal cavity and maxillary sinus: a SEER analysis. Acta Oncol. 2016;55:1107–14. https://doi.org/10.1080/0284186X.2016.1216656.
Liu Q, Qu Y, Wang K, Wu, R, Zhang Y, et al. Lymph node metastasis spread patterns and the effectiveness of phrophylactic neck irradiation in sinonasal squamous cell carcinoma (SNSCC). Front 30;12:793351 https://doi.org/10.3389/fonc.2022.793351
Janik S, Gramberger M, Kadletz L, Pammer J, Grasl MCh, Erovic BM. Impact of anatomic origin of primary squamous cell carcinomas of the nasal cavity and ethmoidal sinus on clinical outcome. Eur Arch Otorhinolaryngol. 2018;275:2363–71. https://doi.org/10.1007/s00405-018-5068-3.
Rosalik K, Tarney C, Han J. Human papilloma virus vaccination Viruses. 2021;13:1091. https://doi.org/10.3390/v13061091.
Egawa N, Doorbar J. The low-risk papillomaviruses. Virus Res. 2017;231:119–27. https://doi.org/10.1016/j.virusres.2016.12.017.
zur Hausen H. Papillomaviruses in the causation of human cancers — a brief historical account. Virology 2009;384:260–265. https://doi.org/10.1016/j.virol.2008.11.046
de Martel C, Plummer M, Vignat J, Franceschi S. Worldwide burden of cancer attributable to HPV by site, country and HPV type: worldwide burden of cancer attributable to HPV. Int J Cancer. 2017;141:664–70. https://doi.org/10.1002/ijc.30716.
• Hoppe-Seyler K, Bossler F, Braun JA, Herrmann AL, Hoppe-Seyler F. The HPV E6/E7 oncogenes: key factors for viral carcinogenesis and therapeutic targets. Trends Microbiol. 2018;26:158–68. https://doi.org/10.1016/j.tim.2017.07.007. A thorough review of the role of the oncogenes E6 and E7 in HPV-related malignancies with future perspectives on new treatment options.
Araldi RP, Sant’Ana TA, Módolo DG, de Melo TC, Spadacci-Morena DD, de Cassia Stocco R, et al. The human papillomavirus (HPV)-related cancer biology: an overview. Biomed Pharmacother 2018;106:1537–1556. https://doi.org/10.1016/j.biopha.2018.06.149.
Wang H, Zhao Q, Zhang Y, Zhang Q, Zheng z, Liu S, et al. Immunotherapy advances in locally advanced and recurrent/metastatic head and neck squamous cell carcinoma and its relationship with human papillomavirus. Front Immunol 2021;8:12:652054. https://doi.org/10.3389/fimmu.2021.652054.
Thompson LDR, Franchi A. New tumor entities in the 4th edition of the World Health Organization classification of head and neck tumors: nasal cavity, paranasal sinuses and skull base. Virchows Arch 2018;472:315–330. https://doi.org/10.1007/s00428-017-2116-0.
Bussu F, Ragin C, Boscolo-Rizzo P, Gallus R, Delogu G, et al. HPV as a marker for molecular characterization in head and neck oncology: looking for a standardization of clinical use and of detection method(s) in clinical practice. Head Neck. 2019;41:1104–11. https://doi.org/10.1002/hed.25591.
Cohen E, Coviello C, Menaker S, Martinez-Duarte E, Gomez C, Lo K, et al. P16 and human papillomavirus in sinonasal squamous cell carcinoma. Head Neck. 2020;42:2021–9. https://doi.org/10.1002/hed.26134.
• Jiromaru R, Yamamoto H, Yasumatsu R, Hongo T, Nozaki Y, Hashimoto K, et al. HPV-related sinonasal carcinoma: clinicopathologic features, diagnostic utility of p16 and Rb immunohistochemistry, and EGFR copy number alteration. Am J Surg Pathol. 2020;44:305–15. https://doi.org/10.1097/PAS.0000000000001410. A retrospective study of the prevalence and prognostic value of HPV infection and EGFR mutations in sinonasal squamous cell carcinomas.
Švajdler M, Němcova J, Dubinský P, Metelkova A, Švajdler P, Straka Ľ, et al. Significance of transcriptionally-active high-risk human papillomavirus in sinonasal squamous cell carcinoma: case series and a meta-analysis. Neoplasma. 2021;67:1456–63. https://doi.org/10.4149/neo_2020_200330N332.
Klemi PJ, Joensuu H, Siivonen L, Virolainen E, Syrjänen S, Syrjänen K. Association of DNA aneuploidy with human papillomavirus-induced malignant transformation of sinonasal transitional papillomas. Otolaryngol Neck Surg. 1989;100:563–7. https://doi.org/10.1177/019459988910000607.
El-Naggar AK, Chan JKC, Grandis Jr, Takta T, Slootweg PJ: Tumors of the nasal cavity, paranasal sinuses and skull base. In: WHO Classification of Tumors 4th Edition, Lyon: IARC Press. 2017.
Chowdhury N, Alvi S, Kimura K, Tawfik O, Manna P, Beahm D, et al. Outcomes of HPV-related nasal squamous cell carcinoma: outcomes of HPV+ nasal SCCa. Laryngoscope. 2017;127:1600–3. https://doi.org/10.1002/lary.26477.
•• Sjöstedt S, von Buchwald C, Agander TK, Aanaes K. Impact of human papillomavirus in sinonasal cancer—a systematic review. Acta Oncol. 2021;60:1175–91. https://doi.org/10.1080/0284186X.2021.1950922. A recent systematic review of the role of HPV in sinonasal cancer with occurrence, influence of HPV-positivity on prognosis and utility of p16 as a surrogate marker.
Oliver JR, Lieberman SM, Tam MM, Liu CZ, Li Z, Hu KS, et al. Human papillomavirus and survival of patients with sinonasal squamous cell carcinoma. Cancer. 2020;126:1413–23. https://doi.org/10.1002/cncr.32679.
Schlussel Markovic E, Marqueen KE, Sindhu KK, Lehrer EJ, Liu J, Miles B, et al. The prognostic significance of human papilloma virus in sinonasal squamous cell carcinoma. Laryngoscope Investig Otolaryngol. 2020;5:1070–8. https://doi.org/10.1002/lio2.468.
Kılıç S, Kılıç SS, Kim ES, Baredes S, Mahmoud O, Gray ST, et al. Significance of human papillomavirus positivity in sinonasal squamous cell carcinoma: HPV-positive SNSCC. Int Forum Allergy Rhinol. 2017;7:980–9. https://doi.org/10.1002/alr.21996.
Li H, Park HS, Osborn HA, Judson BL. Sex differences in patients with high risk HPV-associated and HPV negative oropharyngeal and oral cavity squamous cell carcinomas. Cancers Head Neck. 2018;3:4. https://doi.org/10.1186/s41199-018-0031-y.
Nishikawa D, Sasaki E, Suzuki H, Beppu S, Sawabe M, Terada H, et al. Treatment outcome and pattern of recurrence of sinonasal squamous cell carcinoma with EGFR-mutation and human papillomavirus. J Cranio-Maxillofac Surg. 2021;49:494–500. https://doi.org/10.1016/j.jcms.2021.02.016.
Bauwens L, Baltres A, Fiani D-J, Zrounba P, Buiret G, Fleury B, et al. Prevalence and distribution of cervical lymph node metastases in HPV-positive and HPV-negative oropharyngeal squamous cell carcinoma. Radiother Oncol. 2021;157:122–9. https://doi.org/10.1016/j.radonc.2021.01.028.
Syrjanen KJ. HPV infections in benign and malignant sinonasal lesions. J Clin Pathol. 2003;56:174–81. https://doi.org/10.1136/jcp.56.3.174.
Tong CCL, Palmer JN. Updates in the cause of sinonasal inverted papilloma and malignant transformation to squamous cell carcinoma. Curr Opin Otolaryngol Head Neck Surg. 2021;29:59–64. https://doi.org/10.1097/MOO.0000000000000692.
Yan CH, Newman JG, Kennedy DW, Palmer JN, Adappa ND. Clinical outcomes of sinonasal squamous cell carcinomas based on tumor etiology: sinonasal SCC outcomes based on etiology. Int Forum Allergy Rhinol. 2017;7:508–13. https://doi.org/10.1002/alr.21899.
Weindorf SC, Brown NA, McHugh JB, Udager AM. Sinonasal papillomas and carcinomas: a contemporary update with review of an emerging molecular classification. Arch Pathol Lab Med. 2019;143:1304–16. https://doi.org/10.5858/arpa.2019-0372-RA.
Sham CL, To KF, Chan PKS, Lee DLY, Tong MCF, van Hasselt CA. Prevalence of human papillomavirus, Epstein-Barr virus, p21, and p53 expression in sinonasal inverted papilloma, nasal polyp, and hypertrophied turbinate in Hong Kong patients. Head Neck. 2012;34:520–33. https://doi.org/10.1002/hed.21772.
• Gupta R, Rady PL, Sikora AG, Tyring SK. The role of human papillomavirus in the pathogenesis of sinonasal inverted papilloma: a narrative review. Rev Med Virol. 2021;31:e2178. https://doi.org/10.1002/rmv.2178. A narrative review of HPV infection and the association to formation and malignant transformation of inverted papillomas.
Udager AM, Rolland DCM, McHugh JB, Betz BL, Murga-Zamalloa C, Carey TE, et al. High-frequency targetable EGFR mutations in sinonasal squamous cell carcinomas arising from inverted sinonasal papilloma. Cancer Res. 2015;75:2600–6. https://doi.org/10.1158/0008-5472.CAN-15-0340.
Rooper LM, Bishop JA, Westra WH. Transcriptionally active high-risk human papillomavirus is not a common etiologic agent in the malignant transformation of inverted Schneiderian papillomas. Head Neck Pathol. 2017;11:346–53. https://doi.org/10.1007/s12105-017-0779-0.
• Bishop JA, Andreasen S, Hang J-F, Bullock MJ, Chen TY, Franchi A, et al. HPV-related multiphenotypic sinonasal carcinoma: an expanded series of 49 cases of the tumor formerly known as HPV-related carcinoma with adenoid cystic carcinoma-like features. Am J Surg Pathol. 2017;41:1690–701. https://doi.org/10.1097/PAS.0000000000000944. A description of 49 cases of a distinct HPV-related sinonasal tumor type, the clinical presentation, histological features and survival rate.
Ward ML, Kernig M, Willson TJ. HPV-related multiphenotypic sinonasal carcinoma: a case report and literature review. Laryngoscope. 2021;131:106–10. https://doi.org/10.1002/lary.28598.
Jafari A, Shen SA, Qualliotine JR, Orosco RK, Califano JA, DeConde AS. Impact of margin status on survival after surgery for sinonasal squamous cell carcinoma. Int Forum Allergy Rhinol. 2019;9:1205–11. https://doi.org/10.1002/alr.22415.
Simon C, Nicolai P, Paderno A, Dietz A. Best practice in surgical treatment of malignant head and neck tumors. Front Oncol. 2020;10:140. https://doi.org/10.3389/fonc.2020.00140.
Xiao R, Joshi RR, Husain Q, Cracchiolo JR, Lee N, Tsai J, et al. Timing of surgery and adjuvant radiation therapy for sinonasal malignancies: effect of surgical approach. Head Neck. 2019;41:3551–63. https://doi.org/10.1002/hed.25873.
Crawford KL, Jafari A, Qualliotine JR, Stuart E, DeConde AS, Califano JA, et al. Elective neck dissection for T3 / T4 cN0 sinonasal squamous cell carcinoma. Head Neck. 2020;42:3655–62. https://doi.org/10.1002/hed.26418.
Farrell NF, Mace JC, Detwiller KY, Li R, Andersen PE, Smith TL, et al. Predictors of survival outcomes in sinonasal squamous cell carcinoma: an analysis of the National Cancer Database. Int Forum Allergy Rhinol. 2021;11:1001–11. https://doi.org/10.1002/alr.22737.
Hohenberger R, Beckmann S, Kaecker C, Elicin O, Giger R, Caversaccio M, et al. Morbidity and oncological outcome after curative treatment in sinonasal squamous cell carcinoma. Ear Nose Throat J. https://doi.org/10.1177/01455613221117787.
Murr AT, Lenze NR, Weiss JM, Grilley-Olson JE, Patel SA, Shen C, et al. Sinonasal squamous cell carcinoma survival outcomes following induction chemotherapy vs standard of care therapy. Otolaryngol Neck Surg. 2022;6:1455613221117787. https://doi.org/10.1177/01945998221083097.
Seiwert TY, Burtness B, Mehra R, Weiss J, Berger R, Eder JP, et al. Safety and clinical activity of pembrolizumab for treatment of recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-012): an open-label, multicentre, phase 1b trial. Lancet Oncol. 2016;17:956–65. https://doi.org/10.1016/S1470-2045(16)30066-3.
Ferris RL, Blumenschein G, Fayette J, Guigay J, Colevas AD, Licitra L, et al. Nivolumab for recurrent squamous-cell carcinoma of the head and neck. N Engl J Med. 2016;375:1856–67. https://doi.org/10.1056/NEJMoa1602252.
Perri F, Longo F, Caponigro F, Sandomenico F, Guida A, Della Vittoria Scarpati G, et al. Management of HPV-related squamous cell carcinoma of the head and neck: pitfalls and caveat. Cancers. 2020;12:975. https://doi.org/10.3390/cancers12040975.
Solomon B, Young RJ, Rischin D. Head and neck squamous cell carcinoma: genomics and emerging biomarkers for immunomodulatory cancer treatments. Semin Cancer Biol. 2018;52:228–40. https://doi.org/10.1016/j.semcancer.2018.01.008.
Sanghvi S, Khan MN, Patel NR, Yeldandi S, Baredes S, Eloy JA. Epidemiology of sinonasal squamous cell carcinoma: a comprehensive analysis of 4994 patients. Laryngoscope. 2014;124:76–83. https://doi.org/10.1002/lary.24264.
Sharma A, Tang AL, Takiar V, Wise-Draper TM, Langevin SM. Human papillomavirus and survival of sinonasal squamous cell carcinoma patients: a systematic review and meta-analysis. Cancers. 2021;13:3677. https://doi.org/10.3390/cancers13153677.
Lewis JS, Thorstad WL, Chernock RD, Haughey BH, Yip JH, Zhang Q, et al. p16 positive oropharyngeal squamous cell carcinoma:an entity with a favorable prognosis regardless of tumor HPV status. Am J Surg Pathol. 2010;34:1088–96. https://doi.org/10.1097/PAS.0b013e3181e84652.
Lechner M, Liu J, Masterson L, Fenton TR. HPV-associated oropharyngeal cancer: epidemiology, molecular biology and clinical management. Nat Rev Clin Oncol. 2022;19:306–27. https://doi.org/10.1038/s41571-022-00603-7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hebsgaard, M., Eriksen, P., Ramberg, I. et al. Human Papillomavirus in Sinonasal Malignancies. Curr Otorhinolaryngol Rep 11, 109–116 (2023). https://doi.org/10.1007/s40136-023-00448-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40136-023-00448-3