Abstract
Purpose of Review
To review and summarize current updates in the epidemiology, natural history, and treatment strategies of vestibular schwannoma (VS).
Recent Findings
The incidence of VS has increased in recent decades, which may be due in part to improved detection but may also be an actual biological shift. Based on our improving understanding of VS’s natural history, treatment strategy has shifted toward primary observation. Based on several large studies, we can predict which VS are at the greatest risk of growth and which patients are at risk of losing serviceable hearing. Measurement of tumor volume is a new tool that is more sensitive than linear axial measurements, although the clinical implications are still under investigation.
Summary
Advances in our understanding of VS’s natural history improve our ability to counsel patients on when to pursue intervention and which modality is most appropriate on an individual basis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Our understanding of the natural history of vestibular schwannoma (VS) has undergone significant advancements in recent years. In the past, vestibular schwannomas were usually managed with microsurgery or radiosurgery. However, because of the benign nature of a vestibular schwannoma and the lack of growth seen in many tumors, observation with serial MRI imaging has recently become more common. We aim to review the natural history of vestibular schwannomas and discuss when to actively manage a vestibular schwannoma, either with microsurgical resection or radiosurgery.
Current Epidemiology
The incidence of vestibular schwannoma has increased over the past several decades [1, 2]. Using a database of all vestibular schwannoma patients in Denmark beginning in 1976, Retnitsky et al. showed an increase in the incidence of vestibular schwannoma from three cases per million in 1976 to 34 cases per million in 2015 [3]. Multiple other studies from around the world also show an increased incidence of vestibular schwannoma over the past several decades [1, 4,5,6,7].
Whether or not this increased incidence of vestibular schwannoma is due to a true increase or other factors is controversial. The widespread use of MRI has resulted in the diagnosis of more vestibular schwannomas that would have otherwise been missed by other imaging modalities, such as computed tomography. In addition, increased awareness of vestibular schwannoma and more frequent evaluation of asymmetric otologic complaints such as hearing loss and tinnitus contribute to increased detection. Tumor size at the time of diagnosis has significantly decreased over the past decades [3, 8]. In Denmark, mean tumor size at time of diagnosis decreased from 27.6 mm in the period between 1976 and 1978 to 7 mm in 2015 [3]. The same group showed age at the time of diagnosis increased from a mean age of 49.2 years in 1976 to a mean age of 60 in 2015 [3]. Younger patients were found to have larger tumors at diagnosis than older patients, suggesting an increase in incidentally detected small tumors. Taken together, this evidence suggests that improvements in detection have contributed to the increasing incidence of vestibular schwannoma [3].
On the other hand, some studies suggest the increase incidence of vestibular schwannoma may be due to an underlying true biological shift in addition to improved detection. Marinelli et al. addressed this question by comparing the rate of MRI and the diagnosis of asymptomatic vestibular schwannoma in Olmsted County, Minnesota [2]. Although MRI utilization stabilized after 2004, the incidence of incidentally diagnosed vestibular schwannoma increased by 6.3% per year through 2016 [2]. It is important to note this change approached significance using a log-linear model with a p value of 0.0568 [2]. The most likely cause of a true increased incidence of vestibular schwannoma would be environmental factors such as increased use of cell phones and other similar technologies [2]. However, studies looking at causation of radiofrequency and vestibular schwannoma are mixed and inconclusive [9, 10]. More studies are needed to determine if there is a true rise in the incidence of vestibular schwannomas.
Understanding the Natural History of Vestibular Schwannoma
The majority of vestibular schwannomas may not enlarge after initial diagnosis; however, the challenge is to identify which tumors will enlarge over time and require treatment. Reznitsky et al. followed 2312 patients who were being observed with a vestibular schwannoma over a mean time of 7.7 years [3]. Over this time, 19% of patients entered the active treatment group [3]. During the first 5 years of observation, tumor enlargement was observed in 21% and 37% of intracanalicular and extrameatal tumors, respectively. For tumors observed for at least 10 years, tumor enlargement was observed in 25% and 42% of intracanalicular and extrameatal tumors, respectively [3]. The authors concluded most tumors do not enlarge, extrameatal tumors are more likely to enlarge, and tumors rarely enlarge after 5 years of stability [3]. In contrast, Lees et al. demonstrated a higher rate of tumor growth using both linear and volumetric measurements [11]. In a cohort of 361 patients with a vestibular schwannoma followed over a median of 4.1 years, 48% of tumors grew at a mean of 1.1 years when measured using maximum diameter, and 69% of tumors grew at a mean of 1.8 years when measuring using volumetric measurements. Forty-four percent of patients required treatment [11]. Hunter et al. reported on 564 patients who were being observed for a vestibular schwannoma with a mean follow-up period of 22.9 months. During the observation period, 40.8% tumors grew greater than 2 mm and 32.1% required treatment [12]. The differences in growth rates seen between different institutions could be explained by a number of reasons. The Reznitsky et al. study uses a database of virtually all people in Denmark who were diagnosed with a vestibular schwannoma since 1976. The studies by Lees and Hunter are from a tertiary referral center, which may have a referral bias and a different patient population compared to the Denmark study.
Paldor et al. reported in a recent literature review the mean growth rate for all vestibular schwannomas to be about 1 mm/year and 3 mm/year in tumors that have already been shown to grow [13]. Most tumors will show growth within the first 3–5 years of observation; however, there are reports of tumors going through a period of quiescence before initiating growth over 5 years after diagnosis [3, 11]. Macielak et al., in a series of 361 patients with a vestibular schwannoma that was being observed, showed 8.1% of tumors started to grow after a 5-year period of quiescence [14•]. The longest delay between initial diagnosis and tumor growth was 11.1 years. Because of the possibility of late growth, initially stable vestibular schwannomas should be followed for a minimum of 10 years and probably for a lifetime.
There are inconsistencies among reports about factors that predict tumor growth. Tumor size at time of diagnosis is associated with a higher risk of tumor growth in some series and not in others. Hunter et al. showed a 2.22-fold increase risk of tumor growth for every centimeter increase size at presentation [12].
Other studies have supported that tumors may not demonstrate growth for many years—in some cases up to 15 years [15]. Additionally, there is evidence that tumors that previously grew may stop growing or even spontaneously decrease in size [8, 16]. Recent efforts to characterize potential predictors of growth have highlighted avenues for future areas of study. Hunter et al. found that disequilibrium symptoms at diagnosis increased risk of tumor growth [12]. Another large retrospective study found a correlation between metformin use and reduced growth [17, 18]. A growing area of investigation is the relationship between cyclooxygenase-2 (COX-2) receptor expression and VS growth. A retrospective case series by Kandathil et al. suggested aspirin intake correlates with reduced growth of VS, and the authors concluded this was mediated by COX-2 inhibition [19, 20]. On the other hand, another large retrospective analysis evaluating the role of aspirin dosage, NSAID use, and COX-2 selectivity in VS growth found that none were significantly associated with VS growth or VS diameter at presentation [21]. There were significant differences in the two study designs that limit direct comparison, so the role of COX-2 remains controversial, although there is currently a multi-institutional prospective study ongoing to further investigate this relationship.
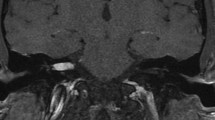
Volumetric Analysis–Challenging the Linear Growth Model
Linear measurements in the axial plane is the most widely used method in measuring acoustic neuroma and subsequent tumor growth. The American Academy of Otolaryngology–Head and Neck Surgery recommended a method of measuring the axial tumor diameter along the axis of the petrous ridge, excluding the internal auditory canal component [22]. There are inherent limitations to extrapolations based on linear measurements; however, access to software for measuring tumor volumes remains limited. Volumetric analysis intuitively gives a more accurate measurement of tumor size for both diagnosis and trending growth during serial observation. However, it was not until recently that a study by Lees et al. directly compared the clinical implications of utilizing volumetric versus linear measurements [11]. They found that volumetric measurements detected tumor growth earlier and were overall more sensitive in detection with 85% of their cohort demonstrating no linear growth at 10-year observation versus only 68% by volumes [11]. The natural conundrum that follows the development of a dramatically more sensitive measurement tool is how to interpret the new findings in the clinical setting. Broadly, the literature utilizing volumetric analysis has defined VS growth criteria as an increase of 20% in tumor volume between serial scans [11, 17, 23]. However, there is a paucity of data to guide the interpretation of a VS that meets criteria for volumetric growth, especially when considering a large number of VS will meet criteria for volumetric growth without meeting criteria for linear growth. Furthermore, while the definition of linear growth is static, the definition of volumetric growth is intrinsically variable as it is a proportion of the index volume. Thus, a very large tumor may threaten the brainstem before meeting growth criteria by volume, whereas a very small tumor may meet criteria based solely on variability of the quality and collimation of scans.
Expanding Role of Observation
For the majority of patients who present with tumors less than 1.5 cm in maximum cerebellopontine angle dimension, most providers recommend a conservative approach with observation [24]. Observation strategies are generally predicated on the knowledge that the majority of VS that demonstrate growth will do so within the first 5 years of detection. There is less agreement about the appropriate strategy for tumors that do not exhibit growth after 5 years of observation. Macielak et al. described a cohort of 361 patients of whom 14 (3.9%) demonstrated linear growth after 5 years of observation [14•]. Based on their findings, they recommended balancing cost-effectiveness with risk mitigation by spacing out the surveillance interval after 5 years but continuing lifelong surveillance. However, once a patient meets criteria for growth either by linear or volumetric measurement during a period of observation, there is still the need for patient-centered collaborative decision-making in selecting the next course of action. As previously discussed, in a cohort of patients with VS meeting criteria for volumetric growth that elected for continued observation, over 40% demonstrated no continued growth after five years of further observation [25••]. This has important implications for counseling patients as there are a litany of reasons a patient might elect for continued observation despite tumor growth including personal preference, tumor in an only hearing ear, poor operative candidate, etc. Studies have suggested that hearing status, distance from hospital, and even marital status are associated with significant differences in selection of treatment versus observation [26].
Natural History of Hearing Loss and Vestibular Schwannomas
The majority of VS patients present with some degree of asymmetric sensorineural hearing loss. The recent literature has focused on the management of patients with serviceable hearing, defined as AAO-HNS class A or B hearing (pure tone average (PTA) ≤ 50 dB HL and word recognition score (WRS) ≥ 50%) [22]. Hunter et al. was the first to quantify the risk of non-serviceable hearing based on presenting audiometric features in a large cohort of patients undergoing initial observation [27•]. The natural history of hearing loss in their cohort was similar to previously described large cohorts by Stangerup et al. [28] and Sughrue et al. [29]. Specifically, at 1, 3, 5, 7, and 10 years following diagnosis, the rate of maintaining serviceable hearing was 94%, 77%, 66%, 56%, and 44%, respectively. PTA and WRS at presentation were independently associated with development of non-serviceable hearing: each 10-dB increase in PTA doubled risk and each 10% decrease in WRS increased risk 1.5-fold. A novel investigation by Carlson et al. sought to add nuance to the interpretation of audiometric trends and found that the rates of early PTA and WRS decline during the initial period of observation are significantly associated with time to development of non-serviceable hearing [30]. The prognostic value of these hearing outcomes after observation should theoretically be more broadly generalizable than reports of hearing outcomes after radiation or microsurgery due to variation in technique and skill. Thus, these reports give us the ability to guide our patients through an informed decision-making process with regard to elective observation.
One additional question with regard to the natural history of hearing loss and vestibular schwannomas is the association between tumor volume and hearing loss. Tumor volume was found to be associated with increased PTA and decreased WRS at the time of diagnosis (and by extension associated with decreased time to loss of serviceable hearing); however, there was no independent increase in risk after accounting for the PTA and WRS at the time of diagnosis [23]. There was notably no significant association between demonstration of volumetric growth and loss of serviceable hearing during the observation period.
Optimal Timing of Intervention
There are several guiding principles that carry general acceptance as reasons to offer an intervention to a patient with VS. A commonly accepted adage is that a VS that has demonstrated growth will continue to grow and eventually confer risks related to mass effect. However, as previously discussed, there is both contentions surrounding the true risk of continued observation after growth and even regarding how growth should be defined. Along similar lines, tumors ≥ 2cm in diameter or contacting the brainstem should be offered intervention due to risk of mass effect. For tumors ≥ 3cm in diameter microsurgery is favored to obviate the risk of mass effect due to post-radiation edema. Another important indication for active treatment is hearing preservation. In patients with serviceable hearing, durable hearing preservation after microsurgery may be favorable to progressive hearing loss with radiosurgery or observation. For example, in a novel comparison of hearing outcomes after retrosigmoid approach microsurgery for a single neurosurgeon versus gamma knife radiosurgery, the rate of hearing preservation after microsurgery was 71.4%, whereas the hearing loss progression–free survival after gamma knife was 80, 66.7, and 53.3% at 1, 3, and 5 years [31]. Rates of hearing preservation vary across practices due to differences in surgical and radiation techniques. It is important to thoroughly counsel patients on the risks and benefits of all treatment strategies and take patient preference into consideration.
Future Directions
Although significant progress has been made in recent years in our efforts to update the evidence-based practice of VS management, there remain numerous avenues for future investigation. The utilization of volumetric analysis is in its early stages; we have not yet reached a consensus on how to define volumetric growth and what the appropriate clinical applications of its measurement should be. As more patients continue to elect for serial observation, there is an increasing need for future studies aimed at identifying features that can predict tumor growth and hearing outcomes. Finally, as a large proportion of tumors are observed in the community setting, there is a need to study the natural history of VS outside of the tertiary referral center setting, which predominates the current literature.
Conclusion
The natural history of vestibular schwannomas is highly variable with some tumors demonstrating stability for many years and others demonstrating rapid growth. Furthermore, tumors that are stable for many years may still demonstrate delayed growth, while other tumors that have grown may stop growing at a later time point. Therefore, the decision to intervene either with microsurgery or radiosurgery should be tailored to each patient, taking into account the tumor size, tumor growth, hearing status, and perhaps most importantly, patient preference. Further characterization of the natural history of vestibular schwannomas will enhance the physician’s ability to accurately counsel the patient.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Marinelli JP, Lohse CM, Carlson ML. Incidence of vestibular schwannoma over the past half-century: a population-based study of Olmsted County, Minnesota. Otolaryngol Head Neck Surg (US). 2018;159:717–23.
Marinelli JP, Lohse CM, Grossardt BR, Lane JI, Carlson ML. Rising incidence of sporadic vestibular schwannoma: true biological shift versus simply greater detection. Otol Neurotol. 2020;41:843–7.
Reznitsky M, Petersen MMBS, West N, Stangerup SE, Cayé-Thomasen P. Epidemiology of vestibular schwannomas – prospective 40-year data from an unselected national cohort. Clin Epidemiol. 2019;Volume 11:981–6.
Kshettry VR, Hsieh JK, Ostrom QT, Kruchko C, Barnholtz-Sloan JS. Incidence of vestibular schwannomas in the United States. J Neuro-Oncol. 2015;124:223–8.
Kleijwegt M, Ho V, Visser O, Godefroy W, van der Mey A. Real incidence of vestibular schwannoma? estimations from a national registry. Otol Neurotol. 2016;37:1411–7.
Evans DGR, Moran A, King A, Saeed S, Gurusinghe N, Ramsden R. Incidence of vestibular schwannoma and neurofibromatosis 2 in the North West of England over a 10-year period: Higher incidence than previously thought. Otol Neurotol. 2005;26:93–7.
Koo M, Lai JT, Yang EYL, Liu TC, Hwang JH. Incidence of vestibular schwannoma in Taiwan from 2001 to 2012: a population-based national health insurance study. Ann Otol Rhinol Laryngol. 2018;127:694–7.
Carlson ML, Habermann EB, Wagie AE, Driscoll CL, van Gompel JJ, Jacob JT, et al. The changing landscape of vestibular schwannoma management in the United States - a shift toward conservatism. Otolaryngol Head Neck Surg (US). 2015.
Bortkiewicz A, Gadzicka E, Szymczak W. Mobile phone use and risk for intracranial tumors and salivary gland tumors - a meta-analysis. Int J Occup Med Environ Health. 2017; 27–43.
Röösli M, Lagorio S, Schoemaker MJ, Schüz J, Feychting M. Brain and salivary gland tumors and mobile phone use: evaluating the evidence from various epidemiological study designs. Annu Rev Public Health. 2019; 221–38.
Lees KA, Tombers NM, Link MJ, Driscoll CL, Neff BA, van Gompel JJ, et al. Natural history of sporadic vestibular schwannoma: a volumetric study of tumor growth. Otolaryngol Head Neck Surg (US). 2018;159:535–42.
Hunter JB, Francis DO, O’Connell BP, Kabagambe EK, Bennett ML, Wanna GB, et al. Single institutional experience with observing 564 vestibular schwannomas: factors associated with tumor growth. Otol Neurotol. 2016;37:1630–6.
Paldor I, Chen AS, Kaye AH. Growth rate of vestibular schwannoma. J Clin Neurosci. 2016;1–8.
Macielak RJ, Patel NS, Lees KA, Lohse CM, Marinelli JP, Link MJ, et al. Delayed tumor growth in vestibular schwannoma: an argument for lifelong surveillance. Otol Neurotol. 2019;40:1224–9 Findings from this study suggest vestibular schwannoma require lifelong surveillance, even after years of no growth during observation.
Stangerup SE, Caye-Thomasen P. Epidemiology and natural history of vestibular schwannomas. Otolaryngologic Clinics of North America. 2012.
Stangerup SE, Caye-Thomasen P, Tos M, Thomsen J. The natural history of vestibular schwannoma. Otol Neurotol. 2006;27:547–52.
Tran S, Killeen DE, Qazi S, Balachandra S, Hunter JB. Association of metformin with the growth of vestibular schwannomas. Otolaryngol Head Neck Surg (US). 2020;
Feng AY, Enriquez-Marulanda A, Kouhi A, Ali NES, Moore JM, Vaisbuch Y. Metformin potential impact on the growth of vestibular schwannomas. Otol Neurotol. 2020;41:403–10.
Kandathil CK, Cunnane ME, McKenna MJ, Curtin HD, Stankovic KM. Correlation between aspirin intake and reduced growth of human vestibular schwannoma: volumetric analysis. Otol Neurotol. 2016;37:1428–34.
Kandathil CK, Dilwali S, Wu CC, Ibrahimov M, McKenna MJ, Lee H, et al. Aspirin intake correlates with halted growth of sporadic vestibular schwannoma in vivo. Otol Neurotol. 2014;35:353–7.
Hunter JB, O’Connell BP, Wanna GB, Bennett ML, Rivas A, Thompson RC, et al. Vestibular schwannoma growth with aspirin and other nonsteroidal anti-inflammatory drugs. Otol Neurotol. 2017;38:1158–64.
Committee on hearing and equilibrium guidelines for the evaluation of hearing preservation in acoustic neuroma (vestibular schwannoma)*. Otolaryngol Head Neck Surg. England; 1995;113:179–180.
Patel NS, Huang AE, Dowling EM, Lees KA, Tombers NM, Lohse CM, et al. The influence of vestibular schwannoma tumor volume and growth on hearing loss. Otolaryngol Head Neck Surg (US). England; 2020;162:530–7.
Carlson ML, van Gompel JJ, Wiet RM, Tombers NM, Devaiah AK, Lal D, et al. A cross-sectional survey of the North American Skull Base Society: current practice patterns of vestibular schwannoma evaluation and management in North America. J Neurol Surg B Skull Base. 2018;79:289–96.
Marinelli JP, Lees KA, Lohse CM, Driscoll CLW, Neff BA, Link MJ, et al. Natural history of growing sporadic vestibular schwannomas: an argument for continued observation despite documented growth in select cases. Otol Neurotol. 2020;41:e1149–53 In this study the authors argue that a vestibular schwannoma that has demonstrated growth will not necessarily continue to grow. This supports an overall paradigm shift towards increasing observation of vestibular schwannoma.
Ostler B, Killeen DE, Reisch J, Barnett S, Kutz JW, Isaacson B, et al. Patient demographics influencing vestibular schwannoma size and initial management plans. World Neurosurg. 2020.
Hunter JB, Dowling EM, Lohse CM, O’Connell BP, Tombers NM, Lees KA, et al. Hearing outcomes in conservatively managed vestibular schwannoma patients with serviceable hearing. Otol Neurotol. 2018;39:e704–11 Findings from this study suggest that the risk of loss of serviceable hearing during conservative management of vestibular schwannoma can be predicted based on baseline audiometry. Specifically, pure tone average and word recognition were independently associated with development of non-serviceable hearing.
Stangerup SE, Tos M, Thomsen J, Caye-Thomasen P. Hearing outcomes of vestibular schwannoma patients managed with wait and scan: predictive value of hearing level at diagnosis. J Laryngol Otol. 2010;124:490–4.
Sughrue ME, Yang I, Aranda D, Lobo K, Pitts LH, Cheung SW, et al. The natural history of untreated sporadic vestibular schwannomas: a comprehensive review of hearing outcomes - Clinical article. J Neurosurg. 2010;112:163–7.
Carlson ML, Dowling EM, Lohse CM, O’Connell BP, Driscoll CLW, Haynes DS, et al. Rate of initial hearing loss during early observation predicts time to non-serviceable hearing in patients with conservatively managed sporadic vestibular schwannoma. Otol Neurotol. 2019;E1012–7.
Han MS, Jung S, Lim SH, Kim IY, Moon KS, Jung TY, et al. What clinicians should consider to determine a more beneficial treatment strategy for small to medium sized vestibular schwannoma with serviceable hearing: a single surgeon’s long-term outcome of microsurgery and gamma knife radiosurgery. Otol Neurotol. 2020;41:1122–30.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Vestibular schwannoma natural history
This article is part of the Topical collection on OTOLOGY: Vestibular Schwannomas
Rights and permissions
About this article
Cite this article
Tan, D., Killeen, D.E. & Kutz, J.W. The Natural History of Vestibular Schwannoma and When to Intervene. Curr Otorhinolaryngol Rep 9, 134–138 (2021). https://doi.org/10.1007/s40136-021-00337-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40136-021-00337-7