Abstract
Purpose of Review
Various imaging techniques used in stroke evaluation have complementary, evolving roles. This article reviews recent updates in emergent stroke neuroimaging.
Recent Findings
Multiple recent randomized trials showing benefit of endovascular therapy in strokes with confirmed large-vessel occlusion emphasize need for vessel imaging, typically CTA, in addition to unenhanced head CT. In addition, because recent trials published in 2018 showed efficacy of mechanical thrombectomy at up to 24 h from symptom onset in stroke patients with favorable ischemic core and/or penumbra assessments, imaging techniques to define viable and infarcted tissue, such as DWI or CT/MR perfusion imaging, have an increasing role in emergent stroke assessment. Other studies contributing to new AHA/ASA stroke guidelines are also discussed.
Summary
Neuroimaging remains crucial to emergent stroke evaluation, with CTA, MRI, and perfusion studies playing an increasing role in identifying patients likely to benefit from treatment.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Acute stroke is a leading cause of morbidity and mortality, affecting ~ 800,000 people in the United States per year [1]. As the vast majority (80–90%) of strokes are ischemic as opposed to hemorrhagic, this review focuses primarily on emergent neuroimaging of acute ischemic stroke (AIS). The field of stroke imaging continues to rapidly evolve, with many recent clinical trials and increasing public awareness. This review article provides an overview of stroke neuroimaging in the emergent setting, with emphasis on recent updates in the stroke literature in the past 5 years.
Role of Imaging in Acute Stroke Management
The primary objective of acute stroke imaging is to identify patients most likely to benefit from rapid reperfusion of potentially salvageable brain tissue. Treatment generally consists of intravenous thrombolysis or intra-arterial therapy (IAT), including mechanical thrombectomy. There is strong evidence of favorable treatment responses in patients receiving intravenous thrombolysis within 4.5 h of symptom onset [2, 3]. The administration of intravenous tissue plasminogen activator (tPA) in moderately symptomatic patients increases positive patient outcome rates from ~ 50 to 75% [4]. IAT can be performed at even later intervals [5•], with recent trials showing beneficial effects of thrombectomy in appropriately selected patients up to 24 h after symptom onset [6••, 7••]. As the benefit of IAT decreases with time by approximately 6% per hour of reperfusion delay [8], prompt evaluation of treatment candidates remains critically important. The 2018 stroke guidelines jointly published by the American Heart Association (AHA) and the American Stroke Association (ASA) now recommend that median door-to-imaging times be at most 20 min among treatment candidates [9••].
As timely accurate interpretation of neuroimaging is crucial for clinical decision-making, it is important for radiologists to be familiar with imaging assessment of AIS. The emergent imaging evaluation of stroke has the following goals: (1) rule out intracranial hemorrhage, mass lesions, or other stroke mimics; (2) define the ischemic core and ischemic penumbra (“tissue-at-risk”); and (3) assess the vasculature. The role of imaging in evaluation of these objectives and their impact on AIS management are discussed below under the subheadings for each modality.
Computed Tomography
Computed tomography (CT) remains the standard of care for initial AIS imaging due to its widespread availability, short scan time, and ability to identify contraindications for thrombolytic therapy. CT can reliably detect intracranial hemorrhage or intracranial mass lesions, which would preclude thrombolytic therapy. In additional to hemorrhagic transformation of an ischemic stroke, acute intracranial hemorrhage may represent a hemorrhagic stroke secondary to various causes, such as hypertension, coagulopathy, vascular malformations, aneurysms, or mass lesions (Fig. 1).
Intracranial hemorrhage in a 32-year-old male presenting with unresponsiveness. a Axial head CT imaging demonstrates hyperattenuating subarachnoid hemorrhage in the sylvian fissures and basal cisterns (arrowheads) and a focal hyperdense clot near the anterior aspect of the suprasellar cistern (arrow). b SWI also depicts subarachnoid and intraventricular hemorrhage (arrowheads) as low signal. A focal clot near the anterior aspect of the suprasellar cistern (arrow) is also visible. c A 3D volume-rendered image from a CTA study shows an anterior communicating artery aneurysm (arrow) as the likely cause of hemorrhage
CT can also identify early signs of ischemia, including parenchymal hypoattenuation, loss of gray–white differentiation, sulcal effacement, and other evidence of mass effect (Figs. 2a, 3a). Sulcal effacement with preservation of gray–white differentiation, i.e., isolated sulcal effacement, is occasionally seen in stroke patients with proximal vascular occlusion and robust collaterals [10]. If present, this finding may indicate preserved underlying parenchyma that could benefit from reperfusion [10]. CT findings of AIS typically become more conspicuous over time as magnitude of hypoattenuation increases (Fig. 2b, c). Growth of infarct volume is common in AIS, and infarct volume at 24 h or at 1 week predicts functional outcome [11].
A 64-year-old female with acutely altered mental status. a Early ischemic changes on the initial non-contrast head CT include subtle hypoattenuation in the left MCA territory (arrows), with indistinctness of the left insular cortex and basal ganglia. b Follow-up CT imaging 24 h after the first head CT shows greater conspicuity of the region of hypoattenuation (arrows), with increased mass effect. c 7 days after presentation, the final infarct volume is more clearly delineated (arrows), with even greater mass effect. d–f MRI acquired 2 days after symptom onset demonstrates diffusion restriction and elevated FLAIR signal within the left MCA territory infarct. g SWI shows small foci of low signal intensity consistent with magnetic susceptibility from petechial hemorrhage (arrows) in the left basal ganglia within the infarcted territory. h Parametric maps from a CTP at initial workup show matched areas of markedly diminished CBF, low CBV, and elevated MTT and Tmax, consisted with a large infarct core without a significant penumbra. i A maximum intensity projection (MIP) of the brain CTA obtained at initial workup shows an LVO of the left M1 segment (arrows). The anterior left temporal lobe shows diffusely decreased vascularity (arrowheads) without appreciable collateral filling of the distal left MCA
A 67-year-old male presenting with right-sided weakness and aphasia. a Findings on head CT include subtle hypoattenuation with loss of gray–white matter differentiation involving the left insula and frontal operculum (arrows), consistent with acute ischemia. b Post-processed CT perfusion data utilizing RAPID software yields fully automated volume estimates of the infarct core (28 mL) and the ischemic penumbra (124 mL). The perfusion data meet DEFUSE 3 criteria for predicting a favorable response to endovascular intervention, including small infarct core size (< 70 mL), high ratio of ischemic tissue to infarct core volume (≥ 1.8), and penumbra volume ≥ 15 mL. c Digital subtraction angiography shows an occlusive thrombus in the proximal inferior division of the left MCA (arrow). d After mechanical thrombectomy was performed, DSA shows recanalized flow within this vessel (arrowhead). The patient subsequently showed a complete functional recovery
A hyperdense artery sign, often of the proximal middle cerebral artery (MCA), may occasionally be seen in large infarcts and is relatively specific but insensitive for intravascular thrombus (Fig. 4a). Although this sign independently predicts poorer functional outcomes [12], its presence or absence does not affect the benefit of tPA or thrombectomy on clinical outcomes [12, 13]. In some studies, lower thrombus density on CT was associated with lower recanalization rates in AIS [14, 15], but one study found no effect of thrombus density on clinical outcomes [16]. The 2018 AHA/ASA stroke guidelines recommend that the hyperdense MCA sign not be used to withhold tPA in an otherwise eligible patient [9].
Acute stroke imaging workup in a 62-year-old female. a The initial non-contrast head CT shows a hyperdense left MCA (arrow). b, c A coronal MIP and a 3D volume-rendered image from a brain CTA show absent contrast opacification of the intracranial left ICA (arrows) and MCA (arrowheads). Neck CTA imaging (not shown) also revealed absent contrast filling within most of the cervical left ICA. d DWI obtained 14 h after the initial head CT confirms the presence of an acute infarct involving the left basal ganglia
Although not sensitive for small or early ischemic changes, CT is nonetheless useful in assessing extent of ischemia, either qualitatively or using semi-quantitative methods such as the Alberta stroke program early CT score (ASPECTS), a 0–10 scale with higher scores denoting smaller infarcts [17]. Extent of ischemia on CT has prognostic implications. Early imaging signs on CT involving greater than one-third of the MCA territory have been associated with greater risk of hemorrhagic transformation and overall poorer outcomes [18,19,20].
Extent of abnormalities on baseline CT may also influence treatment eligibility, as larger baseline infarct volumes typically have poorer treatment responses, and many clinical trials showing benefit of IAT included only patients with small infarcts [21•, 22•, 23•, 24•]. However, the literature is still evolving, with recent data suggesting that strokes with moderate CT-visible infarcts (ASPECTS 5–7) may also benefit from IAT [25]. Although past guidelines had specified involvement of a large hypodensity involving over a third of the MCA territory as a contraindication to tPA, secondary analysis of IST-3 trial data found no significant interaction between baseline CT hypoattenuation and tPA administration on clinical outcomes [26]. The most recent AHA/ASA stroke guidelines state that extent and severity of hypoattenuation or early ischemic changes should not contraindicate tPA in otherwise eligible treatment candidates [9••].
Magnetic Resonance Imaging
Diffusion-weighted imaging (DWI) offers greater sensitivity in detecting early ischemic changes (Figs. 2d, e, 4d), with restricted diffusion often apparent within minutes of stroke onset. In a prospective comparison of MRI and CT, sensitivity of MRI for detection of AIS increases over time from 73% at < 3 h after symptom onset to 92% at > 12 h, whereas CT sensitivities are in the 12–20% range at these time intervals [27]. The absence of DWI abnormality, in addition to resolution of symptoms within 1 h, is needed for distinguishing transient ischemic attack (TIA) from strokes [28]. It is important to note that diffusion abnormality is initially absent in some patients who ultimately receive a diagnosis of AIS, particularly in early or very small strokes. The extent of restriction diffusion may be used to quantify irreversibly infarcted tissue and has been used to determine eligibility for endovascular treatment in recent clinical trials [6••, 7••].
In addition to DWI, other MRI sequences are also helpful in AIS. FLAIR shows signal hyperintensity (Fig. 2f) but typically hours after stroke onset and to a greater extent in patients with poor collaterals [29]. The accuracy of MR imaging for evaluating acute intracranial hemorrhage is likely similar to that of CT and may be higher for detecting chronic cerebral microhemorrhages [30], particularly when using sequences sensitive to paramagnetic susceptibility, such as gradient-recalled echo or susceptibility-weighted imaging (SWI) sequences (Fig. 2g). The presence of microbleeds may be a potential concern when considering thrombolytic therapy due to a higher suspected risk of developing symptomatic intracranial hemorrhage, as supported by recent meta-analyses [31, 32]. However, some authors have argued that the risks attributable to microbleeds are likely small relative to the benefit of thrombolytic therapy [33]. The 2018 AHA/ASA stroke guidelines recommend against routine use of MRI to exclude microbleeds prior to tPA [9••].
Although some authors have proposed routine use of MRI as the initial imaging modality during AIS assessment, expense and timely accessibility are factors limiting MRI use compared to CT in most settings. MR imaging offers greater sensitivity in detecting ischemic stroke within 12 h of onset, but the influence on clinical decision-making or outcomes in the acute setting compared to CT may not be significantly different. A recent systematic review and meta-analysis concluded that routine MR imaging in all patients with AIS is not cost-effective [34].
Perfusion Imaging
Determining the extent of brain that is viable but at risk can be assessed by imaging, including CT perfusion (CTP) and MR perfusion, sometimes in conjunction with clinical neurological assessment using the National Institutes of Health Stroke Scale (NIHSS). CT perfusion, in which multiple CT acquisitions are obtained sequentially during bolus administration of intravenous contrast, is frequently used in emergent stroke assessment. It can detect strokes with 95% specificity and 80% sensitivity in a recent meta-analysis [35]. Limited spatial resolution likely contributes to false negatives, which consists mostly of small lacunar infarcts. Given poor sensitivity of non-contrast CT in detecting posterior fossa strokes, CTP can improve diagnostic accuracy of acute ischemia in the posterior circulation [36].
A major strength of CTP is its ability to characterize the dynamic perfusion status of the brain. The pathophysiology of ischemic stroke is typically based on hypoperfusion of a vascular territory supplied by a stenosed or occluded artery. A markedly hypoperfused ischemic core representing irreversibly damaged tissue may be bordered by a less severely hypoperfused ischemic penumbra. The penumbra is maintained by collateral circulation and is potentially salvageable with timely reperfusion. There could also be an adjacent area not at risk of infarction described as benign oligemia.
Time–density curves from CTP acquisition allow calculation of hemodynamic parameters such as cerebral blood flow (CBF), cerebral blood volume (CBV), mean transit time (MTT), time to peak (TTP), and time to maximum of the tissue residue function (Tmax) (Fig. 2h). The ischemic core may be defined by low CBV or reduction in CBF to below a relative or absolute threshold. Similarly, the penumbra can be estimated as the area of prolonged MTT, TTP, or Tmax that is not included in the infarct core, or it can be defined by CBF values within a defined range. While various postprocessing software packages are available to generate these parameters from CTP data, the RAPID tool (iSchemaView), which has been validated in recent stroke trials, is one example of software that provides fully automated identification of ischemic core and penumbra in a standardized and easily accessible manner. A representative output from the RAPID software, shown in Fig. 3b, illustrates RAPID’s ability to estimate volume of ischemic hypoperfusion based on Tmax > 6 s, estimate core infarct volume based on CBF < 30% of normal tissue, and calculate values for mismatch volume and mismatch ratio based on the difference and ratio of these values, respectively. Automated CTP-based mismatch selection using RAPID software is robust in clinical practice and is associated with faster treatment decisions compared to MRI [37].
Ischemic core sizes on baseline perfusion imaging can predict final infarct sizes [38] and are a major determinant of clinical outcome at 3 months [39]. In general, patients with smaller ischemic core sizes and growth are associated with more favorable outcomes. Patients with very poor collaterals tend to exhibit rapid infarct growth, while those with more developed collaterals typically have smaller ischemic core sizes relative to the hypoperfusing region and are generally favorable candidates for reperfusion therapy.
An inherent disadvantage of routine CTP use is the high radiation exposure related to acquisitions at different spatial levels over time. Typically images are obtained at lower tube voltages (e.g., 80 kVp) than for head CT. Further reduction in tube voltage to 70 kVp and use of variable sampling times have recently been shown to lower radiation dose without significantly compromising imaging quality or diagnostic accuracy [40, 41]. Ionizing radiation exposure can be avoided by using MRI to assess perfusion status, using such techniques as dynamic susceptibility-contrast MRI (DSC-MRI) and interpreted in a manner analogous to CTP. In combination with DWI to define the infarct core, this allows calculation of a diffusion–perfusion mismatch as a parameter for penumbral estimation. Although the concepts underlying CT and MRI perfusion imaging are similar, some perfusion parameters derived from the two modalities may not be concordant, but good agreement between CT and MR perfusion can be achieved when using Tmax [42]. Perfusion status using either CT or MR allows better prediction of clinical outcomes than recanalization assessment [43, 44].
Imaging of the Vasculature
CT Angiography
CT angiography (CTA) is often included in initial stroke workup and can evaluate vessel patency, thrombus characteristics, collateral status, and other vessel abnormalities in the head and neck. CTA can usually be performed rapidly in the emergent setting, often immediately after the initial non-contrast head CT. The need for intravenous administration of iodinated contrast occasionally raises concern for subsequent renal issues, but screening serum creatinine is generally not needed prior to CTA in thrombectomy-eligible patients with suspected proximal occlusions without history of renal impairment [9••], based on growing literature supporting the safety of CTA in acute stroke workup with respect to renal function [45].
CTA is useful for emergent detection of large-vessel occlusion (LVO), a common finding in AIS, typically involving the internal carotid artery or proximal MCA (Figs. 2i, 4b, c), that may be amenable to emergent endovascular therapy. Detection of LVO on CTA is associated with poorer outcome in stroke patients receiving intravenous thrombolysis [46]. CTA can also evaluate thrombus size. In general, longer thrombi are associated with worse 90-day clinical outcomes compared to shorter thrombi but may have a greater relative benefit of thrombectomy over intravenous thrombolysis alone [47]. Although it has been proposed that thrombus length exceeding 8 mm may have lower recanalization rates with intravenous thrombolytics, some of these patients may still benefit from intravenous thrombolysis [47].
Classification methods exist for describing extent and location of thrombus on CTA, including the Boston Acute Stroke Imaging Scale (BASIS) [48] and the clot burden score (CBS) [49]. In BASIS, strokes are dichotomized as major or minor based on detection of proximal occlusions in major arteries or presence of a significant ischemic lesion on DWI or non-contrast CT. CBS assigns strokes to a scale from 0 to 10, and lower values, denoting greater clot burden, are associated with lower odds of reperfusion, larger final infarct sizes at follow-up, and worse functional outcome [50]. Modifications of these scoring systems have been described that better quantify the extent and location of thrombus and may have better prognostic accuracy [51].
CTA also permits evaluation of collateral flow, which contributes to maintaining viability of penumbral tissue and may therefore predict clinical outcomes. In general, the benefit of intra-arterial therapy is greatest in patients with good collateral supply on baseline CTA [52,53,54]. 4D-CTA or dynamic CTA, in which CTA images are reconstructed from whole-brain volumetric CT perfusion data, may also be used in AIS evaluation [55], allowing evaluation of both brain perfusion and vessel patency in a single CTP acquisition. Dynamic CTA may better predict clinical outcome by improved assessment of collateral flow compared to single-phase CTA, likely due to its superior temporal resolution [56]. Dynamic CTA may have other applications, such as evaluating extent and velocity of cortical venous filling downstream of an occluded artery to predict clinical outcome [57].
Magnetic Resonance Angiography
Magnetic resonance angiography (MRA) is an alternative to CTA in assessing the intracranial and neck vasculature. Although useful for evaluating large-vessel stenosis or occlusion, its sensitivity and specificity are less than for CTA [58], and sensitivity of MRA decreases when evaluating smaller caliber intracranial vessels. Although time-of-flight MRA has the advantage of not requiring contrast media, it may occasionally overestimate vessel stenosis, particularly in regions of high and/or turbulent vascular flow. MRA also requires more time to acquire, which may increase likelihood of motion artifact.
Digital Subtraction Angiography
While digital subtraction angiography (DSA) had historically been considered the gold standard for evaluating cerebral vessels due to its superior spatial and temporal resolution, it is infeasible as a fast diagnostic tool as it is resource-intensive and associated with higher complication rates compared to non-invasive imaging. Furthermore, one study found helical CTA to be superior to DSA for assessing posterior circulation patency in the setting of severe stenosis [58]. DSA is useful when concomitant intra-arterial therapy is contemplated (Fig. 3c, d). As a dynamic study, DSA can also provide information on tissue viability. The capillary index score is a method to assess perfusion and identify non-viable brain tissue, based on the observation that brain areas that lack capillary blush on DSA before treatment correspond to non-viable tissue [59]. Successful revascularization is more likely to produce favorable functional outcomes when capillary blush is present [60].
Other Modalities and New Techniques
Relatively new or emerging techniques in stroke imaging include arterial spin labeling (ASL), blood-oxygen-level-dependent (BOLD) MRI, and machine learning. ASL allows assessment of CBF without need for gadolinium contrast and may be comparable to DSC-MRI perfusion in assessing reperfusion in AIS [61]. Combining ASL with SWI sequences may be useful in predicting hemorrhage or functional outcome in AIS patients [62]. A modification of ASL known as territorial arterial spin labeling, in which major individual arteries are labeled separately, can be used to evaluate collateral circulation and yield results comparable to DSA [63].
Perfusion status can also be assessed by evaluating changes in BOLD signal. Resting-state functional MRI temporal analysis using BOLD allows non-invasive evaluation of cerebral hemodynamics, including CBF, without requiring contrast administration. Studies have shown that BOLD delay can be used to detect hypoperfusion in acute stroke [64,65,66], subacute stroke [67], and chronic cerebrovascular disease [65, 68].
In recent years, artificial intelligence (AI) has received increasing attention in radiology, and applications of AI to stroke have been described in recent reviews [69, 70]. For instance, supervised machine learning is a form of AI that can be used to learn complex structures from a training data set and apply that learned knowledge to predict outcomes. Deep learning is a more recently developed and specialized form of machine learning that mimics the structure of the human brain using multiple layers of artificial neural networks (ANNs). One study demonstrated that an ANN may be effective in recognizing acute ischemia and accurately differentiating stroke from mimics [71]. The ability of AI techniques to detect patterns from large amounts of complex data may enable them to eventually play an important role in imaging evaluation of AIS patients. Machine learning and other AI techniques continue to rapidly evolve and become more accessible to clinical users.
Impact of Recent Stroke Intervention Trials on Diagnostic Neuroimaging
There are numerous ongoing and recently completed clinical trials in stroke intervention. This section briefly discusses a few recent randomized clinical trials evaluating endovascular intervention that have implications particularly relevant to diagnostic radiologists. The role of endovascular therapy in AIS has evolved rapidly over the past 5 years, with current evidence now supporting a benefit of IAT in selected patients with LVO. Previously, multiple clinical trials published in 2013 reported no benefit of IAT compared to standard care with intravenous tPA [72,73,74], possibly explained by lack of imaging selection criteria (e.g., CTA confirmation of LVO or perfusion evidence of salvageable tissue), low reperfusion rates, and use of older mechanical thrombectomy devices in contrast to newer stent retrievers that may offer greater recanalization speed and efficacy. The superiority of IAT compared to intravenous tPA alone in treatment of selected patients with AIS secondary to LVO has subsequently been proven in multiple randomized trials published in 2015 and 2016 that include Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands (MR CLEAN) [5•], Endovascular Treatment for Small Core and Anterior Circulation Proximal Occlusion with Emphasis on Minimizing CT to Recanalization Times (ESCAPE) [23•], Extending the Time for Thrombolysis in Emergency Neurological Deficits—Intra-Arterial (EXTEND-IA) [24•], Solitaire With the Intention for Thrombectomy as Primary Endovascular Treatment (SWIFT-PRIME) [22•], Randomized Trial of Revascularization with Solitaire FR Device Versus Best Medical Therapy in the Treatment of Acute Stroke Due to Anterior Circulation Large Vessel Occlusion Presenting Within 8 Hours of Symptom Onset (REVASCAT) [21•], and Trial and Cost Effectiveness Evaluation of Intra-Arterial Thrombectomy in Acute Ischemic Stroke (THRACE) [75•]. In all 6 trials, a large majority of patients in the endovascular treatment arms underwent thrombectomy utilizing retrievable stents within 6 h of symptom onset in addition to standard care or intravenous tPA. These endovascular arms demonstrated improved clinical outcomes compared to standard care or intravenous tPA alone, deemed to be predominantly due to reduction in final infarct volume [76]. The HERMES (Highly Effective Reperfusion evaluated in Multiple Endovascular Stroke Trials), a meta-analysis of pooled data obtained from 5 of these trials, established that the number needed to treat in order to achieve a one-point improvement in the modified Rankin Score, a 7-point scale for assessing post-stroke neurological disability, at 90 days was 2.6 [77].
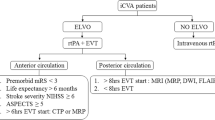
The absolute proportions of patients achieving good outcomes after IAT vary among these trials, likely attributable to differences in patient selection and imaging inclusion and exclusion criteria. However, a common feature of these trials is the requirement of imaging confirmation of LVO, and therefore emergent imaging within 6 h of stroke onset in potentially eligible IAT candidates should generally include CTA or other vascular imaging. Although several of these trials included perfusion imaging or other assessment of the ischemic penumbra or collateral status, the MR CLEAN and THRACE trials demonstrated treatment benefit using only CTA and non-contrast head CT as imaging selection criteria. The AHA/ASA stroke guidelines recommend against additional imaging studies such as CTP for potential thrombectomy candidates presenting within 6 h of stroke onset so as to not exclude patients who could potentially benefit [9••].
Two recent trials published in early 2018 demonstrated efficacy of IAT beyond 6 h of symptom onset. The Clinical Mismatch in the Triage of Wake Up and Late Presenting Strokes Undergoing Neurointervention With Trevo (DAWN) trial reported better clinical outcomes in patients treated with thrombectomy 6–24 h from the last known well time, with 49% of patients achieving functional independence at 90 days in the thrombectomy group compared to 13% with standard medical therapy [6••]. The Diffusion and Perfusion Imaging Evaluation for Understanding Stroke Evolution 3 (DEFUSE 3) trial reported significantly improved 90-day functional outcomes, decreased 90-day mortality, and higher post-treatment reperfusion and recanalization rates in patients undergoing endovascular therapy 6–16 h after the time last known to be well [7••]. Both these trials had inclusion criteria that selected patients likely to have salvageable tissue and/or favorable collateral status. Both trials required imaging confirmation of LVO and used automated postprocessing software (RAPID) to identify key parameters on CTP or MRI diffusion/perfusion imaging. In the DAWN trial, enrolled subjects were required to have a discrepancy between clinical deficit (measured by NIHSS) and infarct volume on baseline CTP or MRI imaging [6••]. The DEFUSE 3 trial required an infarct volume on baseline imaging of less than 70 mL and ischemic penumbra sizes exceeding defined thresholds [7••]. The implication for diagnostic imagers is that MRI, CTP, or other methods for core and penumbral assessment will be increasingly used for identification of thrombectomy-eligible stroke patients presenting more than 6 h after symptom onset. Moreover, given evidence of a thrombectomy benefit at up to 24 h after symptom onset, emergent neuroimaging will likely be needed in a larger number of stroke patients, and therefore, radiology practices may need to plan accordingly so as to accommodate potential increases in volume of emergent imaging requests for acute stroke evaluation.
Conclusions
Acute ischemic stroke is a common and often treatable condition for which neuroimaging plays an increasingly vital role in determining appropriate treatment. The main objectives of imaging are to exclude intracranial hemorrhage, define extent of infarct, distinguish between ischemic core and penumbra, evaluate the vasculature, and exclude mass lesions or other stroke mimics. Unenhanced CT remains the modality of choice for initial brain imaging, particularly for rapidly excluding contraindications for intravenous thrombolysis, but MRI and CTP offer additional complementary information that could affect emergent stroke management and predict prognosis. Imaging of the vasculature, typically with CTA, allows detection of proximal vascular occlusions and is increasingly important in light of recent clinical trials showing benefit of endovascular treatment at up to 24 h after symptom onset. While stroke imaging guidelines have evolved over the past 5 years, reflecting the impact of multiple high-quality studies in the recent stroke literature, neuroimaging continues to have a crucial role in the initial workup of acute stroke.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Writing Group Members, Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, et al. Executive Summary: Heart Disease and Stroke Statistics–2016 Update: A Report From the American Heart Association. Circulation. 2016;133(4):447–54. https://doi.org/10.1161/cir.0000000000000366.
Hacke W, Kaste M, Bluhmki E, Brozman M, Davalos A, Guidetti D, Larrue V, Lees KR, Medeghri Z, Machnig T, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008;359(13):1317–29. https://doi.org/10.1056/NEJMoa0804656.
National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333(24):1581–7. https://doi.org/10.1056/NEJM199512143332401.
Gonzalez RG, Furie KL, Goldmacher GV, Smith WS, Kamalian S, Payabvash S, Harris GJ, Halpern EF, Koroshetz WJ, Camargo EC, et al. Good outcome rate of 35% in IV-tPA-treated patients with computed tomography angiography confirmed severe anterior circulation occlusive stroke. Stroke. 2013;44(11):3109–13. https://doi.org/10.1161/STROKEAHA.113.001938.
• Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, Schonewille WJ, Vos JA, Nederkoorn PJ, Wermer MJ et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372(1):11–20. https://doi.org/10.1056/nejmoa1411587. The MR CLEAN trial was the first randomized trial to document a clinical benefit of intra-arterial therapy over standard medical management in acute ischemic stroke. Unlike preceding trials that failed to demonstrate a treatment benefit, this study required imaging confirmation of a proximal intracranial vascular occlusion.
•• Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, Yavagal DR, Ribo M, Cognard C, Hanel RA et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018;378(1):11–21. https://doi.org/10.1056/nejmoa1706442. A recent multi-center, randomized, controlled study demonstrating beneficial effects of intra-arterial thrombectomy compared to standard medical therapy on functional outcome in stroke patients with proximal occlusions meeting clinical mismatch criteria presenting up to 24 hours from the time last known to be well. Because only patients with a mismatch between clinical neurological deficits and initial infarct sizes on MRI or CT perfusion were included, the study has implications for neuroimaging-based selection of patients for thrombectomy.
•• Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, McTaggart RA, Torbey MT, Kim-Tenser M, Leslie-Mazwi T et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018;378(8):708–718. https://doi.org/10.1056/nejmoa1713973. A recent multi-center, randomized, controlled study in stroke patients with proximal occlusions showing improved functional outcomes following intra-arterial thrombectomy at 6 to 16 hours from the time last known to be well. Of particular relevance to the imaging workup of potential thrombectomy candidates is the use of perfusion imaging criteria as a means of identifying patients who are most likely to benefit from intra-arterial treatment.
Fransen PS, Berkhemer OA, Lingsma HF, Beumer D, van den Berg LA, Yoo AJ, Schonewille WJ, Vos JA, Nederkoorn PJ, Wermer MJ, et al. Time to reperfusion and treatment effect for acute ischemic stroke: a randomized clinical trial. JAMA Neurol. 2016;73(2):190–6. https://doi.org/10.1001/jamaneurol.2015.3886.
•• Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, Biller J, Brown M, Demaerschalk BM, Hoh B et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2018;49(3):e46–e110. A recently updated comprehensive set of evidence-based stroke guidelines. In addition to providing systematic ratings of the strengths of recommendations and quality of available evidence, this publication also contains succinct summaries of numerous studies relevant to stroke.
Haussen DC, Lima A, Frankel M, Anderson A, Belagaje S, Nahab F, Rangaraju S, Nogueira RG. Sulcal effacement with preserved gray-white junction: a sign of reversible ischemia. Stroke. 2015;46(6):1704–6. https://doi.org/10.1161/STROKEAHA.115.009304.
Bucker A, Boers AM, Bot JCJ, Berkhemer OA, Lingsma HF, Yoo AJ, van Zwam WH, van Oostenbrugge RJ, van der Lugt A, Dippel DWJ, et al. Associations of ischemic lesion volume with functional outcome in patients with acute ischemic stroke: 24-hour versus 1-week imaging. Stroke. 2017;48(5):1233–40. https://doi.org/10.1161/STROKEAHA.116.015156.
Mair G, von Kummer R, Morris Z, von Heijne A, Bradey N, Cala L, Peeters A, Farrall AJ, Adami A, Potter G, et al. Effect of alteplase on the CT hyperdense artery sign and outcome after ischemic stroke. Neurology. 2016;86(2):118–25. https://doi.org/10.1212/WNL.0000000000002236.
Man S, Hussain MS, Wisco D, Katzan IL, Aoki J, Tateishi Y, Cheng-Ching E, Hui FK, Masaryk TJ, Rasmussen PA, et al. The location of pretreatment hyperdense middle cerebral artery sign predicts the outcome of intraarterial thrombectomy for acute stroke. J Neuroimaging. 2015;25(2):263–8. https://doi.org/10.1111/jon.12115.
Niesten JM, van der Schaaf IC, van der Graaf Y, Kappelle LJ, Biessels GJ, Horsch AD, Dankbaar JW, Luitse MJ, van Seeters T, Smit EJ, et al. Predictive value of thrombus attenuation on thin-slice non-contrast CT for persistent occlusion after intravenous thrombolysis. Cerebrovasc Dis. 2014;37(2):116–22. https://doi.org/10.1159/000357420.
Moftakhar P, English JD, Cooke DL, Kim WT, Stout C, Smith WS, Dowd CF, Higashida RT, Halbach VV, Hetts SW. Density of thrombus on admission CT predicts revascularization efficacy in large vessel occlusion acute ischemic stroke. Stroke. 2013;44(1):243–5. https://doi.org/10.1161/STROKEAHA.112.674127.
Spiotta AM, Vargas J, Hawk H, Turner R, Chaudry MI, Battenhouse H, Turk AS. Hounsfield unit value and clot length in the acutely occluded vessel and time required to achieve thrombectomy, complications and outcome. J Neurointerv Surg. 2014;6(6):423–7. https://doi.org/10.1136/neurintsurg-2013-010765.
Pexman JH, Barber PA, Hill MD, Sevick RJ, Demchuk AM, Hudon ME, Hu WY, Buchan AM. Use of the Alberta Stroke Program Early CT Score (ASPECTS) for assessing CT scans in patients with acute stroke. AJNR Am J Neuroradiol. 2001;22(8):1534–42.
Hacke W, Kaste M, Fieschi C, Toni D, Lesaffre E, von Kummer R, Boysen G, Bluhmki E, Hoxter G, Mahagne MH. Intravenous thrombolysis with recombinant tissue plasminogen activator for acute hemispheric stroke. The European Cooperative Acute Stroke Study (ECASS). JAMA. 1995;274(13):1017–25.
Larrue V, von Kummer R, del Zoppo G, Bluhmki E. Hemorrhagic transformation in acute ischemic stroke. Potential contributing factors in the European Cooperative Acute Stroke Study. Stroke. 1997;28(5):957–60.
Larrue V, von Kummer RR, Muller A, Bluhmki E. Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator: a secondary analysis of the European-Australasian Acute Stroke Study (ECASS II). Stroke. 2001;32(2):438–41.
• Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, San Roman L, Serena J, Abilleira S, Ribo M et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372(24):2296–2306. https://doi.org/10.1056/nejmoa1503780. The REVASCAT study was a randomized controlled clinical trial showing benefit of thrombectomy at up to 8 hours after symptom onset in strokes with a proximal large vessel occlusion. Imaging was used to exclude patients with large infarct cores.
• Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, Albers GW, Cognard C, Cohen DJ, Hacke W et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015;372(24):2285–2295. https://doi.org/10.1056/nejmoa1415061. The SWIFT-PRIME trial was a randomized controlled clinical trial showing a higher rate of functional independence in patients treated with mechanical thrombectomy and intravenous tPA relative to intravenous tPA alone in acute strokes with large vessel occlusion and small to moderate ischemic cores on imaging.
• Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, Roy D, Jovin TG, Willinsky RA, Sapkota BL et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372(11):1019–1030. https://doi.org/10.1056/nejmoa1414905. The ESCAPE trial was a randomized controlled clinical trial showing that endovascular therapy improves functional outcome and reduces mortality in acute ischemic stroke. It is notable for its emphasis on minimizing time to reperfusion and its use of multiphase CTA to select patients based on small infarct core sizes and favorable collateral circulation distal to a proximal vascular occlusion.
• Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, Yan B, Dowling RJ, Parsons MW, Oxley TJ et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372(11):1009–1018. https://doi.org/10.1056/nejmoa1414792. The EXTEND-IA trial was a randomized controlled trial demonstrating efficacy of endovascular therapy in strokes with large vessel occlusion. A noteworthy feature of the study was that CT perfusion imaging, with automated postprocessing to assess the ischemic core and penumbra, was consistently applied for purposes of selecting patients most likely to benefit from treatment.
Yoo AJ, Berkhemer OA, Fransen PSS, van den Berg LA, Beumer D, Lingsma HF, Schonewille WJ, Sprengers MES, van den Berg R, van Walderveen MAA, et al. Effect of baseline Alberta Stroke Program Early CT Score on safety and efficacy of intra-arterial treatment: a subgroup analysis of a randomised phase 3 trial (MR CLEAN). Lancet Neurol. 2016;15(7):685–94.
IST-3 Collaborative Group. Association between brain imaging signs, early and late outcomes, and response to intravenous alteplase after acute ischaemic stroke in the third International Stroke Trial (IST-3): secondary analysis of a randomised controlled trial. Lancet Neurol. 2015;14(5):485–96. https://doi.org/10.1016/s1474-4422(15)00012-5.
Chalela JA, Kidwell CS, Nentwich LM, Luby M, Butman JA, Demchuk AM, Hill MD, Patronas N, Latour L, Warach S. Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison. Lancet. 2007;369(9558):293–8.
Easton JD, Saver JL, Albers GW, Alberts MJ, Chaturvedi S, Feldmann E, Hatsukami TS, Higashida RT, Johnston SC, Kidwell CS, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009;40(6):2276–93. https://doi.org/10.1161/STROKEAHA.108.192218.
Wouters A, Dupont P, Christensen S, Norrving B, Laage R, Thomalla G, Albers G, Thijs V, Lemmens R. Association between time from stroke onset and fluid-attenuated inversion recovery lesion intensity is modified by status of collateral circulation. Stroke. 2016;47(4):1018–22. https://doi.org/10.1161/STROKEAHA.115.012010.
Kidwell CS, Chalela JA, Saver JL, Starkman S, Hill MD, Demchuk AM, Butman JA, Patronas N, Alger JR, Latour LL, et al. Comparison of MRI and CT for detection of acute intracerebral hemorrhage. JAMA. 2004;292(15):1823–30.
Charidimou A, Shoamanesh A. International META-MICROBLEEDS initiative. clinical relevance of microbleeds in acute stroke thrombolysis: comprehensive meta-analysis. Neurology. 2016;87(15):1534–41.
Tsivgoulis G, Zand R, Katsanos AH, Turc G, Nolte CH, Jung S, Cordonnier C, Fiebach JB, Scheitz JF, Klinger-Gratz PP, et al. Risk of symptomatic intracerebral hemorrhage after intravenous thrombolysis in patients with acute ischemic stroke and high cerebral microbleed burden: a meta-analysis. JAMA Neurol. 2016;73(6):675–83. https://doi.org/10.1001/jamaneurol.2016.0292.
Fiehler J, Albers GW, Boulanger JM, Derex L, Gass A, Hjort N, Kim JS, Liebeskind DS, Neumann-Haefelin T, Pedraza S, et al. Bleeding risk analysis in stroke imaging before thromboLysis (BRASIL): pooled analysis of T2*-weighted magnetic resonance imaging data from 570 patients. Stroke. 2007;38(10):2738–44.
Wardlaw J, Brazzelli M, Miranda H, Chappell F, McNamee P, Scotland G, Quayyum Z, Martin D, Shuler K, Sandercock P et al. An assessment of the cost-effectiveness of magnetic resonance, including diffusion-weighted imaging, in patients with transient ischaemic attack and minor stroke: a systematic review, meta-analysis and economic evaluation. Health Technol Assess. 2014;18(27):1–368, v–vi. https://doi.org/10.3310/hta18270.
Biesbroek JM, Niesten JM, Dankbaar JW, Biessels GJ, Velthuis BK, Reitsma JB, van der Schaaf IC. Diagnostic accuracy of CT perfusion imaging for detecting acute ischemic stroke: a systematic review and meta-analysis. Cerebrovasc Dis. 2013;35(6):493–501. https://doi.org/10.1159/000350200.
van der Hoeven EJ, Dankbaar JW, Algra A, Vos JA, Niesten JM, van Seeters T, van der Schaaf IC, Schonewille WJ, Kappelle LJ, Velthuis BK, et al. Additional diagnostic value of computed tomography perfusion for detection of acute ischemic stroke in the posterior circulation. Stroke. 2015;46(4):1113–5. https://doi.org/10.1161/STROKEAHA.115.008718.
Campbell BC, Yassi N, Ma H, Sharma G, Salinas S, Churilov L, Meretoja A, Parsons MW, Desmond PM, Lansberg MG, et al. Imaging selection in ischemic stroke: feasibility of automated CT-perfusion analysis. Int J Stroke. 2015;10(1):51–4. https://doi.org/10.1111/ijs.12381.
Albers GW, Goyal M, Jahan R, Bonafe A, Diener HC, Levy EI, Pereira VM, Cognard C, Cohen DJ, Hacke W, et al. Ischemic core and hypoperfusion volumes predict infarct size in SWIFT PRIME. Ann Neurol. 2016;79(1):76–89. https://doi.org/10.1002/ana.24543.
Gasparotti R, Grassi M, Mardighian D, Frigerio M, Pavia M, Liserre R, Magoni M, Mascaro L, Padovani A, Pezzini A. Perfusion CT in patients with acute ischemic stroke treated with intra-arterial thrombolysis: predictive value of infarct core size on clinical outcome. AJNR Am J Neuroradiol. 2009;30(4):722–7. https://doi.org/10.3174/ajnr.A1439.
Fang XK, Ni QQ, Schoepf UJ, Zhou CS, Chen GZ, Luo S, Fuller SR, De Cecco CN, Zhang LJ, Lu GM. Image quality, radiation dose and diagnostic accuracy of 70 kVp whole brain volumetric CT perfusion imaging: a preliminary study. Eur Radiol. 2016;26(11):4184–93. https://doi.org/10.1007/s00330-016-4225-6.
Corcuera-Solano I, McLellan AM, Doshi AH, Pawha PS, Tanenbaum LN. Whole-brain adaptive 70-kVp perfusion imaging with variable and extended sampling improves quality and consistency while reducing dose. AJNR Am J Neuroradiol. 2014;35(11):2045–51. https://doi.org/10.3174/ajnr.A4043.
Lin L, Bivard A, Levi CR, Parsons MW. Comparison of computed tomographic and magnetic resonance perfusion measurements in acute ischemic stroke: back-to-back quantitative analysis. Stroke. 2014;45(6):1727–32. https://doi.org/10.1161/STROKEAHA.114.005419.
Cho TH, Nighoghossian N, Mikkelsen IK, Derex L, Hermier M, Pedraza S, Fiehler J, Ostergaard L, Berthezene Y, Baron JC. Reperfusion within 6 hours outperforms recanalization in predicting penumbra salvage, lesion growth, final infarct, and clinical outcome. Stroke. 2015;46(6):1582–9. https://doi.org/10.1161/STROKEAHA.114.007964.
Drewer-Gutland F, Kemmling A, Ligges S, Ritter M, Dziewas R, Ringelstein EB, Niederstadt TU, Heindel W, Hesselmann V. CTP-based tissue outcome: promising tool to prove the beneficial effect of mechanical recanalization in acute ischemic stroke. Rofo. 2015;187(6):459–66. https://doi.org/10.1055/s-0034-1399189.
Ehrlich ME, Turner HL, Currie LJ, Wintermark M, Worrall BB, Southerland AM. Safety of computed tomographic angiography in the evaluation of patients with acute stroke: a single-center experience. Stroke. 2016;47(8):2045–50. https://doi.org/10.1161/STROKEAHA.116.013973.
Rai A, Cline B, Williams E, Carpenter J, Roberts T. Intravenous thrombolysis outcomes in patients presenting with large vessel acute ischemic strokes—CT angiography-based prognosis. J Neuroimaging. 2015;25(2):238–42. https://doi.org/10.1111/jon.12126.
Yoo AJ, Khatri P, Mocco J, Zaidat OO, Gupta R, Frei D, Lopes D, Shownkeen H, Berkhemer OA, Meyer D, et al. Impact of thrombus length on outcomes after intra-arterial aspiration thrombectomy in the THERAPY Trial. Stroke. 2017;48(7):1895–900. https://doi.org/10.1161/STROKEAHA.116.016253.
Torres-Mozqueda F, He J, Yeh IB, Schwamm LH, Lev MH, Schaefer PW, Gonzalez RG. An acute ischemic stroke classification instrument that includes CT or MR angiography: the Boston Acute Stroke Imaging Scale. AJNR Am J Neuroradiol. 2008;29(6):1111–7. https://doi.org/10.3174/ajnr.A1000.
Tan IY, Demchuk AM, Hopyan J, Zhang L, Gladstone D, Wong K, Martin M, Symons SP, Fox AJ, Aviv RI. CT angiography clot burden score and collateral score: correlation with clinical and radiologic outcomes in acute middle cerebral artery infarct. AJNR Am J Neuroradiol. 2009;30(3):525–31. https://doi.org/10.3174/ajnr.A1408.
Treurniet KM, Yoo AJ, Berkhemer OA, Lingsma HF, Boers AM, Fransen PS, Beumer D, van den Berg LA, Sprengers ME, Jenniskens SF, et al. Clot burden score on baseline computerized tomographic angiography and intra-arterial treatment effect in acute ischemic stroke. Stroke. 2016;47(12):2972–8.
Sillanpaa N, Saarinen JT, Rusanen H, Hakomaki J, Lahteela A, Numminen H, Elovaara I, Dastidar P, Soimakallio S. The clot burden score, the Boston Acute Stroke Imaging Scale, the cerebral blood volume ASPECTS, and two novel imaging parameters in the prediction of clinical outcome of ischemic stroke patients receiving intravenous thrombolytic therapy. Neuroradiology. 2012;54(7):663–72. https://doi.org/10.1007/s00234-011-0954-z.
Berkhemer OA, Jansen IG, Beumer D, Fransen PS, van den Berg LA, Yoo AJ, Lingsma HF, Sprengers ME, Jenniskens SF, Lycklama A, Nijeholt GJ, et al. Collateral status on baseline computed tomographic angiography and intra-arterial treatment effect in patients with proximal anterior circulation stroke. Stroke. 2016;47(3):768–76. https://doi.org/10.1161/STROKEAHA.115.011788.
Boers AM, Jansen IG, Berkhemer OA, Yoo AJ, Lingsma HF, Slump CH, Roos YB, van Oostenbrugge RJ, Dippel DW, van der Lugt A, et al. Collateral status and tissue outcome after intra-arterial therapy for patients with acute ischemic stroke. J Cereb Blood Flow Metab. 2017;37(11):3589–98. https://doi.org/10.1177/0271678X16678874.
Menon BK, Qazi E, Nambiar V, Foster LD, Yeatts SD, Liebeskind D, Jovin TG, Goyal M, Hill MD, Tomsick TA, et al. Differential effect of baseline computed tomographic angiography collaterals on clinical outcome in patients enrolled in the interventional management of stroke III trial. Stroke. 2015;46(5):1239–44. https://doi.org/10.1161/STROKEAHA.115.009009.
Klingebiel R, Siebert E, Diekmann S, Wiener E, Masuhr F, Wagner M, Bauknecht HC, Dewey M, Bohner G. 4-D imaging in cerebrovascular disorders by using 320-slice CT: feasibility and preliminary clinical experience. Acad Radiol. 2009;16(2):123–9. https://doi.org/10.1016/j.acra.2008.11.004.
van den Wijngaard IR, Boiten J, Holswilder G, Algra A, Dippel DW, Velthuis BK, Wermer MJ, van Walderveen MA. Impact of collateral status evaluated by dynamic computed tomographic angiography on clinical outcome in patients with ischemic stroke. Stroke. 2015;46(12):3398–404. https://doi.org/10.1161/STROKEAHA.115.010354.
van den Wijngaard IR, Wermer MJ, Boiten J, Algra A, Holswilder G, Meijer FJ, Dippel DW, Velthuis BK, Majoie CB, van Walderveen MA. Cortical venous filling on dynamic computed tomographic angiography: a novel predictor of clinical outcome in patients with acute middle cerebral artery stroke. Stroke. 2016;47(3):762–7. https://doi.org/10.1161/STROKEAHA.115.012279.
Bash S, Villablanca JP, Jahan R, Duckwiler G, Tillis M, Kidwell C, Saver J, Sayre J. Intracranial vascular stenosis and occlusive disease: evaluation with CT angiography, MR angiography, and digital subtraction angiography. AJNR Am J Neuroradiol. 2005;26(5):1012–21.
Al-Ali F, Berkhemer OA, Yousman WP, Elias JJ, Bender EN, Lingsma HF, van der Lugt A, Dippel DW, Roos YB, van Oostenbrugge RJ, et al. The Capillary Index Score as a marker of viable cerebral tissue: proof of Concept-The Capillary Index Score in the MR CLEAN (Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands) trial. Stroke. 2016;47(9):2286–91. https://doi.org/10.1161/STROKEAHA.116.013513.
Al-Ali F, Elias JJ, Tomsick TA, Liebeskind DS, Broderick JP. IMS Study Groups. Relative Influence of Capillary Index Score, revascularization, and time on stroke outcomes from the interventional management of stroke III trial. Stroke. 2015;46(6):1590–4. https://doi.org/10.1161/STROKEAHA.115.009066.
Mirasol RV, Bokkers RP, Hernandez DA, Merino JG, Luby M, Warach S, Latour LL. Assessing reperfusion with whole-brain arterial spin labeling: a noninvasive alternative to gadolinium. Stroke. 2014;45(2):456–61. https://doi.org/10.1161/STROKEAHA.113.004001.
Viallon M, Altrichter S, Pereira VM, Nguyen D, Sekoranja L, Federspiel A, Kulcsar Z, Sztajzel R, Ouared R, Bonvin C, et al. Combined use of pulsed arterial spin-labeling and susceptibility-weighted imaging in stroke at 3T. Eur Neurol. 2010;64(5):286–96. https://doi.org/10.1159/000321162.
Chng SM, Petersen ET, Zimine I, Sitoh YY, Lim CC, Golay X. Territorial arterial spin labeling in the assessment of collateral circulation: comparison with digital subtraction angiography. Stroke. 2008;39(12):3248–54. https://doi.org/10.1161/STROKEAHA.108.520593.
Lv Y, Margulies DS, Cameron Craddock R, Long X, Winter B, Gierhake D, Endres M, Villringer K, Fiebach J, Villringer A. Identifying the perfusion deficit in acute stroke with resting-state functional magnetic resonance imaging. Ann Neurol. 2013;73(1):136–40. https://doi.org/10.1002/ana.23763.
Amemiya S, Kunimatsu A, Saito N, Ohtomo K. Cerebral hemodynamic impairment: assessment with resting-state functional MR imaging. Radiology. 2014;270(2):548–55. https://doi.org/10.1148/radiol.13130982.
Khalil AA, Ostwaldt AC, Nierhaus T, Ganeshan R, Audebert HJ, Villringer K, Villringer A, Fiebach JB. Relationship between changes in the temporal dynamics of the Blood-oxygen-level-dependent signal and hypoperfusion in acute ischemic stroke. Stroke. 2017;48(4):925–31. https://doi.org/10.1161/STROKEAHA.116.015566.
Siegel JS, Snyder AZ, Ramsey L, Shulman GL, Corbetta M. The effects of hemodynamic lag on functional connectivity and behavior after stroke. J Cereb Blood Flow Metab. 2016;36(12):2162–76.
Christen T, Jahanian H, Ni WW, Qiu D, Moseley ME, Zaharchuk G. Noncontrast mapping of arterial delay and functional connectivity using resting-state functional MRI: a study in Moyamoya patients. J Magn Reson Imaging. 2015;41(2):424–30. https://doi.org/10.1002/jmri.24558.
Feng R, Badgeley M, Mocco J, Oermann EK. Deep learning guided stroke management: a review of clinical applications. J Neurointerv Surg. 2017. https://doi.org/10.1136/neurintsurg-2017-013355.
Lee EJ, Kim YH, Kim N, Kang DW. Deep into the brain: artificial intelligence in stroke imaging. J Stroke. 2017;19(3):277–85. https://doi.org/10.5853/jos.2017.02054.
Abedi V, Goyal N, Tsivgoulis G, Hosseinichimeh N, Hontecillas R, Bassaganya-Riera J, Elijovich L, Metter JE, Alexandrov AW, Liebeskind DS, et al. Novel screening tool for stroke using artificial neural network. Stroke. 2017;48(6):1678–81. https://doi.org/10.1161/STROKEAHA.117.017033.
Broderick JP, Palesch YY, Demchuk AM, Yeatts SD, Khatri P, Hill MD, Jauch EC, Jovin TG, Yan B, Silver FL, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013;368(10):893–903. https://doi.org/10.1056/NEJMoa1214300.
Ciccone A, Valvassori L, Nichelatti M, Sgoifo A, Ponzio M, Sterzi R, Boccardi E, SYNTHESIS Expansion Investigators. Endovascular treatment for acute ischemic stroke. N Engl J Med. 2013;368(10):904–13. https://doi.org/10.1056/NEJMoa1213701.
Kidwell CS, Jahan R, Gornbein J, Alger JR, Nenov V, Ajani Z, Feng L, Meyer BC, Olson S, Schwamm LH, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013;368(10):914–23. https://doi.org/10.1056/NEJMoa1212793.
• Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T, Guillemin F, THRACE investigators. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): a randomised controlled trial. Lancet Neurol. 2016; 15(11):1138–1147. https://doi.org/10.1016/s1474-4422(16)30177-6. THRACE is a randomized controlled clinical trial showing clinical benefit of mechanical thrombectomy in addition to intravenous tPA, without requiring ischemic core or penumbral assessments to determine treatment eligibility.
Al-Ajlan FS, Goyal M, Demchuk AM, Minhas P, Sabiq F, Assis Z, Willinsky R, Montanera WJ, Rempel JL, Shuaib A, et al. Intra-arterial therapy and post-treatment infarct volumes: insights from the ESCAPE randomized controlled trial. Stroke. 2016;47(3):777–81. https://doi.org/10.1161/STROKEAHA.115.012424.
Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, Davalos A, Majoie CB, van der Lugt A, de Miquel MA, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016;387(10029):1723–31. https://doi.org/10.1016/S0140-6736(16)00163-X.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Gerald T. Drocton, Michael D. Luttrull, Amna A. Ajam, and Xuan V. Nguyen each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Emergency Radiology.
Rights and permissions
About this article
Cite this article
Drocton, G.T., Luttrull, M.D., Ajam, A.A. et al. Emerging Trends in Emergent Stroke Neuroimaging. Curr Radiol Rep 6, 22 (2018). https://doi.org/10.1007/s40134-018-0282-8
Published:
DOI: https://doi.org/10.1007/s40134-018-0282-8