Abstract
Purpose of Review
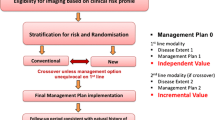
Simultaneous positron emission tomography/magnetic resonance was released few years ago and there is a (non-official) perspective of almost 100 scanners worldwide being installed until 2016. Despite the enormous marketing success for such an expensive and fine hybrid imaging tool, PET/MR is still seen primarily as a research tool. Currently this clinical validation process is more than necessary to justify the additional expenses in a world with increasing difficulties regarding health system reimbursement.
Recent Findings
The current PET/MR feasibility has been demonstrated with the published data so far in almost every body region, with great potential applications. The main fields of research in PET/MR are oncologic and neurologic, basically for two reasons: (1) because almost 90 % of PET/CT studies come from oncology; (2) and also because of the recent development of new medications and treatments for dementia, making PET/MR an important character in this new scenario. Inflammation has become the newest potential application, and will also be discussed further on.
Summary
In this article such potential clinical PET/MR applications are compiled and updated and will be thoroughly discussed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Positron emission tomography/magnetic resonance (PET/MR) offers a major breakthrough in diagnostic and molecular imaging, which enables a high-quality assessment of various groups of diseases, especially in oncologic, inflammatory, and neurologic fields. The synergism of the molecular information provided by PET and the high-resolution morphological imaging and functional data provided by MR allows an outstanding comprehensive evaluation of patients.
The currently available simultaneous PET/MR equipments are a result of extensive work on technology improvement. Efforts have been done to suit the requisite PET devices to the MR magnetic field, such as the photodetectors which are now based on silicon MR-compatible semiconductor material. Another essential overcoming comprised by a better timing resolution, time-of-flight capability, improved reconstruction, and post-processing algorithms provide a competitive diagnostic modality [1].
However, not only the technical development is necessary to optimize PET/MR use. An efficient workflow is of utmost relevance for the application of PET/MR in research and clinical routine. A concise exam protocol based on indication and an objective data visualization and analysis are just examples of the essential to achieve an optimal workup [2].
This paper aims to update the status of the clinical indications of PET/MR, summarizing the available data in the literature and pointing out the next research steps needed in three of the most important fields of molecular imaging: oncology, inflammation, and neurology.
Oncology
The major prospects of PET/MR systems in Oncology are to yield with concrete answers the various drawbacks currently provided by the imaging modalities. As a result of the integration of PET and MRI, both the superior soft-tissue contrast and the metabolic, functional, and biologic features provided by MRI—including advanced techniques and sequences—and PET may be achieved. This synergism of information inevitably would lead to increased diagnostic accuracy. Hence, local and systemic neoplastic diseases may profit of improved detection, evaluation, and therapy planning, especially in organs where CT scans deliver information of substandard quality.
Head and Neck Cancers
With higher spatial resolution and soft-tissue contrast, MR is arguably the best modality to depict local disease and T-status in head and neck cancers. It describes better than CT the extent and delineation of tumors and the involvement of surrounding structures, perineural spread, prevertebral fascia infiltration, and vessel’s wall damage. There are also fewer occult lesions in MR than in CT, and clear superiority of MR over CT in cases of dental implants owing to lower prevalence of artifacts and on clarifying uncertain lesions in patients subject to dramatic anatomic modifications by surgical procedures and radiotherapy, which often hamper PET/CT interpretation [3, 4, 5••].
The quality of MR image from PET/MR systems is considered as being of excellent quality, not poorer than that of conventional MR equipment. Multiparametric and quantitative features, such as spectroscopy, diffusion-weighted imaging, and dynamic contrast-enhanced imaging also reduce ambiguity from heterogeneous and continuously reshaping lesions, both at staging and after chemo and radiation therapy [5••, 6•].
Additionally, the SUVs of PET/MR and PET/CT appear to show great correlation [6•]. This results in the superimposed metabolic data from FDG also providing clues to reinforce the identification of subtle lesions or to strengthen the level of confidence when considering or ruling out the existence of viable lesions among inflammatory and post-treatment changes and complications [4]. This mutualism results in optimal pre- and post-therapy characterization, response evaluation, and recurrent disease identification. Consequently, recent studies have advocated the superiority of PET/MR over PET/CT for evaluation of tumor extent and characterization and local invasion assessment [3, 5••, 6•].
The superiority of PET/MR over MR alone and PET/CT in characterization of lymph node lesions is yet to be confirmed. As nodal staging plays a central role and correlates with patients’ prognosis, the potential superiority of PET/MR systems might fulfill important shortcomings not currently covered by PET/CT examinations. Although new PET/MR devices proved to have a superior sensitivity, it is important to highlight that there are still limitations on the evaluation of subcentimeter lymph nodes, since PET sensitivity is low for nodes smaller than 1 cm [3, 5••].
There are also evidences in literature suggesting that PET/MR might perform at least as effectively as PET/CT in suspected cervical occult tumors, which frequently manifest as metastases in cervical lymph nodes. The main potential superiority rely on better morphologic characterization of the suspected hypermetabolic foci, since MR systems overdo CT and reduce false positive studies caused by benign lesions. More robust data are necessary to further conclusions [5••].
The major known disputed queries regard distant metastases, especially to mediastinal nodes and lungs, which are satisfactory addressed by PET/CT systems, and bone lesions, whose whole-body analysis would be time costly [5••]. Another important issue, not yet established, is whether PET/MR studies accurately identify second or third primary tumors, relatively frequent among patients with head and neck cancers [5••].
Finally, efforts are being put to prove that PET/MR avoids the need for separate studies of PET/CT and MR, a common scenario in clinical practice, and that it delivers equal or greater diagnostic answers than both exams separately would provide. Current studies in the literature suggest that PET/MR is a promising instrument that might be able to replace PET/CT and MRI providing equivalent clinical answers in one single exam [4, 5••]. However, more researches with larger patient groups are still mandatory to improve protocols, delineate other possible additional drawbacks and indications for PET/MR in head and neck cancer.
Thyroid Cancer
Well-differentiated thyroid carcinoma management demands thyroidectomy along, in many cases, with radioiodine therapy. On follow-up, whether there is suspicion of relapse due to rising levels of thyroglobulin, identifying anatomic evidences is often mandatory, leading to the appropriate therapy [7].
However, traditional imaging investigation, such as ultrasound, often shows no abnormality. In turn, hybrid modalities like SPECT/CT and PET/CT frequently demonstrate sites of increased radioiodine or FDG uptake with no corresponding morphologic abnormality on CT, either because small lesions were missed or because of the limitations of the CT protocol, as it must be carried out without intravenous iodinated contrast, a contraindication to a possible further radionuclide therapy.
It has been proved that lesions not appreciable on CT images may be noticeable on MR images, except in cases of small pulmonary lesions. PET/MR imaging could not only bring the benefits of FDG regarding undifferentiated and poorly differentiated thyroid carcinoma, but also be useful on differentiated thyroid carcinoma and overcome 131I SPECT/CT, when performed with 124I, a positron emission tracer which is increasingly gaining ground. Thus, evidences support the superiority of PET/MR for pointing out metabolically active foci to morphologic correlates, increasing diagnostic certainty and reducing equivocal studies [8].
Lung Cancer
FDG-PET/CT is broadly regarded the gold standard for staging of non-small cell lung cancer (NSCLC). It presents high accuracy due to optimal morphologic features in the detection and delineation of the primary lung tumor, when acquired deep-inspiration breath-hold PET/CT of the thorax images. Also, identification of hypermetabolic distant metastases is a meaningful advantage [9, 10•, 11, 12•, 13••]. According to some recent data published, PET/MR using fast MR protocols does not improve diagnostic outcomes of the staging of NSCLC, mainly because MR images have significantly lower detection capability than CT, critically for lesions below 1 cm [12•, 13••].
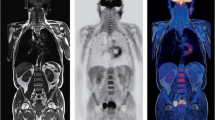
Nonetheless, due to the multiparametric nature of MRI, the replacement of CT by MRI is speculated to delivery profits to T staging of bigger lesions and to N staging [9, 12•]. The integration of DWI and very short echo time imaging leads to better evaluation of lung parenchyma (Fig. 1). As lung parenchyma T2* values are characteristically short, echo times of less than 1 ms ought to be used, enabling the identification of fibrosis and other treatment-related conditions that may increase the concentration of short T2 components and could mimic disease relapse and/or hinder diagnostic certainty [11, 14].
FDG PET/MR for primary staging of non-small cell adenocarcinoma. PET Coronal MIP shows a lung mass with bilateral mediastinal lymph nodes and multiple bone metastasis. Axial T1w Dixon, DWI (b = 800), and FDG-PET/MR show a lung mass in the superior left lobe apparently infiltrating the cortical of the second rib and two right secondary contralateral paratracheal lymph nodes. Axial T1w Dixon and FDG-PET/MR show a good correlation of bone uptake and a lytic lesion in humerus, right rib, and vertebral body. This case shows the good performance of PET/MR to stage lung cancer and to detect bone metastasis
Regarding mediastinal lymph node assessment, despite having a high negative predictive value, FDG-PET/CT possesses low positive predictive value [13••]. There are promising techniques which may establish a new level of quality in functional cancer staging in NSCLC patients, particularly DWI and T2-weighted sequences, which could improve the detection of nodal metastases, avoiding unnecessary surgical procedures [9, 10•, 11].
Lymphomas
FDG-PET/CT may be considered as a cornerstone in staging and response assessment of high-grade lymphomas, chiefly Hodgkin and diffuse large B cell non-Hodgkin lymphoma. Guidelines advocate its employment for staging, response assessment, and restaging purposes, thus, in many cases, yielding to high cumulative radiation exposure [15–17, 18•].
As there is no radiation exposure with MR exams, and given the large number of young patients, many likely to cure, there are huge research concerns on FDG-PET/MR as substitute for PET/CT in the assessment of lymphoma patients [15–17, 18•].
Albeit scarce literature available, limited and preliminary data show that PET/MR is feasible and provides satisfactory image quality [17, 18•]. Also, there are already promising signs, with high reported concordance with PET/CT findings [15–17].
Further, for mucosa-associated lymphoid tissue lymphomas, there are evidence supporting benefits of PET/MR over PET/CT, provided DWI is included in the protocol, given its higher mucosal lymphoid tissue sensitivity, which are handicapped both in PET and CT [18•].
More studies should be carried out in order to confirm data. PET/MR imaging could become an alluring alternative for staging, response assessment, and restaging offering significant reduction of radiation dose, which is attractive especially to pediatric patients and those subjected to several scans.
Gynecological Cancers
There is little debate that MR offers the best depiction of primary tumors and extent of soft-tissue disease in gynecological cancers, even tiny lesions. In turn, FDG-PET/CT is more reliable for assessing N and M status [19, 20••, 21, 22]. Hence, PET/MR is anticipated to be superior for detection, localization, staging, and restaging of uterine and ovarian cancer, offering the same results while avoiding multiple examinations (Fig. 2).
FDG PET/MR for follow-up of cervical cancer treated with surgery and radiotherapy. PET Coronal MIP shows activation of brown fat in the cervical and paravertebral regions as well as a focal uptake in the retrovesical space. Axial PET and FDG-PET/MR and sagittal FDG-PET/MR after injection of vaginal gel elegantly depict a local recurrence in the vaginal vault. This case shows the potential benefit of PET/MR to evaluate gynecological cancers
FDG-PET/MR T2w images are able to appraise myometrial invasion of endometrial cancers, parametrial and pelvic floor and walls involvement of cervical cancers and improved detection of uterine and ovarian lesions [19, 20••, 21]. There is also better estimation of nodal lesions, providing better selection of patients able to undergo lymphadenectomy [19]. DWI also allows higher detection of bone, liver, and peritoneum implants [23].
Prostate Cancer
MR is the best imaging method for the diagnosis and staging of prostate cancer due not only to higher soft-tissue contrast than CT, but also the value of functional sequences, such as DWI and perfusion [24].
FDG-PET has low sensitivity for prostate cancer, since there is little tracer accumulation in early and well-differentiated tumors. Also, urinary excretion causes artifacts that hamper imaging interpretation. Thus, FDG-PET/CT is a limited imaging tool for most of the patients with prostate cancer. Other tracers, such as 68Ga-PSMA, 18F-choline, and 11C-choline are more appropriate agents for this context [26•, 27].
PET/MR with DWI is a promising tool for pre-therapy assessment of prostate tumors, providing the best anatomical overview coupled with molecular parameters, and choline is the most studied tracer so far. 11C-choline PET/MR may improve the staging of prostate cancers not only showing tumor boundaries and adjacent organ invasion, but may also point out the best areas for biopsy sampling, providing more accurate Gleason scores and reducing sampling errors that might misclassify the disease, and ultimately interfere in the patient’s management (Fig. 3). The multiparametric features of PET/MR are also useful in identifying regions of benign prostatic hyperplasia, which may be misinterpreted as tumor due to its high uptake of 11C-choline [24, 25].
68Ga-DOTATATE PET/MR for investigation of a patient with NEM1 syndrome. Axial PET, non-ceCT, and PET/CT show two focal uptake in the body and tail of the pancreas without morphological correlation. Axial T2w-PROPELLER and PET/MR better correlate the pancreatic focal uptakes with two tiny hyperintense lesions in the body and tail of the pancreas, highly suspicious for neuroendocrine tumor. This case example denotes the higher soft-tissue contrast of PET/MR compared to PET/CT
For the diagnosis of recurrent prostate cancer, 68Ga-PSMA ligand is a very promising tracer, mainly in cases of biochemical recurrence, when there are still serious limitations when it comes to explain the origin of increasing levels of prostate-specific antigen (PSA). Conventional imaging often does not reveal any foci of disease [26•], making this new tracer an extremely attractive tool, with increasingly higher attention and popularity among referring urologists and oncologists.
68Ga-PSMA ligand PET/CT has been highly regarded as the best option to clarify prostate cancer metastases in biochemical recurrence, and PET/MR systems are considered to reduce pitfalls of PET/CT, such as uptake in ureter and bowel loops, which may lead to false positive results [27].
Further studies are needed to reveal the additional value of PET/MR imaging for prostate cancer and its potential to replace MR and PET alone for initial tumor staging.
Neuroendocrine Tumors
Neuroendocrine tumors (NET) often develop in gastrointestinal tract, and frequently present liver and nodal metastases [28–30]. Most of the NET presents low avidity to FDG, but high somatostatin receptor expression, which depends on tumor proliferation index (as higher tumor Ki-67 and consequently lower tumor differentiation, higher FDG uptake, and lower somatostatin expression) [30]. 68Ga somatostatin ligand tracers are already gaining ground, and some advocate that PET/MR with those tracers may surpass PET/CT [28, 29].
There are advantages of MR over CT when it comes to evaluation of hepatic and pancreatic lesions, and providing the best anatomic characterization to provide better surgical planning and depiction or resectability (Fig. 4). MR functional parameters might also be valuable tools to aggregate to the molecular data and provide response and recurrence information [28–30].
18F-Choline PET/MR for whole-body staging of prostate cancer. PET Coronal MIP, high-resolution T2w transverse plane, axial DWI (b = 700), and axial 18F-Choline PET/MR show a nodule in the anterior midgland of the peripheral zone on the right side with restricted diffusion and focal choline uptake suggestive of primary prostatic adenocarcinoma. Additionally, several focal uptakes in the central gland are evinced, corresponding to Benign Prostatic Hyperplasia as observed in axial T2w sequence as an “organized chaos” in the transition zone. A normal-sized left-side deep inguinal lymph node is also depicted, with very faint choline uptake, more likely to be inflammatory. This example shows the synergism of PET and MR to differentiate benign and malignant processes.
(This case is a courtesy of Irene Burger, MD from University Hospital of Zurich)
There are few concrete studies performed hitherto, and the field is arguably open to further researches.
Pediatric
As previously mentioned, PET/MR is a very attractive alternative to PET/CT in pediatric, because of the relevant reduction of radiation burden of about 50 –75 %, which becomes more impacting when multiple repeated examinations are required. This could also justify turning PET/MR into the imaging modality of choice for evaluation of pregnant patients likewise [15–18•, 31–33]
PET/MR holds the advantage of the multiparametric characterization of diseases and typically helps reducing the number of imaging studies.
The pediatric population may benefit of PET/MR particularly in oncologic and neurologic diseases, but also in the diagnosis of infectious or inflammatory processes. In oncology, assessment of lymphoma, primary bone tumors, sarcoma, neuroblastoma, and NET stand among the most relevant indications. In neuroimaging, brain tumors and epilepsy are the most important applications. Fever and inflammation of unknown origin, musculoskeletal inflammation, inflammatory bowel disease, and detection of neuroinflammation are other important clinical entities that might benefit of PET/MR [31–33].
Assessing N and M Staging
Besides the various aforementioned advantages of PET/MR regarding T-status evaluation for each group of cancers, which typically display the MR functional imaging techniques as element for potential applications, there are correspondingly possible improvement fields for PET/MRI as regards N and M staging evaluation [34]. In general, MR is typically superior to CT for characterization of metastases in the bone marrow, liver, and brain, although CT is superior for the diagnosis of small lung lesions [35–42].
N Staging
The presence of nodal involvement must be accurately identified as it is pivotal for the selection of therapy modality. Current approach to the discrimination between benign and malignant nodes still leans on size, shape, and glycolytic metabolism of a lymph node, all of them lacking specificity. Nodal status characterization is thought to be optimized with the merger of PET with functional MR imaging techniques, such as ultrasmall superparamagnetic iron oxide contrast agent (USPIO)-enhanced MR imaging [34].
USPIO is a rising contrast agent which might support the recognition of neoplastic nodal involvement independent of lymph nodes size, shape, and glycolytic metabolism. USPIO-enhanced MRI mechanism relies on the capacity of normal lymph nodes of accumulate USPIO agent by macrophages, while metastatic lymph nodes do not. A meta-analysis revealed that USPIO-enhanced MRI is superior to non-enhanced MRI for diagnosis of lymph node metastases. Thus, it would provide an additional tool to improve diagnostic accuracy of PET/MR examinations, alongside hypermetabolism and lymph node enlargement [34, 40, 42].
M Staging: Bone Metastases
In the assessment of bone metastases, preliminary data show that PET/MR achieves better results than PET/CT using a T1-weighted turbo spin-echo sequence. Furthermore, DWI allows detection of still more bone marrow metastases than does contrast-enhanced MR imaging [37–42].
M staging: Liver Metastases
With respect to the diagnosis of liver metastases, it is well known that MR is preferable to CT, and superiority of PET/MR is achieved in lesions without FDG avidity. MR presents higher soft-tissue contrast and comprehensive data from hepatobiliary-specific contrast agents, which improve hepatic lesion characterization, and DWI. Jointly, they offer higher detection rate and diagnostic confidence than PET/CT, mainly for subcentimeter lesions. There are studies in literature showing significantly higher diagnostic results in comparison to contrast-enhanced PET/CT [30, 35, 36, 39–42].
M Staging: Pulmonary Metastases
PET/MR performs poorly for FDG-negative pulmonary lesions, since MR achieves substandard performances with small lesions, lacking sensitivity in comparison to CT. Because of that, additional chest CT is still required when evaluating a patient with PET/MR [40, 42]. It is likely that the development of new sequences using ultrashort echo time will overcome this limitation of MR [43].
M Staging: Brain Metastases
Prompt diagnosis of brain metastases has been shown to improve survival, local control, and quality of life. Current data indicate that PET/CT identifies only 50–70 % of known presumably symptomatic brain metastases. PET/MR, in turn, is expected to deliver results, since CT lacks accuracy and FDG-PET has major drawbacks due to the high physiological uptake of FDG along the gray matter. Therefore, PET/MR with DWI and contrast-enhanced imaging should be considered, since the rates of detection of brain metastases are significantly higher, leading to important changes in management [41, 42].
Radiation Therapy Planning
Apart from all of its potential supplementary profit for diagnosis, integrated PET/MR systems may also enable individualized radiotherapy planning through refined target volume definition and gross tumor volume delineation [44–47].
Some studies have already defended its employment for brain [44], head and neck and cervical cancers [45], and soft-tissue sarcomas [46]. Other study suggested that further investigation may prove its application in prostate cancer [48••]. Delineation of tumor volumes and target lesions by combined PET/MR data is a promising field for researches [47].
Inflammation
PET/MR imaging might present a breakthrough in a wide considerable group of inflammatory diseases, since MR provides superior soft-tissue contrast. Also, DWI, through measurement of diffusivity of water molecules across tissues, alongside with FDG uptake, is thought to enhance depiction of inflammation in relevant anatomic sites suboptimally evaluated by PET/CT [49, 50].
Inflammation is typically followed by immune cell infiltration, augmented blood flow and vascular permeability, and protein transudation in the inflammatory site. FDG targets inflammatory processes because of the metabolic changes mediated by the immune cells that lead to higher glucose consumption [48••]. Furthermore, the microenvironment is led to structural adaptation, such as thrombosis and wall thickening [48••], which are much better portrayed by MR than by CT [49, 50]. Thus, PET/MR imaging is noticeably precise for evaluating inflammatory conditions such as vasculitis and neuropathy [50, 51].
In patients with inflammatory bowel disease, PET/MR is able to evaluate extension and depict lesions before surgery, and appears to give more data than PET/CT. PET/MR is the more accurate imaging tool in the assessment of crucial information, such as presence of extraluminal disease, distant disease localization, fibrotic changes, and the correct differentiation between inflammation and fibrosis. These answers contribute immensely to the clinical management of patients [52].
In musculoskeletal conditions, FDG is highly sensitive to inflammatory changes in the articulations and within the synovial tissue. Additionally, the exquisite soft-tissue contrast provided by MR provides outstanding structural assessment of bone marrow, muscles, tendons, ligaments, cartilage, joint capsules, and fat. This way, the overlapped data are complementary and may in all likelihood be useful to detect and characterize conditions such as osteomyelitis and complications of diabetic foot, both on diagnosis and response assessment [49, 50].
Neurology
There is a myriad of inexhaustible possibilities of PET/MR application in neuroimaging. Neurodegenerative, ischemic and vascular, oncologic, traumatic, psychiatric and behavioral, epilepsy, and aging-related conditions comprise the endless array of diseases to which PET/MR has potential to provide comprehensive multidimensional, multiparametric, structural, and functional data of the central nervous system [53, 54•, 55–58, 59••, 60, 61••, 62–64].
Angiogenesis, gene transfer, function, and migration of transplanted cells are some of the novel fields that PET probes may analyze, in conjunction to the various functional features of MR imaging. The possibilities are so broad that other fields are not even known, devised, and conceived [59••].
The MR properties allow depiction of morphology, vascular anatomy through magnetic resonance angiography (MRA), water kinetics in tissue (DWI), cerebral perfusion patterns (PWI, DCE-MRI), local accumulation of metabolites in tissues (MR spectroscopy for 1H, 13C, 23Na, 31P), cerebral regional functional activation (fMRI), analysis of cerebral fiber tracts (diffusion tensor imaging—DTI—and fiber tracking), patterns of oxygen consumption (17O and BOLD) and cells migration (Fe labeling), among others [59••].
PET probes feature brain flow (H 152 O), metabolism (through FDG), blood volume (C15O), oxygen consumption (15O), vascular permeability (with labeled amino acids), nucleic acid synthesis (with fluorothymidine), neurotransmitter evaluation (e.g., DOPA), receptor assessment (e.g., raclopride), angiogenesis estimation (e.g., 18F-RGB), evaluation of the distribution, and kinetics of tracers and drugs and enzymatic activity in transfected cells [59••].
This means that there is possibility of real-time imaging of huge amounts of complementary information. New techniques may demonstrate intricate local functional impairment in neurodegenerative and autoimmune diseases even before clinical symptoms are apparent. It may become possible to explore and better understand detailed structure and mechanisms of cerebral substructures which play important roles in behavior and cognition, study individual cluster of subcortical nuclei, and quantify their different pathways and metabolic cascades, most of them until recently only possible with in vitro or histologic studies [53, 54•, 55, 59••]. Another potential fields are movement disorders and neurodegenerative diseases.
Dementia and Other Neurodegenerative Diseases
MR has being widely used in clinical practice to evaluate an array of neurodegenerative diseases such as dementias, movement disorders, autoimmune conditions, and prionic diseases, whether to specify typical patterns or to exclude other etiologies [54•, 55].
PET can provide early information of neuronal damage, through FDG and newer, more specific PET tracers, such as probes targeting β-amyloid peptides or dopaminergic receptors. Many biomarkers have emerged recently, addressing different types of neurodegenerative diseases with patterns of imaging abnormalities. Thence, they have aided the improvement of early detection and differentiation of diverse clinical entities [53, 54•].
The integration of PET and MR tends to ameliorate the scenario of early differential diagnosis, providing a number of anatomic and biomarker answers demanded toward specific diagnoses in a one stop shop. There is already evidence in the literature to support this concept. Emerging PET radiopharmaceuticals, such as probes which can bind to tau- or α-synuclein aggregates, alongside recent MR techniques, broaden the yield of PET/MR to image dementias [53, 54•], Parkinson disease, and other neurodegenerative disorders. Furthermore, the system can potentially be used in basic drug testing research of neurodegenerative diseases and anti-neurodegeneration [53, 54•, 59••].
Results obtained so far are encouraging, as the highest ability of differentiation of dementia subtypes and differential diagnoses of neurodegenerative disorders are being reported. The next steps are larger researches and incorporation of the technology to clinical routine [53].
Epilepsy
PET/MR is potentially superior to PET/CT since MR is superior to CT [56–58], and the alignment of FDG-PET and MR information have great impact in the pre-surgical assessment of patients with refractory seizures [58].
Epilepsy surgery is a therapy possibility for patients with focal onset seizures refractory to clinical management. Focal resective epilepsy procedures lean on removing epileptogenic lesions identified on imaging exams. When no focus is encountered, the surgical outcomes decrease [56–58].
Typically, MR is the first exam to be carried out to detect a potential epileptogenic lesion. Advanced MR techniques have arisen, improving detection, such as susceptibility-weighted imaging (SWI), spectroscopy, volumetric analysis, diffusion tensor imaging, arterial spin labeling, and BOLD (blood oxygen-level dependent) [58].
However, as MR not always locates a lesion, FDG PET has been applied to afford additional information and identify functionally epileptogenic foci that are currently used in epilepsy surgery planning [56–58].
With the advent of PET/MR, there are increased diagnostic answers and identification of more and smaller potential epileptic foci. This might be due to the advantage of co-registration and concurrent analysis of structural and functional inputs [56–58].
Hence, non-diagnostic scans are minimized with the superimposed data and detection of subtle changes, such as cortical dysplasia, is enhanced. Studies show that the majority of those newly identified lesions are clinically significant and congruent with EEG results [56–58].
Neoplasms
MR is currently the method of choice for glioma imaging, despite of its shortcomings [60, 61••, 62–66]. Depiction of the boundaries of infiltrating brain tumors along white matter tracts, estimation of tumor grade, biopsy guidance, and post-therapy evaluation are the major handicaps of the method [60, 62, 64–66].
Thus, lining up anatomic and biologic information could be essential for biopsy, treatment planning, and follow-up evaluation. There are several sequences in PET/MR which can be used to assess gliomas.
Among morphological sequences, the most important are FLAIR and T1-weighted images after gadolinium injection, which enable the assessment of tumor boundaries and adjacent structure invasion [62]. Regarding functional sequences, MR perfusion and rCBV and DWI allow appraisement of biologic features of gliomas. Intravoxel incoherent motion (IVIM) imaging helps differentiating high-grade from low-grade gliomas [61••].
All of these information can be integrated with PET information, and the most promising PET tracers are those related to nucleic acid synthesis (FLT), labeled amino acids (18F-fluoro-ethyl-tyrosine—FET), and neurotransmitter evaluation (DOPA). PET information from those tracers might be evaluated both in static and dynamic fashions. In other words: only data on uptake, such as SUV or tumor/brain ratio, or different measurements of the lesion tracer concentration along time, generate wash-in/wash-out graphs [62–64].
There are various application to those data, since for the detection of high-grade brain tumors, differentiating high- from low-grade glioma, discriminating neoplastic lesions from non-neoplastic diseases, evaluating recurrence versus pseudoprogression and radionecrosis (Fig. 5), prognostication, and identifying of higher-risk patients. The issue is a major field of future study and may unveil new paradigms in neuroimaging.
Figure: 50-year-old male with left frontal Anaplastic Astrocytoma showed in MR images a T1w contrast media (upper row) and FLAIR (lower row). Three years after tumor resection, 18F-FET-PET/MR images b demonstrated an area of local recurrence in the posterior margin of the resection cavity, but note that the 18F-FET uptake area of the PET is bigger than the contrast media enhancement in the MR component. The recurrence was resected, however the surgeon removed only the nodular enhancement of the MR component. First recurrence surgery control with 18F-FET-PET/MR (4 months later) c showed an elongated enhancement in the MR with 18F-FET uptake also bigger in the posterior resection margin compatible with leftover local recurrence. Simultaneous 18F-FET-PET/MR could play a role in better diagnostic and surgery planning of gliomas recurrences.
(This case is a courtesy of Martin Huellner, MD from University Hospital of Zurich)
Conclusion
Although its predominant use is as a research tool, the new simultaneous PET/MR system has the potential to be used as the preferred clinical imaging modality for many different diseases. In oncology, neoplasias that are currently evaluated by PET/CT and MR tend to be naturally transferred to the one stop shop PET/MR. Besides, several indications might benefit from a PET/MR examination, considering the low radiation exposure, especially children, pregnant women, and patients under oncologic follow-up. For evaluation of inflammatory processes, the combination of metabolic data with morphological changes may benefit for the depiction of tiny soft-tissue abnormalities and this multiparametric analysis aids relevant information for patient management. Neuroimaging might be the most attractive use for PET/MR, since the brain is constantly changing from a functional perspective and the possibility to correlate anatomy and activity at the same time is not only convenient, but also promising. The use of several MR sequences and PET probes opens a huge perspective in the assessment of the molecular aspects of neurodegenerative diseases, epilepsy, and brain tumors. Thus, PET/MR might represent the next generation of molecular and hybrid imaging and an encouraging diagnostic modality for clinical routine.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
de Galiza Barbosa F, Delso G, Ter Voert EE, et al. Multi-technique hybrid imaging in PET/CT and PET/MR: what does the future hold? Clin Radiol. 2016;71(7):660–72.
de Barbosa FG, von Schulthess G, Veit-Haibach P. Workflow in simultaneous PET/MRI. Semin Nucl Med. 2015;45(4):332–44.
Park JT, Roh JL, Kim JS, et al. 18F FDG PET/CT versus CT/MR imaging and the prognostic value of contralateral neck metastases in patients with head and neck squamous cell carcinoma. Radiology. 2016;279(2):481–91.
Varoquaux A, Rager O, Dulguerov P, et al. Diffusion-weighted and PET/MR Imaging after radiation therapy for malignant head and neck tumors. Radiographics. 2015;35(5):1502–27.
•• Queiroz MA, Huellner MW. PET/MR in cancers of the head and neck. Semin Nucl Med. 2015;45(3):248–65. Complete and comprehensive review of PET/MR applications in cancers of the head and neck.
• Huang SH, Chien CY, Lin WC, et al. A comparative study of fused FDG PET/MRI, PET/CT, MRI, and CT imaging for assessing surrounding tissue invasion of advanced buccal squamous cell carcinoma. Clin Nucl Med. 2011;36(7):518–25. Comparison of current most important imaging methods for head and neck cancers.
Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016;26(1):1–133.
Nagarajah J, Jentzen W, Hartung V, et al. Diagnosis and dosimetry in differentiated thyroid carcinoma using 124I PET: comparison of PET/MRI vs PET/CT of the neck. Eur J Nucl Med Mol Imaging. 2011;38(10):1862–8.
Plathow C, Aschoff P, Lichy MP, et al. Positron emission tomography/computed tomography and whole-body magnetic resonance imaging in staging of advanced nonsmall cell lung cancer—initial results. Investig Radiol. 2008;43:290–7.
• Kim YN, Yi CA, Lee KS, et al. A proposal for combined MRI and PET/CT interpretation criteria for preoperative nodal staging in non-small-cell lung cancer. Eur Radiol. 2012;22(7):1537–15. Interesting approach on nodal staging for lung cancer, proposing combined criteria which may facilitate surgical planning.
Heusch P, Köhler J, Wittsack HJ, et al. Hybrid [(18)F]-FDG PET/MRI including non-Gaussian diffusion-weighted imaging (DWI): preliminary results in nonsmall cell lung cancer (NSCLC). Eur J Radiol. 2013;82:2055–60.
• Schwenzer NF, Schraml C, Müller M, et al. Pulmonary lesion assessment: comparison of whole-body hybrid MR/PET and PET/CT imaging-pilot study. Radiology. 2012; 264:551–8. One of the first studies addressing the major differences between PET/MR and PET/CT on pulmonary lesion assessment.
•• Huellner MW, de Galiza Barbosa F, Husmann L, et al. TNM staging of non-small cell lung cancer: comparison of PET/MR and PET/CT. J Nucl Med. 2016;57(1):21–6. Recent study which evaluates lung cancer staging with PET/CT and PET/MR and portraits potential shortcomings of PET/MR systems.
Mulkern R, Haker S, Mamata H, et al. Lung parenchymal signal intensity in MRI: a technical review with educational aspirations regarding reversible versus irreversible transverse relaxation effects in common pulse sequences. Concepts Magn Reson. 2014;43A(2):29–53.
Buchbender C, Heusner TA, Lauenstein TC, et al. Oncologic PET/MRI, part 2: bone tumors, soft-tissue tumors, melanoma, and lymphoma. J Nucl Med. 2012;53(8):1244–52.
Herrmann K, Queiroz M, Huellner MW, et al. Diagnostic performance of FDG-PET/MRI and WB-DW-MRI in the evaluation of lymphoma: a prospective comparison to standard FDG-PET/CT. BMC Cancer. 2015;23(15):1002.
Platzek I, Beuthien-Baumann B, Langner J, et al. PET/MR for therapy response evaluation in malignant lymphoma: initial experience. MAGMA. 2013;26:49–55.
• Giraudo C, Raderer M, Karanikas G, et al. 18F-Fluorodeoxyglucose positron emission tomography/magnetic resonance in lymphoma: comparison with 18F-fluorodeoxyglucose positron emission tomography/computed tomography and with the addition of magnetic resonance diffusion-weighted imaging. Invest Radiol. 2016;51(3):163–9. Study evaluating PET/CT and PET/MR assessment of nodal and extranodal involvement in patients with Hodgkin and non-Hodgkin lymphomas, presenting the potential capabilities of DWI.
Nakajo K, Tatsumi M, Inoue A, et al. Diagnostic performance of fluorodeoxyglucose positron emission tomography/magnetic resonance imaging fusion images of gynecological malignant tumors: comparison with positron emission tomography/computed tomography. Jpn J Radiol. 2010;28(2):95–100.
•• Queiroz MA, Kubik-Huch RA, Hauser N, et al. PET/MRI and PET/CT in advanced gynaecological tumours: initial experience and comparison. Eur Radiol. 2015;25(8):2222–30. Detailed and comprehensive analysis providing comparison of PET/MR and PET/CT for evaluation of gynaecological cancers and highlighting the potential benefits of each modality.
Siegel CL, Andreotti RF, Cardenes HR, et al. American College of Radiology. ACR appropriateness criteria pretreatment planning of invasive cancer of the cervix. J Am Coll Radiol. 2012;9(6):395–402.
Kitajima K, Murakami K, Sakamoto S, et al. Present and future of FDG-PET/CT in ovarian cancer. Ann Nucl Med. 2011;25(3):155–64.
Kitajima K, Tanaka U, Ueno Y, et al. Role of diffusion weighted imaging and contrast-enhanced MRI in the evaluation of intrapelvic recurrence of gynecological malignant tumor. Plos One. 2015;10(1):e0117411.
Park H, Wood D, Hussain H, et al. Introducing parametric fusion PET/MRI of primary prostate cancer. J Nucl Med. 2012;53(4):546–51.
Afshar-Oromieh A, Haberkorn U, Schlemmer HP, et al. Comparison of PET/CT and PET/MRI hybrid systems using a 68 Ga-labelled PSMA ligand for the diagnosis of recurrent prostate cancer: initial experience. Eur J Nucl Med Mol Imaging. 2014;41(5):887–97.
• How Kit N, Dugué AE, Sevin E, et al. Pairwise comparison of 18F-FDG and 18F-FCH PET/CT in prostate cancer patients with rising PSA and known or suspected second malignancy. Nucl Med Commun. 2016;37(4):348–55. Analysis of the feasibility of promising PET/MRI system for prostate cancer with highly relevant PSMA tracer.
Bluemel C, Krebs M, Polat B, et al. 68Ga-PSMA-PET/CT in patients with biochemical prostate cancer recurrence and negative 18F-choline-PET/CT. Clin Nucl Med. 2016;41(7):515–21.
Beiderwellen KJ, Poeppel TD, Hartung-Knemeyer V, et al. Simultaneous 68Ga-DOTATOC PET/MRI in patients with gastroenteropancreatic neuroendocrine tumors: initial results. Investig Radiol. 2013;48(5):273–9.
Wulfert S, Kratochwil C, Choyke PL, et al. Multimodal imaging for early functional response assessment of (90)Y-/(177)Lu-DOTATOC peptide receptor targeted radiotherapy with DW-MRI and (68)Ga-DOTATOC-PET/CT. Mol Imaging Biol. 2014;16(4):586–94.
Armbruster M, Zech CJ, Sourbron S, et al. Diagnostic accuracy of dynamic gadoxetic-acid-enhanced MRI and PET/CT compared in patients with liver metastases from neuroendocrine neoplasms. J Magn Reson Imaging. 2014;40(2):457–66.
Schäfer JF, Gatidis S, Schmidt H, et al. Simultaneous whole-body PET/MR imaging in comparison to PET/CT in pediatric oncology: initial results. Radiology. 2014;273(1):220–31.
Purz S, Sabri O, Viehweger A, et al. Potential pediatric applications of PET/MR. J Nucl Med. 2014;55(Supplement 2):32S–9S.
Hirsch FW, Sattler B, Sorge I, et al. PET/MR in children: initial clinical experience in paediatric oncology using an integrated PET/MR scanner. Pediatr Radiol. 2013;43:860–75.
Wu L, Cao Y, Liao C, Huang J, et al. Diagnostic performance of USPIO-enhanced MRI for lymph-node metastases in different body regions: a meta-analysis. Eur J Radiol. 2011;80(2):582–9.
Yong TW, Yuan ZZ, Jun Z, et al. Sensitivity of PET/MR images in liver metastases from colorectal carcinoma. Hell J Nucl Med. 2011;14(3):264–8.
Donati OF, Hany TF, Reiner CS, et al. Value of retrospective fusion of PET and MR images in detection of hepatic metastases: comparison with 18F-FDG PET/CT and Gd-EOB-DTPA-enhanced MRI. J Nucl Med. 2010;51(5):692–9.
Samarin A, Hüllner M, Queiroz MA, et al. 18F-FDG-PET/MR increases diagnostic confidence in detection of bone metastases compared with 18F-FDG-PET/CT. Nucl Med Commun. 2015;36(12):1165–73.
Eiber M, Takei T, Souvatzoglou M, et al. Performance of whole-body integrated 18F-FDG PET/MR in comparison to PET/CT for evaluation of malignant bone lesions. J Nucl Med. 2013;55:191–7.
Laurent V, Trausch G, Bruot O, et al. Comparative study of two whole-body imaging techniques in the case of melanoma metastases: advantages of multi-contrast MRI examination including a diffusion-weighted sequence in comparison with PET-CT. Eur J Radiol. 2010;75(3):376–83.
Thomson V, Pialat JB, Gay F, et al. Whole-body MRI for metastases screening: a preliminary study using 3D VIBE sequences with automatic subtraction between noncontrast and contrast enhanced images. Am J Clin Oncol. 2008;31(3):285–92.
Kitajima K, Nakamoto Y, Okizuka H, et al. Accuracy of whole-body FDG-PET/CT for detecting brain metastases from non-central nervous system tumors. Ann Nucl Med. 2008;22(7):595–602.
Melsaether AN, Raad RA, Pujara AC, et al. Comparison of whole-body 18F FDG PET/MR imaging and whole-body 18F FDG PET/CT in terms of lesion detection and radiation dose in patients with breast cancer. Radiology. 2016;281(1):193–202.
Burris NS, Johnson KM, Larson PE, et al. Detection of small pulmonary nodules with ultrashort echo time sequences in oncology patients by using a PET/MR system. Radiology. 2016;278(1):239–46.
Thorwarth D, Muller AC, Pfannenberg C, et al. Combined PET/MR imaging using (68)Ga-DOTATOC for radiotherapy treatment planning in meningioma patients. Recent Results Cancer Res. 2013;194:425–39.
Zhang S, Xin J, Sun H, et al. Accuracy of PET/MR image coregistration of cervical lesions. Nucl Med Commun. 2016;37(6):609–15.
Zhang X, Chen YL, Lim R, et al. Synergistic role of simultaneous PET/MRI-MRS in soft tissue sarcoma metabolism imaging. Magn Reson Imaging. 2016;34(3):276–9.
Leibfarth S, Eckert F, Welz S, et al. Automatic delineation of tumor volumes by co-segmentation of combined PET/MR data. Phys Med Biol. 2015;60(14):5399–412.
•• Gialleonardo VD, Wilson DM, Keshari KR. The potential of metabolic imaging. Semin Nucl Med. 2016;46(1):28–39. Interesting and broad review of basic concepts of metabolic imaging and current and potential applications on hybrid imaging.
Miese F, Scherer A, Ostendorf B, et al. Hybrid 18F- FDG PET-MRI of the hand in rheumatoid arthritis: initial results. Clin Rheumatol. 2011;30(9):1247–50.
Nawaz A, Torigian DA, Siegelman ES, et al. Diagnostic performance of FDG-PET, MRI, and plain film radiography (PFR) for the diagnosis of osteomyelitis in the diabetic foot. Mol Imaging Biol. 2010;12(3):335–42.
White JA, Rajchl M, Butler J, et al. Active cardiac sarcoidosis: first clinical experience of simultaneous positron emission tomography-magnetic resonance imaging for the diagnosis of cardiac disease. Circulation. 2013;127:e639–41.
Pellino G, Nicolai E, Catalano OA, et al. PET/MR Versus PET/CT imaging: impact on the clinical management of small-Bowel Crohn’s disease. J Crohns Colitis. 2016;10(3):277–85.
Drzezga A, Barthel H, Minoshima S, et al. Potential clinical applications of PET/MR imaging in neurodegenerative diseases. J Nucl Med. 2014;55(Supplement 2):47S–55S.
• Barthel H, Schroeter ML, Hoffmann KT, et al. PET/MR in dementia and other neurodegenerative diseases. Semin Nucl Med. 2015;45(3):224–33. Paper featuring insights on multimodality neuroimaging in various diseases.
Dukart J, Mueller K, Horstmann A, et al. Combined evaluation of FDG-PET and MRI improves detection and differentiation of dementia. Plos One. 2011;6(3):e18111.
Won HJ, Chang KH, Cheon JE, et al. Comparison of MR imaging with PET and ictal SPECT in 118 patients with intractable epilepsy. AJNR Am J Neuroradiol. 1999;20(4):593–9.
Salamon N, Kung J, Shaw SJ, et al. FDG-PET/MRI coregistration improves detection of cortical dysplasia in patients with epilepsy. Neurology. 2008;71(20):1594–601.
Shin HW, Jewells V, Sheikh A, et al. Initial experience in hybrid PET-MRI for evaluation of refractory focal onset epilepsy. Seizure. 2015;31:1–4.
•• Heiss WD. The potential of PET/MR for brain imaging. Eur J Nucl Med Mol Imaging. 2009;36(Suppl 1):S105–S112. Provides extensive analysis of potentials advantages of PET/MR systems for gliomas.
Goldberg MF, Chawla S, Alavi A, et al. PET and MRI imaging of brain tumors. PET Clin. 2008;3(3):293–315.
•• Togao O, Hiwatashi A, Yamashita K, et al. Differentiation of high-grade and low-grade diffuse gliomas by intravoxel incoherent motion MR imaging. Neuro Oncol. 2016;18(1):132–41. Illustrates new and promising techniques which may change evaluation of brain tumors.
Hutterer M, Nowosielski M, Putzer D, et al. [18F]-fluoro-ethyl-L-tyrosine PET: a valuable diagnostic tool in neuro-oncology, but not all that glitters is glioma. Neuro Oncol. 2013;15(3):341–51.
Pöpperl G, Kreth FW, Herms J, et al. Analysis of 18F-FET PET for grading of recurrent gliomas: is evaluation of uptake kinetics superior to standard methods? J Nucl Med. 2006;47(3):393–403.
Jansen NL, Suchorska B, Wenter V, et al. Dynamic 18F-FET PET in newly diagnosed astrocytic low-grade glioma identifies high-risk patients. J Nucl Med. 2014;55(2):198–203.
Cruz LC, Sorensen AG. Diffusion tensor magnetic resonance imaging of brain tumors. Magn Reson Imaging Clin N Am. 2006;14(2):183–202.
Boss A, Kolb A, Hofmann M, et al. Diffusion tensor imaging in a human PET/MR hybrid system. Investig Radiol. 2010;45(5):270–4.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Rafael Fernandes Nunes, Felipe de Galiza Barbosa, and Marcelo A. Queiroz each declare no potential conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on PET/CT Imaging.
Rights and permissions
About this article
Cite this article
Nunes, R.F., de Galiza Barbosa, F. & Queiroz, M.A. Hybrid PET/MR: Updated Clinical Use and Potential Applications. Curr Radiol Rep 4, 61 (2016). https://doi.org/10.1007/s40134-016-0191-7
Published:
DOI: https://doi.org/10.1007/s40134-016-0191-7