Abstract
Glomerular filtration rate (GFR) is the most important measure of kidney function used for chronic kidney disease screening, dosing medications, and following kidney disease progression. Gold standard GFR measurement is inulin clearance; however, GFR is most commonly measured by plasma disappearance of exogenously administered substances. Recent improvements in GFR measurement have been made, and understanding the limitations of different methods is important. In clinical practice, GFR is typically estimated using equations. Most equations are based on serum creatinine, but other markers, in particular Cystatin C have been investigated as well. In the last 10 years, several GFR estimation equations have been published, each associated with strengths and limitations. Understanding how these equations were derived and considering individual patient characteristics is helpful to determine what equations are most likely to estimate GFR most accurately. This review will address each of these issues, highlighting recent literature and focusing on clinical application.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Glomerular filtration rate (GFR) is the best overall index of kidney function. GFR assessment is the foundation for diagnosing renal disease in clinical practice. In hospitalized children, GFR evaluation plays a crucial role in ensuring correct medication doses, monitoring for nephrotoxicity, and determining pre-hospital renal function. In children with early chronic kidney disease (CKD) or being screened for CKD, reduced GFR may be the only sign of kidney damage. In patients with established CKD, GFR evaluation is vital for monitoring kidney disease progression. Therefore, accurate methods to evaluate GFR in children are needed.
Direct or gold standard measurement of GFR, performed by measuring clearance of exogenously administered substances, is often infeasible in clinical settings, is costly and labor-intensive, and thus only performed when precise renal function is needed. Equations or formulas that estimate GFR using endogenous renal clearance biomarkers are used most frequently in clinical practice. The most common GFR marker in these formulas is serum creatinine (SCr). However, several factors interfere with SCr measurement and interpretation, thus it is not an ideal marker. Estimating GFR in children comes with special considerations, as factors determining GFR and SCr change physiologically during early life postnatal kidney development. New GFR estimation formulas have been studied in recent years, with the goal of improving the limitations of established formulas. This article will review different methods of GFR measurement, GFR equations, and issues surrounding these measures, with the goal of providing the reader with an appreciation of how to approach interpretation and evaluation of GFR.
What is GFR?
The kidneys perform various regulatory functions including filtration (glomerular), reabsorption and secretion (tubular), and hormonal secretion (renal cells), maintaining hemodynamic, fluid and electrolyte homeostasis, red blood cell production, and healthy bone metabolism. With CKD, several metabolic and endocrine abnormalities are present (e.g., electrolyte disturbances, bone mineral disorders), each of which may potentially serve as biomarkers of abnormal renal function. However, these CKD perturbations are closely related to the most commonly used renal function parameter: GFR. Each nephron has a glomerulus, which contains capillaries. Glomerular filtration is the process of blood flowing through these capillaries, creating an ultrafiltrate. Its rate (GFR) is determined by factors including glomerular number, renal blood flow, capillary pressure, and capillary wall permeability. Total GFR reflects the total nephron mass performance (sum of each single nephron GFR). An average healthy adult GFR is about 120 ml/min/1.73 m2, with a wide normal range (90–149 ml/min/1.73 m2). GFR above this level is considered “hyperfiltration,” which may be a sign of early CKD or lead to CKD. Several factors influence GFR other than the presence of kidney damage, including protein intake, pregnancy, obesity, some vasodilatory antihypertensives or hyperglycemia (tend to increase GFR), or increasing age, some anti-hypertensives, and reduced intravascular volume (may decrease GFR) [1]. Therefore, ideally, GFR measurement and interpretation should be performed when patients are in a “steady state,” well-hydrated and using standardized measurement protocols.
Normal GFR in Children and Staging Decrement in GFR
The Kidney Disease Improving Global Outcomes (KDIGO) clinical practice guideline provides practice recommendations on several kidney disease topics, via international expert group consensus and detailed evidence review [2•]. KDIGO recommends a graded staging of CKD, from normal GFR (>90 ml/min/1.73 m2) to end stage renal disease (GFR < 15 ml/min/1.73 m2), shown in Table 1. These stages are used for screening and following patients with CKD, evaluating risk for abnormalities related to CKD (e.g., anemia) and assisting in decision-making on need for dialysis initiation. As stated in the KDIGO guideline, these GFR-based CKD categories may be applied to children. The exception is in children <2 years of age, before which GFR increases physiologically over the first 2 years of life; therefore, the KDIGO CKD staging is not similarly applicable. For example, GFR < 60 ml/min/1.73 m2 is normal in a 3 month old, but consistent with Grade 2–3 CKD in a 5 year old. By age 2, average normal GFR is similar to older child and adult levels.
Schwartz and Work recently reviewed in detail, studies which have measured GFR using gold standard or plasma disappearance methods in normal children, providing an estimate of normative child GFR values [3]. One work of particular interest is that of Piepsz et al. [4]. They measured GFR by plasma disappearance of [51] Cr-ethylenediamenetetraaceticacid (Cr-EDTA) in 623 children evaluated for potential mild urogenital abnormalities, only including patients with no significant kidney defects and with equal bilateral renal function. They confirmed that GFR rises progressively from neonatal age to 2 years old, stabilizing at a GFR of about 105 ml/min/1.73 m2 thereafter (Table 2). They also provided percentile values for GFR across age groups; for example GFR = 95 ml/min/1.73 m2 for a 1.5 year old child falls approximately at the 50th percentile value for age. Perhaps it would be more rational to express GFR in terms of percentile values (as done with height or weight) in the <2 year old age group; however, this would require research to determine how to use such percentile values in clinical care, determine what percentile is “abnormal” and how this relates to patient outcome. At present, clinicians should at least be aware than “normal GFR” is lower in children less than 2 years of age and may use the values provided in Table 2 as a guide to determining normal versus abnormal GFR.
An important and somewhat controversial issue is the method used to standardize or scale GFR. To compare GFR among infants, children, and adults, a standard reference scale reflecting patient size is required. Kidney weight would be ideal, although reliable measurement methods are not currently available. Body surface area (BSA) has been the traditional and is the current recommended method to scale GFR [2•]. However, one must be cautious when scaling GFR to BSA in patients with extremes of weight, since weight is included in BSA calculation. In very obese patients, scaling to BSA leads to GFR underestimation. For example, a patient with a non-scaled GFR of 90 ml/min and BSA = 2.0 has a BSA-corrected GFR = (90 ml/min × 1.73 m2)/2.0 m2 = 78 ml/min/1.73 m2. If the patient loses weight to a BSA = 1.8, BSA-corrected GFR will rise substantially, simply due to weight loss. This limitation should be considered when applying GFR values to very obese or malnourished individuals. Other body measures have been suggested to scale GFR to, including extracellular volume, total body water, or body cell mass [5–7], but these have not been studied extensively.
GFR Measurement Methods
Gold standard GFR evaluation refers to the measuring renal clearance of an administered exogenous filtration marker, where clearance of a substance (C [S]) is expressed in ml/min by the following equation:
where U [S] is urine concentration of the substance, V is the urine flow rate, (P [S]) is the plasma concentration of the substance. An ideal filtration or clearance marker is freely filtered at the glomerulus (thus not protein-bound), and is neither secreted nor reabsorbed by tubules (i.e., unchanged in urine). GFR measurement agents should be non-toxic and distributed extracellularly. There are generally two methods to measure clearance or GFR: evaluating substance plasma disappearance and a more cumbersome method including urinary collections. The gold standard method requires urine collections. The filtration marker is injected subcutaneously or intravenously (as a bolus or bolus plus infusion), followed by several urine collections obtained every 10–30 min. The substance’s plasma disappearance rate is monitored post-injection, and the average calculated clearance (using the formula above) is calculated with each urine collection and taken as the GFR. To stimulate urine flow, fluid is administered both before and during the protocol [8].
Inulin
The only known ideal gold standard filtration marker is inulin (Table 3). Inulin clearance measurement involves continuous intravenous infusion and meticulous urine sampling through a urinary catheter or voluntary voiding, as described above. Although inulin has the characteristics of an ideal GFR marker, there are limitations to this clearance method [9]. Hydration is required to maintain high-urine flow rate, and complete voiding is not always possible. This is especially problematic in children with urologic issues or who are incontinent. This method is time-consuming and uncomfortable, thus is not part of routine practice. Because of these and other disadvantages, alternative clearance methods and filtration markers are used.
Radioactive Markers of GFR and the Plasma Disappearance Method of Measuring GFR
Nuclear medicine techniques have been developed using radiolabeled agents (or tracers) with similar GFR marker characteristics as inulin (Table 3). Commonly used tracers include radiolabeled 99 m Tc-diethylene triamine penta-acetic acid (DTPA), Cr-EDTA, and iothalamate. These markers are generally used to measure GFR using the plasma disappearance method, avoiding the need for timed urine collection and continuous infusion.
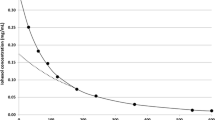
Plasma Disappearance Method of GFR Measurement
Plasma clearance of a marker is measured after a bolus intravenous injection. These methods are described in detail in several reviews and only briefly described here [3, 9]. GFR is calculated using the marker concentration administered divided by the area under the curve of plasma concentration over time. A “two-compartment system” is used to mathematically model the disappearance curve, where the marker is injected into a first compartment (the intravascular space), equilibrates with the second (the extracellular space), and is subsequently excreted via glomerular filtration from the first compartment. Time must be allowed for equilibration to occur before post-injection samples are drawn, otherwise GFR is overestimated [10, 11]. Drawbacks of this GFR measurement method include requirement of multiple blood samples and the time needed to characterize the disappearance curve, especially in patients with very low GFR (more time is needed to clear the substance). A simplified technique has been developed to include only a few blood samples, increasing feasibility of plasma disappearance GFR methods. There is general consensus that obtaining at least 3–4 samples for measuring the markers, up to 4–5 h after injection, is adequate [3, 11, 12]. In children with lower GFR (<30 ml/min/1.73 m2) obtaining samples as long as 12–24 h after injection will provide more accurate results.
Markers Used in Plasma Disappearance GFR Measurement Methods
Table 3 summarizes many of the markers used. Several studies have used the iodine isotope I-iothalamate [13–15]. However, there appears to be significant renal tubular secretion of iothalamate, causing GFR overestimation, which may at least partially explain the recent move away from iothalamate GFR measurement [16, 17].
Other markers commonly used are radio-isotopes 99 m Tc-DTPA [18] and 51 Cr-EDTA [4], both of which correlate strongly with inulin clearance [19]. Cr-EDTA is primarily used in Europe, while DTPA is used more frequently in North America. These markers do have limitations (Table 3) leading to overall GFR underestimation [2•]. However, DTPA plasma disappearance GFR measurement has specifically been shown to overestimate GFR at very low GFR levels, which should be kept in mind if using this method to make treatment decisions about dialysis initiation or CKD progression [20, 21]. Moreover, both tracers are associated with some radiation exposure. There is likely substantial variability between clinical centre protocol GFR measurement methods using DTPA and Cr-EDTA; if these methods continue to be widely used (they are currently the most commonly used GFR measurement methods in clinical practice), their protocols should be standardized.
Recently, an alternative, non-radioactive agent, iohexol, has been studied in children for measuring GFR using the plasma disappearance method. Iohexol is a low osmolarity contrast agent, used in low doses for measuring GFR [10]. Advantages include lack of radiation and favorable toxicity profile [22]. Iohexol is measured by high-performance liquid chromatography and mass spectrometry, so although the substance is inexpensive, the assay is costly. An advantage to iohexol plasma disappearance is that it has been studied and validated in detail by the Chronic Kidney Disease in Children study group (CKiD) [3, 10, 23]. In the original CKiD study (2009), the investigators used 4 post-injection time points to measure iohexol, up to 5 h post-injection, consistent with recommended measurement timepoints described above [10, 23]. This group also demonstrated that accurate iohexol GFR measurement may be possible using fewer blood samples [24]. Moreover, use of “dried capillary blood-spot” samples (capillary blood samples on a filter paper, later measured for ioxehol) for iohexol measurement is being investigated for GFR measurement [25, 26]. If more widely validated, this method of obtaining post-iohexol injection samples would be an exciting and non-invasive alternative to the current method.
Endogenous Creatinine Clearance
Depending on centre resources, GFR measurement methods described above may be impractical for timely GFR evaluation. An alternative method is the creatinine clearance, involving urine collection over a period of time (typically 24 h, but shorter periods may provide similar results [27]) and obtaining a single SCr measurement at the beginning or end of the urine collection. Using the clearance formula above, urine and serum creatinine concentrations and average urine flow rate (total ml of urine collected/minutes of collection, followed by scaling to BSA of 1.73 m2), GFR may be estimated. This method is simple, since SCr measurement is widely available and inexpensive. Although SCr is freely filtered at the glomerulus and not protein-bound, there are several limitations to the creatinine clearance. SCr concentration is associated with gender, age, nutrition and muscle mass, independent of GFR. Urine collection may not always be complete when performed at home, leading to inaccuracy. Importantly, creatinine is secreted by the proximal tubules, more so at lower GFR, leading to GFR overestimation. Cimetidine blocks tubular creatinine secretion, which improves the accuracy of GFR measurement [28, 29]. Thus, if using creatinine clearance to measure GFR, particularly in patients with low GFR or for following renal function over time, these limitations must be considered.
Estimating GFR Using Serum Markers and Equations
SCr
Despite limitations described above, SCr remains the most commonly used GFR marker, is inexpensive and child normative values have been published. Importantly, international efforts have led to promoting SCr assay measurement standardization to the gold standard isotope dilution mass spectroscopy method [30•, 31]. In 1976, Schwartz et al. published the well-known “Schwartz formula” to estimate GFR [32]. For almost 30 years, this equation was recommended to estimate GFR in children. This formula was derived using an older SCr assay, using creatinine clearance as the reference standard and is, therefore, inappropriate for estimating GFR today.
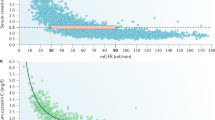
In 2009, the CKiD group published several new equations, in a large CKD child cohort (mean GFR about 40 ml/min/1.73 m2), using iohexol clearance as the reference standard [23]. The CKiD equations include various combinations of physical and laboratory variables (including height, blood urea nitrogen concentration, age, gender, SCr), as well as what is now often referred to as the “new bedside Schwartz formula” (top of Table 4). Similar to the previous Schwartz equation, it is based on the strong linear relationship between the height to serum creatinine ratio (height/SCr) (height, a surrogate of muscle mass, is important in SCr generation) and GFR. Height/SCr is multiplied by a regression-derived constant or k. This equation is currently recommended for child GFR estimation [2•]. It is simple to calculate, only requiring SCr and height. However, considerations should be made when using this equation. The equation was derived from children with substantially reduced kidney function and including few older teens (whose muscle mass is relatively higher and, therefore, may require a different k value to relate height/SCr to GFR). Recent studies actually show that the new Schwartz equation performs reasonably well to estimate GFR in children with higher GFR and older children [33•, 34], but this deserves further study. Because of problems associated with SCr concentrations and non-renal factors, estimating GFR in children at the extremes of muscle mass (particularly very low muscle mass, such as wheelchair bound children) using this equation, will be much less accurate [35]. Some authors have suggested that to achieve the best GFR estimation accuracy within a given centre, a “locally derived” k value may be calculated. Specifically, whatever reference standard GFR method is used within a centre, may be regressed on height/SCr of children who had those GFR measures, deriving a centre-specific k value [33•, 35, 36]. Theoretically, this k value should be the most appropriate for that centre’s patient population, ethnicity profile, and GFR reference method used. However, whether this leads to differences in clinical decision-making has not been evaluated. Other methods proposed to improve SCr-based GFR equations have been to incorporate other easily measured variables (such as blood urea nitrogen [23] or body cell mass [5]), but these methods increase complexity of quick GFR estimation and have not been validated. A non-exhaustive list of SCr-based equations which have been either validated externally or incorporating novel methods of SCr-based eGFR, is provided in Table 4. Of great importance is that adult-derived equations should not be used to estimate GFR in children. Derivation of these equations included small numbers of young adults and several include variables not routinely measured in pediatric care. Moreover, adult equations have been shown to poorly estimate GFR even in adolescents and young adults [37, 38].
Height-Independent GFR Estimation: Is it Possible?
Height is not always available clinically and is not available in laboratory databases, making large, population-based child GFR research impossible. Recently, Pottel et al. developed a height-independent child GFR equation. The equation constant is the Q value, which differs by age; this value represents the median SCr value from a population of healthy children (in the case of the Pottel equation, from European children [39–41]). Although height-dependent GFR estimation was more accurate, their height-independent method performed quite well and may represent a major step forward in population-based child GFR research. These Q values may also be calculated for individual patients, using the calculations shown in Table 4 (population-derived equations). In principle, Q values could be derived in different patient populations, including North America (using SCr values measured in large populations of normal children) or within a given centre. Further study of this GFR estimation method would be highly worthwhile.
Cystatin C
To overcome the limitations of SCr, another endogenous GFR marker, cystatin C (CysC), has been evaluated. CysC is a small, cysteine protease inhibitor protein that is freely filtered at the glomerulus and not significantly affected by age, gender or muscle mass [11]. The exception is in children less than age 1, who have higher CysC concentrations [11], potentially due to GFR being physiologically lower. CysC may be higher in patients treated with steroids and those with a renal transplant [13, 42–48] and concentrations may be affected by inflammatory and thyroid disorders [44–48]. CysC has also been shown to increase as a result of certain malignancies; however, it is unclear whether this is due to CysC production by tumor cells or rather impairment in renal function [45]. Nevertheless, CysC-based formulas demonstrate better performance in oncology patients compared to those based on height/SCr [49–51]. Several CysC-eGFR equations have been derived (some are summarized in Table 4). In general, CysC equations are more accurate for estimating GFR and more diagnostic of abnormal GFR, than SCr equations [52, 53]. CysC cannot be used to measure clearance since it is reabsorbed by proximal tubular cells. It is important to note that the two published CysC assays (turbidimetric and nephelometric) lead to substantially different values [54–56]. Most recent data suggest that the nephelometric CysC assay leads to more accurate GFR estimation [52, 57••]. Currently, the cost of CysC measurement is approximately 8–10 times SCr measurement; however, if its use becomes more widespread, this cost may decrease. Population-based normative CysC values have been published [58, 59•]. Ultimately, whether using CysC in clinical care, versus SCr, actually leads to differences in decision-making or on patient outcomes, remains unknown.
Table 4 displays several eGFR equations, including recently derived equations which combine both SCr and CysC [13, 23, 39–41, 57••, 60–66]. These equations appear to be most accurate for estimating GFR. The CKiD group confirmed that incorporating SCr and CysC in eGFR equations leads to more accurate GFR estimation in children with CKD. Research is needed to validate this finding in different populations and determine if patient outcomes are affected by such improved GFR estimation.
Which Equation to Use?
Given the large number of equations available to estimate GFR, it can become quite overwhelming to decide which equation should be used. It is likely reasonable to use the currently recommended Schwartz equation in most clinical scenarios. However, one must consider individual patient characteristics to decide when using an alternative equation may be most appropriate. When high accuracy is desired, it has been proposed to estimate GFR using both SCr and CysC equations and calculating the mean. However, in cases of reduced muscle mass such as in patients hospitalized for prolonged periods, paralysis or amputation, the SCr-based estimates will be inaccurate and a CysC-eGFR will be more accurate. In some situations, CysC-eGFR will be less accurate, such as in patients receiving high doses of glucocorticoids. Children treated for cancer are of particular consideration since they undergo considerable changes in muscle mass over a short time period and receive many medications including steroids; thus, both SCr-eGFR and CysC-eGFR equations may be inaccurate. In such cases, there may be significant discrepancy between SCr and CysC-based eGFR estimates and GFR measured by a reference procedure should be considered [67]. At our centre, we selectively measure CysC in children whom we feel SCr-eGFR is particularly inaccurate (e.g., wheelchair bound child, evaluated for CKD) and when there is great uncertainty we pursue gold standard GFR measurement.
Other Serum Markers
Other serum markers of GFR have been investigated for estimating GFR in children, including beta trace protein (BTP) and beta 2-microglobulin (B2M), both low molecular weight proteins which are freely filtered at the glomerulus [68–70]. Little research on these markers has been performed, and future studies will elucidate the extent to which they may offer more accurate GFR estimation than is currently feasible with SCr and CysC [60, 71].
Conclusion and Proposed Application
Although there has been a large amount learned on how to measure GFR, estimating GFR as accurately as possible using SCr and on novel markers of GFR, there remain many knowledge gaps. For example, although iohexol GFR plasma disappearance measurement method for measuring GFR is likely the best characterized and most valid current feasible method to measure GFR, the extent to which this method is different to the most commonly used tracer methods is not known. Although we now have new candidate serum GFR markers, like CysC, more accurate for estimating GFR, whether we should actually replace SCr for CysC or in what patients to do so, is unclear. What is clear is that inaccurate GFR measurement or estimation can potentially impact negatively on patients, such as when screening for CKD (overdiagnosis or missed diagnoses), dosing life-saving medications or making critical decisions on prognosis and dialysis initiation in patients with CKD. We propose that given the current state of knowledge and available evidence, when screening for CKD, or estimating GFR in the hospital setting, the bedside Schwartz formula should generally be adequate. However, one must always look for patient characteristics which may be associated with potential for inaccuracy of GFR estimation using this equation (e.g., very low muscle mass, very obese, limb amputation, older adolescent males), especially when critical decisions will be made based on eGFR (e.g., a patient awaiting transplant listing). In such cases, CysC measurement may be useful to provide a better estimate of GFR. Should we change to using CysC to measure renal function? It is unknown if this will lead to improved outcomes. However, until centres and individual physicians begin using this test or until research shows improvement in outcomes or resource use from using CysC, we will never know. In patients evaluated for CKD presence, one should be cautious about assuming that “borderline” eGFR is normal or abnormal (e.g., eGFR between 80 and 100 ml/min/1.73 m2) given the poor precision (variability) of current equations and consider performing a reference standard GFR test. With regards to GFR measurement methods, we suggest that clinicians be aware of what method is being used in their centre (e.g., DTPA plasma disappearance vs. iothalamate) so as to be able to better interpret results with knowledge of the test's potential limitations. For similar reasons, it is also worthwhile to be aware of the specific test methodology used (e.g., 2 vs. 5 point-tracer plasma measurement for DTPA GFR tests). Often, the test may be modified to fit specific patient characteristics, such as in a child presumed to have very low GFR, in whom requesting for prolonged post-injection plasma measurements would be helpful. In the research study setting, the goal should be to estimate GFR as accurately as possible, therefore, whenever feasible, we propose using SCr and CysC-eGFR measurement.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Levey AS, Inker LA, Coresh J. GFR estimation: from physiology to public health. Am J Kidney Dis. 2014;63(5):820–34.
• KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2013; 3(1):163. This guideline is the result of an international consensus expert group review of the evidence base on CKD management in children and adults, including measurement of GFR and defining CKD.
Schwartz GJ, Work DF. Measurement and estimation of GFR in children and adolescents. Clin J Am Soc Nephrol. 2009;4(11):1832–43.
Piepsz A, Tondeur M, Ham H. Revisiting normal (51)Cr-ethylenediaminetetraacetic acid clearance values in children. Eur J Nucl Med Mol Imaging. 2006;33(12):1477–82.
Andersen TB. Estimating renal function in children: a new GFR-model based on serum cystatin C and body cell mass. Dan Med J. 2012;59(7):B4486.
Peters AM. The kinetic basis of glomerular filtration rate measurement and new concepts of indexation to body size. Eur J Nucl Med Mol Imaging. 2004;31(1):137–49.
Piepsz A, Tondeur M, Ham H. Escaping the correction for body surface area when calculating glomerular filtration rate in children. Eur J Nucl Med Mol Imaging. 2008;35(9):1669–72.
Schwartz GJ, Furth SL. Glomerular filtration rate measurement and estimation in chronic kidney disease. Pediatric Nephrol. 2007;22(11):1839–48.
Macedo E, Mehta RL. Measuring renal function in critically ill patients: tools and strategies for assessing glomerular filtration rate. Curr Opin Crit Care. 2013;19(6):560–6.
Schwartz GJ, Furth S, Cole SR, Warady B, Munoz A. Glomerular filtration rate via plasma iohexol disappearance: pilot study for chronic kidney disease in children. Kidney Int. 2006;69(11):2070–7.
Filler G, Yasin A, Medeiros M. Methods of assessing renal function. Pediatric Nephrol. 2014;29(2):183–92.
Nilsson-Ehle P, Grubb A. New markers for the determination of GFR: iohexol clearance and cystatin C serum concentration. Kidney Int Suppl. 1994;47:S17–9.
Zappitelli M, Parvex P, Joseph L, Paradis G, Grey V, Lau S, Bell L. Derivation and validation of cystatin C-based prediction equations for GFR in children. Am J Kidney Dis. 2006;48(2):221–30.
Bajaj G, Alexander SR, Browne R, Sakarcan A, Seikaly MG. 125Iodine-iothalamate clearance in children. A simple method to measure glomerular filtration. Pediatric Nephrol (Berlin, Germany). 1996;10(1):25–8.
Silkalns GI, Jeck D, Earon J, Edelmann CM Jr, Chervu LR, Blaufox MD, Spitzer A. Simultaneous measurement of glomerular filtration rate and renal plasma flow using plasma disappearance curves. J Pediatrics. 1973;83(5):749–57.
Florijn KW, Barendregt JN, Lentjes EG, van Dam W, Prodjosudjadi W, van Saase JL, van Es LA, Chang PC. Glomerular filtration rate measurement by “single-shot” injection of inulin. Kidney Int. 1994;46(1):252–9.
Odlind B, Hallgren R, Sohtell M, Lindstrom B. Is 125I iothalamate an ideal marker for glomerular filtration? Kidney Int. 1985;27(1):9–16.
Piepsz A, Denis R, Ham HR, Dobbeleir A, Schulman C, Erbsmann F. A simple method for measuring separate glomerular filtration rate using a single injection of 99mTc-DTPA and the scintillation camera. J Pediatrics. 1978;93(5):769–74.
Rehling M, Moller ML, Thamdrup B, Lund JO, Trap-Jensen J. Simultaneous measurement of renal clearance and plasma clearance of 99mTc-labelled diethylenetriaminepenta-acetate, 51Cr-labelled ethylenediaminetetra-acetate and inulin in man. Clin Sci (Lond). 1984;66(5):613–9.
Itoh K. Comparison of methods for determination of glomerular filtration rate: Tc-99m-DTPA renography, predicted creatinine clearance method and plasma sample method. Ann Nucl Med. 2003;17(7):561–5.
LaFrance ND, Drew HH, Walser M. Radioisotopic measurement of glomerular filtration rate in severe chronic renal failure. J Nucl Med. 1988;29(12):1927–30.
P N-E. Iohexol clearance for the determination of glomerular filtration rate: 15 years experience in clinical practice. eJIFCC. 13(2).
Schwartz GJ, Munoz A, Schneider MF, Mak RH, Kaskel F, Warady BA, Furth SL. New equations to estimate GFR in children with CKD. J Am Soc Nephrol. 2009;20(3):629–37.
Abraham AG, Munoz A, Furth SL, Warady B, Schwartz GJ. Extracellular volume and glomerular filtration rate in children with chronic kidney disease. Clin J Am Soc Nephrol. 2011;6(4):741–7.
Niculescu-Duvaz I, D’Mello L, Maan Z, Barron JL, Newman DJ, Dockrell ME, Kwan JT. Development of an outpatient finger-prick glomerular filtration rate procedure suitable for epidemiological studies. Kidney Int. 2006;69(7):1272–5.
Mafham MM, Niculescu-Duvaz I, Barron J, Emberson JR, Dockrell ME, Landray MJ, Baigent C. A practical method of measuring glomerular filtration rate by iohexol clearance using dried capillary blood spots. Nephron Clin Pract. 2007;106(3):c104–12.
Herrera-Gutierrez ME, Seller-Perez G, Banderas-Bravo E, Munoz-Bono J, Lebron-Gallardo M, Fernandez-Ortega JF. Replacement of 24-h creatinine clearance by 2-h creatinine clearance in intensive care unit patients: a single-center study. Intensive Care Med. 2007;33(11):1900–6.
Hellerstein S, Berenbom M, Alon US, Warady BA. Creatinine clearance following cimetidine for estimation of glomerular filtration rate. Pediatric Nephrol. 1998;12(1):49–54.
van Acker BA, Koomen GC, Koopman MG, de Waart DR, Arisz L. Creatinine clearance during cimetidine administration for measurement of glomerular filtration rate. Lancet. 1992;340(8831):1326–9.
• Pieroni L, Delanaye P, Boutten A, Bargnoux AS, Rozet E, Delatour V, Carlier MC, Hanser AM, Cavalier E, Froissart M, Cristol JP. A multicentric evaluation of IDMS-traceable creatinine enzymatic assays. Clin Chim Acta. 2011; 412(23–24): 2070–2075. This work describes in detail the standardization of serum creatinine lab measurement, representing an important advancement in renal function evaluation.
Schwartz GJ, Kwong T, Erway B, Warady B, Sokoll L, Hellerstein S, Dharnidharka V, Furth S, Munoz A. Validation of creatinine assays utilizing HPLC and IDMS traceable standards in sera of children. Pediatric Nephrol. 2009;24(1):113–9.
Schwartz GJ, Haycock GB, Edelmann CM Jr, Spitzer A. A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics. 1976;58(2):259–63.
• Bacchetta J, Cochat P, Rognant N, Ranchin B, Hadj-Aissa A, Dubourg L. Which creatinine and cystatin C equations can be reliably used in children? Clin J Am Soc Nephrol. 2011; 6(3):552–560. This work validated the new CKiD GFR equation and proposed new methods for GFR estimation.
Staples A, LeBlond R, Watkins S, Wong C, Brandt J. Validation of the revised Schwartz estimating equation in a predominantly non-CKD population. Pediatric Nephrol. 2010;25(11):2321–6.
Zappitelli M, Joseph L, Gupta IR, Bell L, Paradis G. Validation of child serum creatinine-based prediction equations for glomerular filtration rate. Pediatr Nephrol. 2007;22(2):272–81.
Andersen TB, Eskild-Jensen A, Frokiaer J, Brochner-Mortensen J. Measuring glomerular filtration rate in children; can cystatin C replace established methods? A review. Pediatric Nephrol. 2009;24(5):929–41.
Filler G, Sharma AP. How to monitor renal function in pediatric solid organ transplant recipients. Pediatr Transplant. 2008;12(4):393–401.
Selistre L, Roquet O, Saitovitch D, de Souza VC, Antonello IC, Ranchin B, Hadj-Aissa A, Cochat P, Dubourg L. Comparison of cystatin C- and creatinine-based glomerular filtration rate formulas with inulin clearance in pediatric renal transplantation. Transpl Proc. 2012;44(8):2357–9.
Hoste L, Dubourg L, Selistre L, De Souza VC, Ranchin B, Hadj-Aissa A, Cochat P, Martens F, Pottel H. A new equation to estimate the glomerular filtration rate in children, adolescents and young adults. Nephrol Dial Transplant. 2014;29(5):1082–91.
Pottel H, Hoste L, Martens F. A simple height-independent equation for estimating glomerular filtration rate in children. Pediatric Nephrology. 2012;27(6):973–9.
Pottel H, Mottaghy FM, Zaman Z, Martens F. On the relationship between glomerular filtration rate and serum creatinine in children. Pediatric Nephrol. 2010;25(5):927–34.
Bokenkamp A, Domanetzki M, Zinck R, Schumann G, Byrd D, Brodehl J. Cystatin C serum concentrations underestimate glomerular filtration rate in renal transplant recipients. Clin Chem. 1999;45(10):1866–8.
Filler G, Browne R, Seikaly MG. Glomerular filtration rate as a putative ‘surrogate end-point’ for renal transplant clinical trials in children. Pediatr Transplant. 2003;7(1):18–24.
Holmquist P, Torffvit O, Sjoblad S. Metabolic status in diabetes mellitus affects markers for glomerular filtration rate. Pediatric Nephrol. 2003;18(6):536–40.
Kos J, Stabuc B, Cimerman N, Brunner N. Serum cystatin C, a new marker of glomerular filtration rate, is increased during malignant progression. Clin Chem. 1998;44(12):2556–7.
Cimerman N, Brguljan PM, Krasovec M, Suskovic S, Kos J. Serum cystatin C, a potent inhibitor of cysteine proteinases, is elevated in asthmatic patients. Clin Chim Acta. 2000;300(1–2):83–95.
Risch L, Herklotz R, Blumberg A, Huber AR. Effects of glucocorticoid immunosuppression on serum cystatin C concentrations in renal transplant patients. Clin Chem. 2001;47(11):2055–9.
Risch L, Huber AR. Glucocorticoids and increased serum cystatin C concentrations. Clin Chim Acta. 2002;320(1–2):133–4.
Blufpand HN, Tromp J, Abbink FC, Stoffel-Wagner B, Bouman AA, Schouten-van Meeteren AY, van Wijk JA, Kaspers GJ, Bokenkamp A. Cystatin C more accurately detects mildly impaired renal function than creatinine in children receiving treatment for malignancy. Pediatr Blood Cancer. 2011;57(2):262–7.
Gronroos MH, Jahnukainen T, Irjala K, Harkonen R, Hurme S, Mottonen M, Salmi TT. Comparison of glomerular function tests in children with cancer. Pediatric Nephrol. 2008;23(5):797–803.
Laskin BL, Nehus E, Goebel J, Khoury JC, Davies SM, Jodele S. Cystatin C-estimated glomerular filtration rate in pediatric autologous hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2012;18(11):1745–52.
Dharnidharka VR, Kwon C, Stevens G. Serum cystatin C is superior to serum creatinine as a marker of kidney function: a meta-analysis. Am J Kidney Dis. 2002;40(2):221–6.
Roos JF, Doust J, Tett SE, Kirkpatrick CM. Diagnostic accuracy of cystatin C compared to serum creatinine for the estimation of renal dysfunction in adults and children: a meta-analysis. Clin Biochem. 2007;40(5–6):383–91.
Schwartz GJ, Schneider MF, Maier PS, Moxey-Mims M, Dharnidharka VR, Warady BA, Furth SL, Munoz A. Improved equations estimating GFR in children with chronic kidney disease using an immunonephelometric determination of cystatin C. Kidney Int. 2012;82(4):445–53.
Bariciak E, Yasin A, Harrold J, Walker M, Lepage N, Filler G. Preliminary reference intervals for cystatin C and beta-trace protein in preterm and term neonates. Clin Biochem. 2011;44(13):1156–9.
Harmoinen A, Ylinen E, Ala-Houhala M, Janas M, Kaila M, Kouri T. Reference intervals for cystatin C in pre- and full-term infants and children. Pediatric Nephrol. 2000;15(1–2):105–8.
•• Schwartz GJ, Schneider MF, Maier PS, Moxey-Mims M, Dharnidharka VR, Warady BA, Furth SL, Munoz A. Improved equations estimating GFR in children with chronic kidney disease using an immunonephelometric determination of cystatin C. Kidney Int. 2012; 82(4):445–453. In this work, the CKiD group demonstrated the importance of considered the Cystatin C assay used for measurement and proposed several new Cystatin C based equations, including a “Cystatin C - only” equation.
Hannemann A, Friedrich N, Dittmann K, Spielhagen C, Wallaschofski H, Volzke H, Rettig R, Endlich K, Lendeckel U, Stracke S, Nauck M. Age- and sex-specific reference limits for creatinine, cystatin C and the estimated glomerular filtration rate. Clin Chem Lab Med. 2012;50(5):919–26.
• Fadrowski JJ, Neu AM, Schwartz GJ, Furth SL. Pediatric GFR estimating equations applied to adolescents in the general population. Clin J Am Soc Nephrol. 2011; 6(6):1427–1435. Using data from NHANES, the authors describe population-based serum creatinine and cystatin C values.
Benlamri A, Nadarajah R, Yasin A, Lepage N, Sharma AP, Filler G. Development of a beta-trace protein based formula for estimation of glomerular filtration rate. Pediatric Nephrol. 2010;25(3):485–90.
Bouvet Y, Bouissou F, Coulais Y, Seronie-Vivien S, Tafani M, Decramer S, Chatelut E. GFR is better estimated by considering both serum cystatin C and creatinine levels. Pediatric Nephrol. 2006;21(9):1299–306.
Chehade H, Cachat F, Jannot AS, Meyrat BJ, Mosig D, Bardy D, Parvex P, Girardin E. Combined serum creatinine and cystatin C Schwartz formula predicts kidney function better than the combined CKD-EPI formula in children. Am J Nephrol. 2013;38(4):300–6.
Gao A, Cachat F, Faouzi M, Bardy D, Mosig D, Meyrat BJ, Girardin E, Chehade H. Comparison of the glomerular filtration rate in children by the new revised Schwartz formula and a new generalized formula. Kidney Int. 2013;83(3):524–30.
Hoek FJ, Kemperman FA, Krediet RT. A comparison between cystatin C, plasma creatinine and the Cockcroft and Gault formula for the estimation of glomerular filtration rate. Nephrol Dial Transplant. 2003;18(10):2024–31.
Le Bricon T, Thervet E, Froissart M, Benlakehal M, Bousquet B, Legendre C, Erlich D. Plasma cystatin C is superior to 24-h creatinine clearance and plasma creatinine for estimation of glomerular filtration rate 3 months after kidney transplantation. Clin Chem. 2000;46(8 Pt 1):1206–7.
Rule AD, Bergstralh EJ, Slezak JM, Bergert J, Larson TS. Glomerular filtration rate estimated by cystatin C among different clinical presentations. Kidney Int. 2006;69(2):399–405.
Grubb A. Non-invasive estimation of glomerular filtration rate (GFR). The Lund model: simultaneous use of cystatin C- and creatinine-based GFR-prediction equations, clinical data and an internal quality check. Scand J Clin Lab Invest. 2010;70(2):65–70.
Viberti GC, Keen H, Mackintosh D. Beta 2-microglobulinaemia: a sensitive index of diminishing renal function in diabetics. Br Med J. 1981;282(6258):95–8.
Hoffmann A, Nimtz M, Conradt HS. Molecular characterization of beta-trace protein in human serum and urine: a potential diagnostic marker for renal diseases. Glycobiology. 1997;7(4):499–506.
Juraschek SP, Coresh J, Inker LA, Levey AS, Kottgen A, Foster MC, Astor BC, Eckfeldt JH, Selvin E. Comparison of serum concentrations of beta-trace protein, beta2-microglobulin, cystatin C, and creatinine in the US population. Clin J Am Soc Nephrol. 2013;8(4):584–92.
Filler G, Priem F, Lepage N, Sinha P, Vollmer I, Clark H, Keely E, Matzinger M, Akbari A, Althaus H, Jung K. Beta-trace protein, cystatin C, beta(2)-microglobulin, and creatinine compared for detecting impaired glomerular filtration rates in children. Clin Chem. 2002;48(5):729–36.
Rahn KH, Heidenreich S, Bruckner D. How to assess glomerular function and damage in humans. J Hypertens. 1999;17(3):309–17.
Arant BS Jr, Edelmann CM Jr, Spitzer A. The congruence of creatinine and inulin clearances in children: use of the Technicon AutoAnalyzer. J Pediatrics. 1972;81(3):559–61.
Berns AS. Nephrotoxicity of contrast media. Kidney Int. 1989;36(4):730–40.
Chervu LR, Blaufox MD. Renal radiopharmaceuticals: an update. Semin Nucl Med. 1982;12(3):224–45.
Rehling M, Nielsen LE, Marqversen J. Protein binding of 99Tcm-DTPA compared with other GFR tracers. Nucl Med Commun. 2001;22(6):617–23.
Fogh-Andersen N. Binding of the chromium-ethylenediaminetetraacetic acid complex (CrEDTA) to human albumin. Scand J Clin Lab Invest. 1980;40(8):805–8.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Renal.
Rights and permissions
About this article
Cite this article
Benisty, K., Zappitelli, M. Measures of GFR in Health and Disease. Curr Pediatr Rep 3, 101–110 (2015). https://doi.org/10.1007/s40124-014-0067-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40124-014-0067-3