Abstract
Introduction
In China, the demand for implantable collamer lens (ICL) surgery is booming. Immediate sequential bilateral ICL surgery (ISBICLS) benefits patients and clinics, but it remains controversial and lacks standardization. We aim to investigate the prevalence of, factors for, and surgeon attitudes toward ISBICLS.
Methods
In this cross-sectional survey study, an electronic questionnaire about the practice and attitudes toward performing ISBICLS or delayed sequential bilateral ICL surgery (DSBICLS) was distributed to 792 qualified ICL surgeons in Mainland China, between 4 April and 22 April 2022.
Results
A total of 531 surgeons (66.79%) from 30 provinces in Mainland China responded. Among them, 374 (67.23%) were currently performing ISBICLS. Fifty-two percent (277) of surgeons reported performing ISBICLS more than 50% of the time, while 85.05% of surgeons chose to perform the second eye surgery 1 day after the first eye surgery. Seventy percent (248) of surgeons performing ISBICLS chose to perform the second eye surgery less than 30 min after the first eye surgery. Surgeons who started ICL surgery earlier (before 2010, OR = 2.772, 95% CI = 1.290–5.957, P = 0.009; 2011–2013, OR = 2.479, 95% CI = 1.060–5.800, P = 0.036), completed one-eye ICL surgery faster (< 3 min, OR = 3.936, 95% CI = 1.505–10.293, P = 0.005) and modified the second eye ICL selection less frequently (1–25%, OR = 0.203, 95% CI = 0.054–0.771, P = 0.019; 26–50%, OR = 0.173, 95% CI = 0.041–0.726, P = 0.017; 51–75%, OR = 0.299, 95% CI = 0.041–0.726, P = 0.123; 76–100%, OR = 0.163, 95% CI = 0.039–0.688, P = 0.014) tended to perform ISBICLS. No significant association was found among clinical settings, preoperative measurement devices, and hospital policies with performing ISBICLS. Regarding their attitudes toward ISBICLS, 54.63% preferred ISBICLS and 45.37% preferred DSBICLS. The main supporting reasons were patient convenience (98.64%), faster vision rehabilitation (73.56%), and improved perioperative compliance (73.22%). The concerns regarding ISBICLS included the risk of endophthalmitis (62.22%), lack of recommendation in expert consensus (61.67%), and decreased vault predictability (60.93%). The most common desires for further adoption were expert consensus on surgical criteria and patient indicators for ISBICLS (82.3%).
Conclusions
ISBICLS has been gradually adopted in Mainland China, but has not been widely accepted as a routine procedure. Surgeons’ experience and skills mainly influence whether ISBICLS is performed. Further research is needed to explore standardized protocols to prevent endophthalmitis, the appropriate time interval of two eye surgery, and requisitions for surgeon skills.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
This study developed a novel questionnaire to investigate the prevalence of, factors for, and surgeons’ attitudes toward immediate sequential bilateral ICL surgery(ISBICLS), and distributed it to 792 ophthalmologists in Mainland China. |
ISBICLS has not been widely accepted as a routine procedure in Mainland China. The experience and skill of surgeons mainly influences whether they performed ISBICLS. The broad range of identified factors provides basis for further evidence-based research. |
Endophthalmitis risk and vault predictability should both be predominant factors in determining the appropriate workflow of ICL surgery. |
Our findings may inform the future revision of expert consensus of ICL surgery, including the standardized protocols to prevent endophthalmitis, the appropriate time interval of two eye surgery, and requisitions for surgeon skills. |
Introduction
Refractive surgery has shown rapid development and a large potential market demand [1]. The implantable collamer lens (ICL; STAAR Surgical, Monrovia, CA, USA) is the most widely used and latest phakic intraocular lens (PIOL) worldwide, which has been implanted into over two million eyes for myopic correction [2] and provided satisfactory visual outcomes [3, 4]. In China, ICL implantation has a > 20-year history since 2003 [5, 6]. In 2014, new ICL models—the ICL V4c with central flow—were approved by Chinese Food and Drug Administration (CFDA) and have become the current mainstream in the Chinese market. The central hole design is proven to improve aqueous humor circulation without the need for peripheral iridotomy, and also provides good vision quality [7, 8] [especially the newest model EVO + (V5) with higher optic diameter [9]]. Nowadays, ICL implantation in China accounts for 10.95% of refractive surgeries and is increasing by 40.8% annually [10]. The coronavirus disease 2019 (COVID-19) pandemic also prompted hospitals to minimize individual patient contact [11]. Thus, improving clinical efficiency is attracting increasing attention.
ICL implantation is an intraocular surgery that involves the implantation of ICL lens into the posterior chamber while preserving the natural crystalline lens. Until now, delayed sequential bilateral ICL surgery (DSBICLS), performing the bilateral ICL implantation on different sessions, is preferred to prevent endophthalmitis or other complications according to the expert consensus in many countries, such as China [12], Germany [13], and the USA [14]. Immediate sequential bilateral ICL surgery (ISBICLS), performing the bilateral ICL implantation on the same session, was first described at the annual meeting of the Association for Research in Vision and Ophthalmology in 2019 [15]. It truly brings great convenience for patients and clinicians, but contradicts the existing recommendations. Although immediate sequential bilateral cataract surgery (ISBCS) has gained popularity among developed countries due to its great clinical efficiency [16, 17] and substantial progress has been made in providing appropriate patient indicators for ISBCS [18,19,20], the risk of endophthalmitis remains a concern [16, 18]. In terms of ICL surgery, some surgeons have proposed adjusting the second eye’s ICL size based on the first eye’s vault, which may improve the predictability [21, 22] Other controversies include depriving patients of a surgical selection in the second eye [23], economic factors, and medicolegal issues.
Recently, ISBICLS has been routinely adopted by some hospitals in Mainland China. However, whether bilateral ICL implantation should be performed in the same session remains controversial and is a crucial consideration. Furthermore, hospital administrators and surgeons are likely to be interested in any additional factors associated with its adoption.
In 2019, Chinese expert consensus on PIOL implantation was published to inform future better practices of ICL surgery [12]. In this study, we used a questionnaire reviewed by specialists of Chinese ICL core expert group to investigate prevalence and surgeon attitudes regarding ISBICLS and analyzed the trends in performing ISBICLS. We compared the surgeons’ characteristics between those currently performing ISBICLS or not and assessed factors affecting the adoption of ISBICLS in Mainland China.
Methods
This study adhered to the tenets of the Declaration of Helsinki and was approved by the Ethical Committee Review Board of Fudan University Eye and ENT Hospital (2021018).
Questionnaire Preparation
A questionnaire was formulated from discussion of our research group (consisting of six clinical staff of ophthalmology) and consultations with two clinical professionals at the Fudan University Eye Ear Nose and Throat Hospital (Shanghai, China). The questionnaire was externally reviewed by two methodologists at the School of Public Health of Fudan University and ten clinical professionals from the Chinese core expert group of ICL surgery for further modifications. Before use, the questionnaire was sent to 19 qualified ophthalmologists performing ICL surgery nationwide to consolidate the questions (not included in the final analysis) on two occasions, 3 weeks apart, for validation of repeatability. The questionnaires were initially prepared in Chinese, translated into English, and then back-translated into Chinese to assess the accuracy. Consent was obtained from the participants that the data would be used as part of a study.
Questionnaire Content
ISBICLS was defined as bilateral ICL surgery performed on the same day. DSBICLS was defined as second eye ICL surgery performed > 1 day after the first eye surgery.
To investigate the prevalence of adoption of ISBICLS, we asked surgeons whether the respondent indicated that they had performed ISBICLS. Surgeons who had performed ISBICLS were asked about their current percentage of performed ISBICLS cases as a screening question to identify surgeons who currently performed ISBICLS and those who currently performed DSBICLS (including those who stopped performing ISBICLS and never performed ISBICLS). We also inquired about the time interval between bilateral ICL surgery when performing ISBICLS or DSBICLS. To investigate the surgeons’ attitudes toward ISBICLS, the survey asked whether they preferred ISBICLS or DSBICLS as routine procedure. All respondents were asked about their experience with ICL surgery and hospital policies on ICL surgery, as well as their supporting reasons, concerns, and desire for adopting ISBICLS. A mixture of single-choice, multiple-choice, and free-text entries were included (see Supplementary Material for the questionnaire).
Questionnaire Distribution
The questionnaires were distributed electronically between 4 April and 22 April 2022, on the survey website (https://www.wenjuan.com/) by the STAAR surgical department in Mainland China. The inclusion criteria were qualified ICL surgeons in Mainland China (qualified ophthalmologists by the Chinese National Health Commission and who had independently performed ICL surgeries in at least 20 eyes). The questions were provided in Chinese, which was the first language of all respondents. Final submission was allowed only after all questions were answered.
Statistical Analysis
Categorical variables were presented as numbers along with proportions and compared by chi-square tests. In addition, to evaluate factors associated with surgeons currently performing ISBICLS, a post hoc analysis was performed using univariate and multivariate logistic regression models. The variables in univariate logistic regression model (Supplementary Table 2) with P-value < 0.05 were included as covariables in the multivariate logistic models. For the association of clinical settings with the outcome, we adjusted for demographic characteristics (job title, departments, medical institution type, and medical institution level). For the association of surgeon experience or skills with ICL surgery, we adjusted additionally when to start ICL surgery, the total surgical volume, the time of one-eye ICL surgery, the preoperative measurement devices, and ICL surgery management type, except for percentage of modifying the second eye ICL selection (due to potential mediation). Finally, we made a fully adjusted logistic regression model. All statistical descriptions and analyses were performed in SPSS (version 25.0; SPSS Inc, IBM, China). Two-tailed values were considered statistically significant at P < 0.05.
Results
Our data were collected from all 30 provinces where ICL surgery is available in Mainland China. Of the 795 ophthalmologists sent the questionnaire, a total of 531 (66.79%) responded. The number of respondents from all provinces is presented in Supplementary Table 1. Demographic characteristics of the respondents are presented in Table 1 (205 female and 326 male; mean age, 47.77 ± 7.77 years). Among all 531 respondents, ICL V4c was the most common implanted ICL model (522, 98.3%), EVO + (V5) was reported to be implanted by 19 surgeons (Table 1).
Prevalence and Trends of Performing ISBICLS
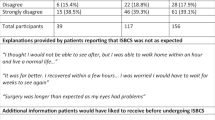
Among all responders, 361 (67.98%) reported performing ISBICLS. In contrast, 170 (32.07%) have not performed ISBICLS. Of the 361 surgeons who had performed ISBICLS, four (1.11%) stopped performing ISBICLS. Thus, a total of 357 (67.23%) were currently performing ISBICLS. In terms of the percentage of performing ISBICLS, 277 (52.17%) reported performing ISBICLS more than 50% of the time (Table 2). Most (69.53%) surgeons performing ISBICLS chose performing the second eye surgery < 30 min after the first eye surgery, while the other surgeons performed the second eye surgery in a separate session with a delay > 30 min. In terms of DSBICLS, 85.05% of surgeons chose performing the second eye surgery 1 day after the first eye surgery (Table 2).
Figure 1 shows the trends of performing ICL implantation and ISBICLS. With the increase in ICL surgeries, an increasing number of surgeons have started performing ISBICLS since 2002. Before 2014, only 88 surgeons performed ISBICLS among the total of 212 ICL surgeons. In 2015, there was a small spike of 5.54% in the percentage of ISBICLS. The increasing rate of ISBICLS peaked in 2020 (11.86%), with 57.44% of all surgeons performing ISBICLS. After the epidemic of COVID-19, the proportion of surgeons performing ISBICLS increased by 22.41% since 2020. The increasing rate of surgeons performing ICL surgery at the same time was 18.27%.
The annual proportion of surgeons who started performing ICL surgery and immediate sequential bilateral ICL surgery (ISBICLS). With the increase in ICL surgeries, an increasing number of surgeons have started performing ISBICLS since 2002. The increasing rate of ISBICLS peaked in 2020 (11.86%), with 57.44% of all surgeons performing ISBICLS
Factors Associated with the Current Adoption of ISBICLS
Surgeons’ Characteristics
A higher percentage of surgeons performing ISBICLS come from optometry departments (65.93% versus 51.76%, P = 0.006), private specialized hospitals (61.06% versus 44.83%, P = 0.002), municipal (34.45% versus 29.31%), or other level of medical institutions (11.76% versus 5.17%, P = 0.027), and had performed higher number of corneal refractive surgeries (80.67% versus 68.39%, P = 0.002) than surgeons who did not perform ISBICLS (Table 1).
Surgeons’ Experience with ICL Surgery
Surgeons currently performing ISBICLS tended to have higher ICL surgery volume during the past year (P = 0.025), have more ICL surgeries overall (P = 0.025), and have lower surgical time per eye (P = 0.001) than surgeons who performed DSBICLS (Table 3). These surgeons also tended to consider parameters measured by Pentacam (83.47% versus 72.41%, P = 0.003) and ultrasound biomicroscope (UBM) (72.27% versus 62.64%, P = 0.024) when designing ICL size. Most surgeons (64.22%) reported modification of the second eye ICL selection according to the postoperative vault of the first eye in < 25% of cases. Surgeons who currently performed ISBICLS were less likely to consider this, compared with those who currently performed DSBICLS (P = 0.037, Table 3).
Most (84.75%) surgeons performed ICL surgery as outpatient or day care surgery. A higher proportion of ICL surgeries were performed as inpatient surgeries among surgeons who did not perform ISBICLS (12.32% versus 21.26%, P = 0.007). The charge for the second eye surgery (P = 0.829) and indicators accounting for individual performance (P = 0.201) did not differ significantly between those currently performing ISBICLS (Table 3).
Logistic Regression Results
The factors that were statistically correlated to performing ISBICLS in univariate logistic regression analysis are presented in Supplementary Table 2. The multivariate logistic regression analysis of factors associated with performing ISBICLS are presented in Table 4. When only adjusting for demographic factors, surgeons who come from private specialized hospitals (OR = 1.724, 95% CI = 1.045–2.843, P = 0.033) were more likely to performed ISBICLS, while those who come from cataract or lens surgery departments (OR = 0.637, 95% CI = 0.422–0.963, P = 0.032) were less likely to perform ISBICLS. However, this association did not achieve significance after we adjusted surgeons’ experience and skills. Surgeons who started performing ICL surgery earlier (before 2010, OR = 2.772, 95% CI = 1.290–5.957, P = 0.009; 2011–2013, OR = 2.479, 95% CI = 1.060–5.800, P = 0.036) and completed one-eye ICL surgery in < 3 min (OR = 3.936, 95% CI = 1.505–10.293, P = 0.005) were more likely to perform ISBICLS. Preoperative measurement devices were not association with their decision of performing DSBICLS or ISBICLS (Pentacam, OR = 1.540, 95% CI = 0.944–2.512, P = 0.084, UBM, OR = 1.427, 95% CI = 0.928–2.194, P = 0.106). In the final fully adjusted model, these associations still persisted and a higher percentage of modifying the second-eye ICL selection according to the first eye’s outcome (1–25%, OR = 0.203, 95% CI = 0.054–0.771, P = 0.019; 26–50%, OR = 0.173, 95% CI = 0.041–0.726, P = 0.017; 51–75%, OR = 0.299, 95% CI = 0.041–0.726, P = 0.123; 76–100%, OR = 0.163, 95% CI = 0.039–0.688, P = 0.014) were less likely to perform ISBICLS.
Surgeons’ Attitudes Regarding ISBICLS and DSBICLS
Overall, 295 (54.63%) supported ISBICLS as a routine procedure compared with 245 (45.37%) who preferred DSBICLS. Most (77.84%) surgeons who performed ISBICLS preferred ISBICLS, but 22.16% of them still preferred DSBICLS.
Reasons for Preferring ISBICLS or DSBICLS
The most common reasons for preferring ISBICLS were the convenience for patient (98.64%), faster recovery of bilateral vision (73.56%), and improved perioperative compliance (73.22%) (Fig. 2A). Higher percentage of surgeons who currently performed ISBICLS (73.67%) agreed that ISBICLS improved perioperative patients’ compliance than those who currently performed DSBICLS (55.56%). Among those preferring DSBICLS, the primary reason for performing DSBICLS was the safety of surgical approach (98.37%) (Fig. 2B).
The reason why surgeons supported immediate sequential bilateral ICL surgery (ISBICLS) or delayed sequential bilateral ICL surgery (DSBICLS) as routine practice. A The most common reasons for preferring ISBICLS were the convenience for patient (98.64%), faster recovery of bilateral vision (73.56%), and improved perioperative compliance (73.22%). B The primary reason for supporting DSBICLS was the safety of surgical approach (98.37%)
Concerns About ISBICLS
Expert consensus was the main concern among surgeons currently performing ISBICLS (62.6%, Fig. 3). Among surgeons performing DSBICLS, they were mainly concerned about the risk of endophthalmitis (76.47%) and vault predictability (74.12%), followed by the risk of other complications (22.98%), visual outcomes (20.90%), patient wishes (12.24%), and hospital policy (18.64%, Fig. 3). Individual financial reasons (2.26%) and insufficient familiarity with sequential bilateral eye surgery (1.32%) were less likely to be reasons for concern than any other factors (Fig. 3).
Surgeons’ concerns about immediate sequential bilateral ICL surgery (ISBICLS). For those who currently performed ISBICLS, the main concern was expert consensus (62.6%). For those who currently performed DSBICLS, the main concern was the risk of endophthalmitis (76.47%) and vault predictability (74.12%), followed by the risk of other complications (22.98%), visual outcomes (20.90%), patient wishes (12.24%), and hospital policy (18.64%)
Desire to Further Adopt or Attempt ISBICLS
The most common desire to support further adoption or attempt ISBICLS was expert consensus on surgical criteria and patient indicators for ISBICLS (82.3%), more evidence regarding effectiveness and safety of ISBICLS (75.71%), and improved ICL surgical design (55.93%). Experience of colleague success in ISBICLS was also important among surgeons currently performing ISBICLS (51.25%, Fig. 4). The other desires, including accurate measurement devices (i.e., intraoperative real-time optical coherence tomography (OCT)) and standardization of sterilization procedure for phakic IOL surgery were mentioned in the free text answer. More detailed opinions or recommendations to the ISBICLS are presented in the Supplementary Material.
Surgeons’ desire for further adoption of immediate sequential bilateral ICL surgery (ISBICLS). The most common desire to support further adoption or attempt ISBICLS was expert consensus on surgical criteria and patient indicators for ISBICLS (82.3%), more evidence regarding ISBICLS effectiveness and safety (75.71%), and improved ICL surgical design (55.93%). Colleague success in ISBICLS was also important among surgeons currently performing ISBICLS (51.25%)
Surgeons Who Abandoned ISBICLS
Four surgeons who have been doing ICL surgeries since 2004, 2010, 2015, and 2016 have abandoned ISBICLS. In 2020, 2011, 2015, and 2018, respectively, they had performed ISBICLS. All of them implanted the ICL V4c model. Two of them preferred ISBICLS and the other two preferred DSBICLS. The reason why they supported ISBICLS or DSBICLS were similar to the total result. All of them reported that they mainly concerned about lack of expert consensus. The other concerns included the increasing risk of endophthalmitis (3/4) and vault predictability (1/4). All of them desired to have expert consensus on surgical criteria and patient indicators for ISBICLS and more evidence regarding effectiveness and safety of ISBICLS.
Discussion
In China, the demand of ICL surgery is booming. Immediate sequential bilateral surgery has greater convenience for patients and improves clinical efficiency, but it remains controversial and lacks standardization. Since refractive surgery has ushered in an era of personalization, establishing uniform rules to carry out ISBICLS or DSBICLS is no longer rational. We identified essential factors to adopt ISBICLS for ICL surgery, hoping to provide a basis for further evidence-based research and revisions of the Chinese expert consensus of PIOL implantation.
In our study, an increasing number of surgeons have started performing ISBICLS in recent decades. The first small spike of ISBICLS was in 2015, 1 year after the introduction of new ICL models, ICL V4c with central hole, in China. We think that the improved safety of the ICL V4c model led to an increase in the number of ISBICLS. The central hole design is proven to improve aqueous humor circulation, which reduces the risk of postoperative excessive intraocular pressure and cataracts. In our clinical practice, peripheral iridotomy can be performed using a neodymium-doped yttrium aluminum-garnet (Nd:YAG) before surgery [24, 25]. Thus, we think the iridotomy in the V4 model did not play a key role in deciding whether bilateral ICL implantation is performed on the same day. According to our data, ICL V4c dominates almost all of the implanted ICL models on the Chinese market (98.31%) as the ICL V5 (19 of 531 responders) and ICL models for hyperopia compensation have not become popularized in China, further studies are needed to explore whether the ICL model may influence the procedure of bilateral ICL surgery. Another peak in ISBICLS occurred in 2020, which could be explained by the fact that the COVID-19 pandemic and the booming demand for refractive surgery prompted hospitals to develop workflows that were both highly efficient and low-contact with patients. Although 67.23% of surgeons currently perform ISBICLS, only 52.16% perform ISBICLS in the majority of cases, and only 54.63% of surgeons prefer ISBICLS as routine practice. These results suggest that ISBICLS has been gradually adopted among surgeons, but it has not been accepted as routine procedure in Mainland China.
The benefits of ISBICLS for patient convenience were commonly accepted by surgeons, which was consistent with previous reports [16, 17]. Interestingly, those who performed ISBICLS tend to believe that ISBICLS may have more potential advantages in clinical outcomes, such as improved perioperative compliance. The medication administration in the early perioperative period that differed between bilateral eyes in DSBICLS may inconvenience patients. In the early postoperative period, the inappropriate usage of prednisolone acetate may lead to steroid intraocular pressure elevation, especially in high myopia. Patients’ compliance and perceptions towards ISBICLS and DSBICLS remains to be explored in further study.
Almost all surgeons who preferred DSBICLS were concerned about the safety of ISBICLS. Endophthalmitis (infectious or aseptic) after ICL surgery has rarely been reported but has serious consequences [26,27,28,29]. Until recently, management of post-ICL endophthalmitis still follows the recommendations for cataract surgery [12]. However, ICL implantation differs from cataract surgery, with younger surgical populations, less comorbidities, simpler surgical procedure, shorter surgical time, and faster recovery. Routine preventive treatments such as intracameral antibiotic injection in cataract surgery, and patient indicators for ISBCS [12, 13] may not be applicable in ICL surgery. In our study, most surgeons reported concerns regarding the risk of endophthalmitis, especially among those who did not perform ISBICLS. We also found that surgeons from cataract departments were less likely to perform ISBICLS in our first logistic regression model, because they may be more familiar with delayed sequential bilateral cataract surgery (DSBCS). More detailed regulations related to perioperative sterilization measures (e.g., changing operating instruments, operating tables, or even operating rooms) for ICL surgery are necessary for the safe practice of ISBICLS.
Vault considerations also affect the choice of ISBICLS or DSBICLS. This was another common concern for those who had never performed ISBICLS. Previous studies proposed that DSBICLS can be used to adjust the size of the second eye based on vault of the first eye 1 day after surgery, thus decreasing the risk of bilateral ICL size exchange [21, 22, 30]. According to our results, although the percentage of such cases was negatively associated with performing ISBICLS, most surgeons reported that it occurred less than 25% of the time. Thus, DSBICLS was performed to improve surgical outcomes only in specific cases rather than routine practice.
In addition, the time interval for bilateral eye surgery also differed among surgeons. In terms of performing ISBICLS, almost one third of surgeons reported that they performed bilateral surgery in separate sessions (with a delay of over 30 min after the first surgery), which may be an alternative choice for ISBICLS. When performing DSBICLS, most (85.05%) surgeons in our survey chose to perform the second eye surgery 1 day later (Table 2). However, the vault on the first postoperative day may not be stable enough to provide a reliable reference [25, 31, 32], while too long of an interval may cause inconvenience to the patient. Studies are needed to determine the reasonable time interval for the better predictability of vault surgical safety.
To further explore factors related to the practice of ISBICLS, we investigated surgeons’ experience and skills with ICL surgery, preoperative devices, and hospital management factors. As expected, the most crucial factor was the surgeon experience with ICL surgery. Surgeons who currently performed ISBICLS had started ICL surgery earlier, had higher annual or total surgical volume, and completed one-eye surgery faster. The numbers of years performing ICL surgery and one-eye surgical time were significantly associated with performing ISBICLS, which suggested that more experienced and skilled surgeons may have the ability to treat corresponding complications to ensure the safe outcomes. Consistently, more surgeons who performed DSBICLS were concerned about vault predictability (Fig. 3), possibly due to lack of experience with ICL selection and surgical skills. Thus, ISBICLS may not be suitable for beginners and is recommended for skilled surgeons. Studies are needed to determine whether surgeons can perform ISBICLS during their learning curve. However, surgeons desired improved ICL surgical design rather than training for surgical skills. Further studies are needed to explore more factors of the surgical teams (including the operative designers).
According to our data, Pentacam and UBM measurements were the main preoperative devices when designing ICL size, and were used more often by those who performed ISBICLS. However, no significant association was found between the devices with adoption of ISBICLS. The manufacturer provided STAAR Surgical Online Calculation & Ordering System (OCOS™) based on white to white (WTW), and anterior chamber depth (ACD) measured by Pentacam are used as standard methods [33]. In addition, the UBM could provide a more accurate assessment of the ciliary sulcus morphology in customized design of ICL size [34,35,36,37], although its repeatability depends largely on the operator’s skill [38]. Real-time OCT is also mentioned by two surgeons in the free text answers to improve the predictability of postoperative vault. These results suggest that accurate preoperative measurement devices may improve the predictability of the postoperative vault and help the adoption of ISBICLS.
The inconvenience to patient daily life caused by unilateral vision loss within the perioperative period may increase the demand for DSBICLS. Thus, we hypothesize that the categories of surgical management may affect the adoption of ISBICLS. In our study, a higher percentage of ISBICLS were performed as outpatient surgeries, and surgeons in private specialized hospitals were more likely to perform ISBICLS. This can be explained by the fact that private hospitals have less hospital beds than public medical institutions in Mainland China [39] and suggests the potential advantage of ISBICLS in improving clinical efficiency. However, this did not achieve a significant association with the outcome after we adjusted for surgeons’ experiences, which suggested that the clinical settings were not the main factors influencing the adoption of ISBICLS when the surgeon had sufficient surgical skills to ensure the surgical safety.
No significant difference was found for performing ISBICLS regarding the other economic factors, including the number of surgical eyes affecting personal individual income and charge for the second eye. Moreover, individual financial reasons were the concern of only 2.26% of surgeons. Thus, the main factors associated with adoption of ISBICLS were regarding surgical safety and predictability, including surgeons’ experience, skills, and vault considerations, rather than the hospital policy or economic factors. Our results inform the future revision of existing expert consensus on PIOL implantation, which was also the most desirable support for the adoption of ISBICLS in our study. Interestingly, out of four surgeons that abandoned ISBICLS in favor of DSBICLS, three had performed ISBICLS before the 2019 Chinese expert consensus of PIOL was published and one surgeon performed ISBICLS in 2020 and then stopped. All of them were mainly concerned about the lack of expert consensus. Thus, we think one of the main cause for abandoning ISBICLS was the medicolegal issues. Actually, our data demonstrated that surgeons currently performing ISBICLS were also concerned about the lack of expert consensus. As an EVO-ICL refractive surgery center with the largest single-center surgical volume in China, we have been through the process of abandoning ISBICLS to DSBICLS due to medicolegal issues, and then finally back to ISBICLS owing to the increased demand for ICL surgery. Future revision may include standardized protocols to prevent endophthalmitis, the appropriate time interval of two eye surgery, and requisitions for surgeon skills and devices. Additional studies are needed to explore the feasibility of ISBICLS in various clinical settings.
To the best of our knowledge, this is the first large-scale survey on the status of practicing ISBICLS and surgeon perceptions regarding adopting ISBICLS, covering all 30 provinces where ICL surgery is available in Mainland China. Our participants come from a variety of geographical locations and medical institution levels, which is one of our strength as we captured the wide range of surgeons’ attitudes and experiences.
Our study had several limitations. First, our study was cross sectional. Although we demonstrated some factors were associated with performing ISBICLS, causal and temporal relationships could not be inferred (e.g., surgical volume). Second, the results were self reported and may introduce reporting bias or recall bias. The detailed information (e.g., when to start, surgical volume) may be over- or underestimated. Third, even though we eliminated a number of possible confounders, there may still be some residual confounders from unmeasured factors, such as the surgical procedures (e.g., the sterilization procedures between the two-eye surgeries) and the rate of complications. Finally, four surgeons had stopped performing ISBICLS, we analyzed their answer separately, and attributed the reason why the abandoned ISBICLS partly to medicolegal issues. However, we did not directly ask them the reason why they stopped performing ISBICLS, so further studies are needed to explore the other factors influencing the adoption of ISBICLS.
Conclusions
In recent decades, increasing numbers of surgeons in Mainland China are performing ISBICSL; however, ISBICLS has not been accepted as routine practice. ISBICLS may benefit patients in convenience and improve their perioperative compliance. The appropriate surgical procedures must be chosen by considering a variety of factors, especially the surgeon’s experience, skills, and vault considerations. Both risks of endophthalmitis and vault predictability should be the predominant factors in determining the appropriate workflow of ICL surgery. Perioperative sterilization for ICL surgery needs to be standardized in detail, instead of following the management of cataract surgery. Additional studies are needed to determine the reasonable time interval for the better predictability of vault. For future better practice of ICL surgery, a set of applicable and standardized surgical protocols remains to be explored to provide evidence for the revision of expert consensus.
References
Kim T, Alió Del Barrio JL, Wilkins M. Refractive surgery. Lancet. 2019;393(10185):2085–98 (10/gf3knp).
STAAR surgical celebrates two million lens milestone for implantable Collamer® lens (ICL). Bus Wire. Accessed June 26, 2022. https://www.businesswire.com/news/home/20220607005138/en/.
Ieong A, Hau SCH, Rubin GS, Allan BDS. Quality of life in high myopia before and after implantable collamer lens implantation. Ophthalmology. 2010;117(12):2295–300 (10/cbrjhn).
Igarashi A, Shimizu K, Kamiya K. Eight-year follow-up of posterior chamber phakic intraocular lens implantation for moderate to high myopia. Am J Ophthalmol. 2014;157(3):532-539.e1. https://doi.org/10.1016/j.ajo.2013.11.006.
Shen Y, Du C, Gu Y, Wang J. Posterior chamber phakic intraocular lens implantation for high myopia. Chin Med J (Engl). 2003;116(10):1523–6.
Wang X, Zhou X. Update on treating high myopia with implantable collamer lenses. Asia Pac J Ophthalmol (Phila). 2016;5(6):445–9. https://doi.org/10.1097/APO.0000000000000235.
Montés-Micó R, Pastor-Pascual F, Artiaga-Elordi E, Ruiz-Mesa R, Tañá-Rivero P. In vivo optical quality of posterior-chamber phakic implantable collamer lenses with a central port. Eye Vis (Lond). 2021;8(1):30. https://doi.org/10.1186/s40662-021-00251-5.
Alfonso J, Fernández-Vega-Cueto L, Alfonso-Bartolozzi B, Montés-Micó R, Fernández-Vega L. Five-year follow-up of correction of myopia: posterior chamber phakic intraocular lens with a central port design. J Refract Surg. 2019;35(3):169–76. https://doi.org/10.3928/1081597X-20190118-01.
Martínez-Plaza E, López-Miguel A, López-de-la-Rosa A, McAlinden C, Fernández I, Maldonado MJ. Effect of the EVO+ visian phakic implantable collamer lens on visual performance and quality of vision and life. Am J Ophthalmol. 2021;226:117–25. https://doi.org/10.1016/j.ajo.2021.02.005.
Wang Y, Li J. Problems and challenges in the development of corneal refractive surgery. Zhonghua Yan Ke Za Zhi. 2018;54(1):3–6 (10/gqck6w).
Ahmed IIK, Hill WE, Arshinoff SA. Bilateral same-day cataract surgery: an idea whose time has come #COVID-19. Ophthalmology. 2021;128(1):13–4 (10/ghfkkg).
Chinese ophthalmology C. Chinese expert consensus on phakic intraocular lens implantation. Chin J Ophthalmol. 2019;55(9):652–7. https://doi.org/10.3760/cma.j.issn.0412-4081.2019.09.005.
German Society of Ophthalmology (Deutsche Ophthalmologische Gesellschaft DOG), Professional Association of German Ophthalmologists (Berufsverband der Augenärzte Deutschlands e.V., BVA). Evaluation and quality assurance of refractive surgery by the German Society of Ophthalmology and the Professional Association of German Ophthalmologists-Commission for refractive surgery recommendations: status. Ophthalmologe. 2020;117(1):25–35. https://doi.org/10.1007/s00347-019-00986-6.
Chuck RS, Jacobs DS, Lee JK, et al. Refractive errors and refractive surgery preferred practice Pattern®. Ophthalmology. 2018;125(1):P1–104. https://doi.org/10.1016/j.ophtha.2017.10.003.
Chung JK, Pak K, Ha SJ, Choi KS. Clinical outcomes of and immediate sequential bilateral phakic intraocular lens implantation effect of the lens size on central vault of implantable collamer lens implantation. Invest Ophthalmol Vis Sci. 2019;60(9):3694.
Malwankar J, Son HS, Chang DF, et al. Trends, factors, and outcomes associated with immediate sequential bilateral cataract surgery among medicare beneficiaries. Ophthalmology. 2021. https://doi.org/10.1016/j.ophtha.2021.12.015 (Published online December).
Lansingh VC, Eckert KA, Strauss G. Benefits and risks of immediately sequential bilateral cataract surgery: a literature review. Clin Exp Ophthalmol. 2015;43(7):666–72 (10/f7tqm9).
Lacy M, Kung TPH, Owen JP, et al. Endophthalmitis rate in immediately sequential versus delayed sequential bilateral cataract surgery within the Intelligent Research in Sight (IRIS) Registry Data. Ophthalmology. 2021. https://doi.org/10.1016/j.ophtha.2021.07.008 (Published online July 2021).
Owen JP, Blazes M, Lacy M, et al. Refractive outcomes after immediate sequential vs delayed sequential bilateral cataract surgery. JAMA Ophthalmol. 2021;139(8):876. https://doi.org/10.1001/jamaophthalmol.2021.2032.
Herrinton LJ, Liu L, Alexeeff S, Carolan J, Shorstein NH. Immediate sequential vs delayed sequential bilateral cataract surgery. Ophthalmology. 2017;124(8):1126–35. https://doi.org/10.1016/j.ophtha.2017.03.034.
Kim WK, Kim JK. The benefits of one day, one eye surgery in bilateral ICL implantation. J Korean Ophthalmol Soc. 2013;54(7):1019–24.
Kim BK, Chung YT. Clinical results of Visian implantable collamer lens implantation according to various sizes and implantation angles. Eur J Ophthalmol. 2021. https://doi.org/10.1177/11206721211033468 (Published online 2021).
Teichmann KD. Simultaneous bilateral LASIK. J Cataract Refract Surg. 2000;26(10):1434–5 (10/b4x3zs).
Chen H, Niu G, Fan Y, Ma J. Comparison of intraocular pressure andvault after implantation of implantable collamer lens with and without a central hole. BMC Ophthalmol. 2016;16(1):203. https://doi.org/10.1186/s12886-016-0375-1.
Chen X, Miao H, Naidu RK, Wang X, Zhou X. Comparison of early changes in and factors affecting vault following posterior chamber phakic Implantable Collamer Lens implantation without and with a central hole (ICL V4 and ICL V4c). BMC Ophthalmol. 2016;16(1):161. https://doi.org/10.1186/s12886-016-0336-8.
Scott IU, Flynn HW, Feuer W. Endophthalmitis after secondary intraocular lens implantation. A case-report study. Ophthalmology. 1995;102(12):1925–31. https://doi.org/10.1016/S0161-6420(95)30774-9.
Allan BD, Argeles-Sabate I, Mamalis N. Endophthalmitis rates after implantation of the intraocular Collamer lens: survey of users between 1998 and 2006. J Cataract Refract Surg. 2009;35(4):766–9. https://doi.org/10.1016/j.jcrs.2008.12.027.
Taneri S, Kießler S, Rost A, Schultz T, Elling M, Dick HB. Atypical endophthalmitis after intraocular collamer lens implantation. J Cataract Refract Surg. 2018;44(12):1521–3. https://doi.org/10.1016/j.jcrs.2018.08.010.
Al-Abdullah AA, Al-Falah M, Al-Rashaed S, Khandekar R, Arevalo JF. Endophthalmitis caused by rhizobium radiobacter after posterior chamber phakic intraocular lens implantation to correct myopia. J Refract Surg. 2015;31(8):561–3. https://doi.org/10.3928/1081597X-20150728-02.
Cerpa Manito S, Sánchez Trancón A, Torrado Sierra O, Baptista A, Serra P. Inter-eye vault differences of implantable collamer lens measured using anterior segment optical coherence tomography. Clin Ophthalmol. 2020;14:3563–73. https://doi.org/10.2147/OPTH.S258817.
Zhu QJ, Chen WJ, Zhu WJ, et al. Short-term changes in and preoperative factors affecting vaulting after posterior chamber phakic Implantable Collamer Lens implantation. BMC Ophthalmol. 2021;21(1):199. https://doi.org/10.1186/s12886-021-01963-x.
Guan N, Zhang XN, Zhang WJ. Correlation between intraoperative and postoperative vaulting of the EVO implantable Collamer lens: a retrospective study of real-time observations of vaulting using the RESCAN 700 system. BMC Ophthalmol. 2022. https://doi.org/10.1186/s12886-021-02237-2.
OCOS STAAR AG. STAAR Surgical Online Calculation & Ordering System. Accessed July 10, 2022. https://ocos.staarag.ch/landing/.
Kojima T, Yokoyama S, Ito M, et al. Optimization of an implantable collamer lens sizing method using high-frequency ultrasound biomicroscopy. Am J Ophthalmol. 2012;153(4):632-637.e1. https://doi.org/10.1016/j.ajo.2011.06.031.
Du C, Wang J, Wang X, Dong Y, Gu Y, Shen Y. Ultrasound biomicroscopy of anterior segment accommodative changes with posterior chamber phakic intraocular lens in high myopia. Ophthalmology. 2012;119(1):99–105. https://doi.org/10.1016/j.ophtha.2011.07.001.
Zhang X, Chen X, Wang X, Yuan F, Zhou X. Analysis of intraocular positions of posterior implantable collamer lens by full-scale ultrasound biomicroscopy. BMC Ophthalmol. 2018;18(1):114. https://doi.org/10.1186/s12886-018-0783-5.
Wei R, Cheng M, Niu L, et al. Outcomes of the EVO ICL using a customized non-horizontal or horizontal implanting orientation based on UBM measurement: a pilot study. Ophthalmol Ther. 2022. https://doi.org/10.1007/s40123-022-00498-8 (Published online April 12, 2022).
Guber I, Bergin C, Perritaz S, Majo F. Correcting interdevice bias of horizontal white-to-white and sulcus-to-sulcus measures used for implantable collamer lens sizing. Am J Ophthalmol. 2016;161:116-125.e1. https://doi.org/10.1016/j.ajo.2015.09.037.
Yip WCM, Hsiao WC, Chen W, Hu S, Ma J, Maynard A. Early appraisal of China’s huge and complex health-care reforms. Lancet. 2012;379(9818):833–42 (10/f2fgs4).
Acknowledgements
We thank Gang Chen and Xiaohua Ying from the School of Public Health of Fudan University for their contribution to the questionnaire consultation.
Funding
Funding for this study, including the journal’s Rapid Service Fee, came from the following: 1) Xiaoying Wang; National Natural Science Foundation of China (Grant No. 81770955 and 82171095). 2) Xingtao Zhou; Project of Shanghai Science and Technology (Grant No.20410710100). 3) Xiaoying Wang; Project of Shanghai Science and Technology (Grant No. 19140900700). 4) Xingtao Zhou; Clinical Research Plan of SHDC (Grant No. SHDC2020CR1043B). 5) Xingtao Zhou; Project of Shanghai Xuhui District Science and Technology (Grant No. 2020-015, XHLHGG202104). 6) Xingtao Zhou; Shanghai Engineering Research Center of Laser and Autostereoscopic 3D for Vision Care (Grant No. 20DZ2255000). 7) Xingtao Zhou; Construction of a 3D digital intelligent prevention and control platform for the whole life cycle of highly myopic patients in the Yangtze River Delta (Grant No. 21002411600).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
The authors were involved in the conception or design of the work(YJJ,XC, XTZ, XYW), the acquisition of data for the work((YJJ,XC, MRC,BLL,YDL, YLX), the analysis or interpretation of data for the work (YJJ,XC); drafting the work or revising it critically for important intellectual content (YJJ,XC); final approval of the version to be published (YJJ,XC, MRC,BLL,YDL, YLX, XTZ, XYW); agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved(YJJ,XC, MRC,BLL,YDL, YLX, , XTZ XYW). All authors read and approved the final manuscript.
Disclosures
Yinjie Jiang, Xun Chen, Mingrui Cheng, Boliang Li, Yadi Lei, Yilin Xu, Xingtao Zhou and Xiaoying Wang have nothing to disclose.
Compliance with Ethics Guidelines
This study adhered to the tenets of the Declaration of Helsinki and was approved by the Ethical Committee Review Board of Fudan University Eye and ENT Hospital (2021018). Consent was obtained from the participants that the data would be used as part of a study.
Data Availability
The datasets during and/or analysed during the current study available on reasonable request from the corresponding author.
Author information
Authors and Affiliations
Corresponding authors
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Jiang, Y., Chen, X., Cheng, M. et al. Immediate or Delayed Sequential Bilateral ICL Surgery: a Survey of Chinese Ophthalmologists. Ophthalmol Ther 12, 217–237 (2023). https://doi.org/10.1007/s40123-022-00599-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40123-022-00599-4