Abstract
Purpose
To evaluate changes in cataract and refractive surgery practice patterns among members of the Japanese Society of Cataract and Refractive Surgery (JSCRS) over the past 20 years.
Study design
Questionnaire survey study.
Subjects and methods
Clinical surveys were conducted annually between February and April from 2004 to 2023. Survey questions covered various areas, including cataract surgical techniques, anesthesia, endophthalmitis prophylaxis, toric and presbyopia-correcting intraocular lenses (IOLs), complications, and refractive surgery.
Results
The highest (n=554 [36.8%]) and lowest (n=316 [19.1%]) numbers of responses were collected in 2012 and 2016, respectively. In perioperative management, the intraoperative use of polyvinyl alcohol-iodine solution and topical antibiotic prescription 3 days before surgery has increased. The use of intracameral injection at the end of surgery has also significantly increased, although it has not been established as common practice. In anesthesia, there is a clear polarization between the use of topical drops and tenon injection. The use of toric IOLs and presbyopia-correcting IOLs has significantly increased from 2010 to 2023. In the latter, the use of trifocal IOLs has particularly increased. Regarding IOL power calculations, the Barrett True K and the Barrett Universal II formulas are rapidly gaining popularity for application with and without post-laser vision correction, respectively. In refractive surgery, phakic IOLs and corneal refractive therapy have attracted considerable interest, followed by laser in situ keratomileusis.
Conclusions
Evaluation of annual clinical survey data over the past two decades provided valuable insights into the shifting practice patterns and clinical opinions among JSCRS members.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trends in both intraocular lenses (IOLs) and surgical techniques tend to change. Therefore, it is crucial to understand the current trends in cataract, IOL, and refractive surgery in Japan to avoid malpractice and deviation from global standards.
The American Society of Cataract and Refractive Surgery (ASCRS) and the European Society of Cataract and Refractive Surgeons (ESCRS) conduct annual surveys involving their members [1,2,3]. Similar annual surveys are conducted in other countries, such as Germany, New Zealand, Canada, and South Korea [4,5,6,7]. In addition, the ASCRS reports details of changes in the use of antibiotic prophylaxis against postoperative endophthalmitis after cataract surgery based on the results of annual surveys [8].
For the past 30 years, the Japanese Society of Cataract and Refractive Surgery (JSCRS) has conducted an annual clinical survey to understand the trends in anterior segment surgery in Japan. The results are presented at the annual meeting of the JSCRS, and reviewed in Japanese; the last report in English was published in 2001 [9]. In this study, we analyzed interesting changes in the practice patterns for cataract and refractive surgery among JSCRS members over the past 20 years.
Materials and methods
Clinical surveys were conducted annually between February and April from 2004 to 2023. Data were collected by mail until 2011 and online since 2012. The survey was anonymous, and careful attention was paid to the content of the questions and the handling of aggregated results to avoid bias in favor of specific interested parties.
All questions were reviewed and updated annually to remain current and relevant. Although the number of questions varied considerably over the years (range: 43–63), several key questions were repeated to identify trends. Changes that have been tracked for at least 7 years are described, and the most recent data included in the analysis were collected from 2018 onward. Because the content of the questions varies annually, the data are presented in a discontinuous rather than an annual format.
The survey questions were developed through discussions between the members of the JSCRS Data Analysis Committee, and covered various areas, including age, sex, workplace, monthly volume of cataract surgery, endophthalmitis prophylaxis (perioperative use of ocular surface solution, prescription of antibiotics, and surgical antibiotic administration), anesthesia techniques, cataract surgical techniques (incision construction, site, size, capsulorhexis and femtosecond laser), presbyopia-correcting and toric IOLs, IOL power calculations, postoprerative complications (management of refractive error and posterior capsule rupture [PCR] rate), and refractive surgery. In four questions regarding the types of presbyopia-correcting IOLs used, the IOL power calculation formulas used, the type of refractive surgery performed, and the views of respondents on refractive procedures, multiple answers were allowed. Multiple responses to questions that requested a single answer, except for the above four questions, were excluded from the tally.
Data analysis
Personal computer database software (Excel 2021 Ver.16.7; Microsoft) was used for data analysis. For each question, proportions were determined based on the percentage of respondents who selected each response. To determine the overall mean score for questions, the proportion of respondents for a given range was multiplied by the midpoint of that range. The resulting products were summed, and the sums were used to represent an overall mean score.
Results
Demographics
Table 1 shows the demographics of respondents who participated in the annual JSCRS survey. Over the past 20 years, despite a slight downward trend in the response rate, the number of survey respondents has been relatively similar. Due to the online nature of the survey, the number of respondents after 2020 was not affected by the coronavirus 2019 pandemic.
Private clinics were the most common type of workplace for respondents each year (252 [49.1]—263 [62.9%]). The question on sex was introduced in 2019, with men accounting for approximately 80% of the respondents. The majority of respondents were aged 50–59 and 40–49 years, accounting for approximately ≥60% of all respondents. The proportion of respondents aged 30–39 years decreased from 21% (2004; 95% confidence interval [CI], 17.3–25.1%) to 9% (2023; 95% CI, 6.4–12.0%), whereas the proportion of those aged 60-69 years increased from 11% (2004; 95% CI, 7.7–13.7%) to 24% (2023; 95% CI, 19.7–28.1%). The age of respondents tended to increase slightly annually, suggesting that some members responded each year. The results demonstrate that the average monthly number of cataract surgeries per respondent has remained between 30 and 40 over the long term, with some variation observed between years. (Fig. 1). Compared to 39 (95% CI, 29.7–48.8) in 2020, a slight decrease in volume was noted in 2021 (32; 95% CI, 28.1–35.4). In 2023, this volume has not yet returned to pre-pandemic levels.
Endophthalmitis prophylaxis
Preoperative eyewash and intraoperative surface irrigation
In 2004, povidone-iodine (PI) solution was the most commonly used preoperative antiseptic (59%; 95% CI, 53.8–63.6%), while polyvinyl alcohol-iodine (PAI) solution was used by only 10% (95% CI, 6.9–12.9%), of respondents (Fig. 2a). However, the number of surgeons using PAI has rapidly increased, accounting for 32% (95% CI, 27.9–36.3%), 48% (95% CI, 42.6–54.2%), and 64% (95% CI, 58.5–68.7%), of respondents in 2011, 2016, and 2023, respectively. In contrast, chlorhexidine, used by 13% (95% CI, 9.9–16.7%) of respondents in 2004, was rarely used (2%; 95% CI, 0.4–3.2%) in 2023.
Intraocular irrigation solution was the most common liquid sprayed onto the ocular surface intraoperatively (57% [95% CI, 52.6–62.2%] and 46% [95% CI, 41.2–51.4%] of respondents in 2015 and 2022, respectively) (Fig. 2b). The use of PI and PAI increased from 10% (2015; 95%CI, 7.3–13.1%) to 16% (2022; 95%CI, 11.8–19.2%) and from 10% (2015; 95%CI, 7.5–13.3%) to 22% (2022; 95%CI, 17.3–25.8%), respectively, demonstrating the increasing use of iodine products.
Perioperative prescription of antibiotics
Figure 3 shows the prescription patterns for preoperative and postoperative topical antibiotics. The number of surgeons initiating administration of antibiotic drops 3 days preoperatively has markedly increased, accounting for 39% (95% CI, 34.0–43.6%), 61% (95% CI, 56.2–65.0%), 78% (95% CI, 73.5–81.5%), and 87% (95% CI, 83.9–90.9%), of respondents in 2004, 2010, 2015, and 2023, respectively (Fig. 3a). Regarding the duration of postoperative administration of topical antibiotics, the number of surgeons who discontinued antibiotics after 2 weeks has gradually increased, accounting for 11% (95% CI, 8.0–14.4%), 21% (95% CI, 17.4–25.2%), and 33% (95% CI, 27.5–38.0%) of respondents in 2006, 2015, and 2023, respectively (Fig. 3b). The number of surgeons who discontinued the administration of topical antibiotics after 2 months decreased from 21% (2006; 95% CI, 16.4–24.6%) to 6% (2023; 95% CI, 3.6–8.8%). The corresponding number after 3 months decreased from 33% (2006; 95% CI, 27.8–37.2%) to 4% (2023; 95% CI, 1.5–5.5%). The number of surgeons who discontinued the administration of topical antibiotics after ≤1 week has remained at approximately <20% annually since the option was introduced in 2021. The combination of data for ≤1 week and 2 weeks revealed that, in recent years approximately half of the surgeons discontinued the administration of topical antibiotics within 2 weeks.
Figure 4 shows the practice for oral or systemic antibiotic prophylaxis. The number of surgeons prescribing oral antibiotics for 4-5 days decreased gradually from 34% (2006; 95% CI, 29.1–38.7%) to 10% (2023; 95% CI, 6.4–12.6%). In contrast, the number of surgeons prescribing oral antibiotics for 2-3 days peaked in 2014 (61%; 95% CI, 56.4–66.2%), followed by an annual decline. The number of respondents who do not prescribe oral antibiotics has significantly increased from 7% (2006; 95% CI, 4.3–9.5%) to 52% (2023; 95% CI, 47.1–57.7%) (Fig. 4a). Overall, the duration of oral administration has been shortened. The number of respondents who do not administer intravenous antibiotics has also increased significantly from 46% (2012; 95% CI, 41.9–50.7%) to 80% (2023; 95% CI, 75.4–84.0%), possibly due to concerns regarding the emergence of resistance (Fig. 4b).
Surgical antibiotic administration
Figure 5 shows the practice for surgical antibiotic administration. The number of surgeons performing subconjunctival injections has decreased gradually from 39% (95% CI, 33.2–43.8%) in 2005 to 11% (95% CI, 7.8–14.6%) in 2023 (Fig. 5a). Among those using intraocular antibiotic prophylaxis, antibiotic infusion through the irrigation bottle was used by 25% (95% CI, 19.8–29.2%), 22% (95% CI, 17.8–26.2%), and 16% (95% CI, 12.0–19.8%) of all respondents in 2005, 2014, and 2023, respectively (Fig. 5b). Although not rapidly, it has been on a gradual downward trend over the past 20 years. In contrast, an almost eight-fold increase in the preference for intracameral (IC) injections was observed from 2005 to 2023 (4% [95% CI, 1.9–6.1%] and 31% [95% CI, 26.0–35.8%] in 2005 and 2023, respectively) (Fig. 5c). Figure 5d shows the rate of IC injections’ use according to the type of workplace in the last 5 years. In university hospitals, the rate was <10% annually, differing considerably from the rates recorded in other types of workplace.
Surgical antibiotic administration. a Subconjunctival injection at conclusion of surgery (2005–2023). b Irrigation bottle infusion (2005–2023). c Intracameral injection at conclusion of surgery (2005–2023). d Percentage of respondents performig intracameral injection according to the type of workplace in the last 5 years (2019–2023)
Figure 6 shows the drug preferences of surgeons using intraocular antibiotic prophylaxis. For antibiotics in irrigation bottles, the preference for fluoroquinolones has increased from 7% (95% CI, 5.0–12.0%) in 2006 to 33% (95% CI, 20.7–45.9%) in 2023, with no increase in the preference for other drugs (Fig. 6a). In terms of antibiotic preference for a direct IC injection at the conclusion of surgery, the use of fluoroquinolones has been very popular at around 70% each year since this question was first initiated in 2015, followed by carbapenems (Fig. 6b).
Drug preferences for those using intraocular antibiotic prophylaxis. a Antibiotics placed in an irrigation bottle (2006–2023). "Fluoroquinolone" and "glycopeptide" have been introduced as one of the options since 2011 and 2015, respectively. b Direct intracameral antibiotic injection at the conclusion of surgery (2015–2023)
Anesthesia
The percentage of surgeons using retrobulbar anesthesia has markedly decreased: 26% (95% CI, 21.3–29.9%) in 2004 and 3% (95% CI, 1.1–4.5%) in 2022 (Fig. 7). In contrast, IC anesthesia has gradually become more popular in recent years (3% [95% CI, 1.0–4.2%] in 2004, 13% [95% CI, 9.4–16.0%] in 2019, and 21% [95% CI, 16.8–25.2%] in 2022). Currently, there appears to be a marked polarization between the use of topical drops and tenon injection.
Incision
Figure 8a shows preferred incision construction for phacoemulsification and aspiration (PEA). The rate of scleral tunnel incision (STI) decreased significantly from 79% (95% CI, 74.9–82.3%) in 2004 to 27% (95% CI, 22.2–31.2%) in 2019. On the other hand, the rate of clear corneal incision (CCI) increased from 21% (95% CI, 17.6–25.0%) to 40% (95% CI, 34.4–44.4%), and this technique became the preferred option. The rate of transconjunctival single-plane sclerocorneal incision (TSSI) [10] increased from 16% (95% CI, 12.6–18.6%) in 2010 to 34% (95% CI, 28.8–38.4%) in 2019, surpassing STI and approaching CCI in 2019.
Incision. a Preferred incision construction (2004–2019). "TSSI" has been introduced as one of the options since 2010. b Preferred incision site (2004–2019). c Preferred incision size (2008–2023). CCI clear corneal incision, STI scleral Tunnel incision, TSSI transconjunctival single-plane sclerocorneal incision
Figures 8b and 8c show the preferred incision site and size, respectively. From 2004 to 2019, the rate of superior incisions decreased from 35% (95% CI, 30.6–39.6%) to 26% (95% CI, 21.8–30.8%), while that of temporal incisions gradually increased from 17% (95% CI, 13.6–20.6%) to 27% (95% CI, 22.3–31.3%). Overall, except for 2009 and 2010, oblique incisions have been the preferred during the study period.
For PEA, there was a marked decreasing trend in incisions’ size: ≥3.1 mm from 2008 (36% [95% CI, 32.1–40.7%]) to 2023 (2% [95% CI, 0.4–3.2%]). In contrast, the incision size ≤2.2 mm and 2.3–2.4 mm increased significantly from 5% (95% CI, 2.7–6.3%) to 13% (95% CI, 9.1–16.1%) and from 9% (95% CI, 6.8–12.0%) to 59% (95% CI, 53.7–64.0%), respectively. These data indicate that the incision size is continuously being reduced, although the limiting value is unknown.
Capsulorhexis
Figure 9 shows preferred instruments for capsulorhexis. From 2004 to 2018, the use of cystotome decreased from 74% (95% CI, 69.8–78.4%) to 44% (95% CI, 38.6–48.4%), whereas that of forceps increased from 18% (95% CI, 13.9–21.3%) to 43% (95% CI, 37.8–47.6%). Only 1% of surgeons performed capsulotomy mainly using femtosecond laser (2018).
From 2013 to 2023, the percentage of surgeons performing femtosecond laser-assisted cataract surgery (FLACS) in some cases increased from 2% (95% CI, 0.4–2.6%) to 9% (95% CI, 6.0–12.2%) (Fig. 10). These results indicate that, currently, most surgeons mainly use conventional PEA, although the number of surgeons using FLACS is increasing.
Toric IOL
Between 2010 and 2023, the percentage of surgeons using toric IOLs increased from 28% (95% CI, 23.6–31.8%) to 87% (95% CI, 83.8–91.0%) (Fig. 11a). From 2016 to 2023, the proportion of all monofocal IOL cases in which toric IOLs were used increased from 6% (95% CI, 4.8–6.5%) to 11% (95% CI, 9.3–11.7%) (Fig. 11b). Use of toric IOLs was most commonly considered for corneal astigmatism with “≥1.5 diopter”, without remarkable change observed from 2013 to 2022 (Fig. 12).
Presbyopia-correcting IOL
From 2010 to 2023, the percentage of surgeons using presbyopia-correcting IOLs increased from 28% (95% CI, 24.2–32.4%) to 60% (95% CI, 54.6–65.0%), not reaching the extent noted for toric IOLs (Fig. 11a). The proportion of all cases in which presbyopia-correcting IOLs are used increased from 2% (95% CI, 1.7–3.1%) to 5% (95% CI, 4.2–6.1%) between 2016 and 2020, and decreased to 4% (95% CI, 3.0–4.5%) in 2021 (Fig. 11b). There has been no increasing trend since then.
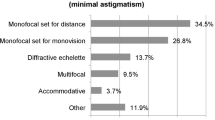
Figure 13 shows the types of presbyopia-correcting IOLs used (multiple choices allowed). Between 2015 and 2023, the use of bifocal IOLs decreased from 83% (95% CI, 77.2–88.4%) to 26% (95% CI, 20.0–32.0%), whereas that of trifocal IOLs increased from 2% (95% CI, 0.0–3.6%) to 80% (95% CI, 75.0–85.8%). The use of extended depth of focus IOLs decreased from 62% (95% CI, 55.4–69.0%) at launch in 2018 to 44% (95% CI, 37.3–50.9%) in 2023. Continuous range of vision IOLs rapidly became popular following their launch in 2021 (60% [95% CI, 53.6–67.0%]; 2023).
IOL power calculation
Figure 14 shows the IOL power calculation formulas used in routine cataract cases, regardless of the ocular axis length (multiple choices allowed). The SRK/T formula was consistently the most commonly used from 2011 to 2023. Notably, the number of surgeons using the Barrett Universal II formula markedly increased from 32% (95% CI, 27.8–37.0%) in 2018 to 72% (95% CI, 67.3–76.9%) in 2023. There was no obvious increase in the use of any other formula.
The percentage of surgeons who performed lens reconstruction after laser vision correction (LVC) in the past year increased significantly from 23% (95% CI, 19.1–26.5%) in 2009 to 64% (95% CI, 58.5–68.7%) in 2023. Figure 15 shows the IOL power calculation formulas used in eyes post LVC (multiple choices allowed). The Haigis-L (59% [95% CI, 51.2–66.4%]) and Barrett True K (73% [95% CI, 67.1–78.9%]) formulas were the most frequently used in 2013 and 2023, respectively. The Barrett True K formula gained more popularity than any other formula, including the calculations on the ASCRS website.
Refractive errors after cataract surgery
As Figure 16a shows, in each year from 2015 to 2022, approximately 20% of surgeons encountered refractive errors requiring additional correction other than spectacles (monofocal or multifocal IOLs). Figure 16b shows the additional corrective procedures performed. IOL exchange was consistently the most commonly procedure employed, increasing from 45% (95% CI, 34.4–55.2%) in 2015 to 59% (95% CI, 46.7–71.3%) in 2022. In contrast, the rate of LVC (touch-up), which is more frequently utilized in the U.S. [11], decreased from 35% (95% CI, 24.5–44.5%) to 18% (95% CI, 8.4–27.6%). The rates of contact lens and the piggyback IOLs were <10%, and did not increase.
PCR
The rates of PCR during the past years are shown in Figure 17. From 2004 to 2023, the percentage of surgeons having a rate of 0% and 0–0.5% of PCR increased from 15% (95% CI, 11.8–19.0%) to 27% (95% CI, 22.0–31.4%) and from 27% (95% CI, 22.9–31.7%) to 43% (95% CI, 37.3–47.7%), respectively. In contrast, the proportion of surgeons presenting a rate >0.5% of PCR exhibited a decreasing trend.
Refractive surgery
As shown in Figure 18, the percentage of members who performed refractive surgery or corneal refractive therapy (CRT; orthokeratology) has remained similar over the past decade. Figure 19 shows the types of refractive surgery performed from 2013 to 2023 (multiple choice allowed). Over the past decade, the number of microkeratome-assisted laser in situ keratomileusis (LASIK) and fetosecond laser-assisted LASIK procedures decreased significantly from 58% (95% CI, 47.1–67.9%) to 10% (95% CI, 4.0–15.6%) and from 48% (95% CI, 37.8–58.8%) to 27% (95% CI, 17.9–35.1%), respectively. The rates of photorefractive keratectomy, laser epithelial keratomileusis, astigmatic keratotomy/limbal relaxing incision, refractive lens exchange, and intrastromal corneal ring decreased, while that of small incision lenticule extraction (SMILE) remained unchanged. Only the rates of phakic IOL and CRT increased from 46% (95% CI, 35.5–56.5%) to 65% (95% CI, 55.4–74.0%) and from 29% (95% CI, 19.2–38.2%) to 63% (95% CI, 53.3–72.1%), respectively.
Types of refractive surgery (refractive surgeons only, multiple choices allowed, 2013–2023). AK astigmatic keratotomy, CRT corneal refractive therapy (orthokeratology), ICR intrastromal corneal ring, IOL intraocular lens, LASEK laser epithelial keratomileusis, LASIK laser in situ keratomileusis, LRI limbal relaxing incision, PRK photorefractive keratectomy, RLE refractive lens exchange, SMILE small incision lenticule extraction
Figure 20 shows the views of respondents on some of these procedures. The interest in surface ablation, LASIK, refractive lens exchange, and intrastromal corneal ring has decreased over the past decade. Since 2016, phakic IOLs have generated the most interest among surgeons, and the interest in CRT has increased significantly from 23% (95% CI, 19.2–26.4%) in 2013 and to 44% (95% CI, 38.9–48.7%) in 2023.
Usefulness of refractive surgery for the future practice of respondents (multiple choices allowed, 2013–2023). CRT corneal refractive therapy (orthokeratology), ICR intrastromal corneal ring, IOL intraocular lens, LASIK laser in situ keratomileusis, RLE refractive lens exchange, SMILE small incision lenticule extraction
Discussion
The 20-year findings of the JSCRS Clinical Survey reveal several key trends in the practice of cataract and refractive surgery. The sample size of the JSCRS survey, including since 2020, is stable with limited annual variations. The increasing age of annual respondents suggests that the same population of surgeons continues to respond to the questionnaire each year. Thus, we are confident that we have accurately captured the long-term changes in this field.
The JSCRS survey shows that the average monthly volume of cataract surgery remained stable. However, a decline was observed in 2021; in 2023, this number has not returned to the previous levels. With the emergence of the pandemic, the volume of cataract surgery also declined significantly in other countries [12]. Nevertheless, the 2022 ESCRS clinical survey indicates that this volume has almost recovered to pre-pandemic levels [13].
PI is a water-soluble polymer that can form a complex with iodine [14]. It possesses antiseptic qualities against multidrug-resistant bacteria and fungi, and is not associated with the development of resistance. It is also inexpensive and, therefore, commonly used by ophthalmologists [15]. It is reported that preoperative topical antibiotics might not be necessary in cases in which intraoperative iodine is applied [16]. Repeated application of diluted PI on the ocular surface is recommended during intraocular surgery, except in cases of iodine allergy where chlorhexidine should be used instead [15, 16]. In JSCRS, regarding preoperative antiseptic measures, there appears to be a marked polarization between the use of Pl and PAI. In particular, PAI is approved for use on ocular surfaces and can be costed. It is expected that the intraoperative application of PAI or PI will become more widespread for the prevention of endophthalmitis and reduction of bacterial resistance.
The practice patterns of the JSCRS members tend to differ significantly from those of ASCRS and ESCRS members in several aspects. Practice guidelines on the appropriate use of antibiotics for the prevention of postoperative infections were published in 2020. These guidelines recommend using preoperative ophthalmic fluoroquinolone drops thrice daily starting 3 days prior to surgery [17]. In conventional cataract surgery without risk factors, prophylactic oral administration is not recommended; instead, only use of topical drops is recommended. At present, there is no consensus on the duration of postoperative eye drop use, and there are no relevant recommendations. Regarding the prescription patterns for topical antibiotics, the 2021 ASCRS survey indicates that the duration of both preoperative and postoperative eye drops is markedly shorter than that previously recorded [8]. Although in JSCRS the duration has been gradually shortened, it remains considerably longer than reported by the ASCRS. In 2023, 48% of surgeons prescribed oral antibiotics. In addition, in the JSCRS the IC administration of anesthetics and antibiotics has been increasing; however, it is considerably lower than the rates recorded by the ESCRS and ASCRS [13]. These findings may be attributed to the conservative thought process which characterizes Japanese surgeons.
Thus far, there are no reports showing obvious evidence for the prevention of endophthalmitis by subconjunctival injections of antibiotics and antibiotic infusions through the irrigation bottle. In 2021, the proportion of surgeons performing each procedure in the ASCRS was ≤5% [8], and was gradually decreasing in Japan. Intracameral antibiotic injections at the conclusion of surgery is almost routinely performed in Europe [18,19,20]. The rate was also increasing in the ASCRS at 58% (2021), 36% (2014), and 14% (2007) [8]. In Japan, this rate also exhibits an increasing trend; however, the trend has almost stabilized at approximately 30% in recent years. The study reveals significant differences in the implementation of this practice in Japan, depending on the type of workplace. It is thought that this difference is mainly attributed to the off-label use of antibiotics for intraocular administration. Hence, university and other hospitals with specific functions need to either use this approach in clinical research or obtain approval from an unapproved drugs review committee, which is a complicated process.
Use of vancomycin (glycopeptide) is currently not recommended because of its potential association with the development of postoperative hemorrhagic occlusive retinal vasculitis [8, 21]. In Europe, cefuroxime (cephem) is used almost routinely due to its availability [20]; in the JSCRS and ASCRS, approximately 80% of the agents used are fluoroquinolones, mostly moxifloxacin (MFLX); the use of these solutions in the ASCRS, is due to the difficulty in obtaining cefuroxime [8, 22]. A Japanese multicenter study shows that endophthalmitis occurred within 1 month postoperatively in eight of 15,958 cases (one in 1,955) without intracameral MFLX administration and in three of 18,794 cases (one in 6,265) with intracameral MFLX administration; importantly, intracameral MFLX (50-500 μg/mL) administration has led to a three-fold decrease in the risk of endophthalmitis [23]. An excessively high dose may cause toxicity as toxic anterior segment syndrome, while an excessively low dose may be ineffective in preventing infection [22]. Currently, it is recommended to inject 0.1 mL of a 0.5% solution of MFLX [22]. Unfortunately, the survey only assessed the type of drug used, and the actual concentration and dosage are unknown. The usefulness and safety of both cefuroxime and MFLX at appropriate concentrations have been established [24]. Nevertheless, cases in which patients experience adverse reactions despite standard doses of cefuroxime are reported [25, 26]. In such cases, the concentration and dosage should be carefully monitored.
When applying anethesia, there appears to be a marked polarization between the use of topical drops and tenon injection. A survey analyzing data from a database of 1.2 million cases over a 10-year period (2010-2020) in the United Kingdom found that topical anesthesia alone, combined topical and intracameral anesthesia, sub-tenon anesthesia, and retrobulbar anesthesia were used in 152,321 (12.7%), 522,849 (43.7%), 461,175 (38.6%), and 59,537 (5.0%) operations, respectively [27]. Currently, it is also assumed that the rate of intracameral anesthesia is increasing in the ASCRS and ESCRS. Regardless of the pros and cons of intracameral anesthesia, it is thought that many Japanese surgeons are reluctant to unnecessarily inject off-label drugs into the anterior chamber. In Japan, this polarization is likely to continue in the future; nonetheless, if dilute anesthetics specific for intracameral injections become commercially available, the situation may change considerably.
In surgical techniques, the increase in the rate of TSSI, the lower percentage of temporal incisions, and the lower percentage of surgeons using FLACS are also significant differences from the ESCRS and ASCRS. It is reported that temporal CCI does not increase the risk of infection when compared with STI [28]. Temporal CCI tends to be highly favored in Europe and the USA [1]. In contrast, this study found an increase in the rates of TSSI and a lower percentage of temporal incisions. TSSI, which combines the merits of CCI and STI, was reported in Japan in 2010 [10]. The number of surgeons who prefer CCI has also slightly increased, suggesting that some surgeons who originally preferred STI have shifted to TSSI.
Two meta-analyses report that both FLACS and conventional techniques were effective and safe, with no difference in terms of prognosis [29, 30]. The American Academy of Ophthalmology does not report any difference in clinical outcomes between FLACS and conventional surgical techniques, and states that FLACS was not a cost-effective option [31]. Japan has its own universal health insurance scheme; by which the costs of FLACS are not covered by this scheme. Therefore, it is unlikely that FLACS will become more widely used in Japan.
In 2023, the proportion of cases in which toric IOLs were used was 11%. This rate was somewhat lower than recorded by the ASCRS (20%; 2018) [32] and ESCRS (14%; 2022) [13], but steadily increasing. A recent long-term follow-up study in Japan indicates that the effects of toric IOLs on astigmatism and visual acuity were sustained for 8 years in eyes with with-the-rule and oblique astigmatism [33]. In eyes with preoperative against-the-rule astigmatism, astigmatism-correcting effects of toric IOLs decreased at 5 years and beyond postoperatively, indicating that overcorrection may be considered at the time of cataract surgery [33]. Although the usefulness of toric IOLs is obvious, it is important to note that extensive misalignment could occur in cases in which plate-haptic multifocal toric IOLs are used [34]. It is expected that more toric IOLs would be used in Europe and the USA following a reduction in cost [2, 3]. Importantly, value-added costs are thought to be a barrier to the introduction of toric IOLs in Japan.
The proportion of cases in which presbyopia-correcting IOLs are used slightly decreased from 5% (2020) to 4% (2021). This rate was lower than reported by the ASCRS (8%; 2019) [11] and ESCRS (11%; 2021) [13], and did not increase after 2021. This observation cannot be explained by the emergence of the pandemic because the percentage of toric IOLs use increased during the same period. In Japan, the Ministry of Health, Labour and Welfare-initiated “advanced medical care system” was created in July 2008, and the cost of presbyopia-correcting IOL surgery can be covered by private medical insurance. However, this system was modified in April 2020. The significant increase in patient co-payment for presbyopia-correcting IOL surgery is thought to be the main reason responsible for the slight decline observed in the rate of this operation. Additionally, as also shown by the ESCRS, trifocal IOLs are becoming very popular among presbyopia-correcting IOLs [13]. ESCRS data are currently not available; nonetheless, data obtained from the JSCRS support the increased use of continuous range of vision IOLs. This type of IOL has exhibited excellent performance in both far and near vision [35, 36], and is expected to attract even greater attention in the future. Currently, high-order aspheric monofocal IOLs are classified as enhanced monofocal (mono-extended depth of focus) IOLs [37]. However, it is expected that more advanced monofocal IOLs will be introduced. Consequently, it may become difficult to distinguish monofocal from multifocal IOLs in the near future. Most presbyopia-correcting IOLs are used under the special environment of selective treatment in Japan. It is difficult to predict whether preferences for these IOLs in Japan will be consistent with or slightly different from those in other countries in the near future.
The SRK/T formula has been the most commonly used IOL power calculation method regardless of the ocular axis length. It is followed by the Barrett Universal II formula, which has rapidly become popular. The results of the 2022 ESCRS survey show a similar polarization trend [3, 13]. The Barrett Universal II formula is considered extremely useful regardless of the axial length [38,39,40] and may be as accurate as intraoperative aberrometry in eyes without a history of refractive surgery [41]. The Hill-RBF (radial basis function) formula, Kane formula, and intraoperative aberrometry have also attracted attention as highly accurate calculation methods [42, 43].
Among the IOL power calculation methods used in post-LASIK patients, the Barrett True K formula (73%) has been rapidly gaining popularity, similar to the results from the ESCRS survey. The Barrett True K formula exhibits high accuracy in post-myopic LASIK [44] and post-SMILE patients [45]. Certain biometric instruments can optionally be equipped with the Barrett True K (and Barrett Universal II and Barrett Toric) formula. The popularity of the Barrett’s formula may be attributed to its accuracy and the option to equip some biometric instruments with this formula. It is reported that intraoperative aberrometry is as accurate as Barrett True K [46], and more useful than Barrett True K particularly for post-hyperopic LASIK [47] and in long-axis eyes (>26.0 mm) [48]. Intraoperative wavefront aberration analysis is extremely accurate; its cost-effectiveness in actual clinical practice is thought to be the key to its widespread use in Japan.
It is reported that IOL exchange is very useful for the treatment of refractive errors after cataract surgery [49]. Consequently, numerous members of the JSCRS prefer this technique. Notably, among IOL exchange, piggyback IOL, and LASIK; LASIK is reported to have the best outcomes in terms of efficacy and predictability [50]. According to the 2019 ASCRS survey, 55% of members performed LVC for additional correction of residual astigmatism in multifocal IOL cases [11]. This is distinctly different from the trend observed in Japan. In Japan, the number of facilities that can perform LASIK (i.e., those with excimer lasers) is extremely limited. Numerous young surgeons have never actually observed LVC, and it is assumed that the gap between Japan and Western countries will persist in this regard. Furthermore, the usefulness of the piggyback implantable collamer lens (ICL) is reported [51, 52]. Nevertheless, thus far, there are only a few reports available, and it is highly likely that awareness regarding the piggyback ICL remains limited.
PCR is the most common complication associated with cataract surgery. However, the JSCRS survey shows that the percentage of surgeons encountering PCR at rates≤0.5% has increased from 43% to 69% over the past 20 years. The data of >2.4 million cataract surgeries collected by the Swedish National Cataract Registry from 1992 to 2021 show that the rate of PCR has decreased from 2.8% to 0.6% [53]. A systematic review revealed that previous intravitreal injections are a risk factor for PCR, and the risk increased by 4% for each such injection [54]. The PCR rates tend to decrease; nonetheless, this situation may change slightly due to the recent increases in the use of intravitreal injections. In the United Kingdom, standby cataract surgery was performed after the lockdown for the coronavirus disease-2019 pandemic was lifted. Moreover, it is reported that the PCR rate was significantly higher after the lockdown was lifted compared to the period before the pandemic, regardless of the skill of the surgeon [55, 56]. It is speculated that this negative impact could concern any surgeon on an extended time off from work due to sickness, sabbatical, research, and parental leave [55]. In the JSCRS survey, the PCR rates since 2020 (post-coronavirus disease-2019) remain very low overall. Since lockdown was not implemented in Japan, it is thought that the pandemic did not exert an effect on the rates of PCR.
In refractive surgery, LASIK as well as phakic IOL implantation has received worldwide recognition as popular surgical approaches for the correction of refractive errors. A multicenter retrospective survey (approximately 78,000 eyes) of refractive surgery in Japan shows that the most common refractive surgery performed in 2013 was LASIK (90.9%), followed by corneal inlay (5.0%), posterior chamber phakic IOL implantation (1.3%), laser epithelial keratomileusis (1.0%), refractive lens exchange (0.9%), photorefractive keratectomy (0.3%), and SMILE (0.2%), and that both LASIK and phakic IOL implantation offered good outcomes for the correction of refractive errors without vision-threatening complications [57]. According to a prospective nationwide study (approximately 15,000 eyes) in Japan, the most common refractive surgery performed in 2015 was LASIK (81.7%), followed by posterior chamber phakic IOL implantation (8.8%), SMILE (5.9%), surface ablation (3.2%), and iris-supported phakic IOL implantation (0.3%), LASIK and phakic IOL implantation were good in all measures of the safety, efficacy, predictability, and stability for the correction of refractive errors [58]. Although LASIK is still the gold standard of choice for overall refractive surgery, phakic IOL implantation has become gradually prevalent, especially in high ametropic eyes [57, 58].
The results of the 2022 ESCRS Clinical Trends Survey shows that 47% and 54% of the delegates performed corneal refractive surgery and implantation of phakic IOLs [13, 59], respectively. In the JSCRS survey, approximately 25% of members performed refractive procedures. The JSCRS survey results included CRT; thus, it could be inferred that the proportion of surgeons performing refractive “surgery” in the JSCRS was markedly lower. In the ESCRS survey, the 7-year clinical data trends show that, after a substantial decrease from 2016 (n=130) to 2020 (n=87), the number of corneal refractive surgeries has been gradually increasing from 2020 to 2022 (n=113); the reasons for this observation are not identified [59]. In Japan, following the occurrence of an outbreak of infectious keratitis in a single center [60] and the provision of important information by the consumer agency of Japan in 2013, the number of refractive procedures performed has remained in decline [57, 58]. Although the JSCRS survey did not inquire the number of refractive surgeries, it might be considerably lower than that reported by ESCRS.
A systematic review comparing SMILE with LASIK shows that, although both generally produce similar outcomes, SMILE tended to undercorrect for astigmatism correction, while LASIK was linked to a higher risk of postoperative spherical aberration [61]. In the 2022 ESCRS survey, 84% of respondents reported that the majority of corneal refractive procedures performed were LASIK, while only 12% reported SMILE as the main corneal refractive procedure performed [13]. In the JSCRS survey, the responses regarding the type of refractive surgery were given as multiple choice; therefore, it was not possible to conduct a simple comparison. Nonetheless, a similar trend was detected, showing that LASIK was more commonly performed than SMILE.
CRT is not a surgical option; hence, only the rate of phakic IOLs is increasing as a surgical procedure in Japan. Thus, the performance of refractive surgery in Japan is currently influenced by both the conservative nature of Japanese surgeons and the true usefulness of phakic IOLs. The latest information on ICL includes a meta-analysis that did not find a difference in long-term results compared with small incision lenticule extraction; however, the use of ICL was associated with more rapid visual recovery [62], excellent long-term outcomes over 11 years after surgery in 3,105 eyes [63], and excellent short-term outcomes in eyes after LASIK [64]. Considering the current status of refractive surgery in Japan, it is expected that the use of LVC will remain at its current level, while that of phakic IOL will increase further.
The results of the present study may not accurately reflect the opinions of all ophthalmologists in Japan because the respondents in this survey were exclusively members of the JSCRS. The sampling population might have represented a group of ophthalmologists who are more active in the field of cataract and refractive surgery. Because of the anonymous nature of this investigation, it is not possible to identify the ophthalmologists who participated in the survey. However, the annual JSCRS survey series covers a similar group of surgeons; thus, we are confident that the data describe the trends and direction of practice for cataract and refractive surgery in Japan. A longer term, ongoing survey, similar to others [1,2,3,4,5,6,7,8,9, 11, 13, 32], would further define the directions in ophthalmology and improve the quality of medical services that patients will receive in the future.
References
Leaming DV. Practice styles and preferences of ASCRS members-2003 survey. J Cataract Refract Surg. 2004;30:892–900.
ASCRS clinical survey 2022. Eyeworld. https://supplements.eyeworld.org/i/1483249-ascrs-clinical-survey-2022. Accessed 20 Aug 2023.
Kohnen T, Findl O, Nuijts R, Ribeiro F, Cochener-Lamard B. ESCRS Clinical Trends Survey 2016–2021: 6-year assessment of practice patterns among society delegates. J Cataract Refract Surg. 2023;49:133–41.
Schmack I, Auffarth GU, Epstein D, Holzer MP. Refractive surgery trends and practice style changes in Germany over a 3-year period. J Refract Surg. 2010;26:202–8.
Pick ZS, Leaming DV, Elder MJ. The fourth New Zealand cataract and refractive surgery survey: 2007. Clin Exp Ophthalmol. 2008;36:604–19.
Ong-Tone L. Practice patterns of Canadian Ophthalmological Society members in cataract surgery: 2017 survey. Can J Ophthalmol. 2018;53:1.
Rho CR, Kim JH, Chung IK, Kim EC, Han YK, Han SY, et al. Cataract surgery practice in the Republic of Korea: a survey of the Korean Society of Cataract and Refractive Surgery 2020. Korean J Ophthalmol. 2021;35:272–9.
Chang DF, Rhee DJ. Antibiotic prophylaxis of postoperative endophthalmitis after cataract surgery: results of the 2021 ASCRS member survey. J Cataract Refract Surg. 2022;48:3–7.
Oshika T, Amano S, Araie M, Majima Y, Leaming DV. Current trends in cataract and refractive surgery in Japan: 1999 survey. Jpn J Ophthalmol. 2001;45:383–7.
Sugai S, Yoshitomi F, Oshika T. Transconjunctival single-plane sclerocorneal incisions versus clear corneal incisions in cataract surgery. J Cataract Refract Surg. 2010;36:1503–7.
ASCRS clinical survey 2019. Eyeworld. https://supplements.eyeworld.org/eyeworld-supplements/ascrs-clinical-survey-2019. Accessed 20 Aug 2023.
Sanjay S, Leo SW, Au Eong KG, Adriono GA, Fong KC, Anand K, et al. Global Ophthalmology Practice Patterns during COVID-19 Pandemic and Lockdown. Ophthalmic Epidemiol. 2022;29:233–44.
ESCRS Clinical Trend Survey 2022 Results. EuroTimes. https://www.escrs.org/media/5cbb4kx4/2022_escrs_clinical-survey-supplement.pdf. Accessed 10 Sept 2023.
Borgia A, Mazzuca D, Della Corte M, Gratteri N, Fossati G, Raimondi R, et al. Prophylaxis of Ocular Infection in the Setting of Intraocular Surgery: Implications for Clinical Practice and Risk Management. Ophthalmol Ther. 2023;12:721–34.
Grzybowski A, Shimada H, Nakashizuka H, Koerner J. Low-concentration povidone-iodine for the prevention of intraocular infections in ophthalmic surgery. Curr Opin Ophthalmol. 2022;33:28–34.
Matsuura K, Miyazaki D, Sasaki SI, Inoue Y, Sasaki Y, Shimizu Y. Effectiveness of intraoperative iodine in cataract surgery: cleanliness of the surgical field without preoperative topical antibiotics. Jpn J Ophthalmol. 2020;64:37–44.
Japanese Society of Chemotherapy, Japan Society for Surgical Infection. Japanese Clinical Practice Guidelines for antimicrobial prophylaxis in surgery (supplemental version). Japanese Journal of Chemotherapy. 2020;68:310–20.
Barry P, Seal DV, Gettinby G, Lees F, Peterson M, Revie CW, et al. ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery: Preliminary report of principal results from a European multicenter study. J Cataract Refract Surg. 2006;32:407–10.
Barry P. Adoption of intracameral antibiotic prophylaxis of endophthalmitis following cataract surgery: update on the ESCRS Endophthalmitis Study. J Cataract Refract Surg. 2014;40:138–42.
Chang DF. The ESCRS intracameral cefuroxime study: the debate continues. J Cataract Refract Surg. 2021;47:150–2.
Matović K, Mekjavić PJ, Groznik AL, Fakin A, Petrovič MG, Pfeifer V, et al. Vancomycin-Associated Hemorrhagic Occlusive Retinal Vasculitis: A Case Series and Systematic Review. Ophthalmic Surg Lasers Imaging Retina. 2022;53:702–12.
Myers WG, Chang DF, Shorstein NH, Mah FS, Mamalis N, Miller KM, et al. ASCRS clinical advisory on intracameral moxifloxacin injection for infection prophylaxis. J Cataract Refract Surg. 2023;49:1068–70.
Matsuura K, Miyoshi T, Suto C, Akura J, Inoue Y. Efficacy and safety of prophylactic intracameral moxifloxacin injection in Japan. J Cataract Refract Surg. 2013;39:1702–6.
Rana K, Bahrami B, van Zyl L, Esterman A, Goggin M. Efficacy of intracameral antibiotics following manual small incision cataract surgery in reducing the rates of endophthalmitis: A meta-analysis. Clin Exp Ophthalmol. 2021;49:25–37.
Davila JR, Mishra K, Leung LS. Macular Edema and Serous Macular Detachment after a Standard Dose of Intracameral Cefuroxime. Ophthalmic Surg Lasers Imaging Retina. 2021;52:615–8.
Spackman W, Raman V. Acute exudative serous macular detachment with intraretinal oedema following uncomplicated phacoemulsification cataract surgery. BMJ Case Rep. 2022;15: e247772.
Neo YN, Gruszka-Goh MH, Braga AJ, de Klerk TA, Lindfield D, Nestel A, et al. Royal College of Ophthalmologists’ National Ophthalmology Database study of cataract surgery: report 11, techniques and complications of local anesthesia for cataract surgery in the United Kingdom. J Cataract Refract Surg. 2023;49:1216–22.
Lundström M, Wejde G, Stenevi U, Thorburn W, Montan P. Endophthalmitis after cataract surgery: a nationwide prospective study evaluating incidence in relation to incision type and location. Ophthalmology. 2007;114:866–70.
Kolb CM, Shajari M, Mathys L, Herrmann E, Petermann K, Mayer WJ, et al. Comparison of femtosecond laser-assisted cataract surgery and conventional cataract surgery: a meta-analysis and systematic review. J Cataract Refract Surg. 2020;46:1075–85.
Wang H, Chen X, Xu J, Yao K. Comparison of femtosecond laser-assisted cataract surgery and conventional phacoemulsification on corneal impact: A meta-analysis and systematic review. PLoS ONE. 2023;18: e0284181.
Lin CC, Rose-Nussbaumer JR, Mohtaseb ZN, Pantanelli SM, Steigleman WA, Hatch KM, et al. Femtosecond Laser Assisted Cataract Surgery: A Report by the American Academy of Ophthalmology. Ophthalmology. 2022;129:946–54.
ASCRS clinical survey 2018. Eyeworld. https://supplements.eyeworld.org/eyeworld-supplements/december-2018-clinical-survey. Accessed 1 Mar 2024.
Oshika T, Nakano S, Fujita Y, Nomura Y, Inoue Y, Takehara H, et al. Long-term outcomes of cataract surgery with toric intraocular lens implantation by the type of preoperative astigmatism. Sci Rep. 2022;19:8457.
Oshika T, Nakano S, Inamura M, Ikai N, Kato Y, Izumi I, et al., et al. Extensive misalignment of plate-haptic rotationally asymmetric multifocal toric intraocular lens. Jpn J Ophthalmol. 2023;67:560–4.
Benyoussef AA, Reboux N, Cochener B. Comparison of Bilateral Reading Performance Among Two Presbyopia-Correcting Intraocular Lenses. J Refract Surg. 2022;38:428–34.
Baur ID, Auffarth GU, Łabuz G, Stengele A, Hallak MK, Khoramnia R. Clinical Evaluation of Reading Performance in Refractive Lens Exchange With a Diffractive Continuous-Range-of-Vision Intraocular Lens. Am J Ophthalmol. 2023;18(250):25–37.
Wan KH, Au ACK, Kua WN, Ng ALK, Cheng GPM, Lam NM, et al. Enhanced Monofocal Versus Conventional Monofocal Intraocular Lens in Cataract Surgery: A Meta-analysis. J Refract Surg. 2022;38:538–46.
Shrivastava AK, Behera P, Kumar B, Nanda S. Precision of intraocular lens power prediction in eyes shorter than 22 mm: An analysis of 6 formulas. J Cataract Refract Surg. 2018;44:1317–20.
Rong X, He W, Zhu Q, Qian D, Lu Y, Zhu X. Intraocular lens power calculation in eyes with extreme myopia: Comparison of Barrett Universal II, Haigis, and Olsen formulas. J Cataract Refract Surg. 2019;45:732–7.
Lin P, Xu J, Miao A, Xu C, Qian D, Lu Y, Zheng T. A Comparative Study on the Accuracy of IOL Calculation Formulas in Nanophthalmos and Relative Anterior Microphthalmos. Am J Ophthalmol. 2023;245:61–9.
Greenwood MD, Hutchison JW, Gorham RA, Kramer BA. The Use of Intraoperative Aberrometry in Normal Eyes: An Analysis of Intraocular Lens Selection in Scenarios of Disagreement. J Refract Surg. 2022;38:304–9.
Stopyra W, Cooke DL, Grzybowski A. A Review of Intraocular Lens Power Calculation Formulas Based on Artificial Intelligence. J Clin Med. 2024;16:498.
Kaufman AR, Pineda R 2nd. Intraoperative aberrometry: an update on applications and outcomes. Curr Opin Ophthalmol. 2023;34:48–57.
Wei L, Meng J, Qi J, Lu Y, Zhu X. Comparisons of intraocular lens power calculation methods for eyes with previous myopic laser refractive surgery: Bayesian network meta-analysis. J Cataract Refract Surg. 2021;47:1011–8.
Meziane Elotmani A, Messerschmidt-Roth A, Nehme A, Müller HH, Sekundo W. Comparison of intraocular lens power calculation formulas with and without total keratometry and ray tracing in patients with previous myopic SMILE. J Cataract Refract Surg. 2023;49:467–73.
Gasparian SA, Nassiri S, You H, Vercio A, Hwang FS. Intraoperative aberrometry compared to preoperative Barrett True-K formula for intraocular lens power selection in eyes with prior refractive surgery. Sci Rep. 2022;12:7357.
Gouvea L, Sioufi K, Brown CE, Waring Iv G, Chamon W, Rocha KM. Refractive Accuracy of Barrett True-K vs Intraoperative Aberrometry for IOL Power Calculation in Post-Corneal Refractive Surgery Eyes. Clin Ophthalmol. 2021;15:4305–15.
Soifer M, Passi SF, Wisely CE, Raufi NN, Thompson AC, Kim T, et al. Refractive Outcomes Using Intraoperative Aberrometry for Highly Myopic, Highly Hyperopic, and Post-refractive Eyes. J Refract Surg. 2021;37:609–15.
Dragnea DC, Truţa RN, Goemaere J, Tassignon MJ, Dhubhghaill SN. Intraocular bag-in-the-lens exchange: indications, outcomes, and complications. J Cataract Refract Surg. 2022;48:568–75.
Fernández-Buenaga R, Alió JL, Pérez Ardoy AL, Quesada AL, Pinilla-Cortés L, Barraquer RI. Resolving refractive error after cataract surgery: IOL exchange, piggyback lens, or LASIK. J Refract Surg. 2013;29:676–83.
Kojima T, Horai R, Hara S, Nakamura H, Nakamura T, Satoh Y, et al. Correction of residual refractive error in pseudophakic eyes with the use of a secondary piggyback toricImplantable Collamer Lens. J Refract Surg. 2010;26:766–9.
Eissa SA, Khafagy MM, Sidky MK. Implantable Collamer Lens in the Management of Pseudophakic Ametropia. J Refract Surg. 2017;33:532–7.
Bro T, Behndig A, Viberg A, Zetterberg M, Kugelberg M, Nilsson I, et al. Two point four million cataract surgeries: 30 years with the Swedish National Cataract Register, 1992–2021. J Cataract Refract Surg. 2023;49:879–84.
Bjerager J, van Dijk EHC, Holm LM, Singh A, Subhi Y. Previous intravitreal injection as a risk factor of posterior capsule rupture in cataract surgery: a systematic review and meta-analysis. Acta Ophthalmol. 2022;2022:614–23.
Matarazzo F, Phylactou M, Day AC, Maurino V. Effect of surgical abstinence on the risk for posterior capsule rupture during cataract surgery. J Cataract Refract Surg. 2022;48:173–6.
Theodoraki K, Naderi K, Lam CFJ, Tan JK, Jameel A, Lai L, et al. Impact of cessation of regular cataract surgery during the COVID pandemic on the rates of posterior capsular rupture and post-operative cystoid macular oedema. Eye (Lond). 2023;37:440–5.
Kamiya K, Igarashi A, Hayashi K, Negishi K, Sato M, Bissen-Miyajima H, et al. A Multicenter Retrospective Survey of Refractive Surgery in 78,248 Eyes. J Refract Surg. 2017;33:598–602.
Kamiya K, Igarashi A, Hayashi K, Negishi K, Sato M, Bissen-Miyajima H, et al. A Multicenter Prospective Cohort Study on Refractive Surgery in 15,011 Eyes. Am J Ophthalmol. 2017;175:159–68.
The Future of Refractive Surgery – Lenticlue Extraction, Phakic IOLs and Beyond. EuroTimes. https://www.escrs.org/media/dmihn22q/feb24_supplement_refractsurg.pdf. Accessed 1 Mar 2024.
Yamaguchi T, Bissen-Miyajima H, Hori-Komai Y, Matsumoto Y, Ebihara N, Takahashi H, et al. Infectious keratitis outbreak after laser in situ keratomileusis at a single laser center in Japan. J Cataract Refract Surg. 2011;37:894–900.
Song J, Cao H, Chen X, Zhao X, Zhang J, Wu G, et al. Small Incision Lenticule Extraction (SMILE) Versus Laser Assisted Stromal In Situ Keratomileusis (LASIK) for Astigmatism Corrections: A Systematic Review and Meta-analysis. Am J Ophthalmol. 2023;247:181–99.
Chen D, Zhao X, Chou Y, Luo Y. Comparison of Visual Outcomes and Optical Quality of Femtosecond Laser-Assisted SMILE and Visian Implantable Collamer Lens (ICL V4c) Implantation for Moderate to High Myopia: A Meta-analysis. J Refract Surg. 2022;38:332–8.
Packer KT, Vlasov A, Greenburg DL, Coggin A, Weightman JW, Beltran T, et al. U.S. military implantable collamer lens surgical outcomes: 11-year retrospective review. J Cataract Refract Surg. 2022;48:649–56.
Kamiya K, Shimizu K, Igarashi A, Kitazawa Y, Kojima T, Nakamura T, et al. Posterior chamber phakic intraocular lens implantation after laser in situ keratomileusis. Eye Vis (Lond). 2022;9:15.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflicts of interest
M. Sato, None; K. Kamiya, None; K. Hayashi, None; H. Tabuchi, None; T. Kojima, None; N. Goto, None; N. Hatsusaka, None; H. Torii, None; M. Nagata, None; K. Miyata, None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Corresponding Author: Masaki Sato
About this article
Cite this article
Sato, M., Kamiya, K., Hayashi, K. et al. Changes in cataract and refractive surgery practice patterns among JSCRS members over the past 20 years. Jpn J Ophthalmol (2024). https://doi.org/10.1007/s10384-024-01081-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10384-024-01081-3