Abstract
Proton beam (PB) therapy is gaining popularity for breast cancer treatment because of its enhanced coverage and potential to minimize late toxicities. The dose and volume of PB irradiation are closely associated with improved breast cancer survival. We aimed to investigate the impact of PB irradiation on the survival of the human breast cancer cells MCF-7 and their resistance to doxorubicin (MCF-7-DR) and paclitaxel (MCF-7-PR). Cells exposed to 0.5, 2, 4, or 8 Gy of PB irradiation showed a significant decrease in the survival of parent cells, even at 2 Gy, indicating therapeutic efficacy. Conversely, drug-resistant cells exhibited notable cytotoxicity at 4 and 8 Gy, which were above the daily recommended dose. Mechanistically, PB irradiation significantly altered the DNA repair proteins RAD51, Ku80, and survivin and cleaved PARP in MCF-7 cells compared to chemo-resistant cells, except for RAD51 and Ku80. In addition, cell-cycle regulators and MAPK expression were notably altered by PB irradiation compared to MCF-7-DR and PR cells, underscoring the importance of tailoring PB irradiation for enhanced efficacy against chemo-resistant breast cancer. These findings suggest that PB irradiation downregulated RAD51 and Ku80, the potent DNA repair markers, underscoring its potential therapeutic efficacy in treating chemo-resistant breast cancer cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
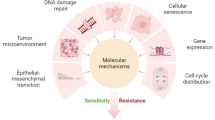
Breast cancer is the most prevalent cancer among women worldwide [1]. Chemotherapy is the conventional treatment for breast cancer; however, chemoresistance often leads to treatment failure in more than 90% of patients with metastatic cancer [2]. The molecular mechanisms underlying chemoresistance in breast cancer include increased drug efflux, activation of DNA damage repair, changes in the cell cycle, and inhibition of cell death [3].
Radiotherapy is employed for all stages of breast cancer. According to the National Comprehensive Cancer Network guidelines, the recommended total doses for external beam radiation therapy involve fractionation of 1.8–2 Gy daily. The dose and volume of irradiation were associated with improved breast cancer survival [4]. Proton beam (PB) therapy is a unique type of radiation treatment that can precisely target tumors and deliver high-radiation doses to kill cancerous cells [5]. This therapy is particularly promising for patients with breast cancer because it minimizes damage to adjacent tissues and critical organs such as the heart and lungs [6]. PB therapy for breast cancer is rapidly improving in terms of treatment delivery and optimization of dose and fractionation schedules [7].
Mechanistically, when cancer cells are exposed to radiation, the cellular DNA is damaged. P53 expression is an important response to radiation and is associated with radiosensitivity [8, 9]. P53 accumulation leads to cell-cycle arrest and facilitates cell survival by enhancing the expression of DNA repair enzymes; it can also trigger apoptosis [10]. However, cell death is determined by radiosensitivity, which depends on the type of cancer cells [11]. Radiosensitivity is an important measure of the efficacy of radiation therapy.
Previously, we showed that PB irradiation-mediated changes in RAD51 and survivin expression are crucial for determining the radiosensitivity of pancreatic cancer cells [12]. PB irradiation-induced apoptosis is caused by direct or indirect DNA damage in various cancer cells [5, 13]. These findings suggest that PB irradiation is a useful therapeutic tool for determining sensitivity and inhibiting the survival of breast cancer cells. We investigated the effects of PB irradiation on the survival of hormone receptor-positive breast cancer cells (MCF-7) and its chemo-resistant subgroups (MCF-7-DR and MCF-7-PR).
2 Materials and methods
2.1 Cell culture
MCF-7cells were obtained from the Korean Cell Line Bank (Seoul, Korea) and grown in Dulbecco’s Modified Eagle Medium (DMEM) supplemented with 1% antimycotic/antibiotic solution (100 units/mL of penicillin, 100 µg/mL of streptomycin, and 0.25 µg/mL of amphotericin B) and 10% heat-inactivated FBS in a 5% CO2 atmosphere at 37˚C. Dox-resistant (MCF-7-DR) and paclitaxel-resistant (MCF-7-PR) breast cancer cells were established as previously described [14].
2.2 PB irradiation
PB irradiation was performed using a 100 MeV proton accelerator in Korea Multi‑Purpose Accelerator Complex at Korean Atomic Energy Research Institute (Gyeongju, Korea). The cells were irradiated with PB at doses of 0.5, 2, 4, or 8 Gy with a spread-out Bragg peak width of 6 cm.
2.3 Cell viabilities
A 3-(4,5-dimethylthiazol-2-yl)-2,5 diphenyl-tetrazolium bromide (MTT) assay was conducted to determine the viability of MCF-7-DR and MCF-7-PR breast cancer cells treated with the indicated doses of PB irradiation (0.5, 2, 4, and 8 Gy), grown for 48 h, and then incubated with MTT for 3 h in the dark. The insoluble formazan produced was dissolved in dimethyl sulfoxide and the absorbance of formazan was measured at 570 nm.
2.4 Clonogenic cell survival assay
MCF-7-DR and MCF-7-PR breast cancer cells were seeded in a 6-well plate at 400 cells/well and attached for 24 h. Then, the cells were irradiated with PB (2, 4, or 8 Gy), and the media were replaced with fresh media every 2–3 days. After 1 week of treatment, the cells were fixed with 10% formalin for 20 min, stained with 1% crystal violet for 40 min, and photographed using a Luminescent Image Analyzer LAS-4000 (Fujifilm Corporation, Tokyo, Japan).
2.5 Western blotting
The cells were seeded, allowed to attach for 24 h, and irradiated with PB (0.5, 2, 4, or 8 Gy). The cells were then incubated for 48 h in DMEM. Cells were then lysed with radioimmunoprecipitation assay lysis buffer (Biosesang, Seongnam, Korea) supplemented with protease inhibitor cocktail and phosphatase inhibitor cocktail (GenDEPOT, LLC, Barker, TX, USA) and centrifuged at 13,000 rpm for 10 min at 4 °C. Whole cell lysates were used to determine protein concentrations using bicinchoninic acid assay. Same amounts of proteins were subjected to sodium dodecyl sulfate–polyacrylamide gel electrophoresis on 6–15% gels and then transferred to polyvinylidene fluoride membranes (Pall Life Science, Port Washington, NY, USA), which were blocked with 1% bovine serum albumin (BSA) or 5% non-fat dry milk (Santa Cruz Biotechnology, Inc.) in Tris-buffered saline-Tween (TBS-T) (50 mM Tris–HCl, 150 mM NaCl, and 0.1% Tween-20) and probed with primary antibodies diluted at 1:3000 in 1% BSA or 5% non-fat dry milk in TBS-T overnight at 4 °C. The membranes were then washed thrice with TBS-T and treated with a secondary antibody diluted 1:5000 in TBS-T for 1 h at RT. Target protein bands were developed using a chemiluminescent substrate and photographed using the Luminescence Image Analyzer LAS-4000 (Fujifilm Corporation, Tokyo, Japan). Target protein band densities were measured using ImageJ (National Institutes of Health, Bethesda, Maryland, USA).
2.6 Statistical analysis
Analyses were conducted using SPSS Ver. 20.0 (SPSS Inc., Chicago, IL, USA). One-way analysis of variance and Tukey’s post hoc test were used to determine the significance of intergroup differences. Experiments were performed independently thrice, and results are expressed as means ± standard deviations (SDs). Statistical significance was set at p < 0.05.
3 Results and discussions
3.1 Inhibition of cell proliferation following PB irradiation
We investigated the effects of PB irradiation on the proliferation and survival of MCF-7and chemo-resistant breast cancer cells (MCF-7-DR and MCF-7-PR). Cell proliferation was notably suppressed in MCF-7 and MCF-7-DR cells, but only slightly decreased in MCF-7-PR cells at 4 and 8 Gy after 48 h (Fig. 1A). Furthermore, the colony formation assay revealed a significant reduction in MCF-7colonies following PB irradiation (Fig. 1B). Interestingly, MCF-7-DR and MCF-7-PR colonies exhibited a substantial decrease after 4 and 8 Gy PB irradiation (Fig. 1B). These findings align with existing research demonstrating the inhibitory effects of PB irradiation on cell growth in hepatocellular carcinoma, pancreatic cancer, and 4T1 murine breast cancer cells [5, 15,16,17].
The effect of proton-beam (PB) irradiation on cell viability and survival. MCF-7, MCF-7-DR, and MCF-7-PR breast cancer cells were exposed to PB (0–8 Gy) and further incubated for 48 h. A Cell viability was compared with 0 Gy-irradiated sample. B Quantitative analysis of colonies formation after treatment. *, **Indicate p < 0.01, p < 0.001 (control vs treatment)
3.2 Regulation of DNA repair mechanism by PB irradiation
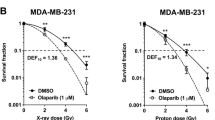
PBs possess unique physical properties that yield a distinctive dose deposition profile, characterized notably by the Bragg peak, occurring at the proton trajectory’s termination where ions come to a halt [17]. Compared to photons, PBs exhibit a slightly higher linear energy transfer (LET), which impacts the complexity of DNA damage and the repair capacity of treated cells. High-LET radiation induced cell death via generating complex DNA damage [18]. DNA double-strand breaks initiated by PB irradiation at the Bragg peak engage the homologous recombination machinery, contributing to the repair process [19]. RAD51, a homologous recombination repair enzyme, serves an important role in the repair of radiation‑induced DNA damage and has been implicated as a radiosensitivity determinant [20]. Moreover, RAD51 and survivin were potent markers for determining the therapeutic efficacy of PB therapy in patients with pancreatic cancer [12]. In addition, the correlation between Ku80 expression and radiation resistance in the head and neck cancer cells were elucidated [21, 22]. In the present study, we observed decreased of the DNA repair proteins RAD51, Ku80, and survivin in MCF-7. Surprisingly, in MCF-7-DR cells, these proteins remained unchanged, except for RAD51 and Ku80, which decreased at 8 Gy only, possibly because of exposure to a high dose of PB (Fig. 2). In MCF-7-PR cells, all these proteins were unaltered by PB irradiation, as shown in Fig. 2. In addition, we observed an increase in the expression of p-H2AX, a DNA damage marker, in MCF-7, whereas no discernible effect was noted in MCF-7-DR and MCF-7-PR cells at 48 h (Fig. 2). Taken together, these results suggest that PB irradiation inhibits the DNA repair system in parent cells, whereas it remains unchanged in chemo-resistant breast cancer cells at 48 h, except at 8 Gy. This indicates that the DNA repair mechanism may be crucial markers in PB therapy for inhibiting the survival of chemo-resistant cells.
Effect of PB on DNA damage response. Phosphorylated of H2A histone family member X (H2A.X), RAD51, survivin, and Ku80 expressions were measured after PB irradiation in MCF-7, MCF-7-DR and MCF-7-PR. Protein expression was quantitatively evaluated. *, **Indicate p < 0.01, p < 0.001 (control vs treatment)
3.3 PB irradiation did not induce cell death by autophagy and necroptosis
Recently, LC3-mediated autophagy was found to be a potential target for overcoming doxorubicin resistance [23]. The phosphorylation of RIPK3 leads to necroptosis [24]. However, in the present study, we observed no effect of PB irradiation on LC3-II, an autophagy marker, or RIPK3, a necroptosis marker, in MCF-7, MCF-7-DR, and MCF-7-PR breast cancer cells (Fig. 3), suggesting that PB irradiation induces cell death independent of autophagy and necroptosis.
Effect of PB on autophagy or necroptosis. Protein levels of the autophagy-related protein LC3-II and necroptosis-related protein RIPK3 were analyzed using western blotting in MCF-7, MCF-7-DR, and MCF-7-PR cells. Protein bands were quantified using β-actin as the internal control. Results are presented as the means ± SDs (n = 3). Significant intergroup differences are indicated as * or **, which indicate p < 0.01 and p < 0.001, respectively
3.4 Induction of apoptotic marker in parent cells whereas ineffective on resistant cells
We determined the PB irradiation-mediated changes in apoptosis-associated proteins, such as cleaved PARP and Bcl-2 family proteins, in different breast cancer cell lines [25, 26]. As shown in Fig. 4, the expression of cleaved PARP and Bcl-xL was only slightly increased, whereas that of BAX remained unaltered. Surprisingly, the protein levels of cleaved PARP, Bcl-xL, and BAX showed no significant changes in chemo-resistant MCF-7-DR and MCF-7-PR cells (Fig. 4). These data suggest that PB irradiation induces apoptosis-mediated cell death in the parent cell, MCF-7. However, the protein levels observed in the chemo-resistant cells remained unaffected by PB irradiation.
Effect of PB on PARP cleavage and expression of Bcl-xL and Bax. PARP cleavage and the expression of Bcl-xL and Bax were analyzed. Relative intensities were measured using β-actin as the internal control. The data are presented as the means ± SDs (n = 3). Significant intergroups differences are indicated as * or **, which indicate p < 0.01 and p < 0.001, respectively
3.5 Modification of cell-cycle regulators upon PB irradiation
Radiation responses primarily involve DNA damage and alterations in cell-cycle regulators [16]. p21 plays an essential role in cell-cycle arrest in response to DNA damage [27]. The cell cycle is regulated by numerous cyclins and cyclin-dependent kinases (CDKs). The activation of cyclins/CDKs is induced by mitogenic signals and inhibited by the activation of cell-cycle checkpoints in response to DNA damage [28]. PB irradiation-induced p21 expression in MCF-7 cells, whereas p21 levels disappeared in MCF-7-DR and MCF-7-PR cells (Fig. 5). The expressions of cyclins D1, B1, and E1 were altered by PB irradiation but remained unaltered in MCF-7-DR and MCF-7-PR, except for cyclin E1 in MCF-7-DR and cyclin B1 in MCF-7-PR. Therefore, PB irradiation inhibits cell-cycle progression in response to DNA damage in parent cells, as evidenced by increased p21 expression and altered cyclin levels. However, this inhibitory effect was not observed in the chemo-resistant cells after 48 h of PB irradiation.
Effect of PB on cell-cycle regulators. Western blotting was used to determine the protein expressions of p21, cyclin D1, cyclin E1, and cyclin B1. β-actin was used as the internal control. Results are presented as the means ± SDs (n = 3). Significant intergroups differences are indicated as * or ** which indicate p < 0.01 and p < 0.001, respectively
3.6 Modulation of MAPKs in response to PB irradiation
MAPKs are key regulators of various cellular pathways that control cell proliferation, survival, cell cycle, and cell death. Depending on the cell type and stimulus, ERK activity mediates different anti-proliferative events, such as apoptosis, autophagy, and senescence in vitro and in vivo [29]. The activation of p38 and JNK may play decisive roles in controlling cell death [30]. Our results revealed the phosphorylation of ERK, p38, and JNK, with a decrease in total JNK when PB was exposed to MCF-7. In contrast, MAPKs expression remained unchanged, except for that of p-ERK, after PB exposure in chemo-resistant MCF-7-DR and MCF-7-PR breast cancer cells (Fig. 6). When DNA is damaged, cell-cycle progression is impeded by the induction of ERK and p38 phosphorylation [31]. Therefore, PB irradiation may induce cell death by modulating the MAPK pathway; however, this effect was not observed in chemo-resistant cells.
Effect of PB on phosphorylation and expression on MAPK family proteins. Representative western blots and quantification data showing p-p38, t-p38, p-ERK, t-ERK, p-JNK, and t-JNK expressions in MCF-7, MCF-7-DR and MCF-7-PR cells exposed to PB. β-actin was used as internal control. Data are presented as the means ± SDs, n = 3. Significant differences between groups are indicated as * or ** indicate p < 0.01 and p < 0.001, respectively
4 Conclusions
The results indicate that the survival of human breast cancer cells may be affected by exposure to PB irradiation. Notably, no discernible effects were observed on DDRs, cell-cycle regulators, or MAPKs in chemo-resistant breast cancer cells, except for RAD51 and Ku80. In a previous study, we highlighted the involvement of RAD51 and survivin in radiosensitivity. The current study further demonstrated that radiosensitivity in chemo-resistant cells may be determined by the regulation of RAD51 and Ku80. Consequently, this study emphasized that a reduction in RAD51 and Ku80 expression is crucial for determining radiosensitivity. This implies that a specialized strategy is required to enhance the efficacy of PB therapy, particularly in patients showing chemoresistance.
References
C.S. Mayo, M.M. Urie, T.J. Fitzgerald, Hybrid IMRT plans—concurrently treating conventional and IMRT beams for improved breast irradiation and reduced planning time. Int. J. Radiat. Oncol. Biol. Phys. 61(3), 922–932 (2005)
C. Christowitz et al., Mechanisms of doxorubicin-induced drug resistance and drug resistant tumour growth in a murine breast tumour model. BMC Cancer 19(1), 1–10 (2019)
G. Housman et al., Drug resistance in cancer: an overview. Cancers 6(3), 1769–1792 (2014)
R.W. Mutter et al., Proton therapy for breast cancer: a consensus statement from the Particle Therapy Cooperative Group Breast Cancer Subcommittee. Int. J. Radiat. Oncol. Biol. Phys. 111(2), 337–359 (2021)
Y.-S. Kwon et al., Suppressive effects of a proton beam on tumor growth and lung metastasis through the inhibition of metastatic gene expression in 4T1 orthotopic breast cancer model. Int. J. Oncol. 49(1), 336–342 (2016)
Y.K. Lim et al., A proton beam irradiation method for a uniform dose distribution over a sample volume. J. Korean Phys. Soc. 48(9), 777 (2006)
K.S. Corbin, R.W. Mutter, Proton therapy for breast cancer: progress & pitfalls. Breast Cancer Manag. 7(1), BMT06 (2018)
T. Ohnishi, The role of the p53 molecule in cancer therapies with radiation and/or hyperthermia. J. Cancer Res. Ther. 1(3), 147–150 (2005)
A.R. Gomes et al., Influence of P53 on the radiotherapy response of hepatocellular carcinoma. Clin. Mol. Hepatol. 21(3), 257 (2015)
K. Okaichi et al., Phosphorylation of p53 modifies sensitivity to ionizing radiation. Anticancer Res 31(6), 2255–2258 (2011)
J. Maeda et al., Intrinsic radiosensitivity and cellular characterization of 27 canine cancer cell lines. PLoS ONE 11(6), e0156689 (2016)
M.G. Lee, K.S. Lee, K.S. Nam, The association of changes in RAD51 and survivin expression levels with the proton beam sensitivity of Capan-1 and Panc-1 human pancreatic cancer cells. Int. J. Oncol. 54(2), 744–752 (2019)
R. Alan Mitteer et al., Proton beam radiation induces DNA damage and cell apoptosis in glioma stem cells through reactive oxygen species. Sci. Rep. 5(1), 13961 (2015)
M.G. Lee, K.S. Lee, K.S. Nam, Combined doxorubicin and arctigenin treatment induce cell cycle arrest-associated cell death by promoting doxorubicin uptake in doxorubicin-resistant breast cancer cells. IUBMB Life 75(9), 765–777 (2023)
V. Verma et al., Proton beam radiotherapy as part of comprehensive regional nodal irradiation for locally advanced breast cancer. Radiotherapy Oncol. 123(2), 294–298 (2017)
S.-Y. Chun, K.-S. Nam, K.-S. Lee, Proton beam induces P53-mediated cell cycle arrest in HepG2 hepatocellular carcinoma cells. Biotechnol. Bioprocess Eng. 25, 141–148 (2020)
D.C. Weber et al., Proton therapy for pediatric malignancies: fact, figures and costs. A joint consensus statement from the pediatric subcommittee of PTCOG. PROS and EPTN. Radiotherapy Oncol. 128(1), 44–55 (2018)
L. Jezkova et al., Particles with similar LET values generate DNA breaks of different complexity and reparability: a high-resolution microscopy analysis of γH2AX/53BP1 foci. Nanoscale 10(3), 1162–1179 (2018)
Q. Zhou et al., Inhibition of ATM induces hypersensitivity to proton irradiation by upregulating toxic end joining. Can. Res. 81(12), 3333–3346 (2021)
X. Zhong et al., R ad51 in regulating the radiosensitivity of non-small cell lung cancer with different epidermal growth factor receptor mutation status. Thorac. Cancer 7(1), 50–60 (2016)
H.W. Chang et al., Expression of Ku80 correlates with sensitivities to radiation in cancer cell lines of the head and neck. Oral Oncol. 42(10), 979–986 (2006)
Y. Nimura et al., Silencing Ku80 using small interfering RNA enhanced radiation sensitivity in vitro and in vivo. Int. J. Oncol. 30(6), 1477–1484 (2007)
C. Chen et al., Autophagy and doxorubicin resistance in cancer. Anticancer Drugs 29(1), 1–9 (2018)
Y. Gong et al., The role of necroptosis in cancer biology and therapy. Mol. Cancer 18(1), 1–17 (2019)
M.A. O’Brien, R. Kirby, Apoptosis: a review of pro-apoptotic and anti-apoptotic pathways and dysregulation in disease. J. Vet. Emerg. Crit. Care 18(6), 572–585 (2008)
A. Bürkle et al., PARP and the release of apoptosis-inducing factor from mitochondria. Poly(ADP-Ribosyl) ation 2006, 103–117 (2006)
M. Malumbres, M. Barbacid, Cell cycle, CDKs and cancer: a changing paradigm. Nat. Rev. Cancer 9(3), 153–166 (2009)
T. Otto, P. Sicinski, Cell cycle proteins as promising targets in cancer therapy. Nat. Rev. Cancer 17(2), 93–115 (2017)
S. Cagnol, J.C. Chambard, ERK and cell death: mechanisms of ERK-induced cell death—apoptosis, autophagy and senescence. FEBS J. 277(1), 2–21 (2010)
E. Berra, M.A.T. Diaz-Meco, J. Moscat, The activation of p38 and apoptosis by the inhibition of Erk is antagonized by the phosphoinositide 3-kinase/Akt pathway. J. Biol. Chem. 273(17), 10792–10797 (1998)
S. Cagnol, E. Van Obberghen-Schilling, J.-C. Chambard, Prolonged activation of ERK1, 2 induces FADD-independent caspase 8 activation and cell death. Apoptosis 11(3), 337–346 (2006)
Acknowledgements
This research was supported by the National Research Foundation of Korea (NRF) grant funded by the Korean Government (MSIT) (#2021R1F1A1060350, #2022R1A2C1013203).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maharjan, S., Lee, MG., Nam, KS. et al. Effect of proton-beam irradiation on cell survival of MCF-7 and its chemo-resistant subgroups. J. Korean Phys. Soc. 85, 271–278 (2024). https://doi.org/10.1007/s40042-024-01089-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40042-024-01089-5