Abstract
Aims
The prognosis and the clinical manifestations of HIV infection have changed with the introduction of the potent combination antiretroviral therapy (cART); however, up to 50% of patients meet research criteria for “HIV-associated neurocognitive disorders” (HAND) according with current nosology. The majority of patients affected by HAND, especially in cohorts with suppressed plasma viremia, showed an Asymptomatic Neurocognitive Impairment (ANI), without any functional impairment. After more than 10 years from the introduction of the current so-called “Frascati criteria”, this mini-review aimed to address the emerging limitations in current diagnosis procedures.
Methods
We discussed the most relevant literature on HAND prevalence, etiology, and diagnosis.
Results
We addressed three main emerging issues: (1) the unclear clinical relevance of ANI entity; (2) the evidences that Frascati criteria could produce a significant overestimation of HAND; (3) the need to better identify patients with a higher risk to develop HAND requiring routine neuropsychological examinations.
Conclusions
Frascati criteria should be updated to better respond to the present characteristics of HIV + cohorts and to help clinicians in their cognitive and global management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Current nosology for HIV-associated neurocognitive disorders
The central nervous system (CNS) represents one of the major targets of HIV, and neurological complications could generate severe disability and worse prognosis. Neuroimaging data show a typical “subcortical” pattern with abnormalities especially in the basal ganglia, thalamus, cerebellum and cortical motor circuits [1, 2].
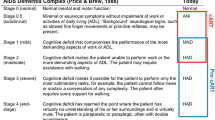
In 1991, the American Academy of Neurology AIDS Task Force published the nosology and diagnostic criteria for the HIV-associated dementia (HAD) [3], emerging as a progressive dementia frequently accompanied by motor and behavioral dysfunctions [4]. In 2007, in light of great changes occurred in incidence, prevalence and profile of HAD with the advent of the potent combination antiretroviral therapy (cART), diagnostic criteria were updated [5] and the term “HIV-associated neurocognitive disorders” (HAND) was introduced for the entire spectrum of neurocognitive diseases in the context of HIV, including a new pathology entity named “asymptomatic neurocognitive impairment” (ANI). These revised “Frascati criteria” identify three patterns of worsening cognitive-functional dysfunctions: (i) and (ii) a performance 1 standard deviation (SD) below the normative mean in at least two cognitive areas detected by a neuropsychological battery including at least five cognitive domains (learning, attention/working memory, executive functions, fine motor skills or sensory perceptual abilities, and language) is needed for a diagnosis of ANI or Mild Neurocognitive Disorder (MND); the discrimination between these two categories depends by functional impairment (usually identified assessing the Instrumental Activities of Daily Living) that must be absent for ANI; (iii) a performance 2 SD below the normative mean in at least two cognitive areas is necessary for a diagnosis of HAD together with a severe functional impairment. These three patterns must not be explained by co-morbidities or confounding conditions (i.e. active psychiatric syndromes or drugs/alcohol abuse), with no evidence of delirium or pre-existing causes.
Frascati criteria suggest administering at least two tests for each cognitive function, but there is a great heterogeneity across studies about neuropsychological methodology. Moreover, Frascati panel recommended the usage of this classification only for research purposes, but it has been regularly adopted into clinical practice [6].
This review, after more than 10 years from the introduction of Frascati criteria, aimed to summarize the most relevant literature available on HAND prevalence and etiology, and to address the emerging limitations in current diagnosis procedures.
HAND in the cART era: a multifactorial etiology
Although the incidence of HAD has significantly decreased after the introduction of cART [7, 8], up to 50% of patients meet research criteria for HAND [9, 10]. Moreover, the longer lifespan of patients with HIV, as a consequence of effective cART, together with older age at seroconversion, has contributed to increase the risk of neurodegeneration [11, 12] with higher incidence of dementia in older people [13]. It is plausible that aging and HIV infection interact and increase the risk of neurodegeneration, particularly in the frontal lobe and hippocampus, and accelerate cognitive decay, especially in processing speed, working memory, and learning [11]. In support of this hypothesis, there are evidences of higher levels of brain beta amyloid and plaque-like lesions in older HIV-infected adults than in those who are seronegative [14]. Thus, it is possible that older HIV-infected adults might be more likely to show some aspects of the cortical cognitive pattern of Alzheimer’s disease than the more typical subcortical cognitive profile observed in younger individuals; however, until now, controversial results have been observed in support to this “cortical hypothesis” [15,16,17,18,19].
Moreover, also in the setting of HIV infection, there are evidences of successful cognitive aging among individuals with a high cognitive reserve, a concept proposed to explain the discrepancy between the degree of brain pathologies and clinical manifestations and strongly correlated to education and premorbid intelligence [20]; in particular, a lower risk of HAND has been observed in patients with higher cognitive reserve [21, 22].
Among HIV-specific key factors that have shown a correlation with HAND in the cART era, we found poor treatment adherence [23] and neurotoxic effects of some antiretroviral agents as Efavirenz [24, 25]. Although there are controversial results, also poor Central Nervous System (CNS) penetration of some antiretroviral drugs, as estimated by CHARTER group [9, 26, 27], may contribute to HAND [28,29,30,31]. Differences in neuro-efficacy across different antiretroviral agents, with the development of drug resistance in brain cells not present in blood, could explain the occurrence of detectable HIV RNA in cerebrospinal fluid (CSF) when undetectable in plasma, event termed as “CSF viral escape” [32, 33]; in clinical practice, it can be seen in around 10% of individuals undergoing lumbar puncture [34, 35], however, the association between viral escape and cognitive impairment is not consistent [36]. One explanation for the weakness of this association is that HIV RNA levels in CSF are an imperfect proxy for HIV replication in brain tissue; an alternative explanation is that CNS pathology is a result of immune dysregulation rather than virus-related cytopathy, thus HIV RNA concentrations in CSF might not be the most accurate biomarker for cognitive impairment [37]. According with this last hypothesis, a strong correlation has been demonstrated with the immunosuppression before ART is initiated, as estimated by the nadir CD4 + cell count [38], that might be due to an irreversible CNS injury before treatment, a so-called “legacy effect” [32]. An alternative reason might be a process of immune or glial cell activation that occurs during advanced immunosuppression, which persists after treatment and immune recovery [39, 40]. Two neuroimaging studies [41, 42] have provided evidences of persistent CNS inflammation, despite viral suppression using, respectively, a PET marker of activated microglia, and a fermoxytolol contrast agent, a substance readily taken up by circulating monocytes, showing monocyte–macrophage pathways and microglia involvement in HAND despite cART treatment [43]. Among brain injury biomarkers, neurofilament protein (NFL) was associated to CNS axonal damage in patients with HAD or without dementia but lower CD4 cell count [44, 45], while successful treatment was associated with normal or slightly elevated CSF NFL levels [44]. Also, plasma NFL levels were found to be highly correlated with CSF NFL measurement, representing a more accessible measure of CNS injury [46, 47]. Additionally, there are evidences that also soluble amyloid precursor proteins alpha and beta are abnormal in HAD [44].
In 2014, a CSF HIV risk score was developed [48] by implementing a prediction modeling to estimate the risk of detectable CSF HIV RNA (threshold > 50 copies/mL). The scoring includes well-known risk factors as plasma HIV RNA, cART drug CNS penetration, duration of cART therapy, medication adherence, race, and depression status and authors identified a threshold associated to a higher risk of detectable CSF HIV RNA; however, there are no evidences of a significant association between this score and abnormal performances at neurocognitive evaluation.
Thus, it could be very useful to develop a combination of biomarkers reflecting neuronal injury and glial cell or immune activation in combination with HIV RNA concentrations in CSF [37].
ANI: what is the clinical relevance?
In countries where cART is widely available as Europe, up to 90% of HIV-positive patients on stable therapy are successfully treated and they might approach a normal life expectancy [49]. The prevalence of HAND in a cohort of patients with suppressed plasma viremia decreased to around 20% or less [50]. Moreover, most of the patients with HAND showed the ANI profile [5] and its clinical relevance is unclear, because the progression to a symptomatic status was documented only in one longitudinal study [51]. Moreover, it was demonstrated that Frascati criteria might generate a high false-positive rate (about 20% if we administer one test/cognitive domain, and about 15% in case of two tests/cognitive domain) that could be reduced to an acceptable level if cognitive evaluation includes two tests for domain with a more stringent threshold to define impairment, as 1.5 SD below the normative mean instead of 1 SD [6, 52]; in other terms, the criteria for ANI could produce a significant overestimation of HAND prevalence due to a statistical artifact. Moreover, the authors argued that the ANI entity arises ethical issues because could generate needless worries, especially in the absence of a clear alarm about the future worsening. Finally, to screen for HAND, all the HIV-infected patients, without an algorithm that takes in account both risk factors and cognitive complaints from patients or relatives, could be not sustainable considering the limited resources in clinical settings.
Latest clinical guidelines, as EACS or BHIVA, take in account the unclear relevance of ANI diagnosis, indeed they are focused only on symptomatic patients for the execution of neurocognitive evaluation, and only in case of clinical relevant damage, they recommended to proceed with brain Magnetic Resonance Imaging (MRI) and CSF examination to verify if damage was associated to HIV or other additional causes: when HIV-associated damage is confirmed, clinicians have to start ART for patients without therapy, or to optimize ART by including more CNS-active drugs for those already on therapy.
Also, in accordance to Frascati criteria, it is important to exclude that cognitive impairment could be due to some co-morbidities. However, patients with HAND are more likely to have co-morbidities, as HCV co-infection [53, 54] cardiovascular diseases [55], or depression [56]. In the only longitudinal study showing a risk of ANI to involve into a symptomatic status [51], drugs abuse and co-morbidities were independently associated with a higher risk to functional decline. However, in that study, specific HIV factors (i.e. AIDS diagnosis, lower CD4 cell count at nadir, and off-therapy) were associated to ANI, suggesting that this pattern may actually represent a cognitive profile which is HIV driven. Nevertheless, taking in account the evidences from other studies, it is plausible that the criteria for ANI generate a significant “false positive” rate or a misclassification of patients with cognitive impairment attributable to non-HIV conditions. Indeed, in cohorts of patients with suppressed plasma viremia, the effects of HIV on cognition seem overshadowed by non-HIV factors, as subclinical cerebrovascular disease [57]. Thus, co-morbidities might lead to overestimate the prevalence of HAND [52], and this “bias” could partially explain differences in HAND proportion across studies [37].
In 2013, Veterans Aging Cohort Study (VACS) Index [58] was developed as a composite marker of HIV severity based on routine clinical blood tests; it includes both HIV traditional biomarkers of severity (i.e. plasma viremia, CD4 cell count) and non-traditional biomarkers related to co-morbidities as HCV co-infection, renal or liver functions. Having a very high VACS index was associated in a longitudinal study to a higher risk of cognitive decline [59], thus it could be a simple tool for identifying HIV-infected patients who are at high risk for HAND and requiring routine neuropsychological evaluations. This kind of simple tools might be very useful due to the multifactorial etiology of HAND.
Finally, a growing body of evidences suggests that neuroinflammation might be a component in Alzheimer’s disease (AD) etiology [60]. Many viral, bacterial, and fungal agents have shown a role in the induction and amplification of chronic neuroinflammation in AD, as human herpesvirus 1 (HHV-1), varizella zoster virus (HHV-2), HHV-6 [61], cytomegalovirus, polyomavirus JC [62]; Porphyromonas gingivalis, Treponema denticola, or Candida albicans or toxoplasma [60]. These infectious agents could contribute or influence the development of HAND. However, probably, we need to gain a better understanding of their role in the context of HIV to evaluate their utility in enlarging Frascati criteria.
Future directions
On the basis of the existing literature, probably, we need to review the adequacy of Frascati criteria and to discuss the aspects that require updating to better respond to the present characteristics of HIV-infected cohorts and to help clinicians in their global management, taking in account also the introduction during the last decade of new antiretroviral agents of increasing tolerability and safety with significant improvements in medical adherence, especially with single-tablet regimen [63]. Key points on what changes should be made to the nosology of HAND are summarized in Fig. 1.
At least in countries with high availability of treatment for all patients as Europe, we are witnessing a process of progressive improvement of quality of life and life expectancy of people living with HIV that involves both the cognitive and functional areas. From an operational point of view, probably, we need to develop an algorithm that includes the impact of the most important specific HIV risk factors in the expression of cognitive decline, and considering also the most sensitive and specific new emerging biomarkers of CNS damage driven by HIV, as soluble CD14, interleukin-6 (IL-6), and tumor necrosis factor-a that have been investigated in a sample of HIV-infected patients on successful ART without co-morbidities, and high IL-6 levels were associated with neurocognitive impairment [64]. Neuronal biomarkers could be useful tools in follow-up monitoring of HIV-infected patients and added to enlarge the Frascati criteria. In other terms, one of the major goals of neuropsychological evaluation could be finding neurocognitive impairment directly attributable to HIV and not to other conditions [65].
Nevertheless, if we take a look to other neurologic diseases, as cognitive decline in Alzheimer’s or Parkinson’s diseases, current nosology includes a borderline status, named “Mild Cognitive Impairment” (MCI), that is partially comparable to MND pattern of HAND, while there is not an issue corresponding to ANI, because MCI criteria are focused only on patients with cognitive complaints and, based on Gaussian distribution, they applied a more stringent cut-off that one applied to ANI to define abnormality (i.e. < 1.5 SD instead of < 1 SD) [66, 67]. Moreover, it has been previously demonstrated that neurologically healthy subjects do not necessarily score above the cut-off in all tasks included in a composite battery [68]. Thus, we need to better define the neuropsychological procedures to avoid possible bias due to statistical artifacts and to reduce the great methodology heterogeneity across studies and clinical practice. However, different methods in detecting HAND could depend by the specific context, as suggested by a recent study of comparison between the clinical rating (impairment in at least two ability domains) and the global deficit scores (number and severity of impairments across all measures) showing strengths and weakness of both approaches [69].
For research purpose, probably, it is always important to include a group of healthy subjects matched with HIV-infected patients not only for demographic characteristics, but also from a cultural–social point of view. Indeed, the normative scores of cognitive tests frequently were obtained in studies completed decades ago and are no longer representative of current populations.
Finally, we need to develop cognitive tests that could be cross-cultural not only for the evaluation in resource-limited settings, but also due to increasing multiethnic HIV cohorts in European and North-American countries.
References
Gongvatana A, Schweinsburg BC, Taylor MJ, Theilmann RJ, Letendre SL, Alhassoon OM, et al. White matter tract injury and cognitive impairment in human immunodeficiency virus-infected individuals. J Neurovirol. 2009;15:187–95.
Klunder AD, Chiang MC, Dutton RA, Lee SE, Toga AW, Lopez OL, et al. Mapping cerebellar degeneration in HIV/AIDS. Neuroreport. 2008;19:1655–9.
Janssen RS, Cornblath DR, Epstein LG, Foa RP, McArthur JC, Price RW, et al. Nomenclature and research case definitions for neurological manifestations of human immunodeficiency virus type-1 (HIV-1) infection. Report of a Working Group of the American Academy of Neurology AIDS Task Force. Neurology. 1991;41:778–85.
Navia BA, Jordan BD, Price RW. The AIDS dementia complex: I. Clinical features. Ann Neurol J. 1986;19:517–24.
Antinori A, Arendt G, Becker JT, Brew BJ, Byrd DA, Cherner M, et al. Updated research nosology for HIV-associated neurocognitive disorders. Neurology. 2007;69:1789–99.
Torti C, Focà E, Cesana BM, Lescure FX. Asymptomatic neurocognitive disorders in patients infected by HIV: fact or fiction? BMC Med. 2011;9:138.
Sacktor N, Lyles RH, Skolasky R, Kleeberger C, Selnes OA, Miller EN, et al. HIV-associated neurologic disease incidence changes: multicenter AIDS Cohort Study, 1990–1998. Neurology. 2001;56:257–60.
Mc Arthur JC. HIV Dementia: an evolving disease. J Neuroimmunol. 2004;157:3–10.
Heaton RK, Clifford DB, Franklin DR Jr, Woods SP, Ake C, Vaida F, et al. HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy: CHARTER Study. Neurology. 2010;75:2087–96.
Simioni S, Cavassini M, Annoni JM, Rimbault Abraham A, Bourquin I, et al. Cognitive dysfunction in HIV patients despite long-standing suppression of viremia. AIDS. 2010;24:1243–50. https://doi.org/10.1097/QAD.0b013e3283354a7b.
Brew BJ, Crowe SM, Landay A, Cysique LA, Guillemin G. Neurodegeneration and aging in the HAART era. J Neuroimmune Pharmacol. 2009;4:163–74.
Deeks SG. HIV infection, inflammation, immunosenescence, and aging. Annu Rev Med. 2011;62:141–55. https://doi.org/10.1146/annurev-med-042909-09375.
Valcour V, Shikuma C, Shiramizu B, Watters M, Poff P, Selnes O, et al. Higher frequency of dementia in older HIV-1 individuals: the Hawaii aging with HIV-1 cohort. Neurology. 2004;63:822–7.
Achim CL, Adame A, Dumaop W, Everall IP, Masliah E. Increased accumulation of intraneuronal amyloid beta in HIV-infected patients. J Neuroimmune Pharmacol. 2009;4:190–9.
Ciccarelli N, Fabbiani M, Baldonero E, Fanti I, Cauda R, Di Giambenedetto S, et al. Effect of aging and human immunodeficiency virus infection on cognitive abilities. J Am Geriatr Soc. 2012;60:2048–55. https://doi.org/10.1111/j.1532-5415.2012.04213.x.
Ciccarelli N, Limiti S, Fabbiani M, Baldonero E, Milanini B, Lamonica S, et al. Verbal list learning and memory profiles in HIV-infected adults, Alzheimer’s disease, and Parkinson’s disease: an evaluation of the “cortical hypothesis” of NeuroAIDS. Appl Neuropsychol Adult. 2017;24:410–9. https://doi.org/10.1080/23279095.2016.1189424.
Cysique LA, Maruff P, Bain MP, Wright E, Brew BJ. HIV and age do not substantially interact in HIVassociated neurocognitive impairment. J Neuropsychiatry. 2011;23:83–9. https://doi.org/10.1176/appi.neuropsych.23.1.83.
Scott JC, Woods SP, Carey CL, Weber E, Bondi MW, Grant I. Neurocognitive consequences of HIV infection in older adults: an evaluation of the “cortical” hypothesis. AIDS Behav. 2011;6:1187–96. https://doi.org/10.1007/s10461-010-9815-8.
Valcour V, Paul R, Neuhaus J, Shikuma C. The effects of age and HIV on neuropsychological performance. J Int Neuropsychol Soc. 2011;17:190–5. https://doi.org/10.1017/S1355617710001438.
Stern Y. What is cognitive reserve? Theory and research application of the reserve concept. J Int Neuropsychol Soc. 2002;8:448–60.
Milanini B, Ciccarelli N, Fabbiani M, Limiti S, Grima P, Rossetti B, et al. Cognitive reserve and neuropsychological functioning in older HIV-infected people. J Neurovirol. 2016;22:575–83.
Morgan EE, Woods SP, Smith C, Weber E, Scott JC, Grant I. Lower cognitive reserve among individuals with syndromic HIV-associated neurocognitive disorders (HAND). AIDS Behav. 2012;16:2279–85.
Lovejoy T, Suhr JA. The relationship between neuropsychological functioning and HAART adherence in HIV-positive adults: a systematic review. J Behav Med. 2009;32:389–405. https://doi.org/10.1007/s10865-009-9212-9.
Ciccarelli N, Fabbiani M, Di Giambenedetto S, Fanti I, Baldonero E, Bracciale L, et al. Efavirenz associated with cognitive disorders in otherwise asymptomatic HIV-infected patients. Neurology. 2011;76:1403–9. https://doi.org/10.1212/WNL.0b013e31821670fb.
Underwood J, Robertson KR, Winston A. Could antiretroviral neurotoxicity play a role in the pathogenesis of cognitive impairment in treated HIV disease? AIDS. 2015;29:253–61.
Letendre S, Marquie-Beck J, Capparelli E, Best B, Clifford D, Collier AC, et al. Validation of the CNS penetration-effectiveness rank for quantifying antiretroviral penetration into the central nervous system. Arch Neurol. 2008;65:65–70.
Letendre S. Central nervous system complications in HIV disease: HIV-associated neurocognitive disorder. Top Antivir Med. 2011;19:137.
Cysique LA, Waters EK, Brew BJ. Central nervous system antiretroviral efficacy in HIV infection: a qualitative and quantitative review and implications for future research. BMC Neurol. 2011;11:148. https://doi.org/10.1186/1471-2377-11-148.
Ciccarelli N, Fabbiani M, Colafigli M, Trecarichi EM, Silveri MC, Cauda R, et al. Revised central nervous system neuropenetration-effectiveness score is associated with cognitive disorders in HIV-infected patients with controlled plasma viraemia. Antivir Ther. 2013;18:153–60. https://doi.org/10.3851/IMP2560.
Ellis RJ, Letendre S, Vaida F, Haubrich R, Heaton RK, Sacktor N, et al. Randomized trial of central nervous system-targeted antiretrovirals for HIV-associated neurocognitive disorder. Clin Infect Dis. 2014;58:1015–22. https://doi.org/10.1093/cid/cit921.
Fabbiani M, Grima P, Milanini B, Mondi A, Baldonero E, Ciccarelli N, et al. Antiretroviral neuropenetration scores better correlate with cognitive performance of HIV-infected patients after accounting for drug susceptibility. Antivir Ther. 2015;20:441–7. https://doi.org/10.3851/IMP2926.
Canestri A, Lescure FX, Jaureguiberry S, Moulignier A, Amiel C, Marcelin AG, et al. Discordance between cerebral spinal fluid and plasma HIV replication in patients with neurological symptoms who are receiving suppressive antiretroviral therapy. Clin Infect Dis. 2010;50:773–8.
Peluso MJ, Ferretti F, Peterson J, Lee E, Fuchs D, Boschini A, et al. Cerebrospinal fluid HIV escape associated with progressive neurologic dysfunction in patients on antiretroviral therapy with well controlled plasma viral load. AIDS. 2012;26:1765–74. https://doi.org/10.1097/QAD.0b013e328355e6b2.
Edén A, Fuchs D, Hagberg L, Nilsson S, Spudich S, Svennerholm B, et al. HIV-1 viral escape in cerebrospinal fluid of subjects on suppressive antiretroviral treatment. J Infect Dis. 2010;202:1819–25.
Valero IP, Letendre S, Ellis R, Deutsch R, Franklin D, Clifford D, et al. Prevalence and risk factors for HIV CSF Viral Escape: results from the CHARTER and HNRP cohorts. J Int AIDS Soc. 2012;15:18189.
Brew BJ, Letendre SL. Biomarkers of HIV related central nervous system disease. Int Rev Psychiatry. 2008;20:73–88. https://doi.org/10.1080/09540260701878082(Review).
Nightingale S, Winston A, Letendre S, Michael BD, McArthur JC, Khoo S, et al. Controversies in HIV associated neurocognitive disorders. Lancet Neurol. 2014;13:1139–51.
Ellis RJ, Badiee J, Vaida F, Letendre S, Heaton RK, Clifford D, et al. CD4 nadir is a predictor of HIV neurocognitive impairment in the era of combination antiretroviral therapy. AIDS. 2011;25:1747–51.
Van Sighem AI, Gras LA, Reiss P, Brinkman K, De Wolf F. Life expectancy of recently diagnosed asymptomatic HIV-infected patients approaches that of uninfected individuals. AIDS. 2010;24:1527–35.
McArthur JC, Steiner J, Sacktor N, Nath A. Human immunodeficiency virus-associated neurocognitive disorders: mind the gap. Ann Neurol. 2010;67:699–714.
Garvey LJ, Pavese N, Politis M, Ramlackhansingh A, Brooks DJ, Taylor-Robinson SD, et al. Increased microglia activation in neurologically asymptomatic HIV-infected patients receiving effective ART. AIDS. 2014;28:67–72.
Nakamoto BK, Shikuma CM, Ogata-Arakaki D, Umaki T, Neuwelt EA, Shiramizu BT, et al. Feasibility and potential role of ferumoxytol-enhanced neuroimaging in HIV-associated neurocognitive disorder. J Neurovirol. 2013;19:601–5.
Hellmuth J, Milanini B, Valcour V. Interactions between ageing and NeuroAIDS. Curr Opin HIVAIDS. 2014;9:527–32. https://doi.org/10.1097/COH.0000000000000104.
Peterson J, Gisslen M, Zetterberg H, Fuchs D, Shacklett BL, Hagberg L, et al. Cerebrospinal fluid (CSF) neuronal biomarkers across the spectrum of HIV infection: hierarchy of injury and detection. PLoS One. 2014;9:e116081.
Krut JJ, Zetterberg H, Blennow K, Cinque P, Hagberg L, Price RW, et al. Cerebrospinal fluid Alzheimer’s biomarker profiles in CNS infections. J Neurol. 2013;260:620–6. https://doi.org/10.1007/s00415-012-6688-y.
Gisslén M, Price RW, Andreasson U, Norgren N, Nilsson S, Hagberg L, et al. Plasma concentration of the neurofilament light protein (NFL) is a biomarker of CNS injury in HIV infection: a cross-sectional study. EBioMedicine. 2015;3:135–40. https://doi.org/10.1016/j.ebiom.2015.11.036.
Milanini B, Valcour V. Differentiating HIV-associated neurocognitive disorders from Alzheimer’s disease: an emerging issue in geriatric NeuroHIV. Curr HIV AIDS Rep. 2017;14:123–32. https://doi.org/10.1007/s11904-017-0361-0(Review).
Hammond ER, Crum RM, Treisman GJ, Mehta SH, Marra CM, Clifford DB, et al. The cerebrospinal fluid HIV risk score for assessing central nervous system activity in persons with HIV. Am J Epidemiol. 2014;180:297–307. https://doi.org/10.1093/aje/kwu098.
May MT, Gompels M, Delpech V, et al. UK collaborative HIV cohort (UK CHIC)-study impact on life expectancy of HIV-1 positive individuals of CD4 + cell count and viral load response to antiretroviral therapy. AIDS. 2014;28:1193–202.
Garvey L, Surendrakumar V, Winston A. Low rates of neurocognitive impairment are observed in neuro-asymptomatic HIV-infected subjects on effective antiretroviral therapy. HIV Clin Trials. 2011;12:333–8. https://doi.org/10.1310/hct1206-333.
Grant I, Franklin DR Jr, Deutsch R, Woods SP, Vaida F, Ellis RJ, et al. Asymptomatic HIV-associated neurocognitive impairment increases risk for symptomatic decline. Neurology. 2014;82:2055–62. https://doi.org/10.1212/WNL.0000000000000492.
Gisslén M, Price RW, Nilsson S. The definition of HIV-associated neurocognitive disorders: are we overestimating the real prevalence? BMC Infect Dis. 2011;11:356.
Ciccarelli N, Fabbiani M, Grima P, Falasca K, Tana M, Baldonero E, et al. Comparison of cognitive performance in HIV or HCV mono-infected and HIV-HCV co-infected patients. Infection. 2013;41:1103–9. https://doi.org/10.1007/s15010-013-0503-2.
Vivithanaporn P, Nelles K, DeBlock L, Newman SC, Gill MJ. Power C Hepatitis C virus co-infection increases neurocognitive impairment severity and risk of death in treated HIV/AIDS. J Neurol Sci. 2012;312:45–51.
Wright EJ, Grund B, Robertson K, Brew BJ, Roediger M, Bain MP, et al. Cardiovascular risk factors associated with lower baseline cognitive performance in HIV-positive persons. Neurology. 2010;75:864–73.
Ammassari A, Antinori A, Aloisi MS, Trotta MP, Murri R, Bartoli L, et al. Depressive symptoms, neurocognitive impairment, and adherence to highly active antiretroviral therapy among HIV-infected persons. Psychosomatics. 2004;45:394–402.
Fabbiani M, Ciccarelli N, Tana M, Farina S, Baldonero E, Di Cristo V, et al. Cardiovascular risk factors and carotid intima-media thickness are associated with lower cognitive performance in HIV-infected patients. HIV Med. 2013;14:136–44. https://doi.org/10.1111/j.1468-1293.2012.01044.x.
Akgün KM, Gordon K, Pisani M, Fried T, McGinnis KA, Tate JP, et al. Risk factors for hospitalization and medical intensive care unit (MICU) admission among HIV-infected Veterans. J Acquir Immune Def Syndr. 2013;62:52–9.
Marquine MJ, Montoya JL, Umlauf A, Fazeli PL, Gouaux B, Heaton RK, et al. The veterans aging cohort study (VACS) index and neurocognitive change: a longitudinal study. Clin Infect Dis. 2016;63:694–702. https://doi.org/10.1093/cid/ciw328.
Sochocka M, Zwolińska K, Leszek J. The infectious etiology of Alzheimer’s disease. Curr Neuropharmacol. 2017;15:996–1009. https://doi.org/10.2174/1570159X15666170313122937(Review).
Romeo MA, Faggioni A, Cirone M. Could autophagy dysregulation link neurotropic viruses to Alzheimer’s disease? Neural Regen Res. 2019;14:1503–6.
Valle Del, Piña-Oviedo S. Human polyomavirus JCPyV and its role in progressive multifocal leukencephalopathy and oncogenesis. Front Oncol. 2019;9:711.
Clay PG, Yuet WC, Moecklinghoff CH, Duchesne I, Tronczyński KL, Shah S, Shao D. A meta-analysis comparing 48-week treatment outcomes of single and multi-tablet antiretroviral regimens for the treatment of people living with HIV. AIDS Res Ther. 2018;15:17. https://doi.org/10.1186/s12981-018-0204-0.
Portilla I, Reus S, León R, van-der Hofstadt C, Sánchez J, López N, et al. Neurocognitive impairment in well-controlled HIV-infected patients: a cross-sectional study. AIDS Res Hum Retrovir. 2019;35:634–41. https://doi.org/10.1089/aid.2018.0279.
Robertson K, Liner J, Heaton R. Neuropsychological assessment of HIV-infected populations in international settings. Neuropsychol Rev. 2009;19:232–49. https://doi.org/10.1007/s11065-009-9096-z.
Jongsiriyanyong & Limpawattana. Mild cognitive impairment in clinical practice: a review article. Am J Alzheimers Dis Other Demen. 2018;33:500–7. https://doi.org/10.1177/1533317518791401.
Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56:303–8.
Capitani E, Laiacona M. Composite neuropsychological batteries and demographic correction: standardization based on equivalent scores, with a review of published data: the Italian group for the neuropsychological study of ageing. J Clin Exp Neuropsychol. 1997;19:795–809.
Blackstone K, Moore DJ, Franklin DR Jr, Clifford DB, Collier AC, Marra CM, For the CHARTER group, et al. Defining neurocognitive impairment in HIV: deficit scores versus clinical ratings. K. Clin Neuropsychol. 2012. https://doi.org/10.1080/13854046.2012.694479.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that they have no competing interests.
Rights and permissions
About this article
Cite this article
Ciccarelli, N. Considerations on nosology for HIV-associated neurocognitive disorders: it is time to update? . Infection 48, 37–42 (2020). https://doi.org/10.1007/s15010-019-01373-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-019-01373-8