Abstract
Human immunodeficiency virus (HIV)-associated neurocognitive disorders (HAND) affect approximately half of people living with HIV despite viral suppression with antiretroviral therapies and represent a major cause of morbidity. HAND affects activities of daily living including driving, using the Internet and, importantly, maintaining drug adherence. Whilst viral suppression with antiretroviral therapies (ART) has reduced the incidence of severe dementia, mild neurocognitive impairments continue to remain prevalent. The neuropathogenesis of HAND in the context of viral suppression remains ill-defined, but underlying neuroinflammation is likely central and driven by a combination of chronic intermittent low-level replication of whole virus or viral components, latent HIV infection, peripheral inflammation possibly from a disturbed gut microbiome or chronic cellular dysfunction in the central nervous system. HAND is optimally diagnosed by clinical assessment with imaging and neuropsychological testing, which can be difficult to perform in resource-limited settings. Thus, the identification of biomarkers of disease is a key focus of the field. In this chapter, recent advances in the pathogenesis of HAND and biomarkers that may aid its diagnosis and treatment will be discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Despite viral suppression with antiretroviral therapy (ART), no cure for HIV exists, and comorbid disease now represents the major challenge for people living with HIV (PLWH). HIV-associated neurocognitive disorders (HAND) affect approximately 18–69% (variability related to characteristics of study population with differing risk factors) of PLWH despite viral suppression with ART (Heaton et al. 2010; Simioni et al. 2010; Sacktor et al. 2016; dos Santos-Silva et al. 2017; Robertson et al. 2007; Cysique and Brew 2011) and are independent risk factors of mortality (Ellis et al. 1997; Tambussi et al. 2000). HAND in the context of virally suppressive ART mainly impairs cognitive function, although mild motor and behavioural deficits are still common. HAND induces brain injury including total and regional brain volume reduction (Cardenas et al. 2009; Küper et al. 2011) as well as neurodegeneration at least in its broadest sense (Boban et al. 2017). However, the complete neuropathological characterisation of HAND with viral suppression is still evolving (Gelman 2015). Thus, HAND may dramatically affect a person’s ability to function and live independently. Typical examples include impacting a person’s ability to drive and use the Internet which may result in social withdrawal and relationship breakdowns (Woods et al. 2017). Furthermore, there is strong evidence to suggest that individuals with HAND are more prone to poor medication adherence (Hinkin et al. 2002; Kamal et al. 2017) which may cause antiviral drug resistance and HIV disease progression. Together with cardiovascular disease and non-AIDS-cancers, HAND represent the major burden that continue to affect virally suppressed PLWH.
HAND is subdivided into three categories (by increasing cognitive and functional severity): (1) asymptomatic neurocognitive impairment (ANI), (2) mild neurocognitive disorders (MND) and (3) HIV-associated dementia (HAD) (Antinori et al. 2007). Effective viral suppression with current ART regimens has reduced the incidence of HAD (once a major cause of HIV-associated mortality) from ~20% to 2–4% of PLWH (Heaton et al. 2010). However, the incidence of ANI and MND remains high in virologically suppressed individuals resulting in impairments that can predominantly affect learning and/or memory functions and complex attention (Heaton et al. 2010, 2011; Robertson et al. 2004; Harezlak et al. 2011; Cysique et al. 2004). Furthermore, the presence of ANI has also been linked to a twofold to sixfold increased risk of earlier development and more rapid onset of symptomatic HAND (Grant et al. 2014), highlighting the potential progressive nature of the disease. Thus, HAND is a significant health, social and financial burden affecting PLWH worldwide.
Traditionally, the pathogenesis of HAND, especially HAD, has been strongly associated with HIV viremia (i.e. low nadir CD4+ T cell count; high plasma and/or CSF viral load). However, HAND in the context of virally suppressive ART is likely related to other factors such as low-level viral replication of whole virus or viral components, epigenetic changes and even systemic inflammation driven by gastrointestinal dysfunction, factors which may present greater prognostic/diagnostic value in this era of suppressive ART. Furthermore, HAND does not affect all PLWH, indicating that some individuals are, for as yet undefined reasons, more susceptible to disease possibly implying that host cell factors may also play a role in disease pathogenesis. Here, we assess the potential mechanisms driving the pathogenesis of HAND in chronically HIV-infected virally suppressed individuals and how they may be targeted to improve health outcomes for people living with HIV (Fig. 1).
Insight from biomarkers of HAND into disease pathogenesis in the presence of ART. HIV-infected monocytes (and T cells) transmigrate the blood-brain barrier (BBB) to seed perivascular macrophages, astrocytes and microglia. Viral persistence may drive activation of microglia and astrocytes inducing pro-inflammatory cytokine production, altered glutamate uptake and altered metabolism which drives neuronal injury and degradation contributing to BBB damage, brain atrophy and ultimately HIV-associated neurocognitive disorders. Both CNS-derived and peripheral biomarkers of HAND are shown
2 HAND Prevalence, Diagnosis, Prognosis and Treatment
HAND is diagnosed by clinical neurological assessment with neuropsychological examination followed by radiology such as magnetic resonance imaging of the brain and CSF analysis. Since 2007 the ‘Frascati’ criteria – a consensus proposed by the National Institute of Mental Health and the National Institute of Neurological Diseases and Stroke (Antinori et al. 2007) – have been used to assess individuals’ neurocognitive capabilities, by scoring their (1) motor skills, (2) sensory-perceptual capacity, (3) speed of information processing, (4) memory (learning and recall), (5) abstraction and executive function, (6) attention and working memory, (7) verbal and language skills and (8) whether individuals need assistance with daily living (Antinori et al. 2007), with impairments in two or more cognitive areas indicative of disease. Scores are compared to the mean scores of age- and education-matched neurologically unimpaired individuals, and diagnosis is made as below:
HAD
Similar to dementia in HIV-uninfected individuals, HAD causes significant deficits in cognitive function and is the most severe form of HAND (Antinori et al. 2007; Vivithanaporn et al. 2010; Tozzi et al. 2005). As such, affected individuals have neurological impairments reflected of at least two standard deviations below those of neurologically unimpaired individuals in at least two cognitive domains, and they show mark decline in everyday function. Although the incidence of HAD has reduced globally (Heaton et al. 2010), HAD remains a significant burden in regions where access to efficacious ART is limited or non-existent with a 31–38% incidence rate (Wong et al. 2007; Lawler et al. 2010). Notably, HAD diagnosis is an independent predicator of mortality in individuals with advanced HIV/AIDS (Sevigny et al. 2007).
MND
MND affects ~11.7% of virally suppressed PLWH receiving ART (Heaton et al. 2010) and interferes with daily functioning mildly to moderately. It requires acquired impairment of at least one standard deviation below that of matched neurologically unimpaired individuals in two cognitive domains (Antinori et al. 2007). Typically, cognitive impairments associated with MND are detected by either self-reporting or observation by close relations. Impairments may present as mild interference in mental acuity; absenteeism; issues regarding relationships and social functioning; and/or poor adherence to ART, for which some individuals may require professional assistance (Hinkin et al. 2002).
ANI
ANI is the most recent subcategory of HAND (Antinori et al. 2007) and has been estimated to affect ~32.7% of PLWH despite viral suppression, representing ~70% of HAND cases (Heaton et al. 2010). Similar to the diagnosis of MND, individuals with ANI exhibit acquired impairment of at least one standard deviation below those of neurologically unimpaired individuals in two cognitive domains (Antinori et al. 2007). However, unlike individuals with MND, those with ANI do not exhibit interference with everyday living (Antinori et al. 2007). As such, ANI remains difficult to diagnose, and the clinical implications of ANI remain unclear and controversial (Torti et al. 2011; Nightingale et al. 2014). For example, some suggest that due to the asymptomatic nature of ANI, the ‘diagnosis’ of ANI may be a result of suboptimal performance in neurocognitive tests due to subjects being ‘tired’ or ‘distracted’ (Levine et al. 2017) and impart an unnecessary categorisation that could incur a degree of stigmatism (Chiao et al. 2013).
Conversely, growing evidence suggests that individuals with ANI are prone to disease progression with a twofold to sixfold increased risk of earlier development of symptomatic HAND (Grant et al. 2014), highlighting the importance of early identification affected individuals. These findings are supported by large longitudinal clinical studies describing disease progression including in patients with ANI (Sacktor et al. 2016; Gott et al. 2017; Heaton et al. 2015). Results from the CNS HIV Antiretroviral Therapy Effects Research (CHARTER) cohort found that 22.7% of participants (436 individuals in total) declined whilst 60.8% remained stable (Heaton et al. 2015). Similarly, the Multicentre AIDS Cohort Study (MACS) showed that whilst the majority of individuals (77%) remained neurocognitively stable, 13% deteriorated to a more severe form of HAND and 10% improved (Sacktor et al. 2016). Further, our recent data have shown that ANI has a biological underpinning of focal frontal brain atrophy, thereby validating its importance (Nichols et al. 2019). Despite these findings, the direct pathogenic mechanisms driving disease progression remain unclear.
2.1 Treatment
One of the early issues with HIV antiretroviral therapies was the variable and often poor ability of drugs to cross the blood-brain barrier (BBB) and target virus in the CNS. Treatment with antiretrovirals with the capacity to penetrate the CNS well (including abacavir, lamivudine, maraviroc, nevirapine, darunavir, lopinavir, dolutegravir and possibly other integrase inhibitors) is associated with improved neurocognitive functions (Cysique et al. 2009) and increased suppression of CSF HIV RNA in comparison to treatment with other drugs with poorer CNS penetrance scores (Carvalhal et al. 2016). However, some evidence suggests that standard ART regimens in some patients are sufficient (Lanoy et al. 2011; Ellis et al. 2014), possibly because there is already BBB impairment which allows drug access to the brain. Definitive results from randomised controlled trials have been hampered by under-recruitment, unexpected drug resistance, confounds and underappreciated delayed time to maximum efficacy of pre-trial entry therapies (sometimes up to 6–12 months) (Ellis et al. 2014). Current guidelines recommend the immediate initiation of therapy following the diagnosis of HIV (Panel on Antiretroviral Guidelines for Adults and Adolescents). Nonetheless, recent results from the START neurology sub-study have shown no neurocognitive advantage of immediate vs delayed initiation of therapy in individuals with CD4+ T cell counts >500 cells/μL (Wright et al. 2018). Novel therapeutic strategies, regimens and limitations are further discussed later in this chapter.
3 Risk Factors of HAND
HAND is influenced by many risk factors including current and nadir CD4+ T cell count, duration of HIV disease, age, co-infection, other comorbidities, notable diabetes and substance use (Saylor et al. 2016). Although viral suppression with ART has improved the life expectancy of PLWH to almost that of uninfected individuals (Trickey et al. 2017), chronic HIV-infection presents its own issues as age is an independent risk factor for HAND and chronic HIV infection is hypothesised to induce ‘premature ageing’ as people living with HIV exhibit higher risk and possibly earlier onset of age-related disease than uninfected individuals. Whether the mechanisms underlying the ‘premature ageing’ phenomenon reflect true ‘accelerated ageing’ (i.e. earlier onset and/or faster progression of disease) or ‘accentuated ageing’ (i.e. heightened severity of disease with same time of onset) is unclear, but work assessing onset/severity of neurocognitive disorders in people living with HIV supports a combination of both scenarios (Sheppard et al. 2017). Older PLWH (>50 years) are 3.26 times more likely to develop HAD than younger PLWH (<40 years) (Valcour et al. 2004) and show more rapid rates of progressive atrophy despite therapy, particularly in subcortical regions, than age-matched individuals (Clifford et al. 2017; Pfefferbaum et al. 2014; Nir et al. 2019). Older PLWH also show deficits in episodic memory and motor function relative to age-matched HIV-uninfected individuals (Goodkin et al. 2017), and functional brain changes in blood flow and brain age appear similar to those observed in ~15–20 year older HIV-uninfected individuals as measured by functional MRI (Ances et al. 2010). Furthermore, recent findings from a longitudinal study assessing 549 people living with HIV for up to 14 years have shown that these individuals exhibit accelerated age-related decline in brain volume, especially in the frontal cortex as measured by MRI (Pfefferbaum et al. 2014, 2018). Importantly, whilst these age-related changes were accentuated in individuals with a history of substance abuse and/or HCV co-infection, they persist even in individuals without these cofounders (Pfefferbaum et al. 2014, 2018).
The discrete mechanisms driving accelerated/accentuated age-related changes are unknown, but persistent inflammation and immune activation are at higher levels than the ageing process alone can explain (Angelovich et al. 2015). Specifically, measures of glial activation, neurotransmitters and ketone bodies in the CSF of PLWH mimic levels observed in older HIV-uninfected individuals and also correlated with age and adverse neurocognitive scores (Cassol et al. 2014). Recently, CSF levels of galectin-9, an immune modulatory protein linked to HIV persistence, was also found to be higher in virally suppressed individuals (Premeaux et al. 2019). However, levels were only indicative of neurocognitive impairment in older individuals, but not younger individuals. Furthermore, structural neuroimaging analyses by MRI suggests that virally suppressed PLWH experience accentuated brain atrophy, indicative of age-related changes, in comparison to HIV-uninfected controls (Cole et al. 2017). Epigenetic changes have also been implicated as the ‘brain age’ of PLWH with HAND, estimated by the epigenetic clock using DNA methylation analysis, appears 3.5 years older than individuals without HAND (Levine et al. 2016). Circulating HIV DNA in PBMCs also correlates with neurocognitive impairment, namely, in executive function, in older PLWH despite viral suppression (de Oliveira et al. 2015), also suggesting the role of HIV reservoirs in disease pathogenesis.
It is of note that whilst the extended duration of HIV infection is known to influence the pathogenesis of HAND, the median age of HIV infection may also influence neurocognitive disease prognosis. In 2016 over 17% of new HIV notifications in the USA were from individuals older than 50 years of age (Centers for Disease Control and Prevention 2017). This is problematic as older individuals tend to present with more advanced clinical disease as they are not routinely tested for HIV despite exhibiting some similar risk factors as younger persons such as multiple sexual partners (Asher et al. 2016). Furthermore, the dynamics of disease pathogenesis, and the use of biomarkers used to identify disease, may also change with age-related risk factors. Specifically, in a study by Fogel and colleagues, lipid dysfunction was found to be more highly associated with HAND in older PLWH, whilst methamphetamine use was more strongly associated with HAND in younger people (Fogel et al. 2015). Thus, chronological age, duration of infection and age of infection are significant confounders in HAND pathogenesis and may influence the efficacy of prognostic biomarkers of disease.
HAND is often associated with several comorbidities as HIV disease progresses (Guaraldi et al. 2011). As such, cardiovascular disease with risk factors such as hypercholesterolemia and hypertension is associated with neurocognitive impairment in virally suppressed PLWH (Wright et al. 2010). HAND has also been associated with dyslipidaemia in the CSF (Bandaru et al. 2013) as well as glomerular filtration rate, an indicator of both kidney function and CVD (Yuen et al. 2017). Non-HAND neurocognitive diseases such as Alzheimer’s disease (AD) may also confound HAND diagnosis. Until recently it was controversial whether PLWH have a propensity to develop AD. Beta-amyloid, characteristic of AD, has been found in brain tissue of PLWH (Green et al. 2005), and phosphorylated tau has been found in the CSF and plasma of PLWH and was associated with HAND (Brew et al. 2005), however, not in all cases (Krut et al. 2017; Clifford et al. 2009). PET scans have provided the first conclusive evidence of beta-amyloid accumulation in the CNS of a HIV-infected individual (Turner et al. 2016), suggesting the possible co-presence of HAND and/or AD. Thus, delineating HAND from AD, and more importantly treating appropriately, is of the utmost importance. Whilst PLWH appear at increased risk of Parkinson’s disease (Tisch and Brew 2009, 2010), the issue remains controversial and requires further study (Moulignier et al. 2015). It seems likely that the increased risk only pertains to those who already have HIV brain involvement as the mechanism is probably a ‘double hit’ to the basal ganglia and dopaminergic pathways both of which are also targets for HIV.
Host gene factors pose a risk to developing HAND with several immune-related genotypes associated with higher risk including CCR5-wt/wt (Singh et al. 2003), 195ApoE ε4, MBL2-O/O (Spector et al. 2010) and CCL2-2578G (Thames et al. 2015), although these genotypes do not encompass all individuals with HAND. Co-infection also contributes to HAND pathology. Cytomegalovirus (CMV) is a common co-infection in people living with HIV, and anti-CMV IgG levels have recently been linked with neurocognitive impairment in PLWH (Brunt et al. 2016; Letendre et al. 2018). Hepatitis C virus co-infection also confers ~twofold increased risk of cognitive impairment than HIV-infection alone (Ciccarelli et al. 2013).
4 HAND Pathophysiology
4.1 Natural HIV Infection of the CNS
HIV probably infects the CNS via a ‘Trojan horse’-like mechanism, whereby HIV-infected peripheral blood monocytes, particularly the CD14+CD16+ subset (Veenstra et al. 2017; Ellery et al. 2007), and T cells cross the BBB (Fischer-Smith et al. 2001; Honeycutt et al. 2018) (Fig. 1). Current thinking considers that BBB damage is a result of CNS infection though the reverse may be true to an extent – that is, systemic infection may also directly damage the BBB. During acute infection, HIV-1 RNA is detected in human CSF as early as 8 days postinfection (Valcour et al. 2012) and probably continues throughout natural infection in response to chemokines produced by microglia and astrocytes, as seen in individuals diagnosed with HAD (Persidsky et al. 1999). Furthermore, monocyte DNA content in untreated individuals is associated with progressive stages of HAND (Valcour et al. 2013). As such, recruitment of HIV-infected monocytes from sites such as the bone marrow to the CNS is thought to be a major contributor to CNS infection and neurological impairment (Burdo et al. 2010; Strickland et al. 2014).
Following transmigration to the CNS, monocytes mature into perivascular macrophages, which may (1) sustain HIV replication and mediate infection of surrounding cells, such as CD4-expressing macrophage and microglia (Fischer-Smith et al. 2001; Thompson et al. 2011; Burdo et al. 2013a; Kim et al. 2006), and (2) harbour latent HIV reservoirs (Thompson et al. 2011). We and others have shown that up to 19% of astrocytes, which express little to no CD4, are infected with HIV in individuals with HAD (Churchill et al. 2009), can latently harbour HIV and may mediate trans-infection HIV to CD4+ T cells (Gray et al. 2014). A recent report also suggests that pericytes forming the BBB may also be a site of HIV infection (Cho et al. 2019). Although HIV-infected CD4+ T cells and cell-free virus also enter the CNS, likely due to breakdown of the tight junctions forming the BBB (Strazza et al. 2011), macrophage-driven viral replication is thought to be the primary source of HIV replication in the CNS of patients at least those with severe HAND (Schnell et al. 2009).
Following CNS infection, HIV viral proteins, such as nef, vpr, gp120 and, in particular, extracellular tat (Bagashev and Sawaya 2013), activate surrounding macrophages, microglia and astrocytes to release cytokines and chemokines that drive localised neuroinflammation (Shah et al. 2011a, b; Shah and Kumar 2010; Sami Saribas et al. 2017); the effects of which target multiple sites in the CNS. Firstly, cytokines and chemokines can activate and actively damage the BBB, resulting in enhanced permeability and monocyte recruitment (driven by MCP-1 and CCL2 (Conant et al. 1998)), particularly of CD14+CD16+ monocytes (Williams et al. 2013). Secondly, cellular activation can act to enhance HIV replication (osteopontin, TNF and CXCL-10 (Brown et al. 2011; Williams et al. 2009)). Finally, components of the inflammatory milieu such as CXCL-10 (Mehla et al. 2012) and quinolinic acid (Kandanearatchi and Brew 2012) ultimately have neurotoxic effects on neurons via the generation of reactive oxygen species and lipid peroxidation; disruption of calcium homeostasis of neurons (Haughey et al. 1999) leading to neuronal apoptosis (IL-1β, IL-8, TNF (Guha et al. 2012)) and dysfunction of astrocytes ability to buffer glutamate via the N-methyl-D-aspartate receptor; all of these contribute to neuronal dysfunction, apoptosis and neurodegeneration. Neuronal injury occurs early in infection with PLWH with primary, untreated infection displaying heightened measures of neuronal injury such as CSF levels of neurofilament light chain protein (NFL) and neurometabolite dysfunction as determined by proton-magnetic resonance spectroscopy (MRS) (Peluso et al. 2013). Thus, HIV-induced neuroinflammation acts as a positive feedback loop driving HAND and other pathological injuries.
One major complication of uncontrolled HIV infection is HIV-associated encephalitis (HIVE), a neuropathological correlate of HAD. HIVE is strongly associated with reduced brain volume (as measured by MRI) and chronic immune activation and inflammation. Specifically individuals with HIVE express a higher percentage of CD163+CD14+CD16+ perivascular macrophages in the brain (Fischer-Smith et al. 2001; Kim et al. 2006); an expansion of ‘inflammatory’ CD16+-expressing monocytes in the periphery (Ancuta et al. 2008); and multinucleated giant cells, comprising aggregated microglia and macrophage cells (Brew et al. 1995; Takahashi et al. 1996). Furthermore, individuals with HIVE have widespread dysregulation of genes involved in synapto-dendritic functioning and integrity, toll-like receptors, interferon responses, mitochondrial genes, synaptic transmission and cell-to-cell signalling (Masliah et al. 2004; Gelman et al. 2012). Recent evidence also suggests that microglia in individuals with HIVE are also dysfunctional, with lower gene expression levels of functional markers (Ginsberg et al. 2018). Thus, HIVE is strongly associated with advanced neurocognitive impairment such as HAD.
Finally, neurotropic HIV variants, geno- and phenotypically distinct from peripheral viruses, exist in PLWH and may drive disease (Gorry et al. 2001, 2002; Haggerty and Stevenson 1991). These variants are detectable at different stages of infection and induce inflammatory responses such as increased neopterin and pleocytosis in CSF (Sturdevant et al. 2015; Hagberg et al. 2010), suggesting that a compartment of neurotropic/neurovirulent viral strains may play a more critical role in HAND than absolute viral load in the CNS.
4.2 HAND Pathophysiology Following Viral Suppression with ART
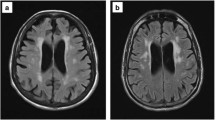
The persistence of HAND despite viral suppression with ART indicates an underlying pathology in the CNS. However, the exact pathophysiology of disease is unclear mainly due to the inability to perform biopsy analysis of the CNS from individuals who are virally suppressed with ART and limited numbers of autopsy samples from such patients. Therefore, most evidence of ongoing pathology in virally suppressed individuals is based on peripheral indicators of CNS disease or MRI/PET scans. Individuals with HAND have heightened indicators of persistent neuronal injury (as measured by cerebral metabolites) (Young et al. 2014), degradation of cortical grey matter, BBB dysfunction (Chaganti et al. 2019), microglial activation (Rubin et al. 2018; Garvey et al. 2014) and a continued reduction of brain volume despite therapy (Cardenas et al. 2009; Küper et al. 2011). Indicators of axonal damage such as CSF neurofilament light chain are also elevated in virologically suppressed PLWH (Jessen Krut et al. 2014) and are associated with cognitive decline (Sun et al. 2017; Sailasuta et al. 2016). Notably, osteopontin, a pro-inflammatory bone-matrix protein, is also found in high levels in virally suppressed individuals with HAND (Brown et al. 2011; Yu et al. 2017; Vera et al. 2016). These biomarkers of disease, discussed further below, are indicative of chronic neuroinflammation and neurodegeneration despite ART (Figure 1).
Virally suppressed individuals also show peripheral indicators of chronic cellular activation and dysfunction that may indicate/contribute to neuropathology. Individuals with HAND have a higher number of activated macrophages/microglia in the CNS relative to neurologically unimpaired individuals (Tavazzi et al. 2014). Plasma levels of MCP-1 and CXCL-10, produced by activated macrophages and monocytes, are associated with neuronal injury and higher inflammation in virally suppressed individuals with HAND (Letendre et al. 2011). Levels of quinolinic acid, a product of tryptophan metabolism, are also elevated in virally suppressed PLWH and are directly associated with levels of pTau that are predictive of neurocognitive impairment in this population (Anderson et al. 2018). Some evidence suggests that the perivascular macrophage phenotype may be predisposed by the precursor monocyte phenotype as monocyte activation (as measured by CSF sCD14) remains elevated in virologically suppressed individuals with HAND (Eden et al. 2007; Spudich et al. 2011; Yilmaz et al. 2013) and is associated with significantly worse neurological outcomes for those on non-suppressive ART (Kamat et al. 2012). Furthermore, PBMCs from individuals with HAD or MND express higher levels of pro-inflammatory cytokine genes (such as TNF, IL-6, IL-27) and lower levels of associated miRNAs (miR-124-3p, miR-210) than PLWH who were neurologically unimpaired (Venkatachari et al. 2017).
HIV-associated astrocyte dysfunction – CNS cells that normally help to maintain cerebral immunity and homeostasis – has been associated with HAND. Specifically, astrocyte dysfunction results in improper buffering of glutamate, dysregulation of BBB permeability, and release of pro-inflammatory cytokines (such as TNFα). Moreover, because astrocytes are susceptible to HIV infection, they may serve as a viral reservoir. We have further shown that astrocytes are less responsive to some antiretroviral drugs (Gray et al. 2013), thus potentially contributing to continued viral presence in the CNS.
5 Mechanisms Driving HAND in Virally Suppressed Patients
It is well accepted that HIV viremia is not the sole driver of neurocognitive impairment as incidence of HAND continues to affect between 18 and 69% of people living with HIV despite viral suppression with ART. Therefore, other factors such as persistent viral transcription in CNS reservoirs and/or chronic peripheral inflammation outside of the CNS play pertinent roles in determining the HAND status of virally suppressed individuals. These mechanisms will be discussed below.
5.1 HIV Viral Presence/Replication in the CNS
HIV is considered to persist in latent reservoirs in the CNS such as macrophages and astrocytes (Thompson et al. 2011) and is controversially thought to directly contribute to HAND pathogenesis (Churchill et al. 2015). HIV RNA (Dahl et al. 2014) and anti-HIV antibodies (Burbelo et al. 2018) are detectable in the CSF after 10 years of ART, potentially indicating viral persistence and ongoing replication in the CNS. Notably, increasing ratios of ‘HIV RNA in CSF’-to-‘HIV RNA in plasma’ are associated with worsening neurological outcomes in virologically suppressed PLWH (Anderson et al. 2017; Canestri et al. 2010) and elevated neopterin levels (Dahl et al. 2014), indicating that localised replication in the CNS may contribute to neuroinflammation and disease progression. A recent longitudinal study identified CNS escape in 6% of cases (6/101 individuals) in the absence of peripheral viremia following 3 years of ART (Joseph et al. 2019). Further genotypic analysis suggests that the virus was derived from persistent CNS replication, likely from macrophage/microglia, linked to emtricitabine resistance and low nadir CD4 count (10 copies/mm3). Interestingly, we have shown that some CNS-derived viruses have impaired transcriptional activity due to polymorphisms in the transcription factor Sp1 (Gray et al. 2016). Thus, whether virus in the CSF truly represents active replication in the CNS of virologically suppressed individuals remains unclear, possibly confounded by poor suppression in the periphery associated with a blip in plasma HIV levels (Eden et al. 2016). HIV resistance to lamivudine and emtricitabine (Mukerji et al. 2017) and also treatment with protease inhibitor + NRTI regimens (Mukerji et al. 2018) are also associated with CSF viral escape. Finally in vivo mouse studies have shown that chronic low levels of neurotoxic tat, a step in the HIV life cycle not affected by current ART, can cause astrocyte activation (Dickens et al. 2017) which may contribute to HAND pathogenesis as tat has been found in both CNS tissue and the CSF of virally suppressed individuals (Johnson et al. 2013). Thus, further studies are required to establish the role of active replication and/or viral persistence in the CNS in HAND associated pathology.
Whilst active replication is an important focus of current research in defining the CNS as a reservoir of HIV, persistence of non-replication competent virus in the CNS is also detrimental to the patient. Studies in the periphery have identified that the bulk (~93%) of the HIV reservoir in T cells consists of non-replication competent viruses harbouring hyper-deletions that may generate short abortive transcripts or viral proteins that are immunogenic (Bruner et al. 2016). As such, generation of highly neurotoxic HIV nef and tat in the CNS by persistent non-productive infection in cells such as astrocytes may drive neuroinflammation, cellular dysfunction and neuronal degradation (as discussed above). Thus, persistent non-replication competent virus in the CNS may play as important a role in HAND pathogenesis as active viral replication and must be considered in appropriate therapeutic strategies.
5.2 Host Cell and Epigenetic Factors
Host cell and environmental factors induced by microRNAs (miRNA) – short non-coding repressors of transcription – and DNA methylation have been identified to be associated with HAND pathogenesis (Tatro et al. 2010), suggesting a role for epigenetic changes to components of the immune system in driving HAND. Large genomic studies have found strong associations between dysregulated miRNAs and mRNA in the brains of individuals with HAD in comparison to neurocognitively unimpaired individuals (Zhou et al. 2012). Specifically, miR-21, known to repress transcription factors involved in neuronal functioning, is present in high levels in the CNS of PLWH with HAD (Yelamanchili et al. 2010). Furthermore, both miR-128a (Eletto et al. 2008) and miR-34a (Mukerjee et al. 2011) are upregulated by HIV Tat or Vpr, respectively, resulting in adverse effects on neuronal function in vitro. HIV Tat also influences histone acetylation/deacetylation via chromatin structure remodelling by histone deacetylases in neuronal cells in vitro, resulting in synaptic plasticity and neuronal dysfunction (Saiyed et al. 2011). Epigenetic changes derived by alterations in DNA methylation sites in monocytes are also strongly associated with worse neurocognitive scores (Corley et al. 2016), implying that epigenetic changes in peripheral cells transmigrating to the CNS may also influence HAND.
5.3 Chronic Peripheral Inflammation
Chronic immune activation and inflammation is a hallmark of HIV infection despite viral suppression, and measures of inflammation/immune activation are reliable indicators of HIV disease progression and have been linked with HAND pathogenesis (Hazenberg et al. 2003; Somsouk et al. 2015; Kuller et al. 2008; Boulware et al. 2011; Hunt et al. 2011; Pandrea et al. 2012). The causes of persistent immune activation in chronic HIV infection are multifactorial, but the host response to translocated microbial products from the gastrointestinal (GI) tract, resulting from the depletion of gut-associated lymphoid tissue CD4+ T cells during acute infection, is thought to be a major contributor (Brenchley et al. 2004, 2006; Estes et al. 2010). This is exemplified in elegant in vivo studies where experimental damage of the GI tract of African green monkeys (AGMs), a natural host of SIV that does not develop AIDS, induces local and systemic inflammation similar to that of HIV infection in humans (Hao et al. 2015). Specifically, bacterial lipopolysaccharide (LPS) – a cell wall component of gram-negative bacteria and potent immune activator – remains elevated in HIV/SIV infection despite ART and is thought to drive chronic inflammation (Deeks et al. 2004). Progression to AIDS in PLWH may be driven (in part) in response to LPS as sooty mangabeys, natural hosts of SIV that do not develop AIDS, have recently been shown to have a C-terminal frameshift in the LPS receptor (TLR-4) which renders it non-functional (Palesch et al. 2018).
Measures of microbial translocation, especially measures of monocyte activation following exposure to LPS such as sCD14 and sCD163, have been linked with neurocognitive impairment, indicating a central role for monocyte activation in neuropathology (Vassallo et al. 2013). Notably, elevated levels of circulating CD16+ monocytes, CD14+ monocyte HIV DNA content, sCD14 and sCD163 are associated with microbial translocation and correlate with an increased risk of neurocognitive impairment (Valcour et al. 2013). sCD14 levels in CSF are also associated with NFL, indicative of axonal damage, in untreated PLWH (Jespersen et al. 2016). Moreover, plasma LPS levels are higher in HIV-HCV co-infected individuals with HAND, relative to HIV-HCV co-infected neurologically unimpaired individuals (Vassallo et al. 2013). GI tract damage in PLWH is also associated with more pathogenic microbial populations, compared to uninfected individuals (Mutlu et al. 2014). Notably, similar alterations in the gut microbiome have been linked to other CNS disorders, namely, multiple sclerosis (Glenn and Mowry 2016) and Parkinson’s disease (Houser and Tansey 2017). Whilst it follows that, within PLWH, changes in the gut microbiome and the resultant inflammatory response may contribute to HAND, studies are required to test this hypothesis.
5.4 ART Neurotoxicity
Whilst current antiretrovirals are less neurotoxic than earlier iterations, ART neurotoxicity continues to be linked to HAND pathogenesis, and many ARVs may have lasting adverse ‘legacy’ effects that may contribute to disease decades after use (Jonathan et al. 2015). Efavirenz, a commonly prescribed non-nucleoside reverse-transcriptase inhibitor, is still in use despite known neurological side effects such as psychiatric episodes and neurocognitive effects on information processing and executive functioning (Ma et al. 2016). The underlying pathology of efavirenz is most likely due to either the induction of pro-inflammatory cytokines or mitochondrial toxicity (Funes et al. 2015) and endoplasmic reticulum stress (Funes et al. 2014; Bertrand and Toborek 2015). Treatment of neuronal cell lines with 15 different ARVs at physiological concentrations identified modest neuronal toxicity in vitro (Robertson et al. 2012). In vitro raltegravir has also been linked with enhanced production of macrophage-derived IL-8 (Tatro et al. 2014).
Protease inhibitors also have a higher risk of drug-drug interactions by metabolism via CYP450 enzymes and have also been linked to neurotoxicity. Treatment of human astrocytes with the protease inhibitors amprenavir and lopinavir induced dysregulation of glutamate transport in vitro and was associated with worse neurocognitive performance in mouse models (Vivithanaporn et al. 2016). In vitro ritonavir or lopinavir treatment also impaired oligodendrocyte maturation, and similar treatment in mice reduced myelin protein levels in the frontal cortex (Jensen et al. 2015). Importantly Jensen and colleagues further showed that levels of myelin basic protein in the frontal cortex of PLWH were lower than those present from untreated PLWH or HIV-uninfected patients. Finally, recent evidence has found that individuals treated with integrase stand transfer inhibitors (INSTIs) such as dolutegravir are associated with poorer neurocognitive performance and reduced brain volume than those on non-INSTI containing regimens (O’Halloran et al. 2019). As many patients transition to regimens including INSTIs, the long-term neurocognitive effects of these drugs need to be closely monitored. Thus, there remains a clinical demand for highly effective and non-neurotoxic antiretrovirals as well as improved treatment strategies to treat HAND.
6 Biomarkers of CNS Infection and HAND
Identifying biomarkers of cognitive impairment, and more specifically HAND, is a major research focus due to the clinical demand for reliable means to (1) predict HAND before it occurs, (2) diagnose HAND, (3) distinguish the early stages of HAND (ANI and MND) and (4) predict and monitor changes in cognition for individuals with HAND. Biomarkers must be readily accessible, cheap and reliable, and as such most emphasis has been placed on indicators of neuroinflammation or neuronal damage in the blood and CSF. Identifying biomarkers of HAND has proven to be a difficult task as well-established plasma and CSF biomarkers of inflammation (such as sCD14, osteopontin (Brown et al. 2011), TNFα, IFNγ, sCD14, IL-1β, IL-6, S100β, TGF-β levels) or HIV viremia (such as the surrogate marker nadir CD4+ T cell count) that are predictive of HAND in viremic or ART-naïve PLWH (Abassi et al. 2017; Lyons et al. 2011) are not predictive of HAND in virologically suppressed individuals receiving ART (Kamat et al. 2012; Lyons et al. 2011). Biomarkers of HAND may be indicative of neuronal damage, altered metabolism, generally neuroinflammation or even HIV itself. Specific biomarkers of HAND and their related pathological implications are discussed in detail below (Fig. 1).
6.1 Measures of HIV Viremia and Viral Latency
Although viral suppression with ART has reduced the predictive value of many traditional HIV-related biomarkers of HAND such as CSF HIV RNA (Ellis et al. 2002; Brew et al. 1997), some measures of HIV remain indicative of HAND despite therapy with ART. Low CD4+ T cell counts continue to be associated with HAND, albeit mainly in individuals failing therapy or with moderate immune suppression (CD4+ T cell count 200–349 cells/mm3) (Bhaskaran et al. 2008). CD4+ T cell nadir may offer some prognostic value (Ellis et al. 2011). However, a recent study found that immediate therapy initiation with a CD4 nadir >500 cells/mm3 had no neurocognitive benefit over delayed treatment initiation (Wright et al. 2018), questioning the predictive value of CD4 nadir at high CD4 T cell counts. Similarly, CSF and/or plasma levels of HIV RNA are also indicative of neurocognitive decline in individuals who exhibit therapy failure or drug resistance (Canestri et al. 2010; Peluso et al. 2012; Bingham et al. 2011).
Additionally, biomarkers of persistent viral replication/presence in the CNS are gaining attention as possible prognostic markers of disease. HIV DNA persists in the CNS despite viral suppression and studies using research tools including PCR and the in situ hybridisation technique DNAscope have offered insight into HIV persistence in the CNS (Churchill et al. 2009; Ko et al. 2019; Lamers et al. 2016; Estes et al. 2017). However, its application as a true diagnostic/prognostic biomarker is limited as these assays generally investigate autopsy brain tissue. Therefore, HIV DNA content in peripheral cells such as T cells and monocytes may be a more practical approach to assessing the CNS reservoir. HIV DNA in peripheral blood monocytes (Valcour et al. 2013; Cysique et al. 2015a) and CSF cells (Oliveira et al. 2017; Shaunak et al. 1990) is associated with risk of HAND and brain atrophy in non-suppressed individuals (Kallianpur et al. 2014) and recent evidence supports that this may also be true in suppressed patients. In a recent study of 69 people living with HIV who were virally suppressed for a median of 8.6 years with ART, Spudich and colleagues found that ~50% of individuals harboured cell-associated HIV DNA in the CSF (Spudich et al. 2019). Furthermore, cell-associated HIV DNA was associated with adverse neurocognitive outcomes, suggesting that persistent HIV in the CSF despite ART may contribute to HAND pathogenesis. BCL11B, an inhibitor of viral transcription, is upregulated in latently infected cells of the CNS (Desplats et al. 2013), and higher CSF levels are associated with lower creatine levels in frontal white matter (Cysique et al. 2019), potentially validating BCL11B as an indicator of latent HIV-related pathology. However, the associations of CSF BCL11B and HAND remain to be defined. CSF escape is also associated with higher neopterin levels (Eden et al. 2016), although as this is a rare phenomenon and neopterin is produced by multiple cells types during cellular activation, this may not be the most robust method of confirming latency. A recent study also found that HIV gp120 protein sequences are predictive of HAD and/or HIVE in silico (Ogishi and Yotsuyanagi 2018), highlighting the possibility of HIV quasi-species as a predictive tool for HAND. However, the methodology required to characterise sequences from isolated immune cells is more challenging than standard biochemical assays which may limit its practical application as a biomarker.
6.2 Neuronal Damage
NFL, a component of myelinated axons, is readily detected in the CSF of neurodegenerative diseases and is indicative of neuronal axon damage. Multiple studies have found that CSF levels of NFL are present at higher levels in untreated individuals with or without neurocognitive impairment and CSF NFL levels in individuals with HAD are significantly higher than those in more mild disease (McGuire et al. 2015; Gisslén et al. 2007, 2015; Peterson et al. 2014). Moreover, NFL is associated with worse CD4 T cell counts and is positively associated with plasma viral load, suggesting that it is indicative of HIV-directed neuropathology. Correlative analysis in individuals with primary infection further shows associations between higher NFL levels in CSF and neuroinflammatory markers (CXCL-10, neopterin) and adverse levels of CNS metabolites (Peluso et al. 2013). NFL has also been shown to be a more sensitive neuronal marker than total and phosphorylated tau and amyloid precursor proteins (Peterson et al. 2014). Furthermore, CSF NFL levels correlate with plasma NFL levels, a significant advantage due to ease of blood draw vs lumbar puncture required for CSF analyses. Therapy reduces NFL levels; however, they remain elevated in comparison to HIV-uninfected controls (Jessen Krut et al. 2014). However, abnormal NFL levels have only been detected in ~16% of virally suppressed subjects, questioning whether this is sensitive enough to detect ANI or MND (Peterson et al. 2014).
Exosomes are gaining attention as biomarkers of neuroinflammation and neurocognitive disorders including AD and HAND (Pulliam et al. 2019). Exosomes are 30–150 nm vesicles containing host cell proteins and DNA that are released following cellular activation into plasma. As plasma exosomes harbour protein and RNA from their host cell such as neurons, they potentially offer a method of interrogating cell-specific pathology from different, difficult-to-access sites such as the brain. Studies in AD have identified the presence of neuronally derived exosomes (NDE) from patients with preclinical AD that predicted AD 10 years prior to onset (Fiandaca et al. 2015). More recently, NDEs have been detected in the plasma of PLWH with cognitive impairment (Sun et al. 2017) and are indicative of neuronal health. Sun and colleagues identified that neurocognitively impaired individuals had fewer NDEs than non-neurocognitively impaired individuals, possibly due to neuronal stress or death. Furthermore, NDEs from these individuals contained higher levels of proteins associated with neuronal damage such as high motility group box 1 (HMGB1), NFL and amyloid β than exosomes from HIV-infected neurocognitively unimpaired individuals (Sun et al. 2017). Thus, exosomes, particularly NDEs, may offer some prognostic benefit over other inflammatory biomarkers that are not truly specific to the CNS.
Mitochondrial DNA (mtDNA) is indicative of the energy levels/demands of a cell. Each cell contains mitochondria with a number of copies of mtDNA; thus mtDNA copy number may be indicative of cellular dysfunction and apoptosis. mtDNA damage is present in approximately 45% of total cells in the frontal cortex of patients with HAND without viral suppression (Zhang et al. 2012). Furthermore, individuals with HAND in this cohort had less mtDNA than those who were not cognitively impaired. Similarly, mtDNA damage can be found in the periphery. Following viral suppression, mtDNA copy number from peripheral blood is associated with worse cognitive performance in CHARTER patients (Hulgan et al. 2018). Furthermore, CSF levels are higher in MND patients in comparison to neurocognitively normal individuals (Mehta et al. 2017); however, no difference was observed in ANI patients – this may just be a reflection of the insensitivity of the CSF as a marker of mild events in a discreet part of the frontal lobe.
6.3 Cellular Activation
Monocytes, and markers of monocyte of activation, are readily measurable indicators of HAND due to their key role in pathogenesis. CCR2 expression on CD14+CD16+ monocytes is negatively associated with neurometabolite levels, and by extension pathology, as measured by MRS imaging (Veenstra et al. 2019). CCR2 expression on CD14+CD16+ monocytes is also associated with HIV DNA copies per 106 PBMCs (Veenstra et al. 2019). CCR2’s ligand, CCL2, is a chemokine that acts to recruit monocytes into the brain. In individuals with the CCL2-2578G, CSF levels of CCL2 are higher than in non-carriers, and higher levels are associated with poor cognitive impairment, albeit mainly in individuals with high plasma viral (Thames et al. 2015). Plasma CCL2 levels are also elevated in individuals with either HAD or minor cognitive motor disorder (precursor to MND) in viremic individuals (Ancuta et al. 2008). However, it is of note that levels are similarly elevated in individuals with non-HIV-related neurocognitive impairments and no difference in ANI patients, and neurocognitively normal individuals were observed in this study.
Soluble indicators of monocyte activation have also been linked to HAND. LPS activates monocytes via TLR-4 as described above, and plasma levels are associated with HAD in individuals with AIDS (Ancuta et al. 2008). LPS levels are known to remain elevated following viral suppression; however, to date no evidence links plasma LPS levels with HAND in the absence of co-infection such as HCV. Nonetheless, following monocyte activation by immunogens such as LPS, monocytes shed CD14, the co-receptor for LPS, which can be measured and has been associated with worse global deficit scores, lower CD4 T cell counts and worse learning, attention and motor T scores in a cohort of generally unsuppressed individuals (Lyons et al. 2011). The reliability and sensitivity of sCD14 to identify HAND in virally suppressed individuals is less clear. Similarly, soluble CD163 – a scavenger receptor – is shed from activated macrophage/microglia and detectable in both plasma and CSF. sCD163 levels are associated with adverse neurocognitive scores (Burdo et al. 2013b; Royal et al. 2016).
Neopterin, a pteridine produced by activated macrophages and monocytes, is commonly found in higher levels in the plasma and CSF of PLWH, despite viral suppression. Neopterin levels have been shown to predict HAND and are associated with HAND severity in therapy-naïve individuals (Brew et al. 1990, 1996); however, there is limited evidence supporting the prognostic value of neopterin in virally suppressed individuals. Plasma levels, but not cellular gene expression in monocytes (Quach et al. 2018), of CCL2, HMGB1, IL-8, CXCL-10 and neopterin are predictive of HAND in virally suppressed individuals (Sun et al. 2017; Eden et al. 2016; Yuan et al. 2013). CSF fractalkine levels are higher in individuals with MND/HAD than ANI (Letendre et al. 2011). CSF levels of HMGB1, produced by activated macrophages and astrocytes, may also be predictive of HAND, even very minor disease, in virally suppressed PLWH (Gougeon et al. 2017).
Whilst many peripheral biomarkers of monocyte/macrophage activation are associated with adverse neurocognitive outcomes (as discussed above), individual biomarkers (such as sCD14, MCP-1, CXCL-10, etc.) are associated with unique neuropathology and inflammation at different locations in the brain (such as frontal white matter, basal ganglia, grey matter). For example, MRS studies assessing levels of neurometabolites in the CNS of virally suppressed individuals found that CSF levels of sCD14 were negatively associated with Cho/Cr ratios in frontal white matter (Anderson et al. 2015), indicative of monocyte-induced neuronal damage. However, MCP-1 levels, indicative of monocyte recruitment, were positively associated with Cho/Cr ratios in the basal ganglia (Anderson et al. 2015), supporting findings from similar studies (Harezlak et al. 2011). Thus, it is important to acknowledge that each biomarker of myeloid activation may be indicative of different stages and/or sites of neurocognitive diseases which must be considered when interpreting results.
S100β is a calcium binding protein mainly expressed on glial cells such as astrocytes and thus is useful as a biomarker of astrocyte activation. S100β levels in the CSF have been associated with cognitive impairment in PLWH and were higher in those with more severe AIDS dementia complex (precursor terminology to HAND) or progressed to more advanced disease more quickly (Pemberton and Brew 2001). S100β levels are also inversely associated with executive function including the rapid generation of verbs testing ‘action fluency’ (Woods et al. 2010).
Finally, measures of T cell activation are also altered with symptomatic HAND (HAD and MND) exhibiting different T-cell immune activation profiles to those with ANI (Vassallo et al. 2015) (diagnosis of MND was associated with a CD4:CD8 ratio <1), suggesting the pathophysiological mechanism underlying symptomatic- and asymptomatic-HAND is different or the difference could reflect a longer time with symptomatic disease given that ANI leads to MND. T-cell phenotype/function and HIV itself are also indicative of neurocognitive impairment. The percentages of IFN-γ producing CD8+ T-cells in the CSF are directly associated with the severity of neurocognitive decline as measured by global deficit scores in virally supressed PLWH (Schrier et al. 2015). However, whether these observations are indicative or causative in disease pathogenesis is unknown.
6.4 Metabolic Dysfunction
PLWH with neurocognitive impairment experience dysregulated kynurenine pathways of tryptophan catabolism, skewing to the production of neurotoxic metabolites. As such CSF levels of quinolinic acid/tryptophan ratios are indicative of CNS neurocognitive impairment in SIV-infected macaques, particularly early in infection (Drewes et al. 2015; Heyes et al. 1990). Furthermore, a recent study showed that virally suppressed individuals had higher CSF levels of quinolinic acid and kynurenine/tryptophan ratios than HIV-uninfected controls (Anderson et al. 2018). Similarly, HAND has been associated with lipid dysfunction and cholesterol accumulation in the brain (Mielke et al. 2010). In a large multi-centre study, HIV-infected virally suppressed individuals had altered levels of cholesterol species in the CSF; namely, an increase in the ceramide species C24:1 that was associated was higher likelihood of neurocognitive decline (Bandaru et al. 2013). Furthermore, a shift in lipid species was associated with progressive disease.
6.5 Novel Non-traditional Biomarkers
Progranulin is produced by microglia and neurons and is thought to have neuroprotective effects by modulating neuroinflammation whilst also acting as a neuronal growth factor. Progranulin also has known anti-viral effects that inhibit HIV replication, and its production by microglia is upregulated during active HIV infection (Suh et al. 2014a). However, during viral suppression with ART, lower levels of progranulin in the CSF are present and are associated with worse cognitive impairment and elevated levels of other pro-inflammatory biomarkers (Suh et al. 2014b). This may be because downregulation of the production of neuroprotective progranulin by microglia may leave neurons more susceptible to damage (Suh et al. 2014a). Thus, low progranulin levels in the CSF may offer insight into underlying CNS neuronal damage and HAND pathogenesis.
Total tau (t-tau) and phosphorylated tau (p-tau) levels in the CSF are commonly used as an indicator of Alzheimer’s disease; however, levels have also been assessed in the context of HAND. We and others have found that CSF levels of p-tau (as well as total-tau levels) are higher in individuals with AIDS dementia complex and HAND than those who are uninfected (Brew et al. 2005; Cysique et al. 2015b), which is in line with more recent reports where p-tau levels in CSF were inversely associated with scores of prospective memory in PLWH (Anderson et al. 2018). However, others have found a difference in only CSF levels of t-tau, but not p-tau (Krut et al. 2017; Steinbrink et al. 2013) in comparison to the HIV-uninfected population, possibly suggesting that patient viral load and/or ongoing neuronal damage at the time of sampling may influence these associations.
MicroRNAs are non-coding molecules that regulate both viral and host gene expression by binding and repressing RNA and can be detected in PBMCs, plasma and CSF. A small cross-sectional study found that HIVE patients express altered CSF levels of 11 different miRNAs in comparison to subjects without HIVE (Pacifici et al. 2013), with miR-937 being highly upregulated in the CSF. Furthermore, levels of miRNAs in plasma are different between individuals with or with HAND (Kadri et al. 2016; Asahchop et al. 2016) making miRNAs a potentially useful biomarker of disease. The Veterans Aging Cohort Study (VACS) index, consisting of traditional HIV biomarkers of disease and non-traditional biomarkers of comorbidity, is also predictive of neurological decline (Marquine et al. 2016).
6.6 Limitations of Biomarkers and Current Challenges
Whilst the aforementioned biomarkers are indicative of cognitive decline in PLWH, no clinically validated biomarker can reliably differentiate the stages of HAND, especially ANI. This may be because many are broad inflammatory components that are not uniquely specific to the brain, or HIV infection, and thus they may be influenced by inflammation from other sites or other diseases/disorders or even age. Furthermore, it is likely that ‘waves’ of neuroinflammation may take place during disease pathogenesis, confounding the accuracy and specificity of biomarkers with HAND. This is evidenced by diffusion tensor imaging assessing white matter damage where reductions in white matter in chronic infection were associated with markers of inflammation (Wright et al. 2015), whilst changes in white matter in primary infection were associated with breakdown of the BBB, thus, representing a change in neuropathogenesis and neuroinflammation with disease progression. Therefore, different biomarkers of disease may be representative of stages of neuropathogenesis that are not strictly related to Frascati Criteria stages of disease. In summary, whilst much work has been conducted evaluating biomarkers of HAND, a need remains for cheap, accessible, and highly accurate biomarkers that accurately diagnoses, distinguishes and compares distinct forms of HAND. Combinations of biomarkers are more likely to be more predictive or diagnostic of disease.
7 Biomarkers of Neurocognitive Decline as Indicators of ART Success
Due to effective ART regimens suppressing HIV viremia to undetectable levels in CSF/plasma, biomarkers of HIV disease such as CSF HIV RNA offer little insight into underlying pathology and neurocognitive disease in virally suppressed individuals. Therefore, biomarkers of underlying neuropathology or cellular activation such as those described above provide critical information regarding the success of novel treatment strategies that complement traditional indicators of HIV viremia.
Intensification of ART to treat CNS infection has been evaluated with some success. Intensive therapy with maraviroc, a CCR5 inhibitor, for 24–52 weeks in combination with standard ART reduced the proportion of CD16+ monocytes harbouring HIV DNA and was associated with better neuropsychological performance in the majority of patients (Ndhlovu et al. 2014; Gates et al. 2016). Early initiation of ART (i.e. <30 days postinfection) also has elicited some neuroprotective effects in both small cross-sectional (Evering et al. 2016) and short-term longitudinal studies (Hellmuth et al. 2016). Furthermore, early initiation also reduced the diversity of HIV DNA in PBMCs, cells isolated from CSF and levels of pro-inflammatory cytokine (IL-6 and TNF) in the CSF, compared to delayed ART initiatives (>14 months post-exposure) (Oliveira et al. 2017). However, the lack of large long-term longitudinal studies limits our understanding of the efficacy of such treatment regimens.
Targeting neuroinflammation using adjunctive therapy in concert with ART also may have beneficial effects. However, to date all attempts to reduce the risk of HAND by targeting neuroinflammation in HIV infection have been unsuccessful (Meulendyke et al. 2014; Sacktor et al. 2011, 2014, 2018; Schifitto et al. 2007). Treatment with the anti-oxidant minocycline reduced CSF levels of some oxidative stress markers in comparison to placebo (Sacktor et al. 2014), but did not improve neurocognitive impairment over 24 weeks (Sacktor et al. 2011). Similarly treatment with selegiline, a MAO-B inhibitor and anti-oxidant, had no neurocognitive or functional benefit in PLWH with mild to moderate neurological impairment (Schifitto et al. 2007). Although treatment with a combination of paroxetine and fluconazole reduced CSF neurofilament light chain and amyloid precursor protein levels in SIV-infected RMs (Meulendyke et al. 2014), a recent double-blind placebo-controlled study using this regimen showed neurocognitive improvement in some, but not all, domains (Sacktor et al. 2018), highlighting that further validation is required. Interestingly, these drugs target HIV gp120 and tat-related neurotoxicity and did not show any improvement in neuroinflammatory markers in plasma or CNS (Meulendyke et al. 2014), suggesting that peripheral inflammation may be more important in human HAND. However, in other studies, drugs specifically targeting extracellular Tat have been shown to counteract its production of IL-1β and TNF in glial cell lines in vitro (Mediouni et al. 2015), and several novel Tat/TAR (and Tat/cyclin T1/CDk9) small molecule inhibitors have been described to date (Serena et al. 2013). These initiatives are important as current therapies do not stop tat secretion from CNS cells (Sonia et al. 2012).
Therapies directed against metabolic dysfunction in the CNS such as intranasal insulin have also been shown to improve neurobehavioural performance in animal models and are currently guiding clinical studies in humans. Specifically, cats who were infected with feline immunodeficiency virus and treated with 20 IU of intranasal insulin for 6 weeks had reduced markers of glial activation and neuroinflammation and improved neurobehavioural performance than placebo controls (Mamik et al. 2016). Furthermore, intranasal insulin treatment of chimeric EcoHIV-infected mice, who exhibit neurocognitive impairment similar to HAND, was found to transiently reverse hippocampal dendritic injury and improve learning and retention ability in some animals; however, this only occurred in the presence of the drug (Kim et al. 2019). These findings support other studies testing intranasal insulin in neurocognitive disorders such as Alzheimer’s disease and have led to Phase I/II clinical trials (NCT03277222, NCT03081117) that are underway testing the effects of intranasal insulin treatment in combination with ART with findings expected in 2020–2021.
Finally, targeting peripheral inflammation is also a possible adjunctive therapy to ART in both HAND and other HIV-associated comorbidities. Targeting monocyte activation using atorvastatin and simvastatin treatment, generally used for treating hyperlipidaemia, reduced the number of circulating CD16+ monocytes (Yadav et al. 2016) and treatment with the dual CCR2 and CCR5 antagonist cenicriviroc; thus migration of CD14+CD16+ monocytes improved neurocognitive performance following 24 weeks of treatment (D’Antoni et al. 2018). Recent in vitro evidence also suggests that treatment with buprenorphine, an opioid derivate used as a replacement for heroin in addicts, may have anti-inflammatory properties by binding monocytes and reducing monocyte transmigration across a BBB model (Jaureguiberry-Bravo et al. 2018). Whilst this treatment may be beneficial in injecting drug using PLWH, its efficacy and safety needs to be confirmed in vivo in non-heroin addicts. Thus, targeting cellular inflammation and immune activation in the periphery may be a viable treatment strategy with beneficial effects across multiple HIV-associated co-morbidities.
8 Where to from Here?
HAND remains a significant burden affecting PLWH globally; however, due to the relatively specialised nature of neurocognitive testing required to diagnose HAND, especially ANI, people living with HIV and neurocognitive impairment are either being misdiagnosed or missed completely. The limited ability to accurately diagnose mild HAND coupled with a change in the HIV epidemic to a chronic inflammatory disease whereby individuals are advancing to older age with an elevated risk of age-related comorbidities represents a difficult problem. Thus, early and accurate diagnoses of HAND are essential in improving health outcomes.
Significant steps forward in understanding the neuropathology of HAND have provided some clues into possible biomarkers for diagnosis and prognosis. Continuous viral presence in the CNS, chronic peripheral immune activation and inflammation as well as underlying drug toxicity and cellular dysfunction all pose viable mechanisms driving neurological diseases in PLWH. However, the discrete effects of each remain unclear. It is likely that a fine balance exists, whereby chronic systemic inflammation, which persists despite viral suppression, may amplify virally induced disease to contribute to severe diseases outcomes such as HAD. This, however, complicates the clinical specificity of many biomarkers that are in effect broad indicators of inflammation such as sCD14 and sCD163. Thus, an added focus on biomarker research delineating underlying CNS pathology such as neuronally derived exosomes, NFL or even MRI of neuroinflammation may be more useful clinically. Furthermore, combining a number of biomarkers to form a ‘risk score’ or ‘index’ using an algorithmic approach may be more predictive than any one biomarker. Whilst significant advances have been made in identifying biomarkers of HAND, the need remains for truly specific, sensitive and reliable biomarkers to reduce the risk of misdiagnosis and delayed treatment and ultimately improve health outcomes in people living with HIV.
References
Abassi M, Morawski BM, Nakigozi G, Nakasujja N, Kong X, Meya DB et al (2017) Cerebrospinal fluid biomarkers and HIV-associated neurocognitive disorders in HIV-infected individuals in Rakai, Uganda. J Neurovirol 23(3):369–375
Ances BM, Vaida F, Yeh MJ, Liang CL, Buxton RB, Letendre S et al (2010) HIV and aging independently affect brain function as measured by functional magnetic resonance imaging. J Infect Dis 201(3):336–340
Ancuta P, Kamat A, Kunstman KJ, Kim E-Y, Autissier P, Wurcel A et al (2008) Microbial translocation is associated with increased monocyte activation and dementia in AIDS patients. PLoS One 3(6):e2516
Anderson AM, Fennema-Notestine C, Umlauf A, Taylor MJ, Clifford DB, Marra CM et al (2015) CSF biomarkers of monocyte activation and chemotaxis correlate with magnetic resonance spectroscopy metabolites during chronic HIV disease. J Neurovirol 21(5):559–567
Anderson AM, Muñoz-Moreno JA, McClernon D, Ellis RJ, Cookson D, Clifford DB et al (2017) Prevalence and correlates of persistent HIV-1 RNA in cerebrospinal fluid during antiretroviral therapy. J Infect Dis 215:105–113
Anderson AM, Croteau D, Ellis RJ, Rosario D, Potter M, Guillemin GJ et al (2018) HIV, prospective memory, and cerebrospinal fluid concentrations of quinolinic acid and phosphorylated Tau. J Neuroimmunol 319:13–18
Angelovich TA, Hearps AC, Maisa A, Martin GE, Lichtfuss GF, Cheng W-J et al (2015) Viremic and virologically suppressed HIV infection increases age-related changes to monocyte activation equivalent to 12 and 4 years of aging, respectively. J Acquir Immune Defic Syndr 69(1):11–17
Antinori A, Arendt G, Becker J, Brew B, Byrd D, Cherner M et al (2007) Updated research nosology for HIV-associated neurocognitive disorders. Neurology 69(18):1789–1799
Asahchop EL, Akinwumi SM, Branton WG, Fujiwara E, Gill MJ, Power C (2016) Plasma microRNA profiling predicts HIV-associated neurocognitive disorder. AIDS 30(13):2021–2031
Asher I, Guri KM, Elbirt D, Bezalel SR, Maldarelli F, Mor O et al (2016) Characteristics and outcome of patients diagnosed with HIV at older age. Medicine 95(1):e2327
Bagashev A, Sawaya BE (2013) Roles and functions of HIV-1 Tat protein in the CNS: an overview. Virol J 10:358
Bandaru VVR, Mielke MM, Sacktor N, McArthur JC, Grant I, Letendre S et al (2013) A lipid storage–like disorder contributes to cognitive decline in HIV-infected subjects. Neurology 81(17):1492–1499
Bertrand L, Toborek M (2015) Dysregulation of endoplasmic reticulum stress and autophagic responses by the antiretroviral drug efavirenz. Mol Pharmacol 88(2):304–315
Bhaskaran K, Mussini C, Antinori A, Walker AS, Dorrucci M, Sabin C et al (2008) Changes in the incidence and predictors of human immunodeficiency virus–associated dementia in the era of highly active antiretroviral therapy. Ann Neurol 63(2):213–221
Bingham R, Ahmed N, Rangi P, Johnson M, Tyrer M, Green J (2011) HIV encephalitis despite suppressed viraemia: a case of compartmentalized viral escape. Int J STD AIDS 22(10):608–609
Boban J, Kozic D, Turkulov V, Ostojic J, Semnic R, Lendak D et al (2017) HIV-associated neurodegeneration and neuroimmunity: multivoxel MR spectroscopy study in drug-naive and treated patients. Eur Radiol 27(10):4218–4236
Boulware DR, Hullsiek KH, Puronen CE, Rupert A, Baker JV, French MA et al (2011) Higher levels of CRP, D-dimer, IL-6, and hyaluronic acid before initiation of antiretroviral therapy (ART) are associated with increased risk of AIDS or death. J Infect Dis 203(11):1637–1646
Brenchley JM, Schacker TW, Ruff LE, Price DA, Taylor JH, Beilman GJ et al (2004) CD4+ T cell depletion during all stages of HIV disease occurs predominantly in the gastrointestinal tract. J Exp Med 200(6):749–759
Brenchley JM, Price DA, Schacker TW, Asher TE, Silvestri G, Rao S et al (2006) Microbial translocation is a cause of systemic immune activation in chronic HIV infection. Nat Med 12(12):1365–1371
Brew BJ, Bhalla RB, Paul M, Gallardo H, McArthur JC, Schwartz MK et al (1990) Cerebrospinal fluid neopterin in human immunodeficiency virus type 1 infection. Ann Neurol 28(4):556–560
Brew BJ, Rosenblum M, Cronin K, Price RW (1995) AIDS dementia complex and HIV-1 brain infection: clinical-virological correlations. Ann Neurol 38(4):563–570
Brew BJ, Dunbar N, Pemberton L, Kaldor J (1996) Predictive markers of AIDS dementia complex: CD4 cell count and cerebrospinal fluid concentrations of β2-microglobulin and neopterin. J Infect Dis 174(2):294–298
Brew BJ, Pemberton L, Cunningham P, Law MG (1997) Levels of human immunodeficiency virus type 1 RNA in cerebrospinal fluid correlate with AIDS dementia stage. J Infect Dis 175(4):963–966
Brew BJ, Pemberton L, Blennow K, Wallin A, Hagberg L (2005) CSF amyloid β42 and tau levels correlate with AIDS dementia complex. Neurology 65(9):1490–1492
Brown A, Islam T, Adams R, Nerle S, Kamara M, Eger C et al (2011) Osteopontin enhances HIV replication and is increased in the brain and cerebrospinal fluid of HIV-infected individuals. J Neurovirol 17(4):382–392
Bruner KM, Murray AJ, Pollack RA, Soliman MG, Laskey SB, Capoferri AA et al (2016) Defective proviruses rapidly accumulate during acute HIV-1 infection. Nat Med 22(9):1043–1049
Brunt SJ, Cysique LA, Lee S, Burrows S, Brew BJ, Price P (2016) Short communication: do cytomegalovirus antibody levels associate with age-related syndromes in HIV patients stable on antiretroviral therapy? AIDS Res Hum Retrovir 32(6):567–572
Burbelo PD, Price RW, Hagberg L, Hatano H, Spudich S, Deeks SG et al (2018) Anti-human immunodeficiency virus antibodies in the cerebrospinal fluid: evidence of early treatment impact on central nervous system reservoir? J Infect Dis 217(7):1024–1032
Burdo TH, Soulas C, Orzechowski K, Button J, Krishnan A, Sugimoto C et al (2010) Increased monocyte turnover from bone marrow correlates with severity of SIV encephalitis and CD163 levels in plasma. PLoS Pathog 6(4):e1000842
Burdo TH, Lackner A, Williams KC (2013a) Monocyte/macrophages and their role in HIV neuropathogenesis. Immunol Rev 254(1):102–113
Burdo TH, Weiffenbach A, Woods SP, Letendre S, Ellis RJ, Williams KC (2013b) Elevated sCD163 in plasma but not cerebrospinal fluid is a marker of neurocognitive impairment in HIV infection. AIDS (London, England) 27(9):1387–1395
Canestri A, Lescure F-X, Jaureguiberry S, Moulignier A, Amiel C, Marcelin A et al (2010) Discordance between cerebral spinal fluid and plasma HIV replication in patients with neurological symptoms who are receiving suppressive antiretroviral therapy. Clin Infect Dis 50(5):773–778
Cardenas VA, Meyerhoff DJ, Studholme C, Kornak J, Rothlind J, Lampiris H et al (2009) Evidence for ongoing brain injury in human immunodeficiency virus-positive patients treated with antiretroviral therapy. J Neurovirol 15(4):324–333
Carvalhal A, Gill MJ, Letendre SL, Rachlis A, Bekele T, Raboud J et al (2016) Central nervous system penetration effectiveness of antiretroviral drugs and neuropsychological impairment in the Ontario HIV Treatment Network Cohort Study. J Neurovirol 22(3):349–357
Cassol E, Misra V, Dutta A, Morgello S, Gabuzda D (2014) Cerebrospinal fluid metabolomics reveals altered waste clearance and accelerated aging in HIV patients with neurocognitive impairment. AIDS 28(11):1579–1591
Centers for Disease Control and Prevention (2017) HIV Surveillance Report, 2016, vol 28. http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Accessed 2 May 2018
Chaganti J, Marripundi K, Staub LP, Rae CD, Gates T, Moffat KJ et al (2019) Imaging correlates of the Blood Brain Barrier disruption in HIV associated neurocognitive disorder and therapeutic implications. AIDS 33(12):1843–1852
Chiao S, Rosen HJ, Nicolas K, Wendelken LA, Alcantar O, Rankin KP et al (2013) Deficits in self-awareness impact the diagnosis of asymptomatic neurocognitive impairment in HIV. AIDS Res Hum Retrovir 29(6):949–956
Cho HJ, Bertrand L, Toborek M (2019) Blood–brain barrier pericytes as a target for HIV-1 infection. Brain 142(3):502–511
Churchill MJ, Wesselingh SL, Cowley D, Pardo CA, McArthur JC, Brew BJ et al (2009) Extensive astrocyte infection is prominent in human immunodeficiency virus-associated dementia. Ann Neurol 66(2):253–258
Churchill MJ, Deeks SG, Margolis DM, Siliciano RF, Swanstrom R (2015) HIV reservoirs: what, where and how to target them. Nat Rev Microbiol 14:55
Ciccarelli N, Fabbiani M, Grima P, Falasca K, Tana M, Baldonero E et al (2013) Comparison of cognitive performance in HIV or HCV mono-infected and HIV–HCV co-infected patients. Infection 41(6):1103–1109
Clifford DB, Fagan AM, Holtzman DM, Morris JC, Teshome M, Shah AR et al (2009) CSF biomarkers of Alzheimer disease in HIV-associated neurologic disease. Neurology 73(23):1982–1987
Clifford KM, Samboju V, Cobigo Y, Milanini B, Marx GA, Hellmuth JM et al (2017) Progressive brain atrophy despite persistent viral suppression in HIV patients older than 60 years. J Acquir Immune Defic Syndr 76(3):289–297
Cole JH, Underwood J, Caan MWA, De Francesco D, van Zoest RA, Leech R et al (2017) Increased brain-predicted aging in treated HIV disease. Neurology 88(14):1349–1357
Conant K, Garzino-Demo A, Nath A, McArthur JC, Halliday W, Power C et al (1998) Induction of monocyte chemoattractant protein-1 in HIV-1 Tat-stimulated astrocytes and elevation in AIDS dementia. Proc Natl Acad Sci U S A 95(6):3117–3121
Corley MJ, Dye C, D’Antoni ML, Byron MM, Yo KL-A, Lum-Jones A et al (2016) Comparative DNA methylation profiling reveals an immunoepigenetic signature of HIV-related cognitive impairment. Sci Rep 6:33310
Cysique LA, Brew BJ (2011) Prevalence of non-confounded HIV-associated neurocognitive impairment in the context of plasma HIV RNA suppression. J Neurovirol 17(2):176–183
Cysique LA, Maruff P, Brew BJ (2004) Prevalence and pattern of neuropsychological impairment in human immunodeficiency virus-infected/acquired immunodeficiency syndrome (HIV/AIDS) patients across pre- and post-highly active antiretroviral therapy eras: a combined study of two cohorts. J Neurovirol 10(6):350–357
Cysique LA, Vaida F, Letendre S, Gibson S, Cherner M, Woods SP et al (2009) Dynamics of cognitive change in impaired HIV-positive patients initiating antiretroviral therapy. Neurology 73(5):342–348
Cysique LA, Hey-Cunningham WJ, Dermody N, Chan P, Brew BJ, Koelsch KK (2015a) Peripheral blood mononuclear cells HIV DNA levels impact intermittently on neurocognition. PLoS One 10(4):e0120488
Cysique LA, Hewitt T, Croitoru-Lamoury J, Taddei K, Martins RN, Chew CSN et al (2015b) APOE ε4 moderates abnormal CSF-abeta-42 levels, while neurocognitive impairment is associated with abnormal CSF tau levels in HIV+ individuals – a cross-sectional observational study. BMC Neurol 15:51
Cysique LA, Juge L, Lennon MJ, Gates TM, Jones SP, Lovelace MD et al (2019) HIV brain latency as measured by CSF BcL11b relates to disrupted brain cellular energy in virally suppressed HIV infection. AIDS 33(3):433–441
D’Antoni ML, Paul RH, Mitchell BI, Kohorn L, Fischer L, Lefebvre E et al (2018) Improved cognitive performance and reduced monocyte activation in virally suppressed chronic HIV after dual CCR2 and CCR5 antagonism. J Acquir Immune Defic Syndr 79(1):108–116
Dahl V, Peterson J, Fuchs D, Gisslen M, Palmer S, Price RW (2014) Low levels of HIV-1 RNA detected in the cerebrospinal fluid after up to 10 years of suppressive therapy are associated with local immune activation. AIDS 28(15):2251–2258
de Oliveira MF, Murrell B, Pérez-Santiago J, Vargas M, Ellis RJ, Letendre S et al (2015) Circulating HIV DNA correlates with neurocognitive impairment in older HIV-infected adults on suppressive ART. Sci Rep 5:17094
Deeks SG, Kitchen CMR, Liu L, Guo H, Gascon R, Narváez AB et al (2004) Immune activation set point during early HIV infection predicts subsequent CD4+ T-cell changes independent of viral load. Blood 104(4):942–947
Desplats P, Dumaop W, Smith D, Adame A, Everall I, Letendre S et al (2013) Molecular and pathologic insights from latent HIV-1 infection in the human brain. Neurology 80(15):1415–1423
Dickens AM, Yoo SW, Chin AC, Xu J, Johnson TP, Trout AL et al (2017) Chronic low-level expression of HIV-1 Tat promotes a neurodegenerative phenotype with aging. Sci Rep 7:7748
dos Santos-Silva AF, Alves JMF, Ramos I, del Cármen Piñeiro-Calvo M, Sousa C, do Rosário Serrão M et al (2017) Neurocognitive disorders in patients with HIV infection with virologic suppression for more than 10 years. World J AIDS 7(01):59
Drewes JL, Meulendyke KA, Liao Z, Witwer KW, Gama L, Ubaida-Mohien C et al (2015) Quinolinic acid/tryptophan ratios predict neurological disease in SIV-infected macaques and remain elevated in the brain under cART. J Neurovirol 21(4):449–463
Eden A, Price RW, Spudich S, Fuchs D, Hagberg L, Gisslen M (2007) Immune activation of the central nervous system is still present after >4 years of effective highly active antiretroviral therapy. J Infect Dis 196(12):1779–1783
Eden A, Nilsson S, Hagberg L, Fuchs D, Zetterberg H, Svennerholm B et al (2016) Asymptomatic cerebrospinal fluid HIV-1 viral blips and viral escape during antiretroviral therapy: a longitudinal study. J Infect Dis 214(12):1822–1825
Eletto D, Russo G, Passiatore G, Valle LD, Giordano A, Khalili K et al (2008) Inhibition of SNAP25 expression by HIV-1 Tat Involves the activity of mir-128a. J Cell Physiol 216(3):764–770
Ellery PJ, Tippett E, Chiu Y-L, Paukovics G, Cameron PU, Solomon A et al (2007) The CD16+ monocyte subset is more permissive to infection and preferentially harbors HIV-1 in vivo. J Immunol 178(10):6581–6589
Ellis RJ, Deutsch R, Heaton RK et al (1997) Neurocognitive impairment is an independent risk factor for death in HIV infection. Arch Neurol 54(4):416–424
Ellis RJ, Moore DJ, Childers ME et al (2002) Progression to neuropsychological impairment in human immunodeficiency virus infection predicted by elevated cerebrospinal fluid levels of human immunodeficiency virus RNA. Arch Neurol 59(6):923–928
Ellis RJ, Badiee J, Vaida F, Letendre S, Heaton RK, Clifford D et al (2011) CD4 nadir is a predictor of HIV neurocognitive impairment in the era of combination antiretroviral therapy. AIDS 25(14):1747–1751
Ellis RJ, Letendre S, Vaida F, Haubrich R, Heaton RK, Sacktor N et al (2014) Randomized trial of central nervous system-targeted antiretrovirals for HIV-associated neurocognitive disorder. Clin Infect Dis 58(7):1015–1022
Estes JD, Harris LD, Klatt NR, Tabb B, Pittaluga S, Paiardini M et al (2010) Damaged intestinal epithelial integrity linked to microbial translocation in pathogenic simian immunodeficiency virus infections. PLoS Pathog 6(8):e1001052
Estes JD, Kityo C, Ssali F, Swainson L, Makamdop KN, Del Prete GQ et al (2017) Defining total-body AIDS-virus burden with implications for curative strategies. Nat Med 23:1271–1276
Evering TH, Applebaum A, La Mar M, Garmon D, Dorfman D, Markowitz M (2016) Rates of non-confounded HIV associated neurocognitive disorders in men initiating cART during primary infection. AIDS 30(2):203–210
Fiandaca MS, Kapogiannis D, Mapstone M, Boxer A, Eitan E, Schwartz JB et al (2015) Identification of preclinical Alzheimer’s disease by a profile of pathogenic proteins in neurally derived blood exosomes: a case-control study. Alzheimers Dement 11(6):600–7.e1
Fischer-Smith T, Croul S, Sverstiuk AE, Capini C, L’Heureux D, Régulier EG et al (2001) CNS invasion by CD14+/CD16+ peripheral blood-derived monocytes in HIV dementia: perivascular accumulation and reservoir of HIV infection. J Neurovirol 7(6):528–541
Fogel GB, Lamers SL, Levine AJ, Valdes-Sueiras M, McGrath MS, Shapshak P et al (2015) Factors related to HIV-associated neurocognitive impairment differ with age. J Neurovirol 21(1):56–65
Funes HA, Apostolova N, Alegre F, Blas-Garcia A, Alvarez A, Marti-Cabrera M et al (2014) Neuronal bioenergetics and acute mitochondrial dysfunction: a clue to understanding the central nervous system side effects of efavirenz. J Infect Dis 210(9):1385–1395
Funes HA, Blas-Garcia A, Esplugues JV, Apostolova N (2015) Efavirenz alters mitochondrial respiratory function in cultured neuron and glial cell lines. J Antimicrob Chemother 70(8):2249–2254
Garvey LJ, Pavese N, Politis M, Ramlackhansingh A, Brooks DJ, Taylor-Robinson SD et al (2014) Increased microglia activation in neurologically asymptomatic HIV-infected patients receiving effective ART. AIDS 28(1):67–72
Gates TM, Cysique LA, Siefried KJ, Chaganti J, Moffat KJ, Brew BJ (2016) Maraviroc-intensified combined antiretroviral therapy improves cognition in virally suppressed HIV-associated neurocognitive disorder. AIDS 30(4):591–600
Gelman BB (2015) Neuropathology of HAND with suppressive antiretroviral therapy: encephalitis and neurodegeneration reconsidered. Curr HIV/AIDS Rep 12(2):272–279
Gelman BB, Chen T, Lisinicchia JG, Soukup VM, Carmical JR, Starkey JM et al (2012) The national NeuroAIDS Tissue Consortium brain gene array: two types of HIV-associated neurocognitive impairment. PLoS One 7(9):e46178
Ginsberg SD, Alldred MJ, Gunnam SM, Schiroli C, Lee SH, Morgello S et al (2018) Expression profiling suggests microglial impairment in human immunodeficiency virus neuropathogenesis. Ann Neurol 83(2):406–417
Gisslén M, Hagberg L, Brew BJ, Cinque P, Price RW, Rosengren L (2007) Elevated cerebrospinal fluid neurofilament light protein concentrations predict the development of AIDS dementia complex. J Infect Dis 195(12):1774–1778
Gisslén M, Price RW, Andreasson U, Norgren N, Nilsson S, Hagberg L et al (2015) Plasma concentration of the neurofilament light protein (NFL) is a biomarker of CNS injury in HIV infection: a cross-sectional study. EBioMedicine 3:135–140
Glenn JD, Mowry EM (2016) Emerging concepts on the gut microbiome and multiple sclerosis. J Interf Cytokine Res 36(6):347–357
Goodkin K, Miller EN, Cox C, Reynolds S, Becker JT, Martin E et al (2017) Effect of aging on neurocognitive function by stage of HIV infection: evidence from the Multi-Center AIDS Cohort Study. Lancet HIV 4(9):e411–ee22
Gorry PR, Bristol G, Zack JA, Ritola K, Swanstrom R, Birch CJ et al (2001) Macrophage tropism of human immunodeficiency virus type 1 isolates from brain and lymphoid tissues predicts neurotropism independent of coreceptor specificity. J Virol 75(21):10073–10089
Gorry PR, Zhang C, Wu S, Kunstman K, Trachtenberg E, Phair J et al (2002) Persistence of dual-tropic HIV-1 in an individual homozygous for the CCR5 Delta 32 allele. Lancet 359(9320):1832–1834
Gott C, Gates T, Dermody N, Brew BJ, Cysique LA (2017) Cognitive change trajectories in virally suppressed HIV-infected individuals indicate high prevalence of disease activity. PLoS One 12(3):e0171887
Gougeon M-L, Poirier-Beaudouin B, Durant J, Lebrun-Frenay C, Saïdi H, Seffer V et al (2017) HMGB1/anti-HMGB1 antibodies define a molecular signature of early stages of HIV-Associated Neurocognitive Isorders (HAND). Heliyon 3:e00245
Grant I, Franklin DR, Deutsch R, Woods SP, Vaida F, Ellis RJ et al (2014) Asymptomatic HIV-associated neurocognitive impairment increases risk for symptomatic decline. Neurology 82(23):2055–2062
Gray LR, Tachedjian G, Ellett AM, Roche MJ, Cheng WJ, Guillemin GJ et al (2013) The NRTIs lamivudine, stavudine and zidovudine have reduced HIV-1 inhibitory activity in astrocytes. PLoS One 8(4):e62196
Gray LR, Turville SG, Hitchen TL, Cheng W-J, Ellett AM, Salimi H et al (2014) HIV-1 entry and trans-infection of astrocytes involves CD81 vesicles. PLoS One 9(2):e90620
Gray LR, Cowley D, Welsh C, Lu HK, Brew BJ, Lewin SR et al (2016) CNS-specific regulatory elements in brain-derived HIV-1 strains affect responses to latency-reversing agents with implications for cure strategies. Mol Psychiatry 21(4):574–584
Green DA, Masliah E, Vinters HV, Beizai P, Moore DJ, Achim CL (2005) Brain deposition of beta-amyloid is a common pathologic feature in HIV positive patients. AIDS 19(4):407–411
Guaraldi G, Orlando G, Zona S, Menozzi M, Carli F, Garlassi E et al (2011) Premature age-related comorbidities among HIV-infected persons compared with the general population. Clin Infect Dis 53(11):1120–1126
Guha D, Nagilla P, Redinger C, Srinivasan A, Schatten GP, Ayyavoo V (2012) Neuronal apoptosis by HIV-1 Vpr: contribution of proinflammatory molecular networks from infected target cells. J Neuroinflammation 9(1):138
Hagberg L, Cinque P, Gisslen M, Brew BJ, Spudich S, Bestetti A et al (2010) Cerebrospinal fluid neopterin: an informative biomarker of central nervous system immune activation in HIV-1 infection. AIDS Res Ther 7:15
Haggerty S, Stevenson M (1991) Predominance of distinct viral genotypes in brain and lymph node compartments of HIV-1-infected individuals. Viral Immunol 4(2):123–131
Hao XP, Lucero CM, Turkbey B, Bernardo ML, Morcock DR, Deleage C et al (2015) Experimental colitis in SIV-uninfected rhesus macaques recapitulates important features of pathogenic SIV infection. Nat Commun 6:8020
Harezlak J, Buchthal S, Taylor M, Schifitto G, Zhong J, Daar ES et al (2011) Persistence of HIV− associated cognitive impairment, inflammation and neuronal injury in era of highly active antiretroviral treatment. AIDS 25(5):625–633
Haughey NJ, Holden CP, Nath A, Geiger JD (1999) Involvement of inositol 1,4,5-trisphosphate-regulated stores of intracellular calcium in calcium dysregulation and neuron cell death caused by HIV-1 protein Tat. J Neurochem 73(4):1363–1374
Hazenberg MD, Otto SA, van Benthem BH, Roos MT, Coutinho RA, Lange JM et al (2003) Persistent immune activation in HIV-1 infection is associated with progression to AIDS. AIDS 17(13):1881–1888
Heaton R, Clifford D, Franklin D, Woods S, Ake C, Vaida F et al (2010) HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy CHARTER Study. Neurology 75(23):2087–2096
Heaton RK, Franklin DR, Ellis RJ, McCutchan JA, Letendre SL, LeBlanc S et al (2011) HIV-associated neurocognitive disorders before and during the era of combination antiretroviral therapy: differences in rates, nature, and predictors. J Neurovirol 17(1):3–16
Heaton RK, Franklin DR Jr, Deutsch R, Letendre S, Ellis RJ, Casaletto K et al (2015) Neurocognitive change in the era of HIV combination antiretroviral therapy: the longitudinal CHARTER study. Clin Infect Dis 60(3):473–480
Hellmuth J, Fletcher JLK, Valcour V, Kroon E, Ananworanich J, Intasan J et al (2016) Neurologic signs and symptoms frequently manifest in acute HIV infection. Neurology 87(2):148–154
Heyes MP, Mefford IN, Quearry BJ, Dedhia M, Lackner A (1990) Increased ratio of quinolinic acid to kynurenic acid in cerebrospinal fluid of D retrovirus-infected rhesus macaques: relationship to clinical and viral status. Ann Neurol 27(6):666–675
Hinkin C, Castellon S, Durvasula R, Hardy D, Lam M, Mason K et al (2002) Medication adherence among HIV+ adults effects of cognitive dysfunction and regimen complexity. Neurology 59(12):1944–1950
Honeycutt JB, Liao B, Nixon CC, Cleary RA, Thayer WO, Birath SL et al (2018) T cells establish and maintain CNS viral infection in HIV-infected humanized mice. J Clin Invest 128(7):2862–2876
Houser MC, Tansey MG (2017) The gut-brain axis: is intestinal inflammation a silent driver of Parkinson’s disease pathogenesis? NPJ Parkinsons Dis 3(1):3
Hulgan T, Kallianpur AR, Guo Y, Barnholtz-Sloan JS, Gittleman H, Brown TT et al (2018) Peripheral blood mitochondrial DNA copy number obtained from genome-wide genotype data is associated with neurocognitive impairment in persons with chronic HIV infection. J Acquir Immune Defic Syndr 80(4):e95–e102
Hunt PW, Landay AL, Sinclair E, Martinson JA, Hatano H, Emu B et al (2011) A low T regulatory cell response may contribute to both viral control and generalized immune activation in HIV controllers. PLoS One 6(1):e15924
Jaureguiberry-Bravo M, Lopez L, Berman JW (2018) Frontline science: buprenorphine decreases CCL2-mediated migration of CD14+CD16+ monocytes. J Leukoc Biol 104(6):1049–1059
Jensen BK, Monnerie H, Mannell MV, Gannon PJ, Espinoza CA, Erickson MA et al (2015) Altered oligodendrocyte maturation and myelin maintenance: the role of antiretrovirals in HIV-associated neurocognitive disorders. J Neuropathol Exp Neurol 74(11):1093–1118
Jespersen S, Pedersen KK, Anesten B, Zetterberg H, Fuchs D, Gisslén M et al (2016) Soluble CD14 in cerebrospinal fluid is associated with markers of inflammation and axonal damage in untreated HIV-infected patients: a retrospective cross-sectional study. BMC Infect Dis 16(1):176
Jessen Krut J, Mellberg T, Price RW, Hagberg L, Fuchs D, Rosengren L et al (2014) Biomarker evidence of axonal injury in neuroasymptomatic HIV-1 patients. PLoS One 9(2):e88591
Johnson TP, Patel K, Johnson KR, Maric D, Calabresi PA, Hasbun R et al (2013) Induction of IL-17 and nonclassical T-cell activation by HIV-Tat protein. Proc Natl Acad Sci U S A 110(33):13588–13593
Jonathan U, Kevin RR, Alan W (2015) Could antiretroviral neurotoxicity play a role in the pathogenesis of cognitive impairment in treated HIV disease? AIDS 29(3):253
Joseph SB, Kincer LP, Bowman NM, Evans C, Vinikoor MJ, Lippincott CK et al (2019) HIV-1 RNA detected in the CNS after years of suppressive antiretroviral therapy can originate from a replicating CNS reservoir or clonally expanded cells. Clin Infect Dis 69:1345–1352
Kadri F, LaPlante A, De Luca M, Doyle L, Velasco-Gonzalez C, Patterson JR et al (2016) Defining plasma microRNAs associated with cognitive impairment in HIV-infected patients. J Cell Physiol 231(4):829–836
Kallianpur KJ, Valcour VG, Lerdlum S, Busovaca E, Agsalda M, Sithinamsuwan P et al (2014) HIV DNA in CD14+ reservoirs is associated with regional brain atrophy in patients naive to combination antiretroviral therapy. AIDS (London, England) 28(11):1619–1624
Kamal S, Locatelli I, Wandeler G, Sehhat A, Bugnon O, Metral M et al (2017) The presence of human immunodeficiency virus-associated neurocognitive disorders is associated with a lower adherence to combined antiretroviral treatment. Open Forum Infect Dis 4(2):ofx070
Kamat A, Lyons JL, Misra V, Uno H, Morgello S, Singer EJ et al (2012) Monocyte activation markers in cerebrospinal fluid associated with impaired neurocognitive testing in advanced HIV infection. J Acquir Immune Defic Syndr Hum Retrovirol 60(3):234–243
Kandanearatchi A, Brew BJ (2012) The kynurenine pathway and quinolinic acid: pivotal roles in HIV associated neurocognitive disorders. FEBS J 279(8):1366–1374
Kim WK, Alvarez X, Fisher J, Bronfin B, Westmoreland S, McLaurin J et al (2006) CD163 identifies perivascular macrophages in normal and viral encephalitic brains and potential precursors to perivascular macrophages in blood. Am J Pathol 168(3):822–834
Kim B-H, Kelschenbach J, Borjabad A, Hadas E, He H, Potash MJ et al (2019) Intranasal insulin therapy reverses hippocampal dendritic injury and cognitive impairment in a model of HIV-associated neurocognitive disorders in EcoHIV-infected mice. AIDS 33(6):973–984
Ko A, Kang G, Hattler JB, Galadima HI, Zhang J, Li Q et al (2019) Macrophages but not astrocytes harbor HIV DNA in the brains of HIV-1-infected aviremic individuals on suppressive antiretroviral therapy. J Neuroimmune Pharmacol 14(1):110–119
Krut JJ, Price RW, Zetterberg H, Fuchs D, Hagberg L, Yilmaz A et al (2017) No support for premature central nervous system aging in HIV-1 when measured by cerebrospinal fluid phosphorylated tau (p-tau). Virulence 8(5):599–604
Kuller LH, Tracy R, Belloso W, Wit SD, Drummond F, Lane HC et al (2008) Inflammatory and coagulation biomarkers and mortality in patients with HIV infection. PLoS Med 5(10):e203
Küper M, Rabe K, Esser S, Gizewski ER, Husstedt IW, Maschke M et al (2011) Structural gray and white matter changes in patients with HIV. J Neurol 258(6):1066–1075
Lamers SL, Rose R, Maidji E, Agsalda-Garcia M, Nolan DJ, Fogel GB et al (2016) HIV DNA is frequently present within pathologic tissues evaluated at autopsy from combined antiretroviral therapy-treated patients with undetectable viral loads. J Virol 90:8968–8983
Lanoy E, Guiguet M, Bentata M, Rouveix E, Dhiver C, Poizot-Martin I et al (2011) Survival after neuroAIDS: association with antiretroviral CNS penetration-effectiveness score. Neurology 76(7):644–651
Lawler K, Mosepele M, Ratcliffe S, Seloilwe E, Steele K, Nthobatsang R et al (2010) Neurocognitive impairment among HIV-positive individuals in Botswana: a pilot study. J Int AIDS Soc 13(1):15
Letendre SL, Zheng JC, Kaul M, Yiannoutsos CT, Ellis RJ, Taylor MJ et al (2011) Chemokines in cerebrospinal fluid correlate with cerebral metabolite patterns in HIV-infected individuals. J Neurovirol 17(1):63–69
Letendre S, Bharti A, Perez-Valero I, Hanson B, Franklin D, Woods SP et al (2018) Higher anti-cytomegalovirus immunoglobulin G concentrations are associated with worse neurocognitive performance during suppressive antiretroviral therapy. Clin Infect Dis 67(5):770–777
Levine AJ, Quach A, Moore DJ, Achim CL, Soontornniyomkij V, Masliah E et al (2016) Accelerated epigenetic aging in brain is associated with pre-mortem HIV-associated neurocognitive disorders. J Neurovirol 22(3):366–375
Levine AJ, Martin E, Sacktor N, Munro C, Becker J, For the multicenter ACS-NWG (2017) Predictors and impact of self-reported suboptimal effort on estimates of prevalence of HIV-associated neurocognitive disorders. J Acquir Immune Defic Syndr 75(2):203–210
Lyons JL, Uno H, Ancuta P, Kamat A, Moore DJ, Singer EJ et al (2011) Plasma sCD14 is a biomarker associated with impaired neurocognitive test performance in attention and learning domains in HIV infection. J Acquir Immune Defic Syndr 57(5):371–379
Ma Q, Vaida F, Wong J, Sanders CA, Kao Y-T, Croteau D et al (2016) Long-term efavirenz use is associated with worse neurocognitive functioning in HIV-infected patients. J Neurovirol 22(2):170–178
Mamik MK, Asahchop EL, Chan WF, Zhu Y, Branton WG, McKenzie BA et al (2016) Insulin treatment prevents neuroinflammation and neuronal injury with restored neurobehavioral function in models of HIV/AIDS neurodegeneration. J Neurosci 36(41):10683–10695
Marquine MJ, Montoya JL, Umlauf A, Fazeli PL, Gouaux B, Heaton RK et al (2016) The Veterans Aging Cohort Study (VACS) Index and neurocognitive change: a longitudinal study. Clin Infect Dis 63(5):694–702
Masliah E, Roberts ES, Langford D, Everall I, Crews L, Adame A et al (2004) Patterns of gene dysregulation in the frontal cortex of patients with HIV encephalitis. J Neuroimmunol 157(1):163–175
McGuire JL, Gill AJ, Douglas SD, Kolson DL (2015) Central and peripheral markers of neurodegeneration and monocyte activation in HIV-associated neurocognitive disorders. J Neurovirol 21(4):439–448
Mediouni S, Jablonski J, Paris JJ, Clementz MA, Thenin-Houssier S, McLaughlin JP et al (2015) Didehydro-cortistatin A inhibits HIV-1 Tat mediated neuroinflammation and prevents potentiation of cocaine reward in Tat transgenic mice. Curr HIV Res 13(1):64–79
Mehla R, Bivalkar-Mehla S, Nagarkatti M, Chauhan A (2012) Programming of neurotoxic cofactor CXCL-10 in HIV-1-associated dementia: abrogation of CXCL-10-induced neuro-glial toxicity in vitro by PKC activator. J Neuroinflammation 9:239
Mehta SR, Pérez-Santiago J, Hulgan T, Day TRC, Barnholtz-Sloan J, Gittleman H et al (2017) Cerebrospinal fluid cell-free mitochondrial DNA is associated with HIV replication, iron transport, and mild HIV-associated neurocognitive impairment. J Neuroinflammation 14(1):72
Meulendyke KA, Queen SE, Engle EL, Shirk EN, Liu J, Steiner JP et al (2014) Combination fluconazole/paroxetine treatment is neuroprotective despite ongoing neuroinflammation and viral replication in an SIV model of HIV neurological disease. J Neurovirol 20(6):591–602
Mielke MM, Bandaru VVR, McArthur JC, Chu M, Haughey NJ (2010) Disturbance in cerebral spinal fluid sphingolipid content is associated with memory impairment in subjects infected with the human immunodeficiency virus. J Neurovirol 16(6):445–456
Moulignier A, Gueguen A, Lescure F-X, Ziegler M, Girard P-M, Cardon B et al (2015) Does HIV infection alter Parkinson disease? J Acquir Immune Defic Syndr 70(2):129–136
Mukerjee R, Chang JR, Del Valle L, Bagashev A, Gayed MM, Lyde RB et al (2011) Deregulation of microRNAs by HIV-1 Vpr protein leads to the development of neurocognitive disorders. J Biol Chem 286(40):34976–34985
Mukerji SS, Misra V, Lorenz D, Cervantes-Arslanian AM, Lyons J, Chalkias S et al (2017) Temporal patterns and drug resistance in CSF viral escape among ART-experienced HIV-1 infected adults. J Acquir Immune Defic Syndr 75(2):246–255
Mukerji SS, Misra V, Lorenz DR, Uno H, Morgello S, Franklin D et al (2018) Impact of antiretroviral regimens on cerebrospinal fluid viral escape in a prospective multicohort study of antiretroviral therapy-experienced human immunodeficiency virus-1–infected adults in the United States. Clin Infect Dis 67(8):1182–1190
Mutlu EA, Keshavarzian A, Losurdo J, Swanson G, Siewe B, Forsyth C et al (2014) A compositional look at the human gastrointestinal microbiome and immune activation parameters in HIV infected subjects. PLoS Pathog 10(2):e1003829
Ndhlovu LC, Umaki T, Chew GM, Chow DC, Agsalda M, Kallianpur KJ et al (2014) Treatment intensification with maraviroc (CCR5 antagonist) leads to declines in CD16-expressing monocytes in cART-suppressed chronic HIV-infected subjects and is associated with improvements in neurocognitive test performance: implications for HIV-associated neurocognitive disease (HAND). J Neurovirol 20(6):571–582
Nichols MJ, Gates TM, Soares JR, Moffat KJ, Rae CD, Brew BJ et al (2019) Atrophic brain signatures of mild forms of neurocognitive impairment in virally suppressed HIV infection. AIDS 33(1):55–66
Nightingale S, Winsto A, Letendre S, Michael BD, McArthur JC, Khoo S et al (2014) Controversies in HIV-associated neurocognitive disorders. Lancet Neurol 13(11):1139–1151
Nir TM, Jahanshad N, Ching CRK, Cohen RA, Harezlak J, Schifitto G et al (2019) Progressive brain atrophy in chronically infected and treated HIV+ individuals. J Neurovirol 25(3):342–353
O’Halloran J, Cooley SA, Strain JF, Boerwinkle A, Paul R, Presti RM et al (2019) Altered neuropsychological performance and reduced brain volumetrics in people living with HIV on integrase strand transfer inhibitors. AIDS 33(9):1477
Ogishi M, Yotsuyanagi H (2018) Prediction of HIV-associated neurocognitive disorder (HAND) from three genetic features of envelope gp120 glycoprotein. Retrovirology 15(1):12
Oliveira MF, Chaillon A, Nakazawa M, Vargas M, Letendre SL, Strain MC et al (2017) Early antiretroviral therapy is associated with lower HIV DNA molecular diversity and lower inflammation in cerebrospinal fluid but does not prevent the establishment of compartmentalized HIV DNA populations. PLoS Pathog 13(1):e1006112
Pacifici M, Delbue S, Ferrante P, Jeansonne D, Kadri F, Nelson S et al (2013) Cerebrospinal fluid miRNA profile in HIV-encephalitis. J Cell Physiol 228(5):1070–1075
Palesch D, Bosinger SE, Tharp GK, Vanderford TH, Paiardini M, Chahroudi A et al (2018) Sooty mangabey genome sequence provides insight into AIDS resistance in a natural SIV host. Nature 553:77
Pandrea I, Cornell E, Wilson C, Ribeiro RM, Ma D, Kristoff J et al (2012) Coagulation biomarkers predict disease progression in SIV-infected nonhuman primates. Blood 120(7):1357–1366
Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of Antiretroviral agents in adults and adolescents living with HIV. Department of Health and Human Services. Available at http://www.aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf. Accessed 30 July 2019
Peluso MJ, Ferretti F, Peterson J, Lee E, Fuchs D, Boschini A et al (2012) Cerebrospinal fluid HIV escape associated with progressive neurologic dysfunction in patients on antiretroviral therapy with well-controlled plasma viral load. AIDS (London, England) 26(14)
Peluso MJ, Meyerhoff DJ, Price RW, Peterson J, Lee E, Young AC et al (2013) Cerebrospinal fluid and neuroimaging biomarker abnormalities suggest early neurological injury in a subset of individuals during primary HIV infection. J Infect Dis 207(11):1703–1712
Pemberton LA, Brew BJ (2001) Cerebrospinal fluid S-100β and its relationship with AIDS dementia complex. J Clin Virol 22(3):249–253
Persidsky Y, Ghorpade A, Rasmussen J, Limoges J, Liu XJ, Stins M et al (1999) Microglial and astrocyte chemokines regulate monocyte migration through the blood-brain barrier in human immunodeficiency virus-1 encephalitis. Am J Pathol 155(5):1599–1611
Peterson J, Gisslen M, Zetterberg H, Fuchs D, Shacklett BL, Hagberg L et al (2014) Cerebrospinal fluid (CSF) neuronal biomarkers across the spectrum of HIV infection: hierarchy of injury and detection. PLoS One 9(12):e116081
Pfefferbaum A, Rogosa DA, Rosenbloom MJ, Chu W, Sassoon SA, Kemper CA et al (2014) Accelerated aging of selective brain structures in human immunodeficiency virus infection: a controlled, longitudinal magnetic resonance imaging study. Neurobiol Aging 35(7):1755–1768
Pfefferbaum A, Zahr NM, Sassoon SA, Kwon D, Pohl KM, Sullivan EV (2018) Accelerated and premature aging characterizing regional cortical volume loss in human immunodeficiency virus infection: contributions from alcohol, substance use, and hepatitis C coinfection. Biol Psychiatry 3(10):844–859
Premeaux TA, D’Antoni ML, Abdel-Mohsen M, Pillai SK, Kallianpur KJ, Nakamoto BK et al (2019) Elevated cerebrospinal fluid Galectin-9 is associated with central nervous system immune activation and poor cognitive performance in older HIV-infected individuals. J Neurovirol 25(2):150–161
Pulliam L, Sun B, Mustapic M, Chawla S, Kapogiannis D (2019) Plasma neuronal exosomes serve as biomarkers of cognitive impairment in HIV infection and Alzheimer’s disease. J Neurovirol 25:702–709
Quach A, Horvath S, Nemanim N, Vatakis D, Witt MD, Miller EN et al (2018) No reliable gene expression biomarkers of current or impending neurocognitive impairment in peripheral blood monocytes of persons living with HIV. J Neurovirol 24(3):350–361
Robertson KR, Robertson WT, Ford S, Watson D, Fiscus S, Harp AG et al (2004) Highly active antiretroviral therapy improves neurocognitive functioning. J Acquir Immune Defic Syndr 36(1):562–566
Robertson KR, Smurzynski M, Parsons TD, Wu K, Bosch RJ, Wu J et al (2007) The prevalence and incidence of neurocognitive impairment in the HAART era. AIDS 21(14):1915–1921
Robertson K, Liner J, Meeker RB (2012) Antiretroviral neurotoxicity. J Neurovirol 18(5):388–399
Royal W III, Cherner M, Burdo TH, Umlauf A, Letendre SL, Jumare J et al (2016) Associations between cognition, gender and monocyte activation among HIV infected individuals in Nigeria. PLoS One 11(2):e0147182
Rubin LH, Sacktor N, Creighton J, Du Y, Endres CJ, Pomper MG et al (2018) Microglial activation is inversely associated with cognition in individuals living with HIV on effective antiretroviral therapy. AIDS (London, England) 32(12):1661–1667
Sacktor N, Miyahara S, Deng L, Evans S, Schifitto G, Cohen BA et al (2011) Minocycline treatment for HIV-associated cognitive impairment: results from a randomized trial. Neurology 77(12):1135–1142
Sacktor N, Miyahara S, Evans S, Schifitto G, Cohen B, Haughey N et al (2014) Impact of minocycline on cerebrospinal fluid markers of oxidative stress, neuronal injury, and inflammation in HIV seropositive individuals with cognitive impairment. J Neurovirol 20(6):620–626
Sacktor N, Skolasky RL, Seaberg E, Munro C, Becker JT, Martin E et al (2016) Prevalence of HIV-associated neurocognitive disorders in the Multicenter AIDS Cohort Study. Neurology 86(4):334–340
Sacktor N, Skolasky RL, Moxley R, Wang S, Mielke MM, Munro C et al (2018) Paroxetine and fluconazole therapy for HIV-associated neurocognitive impairment: results from a double-blind, placebo-controlled trial. J Neurovirol 24(1):16–27
Sailasuta N, Ananworanich J, Lerdlum S, Sithinamsuwan P, Fletcher JLK, Tipsuk S et al (2016) Neuronal-glia markers by magnetic resonance spectroscopy in HIV before and after combination antiretroviral therapy. J Acquir Immune Defic Syndr 71(1):24–30
Saiyed ZM, Gandhi N, Agudelo M, Napuri J, Samikkannu T, Reddy PVB et al (2011) HIV-1 Tat upregulates expression of histone deacetylase-2 (HDAC2) in human neurons: implication for HIV-associated neurocognitive disorder (HAND). Neurochem Int 58(6):656–664
Sami Saribas A, Cicalese S, Ahooyi TM, Khalili K, Amini S, Sariyer IK (2017) HIV-1 Nef is released in extracellular vesicles derived from astrocytes: evidence for Nef-mediated neurotoxicity. Cell Death Dis 8:e2542
Saylor D, Dickens AM, Sacktor N, Haughey N, Slusher B, Pletnikov M et al (2016) HIV-associated neurocognitive disorder – pathogenesis and prospects for treatment. Nat Rev Neurol 12(4):234–248
Schifitto G, Zhang J, Evans SR, Sacktor N, Simpson D, Millar LL et al (2007) A multicenter trial of selegiline transdermal system for HIV-associated cognitive impairment. Neurology 69(13):1314–1321
Schnell G, Spudich S, Harrington P, Price RW, Swanstrom R (2009) Compartmentalized human immunodeficiency virus type 1 originates from long-lived cells in some subjects with HIV-1–associated dementia. PLoS Pathog 5(4):e1000395
Schrier RD, Hong S, Crescini M, Ellis R, Pérez-Santiago J, Spina C et al (2015) Cerebrospinal fluid (CSF) CD8+ T-cells that express interferon-gamma contribute to HIV Associated Neurocognitive Disorders (HAND). PLoS One 10(2):e0116526
Serena M, Stefano S, Oriana T (2013) Blocking HIV-1 replication by targeting the Tat-hijacked transcriptional machinery. Curr Pharm Des 19(10):1860–1879
Sevigny JJ, Albert SM, McDermott MP et al (2007) An evaluation of neurocognitive status and markers of immune activation as predictors of time to death in advanced HIV infection. Arch Neurol 64(1):97–102
Shah A, Kumar A (2010) HIV-1 gp120-mediated increases in IL-8 production in astrocytes are mediated through the NF-κB pathway and can be silenced by gp120-specific siRNA. J Neuroinflammation 7(1):96
Shah A, Singh DP, Buch S, Kumar A (2011a) HIV-1 envelope protein gp120 up regulates CCL5 production in astrocytes which can be circumvented by inhibitors of NF-κB pathway. Biochem Biophys Res Commun 414(1):112–117
Shah A, Verma AS, Patel KH, Noel R, Rivera-Amill V, Silverstein PS et al (2011b) HIV-1 gp120 induces expression of IL-6 through a nuclear factor-kappa B-dependent mechanism: suppression by gp120 specific small interfering RNA. PLoS One 6(6):e21261
Shaunak S, Albright RE, Klotman ME, Henry SC, Bartlett JA, Hamilton JD (1990) Amplification of HIV-1 provirus from cerebrospinal fluid and its correlation with neurologic disease. J Infect Dis 161(6):1068–1072
Sheppard DP, Iudicello JE, Morgan EE, Kamat R, Clark LR, Avci G et al (2017) Accelerated and accentuated neurocognitive aging in HIV infection. J Neurovirol 23(3):492–500
Simioni S, Cavassini M, Annoni J-M, Abraham AR, Bourquin I, Schiffer V et al (2010) Cognitive dysfunction in HIV patients despite long-standing suppression of viremia. AIDS 24(9):1243–1250
Singh KK, Barroga CF, Hughes MD, Chen J, Raskino C, McKinney RE et al (2003) Genetic influence of CCR5, CCR2 and SDF1 variants on human immunodeficiency virus 1 (HIV-1)–related disease progression and neurological impairment, in children with symptomatic HIV-1 infection. J Infect Dis 188(10):1461–1472
Somsouk M, Estes JD, Deleage C, Dunham RM, Albright R, Inadomi JM et al (2015) Gut epithelial barrier and systemic inflammation during chronic HIV infection. AIDS 29(1):43–51
Sonia M, Albert D, Gilbert B, Isabelle R, Catherine D, Herve T-D et al (2012) Antiretroviral therapy does not block the secretion of the human immunodeficiency virus Tat protein. Infect Disord Drug Targets 12(1):81–86
Spector SA, Singh KK, Gupta S, Cystique LA, Jin H, Letendre S et al (2010) 195APOE ε4 and MBL-2 O/O genotypes are associated with neurocognitive impairment in HIV-infected plasma donors from Anhui Province, China. AIDS 24(10):1471–1479
Spudich S, Gisslen M, Hagberg L, Lee E, Liegler T, Brew B et al (2011) Central nervous system immune activation characterizes primary human immunodeficiency virus 1 infection even in participants with minimal cerebrospinal fluid viral burden. J Infect Dis 204(5):753–760
Spudich S, Robertson KR, Bosch RJ, Gandhi RT, Cyktor JC, Mar H et al (2019) Persistent HIV-infected cells in cerebrospinal fluid are associated with poorer neurocognitive performance. J Clin Invest 129(8):3339–3346
Steinbrink F, Evers S, Buerke B, Young P, Arendt G, Koutsilieri E et al (2013) Cognitive impairment in HIV infection is associated with MRI and CSF pattern of neurodegeneration. Eur J Neurol 20(3):420–428
Strazza M, Pirrone V, Wigdahl B, Nonnemacher MR (2011) Breaking down the barrier: the effects of HIV-1 on the blood-brain barrier. Brain Res 1399:96–115
Strickland SL, Rife BD, Lamers SL, Nolan DJ, Veras NMC, Prosperi MCF et al (2014) Spatiotemporal dynamics of simian immunodeficiency virus brain infection in CD8(+) lymphocyte-depleted rhesus macaques with neuroAIDS. J Gen Virol 95(Pt 12):2784–2795
Sturdevant CB, Joseph SB, Schnell G, Price RW, Swanstrom R, Spudich S (2015) Compartmentalized replication of R5 T cell-tropic HIV-1 in the central nervous system early in the course of infection. PLoS Pathog 11(3):e1004720
Suh H-S, Gelman BB, Lee SC (2014a) Potential roles of microglial cell progranulin in HIV-associated CNS pathologies and neurocognitive impairment. J Neuroimmune Pharmacol 9(2):117–132
Suh H-S, Lo Y, Choi N, Letendre S, Lee SC (2014b) Evidence of the innate antiviral and neuroprotective properties of progranulin. PLoS One 9(5):e98184
Sun B, Dalvi P, Abadjian L, Tang N, Pulliam L (2017) Blood neuron-derived exosomes as biomarkers of cognitive impairment in HIV. AIDS 31(14):F9–F17
Takahashi K, Wesselingh SL, Griffin DE, McArthur JC, Johnson RT, Glass JD (1996) Localization of HIV-1 in human brain using polymerase chain reaction/in situ hybridization and immunocytochemistry. Ann Neurol 39(6):705–711
Tambussi G, Gori A, Capiluppi B, Balotta C, Papagno L, Morandini B et al (2000) Neurological symptoms during primary human immunodeficiency virus (HIV) infection correlate with high levels of HIV RNA in cerebrospinal fluid. Clin Infect Dis 30(6):962–965
Tatro ET, Scott ER, Nguyen TB, Salaria S, Banerjee S, Moore DJ et al (2010) Evidence for alteration of gene regulatory networks through microRNAs of the HIV-infected brain: novel analysis of retrospective cases. PLoS One 5(4):e10337
Tatro ET, Soontornniyomkij B, Letendre SL, Achim CL (2014) Cytokine secretion from brain macrophages infected with human immunodeficiency virus in vitro and treated with raltegravir. BMC Infect Dis 14:386
Tavazzi E, Morrison D, Sullivan P, Morgello S, Fischer T (2014) Brain inflammation is a common feature of HIV-infected patients without HIV encephalitis or productive brain infection. Curr HIV Res 12(2):97–110
Thames AD, Briones MS, Magpantay LI, Martinez-Maza O, Singer EJ, Hinkin CH et al (2015) The role of chemokine C-C motif ligand 2 genotype and cerebrospinal fluid chemokine C-C motif ligand 2 in neurocognition among HIV-infected patients. AIDS 29(12):1483–1491
Thompson KA, Cherry CL, Bell JE, McLean CA (2011) Brain cell reservoirs of latent virus in presymptomatic HIV-infected individuals. Am J Pathol 179(4):1623–1629
Tisch S, Brew B (2009) Parkinsonism in HIV-infected patients on highly active antiretroviral therapy. Neurology 73(5):401–403
Tisch S, Brew BJ (2010) HIV, HAART, and Parkinson’s disease: co-incidence or pathogenetic link? Mov Disord 25(13):2257–2258
Torti C, Focà E, Cesana BM, Lescure FX (2011) Asymptomatic neurocognitive disorders in patients infected by HIV: fact or fiction? BMC Med 9(1):138
Tozzi V, Balestra P, Serraino D, Bellagamba R, Corpolongo A, Piselli P et al (2005) Neurocognitive impairment and survival in a cohort of HIV-infected patients treated with HAART. AIDS Res Hum Retrovir 21(8):706–713
Trickey A, May MT, Vehreschild J-J, Obel N, Gill MJ, Crane HM et al (2017) Survival of HIV-positive patients starting antiretroviral therapy between 1996 and 2013: a collaborative analysis of cohort studies. Lancet HIV 4(8):e349–ee56
Turner RS, Chadwick M, Horton WA, Simon GL, Jiang X, Esposito G (2016) An individual with human immunodeficiency virus, dementia, and central nervous system amyloid deposition. Alzheimers Dement 4:1–5
Valcour V, Shikuma C, Shiramizu B, Watters M, Poff P, Selnes O et al (2004) Higher frequency of dementia in older HIV-1 individuals: the Hawaii Aging with HIV-1 Cohort. Neurology 63(5):822–827
Valcour V, Chalermchai T, Sailasuta N, Marovich M, Lerdlum S, Suttichom D et al (2012) Central nervous system viral invasion and inflammation during acute HIV infection. J Infect Dis 206(2):275–282
Valcour VG, Ananworanich J, Agsalda M, Sailasuta N, Chalermchai T, Schuetz A et al (2013) HIV DNA reservoir increases risk for cognitive disorders in cART-Naïve patients. PLoS One 8(7):e70164
Vassallo M, Dunais B, Durant J, Carsenti-Dellamonica H, Harvey-Langton A, Cottalorda J et al (2013) Relevance of lipopolysaccharide levels in HIV-associated neurocognitive impairment: the Neuradapt study. J Neurovirol 19(4):376–382
Vassallo M, Durant J, Lebrun-Frenay C, Fabre R, Ticchioni M, Andersen S et al (2015) Virologically suppressed patients with asymptomatic and symptomatic HIV-associated neurocognitive disorders do not display the same pattern of immune activation. HIV Med 16(7):431–440
Veenstra M, León-Rivera R, Li M, Gama L, Clements JE, Berman JW (2017) Mechanisms of CNS viral seeding by HIV+ CD14+ CD16+ monocytes: establishment and reseeding of viral reservoirs contributing to HIV-associated neurocognitive disorders. MBio 8(5)
Veenstra M, Byrd DA, Inglese M, Buyukturkoglu K, Williams DW, Fleysher L et al (2019) CCR2 on peripheral blood CD14+CD16+ monocytes correlates with neuronal damage, HIV-associated neurocognitive disorders, and peripheral HIV DNA: reseeding of CNS reservoirs? J Neuroimmune Pharmacol 14:120–133
Venkatachari NJ, Jain S, Walker L, Bivalkar-Mehla S, Chattopadhyay A, Bar-Joseph Z et al (2017) Transcriptome analyses identify key cellular factors associated with HIV-1 associated neuropathogenesis in infected men. AIDS 31(5):623–633
Vera JH, Guo Q, Cole JH, Boasso A, Greathead L, Kelleher P et al (2016) Neuroinflammation in treated HIV-positive individuals: a TSPO PET study. Neurology 86(15):1425–1432
Vivithanaporn P, Heo G, Gamble J, Krentz H, Hoke A, Gill M et al (2010) Neurologic disease burden in treated HIV/AIDS predicts survival a population-based study. Neurology 75(13):1150–1158
Vivithanaporn P, Asahchop EL, Acharjee S, Baker GB, Power C (2016) HIV protease inhibitors disrupt astrocytic glutamate transporter function and neurobehavioral performance. AIDS (London, England) 30(4):543–552
Williams R, Dhillon NK, Hegde ST, Yao H, Peng F, Callen S et al (2009) Proinflammatory cytokines and HIV-1 synergistically enhance CXCL10 expression in human astrocytes. Glia 57(7):734–743
Williams DW, Calderon TM, Lopez L, Carvallo-Torres L, Gaskill PJ, Eugenin EA et al (2013) Mechanisms of HIV entry into the CNS: increased sensitivity of HIV infected CD14+CD16+ monocytes to CCL2 and key roles of CCR2, JAM-A, and ALCAM in diapedesis. PLoS One 8(7):e69270
Wong M, Robertson K, Nakasujja N, Skolasky R, Musisi S, Katabira E et al (2007) Frequency of and risk factors for HIV dementia in an HIV clinic in sub-Saharan Africa. Neurology 68(5):350–355
Woods SP, Iudicello JE, Dawson MS, Weber E, Grant I, Letendre SL et al (2010) HIV-associated deficits in action (verb) generation may reflect astrocytosis. J Clin Exp Neuropsychol 32(5):522–527
Woods SP, Iudicello JE, Morgan EE, Verduzco M, Smith TV, Cushman C et al (2017) Household everyday functioning in the internet age: online shopping and banking skills are affected in HIV-associated neurocognitive disorders. J Int Neuropsychol Soc 23(7):605–615
Wright EJ, Grund B, Robertson K, Brew BJ, Roediger M, Bain MP et al (2010) Cardiovascular risk factors associated with lower baseline cognitive performance in HIV-positive persons. Neurology 75(10):864–873
Wright PW, Vaida FF, Fernández RJ, Rutlin J, Price RW, Lee E et al (2015) Cerebral white matter integrity during primary HIV infection. AIDS 29(4):433–442
Wright EJ, Grund B, Robertson KR, Cysique L, Brew BJ, Collins GL et al (2018) No neurocognitive advantage for immediate antiretroviral treatment in adults with greater than 500 CD4+ T-cell counts. AIDS 32(8):985–997
Yadav A, Betts MR, Collman RG (2016) Statin modulation of monocyte phenotype and function: implications for HIV-1 associated neurocognitive disorders. J Neurovirol 22(5):584–596
Yelamanchili SV, Chaudhuri AD, Chen LN, Xiong H, Fox HS (2010) MicroRNA-21 dysregulates the expression of MEF2C in neurons in monkey and human SIV/HIV neurological disease. Cell Death Dis 1(9):e77
Yilmaz A, Yiannoutsos CT, Fuchs D, Price RW, Crozier K, Hagberg L et al (2013) Cerebrospinal fluid neopterin decay characteristics after initiation of antiretroviral therapy. J Neuroinflammation 10(1):62
Young AC, Yiannoutsos CT, Hegde M, Lee E, Peterson J, Walter R et al (2014) Cerebral metabolite changes prior to and after antiretroviral therapy in primary HIV infection. Neurology 83(18):1592–1600
Yu C, Seaton M, Letendre S, Heaton R, Al-Harthi L (2017) Plasma dickkopf-related protein 1, an antagonist of the Wnt pathway, is associated with HIV-associated neurocognitive impairment. AIDS 31(10):1379–1385
Yuan L, Qiao L, Wei F, Yin J, Liu L, Ji Y et al (2013) Cytokines in CSF correlate with HIV-associated neurocognitive disorders in the post-HAART era in China. J Neurovirol 19(2):144–149
Yuen T, Brouillette M-J, Fellows LK, Ellis RJ, Letendre S, Heaton R et al (2017) Personalized risk index for neurocognitive decline among people with well-controlled HIV infection. J Acquir Immune Defic Syndr 76(1):48–54
Zhang Y, Wang M, Li H, Zhang H, Shi Y, Wei F et al (2012) Accumulation of nuclear and mitochondrial DNA damage in the frontal cortex cells of patients with HIV-associated neurocognitive disorders. Brain Res 1458:1–11
Zhou L, Pupo GM, Gupta P, Liu B, Tran SL, Rahme R et al (2012) A parallel genome-wide mRNA and microRNA profiling of the frontal cortex of HIV patients with and without HIV-associated dementia shows the role of axon guidance and downstream pathways in HIV-mediated neurodegeneration. BMC Genomics 13(1):677
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Angelovich, T.A., Churchill, M.J., Wright, E.J., Brew, B.J. (2020). New Potential Axes of HIV Neuropathogenesis with Relevance to Biomarkers and Treatment. In: Cysique, L.A., Rourke, S.B. (eds) Neurocognitive Complications of HIV-Infection. Current Topics in Behavioral Neurosciences, vol 50. Springer, Cham. https://doi.org/10.1007/7854_2019_126
Download citation
DOI: https://doi.org/10.1007/7854_2019_126
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-80758-0
Online ISBN: 978-3-030-80759-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)