Abstract
BACKGROUND:
Diabetes mellitus is a major health concern in current scenario which has been found to affect people of almost all ages. The disease has huge impact on global health; therefore, alternate methods apart from insulin injection are being explored to cure diabetes. Therefore, this review mainly focuses on the current status and therapeutic potential of stem cells mainly mesenchymal stem cells (MSCs) for Type 1 diabetes mellitus in preclinical animal models as well as humans.
METHODS:
Current treatment for Type 1 diabetes mellitus mainly includes use of insulin which has its own limitations and also the underlying mechanism of diseases is still not explored. Therefore, alternate methods to cure diabetes are being explored. Stem cells are being investigated as an alternative therapy for treatment of various diseases including diabetes. Few preclinical studies have also been conducted using undifferentiated MSCs as well as in vitro MSCs differentiated into β islet cells.
RESULTS:
These stem cell transplant studies have highlighted the benefits of MSCs, which have shown promising results. Few human trials using stem cells have also affirmed the potential of these cells in alleviating the symptoms.
CONCLUSION:
Stem cell transplantation may prove to be a safe and effective treatment for patients with Type 1 diabetes mellitus.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
In last few decades, diabetes mellitus (DM) has emerged as one of the major concerns of the public healthcare problems worldwide [1]. It is a chronic, common, non-communicable disease (NCD) which is a group of glucose metabolism disorders characterized by high levels of blood glucose. As per the international diabetic federation (IDF) report, 366 million cases were estimated in 2011 and it is expected to reach 552 million by 2030 [2]. Moreover, 5% of the deaths are being caused by diabetes only and this number is increasing rapidly.
Among the two major types of diabetes, type 1 diabetes mellitus (T1DM) is an autoimmune disorder which is characterized by the attack of the body’s immune cells on insulin-producing β cells in the islets of Langerhans of the pancreas [3]. In contrast, type 2 diabetes mellitus (T2DM) is characterized by either insufficient synthesis of insulin or by insulin resistance at the receptor level which leads to build-up of the glucose in the blood [4].
T2DM majorly accounts for 90–95% of the diabetic cases and is result of mainly excess body weight and physical inactivity. This can be controlled by oral medication and change in lifestyle. Very few cases need insulin administration in T2DM. Whereas, in T1DM, which accounts for 5–10% of total diabetic cases, there occurs destruction of pancreatic β-cells, culminating in absolute insulin deficiency. Diabetic complications in such cases continue to be a major cause of morbidity and mortality [5].
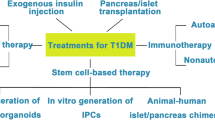
At present, exogenous insulin therapy is the most reliable treatment for managing hyperglycemia caused by T1DM. However, its short life span and cost has come up as limiting factor for this treatment. The short life span of insulin makes it very difficult to keep constant control over glucose level using insulin and hence, its administration becomes critical [6, 7]. Thus, insulin therapy only acts as a life saving measure, but it is not the cure. Therefore, alternative therapies to cure diabetic patients with insulin deficiency have become the major focus of research over past few years. One potential therapy for diabetic patients is infusion of donor islets of Langerhans into the hepatic portal vein. In this procedure, islets containing the insulin-secreting β cells are transplanted from a cadaveric donor to the patient. This procedure has been found successful in relieving T1DM patients from insulin therapy to some extent. However, there exists variation in quality of donor cells which further leads to variations in the success of results. Moreover, it is evident that the limited supply of cadaveric donor islets cannot meet the requirement of ever increasing number of diabetic cases in today’s population [8, 9]. Furthermore, apart from the shortage of organ donor and need for immunosuppressants, this method poses several challenges such as technical difficulties involved in isolation, culture and characterization of islets. In this scenario, stem cell transplantation has emerged as an attractive and promising alternative method for diabetic treatment. It has become major focus for diabetic treatment since last few decades [9].
2 Stem cell transplantation
Stem cells have been found to possess the ability to repair the damaged tissue either by directly differentiating into host cell type and/or by the release of cytokines and other factors. Broadly, stem cells are categorized into embryonic stem cells (ESCs) and adult stem cells (ASCs). ESCs are pluripotent cells that can give rise to cells of all three germ layers. Many protocols have been established for in vitro differentiation of ESCs into insulin secreting cells. Assady et al. for the first time reported the spontaneous differentiation of ESCs into β-islet cells [10, 11]. However, their tumorogenic propensity and the associated ethical issues, limit their use for human usage. On the other hand, ASCs are multipotent cells which can differentiate into cells of various lineages [12,13,14]. These are preferred over ESCs because they lack ethical issues, can be easily isolated and are immunologically naïve. These multipotent adult stem cells have been reported to be present within pancreatic islets and in nonendocrine parts of the pancreas [15, 16] with the ability to differentiate into islet-like cells. Apart from these, other cells such as hepatic oval cells, cells within the spleen have also been differentiated into islet cells both in vitro and in vivo [11, 17,18,19,20,21,22]. However, these cell types have higher chances of rejection due to their allogenic nature and also these sources are not abundant sources of stem cells. Therefore, the other abundant sources of adult, multipotent stem cells have been explored extensively. These include skin, bone marrow, umbilical cord, cord blood, dental pulp, hair follicle and adipose tissue etc. [23,24,25,26,27,28,29]. MSCs are of great advantage compared with other stem cells like ESC or stem cells from organs. The functional cells differentiated from MSCs upon transplantation into MSC donors (autologous transplantation) may also not get rejected.
3 Mesenchymal stem cells (MSCs)
Mesenchymal stem cells (MSCs) are fibroblast like, spindle shaped multipotent cells with tri-lineage differentiation potential. These were first isolated from rat bone marrow by Friedenstein et al. and later have been found in various other tissues. These cells are characterized on the basis of the presence of certain surface markers (CD105, CD29, CD73, CD90, HLA class I molecules) and absence of hematopoietic and endothelial markers (HLA class II molecules, CD34, CD45, CD31, CD14) [30]. These can be expanded easily and have a population doubling time of approximately 24–48 h. In addition, these can be expanded in culture for more than 60 doublings. The most established source of MSCs which has been used for in vitro differentiation into cells of all three lineages is bone marrow [31]. However, in last decade other less invasive sources of MSCs have also been explored including dental pulp, adipose tissue, umbilical cord etc. [23,24,25,26,27,28,29]. Earlier MSCs were supposed to only secrete cytokines and growth factors for the support of hematopoiesis. However, later these cells have been found to differentiate into various lineages including osteoblasts, chondrocytes, neurons, skeletal muscle cells, cardiac cells, hepatocytes etc. Additionally, they migrate to the site of injury and help in regeneration by secretion of various bioactive factors [32]. By virtue of these features, MSCs have come up as a promising modality in human clinical cell therapies. Various clinical trials using bone marrow derived MSCs followed by adipose tissue and umbilical cord derived MSCs have been completed for diseases like Myocardial Infarct, Stroke, Diabetes, Spinal Cord Injury etc. [33,34,35,36].
4 Mesenchymal stem cells in diabetes
Although, during past few years lot of research has been done to explore in vitro differentiation of MSCs into islet cells, but still there is not much consensus on the most suitable protocol and the most suitable source of MSCs for pancreatic regeneration. Majorly, the sources of MSCs that have been explored in this area include bone marrow, adipose tissue and umbilical cord. In general, the ideal cell source should be easy to harvest, expand, abundantly available and be able to generate functional β islet cells. Further, the most suitable inducer/inducer cocktail should be safe, minimally manipulative to cells, with short treatment procedure and have maximum efficiency to generate functional β cells.
Considering the differential response of MSCs from various sources to different protocols, we have organized this review on the biological source of MSCs from which these are obtained and their responses to various chemical regimes, which may depend on a plethora of factors. These MSCs can be differentiated into insulin secreting functional β cells using chemical methods as well genetic manipulations (Fig. 1) [37]. Further, we have discussed about the in vivo behavior of these differentiated islet cells in combating diabetes [38].
4.1 Bone marrow derived mesenchymal stem cells (BM-MSCs)
Bone marrow is the oldest and most commonly utilized source of MSCs. Oh et al. first studied their differentiation into islet cells in 2004. They reported that BM-MSCs under Dimethyl sulfoxide (DMSO) and high glucose concentration are capable of generating insulin secreting cells. When insulin-producing clusters are transplanted into streptozotocin (STZ)-treated NOD/SCID mice, blood glucose levels were normalized [39]. In same line, in 2004, Chen et al. [40] used 2-mercaptoethanol (βME) and nicotinamide under low glucose conditions for the generation of functionally active insulin secreting cells which could control glucose in diabetic rats. Further, Tang et al. [41] isolated, characterized and differentiated single cell derived mouse bone marrow stem cell line into insulin producing cells using nicotinamide and exendin-4. Other pancreatic inducers include a cocktail consisting of human Activin A, N2 supplement, B27 supplement and nicotinamide, which has been used for differentiation of mice SSEA-1 positive cells into insulin secreting cells [42].
Apart from this, Betacellulin (BTC), a ligand of the epidermal growth factor receptor, has been found to enhance the growth and differentiation into β-cells in a synergistic manner with nicotinamide. Additionally, it has proven to improve glucose metabolism in experimental diabetic rodent models [43]. Step wise differentiation has also been investigated for differentiation of hematopoietic-rich stem cells from rat into β-cells by Gabr et al. [44]. They used 1% DMSO for 3 days, followed by culture for 7 days in a glucose-rich medium supplemented with pancreatic extract. Thereafter, they incubated the cells in low glucose media supplemented with 5% fetal bovine serum, nicotinamide and exendin-4 for 7 more days. These islets like clusters when transplanted in the testes of diabetic rats could normalize blood glucose levels for 3 months in 80% of the treated rats. These therapeutic benefits were reversed after orchidectomy [44].
Very few studies have been done which have documented the efficiency of MSCs from different sources to differentiate into islet cells, on a single platform. In 2011, Zanini et al. compared islet differentiation of mesenchymal stem cells derived from human pancreatic islets (Human Islet Mesenchymal stem cells: HI-MSCs) and mesenchymal stem cells isolated from human bone marrow (BM-MSCs) in a custom made serum-free medium, comprising of a basal medium supplemented with platelet lysate (PL), retinoic acid, activin, GLPI-1, epidermal growth factor (EGF), fibroblast growth factor (FGF), betacellulin, nicotinamide and glutamine for 3 weeks. HI-ILCs (Islet like cells derived from HI-MSCs) expressed PDX1 (pancreatic duodenal homeobox gene-1), insulin, C peptide and Glut-2 whereas; BM-ILCs (Islet like cells derived from BM-MSCs) only expressed Glut-2 and insulin. This group also did a proteomic analysis and highlighted differences in the MSCs according to the site of origin, reflecting their spontaneous differentiation and commitment [45].
In another study, by Kao et al. [38], three sources of MSCs Wharton’s jelly (WJ), bone marrow (BM), and surgically resected pancreatic tissue were compared with for their in vitro differentiation potential into insulin producing cell and subsequently WJ-MSCs were found to have better proliferation and differentiation potential than pancreatic MSCs and BM-MSCs. Further, after transplantation of these cells, the animals were monitored for their blood glucose levels till 8 weeks. It was found that WJ-MSC derived islet cells showed better glucose control than islet cells derived from BM-MSCs and resected pancreas. The blood glucose levels were significantly reduced at first week and a significant decrease was maintained till 8 weeks.
The in vitro differentiation of MSCs into islet cells may also be clinically relevant as these cells may not present themselves as fully mature β-cells, thereby evading the cycle of β-cell destruction by the immune system.
Other than chemical cues, viral-mediated gene transfer has also been investigated to differentiate cells into insulin secreting cells [46]. It is used as a method to re-introduce normal copies of DNA into abnormal cells, or other cell types, as a means of treating genetic diseases. Viral-mediated transdifferentiation is an attractive method of obtaining surrogate β cells as they would be less likely to express identical autoantigens against which the primary autoimmune response was developed. In same line, Karnieli et al. [47] transfected BM-MSCs with the key rat pancreatic transcription factor (PDX1) which leads to the production of insulin in vitro in response to high glucose condition. Furthermore, when these cells were transplanted under the kidney capsule of STZ-diabetic immunodeficient mice, they reduced blood glucose levels for a period of 6–8 weeks, after which an abnormal glucose tolerance was observed. The outcome of the transplantation of these naïve MSCs and β-islet cells derived from MSCs using chemical regime and viral transfection has been summarized in Table 1. At pre-clinical level, various independent groups have documented the reversal of hyperglycemia upon stem cell transplantation [41, 48,49,50].
4.2 Adipose tissue-derived mesenchymal stem cells (AD-MSCs)
Adipose tissue has come up as the most abundant source of MSCs in past decade. The use of adipose tissue has amassed significant attention in stem cell treatment due to its ease of isolation and abundance of adipose tissue; it has amassed significant attention [24, 51]. Since 2013, very few reports have been published, which documented the islet β cell generating capacity of AD-MSCs. However, its first report came in 2006, where Timper et al. reported the presence of Isl-1 positive MSCs in human adipose tissue which were able to adopt a pancreatic endocrine phenotype using chemical cues only. Differentiation medium consisted of serum-free DMEM/F12 medium with 17.5 mM glucose supplemented with nicotinamide, activin-A, exendin-4, hepatocyte growth factor (HGF), pentagastrin, B-27 serum-free supplement and N-2 Supplement [52]. Later, in 2013 Dave et al. and Li et al. reported differentiation of human AD-MSCs into islet cells using only chemical inducers. Dave et al. [53] used DMEM-HG supplemented with nicotinamide, activin A, exendin-4, pentagastrin, hepatocyte growth factor (HGF), and serum supplements like B-27 and N-2. Whereas, Li et al. [54] for the first time reported step wise differentiation where they differentiated AD-MSCs to definitive endoderm (DE) using activin A and then differentiated to pancreatic progenitors (PP) using medium consisting of DF-12 supplemented with retinoic acid (RA), Dkk1, EGF, FGF2, B-27 for 6–11 days. These AD-MSC derived PP cells were further induced into endocrine and exocrine cells after being cultured in specific medium for 8 days. Despite the differentiation of AD-MSCs into pancreatic islet cells as depicted by expression of some key pancreatic markers, these still remain unable to regulate insulin secretion. From a therapeutic perspective, ongoing clinical trials have already demonstrated the safety of adipose tissue MSC-like cells, although there have been technical difficulties in interpretation of results due to lack of complete characterization of the cell populations being used [53,54,55,55].
Islet generation potential of AD-MSCs has further been compared with BM-MSCs using step wise chemical treatment with RA, N2, B27, nicotinamide, EGF, activin A, and exendin-4 for 12 days, by Marappagounder et al. [56]. They reported the successful differentiation of both BM-MSCs and AD-MSCs into β-islet cells on the basis of morphology, diathiozone staining, expression of pancreatic development genes and insulin secretion assay. However, insulin secretion assays proved BM-MSCs to be a better source than AD-MSCs [56].
Apart from chemical induction, viral mediated transfection has also been used for differentiation of AD-MSCs. Ectopic expression of PDX1 has not been found to dramatically improve the differentiation of AD-MSCs in vitro. However, under in vivo diabetic microenvironment these seemed to maturate better, and also facilitated long-term reversal of hyperglycemia upon transplantation [57]. Despite this edge, PDX1 induced differentiation has been found to lead to autoimmune destruction [57]. Therefore, this transfection method for in vitro differentiation needs to be explored further before it can be applied in clinical studies.
4.3 Umbilical cord blood and placenta-derived mesenchymal stem cells
Other than bone marrow and adipose tissue, new sources of MSCs which have been found to possess the ability to differentiate into islet like cells include umbilical cord (blood and Wharton’s jelly) and the placenta. These have been differentiated using chemical cues i.e., high glucose media supplemented with mainly BME, nicotinamide, FGF, EGF, retinoic acid and exendin-4 [58,59,59]. Several groups have already shown that umbilical cord blood-derived cells can be coaxed into insulin producing cells, although not with the same efficiency as true islet cells [60,61,62,63,64]. These MSCs are supposed to be more primitive than MSCs derived from adult sources and express pluripotent markers (Oct3/4 and Nanog) like ESCs. Also, umbilical cord blood has been found to inhabit various cell populations with features similar to ESC type which are capable of giving rise to hematopoietic, epithelial, endothelial, and neural tissues both in vitro and in vivo.
4.4 Amniotic fluid-derived mesenchymal stem cells (AF-MSCs)
AF-MSCs are one of the latest source of tissue-derived MSCs. These are fibroblastic-like cells which are shed by the fetus to the surrounding liquid during its development. It shares many properties with MSCs-derived from placental, chorionic, and cord blood/tissue [65, 66]. They can be procured with relative ease, although not routinely, through standard prenatal diagnostic procedures. Preliminary studies have also reported their successful in vitro differentiation into islet like cells [67]. However, further studies are needed to validate its potency in this field.
5 Mode of action of mesenchymal stem cells
MSCs administration has been found to restore normoglycemia in case of diabetes at pre-clinical as well as clinical level. Although, the mechanism involved in therapeutic benefits of MSCs is still poorly understood. Mainly trans-differentiation, immunomodulation, apoptosis prevention, and proliferation/differentiation induction have been found to implicate MSC’s regenerative potential (Fig. 2). In vitro differentiation: In vitro MSCs have been reported to differentiate into β islet cells and restore normoglycemia upon transplantation. The in vivo differentiation of these cells into β islet cells is still skeptical due to very low level of functional integration of transplanted cells in pancreas [68].
Schematic representation of the mechanism of action of mesenchymal stem cells in regeneration process (βME β mercaptoethanol, DMSO dimethyl sulfoxide, HGF hepatocyte growth factor, IDO Indoleamine-pyrrole 2,3-dioxygenase, IL-6 interleukin-6, NO nitric oxide, PGE-2 prostaglandin E, TGF-β transforming growth factor beta, VEGF vascular endothelial growth factor)
5.1 Migration to the site of injury and supporting regeneration and functionality of β cells
MSCs injected via tail vein have been found to reach the pancreas in STZ mice within 7 days and help in regeneration [69]. In addition, these MSCs when injected into NOD-SCID mice and STZ-treated mice have resulted into reduced hyperglycemia by increasing pancreatic islet β cell mass [70,71,72].
5.2 Angiogenesis
Apart from differentiation, paracrine mechanism plays crucial role utilizing several growth factors secreted by MSCs including HGF, Interleukin 6 (IL-6), Transforming growth factor beta (TGF-β), Vascular endothelial growth factor (VEGF), Matrix metalloproteinases (MMPs), Indoleamine-pyrrole 2,3-dioxygenase (IDO), nitric oxide (NO), Programmed death-ligand 1 (PD-1) etc. HGF and Insulin-like growth factor 1 (IGF-1) prevent the apoptosis and stimulate the proliferation of pancreatic beta-cells. In contrast, VEGF and TGF-β have been found to promote islet vascularization [73].
5.3 Immunomodulation
MSCs have been found to suppress T cell proliferation and inhibit dendritic cell differentiation. They interact with immune cells via direct cell to cell contact and secretion of soluble immunomodulatory molecules [74,74,75,76].
6 Clinical studies
Adult Stem Cells have been administered in various disease conditions including myocardial infarction, stroke and diabetes. In a few clinical studies, MSCs-treated with chemical inducers have also been administered. However, in the case of diabetes very few clinical reports have been documented. These studies have been done using fresh MSCs isolated from bone marrow and umbilical cord, with promising results (Table 2). The positive outcomes of these studies have shown ray of hope for such diseases. However, the use of stem cells still needs to be investigated in depth to consolidate the role of stem cells in the treatment of such degenerative diseases.
7 Conclusion
For diabetic treatment, adult stem cells have taken a lead over islet transplantation due to limitations associated with allogenic transplantation and shortage of donors. These cells offer a immense hope for insulin dependent patients. Among these cell types, MSCs are the most desirable candidates due to their ease of isolation, simple preparation, immunomodulatory effect and differentiation into cells of various lineages [83, 84]. These are the most extensively explored stem cell type and have been reported to be administered in maximum clinical trials for various degenerative diseases. The MSCs isolated from different sources have been reported to differentiate into insulin secreting β islet cells using generic differentiation agents like nicotinamide, activin A, exendin-4, etc. Recent studies at driving MSCs to pancreatic cells via same developmental stages that hESCs go through in their differentiation [85] are a significant step forward to establish more robust methods potentially applicable to MSCs isolated from different tissues. These upon transplantation, are supposed to act through various mechanisms including secretion of angiogenic factors, trophic cytokines and growth factors, as well as modulation of inflammatory reactions and immunologic responses [86,87,88,89,90]. Further, MSCs have been transplanted in diabetic mice and rats in undifferentiated as well as differentiated form and have been found to restore glucose metabolism in long term studies. In addition, construction of a three-dimensional artificial matrix has also come up as solution to improve cell viability, act as a carrier for cell transplantation and overcome problem of cell loss upon direct transplantation [91]. However, in clinical settings only undifferentiated BM-MSCs have been administered till date and have found to be safe and effective in case of both T1DM and T2DM. There is an ongoing debate on whether to use allogenic or human leukocyte antigen-matched MSCs for a number of therapies. Although some report the immunoprivilege nature of MSCs, [92, 93] while others claim that upon differentiation MSCs lose their immune privilege [94]. Thus, there is a need for conducting more controlled and randomized trials with larger number of patients to validate the positive results of stem cell treatment noted so far. Moreover, there is a requirement to include parameters like appropriate cell dose, type of stem cell and mode of their administration in order find out the best stem cell approach for human patients. Despite all these challenges, the benefits of stem cell treatment have established them for their clinical prospects and have proven to have potential to significantly improve the lives of millions of people affected with diabetes.
References
Zang L, Hao H, Liu J, Li Y, Han W, Mu Y. Mesenchymal stem cell therapy in type 2 diabetes mellitus. Diabetol Metab Syndr. 2017;9:36.
IDF Diabetes Atlas, 5th edition. International Diabetes Federation. 2011. https://www.idf.org/our-activities/advocacy-awareness/resources-and-tools/20:atlas-5th-edition.html.
Atkinson MA, Eisenbarth GS. Type I diabetes: new perspectives on disease pathogenesis and treatment. Lancet. 2001;358:221–9.
DeFronzo RA. Pathogenesis of type 2 diabetes: metabolic and molecular implications for identifying diabetes genes. Diabetes Rev. 1997;5:177–266.
You WP, Henneberg M. Type 1 diabetes prevalence increasing globally and regionally: the role of natural selection and life expectancy at birth. BMJ Open Diabetes Res Care. 2016;4:e000161.
Madsen OD. Stem cells and diabetes treatment. APMIS. 2005;113:858–75.
Noguchi H. Pancreatic islet transplantation. World J Gastrointest Surg. 2009;1:16–20.
Jamiolkowski RM, Guo LY, Li YR, Shaffer SM, Naji A. Islet Transplantation in Type I Diabetes Mellitus. Yale J Biol Med. 2012;85:37–43.
McCall MD, Toso C, Baetge EE, Shapiro AM. Are stem cells a cure for diabetes? Clin Sci (Lond). 2009;118:87–97.
Assady S, Maor G, Amit M, Itskovitz-Eldor J, Skorecki KL, Tzukerman M. Insulin production by human embryonic stem cells. Diabetes. 2001;50:1691–7.
Hori Y, Rulifson IC, Tsai BC, Heit JJ, Cahoy JD, Kim SK. Growth inhibitors promote differentiation of insulin-producing tissue from embryonic stem cells. Proc Natl Acad Sci U S A. 2002;99:16105–10.
D’souza N, Rossignoli F, Golinelli G, Grisendi G, Spano C, Candini O, et al. Mesenchymal stem/stromal cells as a delivery platform in cell and gene therapies. BMC Med. 2015;13:186.
Sheik Abdulazeez S. Diabetes treatment: a rapid review of the current and future scope of stem cell research. Saudi Pharm J. 2015;23:333–40.
Mohanty S, Jain KG, Nandy SB, Kakkar A, Kumar M, Dinda AK, et al. Iron oxide labeling does not affect differentiation potential of human bone marrow mesenchymal stem cells exhibited by their differentiation into cardiac and neuronal cells. Mol Cell Biochem. 2018. https://doi.org/10.1007/s11010-018-3309-9.
Hardikar AA, Marcus-Samuels B, Geras-Raaka E, Raaka BM, Gershengorn MC. Human pancreatic precursor cells secrete FGF2 to stimulate clustering into hormone-expressing islet-like cell aggregates. Proc Natl Acad Sci U S A. 2003;100:7117–22.
Gao R, Ustinov J, Pulkkinen MA, Lundin K, Korsgren O, Otonkoski T. Characterization of endocrine progenitor cells and critical factors for their differentiation in human adult pancreatic cell culture. Diabetes. 2003;52:2007–15.
Lumelsky N, Blondel O, Laeng P, Velasco I, Ravin R, McKay R. Differentiation of embryonic stem cells to insulin-secreting structures similar to pancreatic islets. Science. 2001;292:1389–94.
Shiroi A, Yoshikawa M, Yokota H, Fukui H, Ishizaka S, Tatsumi K, et al. Identification of insulin-producing cells derived from embryonic stem cells by zinc-chelating dithizone. Stem Cells. 2002;20:284–92.
Kim D, Gu Y, Ishii M, Fujimiya M, Qi M, Nakamura N, et al. In vivo functioning and transplantable mature pancreatic islet-like cell clusters differentiated from embryonic stem cell. Pancreas. 2003;27:e34–41.
Deutsch G, Jung J, Zheng M, Lóra J, Zaret KS. A bipotential precursor population for pancreas and liver within the embryonic endoderm. Development. 2001;128:871–81.
Yang L, Li S, Hatch H, Ahrens K, Cornelius JG, Petersen BE, et al. In vitro trans-differentiation of adult hepatic stem cells into pancreatic endocrine hormone producing cells. Proc Natl Acad Sci U S A. 2002;99:8078–83.
Kodama S, Kühtreiber W, Fujimura S, Dale EA, Faustman DL. Islet regeneration during the reversal of autoimmune diabetes in NOD mice. Science. 2003;302:1223–7.
Vishnubalaji R, Al-Nbaheen M, Kadalmani B, Aldahmash A, Ramesh T. Skin-derived multipotent stromal cells—an archrival for mesenchymal stem cells. Cell Tissue Res. 2012;350:1–12.
Al-Nbaheen M, Vishnubalaji R, Ali D, Bouslimi A, Al-Jassir F, Megges M, et al. Human stromal (mesenchymal) stem cells from bone marrow, adipose tissue and skin exhibit differences in molecular phenotype and differentiation potential. Stem Cell Rev. 2013;9:32–43.
Meirelles Lda S, Nardi NB. Methodology, biology and clinical applications of mesenchymal stem cells. Front Biosci (Landmark Ed). 2009;14:4281–98.
Erices A, Conget P, Minguell JJ. Mesenchymal progenitor cells in human umbilical cord blood. Br J Haematol. 2000;109:235–42.
Gronthos S, Brahim J, Li W, Fisher LW, Cherman N, Boyde A, et al. Stem cell properties of human dental pulp stem cells. J Dent Res. 2002;81:531–5.
Najafzadeh N, Esmaeilzade B, Dastan Imcheh M. Hair follicle stem cells: in vitro and in vivo neural differentiation. World J Stem Cells. 2015;7:866–72.
Baer PC, Geiger H. Adipose-derived mesenchymal stromal/stem cells: tissue localization, characterization, and heterogeneity. Stem Cells Int. 2012;2012:812693.
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8:315–7.
Friedenstein AJ, Gorskaja JF, Kulagina NN. Fibroblast precursors in normal and irradiated mouse hematopoietic organs. Exp Hematol. 1976;4:267–74.
Horwitz EM, Dominici M. How do mesenchymal stromal cells exert their therapeutic benefit? Cytotherapy. 2008;10:771–4.
Price MJ, Chou CC, Frantzen M, Miyamoto T, Kar S, Lee S, et al. Intravenous mesenchymal stem cell therapy early after reperfused acute myocardial infarction improves left ventricular function and alters electrophysiologic properties. Int J Cardiol. 2006;111:231–9.
Lee JS, Hong JM, Moon GJ, Lee PH, Ahn YH, Bang OY. A long-term follow-up study of intravenous autologous mesenchymal stem cell transplantation in patients with ischemic stroke. Stem Cells. 2010;28:1099–106.
Estrada EJ, Valacchi F, Nicora E, Brieva S, Esteve C, Echevarria L, et al. Combined treatment of intrapancreatic autologous bone marrow stem cells and hyperbaric oxygen in type 2 diabetes mellitus. Cell Transplant. 2008;17:1295–304.
Kang SK, Shin MJ, Jung JS, Kim YG, Kim CH. Autologous adipose tissue-derived stromal cells for treatment of spinal cord injury. Stem Cells Dev. 2006;15:583–94.
Cheng SK, Park EY, Pehar A, Rooney AC, Gallicano GI. Current progress of human trials using stem cell therapy as a treatment for diabetes mellitus. Am J Stem Cells. 2016;5:74–86.
Kao SY, Shyu JF, Wang HS, Lin CH, Su CH, Chen TH, et al. Comparisons of differentiation potential in human mesenchymal stem cells from Wharton’s jelly, bone marrow, and pancreatic tissues. Stem Cells Int. 2015;2015:306158.
Oh SH, Muzzonigro TM, Bae SH, LaPlante JM, Hatch HM, Petersen BE. Adult bone marrow-derived cells trans-differentiating into insulin-producing cells for the treatment of type I diabetes. Lab Invest. 2004;84:607–17.
Chen LB, Jiang XB, Yang L. Differentiation of rat marrow mesenchymal stem cells into pancreatic islet beta-cells. World J Gastroenterol. 2004;10:3016–20.
Tang DQ, Cao LZ, Burkhardt BR, Xia CQ, Litherland SA, Atkinson MA, et al. In vivo and in vitro characterization of insulin-producing cells obtained from murine bone marrow. Diabetes. 2004;53:1721–32.
Abouzaripour M, Pasbakhsh P, Atlasi N, Shahverdi AH, Mahmoudi R, Kashani IR. In vitro differentiation of insulin secreting cells from mouse bone marrow derived stage-specific embryonic antigen 1 positive stem cells. Cell J. 2016;17:701–10.
Paz AH, Salton GD, Ayala-Lugo A, Gomes C, Terraciano P, Scalco R, et al. Betacellulin overexpression in mesenchymal stem cells induces insulin secretion in vitro and ameliorates streptozotocin-induced hyperglycemia in rats. Stem Cells Dev. 2011;20:223–32.
Gabr MM, Sobh MM, Zakaria MM, Refaie AF, Ghoneim MA. Transplantation of insulin-producing clusters derived from adult bone marrow stem cells to treat diabetes in rats. Exp Clin Transplant. 2008;6:236–43.
Zanini C, Bruno S, Mandili G, Baci D, Cerutti F, Cenacchi G, et al. Differentiation of mesenchymal stem cells derived from pancreatic islets and bone marrow into islet-like cell phenotype. PLoS One. 2011;6:e28175.
Gerace D, Martiniello-Wilks R, Nassif NT, Lal S, Steptoe R, Simpson AM. CRISPR-targeted genome editing of mesenchymal stem cell-derived therapies for type 1 diabetes: a path to clinical success? Stem Cell Res Ther. 2017;8:62.
Karnieli O, Izhar-Prato Y, Bulvik S, Efrat S. Generation of insulin-producing cells from human bone marrow mesenchymal stem cells by genetic manipulation. Stem Cells. 2007;25:2837–44.
Bassi ÊJ, Moraes-Vieira PM, Moreira-Sá CS, Almeida DC, Vieira LM, Cunha CS, et al. Immune regulatory properties of allogeneic adipose-derived mesenchymal stem cells in the treatment of experimental autoimmune diabetes. Diabetes. 2012;61:2534–45.
Klinker MW, Wei CH. Mesenchymal stem cells in the treatment of inflammatory and autoimmune diseases in experimental animal models. World J Stem Cells. 2015;7:556–67.
Lin G, Wang G, Liu G, Yang LJ, Chang LJ, Lue TF, et al. Treatment of type 1 diabetes with adipose tissue-derived stem cells expressing pancreatic duodenal homeobox 1. Stem Cells Dev. 2009;18:1399–406.
De Ugarte DA, Alfonso Z, Zuk PA, Elbarbary A, Zhu M, Ashjian P, et al. Differential expression of stem cell mobilization associated-molecules on multi lineage cells from adipose tissue and bone marrow. Immunol Lett. 2003;89:267–70.
Timper K, Seboek D, Eberhardt M, Linscheid P, Christ-Crain M, Keller U, et al. Human adipose tissue-derived mesenchymal stem cells differentiate into insulin, somatostatin, and glucagon expressing cells. Biochem Biophys Res Commun. 2006;341:1135–40.
Dave SD, Vanikar AV, Trivedi HL. Extrinsic factors promoting in vitro differentiation of insulin-secreting cells from human adipose tissue-derived mesenchymal stem cells. Appl Biochem Biotechnol. 2013;170:962–71.
Li J, Zhu L, Qu X, Li J, Lin R, Liao L, et al. Stepwise differentiation of human adipose-derived mesenchymal stem cells toward definitive endoderm and pancreatic progenitor cells by mimicking pancreatic development in vivo. Stem Cells Dev. 2013;22:1576–87.
Trivedi HL, Vanikar AV, Thakker U, Firoze A, Dave SD, Patel CN, et al. Human adipose tissue-derived mesenchymal stem cells combined with hematopoietic stem cell transplantation synthesize insulin. Transplant Proc. 2008;40:1135–9.
Marappagounder D, Somasundaram I, Dorairaj S, Sankaran RJ. Differentiation of mesenchymal stem cells derived from human bone marrow and subcutaneous adipose tissue into pancreatic islet-like clusters in vitro. Cell Mol Biol Lett. 2013;18:75–88.
Kajiyama H, Hamazaki TS, Tokuhara M, Masui S, Okabayashi K, Ohnuma K, et al. Pdx1-transfected adipose tissue-derived stem cells differentiate into insulin-producing cells in vivo and reduce hyperglycemia in diabetic mice. Int J Dev Biol. 2010;54:699–705.
Kadam S, Muthyala S, Nair P, Bhonde R. Human placenta-derived mesenchymal stem cells and islet-like cell clusters generated from these cells as a novel source for stem cell therapy in diabetes. Rev Diabet Stud. 2010;7:168–82.
Sun NZ, Ji HS. In vitro differentiation of human placenta-derived adherent cells into insulin-producing cells. J Int Med Res. 2009;37:400–6.
Gao F, Wu DQ, Hu YH, Jin GX, Li GD, Sun TW, et al. In vitro cultivation of islet-like cell clusters from human umbilical cord blood-derived mesenchymal stem cells. Transl Res. 2008;151:293–302.
Harris DT, Rogers I. Umbilical cord blood: a unique source of pluripotent stem cells for regenerative medicine. Curr Stem Cell Res Ther. 2007;2:301–9.
Pessina A, Eletti B, Croera C, Savalli N, Diodovich C, Gribaldo L. Pancreas developing markers expressed on human mononucleated umbilical cord blood cells. Biochem Biophys Res Commun. 2004;323:315–22.
Sun B, Roh KH, Lee SR, Lee YS, Kang KS. Induction of human umbilical cord blood-derived stem cells with embryonic stem cell phenotypes into insulin producing islet-like structure. Biochem Biophys Res Commun. 2007;354:919–23.
Gao F, Wu DQ, Hu YH, Jin GX. Extracellular matrix gel is necessary for in vitro cultivation of insulin producing cells from human umbilical cord blood derived mesenchymal stem cells. Chin Med J (Engl). 2008;121:811–8.
Polgár K, Adány R, Abel G, Kappelmayer J, Muszbek L, Papp Z. Characterization of rapidly adhering amniotic fluid cells by combined immunofluorescence and phagocytosis assays. Am J Hum Genet. 1989;45:786–92.
Priest RE, Marimuthu KM, Priest JH. Origin of cells in human amniotic fluid cultures: ultrastructural features. Lab Invest. 1978;39:106–9.
Trovato L, De Fazio R, Annunziata M, Sdei S, Favaro E, Ponti R, et al. Pluripotent stem cells isolated from human amniotic fluid and differentiation into pancreatic beta-cells. J Endocrinol Invest. 2009;32:873–6.
Ezquer F, Ezquer M, Contador D, Ricca M, Simon V, Conget P. The antidiabetic effect of mesenchymal stem cells is unrelated to their transdifferentiation potential but to their capability to restore Th1/Th2 balance and to modify the pancreatic microenvironment. Stem Cells. 2012;30:1664–74.
Sordi V, Malosio ML, Marchesi F, Mercalli A, Melzi R, Giordano T, et al. Bone marrow mesenchymal stem cells express a restricted set of functionally active chemokine receptors capable of promoting migration to pancreatic islets. Blood. 2005;106:419–27.
Lee RH, Seo MJ, Reger RL, Spees JL, Pulin AA, Olson SD, et al. Multipotent stromal cells from human marrow home to and promote repair of pancreatic islets and renal glomeruli in diabetic NOD/scid mice. Proc Natl Acad Sci U S A. 2006;103:17438–43.
Bell GI, Broughton HC, Levac KD, Allan DA, Xenocostas A, Hess DA. Transplanted human bone marrow progenitor subtypes stimulate endogenous islet regeneration and revascularization. Stem Cells Dev. 2012;21:97–109.
Ezquer FE, Ezquer ME, Parrau DB, Carpio D, Yañez AJ, Conget PA. Systemic administration of multipotent mesenchymal stromal cells reverts hyperglycemia and prevents nephropathy in type I diabetic mice. Biol Blood Marrow Transplant. 2008;14:631–40.
Davis NE, Hamilton D, Fontaine MJ. Harnessing the immunomodulatory and tissue repair properties of mesenchymal stem cells to restore β cell function. Curr Diab Rep. 2012;12:612–22.
Jurewicz M, Yang S, Augello A, Godwin JG, Moore RF, Azzi J, et al. Congenic mesenchymal stem cell therapy reverses hyperglycemia in experimental type 1 diabetes. Diabetes. 2010;59:3139–47.
Abdi R, Fiorina P, Adra CN, Atkinson M, Sayegh MH. Immunomodulation by mesenchymal stem cells: a potential therapeutic strategy for type 1 diabetes. Diabetes. 2008;57:1759–67.
Yagi H, Soto-Gutierrez A, Parekkadan B, Kitagawa Y, Tompkins RG, Kobayashi N, et al. Mesenchymal stem cells: mechanisms of immunomodulation and homing. Cell Transplant. 2010;19:667–79.
Carlsson PO, Schwarcz E, Korsgren O, Le Blanc K. Preserved beta-cell function in type 1 diabetes by mesenchymal stromal cells. Diabetes. 2015;64:587–92.
Cai J, Wu Z, Xu X, Liao L, Chen J, Huang L, et al. Umbilical cord mesenchymal stromal cell with autologous bone marrow cell transplantation in established type 1 diabetes: a pilot randomized controlled open-label clinical study to assess safety and impact on insulin secretion. Diabetes Care. 2016;39:149–57.
Hu J, Yu X, Wang Z, Wang F, Wang L, Gao H, et al. Long term effects of the implantation of Wharton’s jelly-derived mesenchymal stem cells from the umbilical cord for newly-onset type 1 diabetes mellitus. Endocr J. 2013;60:347–57.
Zhao Y. Stem cell educator therapy and induction of immune balance. Curr Diab Rep. 2012;12:517–23.
Zhao Y, Jiang Z, Zhao T, et al. Reversal of type 1 diabetes via islet beta cell regeneration following immune modulation by cord blood-derived multipotent stem cells. BMC Med. 2012;10:3.
Delgado E, Perez-Basterrechea M, Suarez-Alvarez B, Zhou H, Revuelta EM, Garcia-Gala JM, et al. Modulation of autoimmune T-cell memory by stem cell educator therapy: phase 1/2 clinical trial. EBioMedicine. 2015;2:2024–36.
Wei X, Yang X, Han ZP, Qu FF, Shao L, Shi YF. Mesenchymal stem cells: a new trend for cell therapy. Acta Pharmacol Sin. 2013;34:747–54.
Chhabra P, Brayman KL. Stem cell therapy to cure type 1 diabetes: from hype to hope. Stem Cells Transl Med. 2013;2:328–36.
Prabakar KR, Dominguez-Bendala J, Molano RD, Pileggi A, Villate S, Ricordi C, et al. Generation of glucose-sensitive, insulin-producing cells from human umbilical cord blood-derived mesenchymal stem cells. Cell Transplant. 2012;21:1321–39.
Uccelli A, Pistoia V, Moretta L. Mesenchymal stem cells: a new strategy for immunosuppression? Trends Immunol. 2007;28:219–26.
Keating A. Mesenchymal stromal cells. Curr Opin Hematol. 2006;13:419–25.
Prockop DJ. “Stemness” does not explain the repair of many tissues by mesenchymal stem/multipotent stromal cells (MSCs). Clin Pharmacol Ther. 2007;82:241–3.
Deans RJ, Moseley AB. Mesenchymal stem cells: biology and potential clinical uses. Exp Hematol. 2000;28:875–84.
Dazzi F, Horwood NJ. Potential of mesenchymal stem cell therapy. Curr Opin Oncol. 2007;19:650–5.
Kaviani M, Negar Azarpira N. Insight into microenvironment remodeling in pancreatic endocrine tissue engineering: biological and biomaterial approaches. Tissue Eng Regen Med. 2016;13:475–84.
Uccelli A, Moretta L, Pistoia V. Immunoregulatory function of mesenchymal stem cells. Eur J Immunol. 2006;36:2566–73.
Hare JM, Traverse JH, Henry TD, Dib N, Strumpf RK, Schulman SP, et al. A randomized, double-blind, placebo-controlled, dose-escalation study of intravenous adult human mesenchymal stem cells (prochymal) after acute myocardial infarction. J Am Coll Cardiol. 2009;54:2277–86.
Huang XP, Sun Z, Miyagi Y, McDonald Kinkaid H, Zhang L, Weisel RD, et al. Differentiation of allogeneic mesenchymal stem cells induces immunogenicity and limits their long term benefits for myocardial repair. Circulation. 2010;122:2419–29.
Acknowledgements
The authors are grateful to the Datt Mediproducts Pvt. Ltd. for supporting their current research. We sincerely thank Dr. Rajan Datt for valuable scientific discussion.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interests.
Ethical statement
There are no animal expreiments carried out for this article.
Rights and permissions
About this article
Cite this article
Kakkar, A., Sorout, A., Tiwari, M. et al. Current Status of Stem Cell Treatment for Type I Diabetes Mellitus. Tissue Eng Regen Med 15, 699–709 (2018). https://doi.org/10.1007/s13770-018-0143-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13770-018-0143-9