Abstract
Hypoxia suppresses osteoblastic differentiation and the bone-forming capacity. As the leading osteoinductive growth factor used clinically in bone-related regenerative medicine, recombinant human bone morphogenic protein-2 (rhBMP-2) has yielded promising results in unfavorable hypoxic clinical situations. Although many studies have examined the effects of rhBMP-2 on osteoblastic differentiation, mineralization and the related signaling pathways, those of rhBMP-2 on osteoblastic cells remain unknown, particularly under hypoxic conditions. Therefore, this study was conducted under a 1% oxygen tension to examine the differentiating effects of rhBMP-2 on osteoblastic cells under hypoxia. rhBMP-2 could also induce the differentiation and mineralization of Osteoblastic (MC3T3-E1) cells under 1% hypoxic conditions. rhBMP-2 could also induce the differentiation and mineralization of MC3T3-E1 cells under 1% hypoxic conditions. rhBMP-2 increased the alkaline phosphatase {ALP} activity in a time dependent manner, and expression of ALP, collagen type-1 (Col-1) and osteocalcin (OC) mRNA were up-regulated significantly in a time- and concentration-dependent manner. In addition, the area of the mineralized nodules increased gradually in a concentration-dependent manner. Western blot analysis, which was performed to identify the signaling pathways underlying rhBMP-2-induced osteoblastic differentiation under hypoxic conditions, showed that rhBMP-2 significantly promoted the phosphorylation of the p38 mitogen-activated protein kinase (MAPK) in a time-dependent manner. A pretreatment with SB203580, a p38 MAPK inhibitor, inhibited the rhBMP-2-mediated differentiation and mineralization. Moreover, the phosphorylation of p38 induced by rhBMP-2 was inhibited in response to a pretreatment of the cells with Go6976, a protein kinase D {PKD) inhibitor. These findings suggest that rhBMP-2 induces the differentiation and mineralization of MC3T3-E1 cells under hypoxic conditions via activation of the PKD and p38 MAPK signaling pathways.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
The O2 tension in healthy tissues is generally between 2.5-9% oxygen. On the other hand, a disruption of the blood supply to diseased or damaged tissues can result in multiple transient or chronic hypoxic microenvironments, where the O2 tensions can be as low as <1% oxygen [1]. Given that a vascular interruption following a bony and soft tissue injury causes a transient hypoxic gradient within the wound, hypoxia can occur in bone fractures [2] and within the bone graft sites [3]. This is prevalent in situations, such as aging [4], inflammation [1] and diabetes [5]. Hypoxia affects osteoblast proliferation and mineralization by regulating the expression of many genes in osteoblasts, bone-forming cells, and consequently plays an important role in the bone pathophysiology. The effects of a low oxygen tension on the genes involved in osteoblast proliferation and differentiation is controversial and a wide range of responses have been reported [6,7,8]. Generally, osteoblasts and their differentiation tends to be inhibited by hypoxia [9, 10].
To enhance new bone formation and bone repair, osteoinductive proteins, such as bone morphogenetic proteins (BMPs), have been used in a variety of challenging clinical situations in orthopedics and oral and maxillofacial surgery, such as spine surgery, bisphosphonate-associated osteonecrosis of the jaw, vertical bone augmentation in dental implantology, periodontology, and tumor reconstructive surgery [11,12,13]. Since Urist first described the bone inductive proteins isolated from the demineralized bone matrix [14], more than 30 members of the BMP family have been identified, and recombinant deoxyribonucleic acid technology has allowed the production of recombinant human BMP-2 (rhBMP-2) and recombinant human BMP-7 (rhBMP-7) in large quantities. Among these, rhBMP-2 has very high osteogenic activity and promotes bone repair in a range of situations according to various preclinical [15,16,17,18] and clinical studies [19, 20].
BMPs play an important role in osteoblast differentiation and bone remodeling by inducing different signaling pathways in the cells. The BMP signaling pathways are mediated primarily by Smad proteins [21]. Other non-Smad signaling pathways, such as the mitogen-activated protein(MAP) kinase super family are also involved in osteoblastogenesis [22,23,24]. Lemonnier et al. [25] indicated the possible mediators between BMP receptors and MAPKs and suggested the involvement of protein kinase D(PKD) in the activation of c-Jun N-terminal kinases(JNK) and p38 induced by BMP-2. Many studies have examined the effects of rhBMP-2 on osteoblastic differentiation, mineralization and the related signaling pathways [23, 25,26,27,28]. On the other hand, the effects of rhBMP-2 on osteoblastic cells under hypoxic conditions, which clinicians encounter frequently in clinical situations requiring bone regeneration and repair, as well as the precise molecular mechanisms underlying these effects are unknown.
Therefore, this study examined the effects of rhBMP-2 on the differentiation and mineralization of mouse preosteoblastic MC3T3-E1 cells under hypoxic conditions and their underlying pathways.
2 Materials and methods
2.1 Cell culture
This study was exempted ethical approval and consent because of using commercial cell line. MC3T3-E1 cells, a murine osteoblastic cell line, were purchased from the American Type Culture Collection (ATCC) (Rockville, MD, USA). The MC3T3-E1 cells were cultured in α-minimal essential medium (α-MEM)(Gibco BL, Gland island, NY, USA) with 10% fetal bovine serum (FBS) and 1% penicillin–streptomycin, and incubated in a humid incubator at 37 °C, 95% O2 and 5% CO2.
2.2 Differentiation under hypoxic conditions
For osteoblast differentiation, the MC3T3-E1 cells were seeded onto a 24-well plate or 100 mm culture dish and allowed to reach confluence. At confluence (day 0), the cells were induced with osteogenic medium, which was comprised of the above growth medium supplemented with 10 mM β-glycerophosphate and 50 μg/ml ascorbic acid. The cells were transferred to a hypoxic chamber (Anaerobic System PROOX model 110; BioSpherix, Lacona, NY, USA) with 95% N2 and 5% CO2 at 37 °C. The osteogenic media were replaced every 2–3 days. The cells were then incubated within the chamber for different time intervals (1, 3, 7, and 14 days). The cells were exposed to a 1% oxygen tension. The rhBMP-2 (Cowellmedi, Pusan, Korea) and p38 MAPK and PKD inhibitors (SB203580, Go6976) (Calbiochem, San Diego, CA, USA) were dissolved in D.W and DMSO, and then diluted 1000-fold with the cell culture medium. rhBMP-2 was then added to the medium at different concentrations. The final working concentration was 100 ng/ml for rhBMP-2.
2.3 Alkaline phosphatase (ALP) assay
The MC3T3-E1 cells (2 × 105) were plated in 24-well plates and cultured in the osteogenic media for 1 day, and then treated with or without rhBMP-2. The medium and rhBMP-2 were renewed every 3 days. After the treatment with rhBMP-2 at the required dose and time, the cells were washed twice with phosphate-buffered saline (PBS). Subsequently, lysis buffer 500 μL (10 mMTris-HCl (pH 7.5), 0.5 mM MgCl2, 0.1% Triton-X) was added and the resulting mixture was sonicated on ice to lyse the cells. The protein concentrations were measured using the Bradford protein assay. The final concentration of the protein used in this work was 50 μg. The lysates were incubated with 200 μL ALP reaction buffer [25 mM Glycine (pH 9.4), 0.1% Triton X-100, 2 mM MgCl2, and 5mMp-nitrophenyl phosphate] for 1 h at 37 °C. The reaction was quenched using 200μL of 1 M NaOH, and the ALP activity was measured from the optical absorbance at 405 nm using a microplate reader.
2.4 Alizarin red S staining for mineralization analysis
The mineralization of MC3T3-E1 cells was determined by Alizarin Red staining. The cells were grown in osteogenic media and treated with rhBMP-2 for 7 - 14 days. The differentiation medium and rhBMP-2 were changed every 3 days. The cells were fixed with 70% ethanol for 1 h, washed 3 times with distilled water, and then stained with 1% Alizarin Red S (Sigma, Louis, Mo, USA) solution (pH 4.2) for 10 min. The cells were then washed 3 times with distilled water. To quantify the level of calcium deposition, the cells were destained with 10% cetylpyridinium chloride (Sigma, Louis, Mo, USA) and transferred to a 96-well plate, and the absorbance was measured at 550 nm using a microplate reader, as described previously.
2.5 Western blot assay
The cells (2 × 106) were plated in 100 mm culture dishes. After 24 h, the cultured cells were treated with rhBMP-2 and/or a combination treatment of sb203580 and Go6976. The cells were incubated in RIPA buffer (Cell Signaling Technology, Danvers, MA, USA) at 4 °C for 1 h. The cells were then centrifuged at 14 000 rpm for 30 min at 4 °C and the protein extract of the cells was transferred. The protein concentrations were determined using a Bio-Rad Protein Assay Kit (Bio-Rad, Richmond, CA, USA). Equal amounts of protein (20 μg) were separated by 10%SDS polyacrylamide gel electrophoresis (SDS-PAGE) gels and transferred to polyvinylidene fluoride (PVDF) membranes (Millipore, CA, USA). The PVDF membranes were blocked with 5% fat-free dry milk in PBS for 1 h. The membranes were incubated overnight with the primary antibodies for ATF2, phosphor-ATF2, p38MAPK, phospho-p38 MAPK, PKD/PKCμ, and phospho-PKD/PKCμ (Cell signaling, Beverly, MA, USA). After incubation, the membranes were developed using SuperSignal West Femto enhanced chemiluminescence Western blotting detection reagent (Pierce, Rockford, IL, USA)., and the bands were exposed and analyzed using an Alpha Imager HP (Alpha Innotech, Santa Clara, CA, USA).
2.6 Real-time RT-PCR
The total RNA was prepared from the cultured MC3T3-E1 cells using a Trizol reagent (Invitrogen, San Diego, CA, USA) according to the manufacturer’s instruction. The RNA concentration was measured by NanoDrop 1000 (Thermo Fisher Scientific, Wilmington, DE, USA) and cDNA was synthesized from 1 μg of the total RNA using a PrimeScript RT reagent kit (Takara Bio, Shiga, Japan). qPCR was conducted on an ABI 7500 Fast Real-Time PCR System (Applied Biosystems 7500 System, Foster City, CA, USA; with Sequence Detection System(SDS) software version 2.0.1) using a SYBR Green PCR Master Mix (Applied Biosystems, Foster City, CA, USA). The sense and antisense primers used were as follows: mouse Alp sense, 5′-GACTGGTACTCGGATAACGAGA-3′ and antisense, 5′-CTCATGATGTCCGTGGTCAATC-3′; mouse Col1 sense, 5′-ACCTCCCAGTGGCGGTTATGAC-3′ and antisense, 5′-AGTTCTTCTGAGGCACAGACGG-3′. The change from the control values was set to 1-fold, and the fold change relative to the control values was obtained and used to express the change in gene expression.
2.7 Statistical analysis
The results are representative of at least 3 independent experiments and are expressed as the mean ± SEM. All data was analyzed using GraphPad Prism software (GraphPad Prism, Version 5, San Diego, CA). One-way ANOVA models were used to compare the expression levels using a Dunnett’s multiple comparison test as a post hoc analysis. The significance level was set to 0.05.
3 Results
3.1 Effects of rhBMP-2 on the differentiation and mineralization of hypoxic MC3T3-E1 cells
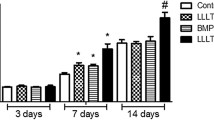
Osteoblast markers, such as ALP, Col-1 and OC, and the ALP activity were examined after 1, 3, 7, and 14 days of treatment with 0-500 ng/mL of rhBMP-2 to evaluate the differentiating effect of rhBMP-2 on the osteoblastic cells under hypoxia (Figs. 1, 2). rhBMP-2 time-dependently increased the ALP activity (P < 0.001), which gradually increased until day 14. The expression of ALP, Col-1 and OC mRNA were up-regulated significantly in a time- and concentration-dependent manner (P < 0.001). Moreover, as shown in Fig. 3, the area of the mineralized nodules, which was positively stained, increased gradually in a concentration-dependent manner after 14 days of culture by Alizarin red S staining.(P < 0.01) These results confirmed the previously demonstrated osteoinductive potential of rhBMP-2 and suggested that it can also stimulate the differentiation of osteoblastic cells, even under hypoxic conditions.
Effects of rhBMP-2 on the ALP activity of MC3T3-E1 cells under hypoxic conditions. MC3T3-E1 cells were cultured in osteogenic medium containing various concentrations (0, 10, 50, 100, 250 and 500 ng/ml) of rhBMP-2, as indicated, for 1, 3, 7, and 14 days, under hypoxic conditions. The ALP activity in the lysates of these cells was then determined by an enzymatic assay. rhBMP-2 time-dependently promoted the ALP activity (p < .001). On the other hand, there was no significant correlation between the ALP activity and concentration of rhBMP-2. Each value represents the mean ± SEM of the fold increase over the control
Effect of rhBMP-2 on the expression of the differentiation markers of MC3T3-E1 cells under hypoxic conditions. The cells were treated with increasing concentrations (0, 10, 50, 100, 250 and 500 ng/ml) of rhBMP-2, as indicated, for 1, 3, 7, and 14 days, under hypoxic conditions. The total mRNA of ALP, Col-1 and OC was collected on days 1, 3, 7, and 14 from hypoxic cultured cells and the gene expression was determined by a real-time reverse transcription-polymerase chain reaction. A-C Each value represents the mean ± SEM of the fold increase over the control
Effect of rhBMP-2 on the mineralization of MC3T3-E1 cells under hypoxic conditions A, B. The cells were cultured in osteogenic medium containing different concentrations (0, 10, 50, 100, 250 and 500 ng/ml) of rhBMP-2 for 14 days. The formation of mineralized nodules was then observed by Alizarin red S staining. Quantification of Alizarin red S staining was performed after extraction with ethylpyridium chloride. Each value represents the mean ± SEM of the fold increase over the control. *P < 0.01, **p < 0.001, ***p < 0.0001
3.2 rhBMP-2 induces the differentiation and mineralization of hypoxic MC3T3-E1 cells via the p38 MAPK pathway
The signaling pathway underlying the differentiation effects of rhBMP-2 in MC3T3-E1 cells was examined under hypoxic conditions. When the hypoxic cells were treated with 100 ng/mL rhBMP-2 for 120 min, the phosphorylation of p38 MAPK was promoted in a time-dependent manner (Fig. 4A). To confirm that rhBMP-2-mediated osteoblast differentiation and mineralization resulted from the activation of p38 MAPK, a pharmacological study using a p38 MAPK inhibitor (SB203580) was induced. In the presence of SB203580, the phosphorylation of activating transcription factor 2(ATF 2), a specific target protein for p38 MAPK, was blunted significantly (Fig. 4B). In addition, the ALP activity, BMP-2-induced differentiation markers expression (ALP, Col-1 OC) and the formation of mineralized nodules were inhibited when pretreated with SB203580 (Fig. 4C, D, E). Therefore, the p38 MAPK pathway may be essential for the rhBMP-2-mediated differentiation of hypoxic MC3T3-E1 cells.
Effects of rhBMP-2 on the activation of p38 in MC3T3-E1 cells under hypoxic conditions. A The cells were treated with 100 ng/ml of rhBMP-2 for up to 120 min. This enhanced time-dependently phosphorylation of p38 MAPK. B The cells were pretreated with 10 or 20 μM of SB203580, a p38 MAPK inhibitor, for 2 h, exposed to 100 ng/ml of rhBMP-2 for 1 h, and the levels of the phosphorylated form of ATF2, a p38 target protein, were then determined by Western blot analysis. GAPDH served as a reference protein. C-E The cells were cultured in osteogenic medium containing 0 or 100 ng/ml of rhBMP-2, in the absence or presence of SB203580 for 14 days. C The formation of mineralized nodules was observed by staining with Alizarin Red S, which was then quantified after extraction with ethylpyridium chloride. D The ALP activity in the lysates of these cells were then determined by an enzymatic assay. E The expression of the osteogenesis-associated mRNAs was determined. Each value represents the mean ± SEM of the fold-change increase over the control. *p < 0.01
3.3 rhBMP-2 activates p38 MAPK via the PKD pathway in hypoxic MC3T3-E1 cells
Previous studies have reported that PKD participate in the BMP-2-mediated osteoblastic cell differentiation by activating MAPKs. Therefore, this study examined the involvement of PKD in the effect of rhBMP-2 on the differentiation of MC3T3-E1 cells under hypoxic conditions. rhBMP-2 time-dependently stimulated the phosphorylation of PKD and p38, which was inhibited by pretreating the cells with Go6976, a PKD inhibitor (Fig. 5A, B). In addition, the rhBMP-2-mediated induction of the osteoblast marker genes, ALP activity and the formation of mineralized crystals were all inhibited by Go6976 (Fig. 5C, D, E). These results suggest that rhBMP-2 can induce the differentiation of MC3T3-E1 cells by activating the PKD and p38 signaling pathways.
Effects of rhBMP-2 on the activation of the signaling molecules in MC3T3-E1 cells under hypoxic conditions. A The cells were treated with 100 ng/ml of rhBMP-2 for up to 120 min. This enhanced phosphorylation of p38 and PKD in a time-dependent manner. B The cells were pretreated with 10 or 20 μM of Go6976, a PKD inhibitor, for 2 h, exposed to 100 ng/ml of rhBMP-2 for 1 h, and the levels of the phosphorylated form of p38 and PKD were then determined by Western blot analysis. GAPDH served as a reference protein. C-E The cells were incubated in osteogenic medium containing 0 or 100 ng/ml of rhBMP-2, in the absence or presence of Go6976 for 14 days. C The formation of mineralized nodules was observed by staining with Alizarin Red S, which was then quantified after extraction with ethylpyridium chloride. D The ALP activity in the lysates of these cells was then determined by an enzymatic assay. E The expression of the osteogenesis-associated mRNAs was determined. Each value represents the mean ± SEM of the fold-change increase over the control. *p < 0.01
4 Discussion
rhBMP-2 is one of the most researched and published therapeutic growth factors that have been approved to enhance the growth of bone for the clinical use for orthopedic and craniofacial indications using several different carrier technologies. In addition, it has become the leading osteoinductive growth factor used clinically in bone-related regenerative medicine. Although several studies have shown that BMP-2 stimulates osteoblastic differentiation in vitro [29,30,31], they were conducted under normoxic conditions. The effects of BMP-2 on osteoblastic differentiation and mineralization under hypoxic conditions is unknown. Furthermore, rhBMP-2 has yielded promising results in a variety of clinical scenarios, some of which are expected to be hypoxic conditions. Therefore, the differentiation effects of rhBMP-2 on MC3T3-E1 cells under 1% hypoxic conditions, which are analogous to the oxygen tension observed in a bone and soft tissue injury [32], and the related signaling mechanisms were evaluated.
The ALP activity, which is a marker of early osteoblastic differentiation, increased gradually throughout the experimental period and reached its highest value on day 14. The levels of ALP, OC, and Col-1 mRNA expression were increased in a time- and concentration-dependent manner. In particular, after a 24 h treatment of rhBMP-2 in hypoxic MC3T3-E1 cells, it potentially induced the expression of these osteogenic genes and ALP activity. This early gene induction indicates that rhBMP-2 may stimulate early osteoblast differentiation. Alizarin Red staining showed that the mineralized area in hypoxic MC3T3-E1 cells was formed in a concentration-dependent manner by rhBMP-2 on day 14. Calcium deposition is used widely as a marker for the late differentiation of osteoblast cells, which indicates that BMP-2 can also promote late osteoblast differentiation. Overall, these results suggest that rhBMP-2 stimulates the maturation and function of osteoblasts by regulating early and late osteoblast differentiation, even under hypoxic conditions.
In the present study, the expression of osteogenesis-associated mRNAs and the area of mineralized nodules increased significantly with increasing rhBMP-2 concentration. The concentration of rhBMP-2 is one of several factors influencing the osteoinductive ability of rhBMP-2 with the possible presence of inhibitors, type of carrier, duration of BMP action, recipient site [33,34,35]. The combination of rhBMP-2 and an absorbable collagen sponge at a 1.5-mg/cc concentration (INFUSE® Bone Graft, Medtronic Spinal and Biologics, Memphis, TN) was FDA-approved for a range of clinical situations in orthopedics and oral and maxillofacial surgery. In the bone graft procedure, BMP-2 is needed at supraphysiologic doses to enhance bone regeneration. The concentration of naturally occurring BMP within the human bone matrix is 1 μg/g bone, which is several orders of magnitude lower than the concentrations applied in clinical studies. Several studies have reported an inverse correlation between the quality of newly formed bone induced by rhBMP-2 and its dose [36,37,38,39]. In addition, using high doses of rhBMP-2 in clinical use may contribute to numerous adverse effects, including cyst-like bone formation, severe tissue inflammation and cervical swelling [40], and osteoclast activation with transiently elevated bone resorption [41]. Cyst-like bone formation, which is diagnosed as a seroma, is observed particularly frequently when high doses of rhBMP-2 required for human bone regeneration are applied [42]. This can be explained on a molecular level, based on published reports showing that osteogenesis and adipogenesis can be induced simultaneously by BMP-2 [43]. This unexpected phenomenon can promote the potentially inferior mechanical properties of the newly formed bone tissue. Therefore, the optimal dose to both enhance bone regeneration and minimize the side effects of rhBMP-2 should be determined.
Both Smads and MAPK pathways are essential components in BMP-2-mediated osteoblast differentiation [21,22,23,24]. MAPKs are involved in the cellular response to growth factors, cytokines, or environmental stress and control many cellular events, including cell proliferation, differentiation, and cell death. They include extra cellular signal-regulated kinase (ERK), p38 kinase and c-Jun N-terminal kinase (JNK). Several studies have demonstrated that p38 plays a crucial role in osteoblast differentiation mediated by BMP-2 [23, 25,26,27,28].. In addition, it plays an important role in the cellular responses to stress stimuli, such as cytokines, ultraviolet irradiation, heat shock, and osmotic shock. Therefore, this study examined the involvement of p38 MAPK in the rhBMP-2-induced differentiation of MC3T3-E1 cells under hypoxic conditions. rhBMP-2 could phosphorylate p38 MAPK in hypoxic MC3T3-E1 cells in a time-dependent manner using a western blot assay.(Fig. 4A) In addition, the rhBMP-2-induced differentiation and mineralization of hypoxic MC3T3-E1 cells was reversed in the presence of SB203580, a specific p38 MAPK inhibitor. These results suggest that p38 MAPK plays an important role in the differentiating effect of rhBMP-2 on MC3T3-E1 cells under hypoxic conditions.
PKD is involved in fundamental biological processes, such as signal transduction, membrane trafficking and cell survival, migration, differentiation, and proliferation. Previous studies reported that PKD is required for the differentiating effect of BMP-2 on osteoblastic cells, and the activation of PKD induced by BMP-2 is involved in osteoblastic cell differentiation by activating the MAPK pathways [25, 28]. In the present study, rhBMP-2 up-regulated the phosphorylation of PKD under hypoxic conditions. G06976, a PKD inhibitor blocked the activation of p38 and the phosphorylation of PKD induced by BMP-2. Moreover, when the cells were treated with G06976, rhBMP-2-induced mineralization, expression of the differentiation marker and ALP activity were all suppressed significantly. These results indicate that BMP-2 can induce the activation of PKD in osteoblastic cells and that this kinase is involved in the activation of p38 induced by BMP-2. Therefore, this pathway appears to be essential to the differentiation effect of BMP-2 in hypoxic MC3E3-T1 cells.
In summary, these results suggest that BMP-2 promotes the differentiation and mineralization of osteoblastic MC3T3-E1 cells under hypoxic conditions via the p38 MAPK and PKD signaling pathway.
References
Lewis JS, Lee JA, Underwood JC, Harris AL, Lewis CE. Macrophage responses to hypoxia: relevance to disease mechanisms. J Leukoc Biol. 1999;66:889–900.
Spector JA, Mehrara BJ, Greenwald JA, Saadeh PB, Steinbrech DS, Bouletreau PJ, Smith LP, Longaker MT. Osteoblast expression of vascular endothelial growth factor is modulated by the extracellular microenvironment. Am J Physiol Cell Physiol. 2001;280:C72–80.
Pyo SJ, Song WW, Kim IR, Park BS, Kim CH, Shin SH, Chung IK, Kim YD. Low-level laser therapy induces the expressions of BMP-2, osteocalcin, and TGF-beta1 in hypoxic-cultured human osteoblasts. Lasers Med Sci. 2013;28:543–50.
Dinenno FA, Seals DR, DeSouza CA, Tanaka H. Age-related decreases in basal limb blood flow in humans: time course, determinants and habitual exercise effects. J Physiol. 2001;531:573–9.
Oikawa A, Siragusa M, Quaini F, Mangialardi G, Katare RG, Caporali A, van Buul JD, van Alphen FP, Graiani G, Spinetti G, Kraenkel N, Prezioso L, Emanueli C, Madeddu P. Diabetes mellitus induces bone marrow microangiopathy. Arterioscler Thromb Vasc Biol. 2010;30:498–508.
Tuncay OC, Ho D, Barker MK. Oxygen tension regulates osteoblast function. Am J Orthod Dentofacial Orthop. 1994;105:457–63.
Matsuda N, Morita N, Matsuda K, Watanabe M. Proliferation and differentiation of human osteoblastic cells associated with differential activation of MAP kinases in response to epidermal growth factor, hypoxia, and mechanical stressin vitro. Biochem Biophys Res Commun. 1998;249:350–4.
Park J, Park B, Kim H, Park T, Baek H. Hypoxia decreases Runx2/Cbfa1 expression in human osteoblast-like cells. Mol Cell Endocrinol. 2002;192:197–203.
Burke D, Dishowitz M, Sweetwyne M, Miedel E, Hankenson KD, Kelly DJ. The role of oxygen as a regulator of stem cell fate during fracture repair in TSP2-null mice. J Orthop Res. 2013;31:1585–96.
Utting J, Robins S, Brandao-Burch A, Orriss I, Behar J, Arnett T. Hypoxia inhibits the growth, differentiation and bone-forming capacity of rat osteoblasts. Exp Cell Res. 2006;312:1693–702.
Roccuzzo M, Ramieri G, Bunino M, Berrone S. Autogenous bone graft alone or associated with titanium mesh for vertical alveolar ridge augmentation: a controlled clinical trial. Clin Oral Implants Res. 2007;18:286–94.
Chan B, Leong K. Scaffolding in tissue engineering: general approaches and tissue-specific considerations. Eur Spine J. 2008;17:467–79.
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22:465–75.
Urist MR. Bone: formation by autoinduction. Science. 1965;150:893–9.
Hanisch O, Tatakis DN, Boskovic MM, Rohrer MD, Wikesjö U. Bone formation and reosseointegration in peri-implantitis defects following surgical implantation of rhBMP-2. Int J Oral Maxillofac Implants. 1996;12:604–10.
Sigurdsson TJ, Fu E, Tatakis DN, Rohrer MD, Wikesjö UM. Bone morphogenetic protein-2 for peri-implant bone regeneration and osseointegration. Clin Oral Implants Res. 1997;8:367–74.
Cochran DL, Schenk R, Buser D, Wozney JM, Jones AA. Recombinant human bone morphogenetic protein-2 stimulation of bone formation around endosseous dental implants. J Periodontol. 1999;70:139–50.
Higuchi T, Kinoshita A, Takahashi K, Oda S, Ishikawa I. Bone regeneration by recombinant human bone morphogenetic protein-2 in rat mandibular defects. An experimental model of defect filling. J Periodontol. 1999;70:1026–31.
Boyne PJ, Marx RE, Nevins M, Triplett G, Lazaro E, Lilly LC, Alder M, Nummikoski P. A feasibility study evaluating rhBMP-2/absorbable collagen sponge for maxillary sinus floor augmentation. Int J Periodontics Restor Dent. 1997;17:11–25.
Howell TH, Fiorellini J, Jones A, Alder M, Nummikoski P, Lazaro M, Lilly L, Cochran D. A feasibility study evaluating rhBMP-2/absorbable collagen sponge device for local alveolar ridge preservation or augmentation. Int J Periodontics Restor Dent. 1997;17:124–39.
Termaat M, Den Boer F, Bakker F, Patka P, Haarman HTM. Bone morphogenetic proteins. J Bone Joint Surg Am. 2005;87:1367–78.
Kozawa O, Hatakeyama D, Uematsu T. Divergent regulation by p44/p42 MAP kinase and p38 MAP kinase of bone morphogenetic protein-4-stimulated osteocalcin synthesis in osteoblasts. J Cell Biochem. 2002;84:583–9.
Guicheux J, Lemonnier J, Ghayor C, Suzuki A, Palmer G, Caverzasio J. Activation of p38 mitogen-activated protein kinase and c-Jun-NH2-terminal kinase by BMP-2 and their implication in the stimulation of osteoblastic cell differentiation. J Bone Miner Res. 2003;18:2060–8.
Hassel S, Schmitt S, Hartung A, Roth M, Nohe A, Petersen N, Ehrlich M, Henis YI, Sebald W, Knaus P. Initiation of Smad-dependent and Smad-independent signaling via distinct BMP-receptor complexes. J Bone Joint Surg Am. 2003;85:44–51.
Lemonnier J, Ghayor C, Guicheux J, Caverzasio J. Protein kinase C-independent activation of protein kinase D is involved in BMP-2-induced activation of stress mitogen-activated protein kinases JNK and p38 and osteoblastic cell differentiation. J Biol Chem. 2004;279:259–64.
Gallea S, Lallemand F, Atfi A, Rawadi G, Ramez V, Spinella-Jaegle S, Kawai S, Faucheu C, Huet L, Baron R. Activation of mitogen-activated protein kinase cascades is involved in regulation of bone morphogenetic protein-2-induced osteoblast differentiation in pluripotent C2C12 cells. Bone. 2001;28:491–8.
Hu Y, Chan E, Wang SX, Li B. Activation of p38 mitogen-activated protein kinase is required for osteoblast differentiation. Endocrinology. 2003;144:2068–74.
Celil AB, Campbell PG. BMP-2 and insulin-like growth factor-I mediate Osterix (Osx) expression in human mesenchymal stem cells via the MAPK and protein kinase D signaling pathways. J Biol Chem. 2005;280:31353–9.
Saito Y, Yoshizawa T, Takizawa F, Ikegame M, Ishibashi O, Okuda K, Hara K, Ishibashi K, Obinata M, Kawashima H. A cell line with characteristics of the periodontal ligament fibroblasts is negatively regulated for mineralization and Runx2/Cbfa1/Osf2 activity, part of which can be overcome by bone morphogenetic protein-2. J Cell Sci. 2002;115:4191–200.
Chen F-M, Chen R, Wang X-J, Sun H-H, Wu Z-F. In vitro cellular responses to scaffolds containing two microencapulated growth factors. Biomaterials. 2009;30:5215–24.
Kobayashi M, Takiguchi T, Suzuki R, Yamaguchi A, Deguchi K, Shionome M, Miyazawa Y, Nishihara T, Nagumo M, Hasegawa K. Recombinant human bone morphogenetic protein-2 stimulates osteoblastic differentiation in cells isolated from human periodontal ligament. J Dent Res. 1999;78:1624–33.
Gordillo GM, Sen CK. Revisiting the essential role of oxygen in wound healing. Am J Surg. 2003;186:259–63.
Wang EA, Rosen V, D’Alessandro JS, Bauduy M, Cordes P, Harada T, Israel DI, Hewick RM, Kerns KM, LaPan P. Recombinant human bone morphogenetic protein induces bone formation. PNAS. 1990;87:2220–4.
Puleo DA. Dependence of mesenchymal cell responses on duration of exposure to bone morphogenetic protein-2 in vitro. J Cell Physiol. 1997;173:93–101.
Raval P, Hsu H, Schneider D, Sarras M, Masuhara K, Bonewald L, Anderson H. Expression of bone morphogenetic proteins by osteoinductive and non-osteoinductive human osteosarcoma cells. J Dent Res. 1996;75:1518–23.
Wikesjö UM, Qahash M, Polimeni G, Susin C, Shanaman RH, Rohrer MD, Wozney JM, Hall J. Alveolar ridge augmentation using implants coated with recombinant human bone morphogenetic protein-2: histologic observations. J Clin Periodontol. 2008;35:1001–10.
Zara JN, Siu RK, Zhang X, Shen J, Ngo R, Lee M, Li W, Chiang M, Chung J, Kwak J. High doses of bone morphogenetic protein 2 induce structurally abnormal bone and inflammation in vivo. Tissue Eng Part A. 2011;17:1389–99.
Song DS, Park JC, Jung IH, Choi SH, Cho KS, Kim CK, Kim CS. Enhanced adipogenic differentiation and reduced collagen synthesis induced by human periodontal ligament stem cells might underlie the negative effect of recombinant human bone morphogenetic protein-2 on periodontal regeneration. J Periodontal Res. 2011;46:193–203.
Park JC, Kim J, Kim BK, Cho KS, Im GI, Kim BS, Kim CS. Dose-and time-dependent effects of recombinant human bone morphogenetic protein-2 on the osteogenic and adipogenic potentials of alveolar bone-derived stromal cells. J Periodontal Res. 2012;47:645–54.
Smucker JD, Rhee JM, Singh K, Yoon ST, Heller JG. Increased swelling complications associated with off-label usage of rhBMP-2 in the anterior cervical spine. Spine. 2006;31:2813–9.
Kaneko H, Arakawa T, Mano H, Kaneda T, Ogasawara A, Nakagawa M, Toyama Y, Yabe Y, Kumegawa M, Hakeda Y. Direct stimulation of osteoclastic bone resorption by bone morphogenetic protein (BMP)-2 and expression of BMP receptors in mature osteoclasts. Bone. 2000;27:479–86.
Sciadini MF, Johnson KD. Evaluation of recombinant human bone morphogenetic protein-2 as a bone-graft substitute in a canine segmental defect model. J Orthop Res. 2000;18:289–302.
Chen TL, Shen WJ, Kraemer FB. Human BMP-7/OP-1 induces the growth and differentiation of adipocytes and osteoblasts in bone marrow stromal cell cultures*. J Cell Biochem. 2001;82:187–99.
Acknowledgements
This study was supported by National Research Foundation of Korea (NRF-2015R1D1A3A01016667). The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
Authors’ contribution
WHH carried out the molecular genetic studies and prepared the manuscript. HSS participated in the design of the study and performed the statistical analysis. BSP conceived of the study, and participated in its design and coordination and helped to draft the manuscript. YDK designed the study, drafted the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
The authors declare that they have no competing interests.
Ethical statement
There are no animal experiments carried out for this article.
Rights and permissions
About this article
Cite this article
Ha, WH., Seong, HS., Choi, NR. et al. Recombinant human bone morphogenic protein-2 Induces the Differentiation and Mineralization of Osteoblastic Cells Under Hypoxic Conditions via Activation of Protein Kinase D and p38 Mitogen-Activated Protein Kinase Signaling Pathways. Tissue Eng Regen Med 14, 433–441 (2017). https://doi.org/10.1007/s13770-017-0046-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13770-017-0046-1