Abstract
Ultraviolet (UV) disinfection technologies are well-known tools for microbial prevention in indoor public places which are frequently employed for disinfecting air, surfaces, and water. Such technologies have drawn a great deal of interest due to its potential application, especially in the domain of healthcare. This article discusses the shortcomings of chemical disinfectants and analyzes the current research standing on the development of various types of UV disinfection technologies for their prospective usage in the healthcare industry. Furthermore, the article provides a thorough analysis and in-depth evaluation of the current antibacterial studies using UV lamps and light-emitting diodes (LEDs) for the treatment of frequently encountered pathogens associated with healthcare. According to the systematic review, UV-LEDs have shown to be a potential source for delivering disinfection which is equally efficient or more effective than traditionally used UV lamps. The findings also provide valuable considerations for potentially substituting conventional lamps with LEDs that would be less expensive, more efficient, more robust, non-fragile and safer. With greater effectiveness and advantages, UV-LEDs have shown to be the potential UV source that could fundamentally be able to transform the disinfection industry. Therefore, the study supports the employment of UV-LED technology as a better and workable approach for effective disinfection applications. The study also offers insightful information that will help to direct future studies in the domain of hygienic practices used in healthcare facilities.
Graphical Abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Healthcare-associated infections (HAIs) are a substantial contributor to patient mortality and morbidity as well as growing healthcare costs (Magill et al. 2018; Haque et al. 2018). When obtaining care, especially in hospitals, nursing homes, and other ambulatory settings, many infections can be acquired. Through invasive treatments, surgery, and medical equipment, bacterial, viral, or fungal infections can spread and result in an infection. Compared to 6.5% in the European Union/European Economic Area, 3.2% of Americans have HAI, and the frequency is likely higher internationally (Suetens et al. 2016; Allegranzi et al. 2011). Modern medicine frequently uses invasive medical equipment such as ventilators and catheters, which are typically associated with a rise in HAI (CMS 2023). HAIs, according to statistics, are a major issue in both developed and developing countries, with 10 out of 100 hospitalized patients in developing countries and 7 out of 100 hospitalized patients in developed countries, respectively, at risk of contracting such infections (Danasekaran et al. 2014). Intensive care unit (ICU) patients, burn patients, organ transplant recipients, and neonates are a few of the groups who are most prone to HAI (Aljerf 2016). The Extended Prevalence of Infection in Intensive Care (EPIC II) study found that the proportion of infected patients in the ICU might occasionally reach a disconcerting 51%. HAIs are more common than before and are associated with a number of adverse outcomes, such as prolonged hospitalization, long-term disability, increased antimicrobial resistance, economic disturbances, and increased mortality rates (Vincent et al. 2009). Unfortunately, the lack of accurate data on the severity of this issue is mostly due to insufficient monitoring systems and weak preventive measures (Allegranzi 2011).
Location of the research: V01, Department of Biomedical Engineering and Health Sciences, Universiti Teknologi Malaysia, Johor Bahru-81310, Malaysia.
Rise in nosocomial infections (NIs) in healthcare settings
The substantial issue of NI, also known as HAIs, has drawn notable attention as a result of contamination in healthcare settings as illustrated in Fig. 1. These infections not only lower the quality of life for the patients but also increase medical costs. However, healthcare workers (HCW)s can work together to prevent and manage hospital-based infections by putting into practice crucial methods including early diagnosis and isolation of infected patients, effective use of personal protective equipment, and environmental cleaning and disinfection (Aljerf 2016). Such events could also give researchers crucial information about how to prevent and manage the spread of NI in the future (Du et al. 2021). NI is still a problem in infant care despite the fact that advances in medicine have already made it possible for weakened and smaller infants to survive. Longer hospital stays, elevated death rates, and short- and long-term morbidity are all linked to such infections (Ramasethu 2017). Hospital infection rates were also the focus of studies by Li et al. (Li et al. 2017) that emphasized on how NI surveillance systems influenced hospital infection rates. The study found that continuous surveillance exhibited a favorable impact on NI rates, with odds ratios/risk ratios varying from 0.43 to 0.95, respectively.
Overview and rate-influencing factors for nosocomial infection (NI) in healthcare
Common NI cases, which, despite the availability of antibiotics, continue to be a serious public health concern. The microorganisms which trigger NI infections frequently are addressed in Table 1. These infections might lead to extended hospital stays, greater rates of morbidity and death, more frequent use of antibiotics, and higher costs. Multidrug-resistant (MDR) bacteria such Staphylococcus aureus (S. aureus), Enterococcus faecium (E. faecium), Klebsiella pneumoniae (K. pneumoniae), Acinetobacter baumannii (A. baumannii), and Pseudomonas aeruginosa (P. aeruginosa) pose a severe threat to public health and have emerged as a result of antibiotic overuse (Darvishi et al. 2020). The three frequently isolated bacterial pathogens such as A baumannii, K. pneumoniae, and methicillin-resistant S. aureus (MRSA) have shown to be a major cause of such infection (Ananda et al. 2022). The studies have found 54 pathogenic microorganisms to be prevalent in 6.9% of culture-confirmed nosocomial infections (NIs). Among them, Gram-positive bacteria made up 55.6% such as S. aureus (18.5%), Escherichia coli (E. coli) (16.7%), and Streptococcus pneumoniae (S. pneumoniae) (14.8%), being the most frequently isolated microorganisms. The most frequently infected surgical sites infections (SSIs) were accounted to be 31.5% which were followed by the bloodstream which were 25.9%. The most prevalent pathogens identified in surgical sites were coagulase-negative staphylococci (17.6%), P. aeruginosa (17.6%), and S. aureus (29.4%). Likewise, S. pneumoniae (41.6%) and Klebsiella spp. (25%) were the top two pathogens isolated from the upper respiratory tract, and E. coli (36.3%), Proteus spp. (18.2%), and Enterococcus spp. (18.2%) were most frequently isolated from urinary tract infections. It was also found that S. aureus and E. coli with the prevalence 28.6 and 21.4%, respectively, were the most commonly isolated microorganisms associated with bloodstream infections (Tolera et al. 2018). Surgical site infections (SSIs), which affect 2–5% of patients undergoing surgery, have posed a serious and prevalent complication of hospitalization. According to studies by Anderson et al. (2011), SSIs have been found to be mostly caused by S. aureus, which is contributing to up to 37% in community hospitals and 20% in hospitals that reported to the Centers for Disease Control and Prevention (CDC).
MRSA is not just the most frequent infection in tertiary care facilities and academic institutions, but also the main contributor to SSI in community hospitals. In hospitalized patients, bloodstream infections (BSI), catheter-related bloodstream infections (CRBSI), lower respiratory tract infections (LRTI), and urinary tract infections (UTI) tend to be caused by microorganisms as reported by Bardi et al. (2021). Furthermore, coagulase-negative staphylococci and Enterococcus faecalis (E. faecalis) were the most common bacteria found in patients with primary BSI. Gram-positive bacteria were also accounted for a large number of CRBSI cases, with Candida albicans (C. albicans) being the most common cause, followed by E. faecalis, Enterococcus faecium (E. faecium). Gram-negative bacteria such as P. aeruginosa was the most often isolated bacterium in patients with ventilator-associated pneumonia (VAP) and tracheobronchitis. Gram-negative microbes were also observed to be the most common cause of LRTI. Moreover, S. aureus was shown as commonly isolated pathogen in the patients with VAP and tracheobronchitis, with a high resistance rate to methicillin observed in 87% of cases. Aspergillus spp. were identified in three cases of LRTI. Enterococcus faecium and E. faecalis were also the most common cause of UTI. Also, according to one article, Enterobacterales and non-fermenting Gram-negative bacilli, such as A. baumannii and Stenotrophomonas maltophilia (S. maltophilia), were occasionally identified as the causative agents of bacteremia, LRTI, UTI, and soft tissue infections. Pseudomonas aeruginosa was also found to be responsible for HAIs that can manifest as bloodstream infections, urinary tract infections, pneumonia, and infections at surgical sites. It accounted for approximately 7.1–7.3% of all HAIs, according to studies (Magill et al. 2014a; Weiner et al. 2016). Moreover, over the past ten years, P. aeruginosa infections have grown increasingly prevalent (Williams et al. 2010; Parker et al. 2008). As much as 22% of all HAIs are caused by hospital-acquired pneumonia (HAP) and VAP, which impose a significant burden on the healthcare system (Kalil et al. 2016). Pseudomonas aeruginosa is second only to S. aureus in VAP infections, accounting for 10–20% of the isolates (Magill et al. 2014a).
Microbial contamination on environmental surfaces
Recent studies have shown that the transmission of Multidrug Resistant Organisms (MDROs), viruses, mycobacteria, and fungi as the main causes of HAIs that contribute to morbidity and mortality among the patients admitted in hospital which is substantially affected by environmental contamination (Rosenthal et al. 2016; Weber et al. 2010). Reports have also shown that such contamination has a substantial impact on the transmission of these microorganisms (see Table 2) in healthcare settings (Dancer 2014; Sood and Perl 2016; Kirk Huslage 2010). In healthcare environments, the long-term persistence of a variety of nosocomial pathogens including S. aureus, Vancomycin-resistant Enterococcus (VRE), MRSA, A. baumannii, C. difficile, and P. aeruginosa has been observed (Boyce 2007; Kramer et al. 2006; Chemaly et al. 2014). These microorganisms continued presence in the environment can act as a source of transmission and spread in hospital settings (Esteves et al. 2016). The type of surface—whether it is smooth, porous, rough, dry, moist, new, or old, influences the degree of contamination. Since rough or porous surfaces tend to harbor more bacteria than smooth ones, it might be challenging to effectively clean and disinfect the surface. Additionally, microorganisms have the capacity to form biofilms on surfaces, which may provide a secure habitat that enables them to persist for a longer period of time (Boer 2006). While certain pathogens can survive for a few days, others can last for weeks or even months. HCW can also contaminate their hands with MRSA, GRE, and Gram-negative bacilli when they come into contact with colonized or infected patient’s environments (Bernard et al. 1999; Bhalla et al. 2004). High-touch surfaces, devices, equipment, and life-support systems require advanced disinfection techniques in hospital settings to avoid contaminating inanimate surfaces (Hayden et al. 2008; Adams et al. 2017). Bacterial contamination may also occur through transmission directly from infected or colonized patients or through the hands of HCWs (see Fig. 2). Objects near patients are more likely to become contaminated, and infections frequently lead to higher levels and rates of bacterial contamination (Rohr et al. 2009; Bonten et al. 1996). Huslage et al. (2010) found out that the bed rails, bed surfaces, supply carts, over-bed tables, and intravenous pumps were among the most frequently touched surfaces by HCW (Shams et al. 2016). In addition, medical equipment and devices like hemodialysis machines, infusion pumps, stethoscopes, electronic thermometers, and blood pressure cuffs may act as potential reservoirs for the transmission of nosocomial infections (Sehulster 2003).
In addition, there is a growing consensus that bacteria in dry surface biofilms may contribute to HAI. The risk of HAI is also derived from the direct transfer of pathogens from biofilms to patients, especially when cleaning and decontamination are insufficient. By touching surfaces, individuals, including staff, patients, and visitors, might acquire infections on their hands and fingertips. They may then inoculate a possible infection site or spread pathogens to additional sensitive regions. This raises serious concerns regarding the effectiveness of typical cleaning techniques for hospital surfaces. These microbial occupants develop defense mechanisms to ensure their survival while also increasing their chances of transferring to more favorable environments (Chowdhury et al. 2018; Tahir et al. 2019). As a result, a biofilm can be thought of as a “microbial village,” with a distinct infrastructure that supports a diversified population of bacteria, viruses, fungi, protozoa, and spores contained within extracellular polymeric substances (EPS) (Lindsay et al. 2006).
One study focused on the occurrence of dry biofilms on hospital surfaces, which has gotten minimal attention compared to wet biofilms associated with medical devices. According to the study, the practically ubiquitous presence of multi-species dry biofilms of Gram-positive bacteria were discovered in three UK hospitals. Notably, MRSA was found in 58% of the samples. Despite a uniform physical cleaning, there were differences in dominant species among hospitals. The study further emphasized the possible underestimating of dry biofilms’ significance in HAI transmission, particularly when combined with ineffective cleaning techniques. It implied that present cleaning processes should be reassessed and improved in order to successfully manage this often-overlooked source of infection (Ledwoch et al. 2018). In addition to this, another study (Chowdhury et al. 2018) looked into the transmission of dry surface biofilms (DSBs) in hospitals. The researchers sought to determine if DSBs were potentially transferred from surfaces to the hands of HCWs. As per findings, 5.5–6.6% of DSB bacteria were reported to be migrated to hands with one touch. The study confirmed hands as the potential transmission route of DSB bacteria, implying their persistence as pathogen sources and emphasizing their potential significance in HAI transmission.
To counter such challenges, one study (Desrousseaux et al. 2013) sought to investigate potential solutions associated with device-related infections in healthcare. A specific technique involved coating or covalently bonding a biocidal chemical onto materials, with the potential for biocide release or contact killing without release. The study emphasized on modifying the chemical or physical surface characteristics of materials to prevent microbe attachment. Another study (Uneputty et al. 2022) highlighted the multifunctional approaches to combat biofilms on surfaces, categorized into four main groups: anti-adhesive, contact active, biocide attached/biocide release, and topographical alteration to prevent bacterial biofilms on the surface. The anti-adhesive procedures may attempt to minimize bacterial attachment to solid surfaces, hence preventing contamination, contact active techniques may entail attaching antibacterial chemicals to offer continuing antibacterial properties, biocide attached/biocide release may combine the controlled release of toxic substances to combat microorganisms on surfaces, and topographical alteration may generate minor structural elements that target biological components in order to eradicate microorganisms. To date, fresh approaches to addressing the challenge of biofilm formation on surfaces are being investigated, particularly in response to the growing problem of antibiotic resistance.
Understanding the microbial transmission pathways
Patients may get transmitted from a wide variety of sources such as HCWs who have not properly or routinely maintained hand hygiene, low- and high-touch surfaces, air and water, which subsequently increases the risk of infection and prolong the recovery period. Aspiration, inhalation, contact with infected people, exposure to contaminated surfaces or medical equipment, and numerous other ways could be a reason of microorganism or virus transmission. These possible routes of transmission highlight the need of putting in place comprehensive infection prevention strategies in hospital settings, including rigorous hand hygiene, regular surface cleaning, and disinfecting medical equipment (Sehulster 2003).
Airborne and water transmission
Concerning airborne transmission, direct transmission can occur when individuals come into contact with substantial aerosolized droplets (> 5 μm) coming from the infected individual’s oral or nasal secretions, while indirect transmission can take place when tiny spores (1–5 μm) containing viable microorganisms shed over long distances with the help of air circulation (Fig. 3) (Gamage et al. 2016). Nontuberculous mycobacteria (NTM) and Gram-negative (GN) bacteria are commonly linked to the first four modes of transmission, including contact, droplet, airborne, and vector-borne, according to studies by Sehulster et al. (2003). In addition to being linked to various different mechanisms of transmission, NTM and Acinetobacter species may also thrive in moist settings. According to the study, a number of sources, including air conditioning units, ornamental fountains, showers, respiratory therapy devices, humidifiers, and taps, develop contaminated aerosols that are associated to pathogen outbreaks in hospital settings (Kanamori et al. 2016). According to studies by Beggs et al. (2015), S. aureus can travel through the air from contaminated mattresses and clothing, depositing itself on a variety of surfaces. It has been reported that patients may come into direct contact with Legionella and other GN bacteria like Pseudomonas through the aerosols produced by showers and faucets. Moreover, microorganisms including Legionella, Pseudomonas, Aeromonas, Burkholderia, Acinetobacter, ESBL-producing and carbapenem-resistant Enterobacteriaceae, Aspergillus, and NTM, are able to transmit through water causing rise in HAIs. The healthcare environment, especially hospital water systems, is shown to be a significant reservoir of Pseudomonas spp. According to studies, hospital water systems are the primary source of P. aeruginosa propagation (Juan et al. 2017).
Transmission through direct contact or indirect contact
Vulnerable patient groups, particularly those who work in healthcare facilities, are at high risk of developing infections owing to these kinds of transmission. Another study found that HCWs who come into contact with patients who are sick either directly or indirectly through contaminated high-touch surfaces may pass along MRSA to patients (Boyce et al. 1997). Person-to-person transmission of VRE when exposed to contaminated HCW hands, contaminated surfaces, and equipment such as thermometers and electrocardiogram machines, as well as previous exposure to VRE-contaminated rooms, according to one recent study, are all risk factors for VRE acquisition (Drees et al. 2008; Falk et al. 2000). Pathogenic bacteria, such as C. difficile, VRE, and MRSA, have been found frequently persist on hospital floors and may come into contact with HCW by means of frequently touching objects (as schematically depicted in Fig. 3), yet they are often overlooked as potential sources of infection transmission (Koganti et al. 2016).
Transmission through low or high-touch surfaces
Additional studies have shown a number of surfaces that are susceptible to infection and aid in the spread of pathogens, including those near patients like bedrails, bedside tables, taps, and knobs in wards (Allegranzi et al. 2007). Additionally, “non-classical” surfaces such as oxygen humidifiers, medical workers’ personal computers, and the protective lead jackets worn in operating rooms are all linked to transmission. Considering the possibility that they could get infected while performing caregiving responsibilities by getting interaction with contaminated objects or infected individual (Allegranzi and Pittet 2009; Squeri et al. 2016). Another research discussed concerning the prevalence of A. baumannii, a bacterium which is considered more resistant to dry surfaces than E. coli and can survive there for longer than 4 months and can remain on glass surfaces for more than 20 days when left at ambient temperature. This demonstrates the toughness of A. baumannii and its ability to survive for a long time on inanimate objects (Lee et al. 2011). Clostridium difficile, a type of bacteria which is known to cause HAI, has been identified on several high-touch surfaces and equipment within healthcare facilities. Moreover, the hands of healthcare professional, cellphones, computers, doorknobs, medical equipment such as pulse oximeter finger probes and electronic rectal thermometers, prescription carts, bed, mop pads, portable beds, and sinks, aid in transmission of various pathogens (Sooklal et al. 2014; Dumford et al. 2009; Best et al. 2010). In neonatal and critical care units, which are high-risk environments for contamination, there has been an increase in the frequency of infections brought on by C. parapsilosis over the past 20 years (Guinea 2014). Based on a review (Ramasethu 2017), HCW represent a substantial source of microorganism transmission in neonatal care. According to the analysis, bacterial counts on healthcare professionals’ hands range from 3.9 × 104 to 4.6 × 106 CFU/cm2 (Bolon et al. 2016), potentially containing bacteria such as S. aureus, K. pneumoniae, Enterobacter, Acinetobacter, and Candida. Human skin sheds live organisms on a daily basis, which adds to contamination of patient clothing, bed linen, and furnishings. Transmission occurs when healthcare personnel' hands are not properly washed or disinfected before and after contact with patients. Even in the absence of prior colonization, C. parapsilosis can survive and proliferate in hospital settings by horizontal transmission from medical devices or outside sources (Trofa et al. 2008). According to the literature (Schechner et al. 2011), contamination by P. aeruginosa is also found out as a significant cause of several kinds of infections in healthcare such as burn wound infections BWI, and NB, with a mortality rate exceeding 30%. These infections can be quite threatening for individuals who are having a weaker immune. The importance of improved cleaning procedures in reducing the spread of MRSA and VRE in hospital rooms previously occupied by patients colonized with these pathogens were demonstrated in one of the studies by Datta et al. (2011). Moreover, the recent investigations by Akiko et al. (2017) examined the S. aureus isolates swabbed from the palms and fingers of mobile phone users and from their respective mobile phones. The findings imply that mobile phones may serve as a potential reservoir for the spread of infection in hospital environments. The study emphasized the significance of using proper hand hygiene prior interacting with patients, which remains to be the most effective way to decrease HAIs. Even so, MRSA and S. aureus could also cause serious infections notably CRI, BI, lung infections, and wound infections (Bal et al. 2016). Staphylococcus aureus is noteworthy as the second-most common cause of HAIs poses a serious threat to the safety of patients and their treatment (Smith and Hunter 2008; Dantes et al. 2013). Research has demonstrated that the presence of a biofilm matrix can increase resistance to disinfectants, as it encapsulates and protects the underlying cells (Percival and Cutting 2010; Abdallah et al. 2015). Another recent study by Dancer et al. (2019) used well-established staphylococcal epidemiology techniques to investigate S. aureus transmission routes within a 10-bed intensive care unit. Over the course of 10 months, the study thoroughly screened a variety of hand-touch surfaces, staff members’ hands, the air, and patients, followed by spa typing, epidemiological analysis, and whole-genome sequencing. The findings showed that there were several cases of transmission between patients and different ecological repositories. The findings provide significant data for the implementation of successful preventative and control strategies as well as for a better understanding of the epidemiology of S. aureus in hospital settings. It is also observed that S. aureus can easily be spread by the touch and has been proven to stay on surfaces for lengthy periods of time, up to 7 months (Kumari et al. 1998). Among the most recent investigations, Samreen et al. (2023) evaluated the prevalence of S. aureus in the hospital environment by collecting 245 environmental samples from a 1030-bed tertiary care hospital. The percentage of S. aureus contamination on hospital environmental surfaces in the current study was noted to be 19.1% which was comparable to prior research in Pakistan (Khattak et al. 2015). The hospital environment’s role in the transmission of HAIs is still being debated, but there’s scientific evidence that nosocomial bacteria can exist as a significant reservoir in various hospital environments such as surfaces, medical equipment, and water systems. Contamination can occur as a result of patients, their family, or healthcare employees, while improper antibiotic administration may result in the selection of multi-drug resistance microorganisms that can thrive and spread within the hospital. Additionally, healthcare workers behavior can facilitate pathogen cross-transmission via environmental and patient-to-patient routes. Proper and routine hospital environmental cleaning, antibiotic management, and educational initiatives aimed at promoting appropriate behavior among healthcare staff are potential answers to this problem.
Strategies for tackling MDRO and mitigating antibiotic resistance in nosocomial infections
In the current scenario, patients referred to hospitals frequently acquire infections triggered by MDR bacteria, which frequently leads to complications and increased mortality rates. The transmission of these diseases in the healthcare is linked to a number of different circumstances. It is critical to implement preventive measures at several levels to precisely address these elements in order to disrupt the transmission chain (Schinas et al. 2023). Preventive measures such as isolation protocols and environmental cleaning are critical in preventing MDR bacteria cross-contamination and dissemination. Despite ongoing issues in achieving compliance, monitoring and resolving hand hygiene adherence are critical components of healthcare hygiene practices. Innovative technology, such as advanced disinfection methods and stringent monitoring systems, can help to reduce the impact of MDR bacteria transmission (Boyce et al. 2016a; Brêda, et al. 2021). Furthermore, advances in healthcare architecture and hospital engineering have demonstrated remarkable possibilities for combating MDR transmission (Elbehiry et al. 2022).
Hand hygiene
The recently published update of “Strategies to Prevent Healthcare-Associated Infections through Hand Hygiene” by the Society for Healthcare Epidemiology of America (SHEA), which was put together through a robust joint effort by numerous notable organizations, has comprehensively addressed the essential practices for preventing HAIs in the healthcare, particularly in ICU (Glowicz et al. 2023). Advocating for the hygiene of the hands and fingernails, using alcohol-based hand sanitizers (ABHS) in various clinical situations, and complying to hand hygiene protocols outlined by the CDC or WHO (prior to patient contact, before aseptic procedures, after exposure to body fluids, following patient contact, and after touching the patient’s surroundings are practical guidelines that promote hand hygiene in acute-care settings (Chou et al. 2012). Promoting short, natural fingernails and making hand moisturizers widely available are essential for reducing dermatitis among healthcare workers. Essential practices also include selecting suitable hand hygiene products, assuring supply accessibility, proper glove use, and minimizing environmental contamination near sinks and drains. According to research, altering washbasin modification, such as increasing washbasin bowl depth and lowering water flow rates, reduces the danger of infection dispersion significantly (Gestrich et al. 2018).
Cleaning of environment
Mechanical, chemical, and human factors are the three basic categories of environmental hygiene interventions. Mechanical interventions, such as plastic isolators, negative pressure ventilation, and air curtains in patient rooms, as well as technologies like as ultraviolet (UV) disinfection and portable high-efficiency particulate absorption (HEPA) filters, have shown efficacy in reducing certain multidrug-resistant (MDR) infections and bacterial contamination on diverse surfaces and equipment in specific environments (Peters et al. 2022). Chemical interventions are frequently used in efforts to sterilize environmental reservoirs of MDRs. Testing numerous active chemicals and formulations, such as ethanol, propanol, formaldehyde, peroxides, inorganic chlorine releasers, and phenol derivatives, is the foundation of sterilization efforts. When selecting disinfectants for use in healthcare, it is critical to evaluate their effectiveness against a wide range of pathogens, including bacteria, viruses, yeasts, mold spores, and bacterial spores (Tapouk et al. 2020).
Determining factors associated with colonization risk
Given the variable efficacy of preventative techniques against specific bacterial species, additional research is needed to find the best effective measures for preventing MDR bacterial colonization. High colonization pressure is typically associated with the proliferation of MDROs in healthcare settings, indicating an increased risk of patient cross-transmission. According to one study, colonization pressure was discovered as an independent risk factor for MDR bacteria in the ICU in a single-center prospective cohort research (Odds Ratio (95% CI) 4.18 (1.03–17.01), p = 0.046), emphasizing its importance in contributing to the spread of such organisms (Masse et al. 2017). The recognition of patient risk factors for MDR bacterial colonization in healthcare is a proposed method that could serve as both a preventive intervention and a treatment strategy in certain patient populations, such as immunocompromised individuals.
Monitoring and responsible management of antimicrobials
The ability of physicians, chemists, microbiologists, and infection control specialists to work together effectively is essential to the success of these programs. Understanding the role, paths, and patterns of contamination from the environment in the transmission of MDR bacteria enables physicians and researchers to implement better procedures, reducing risks in healthcare settings. Environmental cultures, including as swab tests, agar slides, and air and water samples, provide vital information about the presence and persistence of MDRs in the environment. These approaches aid to establishing a clearer link between environmental contamination and pathogen uptake. Direct observation, as previously stated, as well as the use of fluorescent markers and adenosine triphosphate (ATP) bioluminescence, are other approaches for objectively assessing environmental cleanliness (Chen et al. 2021).
Contemporary technological innovations in antimicrobial coatings
Active antimicrobial coatings
Antimicrobial coatings with active qualities contain antiseptics or antibiotics that are either ionic or covalently linked inside a polymeric matrix (Polívková et al. 2017). Coatings containing noble metals can be injected into or coated onto polymeric surfaces as an alternative strategy (Dizaj et al. 2014). Bactericidal characteristics are exhibited by certain metallic compounds or their oxides, including silver (Ag), selenium (Se), silver oxide (Ag2O), titanium dioxide (TiO2), iron oxides (Fe2O3, Fe3O4), zinc oxide (ZnO), and copper oxide (CuO). These materials can be used in the form of nanoparticles or ions, especially when the increased toxicity of the bulk metal is a concern for in vivo applications (Barnes et al. 2019; Gusev et al. 2022; Kranz et al. 2019; Toplitsch et al. 2021). Due to its exceptional antimicrobial activity, coatings containing zinc oxide (ZnO) and silver oxide (Ag2O) have recently gained popularity, owing to breakthroughs in nanotechnology (Dizaj et al. 2014).
Antimicrobial metal coating
For more than three decades, silver has been widely studied for its antibacterial characteristics. It has been used successfully in applications such as urinary catheters. It is now being investigated as a covering for endotracheal tubes (ETTs), which are a substantial contributor to VAP infections. Silver coatings have now been commercialized for medicinal uses due to their success in several clinical trials (Kollef et al. 2008).
Antimicrobial photodynamic therapy (aPDT)
Antimicrobial Photodynamic Therapy (aPDT) is made up of three main components. It requires a visible light source with a certain wavelength to properly activate the photosensitizer, a non-toxic photosensitizer (PS), and the presence of ambient oxygen. When initiated, this process produces cytotoxic reactive oxygen species (ROS), which cause the targeted cells to be inactivated. It has recently emerged as a unique and noninvasive therapeutic approach, with success in treating localized and superficial infections caused by bacteria in biofilms, fungi, and viruses. This novel process offers novel therapeutic approaches and has implications in dentistry for the treatment of biofilm-caused oral infections (Koshi et al. 2011).
Therapeutic mouthwash
Therapeutic mouthwash has the ability to improve oral hygiene by lowering dental plaque and gingivitis efficiently. Dental plaque, which is mostly made up of bacteria, creates a biofilm on teeth and can cause dental decay and gum inflammation. Mouthwash’s antibacterial qualities contribute to its antiplaque efficiency, using common antiseptic components such as chlorhexidine (CHX), Listerine and essential oils. CHX is widely used as a disinfectant in a variety of medical sectors, including dermatology and surgery, due to its powerful antibacterial characteristics (Lim 2008). One recent study (Liu et al. 2023) examined on how short-term gargling with chlorhexidine (CHX) and Listerine® mouthwashes affected oral flora in hospitalized patients. According to the findings, both mouthwashes caused considerable changes in the composition of oral bacteria, with differences noted in the specific bacterial genera affected and the magnitudes of these changes. Notably, CHX had more significant effects, but its use has been linked to higher mortality, possibly due to nitrate-reducing bacteria. Listerine, despite exhibiting lesser magnitude changes than CHX, targeted bacterial species that were less related to nitrate reduction.
General practices for cleaning applied in healthcare
Microorganisms have the ability to survive on surfaces for extended periods of time and can transmit to patients through direct contact with nearby surfaces or indirectly through the hands of HCWs, particularly in situations where HCW hand hygiene compliance is low, with reported rates hovering around 40% (Otter et al. 2011; Sunkesula et al. 2017). Many investigations have shown that if persistent surface contamination remains after terminal cleaning and disinfection, subsequent patients have a chance of contracting the same pathogen as the prior individual (Mitchell et al. 2015; Chen et al. 2019; Shaughnessy et al. 2011). The findings of the Researching Effective Approaches to Cleaning in Hospitals (REACH) trial show that comprehensive environmental cleaning has a substantial influence on the prevention of HAIs (Mitchell et al. 2018). Various studies have suggested to implement a comprehensive cleaning strategy that must incorporate training, technique, product, audits, and communication components, and the performance and the knowledge services staff could be improved (Mitchell et al. 2018; Mitchell et al. 2019a; Hall et al. 2020). Enhanced cleaning and disinfection techniques have been shown to reduce the prevalence of HAIs (Donskey 2013). Additionally, Dancer et al. (2009) demonstrated the inclusion of an extra environmental cleaning services to perform enhanced hand-touch site cleaning in surgical wards having high prevalence of S. aureus resulted in a 32.5% reduction in microbial contamination levels and a 26.6% decrease in new MRSA infections in comparison with control wards. Also, the enhanced terminal cleaning resulted in a 94% reduction in contamination with epidemiologically significant pathogens, according to a prospective research by Rutala et al. (2018).
It is vital to distinguish between critical and non-critical surfaces as well as low-touch and high-touch surfaces when assessing risks related to patient care, staff safety, and pathogen transmission. Low-touch surfaces, such as floors and walls, are less likely to have contact with skin since they are not often handled by patients or HCWs. On the other hand, because it is close to patients and are frequently touched by HCWs, high-touch surfaces like bedrails, door knobs, and medical equipment pose a serious threat of spreading diseases (Weber et al. 2010; Kirk Huslage 2010; Adams et al. 2017; Otter et al. 2011; Boyce et al. 1997; Koganti et al. 2016; Sunkesula et al. 2017). The fact that surfaces and locations outside the patient zone, such hospital canteens or elevator buttons, can potentially host germs, makes them it a significant concern (Christiansen et al. 2004; Matthew Mulle and Armstrong 2018). However, critical surfaces have a higher risk of infection than non-critical surfaces since it comes into contact with objects like needles and intravenous catheters, as well as blood and intravenous catheters (Diseases and Organisms in Healthcare Settings 2016; Friedman et al. 1996). As a result, there is a substantial risk of infection even from low-touch surfaces used for medical procedures or the administration of intravenous medication. In order to reduce the transmission of infections, it is imperative to adopt the proper cleaning and disinfection methods for all types of surfaces.
Cleaning is the process of physically removing dirt and dust until the area is clearly clean using water, either with or without detergent, and physical action. To reduce the danger of infection and prevent cross-contamination, disinfection, on the other hand, aims to eliminate the majority or all harmful bacteria (Matthew Mulle and Armstrong 2018; Peters et al. 2018; Rutala et al. 2008). Disinfection is typically done in conjunction with cleaning to lessen the impact of organic matter and the amount of contamination. Because of this, normal cleaning and disinfection are frequently integrated, performed once daily on general wards, as well as in targeted measures immediately after surfaces are contaminated with blood or other human fluids (Christiansen et al. 2004; Matthew Mulle and Armstrong 2018). If necessary, a disinfectant is often used for cleaning. Once a patient has been released, terminal cleaning and disinfection is carried out in order to stop the spread of dangerous infections to the subsequent patient using a hospital room. In this process, surfaces that are generally hard to reach when a room is occupied, including the mattress and other ones that could have gone unnoticed during the patient’s stay, are cleaned in addition to those that are routinely cleaned (WHO 2019).
An overview of commonly employed disinfectants for cleaning and disinfection
There are a number of novel disinfection products on the market or in research, in addition to the frequently utilized disinfectants like alcohol, chlorine, aldehyde, amine, oxidative (such hydrogen peroxide and peracetic acid), phenolic and quaternary ammonium compounds. They include liquid disinfectants that contain enhanced hydrogen peroxide, peracetic acid and hydrogen peroxide combinations, hydrogen hypochlorite, and polymeric guanidine. Additionally, there are cleaning/disinfectant products that combine both functions available on the market (Matthew Mulle and Armstrong 2018; WHO 2019). However, with the benefits, there are several significant drawbacks of using such disinfectants that must be considered (see Table 3).
No-touch UV disinfection systems: exploring microbial control strategies with disinfection technologies
Surfaces in health centers are frequently infected with harmful microorganisms that may endure routine cleaning and disinfection (Rutala and Weber 2013). The utilization of hydrogen peroxide mist, vapor, or UV radiation is what has conventionally been the focus for most of the studies in regards of no-touch disinfection systems (Simmons et al. 2013; Rutala and Weber 2016b; Sitzlar et al. 2013). Additional no-touch methods, such as high-intensity narrow-spectrum light, quaternary ammonium fogging, and alcohol-mist (Jury et al. 2010), ozone gas, superoxide water, and steam vapor, have also been developed (Sexton et al. 2011). The use of no-touch automated disinfection (NTD) is a successful and promising method for lessening the prevalence of HAIs. NTD systems use a variety of disinfectants to clean surfaces and equipment in healthcare facilities, including vaporized hydrogen peroxide (VHP), hydrogen peroxide vapor (HPV), chlorine dioxide, gaseous ozone, dry mist of hydrogen peroxide (DMHP), and aerosolized hydrogen peroxide (aHP). To increase the effectiveness of these disinfectants, they are frequently combined with other substances including silver cations, aerosolized peracetic acid, quaternary ammonium compounds, high-intensity narrow-spectrum (405 nm) light, ultraviolet (UV) light-emitting diode and pulsed-xenon UV (PX-UV) radiation. Healthcare facilities can successfully lower the risk of HAIs by implementing NTD systems, which might also improve patient health outcomes, lower healthcare costs, and maximize patient satisfaction (Aljerf 2016). NTD systems are especially helpful in settings with complex equipment or high-touch surfaces when conventional cleaning and disinfection techniques are ineffective or impractical (Dancer 2014; Rutala et al. 2008; Otter et al. 2014).
UV radiations
When compared to aHP systems, germicidal UV-C radiation disinfection is much quicker. It provides methods that are controlled and effective for eliminating bacterial contamination specially within medical facilities. Healthcare facilities can offer a secure environment for patients and healthcare staff and lower the risk of HAI by implementing these no-touch disinfection techniques (Kelly et al. 2022; Andersen et al. 2006). UV light refers to radiation with wavelengths between 100 and 380 nm. It is divided into three zones: UV-A (320–380 nm), UV-B (280–320 nm), and UV-C (100–280 nm). UV-A, comprising about 6% of solar energy, is considered the least harmful. Conversely, UV-B, accounting for approximately 1.5% of UV light, can have adverse effects on plants. The most harmful type, UV-C or deep UV-C, poses severe risks to living organisms. Thankfully, the ozone layer acts as a natural shield, absorbing most UV-C radiation, safeguarding the Earth’s biosphere from its harmful impact. Short-wavelength UV radiation (UV-C in the 200–280 nm range) causes DNA/RNA damage in microorganisms, hindering cellular metabolism and replication. Employing portable UV-C lamps or ceiling-mounted fixtures for microbial decontamination significantly contributes toward the disinfection processes (Guerrero-Beltr and Barbosa-C·novas 2016; Hollosy et al. 2002; Conner-Kerr et al. 1998).
Development of UV-based technologies for disinfection purpose
Mercury vapor technologies
Low-pressure mercury (Hg) vapor lamps are the conventionally used in UVGI air disinfection applications. Although these lamps resemble conventional Hg fluorescent bulbs, there are two key distinctions. First off, there is no fluorescent phosphor in the lamp’s tube. Second, fused quartz is employed to build the tube rather than glass. Commercially available lamps are essentially divided into two groups: low output powered by traditional magnetic ballasts; high output powered by electronic ballasts (Van Osdell et al. 2002). Many variables, including lamp pressure, electrical current, voltage, excitation waveform, discharge ignition, and internal gas composition, have an impact on the energy production and spectrum properties of lamps. The high-output lamps are driven at greater power by increasing the current input into the bulbs to produce more output radiation, whereas low-output lamps are normally operated at low power. LP amalgam lamps are one of the newer technologies produced by recent improvements in lamp hardware which can have input conversion efficiencies that are greater than 38%, and operate at higher temperatures (Miller et al. 2013). A germicidal lamp emits UV radiation in the 200–300 nm region (Ryan et al. 2010; Kowalski et al. 2009). LP mercury systems do not have spectral emission profiles. They effectively emit monochromatically at 254 nm. The very small 185 nm peak is filters by the quartz sleeve (Kowalski et al. 2009). In contrast, an MP lamp emits a wide spectrum of wavelengths from 200 to 600 nm and is mostly utilized for advanced oxidation, water treatment, and surface treatment (Kowalski et al. 2009; Kowalski 2009). Mercury-based UV-C lamps are still employed in UVGI systems despite the fact that Minamata Convention on Mercury’s 2013 which made a stipulation against any device containing mercury be banned by 2020 for the protection of human health and the environment. Nonetheless, as shown by recent research in this field, attempts are still being made to substitute out such lamps with UV-C-LEDs (Kessler 2013). The production of ozone using LP mercury lamps is constrained by technical and financial factors including efficiency and lamp lifetime, according to one of the recent researches by Levin et al. (2013). Nevertheless, LP lamps are now more efficient and dependable as a source of visible (V) vacuum UV ozone formation. In one research, the author contrasts the effectiveness of LP UV irradiation with UV-LEDs against E. coli and MS-2. The study achieved 4-log10 reductions in E. coli and reduction in non-enveloped virus (MS-2) with both lamp and LEDs at 260 nm (Sholtes et al. 2016).
Limitations Despite its advantages and germicidal potency, the lamp continues to have a lot of shortcomings. For monochromatic performance, the lamp works at around 130 degrees Celsius, and for polychromatic activity, at a minimum temperature of 300 °C up to more than 500 °C. Also, MP only have a maximum lifespan of 8000 h before they need to be replaced, and LP have a limited lifespan of 8000–10,000 h throughout the germicidal UV lifecycle.
Development of PX-UV technologies
PX-UV, which uses intense UV light pulses to deliver a powerful germicidal effect, is a possible alternative to traditional UV technologies. Since PX-UV exposure is rapid and intense, it could take less time to reach fatal dosages, making it a desirable alternative. PX-UV light, as opposed to other UV lamps, may be more efficient due to its broad spectrum and higher intensity. In a laboratory environment, PX-UV is a strong substitute for conventional UV methods for producing germicidal effects (Levin et al. 2013). According to study by Haddad et al. (2017), using PX-UV as an additional step to a regular cleaning routine causes levels of bacterial contamination to drop. Studies by Jinadatha et al. (2014, 2015) found PX-UV as an effective technology by successfully reducing the presence of identified pathogens in comparison with conventional manual room terminal cleaning by offering an efficient and effective method of disinfection. A source of UV that is not abundantly observed in commercial disinfection equipment is xenon. The absence of mercury vapor has been described as one of its primary benefits over LP. In contrast to mercury, it produces UV radiation using Xenon gas, which hold promise in generating UV-C with a wavelength range of 185–600 nm (Chemaly et al. 2014; Bolton et al. 2008).
Limitations The primary disadvantages of xenon lights are related to their operational requirements, which result in significant power consumption and high working temperatures of about 500 °C, requiring considerable maintenance, warmup requirement etc. Moreover, the lamp’s lifespan is limited and its output light consistency is inefficient, necessitating frequent lamp replacement that simultaneously add huge cost to the users (Lamont et al. 2004).
Development of UV-LED technologies
The research and development industries have given UV-LED technology a significant amount of focus, which has caused a surge in UV-LED producers in recent years. UV-LEDs have proven to be a strong contender, especially for disinfection applications, due to the rapid advancement that is replacing conventional disinfection techniques. Advancements in nitride semiconductors have led to the commercial availability of UV-C LEDs. III-nitrides, which emit UV light at wavelengths spanning from 210 to 365 nm, are the most widely used UV-LED materials. Examples include gallium nitride (GaN), aluminum nitride (AIN), and aluminum gallium nitride (AGaN) (Jang et al. 2010). According to recent research, UV-LEDs are a useful tool for disinfecting water, food, and healthcare applications since they are most efficient at germicidal activity with wavelengths between 100 and 300 nm (Khan et al. 2005), since Pankove et al. created the first AGaN LED in 1972 (Crawford et al. 2005), which have advanced in a remarkable way. These LEDs have broad spectrum, spanning from infrared to UV spectral ranges attributed to the widespread usage of group III nitride materials (Pankove et al. 1873). The development of high-efficiency deep UV-LEDs as a potential replacement for low-pressure mercury lamps has been encouraged by the International Minamata Convention of 2013, which aims to protect the environment. These LEDs have flexibility to change the light-emitting band by modifying the epitaxial structure, making them suitable for a variety of applications. It should be noted, nevertheless, that some organic substances can release UV-C radiation. Organic molecules are colorless in solution and transparent to high-energy light in the UV (200–400 nm) and visible (400–700 nm) regions of the electromagnetic spectrum (Han et al. 1998; Lambert et al. 1998).
Limitations In spite of the numerous advantages of UV-LEDs, such as their potent antibacterial properties, compact package sizes, extended lifespan, affordability, and low operating voltage and temperature, they do have certain limitations. Notably, UV-LEDs tend to offer lower intensity and face challenges in achieving high irradiance at longer distances, in comparison with traditional lamps. However, recent research has indicated the possibility of enhancing the intensity and improving the disinfection capabilities by integrating multiple arrays of LEDs into a single circuit.
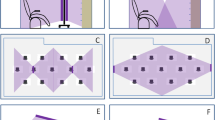
Overall, the use of no-touch disinfection sources that employ UV-C is replacing the use of chemical disinfectants in the context of environmental cleaning, which is experiencing a technological revolution depicted in Fig. 4. Despite the fact that UV-C has been shown to be effective against bacteria and viruses, advances in UV-C technology have compelled professionals to come up with a tool that is robust, energy-efficient, operates at lower temperatures, and is inexpensive. In such regards, UV-C SMD LED sources have exhibited various advantages to accomplish overcome the limitation posed by traditional UV lamps. The comparison of aforementioned commercially available UV sources is compared in Table 4.
The progression of technology from traditional methods to modern innovations. A Microorganism and pathogen transmission pathways, B manual cleaning method by employing liquid disinfectants, C robotic disinfection systems that use mercury vapor or Xenon gas for UV– C generation, D UV-C LEDs directly mounted over SMD chips which comes in various package sizes
UV absorption, penetration, spectral power distribution (SPD), and penetration depth to human skin
Radiation having wavelengths between 100 and 380 nm is referred to as UV light. UV-A (320–380 nm), UV-B (280–320 nm), and UV-C (100–280) are the three zones that fall under such category (Guerrero-Beltrán et al. 2004). UV-A’s spectrum is thought to be the least damaging region of the UV radiation spectrum and makes up around 6% of all solar energy. Contrarily, UV-B is known to have a variety of negative impacts on plant while making up just around 1.5% of the entire UV light spectrum. The most harmful kind of UV radiation, known as UV-C or deep UV-C (Sharma and Demir 2022), is capable of severely damaging living organisms. Yet, the ozone layer in the stratosphere serves as a natural filter and absorbs most UV-C radiation, protecting the Earth’s biosphere from its negative affects (Hollosy et al. 2002). Microorganisms undergo DNA/RNA damage from short-wavelength UV radiation in the 200–280 nm range, or UV-C. This damage actively prevents cellular metabolism and replication. Using either portable UV-C lamps or ceiling-mounted UV-C light fixtures to irradiate various surfaces and spaces for microbial decontamination can enhance the disinfection effectiveness of UV-C radiation (Kowalski et al. 2009). Pyrimidine dimerization is associated with increased incidence for the photoinduced harm caused to microorganism’s DNA and RNA. Particularly, thymine, which is only found in DNA, produces cyclobutene dimers when exposed to UV light. This dimerization prevents nucleic acid replication, and even when replication does occur, it typically produces errors that make the microbe unviable (Conner-Kerr et al. 1998). UV-A is nearly visible and is known to cause damage to skin cells. Due to its shorter waveband, UV-B is also a significant contributor to skin damage and sunburn throughout the day. Both UV-A and UV-B cause harm to our skin because of its deep penetration into human tissue (Kowalski 2009). It is known that all UV wavelengths have some photochemical effects, but high-energy photons in the UV-C range preferentially harm cells as they are absorbed by proteins as well as DNA and RNA (Fig. 5A). The germicidal peaks between 260 and 265 nm, which also happens to be when bacterial DNA and RNA absorbs the most UV energy (Kowalski et al. 2009). Figure 5C depicts spectral comparisons between different UV light sources in relation to the typical absorption spectra of DNA/RNA (also known as the germicidal effectiveness curve (GEC)) and the absorption spectrum of proteins. As demonstrated in Fig. 5C, low-pressure mercury lamps are particularly effective at killing pathogens since they emit the majority of their optical output (around 85%) at a wavelength of 254 nm, which is quite close to the GEC peak (260–265 nm). Recently, excimer lamps have also gained popularity due to their emission at 222 nm, which is thought to be safer due to their shallow depth of penetration in human tissue (Fig. 5B). The 254 nm UV-C range is largely absorbed by DNA/RNA, as shown in Fig. 5B, and it can penetrate further into the epidermal layer of the human skin and disrupt DNA in skin cells, which may lead to the development of cancer. The polychromatic emission pattern of MP UV lamps has a strong peak at about 365 nm. Figure 5C illustrates the monochromatic emissions of LP UV lamps, which are instead centered around 254 nm. LP UV lamps have been used in disinfection as a result because their emission is close to the germicidal curve’s peak (Schalk et al. 2005). Because the far-UV-C wavelength range only penetrates a relatively small depth into human skin, excimer lamps are thought to be safer than mercury lamps (see Fig. 5B) (Sharma and Demir 2022).
A The absorption spectrum for DNA and RNA, also known as the germicidal effectiveness curve, peaks at 265 nm (shown with a vertical dashed line). While the absorption spectrum for proteins tends to increase toward shorter wavelengths. B The wavelengths showing the depth to which UV radiation can penetrate human skin in addition to the degree to which it scatters. The penetration depth and scattering values are specifically 18 μm, 27 μm, and 32 μm over the wavelengths of 222 nm, 254 nm, and 265 nm, respectively. C The typical absorption spectra of DNA/RNA and proteins are compared to those of various UV-C light sources. Reprinted from “Bright Future of Deep-Ultraviolet Photonics: Emerging UVC Chip-Scale Light-Source Technology Platforms, Benchmarking, Challenges, and Outlook for UV Disinfection,” Kumar, ACS Photonics, Copyright 2022 (Sharma and Demir 2022)
Overall, while UV radiation is highly effective in disinfection, it possesses the ability to penetrate beyond the superficial layers of the skin and reach the epidermal layer where our skin cells are located. When UV radiation comes into contact with these skin cells, it has the potential to induce DNA disruption. This DNA disruption within skin cells can have severe consequences, as UV-induced DNA damage is a well-established risk factor for skin cancers. Furthermore, Erythema develops as a consequence of a photochemical reaction in which the skin turns red as a result of high UV-B and UV-C light exposure, namely about 30 J/cm2 at a wavelength of roughly 270 nm. Moreover, the initial challenge lies in the fact that UV-C light requires an unobstructed passage to an object in order to disinfect it efficiently. However, it is conceivable that the light will be obstructed by other objects or will only reach one side of the object. This is known as “shadowing,” and it indicates an increased risk of active pathogens remaining in places that are not exposed to light (Kowalski et al. 2009; Kowalski et al. 2009; Schalk et al. 2005).
Nevertheless, the compact size of UV-LEDs (Bolton et al. 2008; Khan et al. 2005), on the other hand, stands out as a main advantage, allowing for the combination of single or several wavelength outputs to maximize pathogen inactivation. Furthermore, the availability of UV-LEDs in various compact sizes allows for easy integration into a wide range of applications, particularly those featuring intricate designs. When faced with challenges like shaded areas or obstructed passages that can impede traditional UV disinfection equipment, UV-LEDs emerge as an ideal choice for fostering the development of handheld disinfection systems, employing UV SMD LEDs. This flexibility highlights UV-LEDs’ significant potential as a powerful tool in future advancements. In addition, the use of photocatalytic oxidation using titanium dioxide (TiO2) coating and mild ultraviolet A (UVA) light to reduce bacterial contamination on surfaces has been explored as a promising alternative to conventional disinfection system in one study (Klaus et al. 2003). This method produces reactive OH-radicals that effectively kill microorganisms. Rather than using direct UV-C irradiation, the study deployed focused light guiding and a UVA-transmittant Plexiglass layer to ensure bacterial inactivation across the entire surface, overcoming the challenges posed by shaded and obstructed areas.
Recent studies on microbial inactivation using UV technologies
Mercury vapor lamps inactivation experiments
LPML, in particular, are frequently used as the main UV source for disinfection purposes on an industrial scale due to its high wall plug efficiency, which is over 30–35% (Koutchma et al. 2019). Furthermore, their monochromatic emission is close to the peak of DNA absorption which is about 260 nm (Fig. 7A). Various researches have been conducted to evaluate the efficacy of mercury vapor lamps against environmental bacteria. One of the studies by Correa et al. (2017) assessed the efficacy of a handheld device (Surface UV) against diverse clinical pathogens obtained from various surfaces of a public health hospital by employing LPML for treatment. The study showed reduction by a factor of 6.5, 6.7, 6.2, 5.4, 5.4 and 6.7 log10 inactivation against S. aureus, S. mutans, S. pneumoniae, E. coli, P. aeruginosa and C. albicans, respectively, upon exposure to the dose of 0.78 J/cm2, demonstrating a noteworthy reduction in microorganisms in the healthcare setting. Another study addressed the usage of germicidal mercury vapor UV lamp for treating airborne particles, including tuberculosis (TB). The researchers developed a test procedure in a 36 m3 room where bacterial samples are cultured. Upon treatment, the findings indicated that the concentrations of B. subtilis, Micrococcus luteus (M. luteus), and E. coli were all suppressed by 50% and nearly 100%, respectively, by a single 15 W germicidal lamp(Miller and MacHer 2000). Another study aimed to determine at what extent an automated UV-C lamp could eradicate bioburden from hospital’s computer keyboards. Upon treatment against Staphylococcus, Streptococcus, Enterococcus, Pseudomonas, Pasteurella, Klebsiella, Acinetobacter, and Enterobacter, a reduction of greater than 99% in bacteria was observed when pre- and post-UV decontamination median CFU counts were compared. The study therefore validated the performance of UV lamps for disinfecting keyboards existed in healthcare (Gostine et al. 2016).
PX-UV lamps inactivation experiments
Several researches have revealed the effectiveness of PPX-UV in reducing the total environmental bioburden, which suggests its potential to be utilized in conjunction with standard cleaning techniques (Green et al. 2017). One study has shown the effectiveness of a UV-C disinfection system (Codonics D6000™) in lessening contamination on mobile device screens and protective cases. According to the study, the Codonics D6000™ PX-UV-C disinfection equipment managed to keep tablets and cell phones used in healthcare facilities disinfected following the routine treatment (Muzslay et al. 2018), proving Codonics D600™ as an effective tool for disinfection. Three distinct types of handheld electronic devices (HEDs) that are regularly used in hospitals were identified as having infections in a various study. The effectiveness of employing UV-Smart® D25 to disinfect these devices with PX-UV-C radiation was investigated by the researchers (Cremers-Pijpers et al. 2021). The study employed 800 samples obtained from two departments. The results showed that colony-forming organisms were present in more than 50% of the initial measurements in moderately or highly contaminated settings. Yet, compared to the original measurement, 87% of samples following disinfection showed no signs of CFU. According to the study, the UV-Smart® D25 could serve as an effective method for routinely disinfecting non-critical HEDs. In Japan, the effectiveness of PX-UV disinfection in reducing contamination of medical facilities was studied. MDRO containing C. difficile spores were subjected to PX-UV which are often found in hospitals. The results showed that PX-UV disinfection for 15 min significantly reduced the growth of C. difficile spores by more than 3-log CFU/cm2, while PX-UV disinfection for 5 min significantly reduced the growth of all MDRO by more than 5-log CFU/cm2. According to the study, clinical MDROs containing C. difficile responded effectively to PX-UV disinfection (Kitagawa et al. 2020). In one similar study, the research was carried out in 23 hospitals across the USA to validate the PX-UV disinfection’s capability for minimizing contamination on high-touch surfaces in operating rooms (ORs) following manual cleaning. Surface specimens from 732 high-touch surfaces in 136 ORs were obtained. The results revealed that manual cleaning alone only eliminated 67% of the bacteria from surfaces, whereas PX-UV disinfection reduced the number of positive surfaces to 38%, indicating a reduction of 44%. According to the study, PX-UV disinfection, when used after deep cleaning, significantly lowers the contamination on high-touch surfaces specially in ORs (Simmons et al. 2018). The viral load on hard surfaces and N95 respirators was also examined by Simmons et al. (2021) to evaluate the performance of PX-UV disinfection system. According to the findings, the PX-UV disinfection for 1, 2, and 5 min lowered the viral load on hard surfaces by 3.53 log10, > 4.54 log10, and > 4.12 log10. N95 respirators were disinfected with PX-UV for five mins, which lowered the pathogen load by > 4.79 log10. These findings confirmed the efficiency of PX-UV at reducing the load of SARS-CoV-2 on N95 respirators as well as on hard surfaces. Another study assessed the effect of portable PX-UV devices on the microbiological load in four Veterans Affairs hospitals. The study compared the manual cleaning and PX-UV disinfection at two locations. As compared to only 25–30% with manual cleaning alone, the results showed that PX-UV significantly reduced aerobic bacteria counts and MRSA by 75.3 and 84.1%, respectively. The researcher recommends using PX-UV devices in routine cleaning to lessen the infectious burden typically brought on by aerobic bacteria and MRSA (Zeber et al. 2018). Another study looked at how well a PX-UV disinfection system worked to reduce the environmental bacterial load and pathogens that form biofilms on surfaces in clinical laboratories (Chen et al. 2020). According to the results obtained, PX-UV was able to significantly reduce the colony counts of P. aeruginosa, S. aureus, and K. pneumoniae. The authors suggested the use of PX-UV as a potent UV source for disinfection in clinical laboratories. In a similar research, another investigation examined PX-UV against two Candida species: C. auris and C. parapsilosis, that are commonly associated with epidemics in hospital environments and persist on surfaces for a prolonged time. During a 5 min cycle at 1 m distance, the study reported 99.4 and 98.5% reduction in C. auris and in C. parapsilosis, respectively, making PX-UV a significant approach for disinfection (Maslo et al. 2019).
UV-C LEDs inactivation experiments
UV-C LEDs have recently come into focus by researchers due to the several advantages over conventional lamps and robots. In one recently investigated study, Nunayon et al. (2020) evaluated the antimicrobial efficacy of upper-room UV germicidal irradiation LEDs (UR-UVGI-LEDs) at 270 nm (schematically represented in Fig. 6) for disinfecting bioaerosols in enclosed environments. The efficiency of the UR-UVGI-LED at 270 nm was contrasted with that of the more traditional UR-UVGI mercury vapor lamps at 254 nm. The results revealed that the effectiveness of both systems for disinfection against S. marcescens and E. coli was comparable, and that the UR-UVGI-LED system had the most potential to be a credible source of disinfection against indoor airborne pathogens. Another study utilized UV-C LED irradiation to evaluate the antibacterial effectiveness on toilet seats against three bacterial strains (Lai and Nunayon 2021). The study utilized three different combinations (3, 5-two variants, and 8-LEDs), as well as two different 5-LED configurations for evaluation. According to the study, the effectiveness of disinfection initially rose with the number of LEDs but decreased with 8 LEDs. This concluded the mean disinfection efficiency for surfaces and aerosols, which varied from 8.81 to 72.80% and 24.16 to 70.70%, respectively. Another recent review highlighted the key factors which offers several advantages to LEDs in comparison with traditional mercury vapor lamps (MVL), such as longer lifecycle, robustness, compactness, flexibility, and the absence of non-hazardous material. The review found that UV-C LEDs have been applied in various fields, ranging from health applications to wastewater or food decontamination, and in some cases, LEDs even provide better results than MVLs. The complexity of the targets being decontaminated, such as multilayers or thicker individual layers, might, however, reduce the effectiveness of UV-C disinfection (Nicolau et al. 2022). The SMD LEDs are not being in focus by the researchers due to its compact design and availability of various package sizes. One of the most recent studies by Sheikh et al. (2023) evaluated the effectiveness of Everlight’s 275 nm UV-C surface mounted device (SMD) against S. aureus by quantifying inhibitory zones at varied exposure settings. The results reported that at longer exposure times larger inhibition zones were produced. In a similar study by Sheikh et al. (2021), the impact of 275 nm UV-C LED on human skin fibroblast cells and bacteria (P. aeruginosa, S. aureus) was investigated for prototyping a wound disinfection system. The study employed quantitative analysis in which bacterial inhibition zones at three exposure distances and two exposure durations were assessed. The results demonstrated that greater inhibition zones were caused by longer exposure durations and distances. The study also confirmed that the low exposure duration did not affect human skin cells and found out the viability within the acceptable level which can be adequate for wound treatment. A regular 3 mm LED emitting visible light was also compared to UV-A LED in one of the investigations by Malik et al. (2017) against E. coli. In comparison, the UV-A LED samples reached maximal inactivation with only 0.0043 × 106 CFU/mL, while the conventional LED, which lacks UV light emission, failed to achieve any microbial inactivation. Another study assessed the inactivation of biofilm-bound P. aeruginosa by employing a 265 nm UV-C LED. The bacterial load was observed to reduce to a factor of 1.3 ± 0.2 log10, which was lower than that of planktonic P. aeruginosa when inactivated by UV-C LEDs. This result attributed to the greater UV inactivation resistance shown by bacteria that were already attached to biofilms (Gora et al. 2019). In another recent research by Nyangaresi et al. (2023), the efficacy of single UV-C and combined UV-A and UV-C LED irradiation in eradicating various waterborne bacteria was evaluated. The study found that the sensitivity of the different bacteria to UV radiation varied, and that only E. coli produced evidence of healing. The synergistic effect seen in E. coli and B. spizizenii spores was attributable to the different inactivation processes of UV-C and UV-A wavelengths. In comparison with the 267 nm UV-C LED, which had the highest inactivation efficiency, the 278 nm UV-C LED had a better inactivation efficacy and required less energy. Yang et al. (2019) additionally evaluated the Hyper Light Disinfection Robot, an automatic mobile device that used UV-C irradiation to kill pathogens that are MDR, including P aeruginosa, A. baumannii, MRSA, VRE, M. abscess. After 5 min of UV-C irradiation at a distance of 3 m from the device, vegetative bacteria colonies were reduced by a factor of more than 3 log10 with the exception of VRE and M. abscessus, proving the device's effectiveness in eliminating MDR pathogens. Also, at a distance of 1 m, substantial reductions in colony counts were seen for all examined microorganisms, regardless of exposure time. The effectiveness of various UV-C radiation wavelengths for inactivating SARS-CoV-2 on high and low-touch surfaces and in indoor air was also examined in the study by Liang et al. (2021). The efficacy of the prototype UV-C light devices was examined using cell-based assays using UV-C light with wavelengths of 275, 254, and 222 nm. The UV-C LED (275 nm), followed by the mercury lamp (254 nm) and the excimer lamp (222 nm), exhibited the best viricidal activity against SARS-CoV-2, according to the data. In comparison with the other lights, the UV-C LED (275 nm) showed superior SARS-CoV-2 disinfection activity. Furthermore, in one study, the effectiveness of 222-nm UV-LED in eradicating MRSA and aerobic bacteria (AB) on mobile phone surfaces was investigated by Kaiki et al. (2021). It was reported in the study that mean log10 MRSA CFU reductions of 2.91 and 3.95, respectively, were attained following exposure for 1.5 and 2.5 min. Moreover, 9 mJ/cm2 of dose was required to significantly decrease mobile phone AB contamination. In a different pilot crossover trial that was carried out in November 2017, surgical tools that had been infected with S. aureus, E. faecalis, P. aeruginosa, and S. marcescens were placed in a box reactor comprising a number of UV-C LED light sources. It was noticed after being exposed for 10 min, the findings revealed no evidence of bacterial growth, demonstrating the high degree of disinfection efficacy of the UV-C device. These findings suggest that the device’s capacity to eliminate bacterial contamination from surgical instruments may have a significant effect on the reduction in infections associated with medical care (Spataro et al. 2019). The study conducted by Guettari et al. (2021) also examined the use of UV-C LED radiation as a physical disinfectant to prevent the spread of COVID-19 in confined spaces including hospitals, public transportation, and airlines. The article researchers claimed that the i-Robot UV-C robot was able to eradicate 99.999% of bacteria and viruses using i-Robot.
Various studies (see Table 5) have been conducted using UV technologies for the purpose of disinfection and to assess their antimicrobial efficacy. One such comparative investigation (Raeiszadeh and Adeli 2020) was conducted to evaluate the effectiveness of MP, LP, and UV-C LEDs by comparing the actual UV susceptibility of E. coli bacterium and MS-2 virus to the UV absorption value of DNA and RNA (Fig. 7A). It was observed that a UV-LED with a peak wavelength of 265 nm had 1.15 times higher germicidal power than a standard 274 nm mercury UV lamp for inactivation. In other words, compared to a UV disinfection system with a 254 nm, a system with a 265 nm emitting UV source required lower UV dose to accomplish the same amount of DNA/RNA damage. In order to determine the germicidal effectiveness of a UV disinfection system, it is essential to comprehend how the SPD of the UV source being used (Fig. 7C) interacts with the UV susceptibility of microorganisms over the UV-C spectrum. Moreover, as illustrated in Fig. 7B, absorbed UV-C photons could severely damage the genomic structure of microorganisms, impairing their ability to replicate and survive. The adenine–thymine bond collapses, and a covalent linkage identified as a pyrimidine dimer develops between two adenines as a result, rendering the cell incapable of replicating. Because of this, the impact of UV irradiation on microorganisms is referred to as “inactivation” rather than “killing.”
A The germicidal region’s relative UV susceptibility of a generic RNA or DNA, as well as E. coli bacterium and MS2 virus, B Thymine dimerization schematic representation for a UV-exposed double-stranded DNA, C SPD of various germicidal UV sources. Reprinted from “A Critical Review on Ultraviolet Disinfection Systems against COVID-19 Outbreak: Applicability, Validation, and Safety Considerations,” M. Raeiszadeh., ACS Photonics, Copyright 2020 (Raeiszadeh and Adeli 2020)
Study remarks, gaps, and future perspective
The hospital contaminated environment has shown to be an issue of serious concern and it continues to be a major origin for transmitting microorganisms to the healthy individuals. The everyday use of chemical disinfectants for cleaning and disinfection has raised serious concerns due to the fact that it gives rise to several complications while delivering insufficient disinfection (Sehulster 2003; Rutala and Weber 2016a; Canada 1998; Omidbakhsh et al. 2014; Han et al. 2015; Rutala et al. 2008). Also, it has been seen that the procedures that involve chemical products for cleaning purposes are less effective regardless of how expensive the products are Sheikh et al. (2021). However, for such concerns, extensive studies have already been conducted to identify the methods which could significantly substitute the usage of chemical with “no-touch” disinfection technology for disinfection practices. As a result, the interest in an alternative disinfection method is continuing to grow particularly in healthcare facilities. In such regards, researchers have come across UV technologies which have drawn a significant attention due to its efficient and practical capacity to disinfect water, food, air, and surfaces (Kaiki et al. 2021; Duering et al. 2023; Hessling et al. 2023, 2021; Mariita et al. 2022; Nunayon et al. 2022; Nyhan, et al. 2021; Gardner et al. 2021; Grist et al. 2021; Rios de Souza et al. 2020; Cheng et al. 2020; Vernez et al. 2020; Mitchell et al. 2019b; Wallace et al. 2019; Alhmidi et al. 2018; Kim et al. 2017; Kim et al. 2015; Boyce et al. 2016b; Anderson et al. 2013; Mahida et al. 2013; Moore et al. 2012; Sommers et al. 2010; Rutala et al. 2010; Yaun et al. 2004; Palma et al. 2022). Conventionally, low pressure (< 1 atm.) mercury lamps are employed (Liang et al. 2021; Kaiki et al. 2021; Spataro et al. 2019; Guettari et al. 2021; Raeiszadeh and Adeli 2020) to generate shorter wavelength UV radiation. Despite of its high level of disinfection, the component; mercury, poses hazard to the environment (Torok et al. 2016), rapidly absorbs into the skin or respiratory system, accumulates in the body, and frequently have a deadly toxic impact on human being (Palma et al. 2022). As a result, the United Nations Environment Program (UNEP) has formally announced an unconditional ban on the production of mercury-containing products after 2020 with the Minamata Convention on Mercury in 2013 (Larson 2014). This also implies that new approaches are required to replace mercury lamps, which could serve as reliable substitute of such technology and effectively serve as potential source for antibacterial procedures. In such regards, UV technologies have grabbed the attention due to its potential characteristics and advantages over liquid disinfectants as demonstrated in Fig. 8.
With recent advancements, all such limitations are certainly sidestepped by UV-C LEDs, which is why LEDs are gaining popularity in the recent times. Nevertheless, in addition to UV-C LEDs, other UV lamp types, such as the excimer technology (pulsed xenon lamps, krypton-chloride excimer lamps), have gained popularity and have shown to be a worthy replacement to LP mercury vapor lamp. Such technology has several benefits in common with UV-C LEDs, such as being free from the mercury component, longer lifespan with no warm-up requirement time. However, due to the pulsatile nature of these lamps and their poor efficacy, the use of excimer lamps, such as pulsed xenon lamps, in a continuous air disinfection system is limited (Szeto et al. 2020; SHCHEER 2017; Jarvis et al. 2019). UV-C LEDs, on the other side, have overcome such limitations in a number of ways, such as an absence of hazardous component such as mercury, non-pulsatile treatment and employing a metallic substance at a little extent that do not leak out in the case of breakdown or disposal. These LEDs additionally do not produce ozone nor have a high-power density and sustain minimal harm from repeated cycles. Moreover, it does not require warm-up time for maximum intensity output and emits light with various wavelengths. These benefits along with nearly swift starts and adjustable wavelengths offer an abundance of design autonomy for UV-C LED ballasts. It is also essential to emphasize the cost of UV-C LEDs as compared to conventional lamps where UV-C LEDs are typically thought to be more cost-effective. Furthermore, UV-C LEDs have a longer lifespan, which minimizes the need of frequent replacement, eventually giving benefit in terms of buyer’s expense by reducing the maintenance and replacement costs. UV-C LEDs are also a long-term financial option because of its lower energy consumption, which also lowers overall power expenses. By implementing such technology for disinfection in healthcare or other indoor settings, the operational expenses could be lessened while maintaining effective disinfection procedures by implementing the routine disinfection practices.
Conclusion
Ultraviolet (UV) disinfection technologies are tool for microbial prevention in indoor public places which are frequently employed for disinfecting air, surfaces, and water. In conclusion, our research supports the use of UV-C LEDs for environmental disinfection purposes due to its variety of advantages over chemical disinfectants and conventionally used other disinfection procedures utilizing UV technologies. Moreover, it is advisable to combine multiple LED arrays to enhance the overall irradiance and achieve greater disinfection over longer distances. Further research on the arrangement of LEDs and configuration of arrays to maximize intensity while guaranteeing uniform and sufficient UV-C radiation dispersion has a valuable prospect. However, the scalability and efficiency in various applications such as for outdoor environments where the treatment could be affected with the interference of other light sources should be examined. Additionally, ongoing research should also continue to investigate the possible threats to health and safety posed by UV-C LED technology in order to provide useful guidelines and safety measures. By considering all of this, UV-C LED can offer an effective and affordable solution for disinfection, improving hygiene and environmental sustainability. Therefore, it is clear that UV-C LED technologies are promising for disinfection of microorganism present in air, water, food or surface in the healthcare environment.
Change history
19 May 2024
Original version of this article corrected for figure 3 change.
Abbreviations
- HAI:
-
Healthcare associated infection
- ICU:
-
Intensive care unit
- EPIC:
-
Extended Prevalence of Infection in Intensive Care
- NI:
-
Nosocomial infection
- HCW:
-
Healthcare worker
- MDR:
-
Multidrug-resistant
- S. aureus :
-
Staphylococcus aureus
- E. faecium :
-
Enterococcus faecium
- K. pneumoniae :
-
Klebsiella pneumoniae
- A. baumannii :
-
Acinetobacter baumannii
- P. aeruginosa :
-
Pseudomonas aeruginosa
- MRSA:
-
Methicillin-resistant S. aureus
- E. coli :
-
Escherichia coli
- S. pneumoniae :
-
Streptococcus pneumoniae
- SSIs:
-
Surgical sites infections
- CDC:
-
Centers for disease control and prevention
- BSI:
-
Bloodstream infection
- CRBCI:
-
Catheter-related bloodstream infections
- LRTI:
-
Lower respiratory tract infections
- UTI:
-
Urinary tract infection
- C. albicans :
-
Candida albicans
- VAP:
-
Ventilator-associated pneumonia
- S. maltophilia :
-
Stenotrophomonas maltophilia
- HAP:
-
Hospital-acquired pneumonia
- K. oxytoca :
-
Klebsiella oxytoca
- S. marcescens :
-
Serratia marcescens
- S. maltophilia :
-
Stenotrophomonas maltophilia
- A. fumigatus :
-
Aspergillus fumigatus
- H. influenzae :
-
Haemophilus influenzae
- VRE:
-
Vancomycin-resistant enterococcus
- C. auris :
-
Candida auris
- P. mirabilis :
-
Proteus mirabilis
- C. parapsilosis :
-
Candida parapsilosis
- A. fumigatus :
-
Aspergillus fumigatus
- L. monocytogenes :
-
Listeria monocytogenes
- E. cloacae :
-
Enterobacter cloacae
- NTM:
-
Nontuberculous mycobacteria
- GN:
-
Gram-negative
- BWI:
-
Burn wound infections
- NB:
-
Nosocomial bacteremia
- REACH:
-
Researching Effective Approaches to Cleaning in Hospitals
- NTD:
-
No-touch automated disinfection
- VHP:
-
Vaporized hydrogen peroxide
- HPV:
-
Hydrogen peroxide vapor
- aHP:
-
Aerosolized hydrogen peroxide
- UV:
-
Ultraviolet
- LED:
-
Light-emitting diode
- PX:
-
Pulse xenon
- Hg:
-
Mercury
- LP:
-
Low pressure
- MP:
-
Medium pressure
- GaN:
-
Gallium nitride
- AGaN:
-
Aluminum gallium nitride
- SMD:
-
Surface mount device
- TB:
-
Tuberculosis
- M. luteus:
-
Micrococcus luteus
- HED:
-
Handheld electronic devices
- ORs:
-
Operating rooms
- UR-UVGI-LEDs:
-
Upper-room UV germicidal irradiation LEDs
- SPD:
-
Spectral power distribution
- MVL:
-
Mercury vapor lamps
- AB:
-
Aerobic bacteria
- UNEP:
-
United Nations Environment Program
- EPS:
-
Extracellular polymeric substances
- DSB:
-
Dry surface biofilms
References
Abdallah M et al (2015) Impact of growth temperature and surface type on the resistance of Pseudomonas aeruginosa and Staphylococcus aureus biofilms to disinfectants. Int J Food Microbiol 214:38–47
Adams CE et al (2017) Examining the association between surface bioburden and frequently touched sites in intensive care. J Hosp Infect 95(1):76–80
Alhmidi H et al (2018) Evaluation of an automated ultraviolet-C light disinfection device and patient hand hygiene for reduction of pathogen transfer from interactive touchscreen computer kiosks. Am J Infect Control 46(4):464–467
Allegranzi B (2011) Report on the burden of endemic health care-associated infection worldwide. World Health Organization (WHO), Geneva
Allegranzi B, Pittet D (2009) Role of hand hygiene in healthcare-associated infection prevention. J Hosp Infect 73(4):305–315
Allegranzi B et al (2007) The first global patient safety challenge “clean care is safer care”: from launch to current progress and achievements. J Hosp Infect 65(Suppl 2):115–123
Allegranzi B et al (2011) Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet 377(9761):228–241
Amini Tapouk F et al (2020) Comparative efficacy of hospital disinfectants against nosocomial infection pathogens. Antimicrob Resist Infect Control 9:115
Ananda T et al (2022) Nosocomial infections and role of nanotechnology. Bioengineering (basel) 9(2):51
Andersen BM et al (2006) Decontamination of rooms, medical equipment and ambulances using an aerosol of hydrogen peroxide disinfectant. J Hosp Infect 62(2):149–155
Anderson DJ (2011) Surgical site infections. Infect Dis Clin North Am 25(1):135–153
Anderson DJ et al (2013) Decontamination of targeted pathogens from patient rooms using an automated ultraviolet-C-emitting device. Infect Control Hosp Epidemiol 34(5):466–471
Apisarnthanarak A et al (2003) Ventilator-associated pneumonia in extremely preterm neonates in a neonatal intensive care unit: characteristics, risk factors, and outcomes. Pediatrics 112:1283–1289
Arques-Orobon FJ, Vazquez M, Nuñez N (2020) Lifetime analysis of commercial 3 W UV-A LED. Crystals 10(12):1083
Bal AM et al (2016) Genomic insights into the emergence and spread of international clones of healthcare-, community- and livestock-associated meticillin-resistant Staphylococcus aureus: blurring of the traditional definitions. J Glob Antimicrob Resist 6:95–101
Bardi T et al (2021) Nosocomial infections associated to COVID-19 in the intensive care unit: clinical characteristics and outcome. Eur J Clin Microbiol Infect Dis 40(3):495–502
Barnes M et al (2019) Antimicrobial polymer modifications to reduce microbial bioburden on endotracheal tubes and ventilator associated pneumonia. Acta Biomater 91:220–234
Beggs C et al (2015) Environmental contamination and hospital-acquired infection: factors that are easily overlooked. Indoor Air 25(5):462–474
Bernard L, Kereveur A, Durand D et al (1999) Bacterial contamination of hospital stethoscope. Infect Control Hosp Epidemiol 20:274–276
Best EL et al (2010) The potential for airborne dispersal of Clostridium difficile from symptomatic patients. Clin Infect Dis 50(11):1450–1457
Best E et al (2018) Environmental contamination by bacteria in hospital washrooms according to hand-drying method: a multi-centre study. J Hosp Infect 100(4):469–475
Bhalla A et al (2004) Acquisition of nosocomial pathogens on hands after contact with environmental surfaces near hospitalized patients. Infect Control Hosp Epidemiol 25:164–167
Bhatta DR et al (2018) Bacterial contamination of frequently touched objects in a tertiary care hospital of Pokhara, Nepal: how safe are our hands? Antimicrob Resist Infect Control 7:97
Blanco-Cabra N et al (2019) Novel oleanolic and maslinic acid derivatives as a promising treatment against bacterial biofilm in nosocomial infections: an in vitro and in vivo study. ACS Infect Dis 5(9):1581–1589
Bolon MK et al (2016) Hand hygiene: an update. Infect Dis Clin N Am 310:591–607
Bolton JR, Cotton CA (2008) The ultraviolet disinfection handbook, 1st edn. American Water Works Association
Bonten MJ et al (1996) Epidemiology of colonisation of patients and environment with vancomycin-resistant enterococci. Lancet 348(9042):1615–1619
Borrusso PA, Quinlan JJ (2017) Prevalence of pathogens and indicator organisms in home kitchens and correlation with unsafe food handling practices and conditions. J Food Prot 80(4):590–597
Bouchra O et al (2019) Environmental surfaces in healthcare setting: a great potential risk of pathogens transmission. J Adv Microbiol 28:2398–2401
Boyce JM (2007) Environmental contamination makes an important contribution to hospital infection. J Hosp Infect 65(Suppl 2):50–54
Boyce JM et al (1997) Environmental contamination due to meticillin-resistant Staphylococcus aureus: possible infection control implications. Infect Control Hosp Epidemiol 18(8):622–627
Boyce JM et al (2016a) Modern technologies for improving cleaning and disinfection of environmental surfaces in hospitals. Antimicrob Resist Infect Control 5:10
Boyce JM et al (2016b) Impact of room location on UV-C irradiance and UV-C dosage and antimicrobial effect delivered by a mobile UV-C light device. Infect Control Hosp Epidemiol 37(6):667–672
Brêda M et al (2021) Potential application of novel technology developed for instant decontamination of personal protective equipment before the doffing step. PLoS ONE 16:e0250854
Canada H (1998) Infection control guidelines: hand washing, cleaning, disinfection, and sterilization in health care. In Canadian Communicable Disease Report. pp 1–55
Caselli E et al (2018) Reducing healthcare-associated infections incidence by a probiotic-based sanitation system: a multicentre, prospective, intervention study. PLoS ONE 13(7):e0199616
Chemaly RF et al (2014) The role of the healthcare environment in the spread of multidrug-resistant organisms: update on current best practices for containment. Ther Adv Infect Dis 2(3–4):79–90
Chen KH, Chen LR, Wang YK (2014) Contamination of medical charts: an important source of potential infection in hospitals. PLoS ONE 9(2):e78512
Chen LF et al (2019) A prospective study of transmission of multidrug-resistant organisms (MDROs) between environmental sites and hospitalized patients-the TransFER study. Infect Control Hosp Epidemiol 40(1):47–52
Chen LH et al (2020) Evaluation of a pulsed xenon ultraviolet light device for reduction of pathogens with biofilm-forming ability and impact on environmental bioburden in clinical laboratories. Photodiagnosis Photodyn Ther 29:101544
Chen YC et al (2021) Comparing visual inspection and performance observation for evaluation of hospital cleanliness. Am J Infect Control 48:1511–1514
Cheng Y et al (2020) Inactivation of Listeria and E. coli by Deep-UV LED: effect of substrate conditions on inactivation kinetics. Sci Rep 10(1):3411
Chou DT et al (2012) The world health organization ‘5 moments of hand hygiene’: the scientific foundation. J Bone Jt Surg Br 94:441–445
Chowdhury D et al (2018) Transfer of dry surface biofilm in the healthcare environment: the role of healthcare workers’ hands as vehicles. J Hosp Infect 100(3):e85–e90
Christiansen B, Dettenkofer M, Becker E (2004) Anforderungen an die Hygiene bei der Reinigung und Desinfektion von Flächen. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz 47:51–61
Claus H (2021) Ozone generation by ultraviolet lamps(dagger). Photochem Photobiol 97(3):471–476
CMS. Centers for Medicare and Medicaid Services. Hospital Inpatient Quality Reporting Program (2023) https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/hospitalrhqdapu.html
Comar M et al (2019) Introduction of NGS in environmental surveillance for healthcare-associated infection control. Microorganisms 7(12):708
Conner-Kerr TA, Sullivan P, Gaillard J, Franklin ME, Jones RM (1998) The effects of ultraviolet radiation on antibiotic-resistant bacteria in vitro. Ostomy Wound Manag 44:50–56
Correa TQ et al (2017) Manual operated ultraviolet surface decontamination for healthcare environments. Photomed Laser Surg 35(12):666–671
Crawford MH et al (2005) Final LDRD report: ultraviolet water purification systems for rural environments and mobile applications. Sandia Rep 1:37
Cremers-Pijpers S et al (2021) Disinfecting handheld electronic devices with UV-C in a healthcare setting. Infect Prev Pract 3(2):100133
Danasekaran R, Mani G, Annadurai K (2014) Prevention of healthcare-associated infections: protecting patients, saving lives. Int J Community Med Public Health 1(1):67
Dancer SJ (2014) Controlling hospital-acquired infection: focus on the role of the environment and new technologies for decontamination. Clin Microbiol Rev 27(4):665–690
Dancer SJ et al (2009) Measuring the effect of enhanced cleaning in a UK hospital: a prospective cross-over study. BMC Med 7:28
Dancer SJ et al (2019) Tracking Staphylococcus aureus in the intensive care unit using whole-genome sequencing. J Hosp Infect 103(1):13–20
Dantes R et al (2013) National burden of invasive methicillin-resistant Staphylococcus aureus infections, United States, 2011. JAMA Intern Med 173(21):1970–1978
Darge A et al (2019) Bacterial contamination and antimicrobial susceptibility patterns of intensive care units medical equipment and inanimate surfaces at Ayder comprehensive specialized hospital, Mekelle, Northern Ethiopia. BMC Res Notes 12(1):621
Darvishi M, Forootan M, Nazer MR et al (2020) Nosocomial infections, challenges and threats: a review article. J Med Microbiol 14:162–181
Datta R et al (2011) Environmental cleaning intervention and risk of acquiring multidrug-resistant organisms from prior room occupants. Arch Intern Med 171:491–494
de Boer HEL, van Elzelingen-Dekker CM (2006) Use of gaseous ozone for eradication of methicillin-resistant Staphylococcus aureus from the home environment of a colonized hospital employee. Infect Control Hosp Epidemiol 27(10):1120–1122
de Souza RV et al (2020) A comparative study on the inactivation of Penicillium expansum spores on apple using light emitting diodes at 277 nm and a low-pressure mercury lamp at 253.7 nm. Food Control 110:107039
Deshpande A et al (2017) Are hospital floors an underappreciated reservoir for transmission of health care-associated pathogens? Am J Infect Control 45(3):336–338
Desrousseaux C et al (2013) Modification of the surfaces of medical devices to prevent microbial adhesion and biofilm formation. J Hosp Infect 85(2):87–93
Ding X et al (2019) Causative agents and outcome of spontaneous bacterial peritonitis in cirrhotic patients: community-acquired versus nosocomial infections. BMC Infect Dis 19(1):463
Diseases and Organisms in Healthcare Settings, CDC (2016) Healthcare-associated Infections (HAIs). https://www.cdc.gov/hai/organisms/organisms.html#print
Dizaj SM et al (2014) Antimicrobial activity of the metals and metal oxide nanoparticles. Mater Sci Eng C 44:278–284
Donskey CJ (2013) Does improving surface cleaning and disinfection reduce health care-associated infections? Am J Infect Control 41(5 Suppl):S12–S19
Donskey CJ (2019) Decontamination devices in health care facilities: practical issues and emerging applications. Am J Infect Control 47S:A23–A28
Drees M et al (2008) Prior environmental contamination increases the risk of acquisition of vancomycin-resistant enterococci. Clin Infect Dis 46(5):678–685
Du Q, Zhang D, Hu W et al (2021) Nosocomial infection of COVID-19: a new challenge for healthcare professionals (Review). Int J Mol Med 47:31
Duering H et al (2023) Short-wave ultraviolet-light-based disinfection of surface environment using light-emitting diodes: a new approach to prevent health-care-associated infections. Microorganisms 11(2):386
Dumford DM 3rd et al (2009) What is on that keyboard? Detecting hidden environmental reservoirs of Clostridium difficile during an outbreak associated with North American pulsed-field gel electrophoresis type 1 strains. Am J Infect Control 37(1):15–19
El Haddad L et al (2017) Evaluation of a pulsed xenon ultraviolet disinfection system to decrease bacterial contamination in operating rooms. BMC Infect Dis 17(1):672
Elbehiry A et al (2022) The development of technology to prevent, diagnose, and manage antimicrobial resistance in healthcare-associated infections. Vaccines 10:2100
Engur D et al (2014) A milk pump as a source for spreading Acinetobacter baumannii in a neonatal intensive care unit. Breastfeed Med 9(10):551–554
Esteves DC et al (2016) Influence of biological fluids in bacterial viability on different hospital surfaces and fomites. Am J Infect Control 44(3):311–314
Falk PS et al (2000) Outbreak of vancomycin-resistant enterococci in a burn unit. Infect Control Hosp Epidemiol 21(9):575–582
Friedman MM et al (1996) Designing an infection control to meet JCAHO standards. Caring 15:18–25
Gamage SD et al (2016) Water safety and legionella in health care: priorities, policy, and practice. Infect Dis Clin North Am 30(3):689–712
Gardner A et al (2021) Virucidal efficacy of blue LED and far-UVC light disinfection against feline infectious peritonitis virus as a model for SARS-CoV-2. Viruses 13(8):1436
Gaston KJ et al (2012) Reducing the ecological consequences of night-time light pollution: options and developments. J Appl Ecol 49(6):1256–1266
Geadas Farias P et al (2017) Hospital microbial surface colonization revealed during monitoring of Klebsiella spp., Pseudomonas aeruginosa, and non-tuberculous mycobacteria. Antonie Van Leeuwenhoek 110(7):863–876
Gestrich SA et al (2018) A multicenter investigation to characterize the risk for pathogen transmission from healthcare facility sinks. Infect Control Hosp Epidemiol 39:1467–1469
Glowicz JB et al (2023) SHEA/IDSA/APIC practice recommendation: strategies to prevent healthcare-associated infections through hand hygiene: 2022 update. Infect Control Hosp Epidemiol 44:355–376
Gora SL et al (2019) Inactivation of biofilm-bound Pseudomonas aeruginosa bacteria using UVC light emitting diodes (UVC LEDs). Water Res 151:193–202
Gostine A et al (2016) Evaluating the effectiveness of ultraviolet-C lamps for reducing keyboard contamination in the intensive care unit: a longitudinal analysis. Am J Infect Control 44(10):1089–1094
Green J, Wright PA, Gallimore CI et al (1998) The role of environmental contamination with small round structured viruses in a hospital outbreak investigated by reverse-transcriptase polymerase chain reaction assay. J Hosp Infect 39:39–45
Green C et al (2017) Pulsed-xenon ultraviolet light disinfection in a burn unit: Impact on environmental bioburden, multidrug-resistant organism acquisition and healthcare associated infections. Burns 43(2):388–396
Grist SM et al (2021) Current understanding of ultraviolet-C decontamination of N95 filtering facepiece respirators. Appl Biosaf 26(2):90–102
Guerrero DM et al (2012) Acquisition of spores on gloved hands after contact with the skin of patients with Clostridium difficile infection and with environmental surfaces in their rooms. Am J Infect Control 40(6):556–558
Guerrero-Beltr·n JA, Barbosa-C·novas GV (2016) Advantages and limitations on processing foods by UV light. Food Sci Technol Int 10(3):137–147
Guerrero-Beltrán JA et al (2004) Review: advantages and limitations on processing foods by UV light. Int J Food Sci Technol 10:137–147
Guettari M, Gharbi I, Hamza S (2021) UVC disinfection robot. Environ Sci Pollut Res Int 28(30):40394–40399
Guinea J (2014) Global trends in the distribution of Candida species causing candidemia. Clin Microbiol Infect 20(Suppl 6):5–10
Gusev I et al (2022) Electrochemically deposited zinc (tetraamino)phthalocyanine as a light-activated antimicrobial coating effective against S. Aureas. Materials 15:975
Hall L et al (2020) Effectiveness of a structured, framework-based approach to implementation: the researching effective approaches to cleaning in hospitals (REACH) trial. Antimicrob Resist Infect Control 9(1):35
Han J et al (1998) AlGaN/GaN quantum well ultraviolet light emitting diodes. Appl Phys Lett 73(12):1688–1690
Han JH et al (2015) Cleaning hospital room surfaces to prevent health care-associated infections: a technical brief. Ann Intern Med 163(8):598–607
Hanczvikkel A, Víg A, Tóth Á (2018) Survival capability of healthcare-associated, multidrug-resistant bacteria on untreated and on antimicrobial textiles. J Ind Text 48(7):1113–1135
Haque M et al (2018) Health care-associated infections - an overview. Infect Drug Resist 11:2321–2333
Hardy KJ et al (2007) Rapid recontamination with MRSA of the environment of an intensive care unit after decontamination with hydrogen peroxide vapour. J Hosp Infect 66(4):360–368
Hassan K, ElBagoury M (2018) The domestic kitchen – the ‘front line in the battle against foodborne disease.’ J Pure Appl Microbiol 12(1):181–187
Hayden MK et al (2008) Risk of hand or glove contamination after contact with patients colonized with vancomycin-resistant enterococcus or the colonized patients’ environment. Infect Control Hosp Epidemiol 29(2):149–154
Hessling M, Sicks B, Lau B (2023) Far-UVC radiation for disinfecting hands or gloves? Pathogens 12(2):213
Hessling M et al. (2021) Review of microbial touchscreen contamination for the determination of reasonable ultraviolet disinfection doses. GMS Hygiene and Infection Control, 16
Hollosy F et al (2002) Effects of ultraviolet radiation on plant cells. Micron 33:179–197
Huslage K, Rutala WA (2010) A quantitative approach to defining “high-touch” surfaces in hospitals. Infect Control Hospital Epidemiol 31(8):850–853
Jamal M, Ahmad W, Andleeb S et al (2017) Bacterial biofilms and associated infections. J Chin Med Assoc 81:7–11
Jang SH et al (2010) Fabrication and thermal optimization of LED solar cell simulator. Curr Appl Phys 10:S537–S539
Jarvis P et al (2019) Application of ultraviolet light-emitting diodes (UV-LED) to full-scale drinking-water disinfection. Water 11(9):1894
Jinadatha C et al (2014) Evaluation of a pulsed-xenon ultraviolet room disinfection device for impact on contamination levels of methicillin-resistant Staphylococcus aureus. BMC Infect Dis 14:1–7
Jinadatha C et al (2015) Can pulsed xenon ultraviolet light systems disinfect aerobic bacteria in the absence of manual disinfection? Am J Infect Control 43(4):415–417
Joshi SG (2013) Acinetobacter baumannii: an emerging pathogenic threat to public health. World J Clinic Infect Dis 3(3):25
Juan C, Pena C, Oliver A (2017) Host and pathogen biomarkers for severe Pseudomonas aeruginosa infections. J Infect Dis 215(suppl 1):S44–S51
Jury LA et al (2010) Evaluation of an alcohol-based power sanitizing system for decontamination of hospital rooms of patients with methicillin-resistant Staphylococcus aureus carriage. Am J Infect Control 38(3):234–236
Kaiki Y et al (2021) Methicillin-resistant Staphylococcus aureus contamination of hospital-use-only mobile phones and efficacy of 222-nm ultraviolet disinfection. Am J Infect Control 49(6):800–803
Kalil AC et al (2016) Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the infectious diseases society of America and the American thoracic society. Clin Infect Dis 63(5):e61–e111
Kanamori H et al (2016) Healthcare outbreaks associated with a water reservoir and infection prevention strategies. Clin Infect Dis 62:1423–1435
Karlowsky JA et al (2017) Antimicrobial susceptibility of Gram-negative ESKAPE pathogens isolated from hospitalized patients with intra-abdominal and urinary tract infections in Asia-Pacific countries: SMART 2013–2015. J Med Microbiol 66(1):61–69
Katsuse Kanayama A et al (2017) Staphylococcus aureus surface contamination of mobile phones and presence of genetically identical strains on the hands of nursing personnel. Am J Infect Control 45(8):929–931
Kelly S et al (2022) Effectiveness of ultraviolet-C vs aerosolized hydrogen peroxide in ICU terminal disinfection. Hosp Infect 121:114–119
Kessler R (2013) The minamata convention on mercury: a first step toward protecting future generations. Environ Health Perspect 121(10):A304–A309
Kh S et al (2017) Bacterial contamination of hospital surfaces according to material make, last time of contact and last time of cleaning/disinfection. J Bacteriol Parasitol 08(03):9597
Khan MA et al (2005) III–Nitride UV devices. Jpn J Appl Phys 44:10
Khattak SU et al (2015) Study of the genetic traits associated with antibiotic resistance in Staphylococcus aureus isolated from skin wards of Khyber Pakhtunkhwa, Pakistan. Asian Pac J Trop Dis 5(5):393–398
Kim S-J et al (2015) Inactivating foodborne pathogens by using UV-C-LEDs at wavelengths from 266 to 279 nm and application to pasteurize sliced cheese. Appl Environ Microbiol 82:11–17
Kim SJ, Kim DK, Kang DH (2016) Using UVC light-emitting diodes at wavelengths of 266 to 279 nanometers to inactivate foodborne pathogens and pasteurize sliced cheese. Appl Environ Microbiol 82(1):11–17
Kim DK, Kim SJ, Kang DH (2017) Bactericidal effect of 266 to 279nm wavelength UVC-LEDs for inactivation of gram positive and gram negative foodborne pathogenic bacteria and yeasts. Food Res Int 97:280–287
Kitagawa H et al (2020) Efficacy of pulsed xenon ultraviolet disinfection of multidrug-resistant bacteria and Clostridioides difficile spores. Infect Dis Health 25(3):181–185
Klaus P et al (2003) Disinfection of surfaces by photocatalytic oxidation with titanium dioxide and UVA light. Chemosphere 52(1):71–77
Koganti S et al (2016) Evaluation of hospital floors as a potential source of pathogen dissemination using a nonpathogenic virus as a surrogate marker. Infect Control Hosp Epidemiol 37(11):1374–1377
Kollef MH et al (2008) Silver-coated endotracheal tubes and incidence of ventilator-associated pneumonia: the NASCENT randomized trial. JAMA Intern Med 300:805–813
Koscova J, Hurnikova Z, Pistl J (2018) Degree of bacterial contamination of mobile phone and computer keyboard surfaces and efficacy of disinfection with chlorhexidine digluconate and triclosan to its reduction. Int J Environ Res Public Health 15(10):2238
Koshi E et al (2011) Antimicrobial photodynamic therapy: an overview. J Indian Soc Periodontol 15(4):323
Koutchma T, Popović V, Green A (2019) Overview of ultraviolet (UV) LEDs technology for applications in food production. Ultraviolet LED technology for food applications. Elsevier, pp 1–23
Kowalski W (2009) UVGI disinfection theory. Ultraviolet germicidal irradiation handbook. Springer, New York, pp 17–50
Kowalski W et al (2009) Introduction. Ultraviolet germicidal irradiation handbook. Springer, New York
Kowalski W et al (2009a) UVGI lamps and fixtures. Ultraviolet germicidal irradiation handbook. Springer, New York
Kowalski W et al (2009b) UVGI guidelines and standards. Ultraviolet germicidal irradiation handbook. Springer, New York
Kramer A, Schwebke I, Kampf G (2006) How long do nosocomial pathogens persist on inanimate surfaces? a systematic review. BMC Infect Dis 6:130
Kranz S et al (2019) Bactericidal and biocompatible properties of plasma chemical oxidized titanium (TiOB®) with antimicrobial surface functionalization. Materials 12:866
Kumar J et al (2019) Environmental contamination with Candida species in multiple hospitals including a tertiary care hospital with a Candida auris outbreak. Pathog Immun 4(2):260–270
Kumari DN et al (1998) Ventilation grilles as a potential source of meticillin-resistant Staphylococcus aureus causing an outbreak in an orthopaedic ward at a district general hospital. J Hosp Infect 38:213–215
Kushwaha S (2011) A comprehensive study of various lamps through energy flow diagrams in ETEEE 2011
Lai ACK, Nunayon SS (2021) A new UVC-LED system for disinfection of pathogens generated by toilet flushing. Indoor Air 31(2):324–334
Lambert J et al (1998) Organic structural spectroscopy. Prentice Hall Inc., Upper Saddle River
Lamont Y et al. (2004) Effect of visible light exposure on E. coli treated with Pulsed UV-rich light. In: Conference record of the international power modulator symposium and high voltage workshop
Larson HJ (2014) The minamata convention on mercury: risk in perspective. Lancet 383(9913):198–199
Ledwoch K et al (2018) Beware biofilm! dry biofilms containing bacterial pathogens on multiple healthcare surfaces; a multi-centre study. J Hosp Infect 100(3):e47–e56
Lee K et al (2011) Multidrug-resistant Acinetobacter spp.: increasingly problematic nosocomial pathogens. Yonsei Med J 52(6):879–891
Levin J et al (2013) The effect of portable pulsed xenon ultraviolet light after terminal cleaning on hospital-associated Clostridium difficile infection in a community hospital. Am J Infect Control 41(8):746–748
Li Y et al (2017) Impact of nosocomial infections surveillance on nosocomial infection rates: a systematic review. Int J Surg 42:164–169
Liang JJ et al (2021) The effectiveness of far-ultraviolet (UVC) light prototype devices with different wavelengths on disinfecting SARS-CoV-2. Appl Sci 11(22):10661
Lim KS et al (2008) Chlorhexidine–pharmacology and clinical applications. Anaesth Intensive Care 36:502–512
Lin D et al (2017) A meta-analysis of the rates of Staphylococcus aureus and methicillin-resistant S aureus contamination on the surfaces of environmental objects that health care workers frequently touch. Am J Infect Control 45(4):421–429
Lindsay D et al (2006) Bacterial biofilms within the clinical setting: what healthcare professionals should know. J Hosp Infect 64:313–325
Liu J-Q et al (2017) Effect of flushing on the detachment of biofilms attached to the walls of metal pipes in water distribution systems. J Zhejiang Univ-SCIENCE A 18(4):313–328
Liu T et al (2023) Short-term effects of chlorhexidine mouthwash and listerine on oral microbiome in hospitalized patients. Front Cell Infect Microbiol 13:1056534
Loai S (2016) Development of a method for classification of hospitals based on results of the diagnosis-related groups and the principle of case-mix index. East Mediterr Health J 22(5):327–334
Magill SS et al (2014a) Multistate point-prevalence survey of health care-associated infections. N Engl J Med 370(13):1198–1208
Magill SS, Edwards JR, Bamberg W et al (2014b) The emerging infections program healthcare-associated infections and antimicrobial use prevalence survey team. Multistate point-prevalence survey of health care-associated infections. N Engl J Med 370:1198–1208
Magill SS et al (2018) Changes in prevalence of health care-associated infections in U.S. hospitals. N Engl J Med 379(18):1732–1744
Mahida N, Vaughan N, Boswell T (2013) First UK evaluation of an automated ultraviolet-C room decontamination device (Tru-D). J Hosp Infect 84(4):332–335
Maldonado J et al (2020) Label-free detection of nosocomial bacteria using a nanophotonic interferometric biosensor. Analyst 145(2):497–506
Malik SA et al (2017) Comparison of standard light-emitting diode (LED) and 385 nm ultraviolet A LED (UVA-led) for disinfection of Escherichia coli. Malaysian J Fundam Appl Sci 13:430–437
Mariita RM, Wilson Miller AC, Randive RV (2022) Evaluation of the virucidal efficacy of Klaran UVC LEDs against surface-dried norovirus. Access Microbiol 4(1):000323
Maslo C, du Plooy M, Coetzee J (2019) The efficacy of pulsed-xenon ultraviolet light technology on Candida auris. BMC Infect Dis 19(1):540
Masse J et al (2017) Colonization pressure as a risk factor of ICU-acquired multidrug resistant bacteria: a prospective observational study. Eur J Clin Microbiol Infect Dis 36:797–805
Matthew Mulle CA, Armstrong I (2018) Best practices for environmental cleaning for prevention and control of infections in all health care settings, P.H. Ontario, Editor. PIDAC
Miller SL, MacHer JM (2000) Evaluation of a methodology for quantifying the effect of room air ultraviolet germicidal irradiation on airborne bacteria. Aerosol Sci Technol 33(3):274–295
Miller SL, Linnes J, Luongo J (2013) Ultraviolet germicidal irradiation: future directions for air disinfection and building applications. Photochem Photobiol 89(4):777–781
Mitchell BG et al (2015) Risk of organism acquisition from prior room occupants: a systematic review and meta-analysis. J Hosp Infect 91(3):211–217
Mitchell BG et al (2018) Changes in knowledge and attitudes of hospital environmental services staff: the researching effective approaches to cleaning in hospitals (REACH) study. Am J Infect Control 46(9):980–985
Mitchell BG et al (2019a) An environmental cleaning bundle and health-care-associated infections in hospitals (REACH): a multicentre, randomised trial. Lancet Infect Dis 19(4):410–418
Mitchell JB et al (2019b) Modelling of ultraviolet light inactivation kinetics of methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococcus, Clostridium difficile spores and murine norovirus on fomite surfaces. J Appl Microbiol 126(1):58–67
Miyashita T, Ugawa S, Aoki A et al (2001) Photoinduced electron transfer processes in polymer Langmuir-Blodgett films. Stud Surf Sci Catal 132:451–456
Montero DA et al (2019) Antimicrobial properties of a novel copper-based composite coating with potential for use in healthcare facilities. Antimicrob Resist Infect Control 8:3
Moore G et al (2012) Use of UV-C radiation to disinfect non-critical patient care items: a laboratory assessment of the Nanoclave cabinet. BMC Infect Dis 12(1):174
Morgan DJ et al (2012) Transfer of multidrug-resistant bacteria to healthcare workers’ gloves and gowns after patient contact increases with environmental contamination. Crit Care Med 40(4):1045–1051
Morubagal RR, Shivappa SG et al (2017) Study of bacterial flora associated with mobile phones of healthcare workers and non-healthcare workers’. Iran J Microbiol 9:143–262
Muzslay M et al (2018) Ultraviolet-C decontamination of hand-held tablet devices in the healthcare environment using the Codonics D6000 disinfection system. J Hosp Infect 100(3):e60–e63
Nelson MU, Gallagher PG (2012) Methicillin-resistant Staphylococcus aureus in the neonatal intensive care unit. Semin Perinatol 36(6):424–430
Nicolau T et al (2022) A comprehensive analysis of the UVC LEDs’ applications and decontamination capability. Materials (basel) 15(8):2854
NLPIP (2010) Availability of LED lighting products for consumers. Lighting Answers, Editor
Nseir S et al (2011) Risk of acquiring multidrug-resistant Gram-negative bacilli from prior room occupants in the intensive care unit. Clin Microbiol Infect 17(8):1201–1208
Nunayon SS, Zhang H, Lai ACK (2020) Comparison of disinfection performance of UVC-LED and conventional upper-room UVGI systems. Indoor Air 30(1):180–191
Nunayon SS et al (2022) Evaluating the efficacy of a rotating upper-room UVC-LED irradiation device in inactivating aerosolized Escherichia coli under different disinfection ranges, air mixing, and irradiation conditions. J Hazard Mater 440:129791
Nyangaresi PO, Rathnayake T, Beck SE (2023) Evaluation of disinfection efficacy of single UV-C, and UV-A followed by UV-C LED irradiation on Escherichia coli, B. spizizenii and MS2 bacteriophage, in water. Sci Total Environ 859(Pt 1):160256
Nyhan L et al (2021) Investigating the use of ultraviolet light emitting diodes (UV-LEDs) for the inactivation of bacteria in powdered food ingredients. Foods 10(4):797
Olsen M et al (2020) Mobile phones represent a pathway for microbial transmission: a scoping review. Travel Med Infect Dis 35:101704
Omidbakhsh N, Ahmadpour F, Kenny N (2014) How reliable are ATP bioluminescence meters in assessing decontamination of environmental surfaces in healthcare settings? PLoS ONE 9(6):e99951
Van Osdell D et al. (2002) Defining the effectiveness of UV lamps installed in circulating air ductwork. In: Final Report, Air-Conditioning and Refrigeration Technology, Institute, Arlington, Virginia, p 22203
Otter JA, Yezli S, French GL (2011) The role played by contaminated surfaces in the transmission of nosocomial pathogens. Infect Control Hosp Epidemiol 32(7):687–699
Otter JA et al (2014) A guide to no-touch automated room disinfection (NTD) systems. Decontamination in hospitals and healthcare. Elsevier, pp 413–460
Pal S et al (2019) Staphylococcus aureus: a predominant cause of surgical site infections in a rural healthcare setup of Uttarakhand. J Family Med Prim Care 8(11):3600–3606
Palma F et al (2022) Use of eco-friendly UV-C LEDs for indoor environment sanitization: a narrative review. Atmosphere 13(9):1411
Pankove J et al (1873) Luminescence of insulating Be-doped and Li-doped GaN. J Lumin 8:89–93
Parker CM et al (2008) Ventilator-associated pneumonia caused by multidrug-resistant organisms or Pseudomonas aeruginosa: prevalence, incidence, risk factors, and outcomes. J Crit Care 23(1):18–26
Percival S, Cutting K (2010) Microbiology of wounds, 1st edn. CRC Press
Peters A et al (2018) Keeping hospitals clean and safe without breaking the bank; summary of the healthcare cleaning forum 2018. Antimicrob Resist Infect Control 7(1):3
Peters A et al (2022) Impact of environmental hygiene interventions on healthcare-associated infections and patient colonization: a systematic review. Antimicrob Resist Infect Control 11:38
Petti S (2016) Nano-TiO2-based photocatalytic disinfection of environmental surfaces contaminated by meticillin-resistant Staphylococcus aureus. J Hosp Infect 93(1):78–82
Polívková M et al (2017) Antimicrobial treatment of polymeric medical devices by silver nanomaterials and related technology. Int J Mol Sci 18:419
Raeiszadeh M, Adeli B (2020) A critical review on ultraviolet disinfection systems against COVID-19 outbreak: applicability, validation, and safety considerations. ACS Photon 7(11):2941–2951
Rajkhowa S (2020) Heat, solar pasteurization, and ultraviolet radiation treatment for removal of waterborne pathogens. Waterborne pathogens. Elsevier, pp 169–187
Ramasethu J (2017) Prevention and treatment of neonatal nosocomial infections. Matern Health Neonatol Perinatol 3:5
Rice LB (2008) Federal funding for the study of antimicrobial resistance in nosocomial pathogens: no ESKAPE. J Infect Dis 197(8):1079–1081
Rohr U et al (2009) Colonization of patients and contamination of the patients’ environment by MRSA under conditions of single-room isolation. Int J Hyg Environ Health 212(2):209–215
Rosenthal VD et al (2016) International nosocomial infection control consortium report, data summary of 50 countries for 2010–2015: device-associated module. Am J Infect Control 44(12):1495–1504
Rutala WA, Weber DJ (2013) Disinfectants used for environmental disinfection and new room decontamination technology. Am J Infect Control 41(5 Suppl):S36-41
Rutala WA, Weber DJ (2016a) Monitoring and improving the effectiveness of surface cleaning and disinfection. Am J Infect Control 44(5 Suppl):69–76
Rutala WA, Weber DJ (2016b) Disinfection and sterilization in health care facilities: an overview and current issues. Infect Dis Clin North Am 30(3):609–637
Rutala WA, Weber DJ (2019) Best practices for disinfection of noncritical environmental surfaces and equipment in health care facilities: a bundle approach. Am J Infect Control 47S:A96–A105
Rutala WA, Gergen MF, Weber DJ (2010) Room decontamination with UV radiation. Infect Control Hosp Epidemiol 31(10):1025–1029
Rutala WA et al (2018) Enhanced disinfection leads to reduction of microbial contamination and a decrease in patient colonization and infection. Infect Control Hosp Epidemiol 39(9):1118–1121
Rutala WA et al (2019) Antimicrobial activity of a continuously active disinfectant against healthcare pathogens. Infect Control Hosp Epidemiol 40(11):1284–1286
Rutala WA et al. (2008) Guideline for disinfection and sterilization in healthcare facilities. In Centers for Disease Control and Prevention. HICPAC
Rutala WA et al. (2008) Introduction, methods, definition of terms guideline for disinfection and sterilization in healthcare facilities, C.f.D.C.a. Prevention, Editor, CDC, Atlanta, GA
Ryan K et al (2010) Inactivation of airborne microorganisms using novel ultraviolet radiation sources in reflective flow-through control devices. Aerosol Sci Technol 44:541–550
Sarwar S et al (2023) Identifying and elucidating the resistance of Staphylococcus aureus isolated from hospital environment to conventional disinfectants. Am J Infect Control 51(2):178–183
Schalk S et al (2005) UV-lamps for disinfection and advanced oxidation - lamp types. IVA News 8:32–37
Schechner V et al (2011) Pseudomonas aeruginosa bacteremia upon hospital admission: risk factors for mortality and influence of inadequate empirical antimicrobial therapy. Diagn Microbiol Infect Dis 71(1):38–45
Schinas G, Polyzou E, Spernovasilis N et al (2023) Preventing multidrug-resistant bacterial transmission in the intensive care unit with a comprehensive approach: a policymaking manual. Antibiotics 12(8):1255
Sehulster L (2003) Guidelines for environmental infection control in health-care facilities: recommendations of the CDC and the healthcare infection control practices advisory committee (HICPAC), in recommendations and reports: morbidity and mortality weekly report. pp 1–42
Sexton JD et al (2011) Reduction in the microbial load on high-touch surfaces in hospital rooms by treatment with a portable saturated steam vapor disinfection system. Am J Infect Control 39(8):655–662
Shams AM et al (2016) Assessment of the overall and multidrug-resistant organism bioburden on environmental surfaces in healthcare facilities. Infect Control Hosp Epidemiol 37(12):1426–1432
Sharma VK, Demir HV (2022) Bright future of deep-ultraviolet photonics: emerging UVC chip-scale light-source technology platforms, benchmarking, challenges, and outlook for UV disinfection. ACS Photon 9(5):1513–1521
Shaughnessy MK et al (2011) Evaluation of hospital room assignment and acquisition of Clostridium difficile infection. Infect Control Hosp Epidemiol 32(3):201–206
SHCHEER (2017) Scientific Committee on Health, E.a.E.R., Opinion on biological effects of UV-C radiation relevant to health with particular reference to UV-C lamps
Sheikh J et al (2021) Bacterial disinfection and cell assessment post ultraviolet-C LED exposure for wound treatment. Med Biol Eng Comput 59(5):1055–1063
Sheikh J et al (2023) Surface bacterium disinfection using everlight 6565 UV-C SMD. HumEnTec 2:11–17
Sholtes KA et al (2016) Comparison of ultraviolet light-emitting diodes and low-pressure mercury-arc lamps for disinfection of water. Environ Technol 37(17):2183–2188
Sifuentes LY et al (2013) Microbial contamination of hospital reusable cleaning towels. Am J Infect Control 41(10):912–915
Simmons S et al (2013) Impact of a multi-hospital intervention utilising screening, hand hygiene education and pulsed xenon ultraviolet (PX-UV) on the rate of hospital associated meticillin resistant Staphylococcus aureus infection. J Infect Prev 14(5):172–174
Simmons S et al (2018) Environmental effectiveness of pulsed-xenon light in the operating room. Am J Infect Control 46(9):1003–1008
Simmons SE et al (2021) Deactivation of SARS-CoV-2 with pulsed-xenon ultraviolet light: implications for environmental COVID-19 control. Infect Control Hosp Epidemiol 42(2):127–130
Sitzlar B et al (2013) An environmental disinfection odyssey: evaluation of sequential interventions to improve disinfection of Clostridium difficile isolation rooms. Infect Control Hosp Epidemiol 34(5):459–465
Smith K, Hunter IS (2008) Efficacy of common hospital biocides with biofilms of multi-drug resistant clinical isolates. J Med Microbiol 57(Pt 8):966–973
Smith MA, Mathewson JJ, Ulert IA et al (1996) Contaminated stethoscopes revisited. Arch Intern Med 156:82–84
Sommers CH, Sites JE, Musgrove M (2010) Ultraviolet light (254 Nm) inactivation of pathogens on foods and stainless steel surfaces. J Food Saf 30(2):470–479
Sood G, Perl TM (2016) Outbreaks in health care settings. Infect Dis Clin North Am 30(3):661–687
Sooklal S, Khan A, Kannangara S (2014) Hospital Clostridium difficile outbreak linked to laundry machine malfunction. Am J Infect Control 42(6):674–675
Spataro G et al (2019) UV-C emergency kit in hostile conditions. Am J Infect Control 47(6):19
Squeri R et al (2016) “Clean care is safer care”: correct handwashing in the prevention of healthcare associated infections. Ann Ig 28(6):409–415
Sserwadda I et al (2018) Microbial contaminants isolated from items and work surfaces in the post- operative ward at Kawolo general hospital, Uganda. BMC Infect Dis 18(1):68
Staskel DM, Briley ME, Field LH et al (2007) Microbial evaluation of foodservice surfaces in Texas child-care centers. J Am Diet Assoc 107:854–859
Suetens C et al (2018) Prevalence of healthcare-associated infections, estimated incidence and composite antimicrobial resistance index in acute care hospitals and long-term care facilities: results from two European point prevalence surveys, 2016 to 2017. Euro Surveill 23(46):1800516
Suleyman G, Alangaden G, Bardossy AC (2018) The Role of environmental contamination in the transmission of nosocomial pathogens and healthcare-associated infections. Curr Infect Dis Rep 20(6):12
Sunkesula VCK et al (2017) A randomized trial to determine the impact of an educational patient hand-hygiene intervention on contamination of hospitalized patient’s hands with healthcare-associated pathogens. Infect Control Hosp Epidemiol 38(5):595–597
Szeto W et al (2020) The efficacy of vacuum-ultraviolet light disinfection of some common environmental pathogens. BMC Infect Dis 20(1):127
Tahir S et al (2019) Transmission of Staphylococcus aureus from dry surface biofilm (DSB) via different types of gloves. Infect Control Hosp Epidemiol 40:60–64
Tanner WD et al (2021) Environmental contamination of contact precaution and non-contact precaution patient rooms in six acute care facilities. Clin Infect Dis 72(Suppl 1):S8–S16
Tolera M et al (2018) Bacterial nosocomial infections and antimicrobial susceptibility pattern among patients admitted at Hiwot Fana specialized university hospital. Eastern Ethiopia Adv Med 2018:2127814
Toplitsch D et al (2021) Antimicrobial activity of a novel Cu(NO3)2-containing sol-gel surface under different testing conditions. Materials 14:6488
Torok ME, Moran E, Cooke F (2016) Oxford handbook of infectious diseases and microbiology. Oxford University Press, Oxford
Trofa D, Gacser A, Nosanchuk JD (2008) Candida parapsilosis, an emerging fungal pathogen. Clin Microbiol Rev 21(4):606–625
Uneputty A et al (2022) Strategies applied to modify structured and smooth surfaces: a step closer to reduce bacterial adhesion and biofilm formation. Colloid Interface Sci Commun 46:100560
Vernez D et al (2020) Reusability of filtering facepiece respirators after decontamination through drying and germicidal UV irradiation. BMJ Glob Health 5(10):003110
Viana Rel H, dos Santos SG, Oliveira AC (2016) Recovery of resistant bacteria from mattresses of patients under contact precautions. Am J Infect Control 44(4):465–469
Vincent JL, Marshall J, Silva E et al (2009) International study of the prevalence and outcomes of infection in intensive care units. JAMA Intern Med 302:2323–2329
Wagenvoort JH, Sluijsmans W, Penders RJ et al (2000) Better environmental survival of outbreak vs. sporadic MRSA isolates. J Hosp Infect 45(3):231–234
Wallace RL, Ouellette M, Jean J (2019) Effect of UV-C light or hydrogen peroxide wipes on the inactivation of methicillin-resistant Staphylococcus aureus, Clostridium difficile spores and norovirus surrogate. J Appl Microbiol 127(2):586–597
Wang HP et al (2017) Antimicrobial resistance of 3 types of gram-negative bacteria isolated from hospital surfaces and the hands of health care workers. Am J Infect Control 45(11):e143–e147
Weber DJ et al (2010) Role of hospital surfaces in the transmission of emerging health care-associated pathogens: norovirus, Clostridium difficile, and Acinetobacter species. Am J Infect Control 38(5 Suppl 1):S25-33
Weiner LM et al (2016) Antimicrobial-resistant pathogens associated with healthcare-associated infections: summary of data reported to the national healthcare safety network at the centers for disease control and prevention, 2011–2014. Infect Control Hosp Epidemiol 37(11):1288–1301
WHO (2019) Implementation manual to prevent and control the spread of carbapenem-resistant organisms at the national and health care facility level: interim practical manual supporting implementation of the guidelines for the prevention and control of carbapenem-resistant organisms, WHO, Geneva
Williams BJ, Dehnbostel J, Blackwell TS (2010) Pseudomonas aeruginosa: host defense in lung diseases. Respirology 15:1037–1056
Yang JH et al (2019) Effectiveness of an ultraviolet-C disinfection system for reduction of healthcare-associated pathogens. J Microbiol Immunol Infect 52(3):487–493
Yaun BR et al (2004) Inhibition of pathogens on fresh produce by ultraviolet energy. Int J Food Microbiol 90(1):1–8
Yue D et al (2017) Hospital-wide comparison of health care-associated infection among 8 intensive care units: a retrospective analysis for 2010–2015. Am J Infect Control 45(1):e7–e13
Zeber JE et al (2018) Effect of pulsed xenon ultraviolet room disinfection devices on microbial counts for methicillin-resistant Staphylococcus aureus and aerobic bacterial colonies. Am J Infect Control 46(6):668–673
Acknowledgements
We would like to thank the Universiti Teknologi Malaysia and the Ministry of Higher Education (MOHE) Malaysia (Fundamental Research Grant Scheme: (FRGS/1/2020/TK0/UTM/02/105,Vat No. 5F282) for financially supporting this work.
Funding
The research leading to these results received funding from the Ministry of Higher Education, Malaysia (MoHE) (Fundamental Research Grant Scheme: (FRGS/1/2020/TK0/UTM/02/105,Vat No. 5F282).
Author information
Authors and Affiliations
Contributions
All of the authors named in the paper have made substantial contributions to the creation and writing of this article. Mr. Jahanzeb Sheikh contributed to writing–original draft, investigation, resources, and formal analysis; Dr. Tan Tian Swee was involved in supervision and visualization; Dr. Syafiqah Saidin contributed to project administration and writing—review and editing; Dr. Chua Lee Suan was involved in validation, visualization, and co-supervision; Dr. Sameen Ahmed Malik contributed to visualization and resources; and Mr. Leong Kah Meng, Mr. Matthias Tiong Foh Thye, Ma Kun were involved in validation.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Additional information
Editorial responsibility: S. Rangabhashiyam.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sheikh, J., Swee, T.T., Saidin, S. et al. Classic and alternative disinfection practices for preventing of hospital-acquired infections: a systemic review. Int. J. Environ. Sci. Technol. 21, 8261–8296 (2024). https://doi.org/10.1007/s13762-024-05635-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13762-024-05635-3