Abstract
To formulate and validate a dyschromatopsia linear regression model in patients with multiple sclerosis (MS). 64 MS patients (50 to formulate the model and 14 for its validation) underwent neurological (Expanded Disability Status Scale, EDSS), color vision (Farnsworth D15 test), and peripapillary retinal nerve fiber layer (pRNFL) and retinal evaluation with spectral-domain optical coherence tomography (SD-OCT). Neuroradiological examination permitted to obtain brain parenchymal fraction (BPF) and cervical spinal cord volume (SC). Ophthalmic parameters were calculated as the average of both non-optic neuritis (ON) eyes, and in case the patient had previous ON, the value of the fellow non-ON eye was taken. The influence of sex, age, disease duration, and history of disease-modifying treatment (first- or second-line DMT) was tested as covariables that could influence color perception. Color confusion index (log CCI) correlated with pRNFL (r = − 0.322, p = 0.009), ganglion cell layer (GCL, r = − 0.321, p = 0.01), BPF (r = − 0.287, p = 0.021), SC volume (r = − 0.33, p = 0.008), patients’ age (r = 0.417, p = 0.001), disease duration (r = 0.371, p = 0.003), and EDSS (r = 0.44, p = 0.001). The following CCI equation was obtained: log (CCI) = 0.316–0.224 BPF − 0.187 SC volume (mm3) + 0.226 age (years) + 0.012 disease duration (years) − 0.372 GCL (µm). CCI correlates with MS clinical and paraclinical established biomarkers suggesting chronic diffuse neurodegeneration in MS operates at brain, SC, and retina linking all three compartments. Color vision outcome can be calculated through the aforementioned variables for clinical and research purposes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Multiple sclerosis (MS) patients usually suffer from vision problems, mainly caused by acute optic neuritis (ON) [1]. Although optic neuritis treatment trial (ONTT) demonstrated that 85% of participants recovered a visual acuity (VA) better than 20/25 after 15 years of follow-up [2], many patients complain about an incomplete visual recovery and its impact on their daily activities [3, 4].
Beyond acute focal damage, concomitant chronic neurodegeneration drives diffuse central nervous system (CNS) damage and axonal loss what is considered the main cause of permanent disability. Both anterograde and retrograde degeneration may happen along the visual pathway [5]. Current data [6, 7] reveal that primary chronic inflammatory retinopathy may exist in the visual pathway of the non-ON eyes, what reflects global CNS damage. Thus, visual pathway has emerged as a source of imaging biomarkers with useful clinical and research implications [8, 9].
Unlike other dimensions of visual function more widespread in clinical and research practice [10], color vision in MS patients has been less handled and the mechanisms involved in their dysfunction are poorly understood [11, 12].
Color information starts at cone cells according to the different sensitivity to light wavelengths and through parvocellular and koniocellular retino-cortical pathway; it reaches occipital cortex and associative visual cortex areas [13]. Vulnerability to demyelination and axonal injury of the parvocellular system (ganglionic cells and their synapses at lateral geniculate nucleus) compared to the magnocellular system has been demonstrated in multiple sclerosis [14, 15], what justifies dyschromatopsia as one of the main ocular symptoms of the disease. Although color vision physiopathology remains unknown, its origin points to ganglion cell damage [16].
Our hypothesis is that dyschromatopsia in MS correlates with optical coherence tomography (OCT) and magnetic resonance imaging (MRI) measures, what could allow to predict this visual outcome through a validated multivariate linear regression model.
Materials and methods
Study design
This is an observational cross-sectional study carried out by the Neurology and Ophthalmology Departments of the University and Polytechnic Hospital La Fe (Valencia, Spain) from October 2017 to May 2019 after the approval of the research ethics committee of our institution. The research followed the tenets of the Declaration of Helsinki.
Study population and clinical assessment
MS patients who accepted participation were evaluated by clinical interview, as well as through a neurological and ophthalmological examination to fulfill inclusion criteria (age over 18 years and MS diagnosed following the 2010 revised McDonald criteria [17]) and discard exclusion criteria (Table 1, modified from [18]). Out of the 141 volunteers who signed written informed consent, 64 were finally included.
As other papers [19, 20], we opted not to classify patients using the three classic designations (relapsing–remitting, secondary progressive, and primary progressive MS) based on the hypothesis that the different phenotypes are the consequence of the same mechanisms (autoimmune inflammation, axonal loss, demyelination, and remyelination) at different times and intensity in the disease course.
Data for the study were collected in a prospective fashion from the medical, OCT, and MRI records with less than 3 month interval between examinations. For each patient, age (years) at the moment of examination, sex, MS disease duration (years), history of MS disease-modifying treatments (DMT), and disability assessed using the EDSS [21] were determined.
EDSS and color vision assessment, neuroradiological volumes analysis, and OCT performance were made by different researchers. All of them were blind to each other. Statistical analysis was carried out in a blind fashion for the assessment of predictors for the outcome, having masked the predictors.
The pharmacological history of the patients permitted to classify patients according to their DMT as first line (interferon (INF) ß-1a (Rebif® 22/44, Avonex®), INF ß-1b (Betaferon®), peg-INF ß-1a (Plegridy®), teriflunomide, glatiramer acetate, azathioprine, and dimethyl fumarate) or second-line treatment (fingolimod, natalizumab, alemtuzumab, rituximab, bone marrow transplant, cyclophosphamide, and ocrelizumab). Disease duration was defined from the time of the first manifestation of disease until study enrollment.
History of previous ON was determined according to the symptoms defined in the ONTT: pain with eye movement, loss of visual acuity, visual field defect, color vision impairment, and relative afferent pupillary defect [2]. All cases were carefully confirmed by optic nerve MRI, OCT, and/or visual evoked potentials.
Color vision assessment
Color vision was tested monocular using Farnsworth’s panel D-15 (X-Rite, MI, USA) using an illuminant C equivalent light source at an illumination level of 270 lux. In this color test, the patient is asked to organize the tablets sequentially, this organization is represented in a diagram, and the errors are analyzed. The qualitative assessment of the test is based on the disposition of the mistakes made according to the axes represented in the diagram (“protan”, “deutan”, and “tritan”; red, green, and blue respectively), differentiating between the complete absence of pigment (using the suffix “-opia”) or its deficiency (using the suffix “-anomaly”). Quantitative assessment is based on the calculation of the total color difference score (TCDS) and the Color Confusion Index (CCI) defined by Bowman KJ [22]; as well as the total error score (TES), the Selectivity Index (SI), and the Confusion Index (CI) defined by Vingrys and King-Smith [23], as implemented by Török (https://torok.info/colorvision/d15.htm2013).
Although all the indexes described above were collected for descriptive statistics, inferential analysis was carried out with the CCI. The CCI is calculated by dividing the calculated distance in color space for a specific cap replacement by that distance calculated for perfect replacement. A CCI equal to 1 would be normal, while a CCI greater than 1 would be representative of alteration. It was performed monocular after refraction and near correction if necessary.
Optical coherence tomography
Spectral Domain OCT (HRA-OCT Spectralis, Heidelberg Engineering, Germany; Heidelberg Eye Explorer software version 6.3.1.0) was performed for each eye. All subjects underwent a peripapillary retinal nerve fiber layer (pRNFL) protocol scan (3.5 mm-diameter circle scan centered on the optic nerve head with an Automatic Real-time Tracking (ART) of 100 frames and 1536 A-scans per B-scans) with the N-Site Axonal Analytic software version 6.7.
Besides a macular raster scan (25 horizontal B-scans analyzing a macular area of 7.5 mm × 7.5 mm with a mean ART of 9 and 512 A-scans per B-scans) was taken to measure ganglion cell layer (GCL), inner plexiform layer (IPL), inner nuclear layer (INL), and outer nuclear layer (ONL) thickness in macular area using the 1, 3, and 6 mm ETDRS grid centered on the fovea. Conversion of macular volumes (original measurement in mm3) to thicknesses (in µm) was conducted using the following equation: thickness (µm) = [4 × volume (µm3)]/[π × (6000 µm)2]. To be included in the study, all OCT needs to fulfill OSCAR-IB [24, 25] and APOSTEL criteria [26].
Magnetic resonance imaging
Brain and spinal cord (SC) MRIs were performed on a 3 T Philips Archieva scanner (Philips Medical Systems, Best, The Netherlands) with a standard head coil. Brain MRI consisted of an axial 3D T1 sequence (echo time (TE) 3 ms; repetition time (TR) 8 ms; slice thickness 1 m); and a sagittal 3D FLAIR T2 (TE: 2.6 ms; TR 6000 ms; slice thickness 1.1 mm). SC MRI consisted of an axial 3D T1 post-gadolinium sequence (TE 2.6 ms; TR 7.5 ms; slice thickness 1 mm). Percent Phase Field of View was 100 in all cases.
Brain parenchyma fraction (BPF) was quantified by means of the Freesurfer software image analysis version 5.3 (https://surfer.nmr.mgh.harvard.edu/), while SC volume (mm3, measured taken C1/4 disc as landmarks) was assessed manually for its quantification. All images were assessed accurately controlled for errors/artifacts.
Statistical analysis
Statistical analyses were performed using SPSS Statistics version 24.0 (SPSS Inc, Armonk, NY:IBM, USA) software.
First, we performed descriptive statistics to characterize our sample. For the design of the multivariate linear regression model, it is necessary to set boundary reference values in the equation to obtain logical results with real clinical outcomes. These maximum and minimum values have been considered in the variables of the model applying the following formula for typing: variable = [real value − minimum]/[maximum − minimum]. With these formula coefficients of the equation are modified, since all the variables oscillate between 0 and 1 (with the exception of the qualitative ones) and, therefore, changes in the quantitative variables are graded in tenths.
To formulate the model, besides retinal and CNS biomarkers, MS-related clinical variables were assessed for their relation with the dependent variable log (CCI) using Spearman’s correlation coefficient and ANOVA test. All p values were two-tailed and they were considered significant at p ≤ 0.05. Given the collinearity between GCL, pRNFL, and EDSS, we decided to include GCL in the mathematical model because of its better reproducibility and less involvement by artifacts than pRNFL [27, 28] and its close relation with color vision impairment [16]. Natural logarithms of the CCI were taken as previously reported [29].
Global significance of the model was validated through Omnibus test and mathematical procedure through the goodness of fit (deviance and Aikake Information Criteria).
Taking into account previous publications [18] and ON effect in visual and OCT outcomes, eyes with history of ON were excluded from the statistical analysis. For patients without ON, ophthalmological values (CCI, pRNFL, and GCL) were determined as the mean value of both eyes. For patients with prior ON, only the value of the unaffected eye was included for the statistics.
Results
Flow of participants through the study is represented in Fig. 1. The final cohort is characterized demographically, neurologically, and ophthalmologically in Table 2, while qualitative color vision assessments are summarized in Table 3.
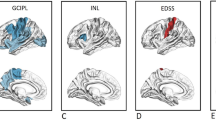
Higher CCI values (log CCI) correlate with thinner pRNFL (r = − 0.322, p = 0.009), thinner GCL (r = − 0.321, p = 0.01), lower BPF (r = − 0.287, p = 0.021), lower SC volume (r = − 0.33, p = 0.008), older age (r = 0.417, p = 0.001), longer disease duration (r = 0.371, p = 0.003), and higher EDSS (r = 0.44, p = 0.001). CCI values (log CCI) did not correlate with IPL (p = 0.06), INL (p = 0.722), ONL (p = 0.145), sex (p = 0.701) nor DMT (p = 0.116).
Table 4 shows the estimation (standardized ß-coefficients) and standard error of the variables that have finally been included, the hypothesis contrast and the 95% confidence interval of each parameter.
Omnibus test (see supplementary material, table S1) reveals a significant global result of the predictive model (p-value < 0.001). On the other hand, goodness of fit (see supplementary material, table S2) shows underdispersion (value/df < 1), so we can conclude the model fits the data properly.
The model is accepted and the following equation that gives the CCI is obtained: log (CCI) = 0.316 –0.224 BPF − 0.187 SC volume (mm3) + 0.226 age (years) + 0.012 disease duration (years) − 0.372 GCL (µm). The model was validated (Fig. 2) with the 14 patients randomly selected as “validation group” obtaining an R2 = 0.392 (r = 0.626).
Conclusions
To the best of our knowledge, this is the first mathematical model to predict CCI from clinical and paraclinical biomarkers already accepted in MS clinical and research practice. The main finding of this study is that color vision impairment in non-ON eyes is associated with disability and surrogate brain, SC, and retinal markers of axonal damage. The most common pathological color vision pattern is diffuse color error discrimination, what supports the idea of no specific pattern of color deficiency in MS [16, 30,31,32].
Despite the impact of the disease on the visual system, clinical scales such as EDSS weight visual impairment minimally, while others such as the multiple sclerosis functional composite (MSFC) do not assess it. Specifically, color vision is a visual dimension sparsely explored with controversial conclusions related to its clinical and research utility. While its usefulness as a diagnostic and monitoring tool has been questioned [33], or has not demonstrated significance [34, 35], there are several articles that support its inclusion in clinical practice and research.
In line with our results, Martínez-Lapiscina et al. [31] showed dyschromatopsia in non-ON eyes relates to older age, longer disease duration, increased clinical disability, and higher central nervous system and retinal damage. 1-year follow-up revealed those who developed color vision impairment in the absence of ON, had a greater disability and gray matter atrophy, relating dyschromatopsia with diffuse axonal damage independent of inflammatory activity.
Unpublished before, we found dyschromatopsia correlates with SC volume and GCL slightly better than BPF. However, in the multivariate model, when SC volume, retinal, and brain atrophy are included simultaneously with other significant covariates (age, disease duration), GCL has the highest regression coefficient, what reflects the importance of the GCL viability in this parameter determination.
Unlike Oh et al. [36], who evaluated high- and low-contrast VA, our results about chromatic vision are mainly dependent on GCL thickness, but also depend, among others, on cervical SC volume, being visual and spinal systems two functionally and spatially unrelated CNS compartments. These findings suggest chronic primary retinal damage not only parallels chronic brain damage, but also SC damage what supports ongoing primary neurodegeneration beyond anatomical landmarks.
Despite being a good biomarker of the clinical course, unless there are spinal findings on the neurological examination, routine SC MRI is not performed [37]. Partly because SC MRI is more complicated to be performed than at brain level, since some factors make the SC a difficult region to assess, such as low resolution or artifacts conditioned by physiological movements like heart rate or breathing [38]. However, the correlation between spinal atrophy and disability is greater than any other MRI measurement [39]. Atrophy rate at SC is higher than in brain (1.78% versus 0.5% annual rate), having SC a greater limitation to neuroplasticity compared to brain involvement, with a relevant importance of the cervical segment, since it represents a key point for trans-synaptic axonal degeneration, and cervical periphery represents the most frequent location for SC lesions [40].
For these reasons, and despite the fact that SC (nor brain) volume measures have no role in the MS diagnostic criteria, there is growing evidence proving that it would help for early evaluation and disease progression [41]. Beyond the fact that an adequate management of the MRI scanner-related factors or an appropriate development of volumetric software tools would permit a better daily clinical decisions, MRI measures would improve our understanding of neurodegenerative mechanisms that are partly independent of inflammatory mechanisms [42]. Current knowledge about these mechanisms is limited being necessary the research of surrogate markers that translates ongoing neurodegeneration in MS independently of anatomical boundaries.
Consequently, and according to our findings, color tests are a potential tool that provides helpful and complementary information, as it correlates with EDSS and CNS parameters, but also with retinal measures (pRNFL and GCL). In this line of argument, Villoslada et al. [32] and Satue et al. [43] showed color vision strongly correlated with OCT measures, while Levin et al. [44] showed retinal thickness in fellow non-ON eyes correlate with color contrast sensitivity. For their part, Gundogan et al. [45] demonstrated Farnsworth–Munsell 100-Hue was more sensitive than pattern visual-evoked potential in the diagnosis of subclinical pathway involvement.
Our work has some methodological limitations that should be noted. First, the heterogeneous study population, who had been treated with various immunomodulating therapies during different time intervals, underestimates retinal, brain, and SC atrophy in different rates. Second, this study is based on the dynamic CNS damage etiopathogenic hypothesis, but does not reject alternatives such as the two-stage hypothesis or the inside-out hypothesis. Third, our results cannot be applied to patients with bilateral ON or a possible EDSS score greater than 6.5. Fourth, the study did not include a healthy age-sex matched control group for comparison. Fifth, despite the strict exclusion criteria and the ophthalmological tests performed, we cannot discard the possibility of subclinical ON that justifies the chromatic alteration, although the existence of a primary retinal degeneration is widely accepted [6, 7]. Sixth, the cross-sectional design and the limited number of patients make us cautious with the obtained results, although, in recent literature, we can find these same limitations [33, 44, 45]. Despite this, we have been able to obtain significant correlations to support our conclusions.
Color vision can be assessed in multiple ways but mainly in daily clinical practice, we can distinguish between pseudoisochromatic plates (Ishihara and Hardy-Rand-Rittler plates) and cap-based test (Farnsworth–Munsell 100-Hue, Farnsworth’panel D-15, and Lanthony’s desaturated 15-hue). While pseudoisochromatic plate test are easier, faster, and independent of the upper-limb function, what makes them useful as a screening test, cap-based tests like Farnsworth D-15 permit a more detailed assessment of color vision impairment [46], less time-consuming than FM 100-hue but less suitable for detecting mild color abnormalities than Lanthony desaturated test. Specifically, Farnsworth D-15 is a non-invasive, inexpensive test to assess chromatic vision that technically presents a short learning curve for its administration and posterior analysis.
Among the strengths of our study, we could highlight the strict clinical exclusion criteria and the mathematical designed developed that includes potential confounding variables, besides retinal and CNS biomarkers less explored such as cervical SC volume or macular nuclear layers.
In conclusion, we found that dyschromatopsia in MS (CCI) correlates with retinal parameters (GCL, pRNFL), physical disability (EDSS), and MRI measures (SC volume, BPF) independent of radiological activity and clinical relapses. Based on our results, we encourage standardizing color vision outcomes to monitor disease activity in clinical consultation and as an end-point in research trials. Our findings extend the idea of the eye as a window to the brain but to the entire CNS, mirroring diffuse chronic ongoing neurodegeneration. Longitudinal studies with homogeneous larger samples of patients are necessary in future research.
Data availability
Data available on request due to privacy/ethical restrictions.
References
Costello F (2016) Vision disturbances in multiple sclerosis. Semin Neurol 36:185–195. https://doi.org/10.1055/s-0036-1579692
Optic Neuritis Study Group (2008) Visual function 15 years after optic neuritis: a final follow-up report from the optic neuritis treatment trial. Ophthalmology 115:1079–1082. https://doi.org/10.1016/j.ophtha.2007.08.004
Heesen C, Böhm J, Reich C, Kasper J, Goebel M, Gold SM (2008) Patient perception of bodily functions in multiple sclerosis: gait and visual function are the most valuable. Mult Scler 14:988–991. https://doi.org/10.1177/1352458508088916
Sanchez-Dalmau B, Martinez-Lapiscina EH, Pulido-Valdeolivas I et al (2018) Predictors of vision impairment in multiple sclerosis. PLoS ONE 13:e0195856. https://doi.org/10.1371/journal.pone.0195856
Graham SL, Klistorner A (2016) Afferent visual pathways in multiple sclerosis: a review. Clin Exp Ophthalmol 45:62–72. https://doi.org/10.1111/ceo.12751
Saidha S, Syc SB, Ibrahim MA et al (2011) Primary retinal pathology in multiple sclerosis as detected by optical coherence tomography. Brain 134:518–533. https://doi.org/10.1093/brain/awq346
Ortiz-Pérez S, Martínez-Lapiscina EH, Gabilondo I et al (2013) Retinal periphlebitis is associated with multiple sclerosis severity. Neurology 81:877–881. https://doi.org/10.1212/WNL.0b013e3182a3525e
Lambe J, Saidha S, Bermel RA (2019) Optical coherence tomography and multiple sclerosis: Update on clinical application and role in clinical trials. Mult Scler. https://doi.org/10.1177/1352458519872751
Brandt AU, Martinez-Lapiscina EH, Nolan R, Saidha S (2017) Monitoring the course of multiple sclerosis with optical coherence tomography. Curr Treat Options Neurol 19:15. https://doi.org/10.1007/s11940-017-0452-7
Balcer LJ, Raynowska J, Nolan R et al (2017) Validity of low-contrast letter acuity as a visual performance outcome measure for multiple sclerosis. Mult Scler 23:734–747. https://doi.org/10.1177/1352458517690822
Katz B (1995) The dyschromatopsia of optic neuritis: a descriptive analysis of data from the optic neuritis treatment trial. Trans Am Ophthalmol Soc 93:658–708
Silverman S, Hart W Jr, Gordon M, Kilo C (1990) The dyschromatopsia of optic neuritis is determined in part by the foveal/perifoveal distribution of visual field damage. Invest Ophthalmol Vis Sci 31:1895–1902
Solomon SG, Lennie P (2007) The machinery of colour vision. Nat Rev Neurosci 8:276–286. https://doi.org/10.1038/nrn2094
Porciatti V, Sartucci F (1996) Retinal and cortical evoked responses to chromatic contrast stimuli. specific losses in both eyes of patients with multiple sclerosis and unilateral optic neuritis. Brain 119:723–740. https://doi.org/10.1093/brain/119.3.723
Evangelou N, Konz D, Esiri MM, Smith S, Palace J, Matthews PM (2001) Size-selective neuronal changes in the anterior optic pathways suggest a differential susceptibility to injury in multiple sclerosis. Brain 124:1813–1820. https://doi.org/10.1093/brain/124.9.1813
Lampert EJ, Andorra M, Torres-Torres R et al (2015) Color vision impairment in multiple sclerosis points to retinal ganglion cell damage. J Neurol 262:2491–2497. https://doi.org/10.1007/s00415-015-7876-3
Polman CH, Reingold SC, Banwell B et al (2011) Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol 69:292–302. https://doi.org/10.1002/ana.22366
Martínez-Lapiscina EH, Fraga-Pumar E, Gabilondo I et al (2014) The multiple sclerosis visual pathway cohort: understanding neurodegeneration in MS. BMC Res Notes 7:910. https://doi.org/10.1186/1756-0500-7-910
Gabilondo I, Martínez-Lapiscina EH, Martínez-Heras E et al (2014) Trans-synaptic axonal degeneration in the visual pathway in multiple sclerosis. Ann Neurol 75:98–107. https://doi.org/10.1002/ana.24030
Kotelnikova E, Kiani NA, Abad E et al (2017) Dynamics and heterogeneity of brain damage in multiple sclerosis. PLoS Comput Biol 13:e1005757. https://doi.org/10.1371/journal.pcbi.1005757
Kurtzke JF (1983) Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology 33:1944–1952. https://doi.org/10.1212/wnl.33.11.1444
Bowman KJ (1982) A method for quantitative scoring of the Farnsworth panel D-15. Acta Ophthalmol 60:907–916. https://doi.org/10.1111/j.1755-3768.1982.tb00621.x
Vingrys AJ, King-Smith PE (1988) A quantitative scoring technique for panel tests of color vision. Invest Ophthalmol Vis Sci 29:50–63
Tewarie P, Balk L, Costello F et al (2012) The OSCAR-IB consensus criteria for retinal OCT quality assessment. PLoS ONE 7:e34823. https://doi.org/10.1371/journal.pone.0034823
Schippling S, Balk LJ, Costello F et al (2015) Quality control for retinal OCT in multiple sclerosis: validation of the OSCAR-IB criteria. Mult Scler 21:163–170. https://doi.org/10.1177/1352458514538110
Cruz-Herranz A, Balk J, Oberwahrenbrock T et al (2016) The APOSTEL recommendations for reporting quantitative optical coherence tomography studies. Neurology 88:2303–2309. https://doi.org/10.1212/WNL.0000000000002774
Saidha S, Syc SB, Durbin MK et al (2011) Visual dysfunction in multiple sclerosis correlates better with optical coherence tomography derived estimates of macular ganglion cell layer thickness than peripapillary retinal nerve fiber layer thickness. Mult Scler 17:1449–1463. https://doi.org/10.1177/1352458511418630
Behbehani R, Al-Moosa A, Sriraman D, Alroughani R (2016) Ganglion cell analysis in acute optic neuritis. Mult Scler Relat Disord 5:66–69. https://doi.org/10.1016/j.msard.2015.10.008
Semple S, Dick F, Osborne A et al (2000) Impairment of colour vision in workers exposed to organic solvents. Occup Environ Med 57:582–587. https://doi.org/10.1136/oem.57.9.582
Moura A, Teixeira R, Oiwa N et al (2008) Chromatic discrimination losses in multiple sclerosis patients with and without optic neuritis using the Cambridge Colour Test. Vis Neurosci 25:463–468. https://doi.org/10.1017/S0952523808080437
Martínez-Lapiscina EH, Ortiz-Pérez S, Fraga-Pumar E et al (2014) Colour vision impairment is associated with disease severity in multiple sclerosis. Mult Scler 20:1207–1216. https://doi.org/10.1177/1352458513517591
Villoslada P, Cuneo A, Gelfand J, Hauser SL, Green A (2012) Color vision is strongly associated with retinal thinning in multiple sclerosis. Mult Scler 18:991–999. https://doi.org/10.1177/1352458511431972
Yuksel B, Dogan B, Koctekin B et al (2019) Color vision testing versus pattern visual evoked potentials and optical coherence tomography parameters in subclinical optic nerve involvement in multiple sclerosis. J Clin Neurosci 61:48–53. https://doi.org/10.1016/j.jocn.2018.11.011
Garcia-Martin E, Ara JR, Martin J et al (2017) Retinal and optic nerve degeneration in patients with multiple sclerosis followed up for 5 years. Ophthalmology 124:688–696. https://doi.org/10.1016/j.ophtha.2017.01.005
Herrero R, Garcia-Martin E, Almarcegui C et al (2012) Progressive degeneration of the retinal nerve fiber layer in patients with multiple sclerosis. Invest Ophthalmol Vis Sci 53:8344–8349. https://doi.org/10.1167/iovs.12-10362
Oh J, Sotirchos ES, Saidha S et al (2015) Relationships between quantitative spinal cord MRI and retinal layers in multiple sclerosis. Neurology 84:720–728. https://doi.org/10.1212/WNL.0000000000001257
Ontaneda D, Thompson AJ, Fox RJ et al (2017) Progressive multiple sclerosis: prospects for disease therapy, repair, and restoration of function. Lancet 389:1357–1366. https://doi.org/10.1016/S0140-6736(16)31320-4
Ontaneda D, Fox RJ (2017) Imaging as an outcome measure in multiple sclerosis. Neurotherapeutics 14:24–34. https://doi.org/10.1007/s13311-016-0479-6
Kearney H, Miller DH, Ciccarelli O (2015) Spinal cord MRI in multiple sclerosis—diagnostic, prognostic and clinical value. Nat Rev Neurol 11:327–338. https://doi.org/10.1038/nrneurol.2015.80
Moccia M, Ruggieri S, Ianniello A et al (2019) Advances in spinal cord imaging in multiple sclerosis. Ther Adv Neurol Disord 12:1756286419840593. https://doi.org/10.1177/1756286419840593
Tsagkas C, Magon S, Gaetano L et al (2018) Spinal cord volume loss: a marker of disease progression in multiple sclerosis. Neurology 91:e349–e358. https://doi.org/10.1212/WNL.0000000000005853
Kawachi I, Lassmann H (2017) Neurodegeneration in multiple sclerosis and neuromyelitis optica. J Neurol Neurosurg Psychiatry 88:137–145. https://doi.org/10.1136/jnnp-2016-313300
Satue M, Rodrigo MJ, Otin S et al (2016) Relationship between visual dysfunction and retinal changes in patients with multiple sclerosis. PLoS ONE 11:e0157293. https://doi.org/10.1371/journal.pone.0157293
Levin N, Devereux M, Bick A, Baker N, Green A (2019) Color perception impairment following optic neuritis and its association with retinal atrophy. J Neurol 266:1160–1166. https://doi.org/10.1007/s00415-019-09246-8
Gundogan FC, Tas A, Altun S, Oz O, Erdem U, Sobaci G (2013) Color vision versus pattern visual evoked potentials in the assessment of subclinical optic pathway involvement in multiple sclerosis. Indian J Ophthalmol 61:100–103. https://doi.org/10.4103/0301-4738.99842
Cole BL, Lian KY, Lakkis C (2006) The new Richmond HRR pseudoisochromatic test for colour vision is better than the ishihara test. Clin Exp Ophthalmol 89:73–80. https://doi.org/10.1111/j.1444-0938.2006.00015.x
Funding
Bonaventura Casanova was supported by a fellowship from Health Institute Carlos III, Spain (FIS 17/551). The funding agency had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; and preparation, review or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
Conceptualization: AB-G, EE-G, BC. Methodology: AB-G, MTS, SC-B, FP-M, CA, EE-G, BC. Formal analysis and investigation: AB-G, MTS, SC-B, FP-M, CA, EE-G, BC. Writing—original draft preparation: AB-G. Writing—review and editing: AB-G, EE-G, BC. Funding acquisition: BC. Resources: AB-G, EE-G, BC. Supervision: EE-G, BC.
Corresponding author
Ethics declarations
Conflict of interest
Francisco Pérez-Miralles has received compensation from Almirall, Biogen Idec, Genzyme, Merk-Serono, Mylan, Novartis, Roche, Sanofi-Aventis, and Teva, outside the submitted work. Bonaventura Casanova has received compensation from Novartis, Roche, Biogen, Merk, Teva, and Sanofi outside the submitted work. All other authors have no conflicts of interest to declare.
Consent to participate
Written informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Barreiro-González, A., Sanz, M.T., Carratalà-Boscà, S. et al. Dyschromatopsia in multiple sclerosis reflects diffuse chronic neurodegeneration beyond anatomical landmarks. Acta Neurol Belg 121, 1767–1775 (2021). https://doi.org/10.1007/s13760-020-01516-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-020-01516-x