Abstract
We aimed to explore whether a migraine with aura (MA) is associated with structural changes in tracts of a white matter and to compare parameters of diffusivity between subgroups in migraineurs. Forty-three MA and 20 healthy subjects (HS), balanced by sex and age, were selected for this study. Analysis of diffusion tensor parameters was used to identify differences between MA patients and HS, and then between MA subgroups. A diffusion tensor probabilistic tractography analysis showed that there is no difference between MA patients and HS. However, using more-liberal uncorrected statistical threshold, we noted a trend in MA patients toward lower diffusivity indices of selected white matter tracts located in the forceps minor and right anterior thalamic radiation (ATR), superior longitudinal fasciculus (temporal part) (SLFT), cingulum-cingulate tract, and left uncinate fasciculus. Migraineurs who experienced somatosensory and dysphasic aura, besides visual symptoms, had tendency toward lower diffusivity indices, relative to migraineurs who experienced only visual symptoms, in the right inferior longitudinal fasciculus, forceps minor, and right superior longitudinal fasciculus (parietal part), SLFT, and cingulum-angular bundle. Aura frequency were negatively correlated with axial diffusivity and mean diffusivity of the right ATR (partial correlation = − 0.474; p = 0.002; partial correlation = − 0.460; p = 0.002), respectively. There were no significant differences between MA patients and HS, neither between MA subgroups. Migraineurs with abundant symptoms during the aura possibly have more myelinated fibers relative to those who experience only visual symptoms. Lower diffusivity indices of the right ATR are linked to more frequent migraine with aura attacks.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Migraine with aura is a specific neurovascular disorder which phenotypes differ among patients. The most common are visual phenomena, followed by somatosensory and dysphasic aura [1]. Currently it is unknown what initiates the aura [2], but it is considered that cortical spreading depression is an underlying mechanism [3]. Classical standing is that the wave of cortical excitation is spreading from the occipital cortex to adjacent cortical regions causing first visual, followed by somatosensory, and eventually dysphasic phenomena. However, recording of sequence and duration of the aura phenomena suggest that besides the cortical spreading, excitation could possibly spread faster or skip some parts of cortex through white matter tracts [4].
Although migraine with aura is considered as transitory brain phenomenon [5], there are increased amounts of evidence that migraineurs have cortical and subcortical changes of the brain matter [6, 7]. It is possible that these alterations are due to disease-related processes in genetically predisposed persons [8].
Several migraine studies have investigated brain white matter alterations using diffusion tensor imaging (DTI) with opposed results [6, 9,10,11]. Only a few of them were focused on migraine with aura [10, 11]; however, these studies poorly specified types of the aura among patients and did not investigate the difference in those subgroups. Also, investigators mainly analyzed regional differences in diffusivity parameters of migraine patients relative to controls, neglecting tract-specific differences that are still incompletely understood and characterized [10].
The main purpose of this study is to investigate whether a migraine with aura, organized into subgroups according to different aura phenotypes, is associated with structural changes in tracts of the white matter in the brain.
Methods
Participants
Patients were eligible for inclusion if they were aged between 18 and 60 years, and had a verified diagnosis of migraine with aura in accordance with the International Headache Society criteria (ICHD, 3rd ed.) [1].
Exclusion criteria were as follows: a history of any other primary headache (except infrequent episodic tension-type headache for ≤ 1 days per month), cardiovascular, cerebrovascular or psychiatric diseases, T2 lesions on their previous MRI scans, chronic migraine, or patients who had a history of taking any prophylactic medications (e.g., topiramate and propranolol). Healthy subjects (HS) were voluntarily recruited from clinical staff of Clinical Center and balanced with migraineurs in terms of sex, age, educational level, and hand predominance. HS were examined by a general practitioner due to excluding metabolic, neuropsychiatric and neurologic diseases. HS, as well as patients, did not take any kinds of medications, nor their general health status was impaired.
Furthermore, participants were referred to a special hospital for prevention and treatment of cerebrovascular diseases, to undergo MRI scans. All patients were a migraine free at least 1 week before and after the MRI scan. Also, all participants gave written consent after receiving detailed oral and written information and the study was done in accordance with the Helsinki II Declaration of 1964, with later revisions.
Subsequently, patients were subdivided into migraineurs who had visual, somatosensory and dysphasic symptoms (MVA+) and those who had only visual symptoms (MVA) during the aura, for additional and more profound analysis of a migraine with aura influence on selected fiber tracts.
Imaging protocol
MR examinations of patients and healthy subjects were performed using 1.5 T MR device with an eight-channel head coil (Signa, General Electric Healthcare, Milwaukee, WI, USA). The protocol consisted of (1) axial T2 weighted spin echo imaging (T2W) [echo time (TE) = 105.8 ms, repetition time (TR) = 5700 ms, flip angle (FA) = 90°, 24 slices with 0.47 × 1 × 5mm2 voxels, slice thickness = 5 mm, acquisition matrix 512 × 512], (2) three-dimensional T1-weighted fast spoiled gradient-echo (T1-3D-FSPGR) series (TE = 3.60 ms, TR = 8.12 ms, FA = 15°, 248 continuous slices with 0.47 × 0.47 × 1.4 mm3 voxels, slice thickness = 1.4 mm, acquisition matrix 512 × 512), and (3) 60 mutually non-parallel directions (b = 1000s/mm2) axial DTI (TR = 8000 ms; TE = 106 ms; 24 axial cross-sectional slices, slice thickness = 5 mm; number of acquisitions = 1; dimension matrix for each cross section was 256 × 256, with in-plane pixel size 0.94 × 0.94 mm). All T2W images were reviewed by a board-certified neuroradiologist and data were excluded from analyses if there were abnormalities.
Freesurfer (version 5.3.0) analysis was performed on HP 350 server (Intel Xeon 1800 MHz, 8 cores, 16 Gb RAM). DT images were post-processed via automatic TRACULA (TRActs Constrained by UnderLying Anatomy) algorithm [12], which is an integral part of the FREESURFER package [13]. The above algorithm consists of three segments: pre-process images for reducing distortions, probabilistic tractography using cortical segmentation and parceling [14], and computation of anisotropy/diffusivity parameters. TRACULA algorithms yielded DTI parameters [fractional anisotropy (FA), mean diffusivity (MD), radial diffusivity (RD), and axial diffusivity (AD)] for ten specific fiber tracts [SLFT—superior longitudinal fasciculus (temporal part), SLFP—superior longitudinal fasciculus (parietal part), ILF—inferior longitudinal fasciculus, CST—corticospinal tract, CCT—cingulum-cingulate tract, CAB—cingulum-angular bundle, ATR—anterior thalamic radiation, uncus, forceps major, and forceps minor] in all participants.
TBSS voxel-wise analysis
Individual FA images were non-linearly registered to the FMRIB58_FA atlas provided within FSL and averaged to obtain a customized atlas. The resulting mean FA image was thinned to create a WM tract “skeleton”, which threshold was set at FA > 0.2 to include only white matter voxels. Individual-participant normalized RD maps were warped onto the FA skeleton before statistical comparisons, by searching perpendicularly from the skeleton for maximum RD values [15].
Statistics
Subject demographics and migraine with aura characteristics were reported using descriptive statistics and compared amongst subject groups and subgroups using independent sample t test (two-tailed), Mann–Whitney U or chi-squared test, as appropriate.
Fiber tracts metrics, as extracted by TRACULA, were imported to R package for statistical analysis. Group data were compared using a general linear model, controlling for the effect of age and sex to avoid spurious results. Partial correlation analysis (controlling for the effect of age and sex) was conducted for significant tracts (MA vs. HS) to investigate the relationship between DTI indices of fiber tract integrity and a number of years with a migraine with aura or annual frequency of a migraine with aura attacks. Data were tested with Bonferroni correction for multiple comparisons, that is, a significance level of p < 0.0007 (p < 0.05/72) was accepted. Data were also presented if they survived a lesser conservative threshold set at 0.05.
TBSS voxel-wise analysis included comparisons of fiber tracts between MVA+ and MVA subgroups, controlling for the effect of age and sex. To visually demonstrate the subtle widespread changes, significant thresholds were set at p < 0.05, uncorrected.
Results
Total of 43 MA and 20 HC were investigated. MA did not differ significantly from HC relative to age (38.8 ± 11.2 vs. 41.6 ± 12.5, p = 0.415), sex (72.1 vs. 80% females, p = 0.502), and hand predominance (93.0 vs. 90.0% right-handed, p = 0.679). MA patients have lived 17.9 ± 10.6 years with a migraine with aura and had 6.1 ± 5.4 annual frequency of attacks. The average duration of the aura was 38.0 ± 24.8 min.
Twenty-two migraineurs (51.2%) experienced, besides visual aura, additional somatosensory and dysphasic symptoms during the aura forming MVA+ subgroup. The MVA+ subgroup did not differ significantly from the MVA subgroup relative to age (38.7 ± 13.3 vs. 39.0 ± 9.0, p = 0.927), sex (81.8 vs. 61.9% females, p = 0.146), hand predominance (90.9 vs. 95.2% right-handed, p = 0.578), duration of disease (18.8 ± 11.2 vs. 17.1 ± 10.2, p = 0.609), and annual frequency of attacks (6.3 ± 6.1 vs. 5.9 ± 4.8, p = 0.961). Duration of the aura is significantly longer in the MVA+ subgroup relative to the MVA subgroup (45.9 ± 29.9 vs. 27.1 ± 11.2, p = 0.011).
DT probabilistic tractography analysis
In DTI analyses, we did not detect any statistically significant differences in FA, MD, AD, and RD values of migraineurs with aura compared with healthy subjects (p > 0.0007, Bonferroni corrected for multiple comparisons, controlled for age and sex). There was a trend of AD reduction in the MA group relative to HS in following tracts: forceps minor, left uncinate fasciculus, and right ATR. Right SLFT and ATR showed trend to lower MD in the MA than in HS. Also, RD of the right CCT was lower in MA compared to HS. No significant difference was found in FA between MA and HS. All measures of diffusivity and anisotropy for uncorrected significant tracts between groups are presented in the Table 1 (data that survived a lesser conservative threshold set at 0.05, controlled for age and sex).
We did not detect any statistically significant differences in FA, MD, AD, and RD values of the MWA+ group compared with the MWA group (p > 0.05, Bonferroni corrected for multiple comparisons, controlled for age and sex). AD of forceps minor and right ILF showed trend to lower values in the MVA+ subgroup relative to the MVA subgroup. The MVA+ subgroup compared to the MVA subgroup showed trend to lower MD in right SLFP and CAB. The MVA+ subgroup also had lower RD in right SLFT, SLFP, and CAB. All measures of diffusivity and anisotropy for significant tracts between subgroups are presented in Table 2 (data that survived a lesser conservative threshold set at 0.05, controlled for age and sex).
TBSS voxel-wise analysis
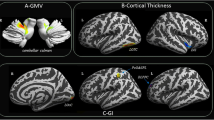
The results of the voxel-wise analysis of the significant fiber tracts (including RD measures) between MVA+ and MVA subgroups are shown in Fig. 1. Compared to the MVA+ subgroup, MVA subgroup had diffuse changes along with fiber tracts. To visually demonstrate the widespread changes, significant thresholds were set at p < 0.05, uncorrected for multiple comparisons.
MVA+ patients showed significantly decreased radial diffusivity (RD) relative to the MVA subgroup (p < 0.05, uncorrected—for illustration purposes only). Areas that were significantly different in selected fiber tracts are marked with yellow color. Patterns of changes in the MVA+ subgroup suggest hypermyelination of selected fiber tracts (SLFT, SLFP, ILF, CAB, and Forceps minor)
Clinical correlations
Aura frequency and AD or MD average values of the right ATR were negatively correlated (Partial correlation = − 0.474; p = 0.002; Partial correlation = − 0.460; p = 0.002), respectively. We did not find any clear correlation between FA or RD values of fiber tracts and duration of the aura or frequency of a migraine with aura attacks.
Discussion
The possible findings in this study were the presence of decreased AD, MD, and RD values in the white matter in a group of individuals with a migraine with aura compared with a similar group of individuals, balanced for age and sex, who have served as healthy controls. These white matter differences were predominantly in fiber tracts of the right hemisphere. Furthermore, this is the first study to show the possible differences of tracts integrity between subgroups of migraineurs with distinct phenotypes of the aura. We found that MD, RD, and AD values could be decreased in several brain bundles of the right hemisphere in patients with “complex” aura relative to those whose aura is limited to visual phenomena. Decreased diffusivity parameters could be due to subtle hypermyelination or increased axonal density of investigated tracts. These findings could possibly suggest structural plastic events in the white matter in patients with MA which are different relative to MA subgroups. Other interesting finding is the link between increased migraine with aura attacks frequency and lower AD and MD values of the right ATR.
Although several studies have investigated white matter alterations in migraineurs [6, 9], there is a lack of published studies investigating whole-tract alterations in migraineurs with aura and their subgroups. The approach used in this study is based on global probabilistic tractography [16]. The advantage of this method is that the automated path reconstruction prevents user-intervention errors and yields an automated procedure of assessing white matter tract integrity [17].
In our study, migraineurs had lower diffusivity and higher anisotropy of the examined fiber tracts in general, with emphasis to the MVA+ subgroup relative to the MVA subgroup. According to the literature, the pattern of FA increase/RD decrease is likely related to the enhancement of a tissue organization due to a reshaping of axonal or glial processes [18]. We could only speculate possible biological underpinnings of the observed diffusivity patterns. Indeed, decreased MD, RD and AD in several brain bundles induced by repeated acute stressors were shown in the experimental animals [19]. Increased white matter FA has been repeatedly associated with learning [20, 21] via neuronal plasticity processes (e.g., synaptogenesis and dendritic branching) and glial remodeling [22]. More recently, tract-based spatial statistics analysis also revealed higher FA/lower MD values in skilled learning rats in comparison with control that could be explained by increases in myelination [23]. Also, data from both human and animal studies indicate the potential for rapid changes in DTI parameters, suggesting changes in structural plasticity in specific brain regions [24]. This is particularly relevant if there is the ability of cortical spreading depolarization/depression (CSD) to trigger structural plastic events in the white matter as the compensatory mechanism of resilience to acute stress.
Having established that diffusion changes exist in patients with MA [9,10,11], it remains to conclude whether these changes are congenital or acquired due to the repetition of migraine attacks over time. The absence of general correlation between diffusion changes and a number of attacks and disease duration suggests that the observed DT MRI changes might represent a phenotypic biomarker of the disease, reflecting a congenital condition rather than a process related to disease progression. This hypothesis is further strengthening with results of Messina et al., where the same pattern of diffusion changes in pediatric migraine population was demonstrated [11]. However, aura frequency was negatively correlated with AD and MD values of the right ATR, according to the results of our study. This finding might reflect a hyperexcitability of the connection between thalamus and frontal lobe in migraineurs with aura, which could lead to more frequent attacks. We are more inclined to believe that subtle adaptation changes in the network and supporting tissue during brain maturation may lead to abnormalities which allow abundant phenomena (called aura) in individuals who suffer from MA. Indirect influences, such as the occurrence of microemboli [25] or impaired glymphatic flow due to CSD [26], should not be neglected.
In this study, we investigated several major fiber tracts with a known neurofunctional role. The fasciculus arcuatus (SLFT and SLFP) is the most important white matter bundle involved in language function because it appears to mediate the ability to understand words and organize the semantic content of verbal memory by connecting cortical regions in the frontal, temporal, and parietal lobes [27]. While these specific white matter tracts can be considered as default pathways when viewed in the context of cortical connectivity of the normal brain, the decreased MD values of these fiber pathways in migraineurs with an aura indicates neuroplastic changes as a result of increased connectivity between these neural loci [19]. Especially, it is interesting that the MVA+ subgroup had trend to decreased RD in the right SLFT and SLFP relative to the MVA subgroup, suggesting possible hypermyelination of fibers due to repetitive stress caused by CSD. Further functional MRI studies correlated with DTI findings should investigate is there a connection between higher cortical disturbances (e.g., dysphasia, dysnomia, and dyslexia) during the aura and decreased RD values in the Fasciculus arcuatus.
There are broad microstructural alterations in the thalamus of MA patients that may underlie abnormal cortical excitability control leading to CSD and migraine aura [28]. ATR project to the frontal lobe and anterior cingulate cortices [29], and it is shown that modulate pain in healthy controls [30]. In our study, we found trend to decreased diffusivity indices in MA relative to HS, which is in line with several studies that have demonstrated that pain and other typical migrainous symptoms result from abnormal activation and sensitization of the trigeminovascular and thalamic tracts [2, 31]. One more intriguing clue that can be derived from our results is that changes of AD and MD values of the ATR could support the notion that ATR is involved in the genesis of migraine-related photophobia, which is previously hypothesized [24]. There is only one study [7], according to our knowledge, which demonstrated opposite pattern of diffusivity changes in ATR among MA patients, but their interpretation of results supported the hypothesis of trigeminal sensory system dysfunction in migraineurs [32]. Further, DaSilva and colleagues speculated that decreased FA values over ATR do not reflect lesions in the brain, but rather an enlargement of axons as a response to over functioning [7]. Because of different findings from our results, further investigation of specific fiber tracts is needed for more conclusive explanation of changes along the anterior thalamic radiation in MA patients.
Numerous studies have demonstrated that the CAB is involved in core processes such as executive function, decision making, and emotion processing [33, 34]. Hence, changes in the CAB of diffusivity could potentially lead to more complex aura (e.g., dysphasia or dysnomia) in migraineurs and/or affect the emotion-affective state of pain [35]. Also, the MVA+ subgroup had decreased MD value of the right ILF relative to the MVA subgroup. The ILF connects posterior occipitotemporal regions to anterior temporal regions and has been implicated in transmitting information about object and face recognition [27], which could possibly explain prosopagnosia and dysnomia in the subgroup of the MVA+ subgroup.
Decreased AD value in the forceps minor, especially in the MVA+ subgroup, suggest his role in the pathogenesis of a migraine with aura, but exact role remains to be determined. One of the reasons for reduced AD value could be an increased density of cellular membranes, for instance of glial cells, that restrict the freedom of diffusion [36]. We could only speculate that this change is linked somehow to the ictal (manifestation of the aura) and non-ictal phase (e.g., depression outside of attacks), because of forceps minor connections with a frontal lobe.
Our study is not without limitations. First, although the number of studied patients is comparable to other studies, the sample size is still small for reliable conclusions. Different auras suggest an involvement of different white matter tracts, so the conflicting results of studies could be a result of patients’ heterogeneity. MA subgroups homogenized in accordance with clinical phenotype could provide more valuable results. Second, we did not assess’ pain severity as well as neuropsychological tests; hence we could not explore those influences on the white matter microstructure abnormalities. Longitudinal studies are also warranted to explore the dynamics of the evolution of white matter microstructural abnormalities to resolve the dilemma whether these abnormalities are cause or consequences of the migraine aura. Finally, we based our discussion on the results that were not corrected for multiple comparisons. Although this could lead to false-positive finding (type 1 error), correction for multiple comparison increases the risk of generating false-negative findings (type 2 error), which could underestimate subtle differences between MA patients and healthy subjects that were found previously [9,10,11] or obscure new one. Because of that, we think that is important to show and discuss uncorrected data for multiple comparisons to achieve better methodological solutions and directions for investigating changes of the white matter in MA patients and their subgroups.
Conclusion
In the current study, we investigated pathophysiological features of specific fiber tracts in MA patients. There were no significant differences between MA patients and HS, neither between MA subgroups. However, we found trend to reduced diffusivity patterns (MD, RD, or AD values) in the forceps minor, right SLFT, ATR, and CCT. Moreover, results demonstrate the possible sensitivity of DTI in revealing microscopic disease-related changes in subgroups (MVA+ and MVA) of migraineurs, yielding DTI indices which suggest hypermyelination of specific fiber tracts (forceps minor, right SLFT, SLFP, ILF, and CAB) in the MVA+ subgroup. Those changes may allow in some patients a faster spreading of the cortical depolarization wave through white matter tracts which could be manifested as higher cortical dysfunctions during an aura. Also, there is a possible connection between increased frequency of migraine with aura attacks and hypermyelination of the right ATR.
Nevertheless, migraine with aura still remains neurofunctional dysfunction, rather than structural. Future research in tractography should focus on identification of clinically distinct subgroups of MA patients to improve our knowledge of the migraine aura pathophysiology and subtle structural changes in the brain of migraineurs.
References
Headache Classification Committee of the International Headache Society (IHS) (2018) The international classification of headache disorders, 3rd ed. Cephalalgia 38:1–211
Noseda R, Burstein R (2013) Migraine pathophysiology: anatomy of the trigeminovascular pathway and associated neurological symptoms, cortical spreading depression, sensitization, and modulation of pain. Pain 154:S44–S53
Hadjikhani N, Sanchez Del Rio M, Wu O et al (2001) Mechanisms of migraine aura revealed by functional MRI in human visual cortex. Proc Natl Acad Sci USA 98:4687–4692
Petrusic I, Zidverc-Trajkovic J (2014) Cortical spreading depression: origins and paths as inferred from the sequence of events during migraine aura. Funct Neurol 29:207–212
Spreafico C, Frigerio R, Santoro P (2004) Visual evoked potentials in migraine. Neurol Sci 24:S288–S290
Rocca MA, Pagani E, Colombo B, Tortorella P, Falini A, Comi G, Filippi M (2008) Selective diffusion changes of the visual pathways in patients with migraine: a 3-T tractography study. Cephalalgia 28:1061–1068
DaSilva AF, Granziera C, Tuch DS, Snyder J, Vincent M, Hadjikhani N (2007) Interictal alterations of the trigeminal somatosensory pathway and periaqueductal gray matter in migraine. Neuroreport 18:301–305
Rocca MA, Messina R, Colombo B, Falini A, Comi G, Filippi M (2014) Structural brain MRI abnormalities in pediatric patients with migraine. J Neurol 261:350–357
Szabo N, Kincses ZT, Pardutz A et al (2012) White matter microstructural alterations in migraine: a diffusion weighted MRI study. Pain 153:651–656
Chong CD, Schwedt TJ (2015) Migraine affects white-matter tract integrity: a diffusion-tensor imaging study. Cephalalgia 35:1162–1171
Messina R, Rocca MA, Colombo B, Pagani E, Falini A, Comi G, Filippi M (2015) White matter microstructure abnormalities in pediatric migraine patients. Cephalalgia 35:1278–1286
Yendiki A, Panneck P, Srinivasan P et al (2011) Automated probabilistic reconstruction of white-matter pathways in health and disease using an atlas of the underlying anatomy. Front Neuroinform 5:23
Dale AM, Fischl B, Sereno MI (1999) Cortical surface-based analysis I: segmentation and surface reconstruction. Neuroimage 9:179–194
Behrens TEJ, Woolrich MW, Jenkinson M et al (2003) Characterization and propagation of uncertainty in diffusion-weighted MR imaging. Magn Reson Med 50:1077–1088
Smith SM, Jenkinson M, Johansen-Berg H et al (2006) Tract based spatial statistics: voxelwise analysis of multi-subject diffusion data. Neuroimage 31:1487–1505
Jbabdi S, Woolrich MW, Andersson JL, Behrens TEJ (2007) A Bayesian framework for global tractography. NeuroImage 37:116–129
Yan J, Yonggang S, Liang Z et al (2014) Automatic clustering of white matter fibers in brain diffusion MRI with an application to genetics. Neuroimage 100:75–90
Assaf Y, Pasternak O (2008) Diffusion tensor imaging (DTI)-based white matter mapping in brain research: a review. J Mol Neurosci 34:51–61
Magalhães R, Bourgin J, Boumezbeur F et al (2017) White matter changes in microstructure associated with a maladaptive response to stress in rats. Transl Psychiatry 7:e1009
Blumenfeld-Katzir T, Pasternak O, Dagan M, Assaf Y (2011) Diffusion MRI of structural brain plasticity induced by a learning and memory task. PLoS One 6:e20678
Ding AY, Li Q, Zhou IY, Ma SJ, Tong G, McAlonan GM, Wu EX (2013) MR diffusion tensor imaging detects rapid microstructural changes in amygdala and hippocampus following fear conditioning in mice. PLoS One 8:e51704
Zatorre RJ, Fields RD, Johansen-Berg H (2012) Plasticity in gray and white: neuroimaging changes in brain structure during learning. Nat Neurosci 15:528–536
Sampaio-Baptista C, Khrapitchev AA, Foxley S et al (2013) Motor skill learning induces changes in white matter microstructure and myelination. J Neurosci 33:19499–19503
Hofstetter S, Tavor I, Tzur Moryosef S, Assaf Y (2013) Short-term learning induces white matter plasticity in the fornix. J Neurosci 33:12844–12850
Petrusic I, Podgorac A, Zidverc-Trajkovic J, Radojicic A, Jovanovic Z, Sternic N (2016) Do interictal microembolic signals play a role in higher cortical dysfunction during migraine aura? Cephalalgia 36:561–567
Schain AJ, Melo-Carrillo A, Strassman AM, Burstein R (2017) Cortical spreading depression closes paravascular space and impairs glymphatic flow: implications for migraine headache. J Neurosci 37:2904–2915
Catani M, Mesulam M (2008) The arcuate fasciculus and the disconnection theme in language and aphasia: history and current state. Cortex 44:953–961
Granziera C, Daducci A, Romascano D, Roche A, Helms G, Krueger G, Hadjikhani N (2014) Structural abnormalities in the thalamus of migraineurs with aura: a multiparametric study at 3 T. Hum Brain Mapp 35:1461–1468
Mamah D, Conturo TE, Harms MP et al (2010) Anterior thalamic radiation integrity in schizophrenia: a diffusion tensor imaging study. Psychiatry Res 183:144–150
Erpelding N, Davis KD (2013) Neural underpinnings of behavioural strategies that prioritize either cognitive task performance or pain. Pain 154:2060–2071
Charles AC, Baca SM (2013) Cortical spreading depression and migraine. Nat Rev Neurol 9:637–644
Gustin SM, Peck CC, Wilcox SL, Nash PG, Murray GM, Henderson LA (2011) Different pain, different brain: thalamic anatomy in neuropathic and non-neuropathic chronic pain syndromes. J Neurosci 31:5956–5964
Heilbronner SR, Haber SN (2014) Frontal cortical and subcortical projections provide a basis for segmenting the cingulum bundle: implications for neuroimaging and psychiatric disorders. J Neurosci 34:10041–10054
Adnan A, Barnett A, Moayedi M, McCormick C, Cohn M, McAndrews MP (2016) Distinct hippocampal functional networks revealed by tractography-based parcellation. Brain Struct Funct 221:2999–3012
Vogt BA (2005) Pain and emotion interactions in subregions of the cingulate gyrus. Nat Rev Neurosci 6:533–544
Beaulieu C (2002) The basis of anisotropic water diffusion in the nervous system - a technical review. NMR Biomed 15:435–455
Acknowledgements
We thank Snezana Dikic for excellent technical MR scanning skills.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: IP and MD received research grant support from the Ministry of Education and Science, Republic of Serbia (project no. III 41005), and JZT received research grant support from the Ministry of Education and Science, Republic of Serbia (project no. 175022).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Petrušić, I., Daković, M., Kačar, K. et al. Migraine with aura and white matter tract changes. Acta Neurol Belg 118, 485–491 (2018). https://doi.org/10.1007/s13760-018-0984-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13760-018-0984-y