Abstract
Carbamazepine (CBZ) intoxication can occur due to various factors, including drug interactions and over-ingestion. Extracorporeal elimination, particularly through hemodialysis and hemoperfusion, is effective in treating severe carbamazepine intoxication. However, as the effectiveness of various modalities can differ, method selection may be based on a specific clinical situation. A 47-year-old woman who took CBZ for schizophrenia presented to our hospital with episodes of vomiting and consciousness disorder. As the CBZ concentration was > 20 μg/mL, she was admitted to the intensive care unit with a diagnosis of acute CBZ poisoning. She underwent one session of hemoperfusion for 2 h, and her CBZ level decreased from > 20 µg/mL to 6.4 µg/mL. However, she developed acute kidney and liver injuries 2 days after admission and underwent intermittent hemodialysis, plasma exchange, continuous hemodiafiltration (CHDF), and online HDF, depending on her condition. Her general condition improved, and she was transferred to the psychiatric department. To our knowledge, no case reports have described severe acute CBZ poisoning in a patient who developed multiorgan failure to date, which was successfully treated with multimodal blood purification therapy. When treating severe CBZ intoxication, blood purification therapy should be tailored to the changing pathophysiology of the condition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Carbamazepine (CBZ), a widely used anticonvulsant agent, is also being increasingly used for pain management, mood disorders, and schizophrenia [1]. With increasing blood concentrations of CBZ, intoxication symptoms may occur. In mild-to-moderate cases, involuntary movements, ataxia, and nystagmus are observed. In severe cases, patients present with arrhythmia, deep coma, convulsions, multiorgan failure, and respiratory arrest. The mortality rate of CBZ intoxication is approximately 13% [2]. The adult therapeutic plasma level of CBZ is between 4 and 12 µg/mL [3]. CBZ intoxication can be treated by supportive care, prevention of further drug absorption, and enhancement of drug elimination with blood purification therapy. The treatments are also effective for cases of acute liver or acute kidney injury, which are severe symptoms of CBZ intoxication. Several extracorporeal therapies (ECTRs), including charcoal hemoperfusion (HP), hemodialysis (HD), hemodiafiltration (HDF), and plasma exchange (PE), are applied for treating severe CBZ intoxication [4]. However, no report has shown that the combined modality mode technique is effective for saving lives. Here, we report a case of severe acute CBZ intoxication in a patient who developed multiorgan failure, which was successfully treated by multimodal blood purification therapy.
Case report
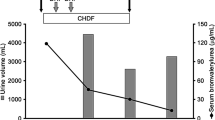
A 47-year-old woman who presented with episodes of vomiting and disorder of consciousness was transferred to our hospital. Prior to hospital presentation, she experienced abdominal pain and nausea for 2 weeks and was unable to eat for 5 days. Regarding her medical history, she had schizophrenia and was taking CBZ, brexpiprazole, sulpiride, biperiden, quetiapine fumarate, alprazolam, lorazepam, and duloxetine hydrochloride. At the time of hospitalization, her temperature was 37.2 °C, her pulse rate was 134 beats per minute, her blood pressure was 129/97 mmHg, and her oxygen saturation was 73% in room air. On physical examination, her Glasgow Coma Scale score was E1V1M3, her pupils were dilated, and her pupil reflexes were decreased. Laboratory studies demonstrated mildly elevated hepatobiliary enzyme levels, renal dysfunction, hyperkalemia, hypochloremia, hypocalcemia, and hyperphosphatemia. CK was within normal range although there was a discrepancy between the occult blood reaction and the RBC count in the urine sample. Importantly, the CBZ concentration was > 20 µg/mL. Other clinical laboratory data are shown in Table 1. Twelve-lead EKG records showed a normal sinus and no irregular rhythm. Computed tomography of the head revealed no abnormality. Given the abovementioned findings, the patient was admitted to the intensive care unit with a diagnosis of CBZ intoxication. After admission, she was intubated, and activated charcoal was administered twice, but her level of consciousness and pupil condition showed little improvement. She underwent one session of HP for 2 h. The blood flow rate was 100 mL/min (Supplementary Table 1). After HP, her CBZ level decreased from > 20 µg/mL to 6.4 µg/mL, and her pupil dilation improved. On the second day, the hepatobiliary enzyme and creatinine levels were highly elevated, and her urine output was decreased; therefore, she was treated with 6 units of fresh frozen plasma (FFP) and intermittent hemodialysis (IHD) (Supplementary Table 1). The next day, the level of her hepatobiliary enzymes were further elevated; thus, she received PE with 30 units of FFP (Supplementary Table 1). Her blood pressure was slightly unstable; therefore, continuous hemodiafiltration (CHDF) was also performed (Supplementary Table 1). Thereafter, her vitals became stable, and she was treated with online HDF to address her hyperammonemia and hepatic insufficiency (Supplementary Table 1). Gradually, the hepatobiliary enzyme and ammonia levels decreased, and her level of consciousness also improved. Her renal function also tended to improve, and her urine output increased; therefore, she was weaned off online HDF on the 30th day. Her general condition tended to improve, and she was weaned off the ventilator and transferred to the psychiatric department on day 42 (Fig. 1).
Discussion
In this case, we discovered the importance of multimodal blood purification therapy for saving lives due to the dramatically changing pathophysiology of multiorgan failure due to CBZ intoxication.
The pharmacological toxicity of CBZ results from its binding to sodium channels, inhibition of neuronal depolarization, and a reduction in glutamate release. CBZ has anticholinergic effects at high concentrations, and its intoxication frequently presents with neurological, cardiovascular, and anticholinergic symptoms. While mild toxicity results in drowsiness, nystagmus, tachycardia, hyperreflexia, or dysmetria, severe cases may lead to lethargy, seizure, coma, QRS prolongation, hemodynamic instability, and pronounced anticholinergic symptoms, especially ileus. CBZ intoxication diagnosis relies on the history and presence of typical clinical findings and is confirmed using laboratory examinations. The symptoms become more severe at concentrations of > 40 µg/mL, although a clear correlation with mortality is uncertain [2, 5]. Most patients with CBZ poisoning can be managed with supportive care alone, including fluid administration, ventilatory support, benzodiazepine use for seizure control, and vasopressor use for hypotension. Activated charcoal is mostly used for gastrointestinal decontamination for acute CBZ poisoning, although its effectiveness in improving the clinical outcomes has not been proven and is contraindicated in cases with ileus [6]. The American Academy of Clinical Toxicologists and European Association of Poisons Centers and Clinical Toxicologists recommend that activated charcoal should be considered only if a patient has ingested a life-threatening amount of CBZ [7].
Severe CBZ intoxication can be treated using ECTR, which can provide better and more predictable clearance than activated charcoal, particularly in cases with an ileus. Sikma et al. reported that the elimination rate constant (Ke) of CBZ, which is calculated as ke = ln 2/half-life (h) and reflects the effectiveness of the elimination route, was 0.009/h, 0.039/h, and 0.059/h during endogenous metabolism, administration of activated charcoal, and ECTR, respectively [8]. The Extracorporeal Treatments in Poisoning workgroup has reported that ECTR is beneficial for reducing short-term morbidity (related to severe hypotension and recurrent seizures) and avoiding complications related to prolonged respiratory insufficiency and coma (e.g. ventilator-associated pneumonia, pulmonary emboli, and immobilization). Moreover, it proposed the indications for ECTR [4]. ECTR is recommended in the following conditions: if multiple seizures refractory to treatment occur, life-threatening dysrhythmias occur, prolonged coma or respiratory depression requiring mechanical ventilation is present or expected, and significant toxicity persists, especially if the CBZ concentrations increase or remain elevated despite the administration of activated charcoal and application of support measures. The workgroup proposed that ECTR should be indicated until sustained clinical improvement is apparent or the serum CBZ concentration is < 10 µg/mL.
CBZ (molecular weight, 236 Da) is lipophilic and has a volume of distribution of 1.2L/kg and protein binding rate of approximately 75%, which does not decrease much in cases of overdose. Therefore, HP is the most effective technique for CBZ elimination. Yang et al. reported that patients managed with early HP experienced lower peak CBZ concentrations, fewer cases of respiratory depression, fewer episodes of seizures, and shorter hospitalization than patients not treated with extracorporeal elimination [9].
Recent data have demonstrated that IHD is almost as effective as HP because of improved clearances provided by high-flux membranes, high blood flow, and larger catheters [10]. Globally, IHD is preferred for maintenance dialysis in patients with end-stage kidney disease and acute kidney injury, making it the most available modality. Meanwhile, the availability of HP cartridges is limited worldwide. Therefore, the travel distance to an HD center for a poisoned patient would likely be minimized [4]. Moreover, IHD is preferred because of its lower cost and complication rate as compared to HP [11]. However, several studies have shown a greater initial CBZ clearance with charcoal HP than with IHD. Isik et al. have shown that the removal rate of CBZ with HP is 58% within 1 h, which is superior to that of IHD (15% within 4 h) [12]. Pilapil et al. demonstrated that, during a 4-h treatment, the extraction ratio of CBZ was excellent with HP at the start of treatment; however, it decreased over time and approached the extraction ratio achieved with IHD because of the reduced charcoal absorptive capacity after the first hour with prolonged treatment, reflecting cartridge saturation [13]. Therefore, HP is the most effective therapy based on the efficacy of CBZ extraction, if cartridges are available and physicians and nursing personnel are comfortable performing this technique.
Severe CBZ intoxication can result in multiorgan failure. In this case, the patient developed acute kidney and acute liver injuries on day 2 after admission and was treated with IHD, PE, continuous HDF, and online HDF, depending on her condition. Durelli have reported fatal liver injury as an unforeseeable idiosyncratic reaction of CBZ [14]. Skopp et al. demonstrated that the autopsy of a 22-year-old woman with a history of developmental delay and seizures treated with CBZ who died of fulminant hepatic failure showed acute tubular necrosis in the kidneys, preexisting and marked accumulation of neutral lipids within the hepatocytes, and hyperacute liver damage with almost complete hepatocyte necrosis [15]. Moreover, they described that long-term administration of CBZ increases the production of free radicals, leaving the hepatic cell more vulnerable to oxidative injury [15]. Although hyperammonemia as a symptom of CBZ intoxication is less commonly observed than valproic acid toxicity, Adams et al. reported a case of CBZ-induced hyperammonemia [16]. In this case, acute liver injury and CBZ intoxication may have induced hyperammonemia. Hyperammonemia is associated with intracranial hypertension and mortality in patients with acute liver failure. Blood purification therapy for acute liver failure can bring the patient out of a coma and keep him/her in good condition until the liver regenerates. PE is recommended in acute liver failure to replace the deficient plasma proteins and coagulation factors; however, it has poor coma-waking effects. This is because PE only replaces a plasma portion, and the amount of solutes removed is determined by plasma volume used. Therefore, when water-soluble substances with a large volume of distribution in the body are targeted, the removal capacity is inferior to that of HDF using a large volume of replacement fluid. HDF can remove low-molecular-weight substances with a large volume of distribution, including ammonia, and medium-molecular-weight substances, which are assumed to be related to hepatic encephalopathy. Fujiwara et al. showed that the recovery rate of consciousness abnormalities of PE and online HDF is 37.5% and 92.9%, respectively [17]. In this case, online HDF was performed for acute liver injury due to CBZ intoxication, which gradually improved the patient’s ammonia and consciousness levels.
In conclusion, Blood purification therapy for severe CBZ intoxication should be flexible according to the changing pathophysiology of the condition.
Data availability
The dataset supporting the conclusions of this article was included within the article.
Abbreviations
- CBZ:
-
Carbamazepine
- CHDF:
-
Continuous hemodiafiltration
- ECTR:
-
Extracorporeal therapy
- FFP:
-
Fresh frozen plasma
- HD:
-
Hemodialysis
- HDF:
-
Hemodiafiltration
- HP:
-
Hemoperfusion
- IHD:
-
Intermittent hemodialysis
- PE:
-
Plasma exchange
References
Israel M, Beaudry P. Carbamazepine in psychiatry: a review. Can J Psychiatry. 1988. https://doi.org/10.1177/070674378803300701.
Schmidt S, Schmitz-Buhl M. Signs and symptoms of carbamazepine overdose. J Neurol. 1995. https://doi.org/10.1007/bf00936891.
Lai MW, Klein-Schwartz W, Rodgers GC, Abrams JY, Haber DA, Bronstein AC, et al. Annual Report of the American Association of Poison Control Centers’ national poisoning and exposure database. Clin Toxicol (Phila). 2005. https://doi.org/10.1080/15563650600907165.
Ghannoum M, Yates C, Galvao TF, Sowinski KM, Vo TH, Coogan A, et al. Extracorporeal treatment for carbamazepine poisoning: systematic review and recommendations from the EXTRIP workgroup. Clin Toxicol (Phila). 2014. https://doi.org/10.3109/15563650.2014.973572.
Hojer J, Malmlund HO, Berg A. Clinical features in 28 consecutive cases of laboratory confirmed massive poisoning with carbamazepine alone. J Toxicol Clin Toxicol. 1993. https://doi.org/10.3109/15563659309000412.
Mise S, Jukić I, Tonkić A, Titlić M, Mise S. Multidose activated charcoal in the treatment of carbamazepine overdose with seizures: a case report. Arh Hig Rada Toksikol. 2005;56:333–8.
American Academy of Clinical Toxicology, European Association of Poisons Centres and Clinical Toxicologists. Position statement and practice guidelines on the use of multi-dose activated charcoal in the treatment of acute poisoning. American Academy of Clinical Toxicology; European Association of Poisons Centres and Clinical Toxicologists. J Toxicol Clin Toxicol, https://doi.org/10.1081/clt-100102451 (1999)
Sikma MA, van den Broek MP, Meulenbelt J. Increased unbound drug fraction in acute carbamazepine intoxication: suitability and effectiveness of high-flux haemodialysis. Intensive Care Med. 2012. https://doi.org/10.1007/s00134-012-2501-8.
Yang X, Xin S, Zhang Y, Li T. Early hemoperfusion for emergency treatment of carbamazepine poisoning. Am J Emerg Med. 2018. https://doi.org/10.1016/j.ajem.2017.10.048.
Tapolyai M, Campbell M, Dailey K, Udvari-Nagy S. Hemodialysis is as effective as hemoperfusion for drug removal in carbamazepine poisoning. Nephron. 2002. https://doi.org/10.1159/000049045.
Shannon MW. Comparative efficacy of hemodialysis and hemoperfusion in severe theophylline intoxication. Acad Emerg Med. 1997. https://doi.org/10.1111/j.1553-2712.1997.tb03758.x.
Isik Y, Soyoral L, Karadas S, Emre H, Cegin MB, Goktas U. Effectivity of one session charcoal hemoperfusion treatment in severe carbamazepine poisoning. Iran Red Crescent Med J. 2013. https://doi.org/10.5812/ircmj.7516.
Pilapil M, Petersen J. Efficacy of hemodialysis and charcoal hemoperfusion in carbamazepine overdose. Clin Toxicol (Phila). 2008. https://doi.org/10.1080/15563650701264300.
Durelli L, Massazza U, Cavallo R. Carbamazepine toxicity and poisoning. Incidence, clinical features and management. Med Toxicol Adverse Drug Exp. 1989. https://doi.org/10.1007/bf03259906.
Skopp G, Schmitt HP. Pedal I [Fulminant liver failure in a patient on carbamazepine and levetiracetam treatment associated with status epilepticus]. Arch Kriminol. 2006;217:161–75.
Adams EN, Marks A, Lizer MH. Carbamazepine-induced hyperammonemia. Am J Health Syst Pharm. 2009. https://doi.org/10.2146/ajhp080454.
Fujiwara K, Abe R, Yasui S, Yokosuka O, Kato N, Oda S. High recovery rate of consciousness by high-volume filtrate hemodiafiltration for fulminant hepatitis. Hepatol Res. 2019. https://doi.org/10.1111/hepr.13255.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
CS, MH, YH, YS, AO, and HK were involved in the clinical care of the patient, managed the literature searches, and wrote the first draft of the manuscript. SY and IN helped in drafting the manuscript. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Sakurazawa, C., Habuka, M., Hoshino, Y. et al. A case of multiorgan failure due to carbamazepine intoxication successfully treated with multimodal blood purification therapy. CEN Case Rep (2024). https://doi.org/10.1007/s13730-024-00900-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13730-024-00900-3




