Abstract
Introduction
Valproic acid (VPA) toxicity commonly results in a self-limited state of CNS depression that is managed with supportive care and levocarnitine. In massive overdose, patients can develop toxic encephalopathy, shock, multisystem organ failure, and death. We present a case with relevant toxicokinetics of a patient presenting with a profoundly elevated VPA concentration resulting in survival, treated with supportive care including high-dose continuous venovenous hemodiafiltration (CVVHDF).
Case Report
A 17-year-old female presented to an emergency department after being found unresponsive at home with concern for massive VPA ingestion. She arrived obtunded and hypotensive with initial VPA concentration of 2226 mg/L, estimated 9 h post-ingestion. Her early hospital course was marked by hypotension requiring multiple vasopressors, and her workup was notable for multiple severe metabolic derangements. High-dose CVVHDF was initiated upon transfer to a tertiary children’s hospital with the aim to enhance VPA removal and normalize metabolic derangements. At that time, her VPA concentration was 1071 mg/L. Apparent half-life of VPA improved modestly with extracorporeal treatment, but her metabolic derangements and hemodynamic instability corrected rapidly. Her clinical course was complicated by necrotizing pancreatitis, pancytopenia requiring transfusions of multiple cell lines, coma, and seizures. She ultimately recovered with normal neurological function.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Valproic acid (VPA) is a commonly prescribed medication, frequently used as an anticonvulsant and mood stabilizer. Overdose is common, with over 3000 single agent exposures reported to poison centers in 2019 [1]. Multiple case series have demonstrated that most patients with VPA ingestion have minimal toxicity with lethargy being the most common manifestation, and hospital stays are usually short [2, 3]. Treatment in cases of mild toxicity is largely supportive, though l-carnitine supplementation is indicated in cases of associated hyperammonemia.
However, patients with massive overdose can develop more serious complications. A large case series identified patients with a VPA concentration greater than 450 mg/L more likely to develop serious clinical effects and longer hospitalization. Patients with VPA concentration greater than 850 mg/L were more likely to develop coma, respiratory depression, or metabolic acidosis [3].
Extracorporeal treatment (ECTR) is effective in enhancing VPA elimination and is a recommended treatment for severe toxicity [4]. Intermittent HD (IHD) is superior to continuous renal replacement therapy (CRRT) in enhancing VPA elimination, though the clinical implication of this difference is unclear. We highlight our management including high-dose CRRT in a patient with a massive overdose with a profoundly elevated VPA concentration resulting in survival.
Case Report
Our patient was a 17-year-old female with a history of bipolar type II disorder and ADHD found unresponsive but breathing at home after a night of sleep. Her prescription VPA bottle had 88 (eighty eight) 500 mg pills missing. EMS was called, and she was transported to a nearby hospital.
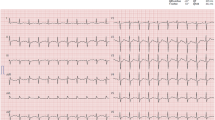
Upon arrival, she was hypotensive with a BP 89/46 mmHg, heart rate in the 80s, and SpO2 > 95% on room air. She was intubated due to unresponsiveness. Her VPA concentration approximately 9 hours post-ingestion was elevated at 2226 mg/L (normal 50-125 mg/L), and other standard labs were otherwise notable for a mixed metabolic and respiratory acidosis on venous blood gas, hyperammonemia, and mild hyperlactatemia. Aspirin, acetaminophen, and ethanol were undetectable and urine drug screen was negative. Her head CT was normal. She was given one dose of activated charcoal via gastric tube and IV levocarnitine 100 mg/kg. She was also given 1 L of 0.9% NaCl, started on an epinephrine infusion, and treated with calcium gluconate and sodium bicarbonate in response to ectopy on cardiac monitor. She was then transferred to a tertiary care children’s hospital via fixed wing transport for emergent dialysis and further critical care.
On arrival to the children’s hospital, she was hypotensive with mean arterial pressure ranging 40–50 mmHg. Her physical exam demonstrated no response to painful stimuli, minimally reactive dilated pupils, and no corneal reflexes. Her labs were notable for hypernatremia, metabolic acidosis with markedly rising lactate, and persistently toxic VPA concentration of 1071 mg/L with resultant hyperammonemia (Table 1). She was treated with escalation of norepinephrine, epinephrine, and fluid boluses.
CRRT was chosen in favor of IHD due to her hemodynamic instability. Within 2 hours of arrival to the children’s hospital, she was initiated on CRRT with continuous venovenous hemodiafiltration (CVVHDF) using HF1000 filter on Prismax system and citrate anticoagulation. Her CRRT dose was prescribed with dialysis and replacement fluids at a rate of 6100 mL/hour/1.73 m2 (compared with 2000–3000 mL/hour/1.73 m2 with standard CRRT) and a blood flow rate of 4.5–5 mL/kg/minutes (compared to standard blood flow rate of 2–4 mL/kg/minutes for her age). Her CRRT clotted off and needed to be restarted once during her treatment period. Once VPA was less than 100 mg/L, flow rates were decreased to 5000 mL/hour/1.73 m2 and finally to 3600 mL/hour/1.73 m2.
Her VPA concentration decreased to 462 mg/L over the first 7 hours of her admission and was less than 100 mg/L by 32 hours. Lactate, blood gas, and electrolytes normalized on CRRT within 8–10 hours, and her vasoactive agents were weaned off within 24 hours. She was treated with IV levocarnitine 15 mg/kg every 4 hours from time of admission until VPA concentrations were less than 100 mg/L. Her neurological exam upon discontinuation of CRRT demonstrated encephalopathy with reactive pupils and non-purposeful movements of all extremities. CRRT was continued for a total of 21 hours.
After extubation, her course was complicated by other organ dysfunctions, most notably pancreatitis, encephalopathy, anemia, and thrombocytopenia. Due to increased abdominal distention with advancement of enteral feeds, a CT scan was obtained that showed necrotizing pancreatitis; the pancreas was nearly replaced with fluid and there was a large amount of abdominal and pelvic free fluid. She tolerated slow advancement of enteral nutrition while parenteral nutrition was continued. She was diagnosed with type 3C diabetes and initiated on subcutaneous glargine and lispro regimen. Despite a normal brain MRI obtained on hospital day 3, her neurologic status was slow to improve, and she had an EEG that diagnosed presumed underlying epilepsy for which she was started on lacosamide. Her hemoglobin and platelets were normal on arrival but trended down early in her clinical course, reaching nadirs on hospital days 4 and 3, respectively, with her thrombocytopenia prompting transfusion of 4 units of platelets. After 22 days of inpatient hospitalization, she was transferred to inpatient psychiatry hospitalization with a normal cardiopulmonary status, normal renal function, normal neurologic exam, eating a regular diet, and on new baseline medications of subcutaneous insulin and lacosamide. Consent for publication of this case was obtained and provided to the journal in accordance with JMT policy.
Discussion
We report a case of survival from life-threatening VPA toxicity and metabolic derangement after overdose. Previously reported cases with similarly high concentrations have been associated with death. To our knowledge, the highest VPA concentration reported in the literature prior to this report was 2725 mg/L in a 40-year-old female who died 72 hours after ingestion [5]. Her development of encephalopathy, seizures, acidosis, pancreatitis, pancytopenia, and shock is a classic manifestation of life-threatening toxicity [6,7,8,9].
Because of its small molecular size and volume of distribution, VPA is amenable to removal by ECTR. At therapeutic concentrations, VPA is highly protein bound. However, protein binding is saturable, and percent binding decreases in the setting of overdose. One case report documents an unbound VPA fraction of 85% at a total plasma concentration of 1244 mg/L, as compared to 56% at plasma concentration 105 mg/L [10]. The need for patient transfer delayed time to initiation of ECTR. However, her VPA concentration remained markedly elevated, her electrolyte and metabolic derangements worsened upon arrival to our facility, and we therefore anticipated ECTR would positively impact her care.
The EXTRIP consortium recommends ECTR in cases of severe VPA toxicity, specifically cases with VPA concentration greater than 1300 mg/L, shock, and cerebral edema. Several studies demonstrate superior removal of VPA via IHD over CRRT (half-lives 2.5 vs 9.6 h, respectively), correction of acidemia, and clearance of ammonia. However, in this case, it was unclear if the patient would tolerate the volume shifts attendant with IHD given her hemodynamic instability as evidenced by her significant vasopressor requirements. Therefore, high-dose CVVHDF was utilized with the aim of enhancing VPA clearance and normalizing metabolic derangement.
VPA was eliminated under first-order kinetics throughout her hospitalization. Apparent half-life was minimally impacted by use of CVVHDF, decreasing from 8.5 to 5.8 hours, though the terminal half-life did extend to 22 hours post-CVVHDF (Fig. 1). Despite its unclear, and potentially minimal, impact on acute VPA elimination, the use of CVVHDF rapidly improved numerous metabolic derangements including her hypernatremia, metabolic acidosis, and moderately elevated serum lactate. The correction of these derangements led to the stabilization of her hemodynamic status and the ability to wean off vasopressor support. Furthermore, continuing the therapy for 21 h likely prevented VPA concentration “rebound” from redistribution.
It is unclear if IHD and more rapid drug removal would have prevented her subsequent complications from VPA toxicity. Previous reports and kinetics analyses of ECTR in massive VPA overdose demonstrate superior drug clearance and more rapid clinical improvement using IHD for ECTR as compared to CRRT. Our patient’s metabolic derangements, shock, and encephalopathy resolved rapidly, but her clinical course was otherwise complicated by thrombocytopenia and anemia requiring transfusions, necrotizing pancreatitis with resulting insulin dependent diabetes, acute kidney injury, and seizures. Given this patient’s complicated course and the unclear impact of CVVHDF on her VPA elimination, we concur with the EXTRIP conclusion that IHD should remain the first-line ECTR modality for rapid VPA removal in cases of massive overdose. In patients with severe hemodynamic instability, CRRT may be the only form of ECTR that can be tolerated in life-threatening VPA poisoning. Its benefits are primarily reversal of metabolic derangement in such cases, and the potential for possible limited enhancement of VPA clearance. This may explain our patient’s clinical improvement.
As this is a single case report, our conclusions and their generalizability are limited. It is important to acknowledge that dialysate VPA concentrations were not collected, and thus we were unable to calculate VPA extraction ratio and clearance. While we do report apparent half-life over her clinical course, its use as a marker of efficacy of ECTR has inherent limitations, as it cannot account for concurrent processes such as ongoing drug absorption, redistribution into the tissue, or endogenous metabolism and elimination. The benefits of aggressive and goal-directed resuscitation and critical care support in this case must also me acknowledged. However, these limitations do not impact our conclusion that its role in managing concomitant metabolic disturbances may be beneficial in patients with severe VPA poisoning and hemodynamic instability.
Conclusion
Intermittent hemodialysis (IHD) is reported to have superior VPA clearance compared to continuous renal replacement therapy (CRRT). However, in cases of severe hemodynamic instability, CRRT may be the only tolerated modality in severe VPA poisoning. This case suggests CRRT strategies may have a role in correcting metabolic derangements in patients who are hemodynamically unstable.
References
Gummin D, Mowry J, Beuhler M, et al. 2019 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 37th Annual Report. Clin Toxicol (Philadelphia, Pa). 2020;58(12):1360–541.
Isbister GK, Balit CR, Whyte IM, Dawson A. Valproate overdose: a comparative cohort study of self poisonings. Br J Clin Pharmacol. 2003;55(4):398–404. https://doi.org/10.1046/j.1365-2125.2003.01772.x.
Spiller HA, Krenzelok EP, Klein-Schwartz W, Winter ML, Weber JA, Sollee DR, Bangh SA. Multicenter case series of valproic acid ingestion: serum concentrations and toxicity. J Toxicol Clin Toxicol. 2000;38(7):755–60. https://doi.org/10.1081/CLT-100102388.
Ghannoum M, Laliberté M, Nolin TD, Mactier R, Lavergne V, Hoffman RS, Gosselin S, Anseeuw K, Bhalla A, Burdmann EA, Calello DP, Dargan PI, Decker BS, Galvao TF, Goldfarb DS, Hoegberg LC, Juurlink DN, Li Y, Liu KD, … Yates C. Extracorporeal treatment for valproic acid poisoning: systematic review and recommendations from the EXTRIP workgroup. Clin Toxicol 2015;53(5):454–465. https://doi.org/10.3109/15563650.2015.1035441
Connacher AA, Macnab MS, Moody JP. Fatality due to massive overdose of sodium valproate. Scott Med J. 1987;32:85–6.
Muñiz AE. Valproic acid overdose review of a case with electrocardiographic changes. J Emerg Med. 2017;53(3):333–8. https://doi.org/10.1016/j.jemermed.2016.07.017.
Patrick KA, Jarriel JT, Hieger MA. Pancreatic pseudocyst due to acute valproic acid overdose. Am J Ther. 2018;25(5):E584–5. https://doi.org/10.1097/MJT.0000000000000684.
Ray S, Khamrui S, Kataria M, Biswas J, Saha S. Valproic acid-induced severe acute pancreatitis with pseudocyst formation: report of a case. Cureus. 2015;7(8):5–10. https://doi.org/10.7759/cureus.297.
Sztajnkrycer MD. Valproic acid toxicity: overview and management. J Toxicol Clin Toxicol. 2002;40(6):789–801. https://doi.org/10.1081/CLT-120014645.
van den Broek MPH, Sikma MA, Ververs TF, Meulenbelt J. Severe valproic acid intoxication: case study on the unbound fraction and the applicability of extracorporeal elimination. Eur J Emerg Med. 2009;16(6):330–2. https://doi.org/10.1097/MEJ.0b013e32832c7b18.
Funding
None
Consent for publication of this case was obtained and provided to the journal in accordance with JMT policy.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
None.
Additional information
Supervising Editor: Andis Graudins, MB BS, Ph D.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Previous presentations: Data in this manuscript were previously presented at the North American Congress of Clinical Toxicology (NACCT) in October 2021.
Rights and permissions
About this article
Cite this article
Comstock, G., Kilgallon, K., Wang, G.S. et al. Management and Associated Toxicokinetics of Massive Valproic Acid Ingestion with High Flow Continuous Venovenous Hemodiafiltration. J. Med. Toxicol. 18, 239–242 (2022). https://doi.org/10.1007/s13181-022-00881-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13181-022-00881-8