Abstract
Purpose of Review
Atopic dermatitis (AD) poses a significant financial and disease burden on affected patients and families, prompting increased interest in primary prevention strategies. This review summarizes promising interventions aimed at preventing AD in childhood, with a focus on evidence from recent clinical trials and large cohort studies.
Recent Findings
While prophylactic emollient use for AD prevention initially appeared promising, recent follow up studies have cast doubt on its effectiveness. Perinatal probiotics may moderately reduce the risk of childhood AD, especially among children at high-risk of allergic disease. However, there are insufficient high-quality studies to support prebiotic supplements, breastfeeding, partially hydrolyzed infant formula, other perinatal nutritional supplements, or specific material diets for prevention of AD.
Summary
Given the prevalence of AD, interventions with relatively small effect sizes would have a major impact on population health. Based on available evidence, the use of probiotic supplements for infants, pregnant women, and breastfeeding mothers is the most promising strategy. However, additional large clinical trials are likely needed before universal recommendations can be issued.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Atopic dermatitis (AD) is a common chronic inflammatory skin disorder that affects more than 200 million individuals worldwide [1]. It typically begins in infancy and often improves with age, although it can persist into or onset during adulthood [1]. Due to its intensely pruritic nature and chronic disease course, AD has an enduring impact on the quality of life of both patients and caregivers. AD is associated with sleep disturbance, irritability, behavioral problems, and other psychosocial comorbidities, especially in children [2]. There is also a significant financial cost to managing AD, both to patients and to the healthcare system [3]. As such, tremendous research efforts have been directed towards AD treatments, and new effective topical and systemic medications continue to emerge.
Prevention of AD has also been a topic of increasing interest. Considering the high prevalence of AD in infants and children, preventing even a small fraction of cases would provide immense benefit to society. While pathogenesis of AD is a complex interplay between genetic factors, immune dysregulation, and epidermal barrier dysfunction, studies thus far have largely focused on modifiable environmental factors such as probiotic supplementation during pregnancy and proactive emollient use [4].
This article summarizes recent literature on primary prevention strategies for AD and provides brief commentary on the proposed mechanism of action for each intervention. Our objective is to equip dermatologists and general practitioners with a broad understanding of the AD prevention landscape to guide patient and family counseling efforts.
Brief Background on AD Pathogenesis
The pathophysiology of AD involves epidermal barrier dysfunction, immune dysregulation, and microbial dysbiosis. The importance of the epidermal barrier is particularly evident in patients who have a filaggrin mutation. Filaggrin is a major structural component of the stratum corneum, and mutations in filaggrin have been associated with increased trans-epidermal water loss and the development of atopic dermatitis [5]. Therefore, early identification of infants with epidermal barrier dysfunction and addressing this deficiency prior to the development of AD represents one primary prevention strategy [6].
Another key feature of AD pathogenesis is alteration in immune pathways, particularly the skewed activation of the T-helper-cell-2 (Th2) signaling pathway. Research indicates that type 2 immune cytokines like IL-4 and IL-13 contribute to skin barrier dysfunction, suppression of antimicrobial peptides, and allergic inflammation [7]. The success of targeted blockade of IL-4 and IL-13 with dupilumab in treating moderate-to-severe AD underscores the critical role of these cytokines in AD pathogenesis [8]. Individuals may have a genetic predisposition towards dysregulated Th2 pathways or may experience immune dysregulation triggered by environmental factors such as allergens, microorganisms, and other irritants [7].
AD is also linked to microbial dysbiosis of both the skin and the gut. Exposure to antibiotics during pregnancy or delivery is associated with increased risk of AD in infants [9]. Patients with AD also exhibit increased Staphylococcus aureus and Staphylococcus epidermis on their skin, alongside decreased overall microbial diversity [10]. S. aureus colonization of the skin can upregulate proinflammatory cytokines and stimulate mast cell degranulation, which results in Th2 pathway activation and skin inflammation [11, 12]. Decreased microbial diversity is also observed in the gut microbiome of patients with AD, although its exact relationship with AD pathogenesis remains uncertain. Certain bacterial species, such as Bifidobacteria and Lactobacilli, play an important role in stimulating regulatory T-cells, which can mitigate systemic allergic responses [13]. Loss of these important bacterial species is thought to predispose children to allergic disease including AD [13]. Thus maintenance of a diverse skin and gut microbiome with prebiotic and probiotic supplementation is yet another strategy that has been considered in the primary prevention of AD.
Targeting Epidermal Barrier Disruption
Proactive Emollients
Emollients represent the mainstay of AD treatment regimens, and studies have investigated whether proactive application of emollients might prevent the development of AD in high-risk children [14]. Emollients are defined as topical substances without any active ingredients which are used to restore the skin barrier, decrease trans-epidermal water loss (TEWL), moisturize, and/or relieve pruritus and inflammation [14]. Skin barrier dysfunction represents a major driver of AD, and increased TEWL is seen early on in infants who go on to develop AD [15]. It therefore follows that efforts to strengthen the skin barrier could delay or prevent the development of AD [15, 16]. Additionally, AD pathogenesis is also driven by immune dysregulation, and emollient use has also been shown to alter the inflammatory immune response in AD patients [17].
Initial small pilot studies suggested potential benefits of daily emollient use in preventing AD in childhood [16, 18]. However, two large subsequent randomized control trials (RCTs) found no significant reduction in AD risk in those infants receiving daily emollients [19,20,21,22]. The 2020 Barrier Enhancement for Eczema Prevention (BEEP) trial investigated the efficacy of daily emollients in eczema prevention in 1,394 high-risk infants. The authors found that daily emollient use during the first 12 months of life failed to prevent the development of atopic dermatitis, food allergy, asthma or hay fever at two and five year follow ups [19, 20]. Interestingly, however, there was an increased number of skin infections in the emollient group during the first year of life (adjusted incidence rate ratio 1.55; 95% CI 1.15 – 2.09), which was hypothesized to occur as a result of increased exposure to pathogens or disturbance of the normal skin microbiome due to frequent emollient application [19]. Furthermore, a 2020 Swedish study with 2,397 infants also found that neither skin emollients (defined as bath additives and facial cream) nor early complementary feeding (peanut, cow's milk, wheat, and egg) significantly reduced the risk of AD [22]. Notably, the intervention compliance within their study was low, with full protocol adherence in only 27% of the emollient arm [22].
The evidence from smaller studies regarding the protective effects of specific emollients is mixed [23,24,25,26]. The STOP-AD trial, which randomized 321 high-risk full-term infants into either twice-daily application of AVEENO® Dermexa Fast & Long Lasting Balm for the first 8 weeks of life or to standard skin care, identified a significantly lower cumulative incidence of AD at 12 months in the emollient group, compared to the control group (Relative risk (RR) 0.707; 95% CI 0.516—0.965). Several meta-analyses have been conducted to try and provide clarity on these conflicting findings; however, meta-analysis on this topic is complicated by heterogeneity among smaller trials regarding their definitions of AD and AD risk, age at trial onset and treatment duration, type of emollient used, and emollient dosage and usage instructions [14, 27, 28]. Additionally, adherence to trial protocol is inconsistent, and many studies do not report adherence rates [28]. Risk of adverse events such as skin infections associated with prophylactic emollients is also not fully characterized. Overall, there is not enough evidence to recommend prophylactic emollient use in children with a family history of atopy, though more targeted studies that take advantage of personalized medicine to identify children with a genetic predisposition to epidermal barrier dysfunction and/or evidence of epidermal barrier dysfunction early in life have yet to be performed.
Targeting Microbiome Dysbiosis
Probiotic Supplementation
Probiotics are live microorganisms that can enhance barrier function, protect against pathogen colonization, and modulate immune system activity [29, 30]. In the context of AD, bolstering gastrointestinal microflora is believed to counteract the T-helper-2-skewed immune response characteristic of AD pathogenesis [31, 32]. It has also been proposed that probiotic supplementation lowers pro-inflammatory protein expression in children [33]. The composition of the gut microbiome in infants is influenced by maternal microbiota during pregnancy and dietary exposures after birth, along with other environmental and genetic factors [13, 32, 34].
In a seminal double-blinded RCT in 2001, Kalliomaki et al. demonstrated that supplementing both pregnant mothers and infants with Lactobacillus rhamnosus GG effectively prevented early atopic diseases, including AD, in high-risk children [31]. The study included 159 mother-infant pairs, and found that the frequency of AD in children given probiotics was one-half that of the placebo group at two years of age (23% vs 46%; RR 0.51, 95% CI 0.32–0.84).
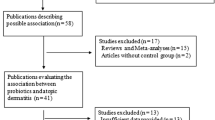
Many RCTs have subsequently been conducted to investigate the role of probiotic supplementation for pregnant mothers, lactating mothers, and infants with conflicting results, likely due to the significant heterogeneity in study designs such as microbial strain(s) type, timing of supplementation, and participant selection [8, 35,36,37,38,39]. In 2015, the World Allergy Organization-McMaster University Guidelines for Allergic Disease Prevention (GLAD-P): Probiotics guideline conditionally recommended prebiotic supplementation in not-exclusively breastfed infants, both at high and at low risk for developing allergy based on a very low quality evidence [40]. Further supporting this recommendation, a 2023 recent meta-analysis including 6131 subjects showed that probiotics were superior to placebo in AD prevention (RR 0.8, 95% CI 0.73–0.94) [41]. Clinical efficacy of probiotics was greater when administered to both infants and mothers and with mixed strain probiotics or Lactobacillus rhamnosus [41]. Probiotic supplementation has been found to be effective in reducing risk of AD in infants both with and without filaggrin gene mutations, suggesting that probiotic supplementation may also be beneficial to children at low risk of AD [42].
While perinatal probiotics show promise in AD prevention, it cannot be excluded that perinatal probiotics delay rather than prevent AD onset. Follow-up periods of studies ranged from 6 months to nine years, and no studies thus far have examined whether the length of follow-up was associated with the significance or magnitude of the AD risk reduction [38]. In one double-blinded RCT of 415 pregnant women who received either probiotic or placebo milk, probiotics significantly reduced the cumulative incidence of AD in their infants at two years of age, but not at six years of age [35]. This suggests that perinatal probiotics may delay rather than prevent AD onset in childhood. Long-term effects remain uncertain, as do potential risks. In one study, probiotic supplementation was linked to higher risk of infection and mucosal-associated illnesses in infants, although probiotics are generally considered safe in humans [43].
Of all the interventions studied, probiotic supplementation for pregnant and breastfeeding mothers, as well as for infants, has the most substantial evidence to reduce risk of AD development in children. However, additional studies are needed to evaluate long-term outcomes, determine the optimal probiotic supplementation regimen, and assess whether probiotic supplementation prevents not only mild AD but also moderate to severe AD.
Prebiotic Supplementation
Prebiotics are food components that selectively stimulate growth and activity of beneficial gut microorganisms by resisting digestion in the upper gastrointestinal tract and serving as a substrate for fermentation in the colon. Oligosaccharides are the most common form of ingested prebiotics and are ideal substrates for beneficial bacteria like Bifidobacteria [44, 45]. Consequently, prebiotic ingestion selectively nurtures beneficial bacterial and inhibits pathogenic bacteria proliferation. Analogous to probiotics, prebiotics are posited to prevent AD development by altering the infant gut microbiome [44]. Prebiotics supplementation has primarily been investigated in formula-fed infants, given the natural abundance of oligosaccharides in human breastmilk [45].
Studies evaluating the efficacy of prebiotic supplementation for infants in preventing AD development remain limited, with varied outcomes. Several early RCTs suggested a reduction in AD incidence among both high-risk and low-risk infants given prebiotics [46,47,48]. Notably, in a 2010 RCT involving 830 subjects, Gruber et al. showed that low-atopy-risk healthy term infants fed with formula supplemented with prebiotics had 44% lower prevalence of AD compared to the group fed with control formula [47]. However, in the subsequent 2018 Prebiotics in the Prevention of Atopy (PIPA) trial of 400 high-risk infants, prebiotics-supplemented formula failed to show a significant reduction in the cumulative incidence of AD compared to standard formula and breastfeeding [49]. Several other studies have also demonstrated no significant effect of prebiotics on AD risk reduction [50, 51]. A 2021 position paper by the European Academy of Allergy and Clinical Immunology (EAACI) concluded that current evidence does not support prebiotic supplementation in preventing eczema among high-risk infants [52].
Breastfeeding
Breastmilk naturally contains anti-inflammatory compounds that are thought to affect the infant gut microbiome, increase immune function, and decrease allergic sensitivity of infants [53]. The effectiveness of breastfeeding on AD prevention remains controversial. A cluster randomized controlled trial in Belarus found a reduction in the risk of AD in the groups with higher rates of breastfeeding at 12 months, but this association was not statistically significant at age 6.5 years [54, 55]. There have been no other subsequent randomized control trial comparing AD risk in breastfed and formula-fed infants. A 2019 meta-analysis of prospective observational studies found weak evidence for the protective effect of breastfeeding against AD in high-risk infants [56]. The protective effect of breastfeeding on AD remains uncertain.
Targeting the Immune System
Partially Hydrolyzed Formula
Partially hydrolyzed formula (pHF) contains oligopeptides with molecular weights generally less than 5 kD and have been suggested to prevent AD by modulating the immune system [57]. In 2019, the American Academy of Pediatrics concluded that there is a lack of evidence that either partially or extensively hydrolyzed formula prevents AD, even in high-risk children [58]. Despite this, interest in the role of pHF in AD prevention has persisted. The Allergy Reduction Trial (A.R.T) conducted in Europe recently did show that AD incidence within the first six months life was lower in high-risk infants receiving whey-based pHF compared to standard cow’s milk formula and exclusive breastmilk [59, 60]. However, the trial was notably funded by a formula company, which also supplied the infant formulas used in the study. Many RCTs on pHF exhibit high or unclear overall risk of bias and conflicts of interest [61]. Overall, current evidence does not support the efficacy of pHF in preventing AD.
Other Interventions
Maternal Diet and Nutrition
Maternal diet during pregnancy plays a crucial role in fetal development and genome expression, prompting investigation into the relationship between various dietary factors in pregnancy and AD development in offspring [62, 63]. While vitamin D and omega-3 supplements initially appeared to be the most promising based on observational studies and several small RCTs, recent meta-analyses found no significant effect of either supplement on offspring AD outcome [64, 65]. A 2022 RCT of 703 British pregnant women, which was not included in prior meta-analyses, did show a statistically significant reduction in AD risk at age 12 months among offspring of mothers supplemented with vitamin D (cholecalciferol 1000 IU daily) during pregnancy, although the effect was no longer significant at age 24 or 48 months [66]. There is additionally an ongoing trial evaluating vitamin D supplementation in the first year of life for prevention of atopic diseases.[67] Observational studies have suggested association between decreased risk of AD and maternal intake of other vitamins and minerals including beta-carotene, vitamin E, zinc, magnesium, and vitamin C,(62) but no RCTs have been performed to corroborate these findings.
Regarding overall maternal diet, increased intake of vegetables and yogurt was associated with decreased odds of AD diagnosis in offspring in the 2021 Healthy Start study involving 1253 pregnant women [68]. However, a 2024 cohort study of 1330 mother–child pairs found no association between maternal dietary index during pregnancy and offspring AD during the first year of life [69]. Overall, vitamin D supplementation is the only prenatal nutrient supplementation that may contribute to AD prevention in offspring.
Conclusions
In this review, we discussed the current evidence behind various interventions for the primary prevention of childhood AD. These interventions target the fundamental aspects of AD pathogenesis, including epidermal barrier dysfunction, microbiome dysbiosis, and immune dysregulation.
Based on available evidence, mixed-strain probiotic or Lactobacillus rhamnosus supplementation to a combination of pregnant mothers, breastfeeding mothers, and infants holds the greatest potential for preventing AD development in children [41, 70, 71] although further studies are needed to elucidate long-term outcomes and the effect of different probiotic regimens. While emollients are essential in the treatment of AD, recent large well-designed RCTs have shown that prophylactic emollient use is not effective in preventing AD in high-risk children [19,20,21,22]. Efficacy of breastfeeding on the prevention of AD remains uncertain, limited by the challenges of conducting a RCT [72]. Preliminary studies of prebiotic supplementation, pHF, and nutritional supplements for pregnant and lactating mothers suggest that these interventions are unlikely to be highly effective in the primary prevention of AD [52, 58, 59].
The primary prevention of AD is an incredibly exciting field that tests our understanding of AD pathogenesis. Environmental factors must play a role in the pathogenesis of AD as the concordance rate in twin studies is not 100% [73]. As such, primary prevention of AD should be possible with modification of environmental factors. However, as demonstrated in this review, additional studies are needed to (1) better characterize the environmental factors that contribute to the pathogenesis of AD, (2) determine the simplest and most cost-effective means of modifying these factors, and (3) identify those who would benefit most from the intervention.
Data Availability
No datasets were generated or analysed during the current study.
References
Tian J, Zhang D, Yang Y, Huang Y, Wang L, Yao X, et al. Global epidemiology of atopic dermatitis: a comprehensive systematic analysis and modelling study. Br J Dermatol. 2023;190(1):55–61.
Na CH, Chung J, Simpson EL. Quality of Life and Disease Impact of Atopic Dermatitis and Psoriasis on Children and Their Families. Children. 2019;6(12):133.
Chung J, Simpson EL. The socioeconomics of atopic dermatitis. Ann Allergy Asthma Immunol Off Publ Am Coll Allergy Asthma Immunol. 2019;122(4):360–6.
Chu DK, Koplin JJ, Ahmed T, Islam N, Chang CL, Lowe AJ. How to prevent Atopic Dermatitis (Eczema) in 2024: theory and evidence. J Allergy Clin Immunol Pract. 2024;S2213–2198(24):00434–43.
Flohr C, England K, Radulovic S, McLean WHI, Campbell LE, Barker J, et al. Filaggrin loss-of-function mutations are associated with early-onset eczema, eczema severity and transepidermal water loss at 3 months of age. Br J Dermatol. 2010;163(6):1333–6.
Berents TL, Lødrup Carlsen KC, Mowinckel P, Skjerven HO, Rolfsjord LB, Bradley M, et al. Transepidermal water loss in infancy associated with atopic eczema at 2 years of age: a population-based cohort study. Br J Dermatol. 2017;177(3):e35–7.
Kim J, Kim BE, Leung DYM. Pathophysiology of atopic dermatitis: Clinical implications. Allergy Asthma Proc. 2019;40(2):84–92.
Simpson EL, Paller AS, Siegfried EC, Boguniewicz M, Sher L, Gooderham MJ, et al. Efficacy and Safety of Dupilumab in Adolescents With Uncontrolled Moderate to Severe Atopic Dermatitis: A Phase 3 Randomized Clinical Trial. JAMA Dermatol. 2020;156(1):44–56.
Wan M, Yang X. Maternal exposure to antibiotics and risk of atopic dermatitis in childhood: a systematic review and meta-analysis. Front Pediatr [Internet]. 2023 May 15 [cited 2024 May 16];11. Available from: https://www.frontiersin.org/articles/10.3389/fped.2023.1142069.
Koh LF, Ong RY, Common JE. Skin microbiome of atopic dermatitis. Allergol Int Off J Jpn Soc Allergol. 2022;71(1):31–9.
Nakamura Y, Oscherwitz J, Cease KB, Chan SM, Muñoz-Planillo R, Hasegawa M, et al. Staphylococcus δ-toxin induces allergic skin disease by activating mast cells. Nature. 2013;503(7476):397–401.
Nakatsuji T, Chen TH, Two AM, Chun KA, Narala S, Geha RS, et al. Staphylococcus aureus Exploits Epidermal Barrier Defects in Atopic Dermatitis to Trigger Cytokine Expression. J Invest Dermatol. 2016;136(11):2192–200.
Pantazi AC, Mihai CM, Balasa AL, Chisnoiu T, Lupu A, Frecus CE, et al. Relationship between Gut Microbiota and Allergies in Children: A Literature Review. Nutrients. 2023;15(11):2529.
Grześk-Kaczyńska M, Petrus-Halicka J, Kaczyński S, Bartuzi Z, Ukleja-Sokołowska N. Should Emollients Be Recommended for the Prevention of Atopic Dermatitis?—New Evidence and Current State of Knowledge. J Clin Med. 2024;13(3):863.
Horimukai K, Morita K, Narita M, Kondo M, Kabashima S, Inoue E, et al. Transepidermal water loss measurement during infancy can predict the subsequent development of atopic dermatitis regardless of filaggrin mutations. Allergol Int Off J Jpn Soc Allergol. 2016;65(1):103–8.
Horimukai K, Morita K, Narita M, Kondo M, Kitazawa H, Nozaki M, et al. Application of moisturizer to neonates prevents development of atopic dermatitis. J Allergy Clin Immunol. 2014;134(4):824-830.e6.
Zhang J, Xu X, Wang X, Zhang L, Hu M, Le Y, et al. Topical emollient prevents the development of atopic dermatitis and atopic march in mice. Exp Dermatol. 2023;32(7):1007–15.
Simpson EL, Chalmers JR, Hanifin JM, Thomas KS, Cork MJ, McLean WHI, et al. Emollient enhancement of the skin barrier from birth offers effective atopic dermatitis prevention. J Allergy Clin Immunol. 2014;134(4):818–23.
Chalmers JR, Haines RH, Bradshaw LE, Montgomery AA, Thomas KS, Brown SJ, et al. Daily emollient during infancy for prevention of eczema: the BEEP randomised controlled trial. Lancet Lond Engl. 2020;395(10228):962–72.
Bradshaw LE, Wyatt LA, Brown SJ, Haines RH, Montgomery AA, Perkin MR, et al. Emollients for prevention of atopic dermatitis: 5-year findings from the BEEP randomized trial. Allergy. 2023;78(4):995–1006.
Perrett KP, Peters RL. Emollients for prevention of atopic dermatitis in infancy. The Lancet. 2020;395(10228):923–4.
Skjerven HO, Rehbinder EM, Vettukattil R, LeBlanc M, Granum B, Haugen G, et al. Skin emollient and early complementary feeding to prevent infant atopic dermatitis (PreventADALL): a factorial, multicentre, cluster-randomised trial. Lancet Lond Engl. 2020;395(10228):951–61.
Lowe AJ, Su JC, Allen KJ, Abramson MJ, Cranswick N, Robertson CF, et al. A randomized trial of a barrier lipid replacement strategy for the prevention of atopic dermatitis and allergic sensitization: the PEBBLES pilot study. Br J Dermatol. 2018;178(1):e19-21.
Ní Chaoimh C, Lad D, Nico C, Puppels GJ, Wong XFCC, Common JE, et al. Early initiation of short-term emollient use for the prevention of atopic dermatitis in high-risk infants—The STOP-AD randomised controlled trial. Allergy. 2023;78(4):984–94.
Harder I, Stölzl D, Sander N, Hartmann J, Rodriguez E, Mazur C, et al. Effects of Early Emollient Use in Children at High Risk of Atopic Dermatitis: A German Pilot Study. Acta Derm Venereol. 2023;103:adv5671.
Kottner J, Hillmann K, Fastner A, Conzade R, Heidingsfelder S, Neumann K, et al. Effectiveness of a standardized skin care regimen to prevent atopic dermatitis in infants at risk for atopy: a randomized, pragmatic, parallel-group study. J Eur Acad Dermatol Venereol JEADV. 2022;37(3):540–8.
Liang J, Hu F, Tang H, Jiang F, Sang Y, Hong Y, et al. Systematic review and network meta-analysis of different types of emollient for the prevention of atopic dermatitis in infants. J Eur Acad Dermatol Venereol JEADV. 2023;37(3):501–10.
Zhong Y, Samuel M, van Bever H, Tham EH. Emollients in infancy to prevent atopic dermatitis: A systematic review and meta-analysis. Allergy. 2022;77(6):1685–99.
Suez J, Zmora N, Segal E, Elinav E. The pros, cons, and many unknowns of probiotics. Nat Med. 2019;25(5):716–29.
Food and Agriculture Organization of the United Nations, World Health Organization, editors. Probiotics in food: health and nutritional properties and guidelines for evaluation. Rome: Food and Agriculture Organization of the United Nations : World Health Organization; 2006. 50 p. (FAO food and nutrition paper). https://www.ncbi.nlm.nih.gov/nlmcatalog/101617803.
Kalliomäki M, Salminen S, Arvilommi H, Kero P, Koskinen P, Isolauri E. Probiotics in primary prevention of atopic disease: a randomised placebo-controlled trial. The Lancet. 2001;357(9262):1076–9.
Fang Z, Li L, Zhang H, Zhao J, Lu W, Chen W. Gut Microbiota, Probiotics, and Their Interactions in Prevention and Treatment of Atopic Dermatitis: A Review. Front Immunol [Internet]. 2021 Jul 14 [cited 2024 Mar 27];12. Available from: https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.720393/full.
Zakiudin DP, Rø ADB, Videm V, Øien T, Simpson MR. Systemic inflammatory proteins in offspring following maternal probiotic supplementation for atopic dermatitis prevention. Clin Mol Allergy. 2023;21(1):5.
Anania C, Brindisi G, Martinelli I, Bonucci E, D’Orsi M, Ialongo S, et al. Probiotics Function in Preventing Atopic Dermatitis in Children. Int J Mol Sci. 2022;23(10):5409.
Dotterud CK, Storrø O, Johnsen R, Øien T. Probiotics in pregnant women to prevent allergic disease: a randomized, double-blind trial. Br J Dermatol. 2010;163(3):616–23.
Simpson MR, Dotterud CK, Storrø O, Johnsen R, Øien T. Perinatal probiotic supplementation in the prevention of allergy related disease: 6 year follow up of a randomised controlled trial. BMC Dermatol. 2015;1(15):13.
He J huan, Zhao X guo, Sun F, Peng W qi, Li H yun, Li H. Clinical study on prevention of atopic dermatitis by oral administration of probiotics in infants. Arch Med Sci [Internet]. 2020 Nov 5 [cited 2024 Mar 27]; Available from: https://www.archivesofmedicalscience.com/Clinical-study-on-prevention-of-atopic-dermatitis-by-oral-administration-of-probiotics,127658,0,2.html.
Li L, Han Z, Niu X, Zhang G, Jia Y, Zhang S, et al. Probiotic Supplementation for Prevention of Atopic Dermatitis in Infants and Children: A Systematic Review and Meta-analysis. Am J Clin Dermatol. 2019;20(3):367–77.
Husein-ElAhmed H, Steinhoff M. Meta-analysis on preventive and therapeutic effects of probiotic supplementation in infant atopic dermatitis. JDDG J Dtsch Dermatol Ges. 2023;21(8):833–43.
Fiocchi A, Pawankar R, Cuello-Garcia C, Ahn K, Al-Hammadi S, Agarwal A, et al. World Allergy Organization-McMaster University Guidelines for Allergic Disease Prevention (GLAD-P): Probiotics. World Allergy Organ J. 2015;8(1):4.
Wang F, Wu F, Chen H, Tang B. The effect of probiotics in the prevention of atopic dermatitis in children: a systematic review and meta-analysis. Transl Pediatr. 2023;12(4):73148–748.
Zakiudin DP, Thyssen JP, Zachariae C, Videm V, Øien T, Simpson MR. Filaggrin Mutation Status and Prevention of Atopic Dermatitis with Maternal Probiotic Supplementation. Acta Derm Venereol. 2024;24(104):24360.
Quin C, Estaki M, Vollman DM, Barnett JA, Gill SK, Gibson DL. Probiotic supplementation and associated infant gut microbiome and health: a cautionary retrospective clinical comparison. Sci Rep. 2018;29(8):8283.
Lee YH, Verma NK, Thanabalu T. Prebiotics in atopic dermatitis prevention and management. J Funct Foods. 2021;1(78): 104352.
Enam F, Mansell TJ. Prebiotics: tools to manipulate the gut microbiome and metabolome. J Ind Microbiol Biotechnol. 2019;46(9–10):1445–59.
Moro G, Arslanoglu S, Stahl B, Jelinek J, Wahn U, Boehm G. A mixture of prebiotic oligosaccharides reduces the incidence of atopic dermatitis during the first six months of age. Arch Dis Child. 2006;91(10):814–9.
Grüber C, van Stuijvenberg M, Mosca F, Moro G, Chirico G, Braegger CP, et al. Reduced occurrence of early atopic dermatitis because of immunoactive prebiotics among low-atopy-risk infants. J Allergy Clin Immunol. 2010;126(4):791–7.
Arslanoglu S, Moro GE, Schmitt J, Tandoi L, Rizzardi S, Boehm G. Early Dietary Intervention with a Mixture of Prebiotic Oligosaccharides Reduces the Incidence of Allergic Manifestations and Infections during the First Two Years of Life12. J Nutr. 2008;138(6):1091–5.
Ranucci G, Buccigrossi V, Borgia E, Piacentini D, Visentin F, Cantarutti L, et al. Galacto-Oligosaccharide/Polidextrose Enriched Formula Protects against Respiratory Infections in Infants at High Risk of Atopy: A Randomized Clinical Trial. Nutrients. 2018;10(3):286.
Boyle RJ, Tang MLK, Chiang WC, Chua MC, Ismail I, Nauta A, et al. Prebiotic-supplemented partially hydrolysed cow’s milk formula for the prevention of eczema in high-risk infants: a randomized controlled trial. Allergy. 2016;71(5):701–10.
Cuello-Garcia CA, Fiocchi A, Pawankar R, Yepes-Nuñez JJ, Morgano GP, Zhang Y, et al. World Allergy Organization-McMaster University Guidelines for Allergic Disease Prevention (GLAD-P): Prebiotics. World Allergy Organ J. 2016;9:10.
Venter C, Meyer RW, Greenhawt M, Pali-Schöll I, Nwaru B, Roduit C, et al. Role of dietary fiber in promoting immune health—An EAACI position paper. Allergy. 2022;77(11):3185–98.
Järvinen KM, Martin H, Oyoshi MK. Immunomodulatory Effects of Breast Milk on Food Allergy. Ann Allergy Asthma Immunol Off Publ Am Coll Allergy Asthma Immunol. 2019;123(2):133–43.
Kramer MS, Chalmers B, Hodnett ED, et al. Promotion of Breastfeeding Intervention Trial (PROBIT): a randomized trial in the Republic of Belarus. JAMA. 2001;285(4):413–20.
Kramer MS, Matush L, Vanilovich I, et al. Effect of prolonged and exclusive breast feeding on risk of allergy and asthma: cluster randomised trial. BMJ. 2007;335(7624):815.
Lin B, Dai R, Lu L, Fan X, Yu Y. Breastfeeding and Atopic Dermatitis Risk: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Dermatology. 2019;236(4):345–60.
Vandenplas Y, Meyer R, Chouraqui JP, Dupont C, Fiocchi A, Salvatore S, et al. The role of milk feeds and other dietary supplementary interventions in preventing allergic disease in infants: Fact or fiction? Clin Nutr. 2021;40(2):358–71.
Greer FR, Sicherer SH, Burks AW, Abrams SA, COMMITTEE ON NUTRITION, SECTION ON ALLERGY AND IMMUNOLOGY, et al. The Effects of Early Nutritional Interventions on the Development of Atopic Disease in Infants and Children: The Role of Maternal Dietary Restriction, Breastfeeding, Hydrolyzed Formulas, and Timing of Introduction of Allergenic Complementary Foods. Pediatrics. 2019;143(4):e20190281.
Nicolaou N, Pancheva R, Karaglani E, Sekkidou M, Marinova-Achkar M, Popova S, Tzaki M, Kapetanaki A, Iacovidou N, Boutsikou T, Iliodromiti Z, Papaevangelou V, Sardeli O, Xepapadaki P, Papathoma E, Thijs-Verhoeven I, Kudla U, Ulfman LH, Schaafsma A, Manios Y. The Risk Reduction Effect of a Nutritional Intervention With a Partially Hydrolyzed Whey-Based Formula on Cow's Milk Protein Allergy and Atopic Dermatitis in High-Risk Infants Within the First 6 Months of Life: The Allergy Reduction Trial (A.R.T.), a Multicenter Double-Blinded Randomized Controlled Study. Front Nutr. 2022;9:863599. https://doi.org/10.3389/fnut.2022.863599.
Boutsikou T, Sekkidou M, Karaglani E, Krepi A, Moschonis G, Nicolaou N, et al. The Impact of Infant Feeding Regimen on Cow’s Milk Protein Allergy, Atopic Dermatitis and Growth in High-Risk Infants during the First 6 Months of Life: The Allergy Reduction Trial. Nutrients. 2023;15(11):2622.
Greer FR, Sicherer SH, Burks AW, American Academy of Pediatrics Committee on Nutrition, American Academy of Pediatrics Section on Allergy and Immunology. Effects of early nutritional interventions on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, timing of introduction of complementary foods, and hydrolyzed formulas. Pediatrics. 2008;121(1):183–91.
Venter C, Agostoni C, Arshad SH, Ben-Abdallah M, Du Toit G, Fleischer DM, et al. Dietary factors during pregnancy and atopic outcomes in childhood: A systematic review from the European Academy of Allergy and Clinical Immunology. Pediatr Allergy Immunol. 2020;31(8):889–912.
Kang CM, Chiang BL, Wang LC. Maternal Nutritional Status and Development of Atopic Dermatitis in Their Offspring. Clin Rev Allergy Immunol. 2021;61(2):128–55.
Jia Y, Huang Y, Wang H, Jiang H. Effect of Prenatal Omega-3 Polyunsaturated Fatty Acid Supplementation on Childhood Eczema: A Systematic Review and Meta-Analysis. Int Arch Allergy Immunol. 2023;184(1):21–32.
Zeng R, Li Y, Shen S, Qiu X, Chang CL, Koplin JJ, et al. Is antenatal or early-life vitamin D associated with eczema or food allergy in childhood? A systematic review. Clin Exp Allergy. 2023;53(5):511–25.
El-Heis S, D’Angelo S, Curtis EM, Healy E, Moon RJ, Crozier SR, et al. Maternal antenatal vitamin D supplementation and offspring risk of atopic eczema in the first 4 years of life: evidence from a randomized controlled trial. Br J Dermatol. 2022;187(5):659–66.
Murdoch Childrens Research Institute. Can Vitamin D Supplementation Prevent Food Allergy in Infants? The VITALITY Trial [Internet]. clinicaltrials.gov; 2023 Nov [cited 2023 Dec 31]. Report No.: NCT02112734. Available from: https://clinicaltrials.gov/study/NCT02112734.
Venter C, Palumbo MP, Glueck DH, Sauder KA, O’Mahony L, Fleischer DM, et al. The maternal diet index in pregnancy is associated with offspring allergic diseases: the Healthy Start study. Allergy. 2022;77(1):162–72.
Sivula E, Puharinen H, Hantunen S, Keski-Nisula L, Backman K. Maternal dietary indexes are not linked to early childhood wheezing or atopic eczema. Pediatr Allergy Immunol. 2024;35(3): e14099.
Amalia N, Orchard D, Francis KL, King E. Systematic review and meta-analysis on the use of probiotic supplementation in pregnant mother, breastfeeding mother and infant for the prevention of atopic dermatitis in children. Australas J Dermatol. 2020;61(2):e158–73.
Jiang W, Ni B, Liu Z, Liu X, Xie W, Wu IXY, et al. The Role of Probiotics in the Prevention and Treatment of Atopic Dermatitis in Children: An Updated Systematic Review and Meta-Analysis of Randomized Controlled Trials. Pediatr Drugs. 2020;22(5):535–49.
Güngör D, Nadaud P, LaPergola CC, et al. Infant milk-feeding practices and food allergies, allergic rhinitis, atopic dermatitis, and asthma throughout the life span: a systematic review. Am J Clin Nutr. 2019;109(Suppl 1):772S-799S.
Larsen FS. Atopic dermatitis: A genetic-epidemiologic study in a population-based twin sample. J Am Acad Dermatol. 1993;28(5, Part 1):719–23.
Acknowledgements
We would like to thank Dr. Lynda Schneider for her contributions through insightful brainstorming sessions on the topic of atopic dermatitis prevention.
Author information
Authors and Affiliations
Contributions
E.K., M.S., and T.H. contributed to the brainstorming and outlining of the manuscript, E.K and M.S. wrote the main manuscript text, and T.H. provided detailed manuscript edits. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, E.J., Sandler, M. & Ho, T. Prevention of Atopic Dermatitis in Children: Can It be Done?. Curr Derm Rep (2024). https://doi.org/10.1007/s13671-024-00448-6
Accepted:
Published:
DOI: https://doi.org/10.1007/s13671-024-00448-6