Abstract
Purpose of Review
This comprehensive review covers the advantage and limitations of some dressing materials and the current knowledge on wound dressings and emerging technologies to achieve proper wound healing.
Recent Findings
Traditional and modern dressings are helpful in the wound healing process; however, they cannot substitute lost tissue. Human skin equivalents have been developed conceptually to fill this void as they do not only facilitate wound healing but also may replace lost tissue. Several studies have shown that the addition of mesenchymal stem cells, such as in human placenta, has promising results in wound healing.
Summary
A wound is defined as a disruption in the continuity of the skin or mucosa due to physical or thermal damage, or an underlying medical condition. Wound healing is a complex, dynamic, and multistep process which occurs after skin damage leading to tissue repair. Although the skin normally undergoes repair after a disruption, the healing process can be affected in different conditions such as diabetes mellitus, infections, venous/arterial insufficiency, among others. To enhance healing, a wide range of wound dressings are available; however, a thorough wound assessment (e.g., wound type, size, depth, or color) is required to choose the appropriate dressing. The emergence of new dressings has brought a new perspective of wound healing, but there is no superior product yet to treat acute and/or chronic wounds. Therefore, wound dressing research studies need to be carried out in order to help improve wound healing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
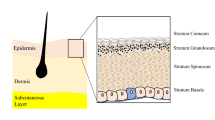
A wound can be defined as a defect or disruption in the continuity of the epidermis of the skin or mucosa as a result of physical or thermal damage or the presence of an underlying medical disorder [1]. Depending on the duration and nature of the healing process, wounds are classified as acute or chronic wounds. An acute wound is a damage to the skin that frequently heals completely within a predictable time range, depending on the wound depth, size, and the magnitude of the damage [2•, 3]. The primary causes of acute wounds include mechanical injuries (abrasions, tears, penetrating injuries, or surgical wounds), radiation, electricity, corrosive chemicals, or thermal sources. On the other hand, a chronic wound results when skin injuries do not heal in a timely manner and may be at risk to recur [1, 2•]. These wounds fail to heal because of persistent wound pathology, vascular disease, repetitive trauma or prolonged pressure, coincident wound complications such as infection or ischemia, or concurrent medical condition [4], for instance, diabetes mellitus, venous insufficiency, or the presence of a malignancy [1]. A variety of causes for chronic wounds exist with the most common being pressure ulcers, venous ulcers, and diabetic foot ulcers [1, 2•]. Wounds are also categorized depending on the amount of skin layers affected. Very superficial wounds encompass those injuries affecting the epidermal surface only are termed erosions, while deeper injuries are termed ulcers. Ulcers that involve both the epidermis and part of dermal layers but retain adnexal structures (i.e., hair follicles, blood vessels, sweat glands) are called partial-thickness wounds. Should deeper structures including the entire dermis or deeper be involved, it is called a full-thickness wound [1].
Wound healing is a complex, dynamic, and multistep process that occurs after damage leading to tissue repair, most commonly for ulcers and regeneration for erosions. The wound healing process is typically characterized as four successive and overlapping phases [2•]: (i) coagulation and hemostasis (0 h after injury) targeting for the bleeding control and limiting the spread of microorganisms within the body; (ii) inflammation (1–3 days), which occurs concurrently with hemostasis, and release of pro-inflammatory cytokines and swelling take place; (iii) proliferation (4–21 days) in which fibroblasts migrate to injured area, resulting in capillary growth, collagen synthesis, and new tissue formation; and eventually migration of epithelial cells (iv) remodeling (21 days–1 year) where this new tissue is constantly remodeled which will determine the nature of the final scar [5]. Disruption of any of these steps may lead to impaired healing such as excessive scarring or chronic ulcers.
Although the skin typically undergoes repair (wound healing) after an injury, this ability can be altered in certain conditions such as infections, immobility, poor blood supply, medications, diabetes mellitus, inappropriate hydration and nutrition, trauma, and vast skin loss [6, 7, 8•]. To optimize healing, a variety of wound healing dressing materials are available; however, the choice of a material for a specific wound type is important for proper healing. Additionally, dressings need to be in contact with the wound in order to work, unlike wounds bandages that are designed to keep wound dressings in the wound place. For acute wounds, one important role of the dressing is to maintain wound exposure to pro-healing cytokines and growth factors, which are less readily available when the wound is uncovered [2•]. Dressings also prevent trauma, allow matrix materials to remain in contact with the wound, reduce wound infection, and optimize the electrical gradient of the wound. The ideal wound dressing is characterized by the capacity to keep a moist environment and prevent wound desiccation while absorbing wound drainage and preventing maceration, increase epidermal migration, allow gas exchange, stimulate angiogenesis and connective tissue production, give protection against bacterial infection, keep adequate tissue temperature enhancing blood flow, maintain electrical gradient, be non-adherent leading to an easy removal and debriding action, and be sterile, non-allergic, and non-toxic [2•]. In this comprehensive review, we summarize the current knowledge on wound healing dressings, and their function on healing process.
Wound Examination
Thorough wound assessment will determine the type of wound dressing to use. This wound evaluation includes wound type, size, depth, color, shape, exudate level, and location [8•]. Cost-effectiveness, easiness of use, and patient satisfaction also need to be considered at the moment of choosing the appropriate wound dressing. Additionally, the type of dressing to use may depend on the phase the wound healing is going through [1].
The wound color can indicate the process is occurring inside the wound, from the presence of granulation tissue in a red-colored wound to the existence of necrotic tissue in those black-colored [8•] (Table 1).
As mentioned before, a wound may be superficial, partial thickness, or full thickness, even with a deep cavity. The depth and some characteristics of a wound may be based on the underlying disorder. For instance, arterial ulcers are often deep and have a “punched out” appearance with scarce exudate; venous ulcers are generally more superficial and can be highly exudative. In wounds with undermined edges or cavities, careful dressing removal needs to be taken with prevention of left-over dressing in the cavity. Location is another factor that can influence the selection of a specific dressing. Pilonidal sinus breakdown, local skin deep surgeries, or perianal wounds need cavity dressings to stimulate healing [1, 8•].
Exudate is a fluid that filters from the bloodstream into wounds or areas of inflammation. It is composed of serum, fibrin, and leukocytes. Most wounds contain some exudate from small amount to copious amounts. The selection of primary or secondary dressing will depend on the exudate amount. For example, infected wounds or venous ulcers often have large amounts of exudate and the appropriate dressing needs to be chosen to absorb this drainage and avoid the damage of adjacent skin due to proteases often contained in the exudate.
Wound Dressings
Wound treatment has passed through several changes over time to time. Materials collected from nature have been used such as leaves, honey, spider webs, tree bark, vinegar, beer, and wine. Around 1600 BC, linen strips soaked in oil enclosed with plasters were used as wound dressings. In 400 BC, Hippocrates used wine or vinegar with honey for wound cleansing. They also used water/wine-boiled wool as bandages [2•, 9]. As research and understanding evolved, during the nineteenth century, there was an important advancement in antiseptic methods and antibiotics, and later in the twentieth century, modern wound dressing was developed [10]. Currently, we are better able to support the skin not only by covering the wound but also by accelerating the wound healing process via wound dressings.
Traditional Wound Dressing
Traditional wound dressing products include gauze, lint, plasters, natural, or synthetic bandages and cotton wool, which are dry and used as primary or secondary dressings [1, 2•]. Gauze dressings are made of woven and non-woven fibers of cotton, rayon, and polyester [11]. Inexpensive and readily available, they may be appropriate for a number of wounds, to help with wound drainage, but as dressings dry, they become adherent to the wound leading to traumatic and painful removal [2•, 11]. Affording some protection from the outside world and against bacterial infection, this is imperfect compared to more modern dressings [11]. Gauze dressings need to be changed frequently to prevent maceration of healthy adjacent tissue and may increase cost and cause repetitive tissue damage [1]. Impregnated gauze with soft paraffin, zinc, iodine, or petrolatum help avoid desiccation and offer a non-adherent coverage [1, 2•, 11]. Bandages are often used in concert with dressings. The different functions that bandages can perform will depend on what they are made of, either of cotton wool and cellulose (natural) or polyamide (synthetic) [2•, 11]. All cotton, cellulose, and polyamide bandages can be used for retention of light dressings. While elastic high compression bandages are used for sustained compression in venous insufficiency, short stretch (less than 50 % stretch, also known as inelastic compression bandages) are used for venous leg ulcers (VLUs) and lymphedema [11]. Traditional dressings have been mostly replaced by modern dressings to allow for maintaining a moist environment for healing [1].
Modern Wound Dressing
Modern dressings significantly differ from traditional in keeping and creating a moist environment around the wound facilitating wound healing [1]. They are based on synthetic polymers and are primarily categorized as hydrocolloids, alginates and hydrogels, films, and foams [1, 2•].
Hydrocolloid Dressings
Hydrocolloid dressings are historically one of the most widely used and best studied dressings. They have two layers, inner colloidal layer and outer water-impermeable layer. They are composed of gel forming materials (carboxymethylcellulose, gelatin, and pectin) and other agents such as elastomers and adhesives [1, 2•]. When the dressing is in contact with the wound exudate, hydrocolloids entrap liquid and form a covering gel. Having some absorbing properties, they are permeable to water but less permeable to bacteria [2•, 12]. The moist environment created under the dressing stimulates wound healing by increasing collagen synthesis and fibroblast proliferation and rapid epithelialization [12]. Hydrocolloid dressings are used for mild to moderate exuding wounds such as pressure sores, minor burn wounds, and traumatic wounds. Through their occlusive properties, these dressings provide an excellent environment for autolytic debridement as retained proteases released by the wound help remove necrotic or non-viable tissue. They may also be used for leg ulcers under compression therapy [13] and for pediatric wound care management since they do not cause pain on removal [1]. Granuflex™ (ConvaTec, Princeton, NJ), Comfeel™ (Coloplast Ltd, UK), DuoDerm® (ConvaTec, Princeton, NJ), and Tegasorb™ (3M Health Care, Saint Paul, MN) are some examples of hydrocolloid dressings available in thin films or sheets. Besides the advantages mentioned before, they also adhere to both moist and dry sites; nevertheless, a disadvantage of these dressings is that they are not indicated for neuropathic ulcers or highly exuding wounds [1, 2•]. Importantly, they are changed only when drainage or leakage occurs to prevent wound trauma with removal.
Hydrogel Dressings
Hydrogel is an insoluble material with water dispersion medium (70–90 % of water content) made from synthetic polymers (methacrylates and polyvinyl pyrrolidine) [2•, 14]. These polymeric components are cross-linked in order to entrap water [1]. In addition to its high water content which keeps granulation tissue and epithelium in a moist environment, its rubbery texture and low interfacial tension contribute to a great biocompatibility, non-irritant nature and minimize inflammatory reactions in the adjacent areas [2•, 14, 15]. The hydrogel dressings also have soft elastic properties which contribute to an easy application and removal after wound is healed without any discomfort. These dressings also decrease the temperature of cutaneous wounds, giving a cooling effect and leading to pain reduction. Hydrogels can be applied either as an amorphous gel or as elastic sheet or film. Hydrogels may need a secondary covering and frequent changing. Hydrogels do not need secondary dressing but rather a bandage to keep the dressing in place and can be trimmed to fit around the wound due to their flexibility [1]. They are used for necrotic wounds, pressure ulcers, burn wounds, and dry chronic wounds [2•]. Due to its significant water content, they have limited absorptive capacity; therefore, they are also used for mild exudating wounds. In more highly exudative wounds, maceration and bacterial proliferation may lead to foul smelling wounds. Some examples of hydrogel dressings include Nu-gel™ (Johnson and Johnson, New Brunswick, NJ), Intrasite™ (Smith and Nephew, London, UK), Aquaform™ (Maersk Medical, Suffolk, UK) polymers, and sheet dressings.
Alginate Dressings
Alginate, a natural herbal polysaccharide derived from seaweed, is composed of linear chains of two uronic acids—mannuronic and guluronic acid—that interact with calcium to form calcium alginate [2•, 16, 17]. It is characterized by good water-absorbing quality, biodegradability, biocompatibility [17, 18]. This absorption capability is due to its great hydrophilic gel formation upon contact with wound exudate, reducing fluid accumulation and bacterial contamination. In contact with wounds, calcium ions from the alginate fiber are exchanged with sodium ions in exudate, leading to a protective gel formation [8•]. Thus, the wound is kept at an ideal moist environment and temperature [1]. The gel forming feature is due to the presence of divalent cations, typically calcium ions acting as cross-linking agents [1, 19]. This cross-linking ability of calcium ions with alginic acid polymer makes calcium alginate dressings ideal for tissue engineering scaffolding [20]. These dressings also have a clotting mechanism and can be hemostatic due to the presence of calcium ions during the first stage of wound healing [21–23]. They can be easily rinsed away with irrigation without compromising newly formed granulation tissue, when removed. Some studies have reported the inhibition of keratinocyte migration by alginate; however, Thomas et al. [24] reported that the healing process is hastened by alginate via the activation of macrophages to produce TNF-α, a pro-inflammatory component which may initiate a resolving inflammation characteristic of healing wounds. Other studies demonstrated that calcium alginate increases the proliferation of fibroblast but decreases their motility [25, 26]. Additionally, Wang et al. [17] found that calcium alginate enhances wound healing via the upregulation of collagens I/III ratio. Alginate dressings can be used for wounds with moderate to high exudate production, but not recommended for dry wounds, wounds with exposed bone, third-degree burn wounds, and wounds with eschar [1]. Also, these dressings require secondary dressings since it could dehydrate the wound, delaying healing [2•]. Alginate dressings present either as freeze-dried porous sheets (foams) or as flexible fibers. Kaltostat™ (ConvaTec, Princeton, NJ), rich in guluronic acid, forms gels in contact with wound exudate while Maxsorb® (Medline Industries, Mundelein, IL), which is rich in carboxymethylcellulose, creates a soft flexible gel with hydration. Tegagen™ (3M Health Care, Saint Paul, MN) and Comfeel Plus™ (Coloplast Ltd, UK) are other alginate dressings available, the latter being a hydrocolloid/alginate combination dressing [1, 2•].
Semi-permeable Film Dressings
These film dressings are made of adhesive, porous, thin transparent polyurethane, which are permeable to O2, CO2, and water vapor from the wound; it also has autolytic debridement properties and impermeable to liquid and bacteria [1, 2•, 8•]. These dressings are very flexible and elastic, conforming to any shape without any additional taping [1, 2•]. Wound closure inspection is feasible without dressing removal due to transparent films. Because these films are non-absorbent, they are not appropriate for exuding wounds. Therefore, these dressings are suitable for epithelializing wounds and superficial wounds with low exudates. These films can also work as secondary dressings to waterproof primary dressings. Inappropriate dressing removal may produce damage to surrounding tissues [8•]. Opsite™ (Smith and Nephew, Hull, UK), Biooclusive™ (Johnson and Johnson, New Brunswick, NJ), and Tegaderm™ (3M Health Care, Saint Paul, MN) are some commercially available film dressings, which vary in their conformability, elasticity, vapor permeability, and adhesive properties [2•].
Semi-permeable Foam Dressings
Foam dressings consist of porous polyurethane foam that is hydrophilic and hydrophobic with or without adhesive borders [8•, 27]. The exterior layer is impermeable to liquid because of its hydrophobic properties but permits O2, CO2, and water vapor exchange due to its open pore structure [1]. Foam dressings are highly absorbent (depending on foam’s texture, thickness, and pore size), cushioning, and protective; they also provide good thermal insulation, keep a moist environment, and conform well to body surfaces [1, 8•]. Vermeulen et al. reported in a systemic review that foam dressings are preferable in terms of reducing pain, patient satisfaction, and nursing time in comparison to gauze on postoperative wounds healing by secondary intention [28•]. Foams are available as sheets or cavity filling shapes, and they also are available with charcoal impregnation for foul smell-wounds. Foam dressings are changed when exudate exceeds dressing capacity [8•]. They are recommended for lower leg ulcers, granulating wounds, and moderate to greatly exuding wounds. They are usually used as primary dressings for exudate absorption, and secondary dressings are not necessary because of their high liquid absorption and permeability to water vapor. Examples of foam dressings include Allevyn™ (Smith and Nephew, Hull, UK), Lyofoam™ (Conva Tec, Princeton, NJ), and Tielle™ (Johnson and Johnson, New Brunswick, NJ) [2•]. They can also be used for deep cavity wounds refractive to treatment [29]. Foam dressings are not recommended for dry epithelializing wounds, low exuding wounds, and dry scars [1, 2•, 8•].
Bioactive Wound Dressing
These dressings are made of biomaterials involved in the wound healing process. They are characterized by their biocompatibility, non-toxic property, and biodegradability and are also derived from natural or artificial sources [1, 2•], for example, collagen [30, 31], hyaluronic acid [32–34], chitosan [35–37], alginate, and elastin. These polymers can be used alone or in combination depending upon the type of wound [2•, 38–40]. In some cases, these dressings may be combined with growth factors and antimicrobials [1].
Collagen is the most abundant protein in the extracellular matrix (ECM). Scaffolds made up of collagen show low antigenicity, good biocompatibility, and excellent biodegradability [38]. Collagen participates in normal wound healing processes, including fibroblast formation, acceleration of endothelial migration, induction of clotting, and formation of the final scar [1, 41]. They can also be impregnated with antibiotic drugs, working as a reservoir for drug delivery [42].
Hyaluronic acid (HA) is a glycosaminoglycan constituent of the ECM that is also biodegradable, biocompatible, and has weak antigenicity [1, 2•]. Cross-linked HA has also been used as a drug delivery system, biopolymer for structural support, and stem cell delivery in bone regeneration [1, 43•, 44]. Studies have found that the HA degradation by-products can help in epithelial proliferation and migration and that HA degradation enzymes can accelerate cell proliferation. These findings suggest that HA should be broken down in order to stimulate epithelial growth [43•, 45, 46]. The molecular weight of HA may affect repair as medium molecular weight HA (MMW-HA, between 100 and 300 kDa) enhances wound repair [47].
Chitosan is a linear copolymer obtained from crustacean’s exoskeletons such as shrimp and crab [43•]. Chitosan shows also features such as biodegradability, biocompatibility, and antimicrobial activity against bacteria and fungi [43•, 48]. Chitosan stimulates granulation tissue formation during the proliferative stage of wound healing [49]. It also has haemostatic and anesthetic effect, making it attracting in the wound dressing area [48]. They have been used as delivery system as well; for instance, Moursa et al. used chitosan to deliver neurotensin, a neuropeptide that works as inflammatory modulator, for diabetic foot ulcer (DFU) [50]. Wound dressings based on chitosan-collagen complex applied to thermal skin burn have been reported showing an increased healing rate via the acceleration of the formation of granulation and fibrous tissue [51].
Bioactive dressings have been reported to be better than synthetic and conventional dressings such as hydrogel and gauze, respectively, but are typically more expensive [1].
Cell and Tissue-Based Products
Even though traditional and modern dressings are helpful in the wound healing process, they cannot substitute lost tissue, for instance missing dermis in severe burns. Human skin equivalents (HSE) have been developed conceptually to fill this void as they do not only facilitate wound healing but also may replace lost tissue, at least transiently [1]. HSE secretes and promotes wound growth factors and cytokines embedded in the dressings resulting in epithelialization. There are three types of HSE available: the first contains cell such as keratinocytes (patient’s or recombinant sources), and/or fibroblasts often within in a collagen matrix; the second has a decellularized dermal structure, also known as acellular matrix [2•]. The third type of HSE is made of human placenta that works as a dermal substitute for re-formation of full-thickness wounds and has a highly rich reservoir of ECM [52]. These scaffold dressings, when introduced into the body, are progressively degraded, leaving behind a matrix of connective tissue with the suitable architectural and mechanical properties [1]. Bioengineered dressings are recommended for DFUs, VLUs, and other chronic wounds.
The cellular constructs take advantage of the keratinocytes and/or fibroblasts which provide signaling molecules, growth factors, and ECM proteins that help in healing. Commercially available therapies comprise those that contain keratinocytes as in EpiCel™ (Genzyme Biosurgery, Cambridge, MA), fibroblasts (e.g., Dermagraft®, Advanced Tissue Sciences, La Jolla, CA), or both keratinocytes and fibroblasts (e.g., Apligraf®, Organogenesis, Canton, MA) [53]. Stratagraft™ (StrataGraft Corp, Madison, WI) is a product under development and contains immortalized neonatal keratinocytes to generate a fully stratified epidermis above a dermal component. It has a barrier function and is pathogen-free. It is being studied for burn patients and functions as a bridge before autologous cells migrate into the wound [54]. To date, Stratagraft™ has been shown to be well tolerated and not immunogenic [55]. Many patients have also been treated with cultured epidermal autografts for ulcers and burns such as EpiCel™. It is used in dermal or full-thickness burns spreading more than 30 % of the body surface [54]. EpiCel™ is usually used in combination with dermal substitutes, since dermal layer takes long time to develop [54, 56]. Dermagraft® is derived from fibroblast cells from neonatal foreskin, which are seeded over a polygalactin mesh scaffold. Once placed on the wound, the fibroblast and ECM secrete cytokines and growth factors stimulating autologous tissue repair. This dermal substitute is recommended for neuropathic DFUs [54]. Marston et al. showed that Dermagraft® is an effective and safe for chronic DFUs [57], but it should be accompanied by debridement and pressure offloading in chronic wound treatment [54]. Apligraf® is a composite allograft that is similar to a full-thickness human skin without vasculature, appendages, and rete ridges. It contains a layer of bovine collagen type I scaffold with neonatal fibroblasts in the dermis and overlying layer of stratified neonatal keratinocytes as epidermis [54]. It should be applied covering the whole wound bed and secured with sutures, adhesives, or conforming dressings (Fig. 1). Apligraf® has been shown to be effective for DFUs lasting more than 3 weeks [58] and to accelerate complete closure of hard-to-heal VLUs [59]. A recent study reported that this bilayered living cellular construct reduced the time for wound closure in comparison to porcine small intestine submucosa wound dressing [60]. It can also be used in epidermolysis bullosa [61], split-thickness graft donor sites, and surgical wounds [54, 62].
Apligraf® application. a Apligraf® is provided as a circular disc with 75 mm in diameter and 0.75 mm thick inside of a plastic tray. It is supplied with the epidermal layer (matte surface) facing up and dermal layer (shiny, not seen) facing down on a polycarbonate membrane. b VLU is located on the right medial ankle. Wound bed must be prepared before Apligraf® placement. Thus, removal of all devitalized tissue (i.e., necrotic tissue and fibrinous exudate) and hemostasis should be achieved. c Post-application of Appligraf®. Dermal layer should be in direct contact to the wound bed. Any visible air pockets are removed
There are varieties of different kinds of acellular matrix. One of them is acellular allograft which consists of cryopreserved human cadaverous dermis, in which the donor cells and antigenic material have been removed decreasing the antigenic response. The remaining dermis functions as a scaffold for growth of host fibroblast and vascularity. They are recommended for chronic ulcers such as DFU [54]. Some disadvantages of these products include possible disease transmission [63], poor barrier function, and short shelf life [54, 58]. Graftjacket® (Wright Medical Technology, Inc, Arlington, TN), a type of acellular allograft, showed statistically significant higher percentage of DFU wound closure when accompanied with sharp debridement in comparison with debridement only [64]. Other acellular construct includes synthetic bilayers which contain a porous collagen matrix with other ECM components. It also has a layer of silicone that works as epidermis, protecting the wound from fluid loss and infections [54, 58]. They are generally used for partial-thickness wounds, full-thickness wounds, chronic ulcers, and burns [58]. Integra™ (Integra LifeScience, Plainsborough, NJ) is a type of synthetic bilayer made of synthetic collagen, chondroitin 6 sulfate, and hyaluronic acid matrix with or without a thin silicone sheet on top. Benefits of Integra include minimal discomfort, capacity to cover lesions without sacrificing other tissues, and may prevent scarring [65]; however, it also has some drawbacks such as failure rate of 25 % [65, 66] and the requirement of a replacement of the superficial silicone layer, when present, with autografts after 3 to 4 weeks. Several studies reported that combined use of negative pressure wound therapy and Integra accelerates wound healing and the time between the first dermal regeneration template and following skin grafting [65, 67].
Xenografts incorporate exogenous collagen in the wound, helping dermal regeneration. This collagen stimulates macrophages and fibroblasts chemotaxis and supplies a scaffold for tissue growth as well [54]. In general, less well-studied, xenografts can be used for partial-thickness wounds, full-thickness wounds (e.g., chronic ulcers and traumatic injuries) and acute burns. As the wound heals, xenografts are absorbed which makes them ideal wound healing by secondary intention. Some studies have shown xenografts decrease pain maybe due to the coverage of vital structures during secondary intention healing [54, 68]. Commercially available therapies include Permacol (Tissue Science Laboratories, Covington, GA), made of porcine dermis; Matriderm (Suwelack Skin and Health Care Ag, Billerbeck, Germany) that contains bovine collagen covered with elastin; and best studied Oasis® (Smith and Nephew, Fort Worth, Texas) (Fig. 2) that consists of porcine intestinal submucosa [54, 58]. Romanelli et al. found that Oasis® was more beneficial than moist wound dressings for the treatment of mixed arterial/venous ulcers [69]. Oasis® also showed significant healing improvement in chronic VLUs as adjunct therapy over compression therapy only [70•].
OASIS® application. a OASIS® is available in variable sizes. Wound measures should be taken in order to select the proper xenograft size. As it is an acellular matrix, it does not have neither a top nor bottom surface. b Trauma wound on the left anterior leg after appropriate debridement before OASIS® placement. c Post-application of OASIS®. It should be positioned covering the entire wound surface beyond borders. The graft is anchored with adhesives to avoid sliding. Once OASIS® is fixed in place, it can gently be rehydrated with sterile saline
Talymed® (Marine Polymer Technologies, Inc, Danvers, MA) is a matrix composed of shortened nanofibers of poly-N-acetyl glucosamine (sNAG) isolated from a microalgae diatom, which is currently used as a hemostatic agent [71, 72]. Recent findings show treatment of cutaneous wounds with sNAG results in the increased wound healing rate due to augmented angiogenesis, cell proliferation, and migration [73, 74]. sNAG also stimulates the endothelial cells which leads to an increased expression of various cytokines including IL-1 and vascular endothelial growth factor which are vital for wound healing. A recent study found Talymed fibers (sNAG) activate expression of defensin peptides showing antimicrobial properties [72]. A randomized control trial (RCT) demonstrated that sNAG was effective in the treatment of patients with VLUs with no significant adverse effects [75].
All the aforementioned HSE have been promising for chronic wound healing because they have bioagents necessary for wound healing; however, they lack mesenchymal stem cells (MSCs) which are present in healthy skin [76]. MSCs have been effectively used to treat chronic wounds and promote healing process [77]. Several studies have demonstrated that human placenta is rich in MSCs, growth factors, and ECM which provides tissue repair in the wound healing process. They have antimicrobial, anti-inflammatory, and angiogenic properties which make placental membranes suitable for wound therapy [78, 79]. Grafix® (Osiris Therapeutics, Inc., Columbia, MD) is a cryopreserved, human placental membrane that consists of growth factors, ECM, and living cells including MSCs, fibroblasts, and epithelial cells [79]. RCT have revealed that Grafix® led to high closure rates for hard-to-heal DFUs and other chronic wounds [80•, 81]. EpiFix® (MiMedx, Kennesaw, GA) is a dehydrated human amnion/chorion membrane (dHACM) allograft composed of a single layer of epithelial cells, a basement membrane, and a non-vascular connective tissue matrix. A small RCT found that dHACM stimulates wound closure leading to a faster healing of DFUs in comparison to standard therapy [82, 83]. In a small biased study, Zelen et al. found DFU patients treated with EpiFix® showed the highest rates of complete healing and a faster wound healing than those treated with Apligraf® [84].
Medicated Dressings
Medicated dressings contain compounds that have therapeutic activity, overcoming the drawbacks found with topical agents. Plain gauze and paraffin-impregnated gauze are some of the traditional dressings utilized to deliver drugs. Within the modern dressings used to deliver therapeutic materials are hydrocolloids, hydrogels, alginates, and polyurethane foam/films [1]. These incorporated drugs participate in the wound healing process as debriding agent by removing necrotic tissue, antimicrobials avoiding or treating infection, or growth factors in order to stimulate skin regeneration. Some of these regularly incorporated drugs include antimicrobial agents, growth factors, and enzymes.
One factor that delays the wound healing process is wound infection. Therefore, antibiotics-loaded wound dressings are required for the prevention and elimination of microorganisms at the wound bed, especially in diabetic foot ulcers [85], and surgical and accident wounds [1, 86]. Some therapeutic agents-impregnated wound dressings include povidone-iodine and silver [87], gentamicin sulfate, dialkylcarbamoyl chloride [85], norfloxacin [88], and minocycline [89]. The mechanism of action by which iodine dressings may work is via oxidative degradation of bacterial cell components by blocking the function of proteins. Although, prolonged use of iodine results in staining and skin irritation [2•]. Diakylcarbamoyl chloride, which is impregnated into Cutisorb® (BSN Medical, Hamburg, Germany), is a fatty acid derivative that irreversibly attaches microorganisms to the dressing fibers via hydrophobic interaction. This feature makes Cutisorb® a highly absorbent cotton wool dressing [1]. The antimicrobial activity of silver is due to the interaction of silver ions with thiol groups in enzymes and proteins; additionally, silver was also proposed to work by releasing K+ ions from bacteria [90]. Silver-loaded dressings available are fibrous hydrocolloid, silicone gels, and polyurethane foam film. Gentamicin is usually delivered to the wound from collagen sponges, and under investigation, norfloxacin from silicone gel sheets, and minocycline from chitosan film dressings [1].
Growth factors also play an important role in the wound healing process. Growth factors participate in cell division, migration, differentiation, protein expression, and enzyme production. Their wound healing features are result of the angiogenesis stimulation and the modulation of fibroblast activity and inflammation, affecting the inflammatory, proliferation, and migration phases of wound healing [1, 91]. The growth factors get caught in the wound bed within the clots, delaying the healing process; thus, exogenous administration of growth factors benefits the healing process. Platelet-derived growth factor (PDGF) is the only approved growth factor for wound healing, specifically for neuropathic diabetic foot ulcers, promoting chemotactic recruitment, cell proliferation, and angiogenesis. Other growth factors that have been or are being studied include epidermal growth factor (EGF), fibroblast growth factor (FGF), transforming growth factor (TGF-b1), insulin-like growth factor (IGF-1), granulocyte-macrophage colony-stimulating factor (GM-CSF), and autologous platelet thrombin. Huang et al. found combined application of GM-CSF with alginate promotes healing in refractory chronic skin ulcers [92], while Yan et al. found that GM-CSF promotes healing of deep partial-thickness burn wounds and has been shown to speed healing of VLU [93, 94]. A study in EGF-loaded dressings found that it stimulates the hastening of wound healing process with less scarring [95]. Different dressings have been applied to deliver the aforementioned growth factors to the wound area, such as hydrogel, collagen film, alginate, and polyurethane dressings [1].
If necrotic tissues are present in the wound bed, wound healing can be delayed; hence, wound debridement is required in order to remove the cellular waste, harmful exudate, and necrotic tissue [96]. Enzymatic wound dressings use proteolytic enzymes to hydrolyze the denatured proteins in wound necrotic/devitalized tissue [97]. Although, to have an optimal debriding efficacy, a good delivery system, a constant period of enzyme activity, an ideal wound environment, and a good compatibility between the enzyme and the dressing are required [96]. Collagenase-based ointments are now used to destroy necrotic tissue, and previously available papain products are no longer available on the market in the USA. Clostridium collagenase is the active enzyme used in Collagenase SANTYL Ointment which selectively degrades non-viable collagen fibers while conserving living collagen tissue [98]. Furthermore, papain is largely used as a debriding agent in developing countries for burn wounds. Papain is a proteolytic enzyme, specifically cleaves cysteine residues, with an advantage of being active over a broad pH range of 3–12 [99]. Mustafah and Chung revealed that crushed Papase (papain enzyme in tablets)-loaded dressing applied to chronic diabetic foot ulcer cleared associated overgranulation [100].
Conclusions
Wound healing is a dynamic process that requires a proper environment to promote wound closure. To enhance the healing process, a variety of wound dressing materials are available from traditional to modern dressings; nevertheless, the selection of a specific wound dressing is imperative for proper healing. The emergence of advanced dressings such as bioactive wound dressing and HSE has brought a new perspective of wound healing, but there is no best-in-breed product yet to treat acute and/or chronic wounds. Therefore, wound dressing research studies that address the main involved factors of normal healing process will significantly help improve wound healing process and timing.
Abbreviations
- DFU:
-
Diabetic foot ulcer
- dHACM:
-
Dehydrated human amnion/chorion membrane
- ECM:
-
Extracellular matrix
- EGF:
-
Epidermal growth factor
- FGF:
-
Fibroblast growth factor
- GM-CSF:
-
Granulocyte-macrophage colony-stimulating factor
- HA:
-
Hyaluronic acid
- HSE:
-
Human skin equivalents
- IGF-1:
-
Insulin-like growth factor
- MSC:
-
Mesenchymal stem cell
- PDGF:
-
Platelet-derived growth factor
- RCT:
-
Randomized control trial
- sNAG:
-
Shortened nanofibers of poly-N-acetyl glucosamine
- TGF-β1:
-
Transforming growth factor
- VLU:
-
Venous leg ulcer
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Boateng JS, Matthews KH, Stevens HN, Eccleston GM. Wound healing dressings and drug delivery systems: a review. J Pharm Sci. 2008;97(8):2892–923.
Dhivya S, Padma VV, Santhini E. Wound dressings—a review. Biomedicine (Taipei). 2015;5(4):22. Comprehensive review article that offers a critical discussion of several kinds of wound dressings.
Percival JN. Classification of wounds and their management. Surgery. 2002;20:114–7.
Moore K, McCallion R, Searle RJ, Stacey MC, Harding KG. Prediction and monitoring the therapeutic response of chronic dermal wounds. Int Wound J. 2006;3(2):89–96.
Landén NX, Li D, Ståhle M. Transition from inflammation to proliferation: a critical step during wound healing. Cell Mol Life Sci. 2016;73(20):3861–85.
Guo S, Dipietro LA. Factors affecting wound healing. J Dent Res. 2010;89(3):219–29.
Pereira RF, Bártolo PJ. Traditional therapies for skin wound healing. Adv Wound Care (New Rochelle). 2016;5(5):208–29.
Weller C, Sussman G. Wound dressings update. J Pharm Pract Res. 2006;36:318–24. Review article which covers a thorough description in wound assessment and different types of wound dressings.
Daunton C, Kothari S, Smith L, Steele D. A history of materials and practices for wound management. Wound Pract Res. 2012;20:174–86.
Shah JB. The history of wound care. J Am Col Certif Wound Spec. 2011;3(3):65–6.
Jones VJ. The use of gauze: will it ever change? Int Wound J. 2006;3(2):79–86.
Sung KY, Lee SY. Nonoperative management of extravasation injuries associated with neonatal parenteral nutrition using multiple punctures and a hydrocolloid dressing. Wounds. 2016;28(5):145–51.
Koksal C, Bozkurt AK. Combination of hydrocolloid dressing and medical compression stockings versus Unna’s Boot for the treatment of venous leg ulcers. Swiss Med Wkly. 2003;133(25–26):364–8.
Jiang Q, Zhou W, Wang J, Tang R, Zhang D, Wang X. Hypromellose succinate-crosslinked chitosan hydrogel films for potential wound dressing. Int J Biol Macromol. 2016;91:85–91.
Wichterle O, Lim D. Hydrophilic gels for biological use. Nature. 1960;185:117–8.
Jayakumar R, Rajkumar M, Freitas H, Selvamurugan N, Nair SV, Furuike T, et al. Preparation, characterization, bioactive and metal uptake studies of alginate/phosphorylated chitin blend films. Int J Biol Macromol. 2009;44(1):107–11.
Wang T, Qisheng G, Zhao J, Mei J, Shao M, Pan Y, et al. Calcium alginate enhances wound healing by up-regulating the ratio of collagen types I/III in diabetic rats. Int J Clin Exp Pathol. 2015;8(6):6636–45.
Balakrishnan B, Mohanty M, Umashankar PR, Jayakrishnan A. Evaluation of an in situ forming hydrogel wound dressing based on oxidized alginate and gelatin. Biomaterials. 2005;26:6335–42.
Kurczewska J, Sawicka P, Ratajczak M, Gajęcka M, Schroeder G. Will the use of double barrier result in sustained release of vancomycin? Optimization of parameters for preparation of a new antibacterial alginate-based modern dressing. Int J Pharm. 2015;496(2):526–33.
Kuo CK, Ma PX. Ionically crosslinked alginate hydrogels as scaffolds for tissue engineering: part 1. Structure, gelation rate and mechanical properties. Biomaterials. 2001;2(6):511–21.
Blair SD, Jarvis P, Salmon M, McCollum C. Clinical trial of calcium alginate haemostatic swabs. Br J Surg. 1990;77:568–70.
Blair SD, Backhouse CM, Harper R, Matthews J, McCollum CN. Comparison of absorbable materials for surgical haemostasis. Br J Surg. 1988;75:69–71.
Segal HC, Hunt BJ, Gilding K. The effects of alginate and non-alginate wound dressings on blood coagulation and platelet activation. J Biomater Appl. 1998;12:249–57.
Thomas A, Harding KG, Moore K. Alginates from wound dressings activate human macrophages to secrete tumor necrosis factor-alpha. Biomaterials. 2000;21(17):1797–802.
Schmidt RJ, Turner TD. Calcium alginate dressings. Pharm J. 1986;236:578.
Doyle JW, Roth T, Smith M. Effects of calcium alginate on cellular wound healing processes modelled in vitro. J Biomed Mater Res. 1996;32(4):561–8.
Morgan DA. Wounds: what should a dressing formulary include? Hosp Pharm. 2009;9:261–6.
Vermeulen H, Ubbink DT, Goossens A, de Vos R, Legemate DA. Systematic review of dressings and topical agents for surgical wounds healing by secondary intention. Br J Surg. 2005;92(6):665–72. Epidemiological study which highlights the differences between dressings and topical agents.
Ramos-e-Silva M, Ribeiro de Castro MC. New dressings, including tissue-engineered living skin. Clin Dermatol. 2002;20(6):715–23.
Ramshaw JA, Werkmeister JA, Glattauer V. Collagen-based biomaterials. Biotechnol Genet Eng Rev. 1996;13:335–82.
González A. Use of collagen extracellular matrix dressing for the treatment of a recurrent venous ulcer in a 52-year-old patient. J Wound Ostomy Continence Nurs. 2016;43(3):310–2.
Doillon CJ, Silver FH. Collagen-based wound dressing: effects of hyaluronic acid and fibronectin on wound healing. Biomaterials. 1986;7(1):3–8.
Lee M, Han SH, Choi WJ, Chung KH, Lee JW. Hyaluronic acid dressing (Healoderm) in the treatment of diabetic foot ulcer: a prospective, randomized, placebo-controlled, single-center study. Wound Repair Regen. 2016;24(3):581–8.
Ferrari R, Boracchi P, Romussi S, Ravasio G, Stefanello D. Application of hyaluronic acid in the healing of non-experimental open wounds: a pilot study on 12 wounds in 10 client-owned dogs. Vet World. 2015;8(10):1247–59.
Ishihara M, Nakanishi K, Ono K, Sato M, Kikuchi M, Saito Y, et al. Photocrosslinkable chitosan as a dressing for wound occlusion and accelerator in healing process. Biomaterials. 2002;23(3):833–40.
Abdel-Mohsen AM, Jancar J, Massoud D, Fohlerova Z, Elhadidy H, Spotz Z, et al. Novel chitin/chitosan-glucan wound dressing: isolation, characterization, antibacterial activity and wound healing properties. Int J Pharm. 2016;510(1):86–99.
Anjum S, Arora A, Alam MS, Gupta B. Development of antimicrobial and scar preventive chitosan hydrogel wound dressings. Int J Pharm. 2016;508(1–2):92–101.
Fan X, Chen K, He X, Li N, Huang J, Tang K, et al. Nano-TiO2/collagen-chitosan porous scaffold for wound repairing. Int J Biol Macromol. 2016;91:15–22.
Choi SM, Ryu HA, Lee KM, Kim HJ, Park IK, Cho WJ, et al. Development of stabilized growth factor-loaded hyaluronate-collagen dressing (HCD) matrix for impaired wound healing. Biomater Res. 2016;20:9.
Catanzano O, D’Esposito V, Acierno S, Ambrosio MR, De Caro C, Avagliano C, et al. Alginate-hyaluronan composite hydrogels accelerate wound healing process. Carbohydr Polym. 2015;131:407–14.
Mian M, Beghè F, Mian E. Collagen as a pharmacological approach in wound healing. Int J Tissue React. 1992;14(Suppl):1–9.
Ruszczak Z, Friess W. Collagen as a carrier for on-site delivery of antibacterial drugs. Adv Drug Deliv Rev. 2003;55(12):1679–98.
Dreifke MB, Jayasuriya AA, Jayasuriya AC. Current wound healing procedures and potential care. Mater Sci Eng C Mater Biol Appl. 2015;48:651–62. Analytical review of wound dressings based on biocompatible polymers.
Dreifke MB, Ebraheim NA, Jayasuriya AC. Investigation of potential injectable polymeric biomaterials for bone regeneration. J Biomed Mater Res A. 2013;101(8):2436–47.
Turley EA, Torrance J. Localization of hyaluronate and hyaluronate-binding protein on motile and non-motile fibroblasts. Exp Cell Res. 1985;161(1):17–28.
Moczar M, Robert L. Stimulation of cell proliferation by hyaluronidase during in vitro aging of human skin fibroblasts. Exp Gerontol. 1993;28(1):59–68.
Ghazi K, Deng-Pichon U, Warnet JM, Rat P. Hyaluronan fragments improve wound healing on in vitro cutaneous model through P2X7 purinoreceptor basal activation: role of molecular weight. PLoS One. 2012;7(11):e48351.
Abdel-Mohsen AM, Jancar J, Massoud D, Fohlerova Z, Elhadidy H, Spotz Z, Hebeish A. Novel chitin/chitosan-glucan wound dressing: Isolation, characterization, antibacterial activity and wound healing properties. Int J Pharm. 2016;510(1):86–99.
Ueno H, Mori T, Fujinaga T. Topical formulations and wound healing applications of chitosan. Adv Drug Deliv Rev. 2001;52(2):105–15.
Moura LI, Dias AM, Leal EC, Carvalho L, de Sousa HC, Carvalho E. Chitosan-based dressings loaded with neurotensin—an efficient strategy to improve early diabetic wound healing. Acta Biomater. 2014;10(2):843–57.
Kirichenko AK, Bolshakov IN, Ali-Riza AE, Vlasov AA. Morphological study of burn wound healing with the use of collagen-chitosan wound dressing. Bull Exp Biol Med. 2013;154(5):692–6.
Choi JS, Kim JD, Yoon HS, Cho YW. Full-thickness skin wound healing using human placenta-derived extracellular matrix containing bioactive molecules. Tissue Eng Part A. 2013;19(3–4):329–39.
Wojtowicz AM, Oliveira S, Carlson MW, Zawadzka A, Rousseau CF, Baksh D. The importance of both fibroblasts and keratinocytes in a bilayered living cellular construct used in wound healing. Wound Repair Regen. 2014;22(2):246–55.
Nathoo R, Howe N, Cohen G. Skin substitutes: an overview of the key players in wound management. J Clin Aesthet Dermatol. 2014;7(10):44–8.
Centanni JM, Straseski JA, Wicks A, et al. StrataGraft skin substitute is well-tolerated and is not acutely immunogenic in patients with traumatic wounds: results from a prospective, randomized, controlled dose escalation trial. Ann Surg. 2011;253(4):672–83.
Sun T, Han Y, Chai J, Yang H. Transplantation of microskin autografts with overlaid selectively decellularized split thickness porcine skin in the repair of deep burn wounds. J Burn Care Res. 2011;32(3):e67–73.
Marston WA, Hanft J, Norwood P, Pollak R, Dermagraft Diabetic Foot Ulcer Study Group. The efficacy and safety of Dermagraft in improving the healing of chronic diabetic foot ulcers, results of a prospective randomized trial. Diabetes Care. 2003;26(6):1701–5.
Límová M. Active wound coverings: bioengineered skin and dermal substitutes. Surg Clin North Am. 2010;90(6):1237–55.
Falanga V, Sabolinski M. A bilayered living skin construct (APLIGRAF) accelerates complete closure of hard-to-heal venous ulcers. Wound Repair Regen. 1999;7(4):201–7.
Marston WA, Sabolinski ML, Parsons NB, Kirsner RS. Comparative effectiveness of a bilayered living cellular construct and a porcine collagen wound dressing in the treatment of venous leg ulcers. Wound Repair Regen. 2014;22(3):334–40.
Falabella AF, Valencia IC, Eaglstein WH, Schachner LA. Tissue-engineered skin (Apligraf) in the healing of patients with epidermolysis bullosa wounds. Arch Dermatol. 2000;136(10):1225–30.
Muhart M, McFalls S, Kirsner RS, Elgart GW, Kerdel F, Sabolinski ML, et al. Behavior of tissue-engineered skin: a comparison of a living skin equivalent, autograft, and occlusive dressing in human donor sites. Arch Dermatol. 1999;135(8):913–8.
Mathur M, De A, Gore M. Microbiological assessment of cadaver skin grafts received in a Skin Bank. Burns. 2009;35(1):104–6.
Brigido SA. The use of an acellular dermal regenerative tissue matrix in the treatment of lower extremity wounds: a prospective 16-week pilot study. Int Wound J. 2006;3(3):181–7.
González Alaña I, Torrero López JV, Martín Playá P, Gabilondo Zubizarreta FJ. Combined use of negative pressure wound therapy and Integra® to treat complex defects in lower extremities after burns. Ann Burns Fire Disasters. 2013;26(2):90–3.
Park CA, Defranzo AJ, Marks MW, Molnar JA. Outpatient reconstruction using Integra and sub atmospheric pressure. Ann Plast Surg. 2009;62(2):164–9.
Molnar JA, DeFranzo AJ, Hadaegh A, Morykwas MJ, Shen P, Argenta LC. Acceleration of Integra incorporation in complex tissue defects with sub atmospheric pressure. Plast Reconstr Surg. 2004;113(5):1339–46.
Raimer DW, Group AR, Petitt MS, Nosrati N, Yamazaki ML, Davis NA, et al. Porcine xenograft biosynthetic wound dressings for the management of postoperative Mohs wounds. Dermatol Online J. 2011;17(9):1.
Romanelli M, Dini V, Bertone MS. Randomized comparison of OASIS wound matrix versus moist wound dressing in the treatment of difficult-to-heal wounds of mixed arterial/venous etiology. Adv Skin Wound Care. 2010;23(1):34–8.
Mostow EN, Haraway GD, Dalsing M, Hodde JP, King D, OASIS Venus Ulcer Study Group. Effectiveness of an extracellular matrix graft (OASIS Wound Matrix) in the treatment of chronic leg ulcers: a randomized clinical trial. J Vasc Surg. 2005;41(5):837–43. One of the first papers to show the effectiveness of this graft in VLUs. This paper may have increased the frequency of using this graft for VLUs treatment.
Palmer BL, Gantt DS, Lawrence ME, Rajab MH, Dehmer GJ. Effectiveness and safety of manual hemostasis facilitated by the SyvekPatch with one hour of bedrest after coronary angiography using six-French catheters. Am J Cardiol. 2004;93(1):96–7.
Lindner HB, Zhang A, Eldridge J, Demcheva M, Tsichlis P, et al. Anti-bacterial effects of poly-N-acetyl-glucosamine nanofibers in cutaneous wound healing: requirement for Akt1. PLoS One. 2011;6(4):e18996.
Pietramaggiori G, Yang HJ, Scherer SS, Kaipainen A, Chan RK, et al. Effects of poly-N-acetyl glucosamine (pGlcNAc) patch on wound healing in db/db mouse. J Trauma. 2008;64(3):803–8.
Scherer SS, Pietramaggiori G, Matthews J, Perry S, Assmann A, et al. Poly-N-acetyl glucosamine nanofibers: a new bioactive material to enhance diabetic wound healing by cell migration and angiogenesis. Ann Surg. 2009;250(2):322–30.
Kelechi TJ, Mueller M, Hankin CS, Bronstone A, Samies J, et al. A randomized, investigator-blinded, controlled pilot study to evaluate the safety and efficacy of a poly-N-acetyl glucosamine-derived membrane material in patients with venous leg ulcers. J Am Acad Dermatol. 2012;66(6):e209–15.
Maxson S, Lopez EA, Yoo D, Danilkovitch-Miagkova A, Leroux MA. Concise review: role of mesenchymal stem cells in wound repair. Stem Cells Transl Med. 2012;1(2):142–9.
Shin L, Peterson DA. Human mesenchymal stem cell grafts enhance normal and impaired wound healing by recruiting existing endogenous tissue stem/progenitor cells. Stem Cells Transl Med. 2013;2(1):33–42.
Faulk WP, Matthews R, Stevens PJ, Bennett JP, Burgos H, et al. Human amnion as an adjunct in wound healing. Lancet. 1980;1:1156–8.
Gibbons GW. Grafix®, a cryopreserved placental membrane, for the treatment of chronic/stalled wounds. Adv Wound Care (New Rochelle). 2015;4(9):534–44.
Lavery LA, Fulmer J, Shebetka KA, et al. The efficacy and safety of Grafix((R)) for the treatment of chronic diabetic foot ulcers: results of a multicentre, controlled, randomized, blinded, clinical trial. Int Wound J. 2014;11:554–60. Seminal study which demonstrates this graft as a good option for DFUs. This paper may have expanded this graft use to other pathologies.
Regulski M, Jacobstein DA, Petranto RD, Migliori VJ, Nair G, et al. A retrospective analysis of a human cellular repair matrix for the treatment of chronic wounds. Ostomy Wound Manage. 2013;59:38–43.
Zelen CM, Serena TE, Denoziere G, Fetterolf DE. A prospective randomised comparative parallel study of amniotic membrane wound graft in the management of diabetic foot ulcers. Int Wound J. 2013;10(5):502–7.
Fetterolf DE, Istwan NB, Stanziano GJ. An evaluation of healing metrics associated with commonly used advanced wound care products for the treatment of chronic diabetic foot ulcers. Manag Care. 2014;23:31–8.
Zelen CM, Gould L, Serena TE, Carter MJ, Keller J, Li WW. A prospective, randomised, controlled, multi-centre comparative effectiveness study of healing using dehydrated human amnion/chorion membrane allograft, bioengineered skin substitute or standard of care for treatment of chronic lower extremity diabetic ulcers. Int Wound J. 2015;12(6):724–32.
Amin N, Doupis J. Diabetic foot disease: from the evaluation of the “foot at risk” to the novel diabetic ulcer treatment modalities. World J Diabetes. 2016;7(7):153–64.
Phaechamud T, Issarayungyuen P, Pichayakorn W. Gentamicin sulfate-loaded porous natural rubber films for wound dressing. Int J Biol Macromol. 2016;85:634–44.
Meaume S, Vallet D, Morere MN, Téot L. Evaluation of a silver-releasing hydroalginate dressing in chronic wounds with signs of local infection. J Wound Care. 2005;14(9):411–9.
Denkbaş EB, Oztürk E, Ozdemir N, Keçeci K, Agalar C. Norfloxacin-loaded chitosan sponges as wound dressing material. J Biomater Appl. 2004;18(4):291–303.
Aoyagi S, Onishi H, Machida Y. Novel chitosan wound dressing loaded with minocycline for the treatment of severe burn wounds. Int J Pharm. 2007;330(1–2):138–45.
Jung WK, Koo HC, Kim KW, Shin S, Kim SH, Park YH. Antibacterial activity and mechanism of action of the silver ion in Staphylococcus aureus and Escherichia coli. Appl Environ Microbiol. 2008;74(7):2171–8.
Komarcević A. The modern approach to wound treatment. Med Pregl. 2000;53(7–8):363–8 [Article in Croatian].
Huang G, Sun T, Zhang L, Wu Q, Zhang K, Tian Q, et al. Combined application of alginate dressing and human granulocyte-macrophage colony stimulating factor promotes healing in refractory chronic skin ulcers. Exp Ther Med. 2014;7(6):1772–6.
Yan H, Chen J, Peng X. Recombinant human granulocyte-macrophage colony-stimulating factor hydrogel promotes healing of deep partial thickness burn wounds. Burns. 2012;38(6):877–81.
Da Costa RM, Ribeiro Jesus FM, Aniceto C, Mendes M. Randomized, double-blind, placebo-controlled, dose-ranging study of granulocyte-macrophage colony stimulating factor in patients with chronic venous leg ulcers. Wound Repair Regen. 1999;7(1):17–25.
Khanbanha N, Atyabi F, Taheri A, Talaie F, Mahbod M, Dinarvand R. Healing efficacy of an EGF impregnated triple gel based wound dressing: in vitro and in vivo studies. Biomed Res Int. 2014;2014:493732.
Shi L, Ermis R, Kiedaisch B, Carson D. The effect of various wound dressings on the activity of debriding enzymes. Adv Skin Wound Care. 2010;23(10):456–62.
Ramundo J, Gray M. Enzymatic wound debridement. J Wound Ostomy Continence Nurs. 2008;35:273–80.
Miller JD, Carter E, Hatch DC, Zhubrak M, Giovinco NA, Armstrong DG. Use of collagenase ointment in conjunction with negative pressure wound therapy in the care of diabetic wounds: a case series of six patients. Diabet Foot Ankle. 2015;6:24999.
Singh D, Singh R. Papain incorporated chitin dressings for wound debridement sterilized by gamma radiation. Radiat Phys Chem. 2012;81:1781–5.
Mustafah NM, Chung TY. Papase as a treatment option for the overgranulating wound. J Wound Care. 2014;23(2 Suppl):S10–2.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Luis J. Borda and Flor E. Macquhae declare that they have no conflicts of interest to disclose.
Dr. Kirsner reports grants from Smith and Nephew, personal fees from Organogenesis, outside the submitted work.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Wound Care and Healing
Rights and permissions
About this article
Cite this article
Borda, L.J., Macquhae, F.E. & Kirsner, R.S. Wound Dressings: A Comprehensive Review. Curr Derm Rep 5, 287–297 (2016). https://doi.org/10.1007/s13671-016-0162-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13671-016-0162-5