Abstract
Purpose of Review
Present the major aspects of fragility fractures, emphasizing their prevention and care in low- and middle-income countries (LMICs).
Recent Findings
Fragility fractures will increase significantly during the next few decades, especially in LMICs. Demographic and socioeconomic data remain limited. Fragility fractures have a low priority for most LMICs, as well as for global public health leadership.
Summary
The majority of the world’s population lives in LMICs. Their socioeconomic features and healthcare resources are heterogeneous, but all lack access to medical and surgical care, especially in more impoverished and rural regions. Fragility fractures are a major cause of disability with negative economic impact. Population growth and aging drive their increasing number and burden. Resources necessary for prevention and treatment are deficient. Present plans and corrective measures may be insufficient to address the global needs of fragility fractures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Fragility Fractures in the Developing World
“A global call to action to improve the care of people with fragility fractures” was recently made by the Fragility Fracture Network, with co-sponsors and endorsers [1]. It urges cooperative action, to address the “enormous increase in fragility fracture incidence …imposing a massive burden on patients, their families, health systems and societies globally.” The intent is to move the world’s policymakers to recognize and address the burden of fragility fractures (FFxs), especially in poorer countries. The purpose of this review is to emphasize the special challenges that FFxs pose for countries with more limited resources and to consider some possible solutions.
Fragility Fractures
The World Health Organization defined fragility fracture as “a fracture caused by injury that would be insufficient to fracture a normal bone...the result of reduced compressive and/or torsional strength of bone.” Clinically, a fragility fracture may be defined as a fracture “...that occurs as a result of a minimal trauma, such as a fall from a standing height or less, or no identifiable trauma” [2].
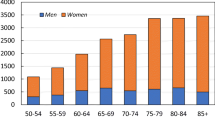
Fractures, especially low-energy fractures, are relatively common among the elderly [3]. Their overall frequency increases with age, especially in women after menopause. The high incidence of fractures among elders was recognized long ago, but under-appreciated because short life expectancies resulted in fewer older individuals and thus fewer fractures. Increases in the number of elderlies are causing a worldwide increase in the number of their fractures. The vast majority of these injuries result from low-energy forces and are associated with reduced bone strength, as well as greater risk of falling, due to impaired mobility and frailty [4, 5]. An estimated nine million FFxs occurred worldwide in 2000 [6]. After age 50, approximately a third of women will sustain an FFx, while the figure for men is about 20%.
Women sustain the majority of hip fractures, but the 30% occurring in men carry higher mortality and morbidity [7]. The costs of caring for FFxs are immense. For EU countries, they totaled $37,000,000,000 in 2010. The US cost in 2015 was $20,000,000,000 [8•].
Frequency Increasing
Estimates for the number of hip fractures worldwide generally show significant increases. In 1990, there were 1.3 million, and in 2010, 2.7 million. The projected incidence for 2050 is 4.5 million, but it could range from 7 to 21 million cases per year [6]. Similar increases can be expected for all FFx. Since recovery from these injuries is often incomplete, there is an expanding population of disabled individuals. For hip fractures alone, the number living with disability (prevalence) is expected to exceed 21 million in the next 40 years.
Anatomic Sites
FFxs most commonly affect the proximal femur (hip), vertebral body (spine), or distal forearm. In Johnell’s review, 18% involved the proximal femur, 19% the distal forearm, 16% the spine, 8% the humerus, and 40% were at other sites [9]. Hip fractures receive the bulk of attention, because their impact and burden are the most significant, with increased mortality as well as morbidity. Their costly treatment often involves hospitalization and surgery, when these resources are available [10].
Geographic Variation
There is significant geographic and ethnic variation of FFx incidence, ranging from less than 100/100,000 to over 500/100,000 per year, corrected for age [11••, 12]. Rates are increasing in Asia and Latin America. More developed countries have higher hip fracture incidence, raising the possibility that lifestyle differences might play a role. The reasons for variation in FFx incidence are not known but both genetic and environmental factors are likely to be involved [13,14,15].
Risk Factors
In addition to age and female sex, a most clinically compelling risk factor for a FFx is the history of a previous such injury, particularly involving hip, wrist, or spine. This risk is highest during the first several months, more than doubling the probability of another fracture [16, 17].
Epidemiology studies continue to inform us about factors associated with FFx risk and potential measures for prevention and treatment [18]. Table 1 lists a number of recognized risk factors for FFxs. With regard to developing countries, it is important to recognize lifestyle issues, like tobacco and alcohol consumption, as well as physical activity and nutritional factors (vitamin D and calcium deficiency, obesity, excessively low weight, etc.) [19,20,21,22].
Recently, HIV with and without anti-retroviral medication has been associated with reduced bone density and FFxs [23,24,25,26].
Relationship of Fragility Fractures to Osteoporosis [27]
Bone fragility is of course an essential feature of FFxs. Bone strength is largely dependent upon its mineral content. Bones grow in strength and mineral density during adolescence and early adulthood [28]. This is stimulated by weight-bearing activity and requires adequate calcium, vitamin D, and protein. By age 40, bone mineral density gradually declines, accelerating in women at menopause. Bone strength decreases along with mineral content, although it depends upon anatomic factors as well. Individuals who fail to acquire sufficient strength during their early years are likely to have earlier and more profound bone fragility, with increased risk of FFxs. Other factors are also important, so that reduced bone mineral density, below the threshold set to define osteoporosis (≤ 2.5 standard deviations below a healthy young adult), does not predict 100% likelihood of a FFx. Furthermore, many individuals with lesser degrees of low bone mineral density do sustain FFxs. In fact, these individuals, with T scores in the range from − 1.0 to − 2.5, defined as the bounds for osteopenia, are the majority of patients with FFxs.
Since bone density alone does not determine FFx risk, other factors must also be considered [29••]. There is a clear trend away from relying only on BMD for FFX risk assessment. Several assessment tools have been developed to include other risks [30]. The FRAX algorithm is prominent among these, though it does not include all important risks, particularly those related to falling. Adapting FRAX to a new population group requires accurate and voluminous epidemiologic data. Because FRAX can be used with or without bone mineral density measurements, it has been adopted by a number of less developed countries [31,32,33,34]. Oden et al. used country-specific FRAX data to estimate the number of individuals at high risk of FFx [35]. They determined that this population was 158 million globally in 2010 and predicted it would double by 2040. Fifty-five percent of these patients live in Asia.
Impact and Burden
The impact of FFxs is manyfold. They cause disability, pain, and loss of participation in society.
Substantial burden falls on family and friends. Care for FFxs strains the capacity and finances of healthcare systems and social services [36•]. Total costs include acute treatment, rehabilitation, ongoing support for those whose disabilities necessitate assistance, and reduced productivity by patient and caregivers. Where facilities are available, hip fracture patients may become institutionalized [37]. Williamson et al. recently reviewed costs and their drivers for patients with fragility hip fractures. Their pooled studies included over 670,000 patients, from 27 different countries (none from Africa, since no data were available). This study reported the cost of index hospitalization, as well as the total health and social costs for the first 12 months. The pooled estimate for the former was $10,075, and the total was $43,669 per patient. Prior co-morbidity and the development of complications were the two most significant drivers of higher costs [38].
The costs of caring for FFxs are challenging for the wealthiest of nations and hard to imagine for the majority of economies, which have far fewer resources to devote to the foreseeable needs of the looming FFx epidemic [39].
Disability-adjusted life years (DALYs) provide a quantitative measure of morbidity and mortality. Johnell and Kanis report a burden estimated at 5,800,000 DALYs, 0.8% of the global burden due to noncommunicable diseases [9]. Eighteen percent of their total fractures involved the hip, which accounted for 40% of the DALYs. However, 60% of the overall burden was due to other than hip fractures.
Papadimitriou’s recent study robustly assessed the burden of hip fractures with a pooled analysis of prospective cohorts and real-life follow-up data [40••]. During 13 years, 3.5% of almost 224,000 men and women sustained hip fractures, with 5.3% mortality and 5964 DALYs, 70% of which were attributed to disability and the rest to premature death. The 27/1000 individual DALY rate was similar to those found in the same pool for breast or pancreatic cancer.
The International Osteoporosis Foundation’s Regional Surveys, from 2010 to 2013, obtained data from selected countries worldwide. In the Asia-Pacific region, population percentage over 50 ranged from 10 to 45%, reported annual hip fracture rates ranged from 90 to 400 per 100,000, and several countries reported surgical treatment for hip fractures of 50% or less [41,42,43,44].
The Institute for Health Metrics and Evaluation (IHME) has developed a truly remarkable approach to studying the global burden of disease (GBD) and presenting data about the relative significance of death and disability of each health problem [45]. Hoy et al. point out that these studies have progressively improved, but in the case of musculoskeletal conditions, the impact of disability probably remains under-appreciated especially for LMICs [46, 47••]. Musculoskeletal conditions contribute much more to the global burden through the disability they cause than from premature mortality. Over 20% of the world’s disability burden, measured as years lived with disability (YLD), is due to musculoskeletal conditions. Failure to consider properly the musculoskeletal disability burden may result in misappropriation of resources (scarce enough already in LMICs). Presently, a disproportionately low level of resources is devoted to prevention, treatment, and research of MSK conditions, including FFxs. More high-quality local data, with improved aggregation, may provide a stronger stimulus for prevention and treatment of the expanding problem of FFxs.
The GBD, for all its many strengths, does not specifically identify FFxs, nor proximal femur (hip) fractures or others by anatomic location. To date, the IHME’s GBD presents osteoporosis as a risk factor, not as a diagnosis per se. GBD 2016, as presented online by the IHME, indicates that the proportion of the World’s disease burden in DALYs due to falls with a low BMD 1.49%, with a 19.5% risk factor attribution. It is hard to know how valid an indicator this is for the worldwide contribution of FFxs [46, 47••, 48, 49••].
The World Health Organization played a significant role in early studies of osteoporosis and FFxs. However, in 1998, the World Health Assembly urged a more comprehensive approach to noncommunicable diseases (NCDs), focusing on the four major ones—cardiovascular, chronic respiratory disease, cancer, and diabetes—with their greater contribution to mortality rates compared to disability [50]. Subsequently, osteoporosis and FFxs have received scant mention among the “other NCDs” in current WHO documents, regarding NCDs, aging, universal health care, and other international public health issues [51, 52]. Disability, often severe and long-lasting, contributes more than early death to the burden of FFxs. Measured in DALYs, the most significant contributors to disease burden of those 60 years and older are cardiovascular diseases (30%), cancer (15%), chronic respiratory diseases (10%), musculoskeletal diseases (8%), and neurological and mental disorders (7%) [53]. It is understandable why fragility fractures (2016 estimate of approximately 1.5%) have been assigned a lower priority.
Developing World
There is no universally accepted definition for “the developing world.” This term is commonly applied to those countries classified by the World Bank as either low (N = 31) or middle (N = 109) income, based on the gross national income per capita [54, 55]. For the 2018 fiscal year, the defining levels are based on the 2016 GNI figures for annual per capita income. Those at $1005 or less were defined as low income. Those from $1006 to $3995 were defined as lower-middle-, those from $3996 to $12,235 as upper-middle-, and those equal to or greater than $12,236 as high-income economies. The majority of the world’s population lives in countries classified as either low- or middle-income countries (LMICs). Low levels on the Human Development Index and limited industrialization are associated features of LMICs.
Table 2 presents 2017 population data for the world and the four World Bank economic groups, with their predicted population in 2050. The proportion of people aged 65 and over and those 80 and over are included, to represent elderly and extreme elderly populations. Table 3 lists the World Bank geographic regions, with percentage population in the LMIC range. These two tables demonstrate predicted growth and aging of the regional populations, of which Asia and sub-Saharan Africa are most notable. Elderly and extreme elderly populations are those with the highest rates of FFxs. While these age groups are still relatively less numerous in many LMICs, significant increases, along with an epidemic of FFxs, are foreseen in the next few decades.
The UN has a separate category for the world’s poorest and weakest countries—the so-called least developed countries (LDCs) [56]. There are currently 47 such countries, 33 from Africa, 13 from Asia-Pacific, and 1 from Latin America. The LDCs include 31 of the 34 low-income countries and 15 of the 47 lower-middle-income countries. Their total population is over 880 million (approximately 12% of the world’s), but generates less than 2% of the world’s gross domestic product. The LDCs share a number of significant socioeconomic weaknesses.
By any measure, the human and institutional capacities of LMICs are limited. Their overall incomes are low and distributed unequally. Political instability, fragile governance, and various conflicts are common. Education levels are low. Their environmental conditions are poor (sanitation, indoor and outdoor air quality, water quality). Their primarily agrarian economies are typified by low productivity and limited investment. Seeking work, many citizens of LMICs are moving from rural to urban areas, with steadily growing slums. LMICs’ primary external source of income is a small, non-diverse number of agricultural and extractive exports, vulnerable to international market variation. Manufacturing, if present, is very limited and primarily labor-intensive. Their economies are seriously constrained, with chronic deficits, debts, and dependence on external support. Those LMICs not included among the LDCs have similar features, although less concentrated and in different proportions. Table 4 lists major characteristics of developing economies.
While the economic status of countries is defined by average income levels, it is important to remember that the distribution of income, and other resources, is far from uniform. Low- and middle-income countries vary greatly from one to another, just as they do internally. Pockets of relative wealth, and of significant poverty, are the norm. The overriding reality is that each of the countries in this group lacks the resources necessary for addressing various needs which might reasonably be regarded as essential. These needs, and efforts to meet them, are comprehensively set forth by the United Nations Sustainable Development Goals (SDGs), “a universal call to action to end poverty, protect the planet, and ensure that all people enjoy peace and prosperity” [57]. There is a strong association between low income, low socioeconomic status, low education, and noncommunicable diseases [58•]. The SDG program recognizes the need for concurrently addressing all 17 goals.
Efforts to meet the interconnected SDGs began in January 2016, with a target date of 2030. Progress is being monitored through use of 230 specific, measurable indicators. The world’s health needs are addressed by the third SDG, “Good Health and Wellbeing.” This seeks to ensure healthy lives and promote well-being for all at all ages. Its overriding thrust is to “Achieve universal health coverage, including financial risk protection, access to quality essential healthcare services and access to safe, effective, quality and affordable essential medicines and vaccines for all.” Health-related indicators and progress toward meeting them are being collected and presented by the IHME [59]. Their most recent report, using data from the 2016 Global Burden of Disease study showed “many places are facing challenges in meeting defined health-related SDG targets, particularly among countries that are the worst off” [60]. This report holds out hope that the ambitious targets can be met, but clearly demonstrates the gaps between present status and attainment of the health-related SDG.
Healthcare Resources in Developing Countries
Access to healthcare resources is significantly limited in developing countries. This is true on both the supply side (available healthcare services) and the demand side (people in need of healthcare) [61•, 62•, 63•].
Striking disparities exist in healthcare funding and necessary resources for healthcare generally and surgical care in particular. Worldwide, in 2015, the percentage of GDP devoted to health expenditures was 9.9%. In the low-income (LI) population, it was 6%, in the lower-middle (L-M) 4%, and in the upper-middle (U-M) 5.7%, vs. 12.4% in the high-income group. Using purchasing power parity–adjusted US dollars per capita per year, the LI group was $98, L-M $259, U-M $904, and high income (HI) $5280 [64]. Available human resources are similarly limited in poorer countries. The numbers of physicians per 1000 people are 0.3 in LI, 0.7 in L-M, and 1.9 in U-M countries, vs. 3.0 in the HI group. The numbers of surgical specialists (surgeons, anesthesiologists, and obstetricians) per 100,000 population are 1.6 in LI countries, 10.1 in L-M, 40 in U-M vs. 67 in HI countries [64].
The entire health systems of LMICs are deficient. Mills has reviewed and listed various deficiencies and provided suggestions for funding options and incentives for improvement [65].
Limited Access to Surgical Treatment
Recently, surgical treatment has been recognized as an essential, yet deficient, part of healthcare for all countries [66, 67]. Almost one third of conditions which contribute to the global burden of disease can only be addressed through surgical treatment. However, it is estimated that more than 5 billion of the world’s 7.4 billion population lack access to safe, effective surgical care. Furthermore, in LI and L-M countries, nine of ten people are unable to obtain basic surgical care [68]. While prodigious efforts are underway to rectify these shortcomings by the energetic Global Surgery movement, including WHO, World Bank, and UN, it is clear that in many parts of the developing world, the necessary resources for operative care of FFxs are simply missing [62•, 69, 70]. This is true for all types of surgery, including for fractures and other essential musculoskeletal conditions [71•, 72••]. Essentially every element of the complex set of required resources required for safe effective surgery is missing, in short supply, or available only at costs which are impoverishing for those in need. A good picture of the impact of these limited resources is that they include essentially every element of what DeVries and Rosenberg call the global surgical ecosystem [73]—from surgeons and anesthesiologists to medications, X-rays, electricity, water, sanitation, hygiene, sterile supplies, and workable systems to procure, deploy, deliver, and dispose, not to mention information management and financing [71, 74, 75]. Hospital accreditation is in its infancy in LMICs [76]. The Global Surgery target for musculoskeletal care is to provide surgical treatment for open fractures, thus decreasing the mortality and morbidity associated with non-operative care for these injuries. Complex open or radiologically guided minimally invasive internal fixation procedures are beyond the horizon of current goals for LMICs. In fact, surgical care for FFxs presently plays a minor role in the developing world. (For example, in many of the poorest countries, few patients with hip fractures receive any operative care [41,42,43,44]. Many are never seen by accredited healthcare providers in clinics or hospitals. The injured, or their families, may choose not to seek care for various reasons [61•, 77•, 78]. Sometimes, they choose traditional healers or bone setters [79,80,81,82]. Subsequently, some whose care has been initiated by traditional providers change to “western medicine” through national, non-governmental, or other private institutions. Their delayed presentations are often associated with poor results.
Possibilities for Improving Care of Fragility Fractures in Developing World
Optimal Treatment for Fragility Fractures in the Developed World
A number of advances in the treatment of FFxs have improved outcomes in well-resourced settings. Regrettably, most of these are difficult if not impossible to implement in the developing world, but we should consider them as now-established standards for optimal care of an aged population with multiple co-morbidities, reduced physical function, mechanically fragile bone, and a limited lifespan. It is clear that every effort must be made to minimize complications related to either medical or surgical issues, since these increase morbidity, mortality, and costs [83]. A robust multidisciplinary quality assurance program is an essential component of the overall care bundle [84]. Others are as follows:
-
A co-management team combining geriatric medicine and surgeons with interest and expertise in the care of patients with FFx. Anesthesia staffing and care must be optimal as well [85].
-
A fracture-liaison service to plan and execute osteoporosis treatment and follow-up to reduce the risk of secondary fractures [86, 87].
-
Organized clinical pathways for expeditious, well-planned care [88, 89].
-
Appropriate implants and surgical techniques, including intra-operative imaging, are key, including options for augmenting fixation and using special implants and techniques, including prostheses, when more standard treatments are unlikely to succeed [90,91,92,93].
-
Comprehensive rehabilitation, both in-patient and community-based [94, 95].
-
Ongoing research to assess and address needed improvements going forward [96].
However, it is noteworthy that these measures have not been successfully adopted throughout the developed world [97••]. For the few fortunate LMIC citizens who can gain access to developed world care in their own countries, through their own resources, through travel elsewhere, or through proximity to better-prepared institutions, adequate care may be possible. However, the vast majority of their countrymen will need to await substantially more progress toward the goals of universal healthcare.
Prevention of Fragility Fractures
Various strategies are being developed to identify individuals with an increased risk of FFxs and to provide cost-effective treatments. Primary preventive measures seek to identify individuals at higher, but reducible, risks and provide timely prevention. On a patient by patient basis, this might be considered as a component of primary medical care [50]. However, the costs would probably exceed benefits if this approach were applied on a population basis in the developing world. Secondary prevention, vs. additional FFxs, has an obvious role, since an individual who has sustained one FFx does have substantial risk of subsequent occurrences [16]. The so-called primordial prevention (prevention of risk factors themselves) might reasonably be considered to reduce FFx risks through population-based public health measures. The normal life course of bone development and aging leads to a peak in bone mass in early adulthood, with a subsequent gradual decline, which accelerates in women during menopause. Measures to promote bone formation during early life, such as nutritional support (adequate calcium, vitamin D, and protein) as well as encouragement of physical activity, and avoidance of tobacco use, alcohol consumption, obesity, and sedentary lifestyle, help promote maximal peak bone mass [98]. If this becomes high enough, bone mineral density may never decline into the range of high FFx risk. Nutritional and lifestyle factors may also help reduce the risk of FFxs throughout life [99]. Other factors, such as medications or diseases that cause secondary osteoporosis, are also associated with potentially preventable FFx risk. Fortunately, many of these risk factors are being included in WHO efforts toward controlling noncommunicable diseases and promoting healthy aging [51, 52]. Osteoporosis screening and management guidelines are best tailored according to the needs and resources of individual counties. While a few countries have succeeded in generating valuable epidemiological data on osteoporotic fractures, to validate risk calculation tools and formulate treatment guidelines, most have not yet done so [33].
Morales-Torres offers several recommendations to control osteoporosis and thus the frequency of FFxs in developing countries: (1) campaigns to increase awareness of individuals at risk and relevant healthcare professionals, (2) healthy lifestyle strategies, (3) evidence-based medical guidelines, (4) emphasis on prevention of falls, quality fracture care, and effective rehabilitation, (5) collection and monitoring of economic data, and (6) the use of country-specific FFx databases [34]. Ultimately, the leaders of each LMIC will need to determine appropriate priorities for their country, based on their own evidence as well as worldwide experience. The major challenge will probably always involve financing the priority-driven needs.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Dreinhofer KE, Mitchell PJ, Begue T, Cooper C, Costa ML, Falaschi P, et al. A global call to action to improve the care of people with fragility fractures. Injury. 2018;49(8):1393–7. https://doi.org/10.1016/j.injury.2018.06.032.
Vanasse A, Dagenais P, Niyonsenga T, Gregoire JP, Courteau J, Hemiari A. Bone mineral density measurement and osteoporosis treatment after a fragility fracture in older adults: regional variation and determinants of use in Quebec. BMC Musculoskelet Disord. 2005;6:33. https://doi.org/10.1186/1471-2474-6-33.
Court-Brown CM, McQueen MM. Global forum: fractures in the elderly. J Bone Joint Surg Am. 2016;98(9):e36. https://doi.org/10.2106/JBJS.15.00793.
World Health Organization. WHO global report on falls prevention in older age. [Internet]. WHO, Geneva, Switzerland. 2007. http://www.who.int/ageing/projects/falls_prevention_older_age/en/index.html
Jorgensen TS, Hansen AH, Sahlberg M, Gislason GH, Torp-Pedersen C, Andersson C, et al. Falls and comorbidity: the pathway to fractures. Scand J Public Health. 2014;42(3):287–94. https://doi.org/10.1177/1403494813516831.
Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. 2004;15(11):897–902. https://doi.org/10.1007/s00198-004-1627-0.
Cauley JA, Cawthon PM, Peters KE, Cummings SR, Ensrud KE, Bauer DC, et al. Risk factors for hip fracture in older men: the osteoporotic fractures in men study (MrOS). J Bone Miner Res. 2016;31(10):1810–9. https://doi.org/10.1002/jbmr.2836.
• Cooper C, Ferrari, S. IOF compendium of osteoporosis [Internet]. International Osteoporosis Foundation 2017. https://www.iofbonehealth.org/compendium-of-osteoporosis. A comprehensive yet usable review of important and persuasive literature of osteoporosis and fragility fractures, with worldwide focus.
Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17(12):1726–33. https://doi.org/10.1007/s00198-006-0172-4.
Tajeu GS, Delzell E, Smith W, Arora T, Curtis JR, Saag KG, et al. Death, debility, and destitution following hip fracture. J Gerontol A Biol Sci Med Sci. 2014;69(3):346–53. https://doi.org/10.1093/gerona/glt105.
•• Cauley JA, Chalhoub D, Kassem AM, Fuleihan GH. Geographic and ethnic disparities in osteoporotic fractures. Nat Rev Endocrinol. 2014;10(6):338–51. https://doi.org/10.1038/nrendo.2014.51 Excellent review of global variations in incidence and prevalence of fragility fractures.
Kanis JA, Oden A, McCloskey EV, Johansson H, Wahl DA, Cooper C, et al. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int. 2012;23(9):2239–56. https://doi.org/10.1007/s00198-012-1964-3.
Adams DJ, Rowe DW, Ackert-Bicknell CL. Genetics of aging bone. Mamm Genome. 2016;27(7–8):367–80. https://doi.org/10.1007/s00335-016-9650-y.
Boudin E, Van Hul W. Mechanisms in endocrinology: genetics of human bone formation. Eur J Endocrinol. 2017;177(2):R69–r83. https://doi.org/10.1530/eje-16-0990.
Taylor KC, Evans DS, Edwards DRV, Edwards TL, Sofer T, Li G, et al. A genome-wide association study meta-analysis of clinical fracture in 10,012 African American women. Bone Rep. 2016;5:233–42. https://doi.org/10.1016/j.bonr.2016.08.005.
Johansson H, Siggeirsdottir K, Harvey NC, Oden A, Gudnason V, McCloskey E, et al. Imminent risk of fracture after fracture. Osteoporos Int. 2017;28(3):775–80. https://doi.org/10.1007/s00198-016-3868-0.
Bliuc D, Alarkawi D, Nguyen TV, Eisman JA, Center JR. Risk of subsequent fractures and mortality in elderly women and men with fragility fractures with and without osteoporotic bone density: the Dubbo Osteoporosis Epidemiology Study. J Bone Miner Res. 2015;30(4):637–46. https://doi.org/10.1002/jbmr.2393.
Cauley JA. Osteoporosis: fracture epidemiology update 2016. Curr Opin Rheumatol. 2017;29(2):150–6. https://doi.org/10.1097/BOR.0000000000000365.
van der Meer IM, Middelkoop BJ, Boeke AJ, Lips P. Prevalence of vitamin D deficiency among Turkish, Moroccan, Indian and sub-Sahara African populations in Europe and their countries of origin: an overview. Osteoporos Int. 2011;22(4):1009–21. https://doi.org/10.1007/s00198-010-1279-1.
Balk EM, Adam GP, Langberg VN, Earley A, Clark P, Ebeling PR, et al. Global dietary calcium intake among adults: a systematic review. Osteoporos Int. 2017;28(12):3315–24. https://doi.org/10.1007/s00198-017-4230-x.
Kai Ming Chan MA, 2 & Edith M.C. Lau3. Exercise interventions: defusing the world’s osteoporosis time bomb. Bulletin of the World Health Organization 2003, 81 (11). 2003;81(11).
Nguyen VH. Community osteoporosis screening services for the prevention of osteoporotic fractures in population health: a literature review. Int J Evid Based Healthc. 2017;15(2):43–52. https://doi.org/10.1097/XEB.0000000000000104.
Matovu FK, Wattanachanya L, Beksinska M, Pettifor JM, Ruxrungtham K. Bone health and HIV in resource-limited settings: a scoping review. Curr Opin HIV AIDS. 2016;11(3):306–25. https://doi.org/10.1097/COH.0000000000000274.
Womack JA, Goulet JL, Gibert C, Brandt C, Chang CC, Gulanski B, Fraenkel L, Mattocks K, Rimland D, Rodriguez-Barradas MC, Tate J, Yin MT, Justice AC, for the Veterans Aging Cohort Study Project Team Increased risk of fragility fractures among HIV infected compared to uninfected male veterans. PLoS One 2011;6(2):e17217. doi:https://doi.org/10.1371/journal.pone.0017217.
Gonciulea A, Wang R, Althoff KN, Palella FJ, Lake J, Kingsley LA, et al. An increased rate of fracture occurs a decade earlier in HIV+ compared with HIV- men. AIDS. 2017;31(10):1435–43. https://doi.org/10.1097/QAD.0000000000001493.
Yin MT, Shiau S, Rimland D, Gibert CL, Bedimo RJ, Rodriguez-Barradas MC, et al. Fracture prediction with modified-FRAX in older HIV-infected and uninfected men. J Acquir Immune Defic Syndr. 2016;72(5):513–20. https://doi.org/10.1097/QAI.0000000000000998.
Sanchez-Riera L, Wilson N, Kamalaraj N, Nolla JM, Kok C, Li Y, et al. Osteoporosis and fragility fractures. Best Pract Res Clin Rheumatol. 2010;24(6):793–810. https://doi.org/10.1016/j.berh.2010.10.003.
Chew CK, Clarke BL. Causes of low peak bone mass in women. Maturitas. 2018;111:61–8. https://doi.org/10.1016/j.maturitas.2017.12.010.
•• Curtis EM, Moon RJ, Harvey NC, Cooper C. The impact of fragility fracture and approaches to osteoporosis risk assessment worldwide. Bone. 2017;104:29–38. https://doi.org/10.1016/j.bone.2017.01.024 Up-to-date review of fragility Fx epidemiology and risk assessment with implications for treatment, health care policies, and the current osteoporosis treatment gap.
Aspray TJ. Fragility fracture: recent developments in risk assessment. Ther Adv Musculoskelet Dis. 2015;7(1):17–25. https://doi.org/10.1177/1759720X14564562.
Kanis JA, Johansson H, Oden A, Cooper C, EV MC, et al. Worldwide uptake of FRAX. Arch Osteoporos. 2014;9:166. https://doi.org/10.1007/s11657-013-0166-8.
Kanis JA, Harvey NC, Cooper C, Johansson H, Oden A, McCloskey EV, et al. A systematic review of intervention thresholds based on FRAX: a report prepared for the National Osteoporosis Guideline Group and the International Osteoporosis Foundation. Arch Osteoporos. 2016;11(1):25. https://doi.org/10.1007/s11657-016-0278-z.
El-Hajj Fuleihan G, Chakhtoura M, Cauley JA, Chamoun N. Worldwide Fracture Prediction. J Clin Densitom. 2017;20(3):397–424. https://doi.org/10.1016/j.jocd.2017.06.008.
Morales-Torres JSGr-Ua. Strategies for the prevention and control of osteoporosis in developing countries. Clin Rheumatol. 2007;26(2):139–43. https://doi.org/10.1007/s10067-006-0314-2.
Oden A, McCloskey EV, Kanis JA, Harvey NC, Johansson H. Burden of high fracture probability worldwide: secular increases 2010–2040. Osteoporos Int. 2015;26(9):2243–8. https://doi.org/10.1007/s00198-015-3154-6.
• Sanchez-Riera L, Wilson N. Fragility fractures and their impact on older people. Best Pract Res Clin Rheumatol. 2017;31(2):169–91. https://doi.org/10.1016/j.berh.2017.10.001 Nicely summarizes the burden of fragility fractures for the elderly and national economies, especially in the developing world. Also includes risk factors, fall prevention, and nutritional deficiencies.
Cooper C, Campion G, Melton L. Hip fractures in the elderly - a world-wide projection. Osteoporosis Int. 1992;2:285–9.
•• Williamson S, Landeiro F, McConnell T, Fulford-Smith L, Javaid MK, Judge A, et al. Costs of fragility hip fractures globally: a systematic review and meta-regression analysis. Osteoporos Int. 2017;28(10):2791–800. https://doi.org/10.1007/s00198-017-4153-6 Excellent systematic review of the economics of economic burden of fragility fractures.
Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury. 2018;49(8):1458–60. https://doi.org/10.1016/j.injury.2018.04.015.
•• Papadimitriou N, Tsilidis KK, Orfanos P, Benetou V, Ntzani EE, Soerjomataram I, et al. Burden of hip fracture using disability-adjusted life-years: a pooled analysis of prospective cohorts in the CHANCES consortium. Lancet Public Health. 2017;2(5):e239–e46. https://doi.org/10.1016/s2468-2667(17)30046-4 Best available study using large database to produce well-validated DALY estimates for fragility fractures.
El-Hajj FG. The Middle East and Africa Regional Audit Epidemiology, costs and burden of osteoporosis in 2011. Nyon: International Osteoporosis Foundation; 2011.
Lesnyak O. Eastern European & Central Asian Regional Audit. Epidemiology, costs and burden of osteoporosis in 2010: Nyon, International Osteoporosis Foundation; 2010.
Mithal AEP. ASIA-PACIFIC REGIONAL AUDIT Epidemiology, costs and burden of osteoporosis in 2013. Nyon: International Osteoporosis Foundation; 2013.
Zanchetta J. Latin_America_Audit_2012 IOF Epidemiology, costs and burden of osteoporosis in 2012. Nyon: International Osteoporosis Foundation; 2012.
Murray CJL, Lopez AD. Measuring global health: motivation and evolution of the Global Burden of Disease Study. Lancet. 2017;390(10100):1460–4. https://doi.org/10.1016/s0140-6736(17)32367-x.
Hoy D, Geere JA, Davatchi F, Meggitt B, Barrero LH. A time for action: Opportunities for preventing the growing burden and disability from musculoskeletal conditions in low- and middle-income countries. Best Pract Res Clin Rheumatol. 2014;28(3):377–93. https://doi.org/10.1016/j.berh.2014.07.006.
•• Hoy D, Smith E, Cross M, et al. Reflecting on the global burden of musculoskeletal conditions - lessons learned from GBD10 and next steps forward. Ann Rheum Dis. 2015;74:4–7. https://doi.org/10.1136/annrheumdis-2013-204431 A thorough critique of IHME Global Burden of Disease 2010 study’s strengths and limitations regarding global burden of musculoskeletal conditions generally and fragility fractures specifically.
Fischer S, Kapinos KA, Mulcahy A, Pinto L, Hayden O, Barron R. Estimating the long-term functional burden of osteoporosis-related fractures. Osteoporos Int. 2017;28(10):2843–51. https://doi.org/10.1007/s00198-017-4110-4.
•• Sanchez-Riera L, Carnahan E, Vos T, Veerman L, Norman R, Lim SS, et al. The global burden attributable to low bone mineral density. Ann Rheum Dis. 2014;73(9):1635–45. https://doi.org/10.1136/annrheumdis-2013-204320 The best information about fragility Fx burden that can be gleaned from GBD 2010. To date, there has been no further progress reported.
Kanis J. Assessment of osteoporosis at the primary health-care level. WHO TR-2007. Printed by the University of Sheffield.: World Health Organization Collaborating Centre for Metabolic Bone Diseases, University of Sheffield, UK. 2007 2007.
World Health Organization. Noncommunicable diseases progress monitor, 2017 [Internet]. WHO, Geneva. 2017. www.who.int/nmh/publications/ncd-progress-monitor-2017/en/.
World Health Organization. Global strategy and action plan on ageing and health [Internet]. World Health Organization, Geneva. 2017. http://www.who.int/ageing/WHO-GSAP-2017.pdf?ua=1.
Prince MJ, Wu F, Guo Y, Gutierrez Robledo LM, O’Donnell M, Sullivan R, et al. The burden of disease in older people and implications for health policy and practice. Lancet. 2015;385(9967):549–62. https://doi.org/10.1016/s0140-6736(14)61347-7.
World Bank. World Bank country and lending groups - country classification [Internet]. In: Data. World Bank, Washington, DC USA. 2018. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
Khokhar TS, U. Should we continue to use the term “developing world”? World Bank, 1818 H Street, NW Washington, DC 20433 USA. 2015. https://blogs.worldbank.org/opendata/should-we-continue-use-term-developing-world. Accessed 10/04/2018 2018.
United Nations. Handbook on the Least developed country category: inclusion, graduation and special support measures [Internet]. United Nations New York 2015. https://www.un.org/development/desa/dpad/wp-content/uploads/sites/45/publication/2015cdphandbook.pdf.
United Nations. The sustainable development goals report 2018 [Internet]. United Nations, New York, NY. 2018. https://unstats.un.org/sdgs/files/report/2018/TheSustainableDevelopmentGoalsReport2018-EN.pdf.
• Niessen LW, Mohan D, Akuoku JK, Mirelman AJ, Ahmed S, Koehlmoos TP, et al. Tackling socioeconomic inequalities and non-communicable diseases in low-income and middle-income countries under the Sustainable Development agenda. Lancet. 2018;391(10134):2036–46. https://doi.org/10.1016/s0140-6736(18)30482-3 Presents relationships between NCDs and socio-economic issues in LMICs and how the UN’s inter-related SDGs must be addressed as a group instead of one by one.
Institute for Health Measurement and Evaluation (IHME). Health-related SDGs [Internet]. University of Washington, 2017. , Seattle, WA:. 2017. http://vizhub.healthdata.org/sdg.
Fullman N, Barber RM. Measuring progress and projecting attainment on the basis of past trends of the health-related Sustainable Development Goals in 188 countries: an analysis from the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1423–59. https://doi.org/10.1016/s0140-6736(17)32336-x.
• Barber RM, Fullman N, Sorensen RJD, Bollyky T, McKee M, Nolte E, et al. Healthcare Access and Quality Index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990–2015: a novel analysis from the Global Burden of Disease Study 2015. Lancet. 2017;390(10091):231–66. https://doi.org/10.1016/s0140-6736(17)30818-8 Compelling study that presents country-specific deficiencies of health-care access and quality using GBD 2015 data.
• Forrester JD, Forrester JA, Kamara TB, Groen RS, Shrestha S, Gupta S, et al. Self-reported determinants of access to surgical care in 3 developing countries. JAMA Surg. 2016;151(3):257–63. https://doi.org/10.1001/jamasurg.2015.3431 Presents details of barriers to healthcare access in resource-limited countries.
• Stephens T, Mezei A, O’Hara NN, Potter J, Mugarura R, Blachut PA, et al. When surgical resources are severely constrained, who receives care? Determinants of access to orthopaedic trauma surgery in Uganda. World J Surg. 2017;41(6):1415–9. https://doi.org/10.1007/s00268-017-3874-1 Presents the realities and personal impact for patients trying to obtain fracture surgery in a developing country.
World Bank. World development indicators 2.12_Health_systems [Internet]. In: World Development Indicators. World Bank 2017. http://wdi.worldbank.org/table/2.12. Accessed 10/5/2018 2018.
Mills A. Health care systems in low- and middle-income countries. N Engl J Med. 2014;370(6):552–7. https://doi.org/10.1056/NEJMra1110897.
Meara JG, Leather AJM, Hagander L, Alkire BC, Alonso N, Ameh EA, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386(9993):569–624. https://doi.org/10.1016/s0140-6736(15)60160-x.
Rose J, Weiser TG, Hider P, Wilson L, Gruen RL, Bickler SW. Estimated need for surgery worldwide based on prevalence of diseases: a modelling strategy for the WHO Global Health Estimate. Lancet Glob Health. 2015;3:S13–20. https://doi.org/10.1016/s2214-109x(15)70087-2.
Alkire BC, Shrime MG, Dare AJ, Vincent JR, Meara JG. Global economic consequences of selected surgical diseases: a modelling study. Lancet Glob Health. 2015;3:S21–S7. https://doi.org/10.1016/s2214-109x(15)70088-4.
Ologunde R, Maruthappu M, Shanmugarajah K, Shalhoub J. Surgical care in low and middle-income countries: burden and barriers. Int J Surg (London, England). 2014;12(8):858–63. https://doi.org/10.1016/j.ijsu.2014.07.009.
Blair KJ, Paladino L, Shaw PL, Shapiro MB, Nwomeh BC, Swaroop M. Surgical and trauma care in low- and middle-income countries: a review of capacity assessments. J Surg Res. 2017;210:139–51. https://doi.org/10.1016/j.jss.2016.11.005.
• Leslie HH, Spiegelman D, Zhou X, Kruk ME. Service readiness of health facilities in Bangladesh, Haiti, Kenya, Malawi, Namibia, Nepal, Rwanda, Senegal, Uganda and the United Republic of Tanzania. Bull World Health Organ. 2017;95(11):738–48. https://doi.org/10.2471/BLT.17.191916 Further confirmation of widespread deficiencies of healthcare facilities in LMICs.
•• Spiegel DA, Nduaguba A, Cherian MN, Monono M, Kelley ET. Deficiencies in the availability of essential musculoskeletal surgical services at 883 health facilities in 24 low- and lower-middle-income countries. World J Surg. 2015;39(6):1421–32. https://doi.org/10.1007/s00268-015-2971-2 Another powerful example of why operative care for fragility fractures is just not available for much of the world’s population.
deVries CR, Rosenberg JS. Global surgical ecosystems: a need for systems strengthening. Ann Glob Health. 2016;82(4):605–13. https://doi.org/10.1016/j.aogh.2016.09.011.
Chawla S, Kurani S, Wren SM, Stewart B, Burnham G, Kushner A, et al. Electricity and generator availability in LMIC hospitals: improving access to safe surgery. J Surg Res. 2018;223:136–41. https://doi.org/10.1016/j.jss.2017.10.016.
Cronk R, Bartram J. Environmental conditions in health care facilities in low- and middle-income countries: coverage and inequalities. Int J Hyg Environ Health. 2018;221(3):409–22. https://doi.org/10.1016/j.ijheh.2018.01.004.
Smits H, Supachutikul A, Mate K. Hospital accreditation: lessons from low- and middle-income countries. Glob Health. 2014;10:65. https://doi.org/10.1186/s12992-014-0065-9.
• Dash SK, Panigrahi R, Palo N, Priyadarshi A, Biswal M. Fragility hip fractures in elderly patients in Bhubaneswar, India (2012–2014): a prospective multicenter study of 1031 elderly patients. Geriatr Orthop Surg Rehabil. 2015;6(1):11–5. https://doi.org/10.1177/2151458514555570 Remarkable barriers and inequities in hip fracture care, well documented from the world’s second most populous country.
Tewari A, Pati S, Nallala S, Webster P, Rath S, Yadav L, et al. Care seeking behaviour of older adults with hip fracture in India: a qualitative study. J Patient Care. 2017;03(01). https://doi.org/10.4172/2573-4598.1000128.
Nwachukwu. Traditional bonesetters and contemporary orthopaedic fracture care in a developing nation: historical aspects, contemporary status and future directions. Open Orthop J. 2011;5:20–6.
Edusei AK, Owusu-Ansah FE, Dogbe JA, Morgan J, Sarpong K. Perspectives in musculoskeletal injury management by traditional bone setters in Ashanti, Ghana. Afr J Disabil. 2015;4(1):97. https://doi.org/10.4102/ajod.v4i1.97.
Tantray M-D. Orthopedic trauma care by traditional bone setters in developing nations: an observational hospital study from Kashmir. Int J Curr Trends Sci Technol. 2018;8(2):20402–7. https://doi.org/10.15520/ctst.v8i02.314.pdf.
Walker G. The role of the traditional healer in developing countries. Bull R Coll Surg Engl. 2015;97(5):216–8. https://doi.org/10.1308/147363515x14272809070924.
Broderick JM, Bruce-Brand R, Stanley E, Mulhall KJ. Osteoporotic hip fractures: the burden of fixation failure. Sci World J. 2013;2013:515197. https://doi.org/10.1155/2013/515197.
Bhandari M, Swiontkowski M. Management of acute hip fracture. N Engl J Med. 2017;377(21):2053–62. https://doi.org/10.1056/NEJMcp1611090.
Mitchell P, Akesson K, Chandran M, Cooper C, Ganda K, Schneider M. Implementation of Models of Care for secondary osteoporotic fracture prevention and orthogeriatric Models of Care for osteoporotic hip fracture. Best Pract Res Clin Rheumatol. 2016;30(3):536–58. https://doi.org/10.1016/j.berh.2016.09.008.
Bawa HS, Weick J, Dirschl DR. Anti-osteoporotic therapy after fragility fracture lowers rate of subsequent fracture: analysis of a large population sample. J Bone Joint Surg Am. 2015;97(19):1555–62. https://doi.org/10.2106/JBJS.N.01275.
Akesson K, Marsh D, Mitchell PJ, McLellan AR, Stenmark J, Pierroz DD, et al. Capture the fracture: a best practice framework and global campaign to break the fragility fracture cycle. Osteoporos Int. 2013;24(8):2135–52. https://doi.org/10.1007/s00198-013-2348-z.
Mears SC, Kates SL. A guide to improving the care of patients with fragility fractures, edition 2. Geriatr Orthop Surg Rehabil. 2015;6(2):58–120. https://doi.org/10.1177/2151458515572697.
Khan AZ, Rames RD, Miller AN. Clinical management of osteoporotic fractures. Curr Osteoporos Rep. 2018;16:299–311. https://doi.org/10.1007/s11914-018-0443-y.
Augat P, Goldhahn J. Osteoporotic fracture fixation - a biomechanical perspective. Injury. 2016;47(S2):S1–2.
Grant KD, Busse EC, Park DK, Baker KC. Internal fixation of osteoporotic bone. J Am Acad Orthop Surg. 2018;26(5):166–74. https://doi.org/10.5435/JAAOS-D-16-00142.
Johnson JP, Norris G, Giannoudis PV. Bone augmentation: is it really needed? Injury. 2018;49(8):1367–72. https://doi.org/10.1016/j.injury.2018.07.020.
Van Lieshout EMM, Alt V. Bone graft substitutes and bone morphogenetic proteins for osteoporotic fractures: what is the evidence? Injury. 2016;47:S43–S6. https://doi.org/10.1016/s0020-1383(16)30011-0.
Roberts JL, Din NU, Williams M, Hawkes CA, Charles JM, Hoare Z, et al. Development of an evidence-based complex intervention for community rehabilitation of patients with hip fracture using realist review, survey and focus groups. BMJ Open. 2017;7(10):e014362. https://doi.org/10.1136/bmjopen-2016-014362.
Wilson H. Orthogeriatrics in hip fracture. Open Orthop J. 2017;11:1181–9. https://doi.org/10.2174/1874325001711011181.
Wu HH, Liu M, Patel KR, Turner W, Baltus L, Caldwell AM et al Impact of academic collaboration and quality of clinical orthopaedic research conducted in low- and middle-income countries SICOT J 2017;3:6. doi:https://doi.org/10.1051/sicotj/2016042.
•• Harvey NC, McCloskey EV, Mitchell PJ, Dawson-Hughes B, Pierroz DD, Reginster JY, et al. Mind the (treatment) gap: a global perspective on current and future strategies for prevention of fragility fractures. Osteoporos Int. 2017;28(5):1507–29. https://doi.org/10.1007/s00198-016-3894-y Barriers to prevention of fragility fractures, with options for overcoming them, from rich as well as developing countries.
Cooper C, Dawson-Hughes, B, Gordon, CM, Rizzoli, R. Healthy nutrition, healthy bones: how nutritional factors affect musculoskeletal health throughout life International Osteoporosis Foundation, Nyon, Switzerland. 2015. https://www.iofbonehealth.org/thematic-report-2015.
Abrahamsen B, Brask-Lindemann D, Rubin KH, Schwarz P. A review of lifestyle, smoking and other modifiable risk factors for osteoporotic fractures. Bonekey Rep. 2014;3:574. https://doi.org/10.1038/bonekey.2014.69.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Peter Trafton reports being a trustee of AO North America, a trustee of Orthopaedics Overseas, and a member of the Orthopaedic Trauma Association’s Humanitarian Committee.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Geriatric Orthopedics
Rights and permissions
About this article
Cite this article
Trafton, P.G. Fragility Fractures in the Developing World: a Rising Challenge. Curr Geri Rep 7, 278–287 (2018). https://doi.org/10.1007/s13670-018-0267-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13670-018-0267-8