Abstract
Knee osteoarthritis (OA) is prevalent and disabling condition in older adults. Pain, weakness, instability, stiffness, and loss of mobility result in a reduction of physical, recreational, and social activities that impact an individual’s health, lifestyle, and societal role. Exercise is highly beneficial for the many body systems that are impacted indirectly by this disease as well as for improving quality of life. The purpose of this narrative review is to identify exercise options and dosage parameters to aid the clinician in assisting individuals with knee OA. These exercise options include cardiovascular training, resistance training, and balance or neuromuscular control training, which work to improve the cardiovascular and neuromuscular systems to improve function. The application of exercise by health care professionals is often dosed at levels which may not achieve optimal gains for the individual desiring to restore functional activities and improve recreational and social participation. Understanding the current literature on prescribing exercise for individuals with knee OA aids clinicians in obtaining better patient outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is the leading cause of chronic disability in the elderly [1] affecting over 21 million people [2] in the USA. That number is expected to rise in the coming decades owing to growth in the older population as baby boomers age [3]. The prevalence of symptomatic knee OA has been reported to increase with every decade of life, with the annual incidence of knee OA being highest between 55 and 64 years of age [4]. Recent evidence estimates that 14 million persons in the National Health Interview Survey of 2007–2008 had symptomatic knee OA including one in eight individuals under 45 years of age, which represented nearly two million cases and almost half the individuals between age 45 and 65 years representing 6 million cases [4]. In addition, evidence exists that younger adults in the military experience primary knee OA at rates of 1.41 per 1000 person-years [5]. Both of these suggest that individuals often begin the degenerative process of knee OA much earlier in life than originally believed. Early effects of knee OA can result in higher and more frequent activity restrictions with resulting longer declines in physical activity possibly accounting for some of the low levels of function seen in older adults with knee OA. There is a large physical, social, and economic burden with inactivity [6]. As many adults are living longer into their seventh, eighth, and ninth decades, longer inactivity could potentially result in greater disability and healthcare utilization for knee OA.
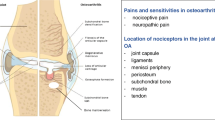
OA most commonly affects the joints of the knees, hips, spine, and hands [7]. The knees followed by the hips are the most commonly affected weight-bearing joints. Women have a higher incidence and prevalence of hand and knee OA [8], whereas men have higher incidence and prevalence of hip OA [9]. The pathogenesis of OA is no longer thought to be just related to joint stresses that cause degeneration. Synovitis, or an inflammation of the synovium in the joints, has been found to be responsible for pro-inflammatory cytokines including interleukins (IL), tumor necrosis factors (TNF), and transforming growth factor beta (TGF-b) that may regulate other pro-inflammatory substances including collagenases and a disintegrin and metalloproteinase with a thrombospondin type 1 motif (ADAMTS) proteases, which break down cartilage. In addition, bone growth related to osteophyte formation at joint margins facilitated by TGF-b can result in altered joint mechanics and increase the inflammation at the joint. The result of inflammation and altered joint mechanics can be cartilage damage within the joint.
There is no cure for OA, and therefore, management and treatment options are imperative. Reducing disability resultant from OA is paramount, as the economic consequences related to the disease are high [10]. Conservative treatment options for the relief of many OA symptoms include multimodal approaches such as orthotics and bracing, cold packs and ice massage, modalities (both pulsed ultrasound and NMES), manual therapy, and exercise including range of motion (ROM), resistance training, functional training, and cardiovascular training. A recent review of the Cochrane database for conservative care of primarily low to moderate severity knee OA found small and short-term improvements with NSAIDs and other medications, some herbal supplementation, land and aquatic exercise, acupuncture, intra-articular injections, and viscosupplementation [11]. A recent study using supervised multi-modal land and aquatic exercise as compared to NSAIDs, intra-articular hyaluronic acid injections, and advice in individuals with severe knee OA (grade 3 or above using Kellgren-Lawrence scale) found superior results for general fitness and function in the exercise group and improved pain and stiffness in the medication group at 1-year follow-up [12]. Manual therapy has been shown to have short-term benefits as well long-term benefits in addition to exercise [13, 14]. Other treatment options, such as bracing and ultrasound, have low quality to no evidence for improvement of knee OA symptoms [11]. At the most basic level, information and advice for weight loss, exercise, and lifestyle alterations are important, although self-management education alone has shown no to small improvements in individuals with knee OA [11]. Education combined with exercise and weight loss appears to be much more beneficial in the long term and result in cost efficiencies such as reduced medical visits and other health care costs after 12 months due to improved self-management [15].
Individuals with knee OA often have co-morbidities such as cardiovascular disease and diabetes along with hypertension and obesity that all have strong evidence supporting exercise [16]. Recommended guidelines for activity in individuals with knee OA include 20–30 min of moderate-intensity activities three times per week. However, this falls short for more recent minimum guidelines for all adults needed to prevent heart disease and diabetes and achieve health benefits [16, 17]. Using any mode of exercise, programs that include more frequent exercise three or more days per week have been found to reduce pain and disability more than programs less than 2 days per week [18••]. Regardless of the guidelines, individuals with knee OA often do not meet the minimum recommended amount of activity for older adults for primary or secondary prevention of cardiovascular disease and diabetes. Reduced fitness levels and increased obesity often indirectly increase the challenges for functional and recreational activities in these individuals. Advanced non-surgical interventions such as injections or surgery including joint preserving techniques or partial and total joint replacement techniques are common but recommended only when other more conservative approaches such as exercise have been exhausted [9].
The role of exercise in the disease process and progression of OA has conflicting results in the literature. Adverse events in the performance of exercise are rare for most individuals and do not limit participation in exercise [19]. Multiple studies show that individuals who have had an active lifestyle do not increase the risk for OA and even have less radiologic evidence of OA [20–24]. Individuals who perform resistance exercise particularly focusing on knee extensors and hip abductors have been shown to decrease the development of knee OA [25–27]. However, there is some evidence that elite athletic activity [22, 28] and even some recreational exercise [29] can increase the risk of developing knee OA.
The main goals for exercise in individuals with OA are to reduce pain; improve physical fitness capacity and endurance measures; and increase function and participation in work, recreation, and social activities. Specifically for knee OA, exercise has found to be beneficial [30]. A review by Jull et al. [18••] found that overall pooled standard mean difference (SMD) for pain reduction in patients with knee OA due to exercise was 0.50 (95 % CI 0.39, 0.62; P < 0.001). In addition, they found that the effect size transformed into a VAS (0–100 mm) for exercise to reduce pain was 8.5 mm (95 % CI 6.5, 10.5) and to reduce disability was 8.3 mm (95 % CI 5.9, 10.7). The number needed to treat (NNT) was estimated to be six patients for pain reduction (95 % CI 5, 7) and six patients for disability reduction (95 % CI 5, 8). Additionally, a Cochrane Review identifying 32 studies including over 3500 individuals with knee OA found platinum level evidence that there is at least short-term benefit in reduced knee pain and improved physical function with exercise [31]. A moderate treatment benefit was found with effect sizes of 0.40 (95 % CI 0.30–0.50) for pain and 0.37 (95 % CI 0.25–0.49) for physical function. The treatment effect for pain in these study populations was comparable to that reported for NSAIDs but with better functional gains and less side effects [32]. A separate review by Bosomworth [33] evaluating an additional 25 studies found that exercise did not increase the rate of progression of knee OA compared to those who had knee OA and did not exercise. In addition, this review highlighted the lower incidence of musculoskeletal pain and disability along with an increased functional capacity in the individuals with knee OA who exercised.
Across the many studies that include exercise as a conservative approach to management of knee OA, the mode or type and the dosage of exercise vary. A systematic review by Smith [34•] found that exercise is superior to no exercise in knee OA; however, exercise modes and intensities did not have statistically different functional outcomes. A recent meta-analysis found that similar effects on pain and disability can be seen with most modes of exercise including cardiovascular, resistance, and performance or neuromuscular control-type exercise [18••]. In a recent Cochrane review by Fransen et al. [35••], statistically significant pooled effects were found from exercise intervention for physical function immediately (SMD of 0.52, 95 % CI 0.39 to 0.64) and in 2–6 months post-intervention (SMD 0.15, 95 % CI 0.04 to 0.26), pain 2–6 months post-intervention (SMD 0.24, 95 % CI 0.14 to 0.35), and quality of life immediately post-intervention (SMD of 0.28, 95 % CI 0.15 to 0.40). Ulhman et al. [30] in a meta-analysis found that there was a slight benefit from resistance training in addition to exercises improving flexibility and aerobic capacity. In another meta-analysis by Juhl et al. [18••], the best results for outcomes of pain and disability were found when using one type of exercise as compared to mixing two or more modes during the same session SMD for pain 0.45(95 % CI 0.20, 0.69; P < 0.001) and SMD for disability 0.36 (95 % CI 0.13, 0.58; P < 0.002). A high adherence to exercise has been reported to be important to improve outcomes [19]. Overall, exercise has been found to have good, but primarily short term, benefits for the individual with knee OA, indicating that successful integration and adoption of exercise to an individual’s life are important for long-term management [35••, 36]. With abundant evidence that exercise is beneficial for persons with knee OA, this review focuses on both the type of exercise and optimal dosage parameters identified in the literature to assist clinicians in developing management strategies to achieve improved outcomes.
General considerations for exercise in individuals with knee OA need to include longer warm-up and cooldown times. Guidelines suggest that both warm-up and cooldown include cardiovascular activity sustained for 5 to 10 min in length [37]. Proper foot wear that has higher levels of stability and cushioning should be used to avoid any additional aggravating factors during exercise. More recently, footwear with higher levels of cushioning is available and individuals with knee OA may find these options beneficial. At the least, poor quality or well-worn footwear should be avoided during exercise, although this consideration may be a financial barrier to exercise for some individuals. Impact activities are suggested to be avoided. Progression of exercise intensity and mode is important to successful adoption of exercise programs by individuals who were previously sedentary or have low fitness levels. Often, individuals with knee OA can participate in many different activities if they have increased their activity tolerance over an extended time. If an individual is experiencing a flare up, severe joint pain or is obese, it is often recommended to start exercise in water or in non-weight-bearing modes of exercise. These load reduced modes can help progress an individual’s physiologic tolerance without limiting joint aggravation or irritation. Weight loss has also been found to be an important component and should be encouraged through diet as well as exercise [38]. Some evidence cites joint pain, joint effusion, and apprehension to be key problems for exercise tolerance and exercise adherence [15, 39–45]. It is common for individuals with knee OA to experience joint pain during or after an exercise session. If joint pain continues after exercise greater than 2 h, it is recommended that the exercise parameters such as mode, intensity, and duration be altered for future sessions [37]. When educated about the benefits of exercise and improving coping behaviors, often, individuals with knee OA can improve their self-efficacy for exercise and beliefs related to pain management [15].
Cardiovascular Exercise
Outcomes with Cardiovascular Exercise
Cardiovascular or aerobic exercise has been found to provide benefit for individuals with knee OA. Zhang et al. [46] performed pooled effect sizes for pain relief and disability from cardiovascular exercise and found moderate effects for pain (ES = 0.52; 95 % CI 0.34, 0.70) and disability (ES = 0.46; 95 % CI 0.25, 0.67). In general, outcomes of cardiovascular training improve physical function and reduce pain. Several studies have found that cardiovascular exercise is as beneficial to the pain relief seen with NSAIDs [18••, 32]. Specifically, Jull et al. [18••] found that for every additional ten supervised cardiovascular exercise sessions, the effect size for pain was increased by more than 0.2, comparable to the pain relief seen with acetaminophen for knee OA. Short- and long-term gait function is reported to improve with cardiovascular exercise [19]. An additional systematic review investigating only cardiovascular exercise found that across 12 clinical trials, the overall benefits of cardiovascular training include reduced pain and joint tenderness with improved functional status and respiratory capacity [47]. There are mixed reviews on the psychological benefits or health perception changes from cardiovascular exercise with some identifying no benefits [19] and others noting improvements [48, 49].
Specific outcomes in a number of clinical trials that used cardiovascular exercise as the primary exercise have found beneficial effects of cardiovascular exercise alone. Outcomes in Ettigner et al. [50] found individuals who participated in a 3-month supervised plus 15-month home walking program had small, but significant improvements in self-reported disability, peak VO2, pain, 6-min walk test (6MWT) distance, stair time, and physical performance measures. A significant protective effect was found for ADL disability for individuals who participated in the same 3-month supervised plus 15-month home walking program [51]. Kovar et al. [52] found significant effects for pain, 6MWT distance, and self-reported function after 8-week walking exercise plus health education as compared to a control group receiving only health education. Bautch et al. [53] found that those walked at low to moderate intensity on a treadmill for 12 weeks had significant reductions in pain compared to controls but no change in biologic markers of collagen matrix at the knee. Further, cardiovascular exercise was found to not cause disease progression in knee OA [53, 54]. Several studies have evaluated exercise groups in comparison to controls who perform no exercise. The exercise groups result in better outcomes in pain, physical performance, quality of life, and disability measures than those who did no exercise activity [50, 51, 55–57]. In addition, lack of exercise or physical activity is actually detrimentally resulting in increased joint stress owing to weakened muscles and joint structures, thinning of cartilage, oxidative stress, increased low grade inflammation, and decreased synovial fluid production [58–60]. All of these factors can further contribute to the development and progression of OA. Evcik et al. [61] found improvements in pain, disability, and quality of life for those who participated in a low-intensity and low-duration home walking program for 3 months. Minor et al. [62] found a significant effect on aerobic capacity but did not find a significant effect for disability and pain for participants with knee OA performing 12 weeks of either walking or aquatic exercise. Swimming and cycling has been found to increase vascular function in individuals with lower extremity OA [63]. In addition, walking programs have been shown to improve psychological functioning [64]. Finally, cycling has been found to be beneficial to improve pain, stiffness, preferred gait velocity, aerobic capacity, timed chair rise, 6MWT, and self-rated ADL performance [65, 66].
Dosage with Cardiovascular Exercise
Guidelines for persons with OA support cardiovascular exercise that is at least 20–30 min a day for three or more days of the week at low to moderate intensities [46]. Since more recent guidelines of the American Heart Association and American College of Sports Medicine support the need for exercise in adults to be at a minimum of 30 min 5 days/week at moderate intensities for cardiovascular health, some of the previous evidence may not be dosing cardiovascular exercise for individuals with knee OA at appropriate levels for health [16, 17]. Determining what is moderate-intensity cardiovascular exercise for each individual is important since individuals can be at different physical fitness states regardless of age. It is important that older adults with knee OA recognize and participate in cardiovascular activities with these minimal durations and intensities to prevent more life-threatening morbidity and mortality due to cardiovascular disease (see Table 1) [17].
Cardiovascular exercise using walking has been recommended for individuals who have knee OA to manage pain [46]. Walking is a safe and easy exercise for individuals with knee OA to perform either on land or with the use of a treadmill. Often, individuals with knee OA self-select lower intensities and clinicians underestimate their client’s cardiovascular systems resulting in diminished abilty to increase cardiovascular capacity. To avoid this, proper intensity dosing is recommended. Direct evidence on cardiovascular exercise in individuals with knee OA has shown that walking programs are safe and effective at moderate to vigorous intensities of 50–70 % of heart rate reserve (HRR) [38, 50, 56]. When using the HRR method, 40–60 % of HRR is moderate intensity and over 60 % HRR is vigorous. Lower intensities have been used in the literature including self-pacing and intensities up to 40–60 % HR max [53, 67, 68]. A submaximal aerobic capacity test provides a more accurate method to dose cardiovascular exercise. For example, Bautch et al. [53] used the Balke protocol in subjects with knee OA. This test and others have been validated and can easily be applied to this population.
Duration has also been evaluated for walking programs. Several studies used an aerobic initiation period of one to two sessions for a week to increase walking duration from 10 to 15 min up to 30–40 min [38, 50, 56, 61, 69]. One study used baseline number of daily steps as a starting point and increased the number of steps by 10 % every 4 weeks [68]. All these studies reported maintained and reduced pain in the participants over the course of the study [50, 53, 56, 61, 69, 70]. Only one study found that if an individual was obese (BMI ≥30) and the baseline number of steps was <10,000 on average, individuals had increased pain with walking, and therefore, walking may not be the preferred mode of cardiovascular exercise [69].
Cycling has also been found to be beneficial for cardiovascular exercise. Individuals with knee OA tolerate upright bicycles well, but those with reduced balance may prefer recumbent cycling. The literature supports cycling exercise at intensities of 40–70 % HRR (moderate to vigorous) or 70–75 % of HR max (high end of moderate) [63, 65, 66]. The duration of cycling exercise seems to extend slightly longer than walking programs with the time ranging from 20 up to 60 min [63, 65, 66].
Aquatic exercise has been used to perform cardiovascular training, although aquatic programs are often multimodal in nature and difficult to determine the cardiovascular exercise prescription. One study used music at 125 bpm for 40 min and a series of rhythmic movements such as bounces, knee jogging, kicks, ankle reaches, twists, steps and crosses, leaps, rocks, scissors, jumping jacks, and slide steps to maintain elevation of the cardiovascular system in aquatic sessions [49]. Swimming has been used 20 to 30 min/day progressing to 40 to 45 min, 3 days/week at an intensity of 40 to 50 % of HRR progressing to 60 to 70 % of HRR [63]. Another study looked at aquatic treadmill walking at a self-paced speed for 20 min in comparison to land treadmill walking [71]. In this study, both aquatic and land treadmill walking had similar benefits, but the aquatic walking program had additional benefits in joint angular velocity and pain reduction.
Resistance Exercise
Outcomes with Resistance Exercise
Resistance training can have important effects on body composition, strength, and power that are independent of age [72]. A number of exercise trials for persons with OA report a strengthening component in the intervention [40, 50, 57, 64, 73–77, 78••]. The heterogeneity of resistance training programs makes identifying significant dosage parameters difficult, and in a recent meta-analysis, only programs focusing on quadriceps strength showed an effect on pain and disability [18••]. Quadriceps strengthening, in particular, is recommended for individuals who have knee OA [46]. Wang et al. [19] performed a systematic review with nine RCTs and found significant effects from resistance training for pain, function, and gait but no significant effects for disability or quality of life. Zhang et al. [46], in a separate systematic review, performed pooled effect sizes for pain relief and disability from muscle strengthening exercise and found moderate effects for pain (ES = 0.32, 95 % CI 0.23, 0.42) and disability (ES = 0.32, 95 % CI 0.23, 0.41). Lange and Vanwanseele [79] performed a systematic review specifically related to strength training in persons with knee OA. They summarize significant outcomes across studies comparing strength training to a control group improve pain, stiffness, quality of life, self-efficacy, depression, strength outcomes, ROM outcomes, walking endurance, walk time and speed, stair climb, and sit-to-stand ability.
Specific studies identifying older adults with knee OA show improved outcomes after training that uses resistance exercises dosed at a variety of parameters. Non-weight-bearing positions and loads have been reported to be superior to weight bearing with resistance training in knee OA [80]. Outcomes have shown individuals improving strength, muscle mass, power [39, 50, 64, 73, 79, 81–87], and decreased stiffness [50, 64, 73, 81–84] after performing resistance exercise. Individuals also have short-term decreased pain with resistance exercise [50, 64, 73, 80–83, 88–90]. Moderate- to high-intensity loads two to three times a week have been found to be even more effective at reducing pain in individuals with knee OA [91]. Combined physical and psychosocial measures such as the Osteoarthritis Severity Index (OASI) [73], SF-36 [81], WOMAC [39, 81, 85, 86], Arthritis Impact Measurement Scale (AIMS) [73, 81], and Arthritis Self-Efficacy (ASE) [39] scores have all been found to improve with resistance exercise. A variety of functional tests have improved after resistance exercise such as chair rise, gait speed, stair climb, and TUG [39, 50, 64, 73, 81–86, 90, 92].
Improved function also has resulted in reduced fall risk and decreased number of falls [92]. Individuals with knee OA have reported decreased depressive symptoms [73, 81] and improved quality of life [90, 93] with resistance training. Even comorbid conditions have improved with disease severity measures such as reduced cardiovascular disease risk, increased insulin uptake, improved bone density, and improved energy metabolism [79].
There is no current evidence that the type of resistance exercise—isotonic, isometric, or isokinetic—influences outcome [47]. Dynamic or isotonic training is the most common exercise intervention reported in strength training trials using machines, free weights, and resistance bands [79]. The functional benefits from isometric resisted exercises are limited to a 10- to 15-degree range from the joint angle exercised [94]. In open chain isotonic exercise, often, the quadriceps are targeted in knee extension exercises, but this approach misses the strength and stability training in the hip and ankle needed for closed chain functional activities. In addition, closed-chain activities need strengthening and endurance of not only the lower extremity musculature but also the trunk and pelvic musculature that work synergistically in functional motions such as rising from a chair.
Few studies have evaluated the effect of resistance exercise on the disease progression of knee OA. Mikesky et al. [87] investigated if a 30-month program of resistance training with an emphasis on quadriceps and hamstring strengthening in comparison to ROM exercises had an effect on the radiographic disease progression in individuals with knee OA. They found no significant difference in radiographs pre- and post-intervention between the treatment groups, demonstrating that resistance training does not increase joint changes or disease progression.
Resistance Exercise Dosage
All types of resistance exercise can be used effectively. The frequency, intensity, time, and type (FITT) parameters for resistance training exercise programs with individuals with knee OA have varied. Most research training programs follow strength training guidelines [16] for two to three times/week, although the range has been reported between one and seven times per week [42, 79, 95–99]. Caution must be used when interpreting strength training programs that are performed on consecutive days (>3–4 days/week). Often, these programs are capturing muscle endurance gains and not increasing the physiologic force capacity of the neuromuscular system (see Table 1 for general FITT parameters for resistance training).
The duration of within exercise session and length of training can also have an effect on the outcomes of the study. Lange et al. [79] report within-session durations lasting from 10 to 60 min. The average duration or length of programs is between 1 and 6 months [79]. Of these programs, the duration of training has been 4 weeks [100, 101], 6 weeks [96], 8 weeks [95, 97], 12 weeks [98], 26 weeks, and even up to 30 months [42, 79]. The shorter-duration programs with good outcomes may be more relevant for clinicians as a 6–8-week program would be able to be accomplished in an average outpatient setting. However, if an individual was in a health care facility or in a community center where they might be followed for longer periods of time intermittently, the longer duration programs would be beneficial particularly to maintain improved outcomes seen with resistance exercise.
When prescribing resistance exercise for individuals with knee OA, a variety of intensities have been used in the literature. Heavier loads in a strength training range of 60–80 % of one repetition maximum (1RM) have been shown to have optimum outcomes and have been well tolerated by participants [42, 95, 97, 98, 102, 103]. When performing muscle capacity testing, individuals should fatigue to the point that they cannot perform another repetition. If they fatigue at 8–12 repetitions, they should be in the 80 to 60 % of 1RM range, respectively [104]. Studies occasionally use a ten-repetition maximum test to determine maximal capacity. Theoretically, if the participant truly fatigued at repetition no. 10 and unable to do no. 11, then, this should have been at 70 % of their 1RM. However, many self-limit due to predetermined repetitions rather than actual physiologic capacity using this method. Determining a one repetition maximum will assist in accurately prescribing intensity.
A few programs have used muscle endurance parameters such as repetitions to fatigue, greater than 12 repetitions (<60 % 1RM), using body weight or lighter loads that effectively work the individual at <60 % of 1RM [50, 105]. A few other studies have shown gains with resistance training at low loads such as 10 % of 1RM [97], 10 % of body weight [86], or muscle endurance type exercise where the participants do not reach a maximal fatigue point [106]. Gains made at these lower intensities generally are seen in individuals who are inactive or untrained [107].
Balance and Neuromuscular Control Exercise
Outcomes with Balance and Neuromuscular Control Exercise
Individuals with knee OA have a loss of muscle function beyond force-generating capacity. Muscles in the lower extremities have also been found to have lost sensorimotor capabilities that impact functional performance [108]. Proprioception involving the muscle spindles, Golgi tendon organs, and articular and cutaneous proprioceptors can all be impaired altering the proprioceptive acuity of the muscle. Maintaining intact control of the sensorimotor systems is essential in balance and coordination activities found in gait and other functional activities [109]. Incorporating balance, coordination, and other neuromuscular control-type exercises has been advocated, although few studies have incorporated this exercise mode (see Table 1 for general FITT parameters for balance and neuromuscular control exercises).
Tai Chi Exercise: Outcomes and Dosage
There have been a variety of programs investigating balance-type exercise focusing on motor control, agility, and perturbation training. One type of exercise that includes all of these that has been investigated in multiple studies is tai chi [110–114]. Tai chi is becoming a more popular exercise in older adults due to its focus on slow gentle movements, constant weight shifting, body weight-loaded postures, and deep controlled breathing techniques. The weight shifting in loaded postures is believed to help to improve neuromuscular control in individuals with knee OA. A systematic review of three RCTs using tai chi as exercise found that participating in tai chi improved composite functional scores over 3 months, but there were no significant effects for pain and disability in individuals with knee OA [19]. In individual trials, tai chi has been reported to improve gait velocity and functional measures in older adults [110]. Other outcomes have been reported in individual studies using tai chi in pain, function, balance, flexibility, strength of knee extension, aerobic capacity, and the reduced occurrence of falls in community-dwelling older adults and specifically those with OA [110, 114, 115].
In the literature, the use of tai chi as an exercise program entails performing 24-form Yang-style method. A systematic review reports performing this 24-form method five times in sequence at a rate of approximately 6 min per full sequence for a total of 30 min [110]. Across the previous studies, benefits have been found from performing tai chi two to four times/week for duration of 12–48 weeks [111–114].
Balance and Neuromuscular Control Exercise: Outcomes and Dosage
Other types of balance exercises have focused on coordination, agility, and perturbation training. This includes standing balance [40], multi-directional stepping [116], and multi-directional walking tasks such as side stepping, braiding, forward and backward walking with crossover steps, shuttle walking, multi-directional changes on cue when walking, and manual perturbations while on foam, balance board, roller board [117, 118]. In addition, functional dynamic balance exercises such as sit to stand and step ups or static balance exercises such as single-leg stance have been used [118]. Outcomes using a functional dynamic balance exercise program found that patients were able to perform the aggregate functional performance testing in less time than the control group [118]. A separate study looked at the effects of closed kinetic chain exercise with individuals with knee OA at higher loads and found beneficial outcomes of improved lower extremity muscle co-activation, improved transfer of motor learning, and heightened postural reactions [119].
Specific dosage was given in Hurley and Scott [118] performing each of the static, dynamic, and multi-directional exercises for 1 minute with the goal of progressively increasing repetitions during this time as well as increasing the challenge of the exercise by changing parameters such as surfaces or heights. Chaipinyo and Karoonsupcharoen [116] had four balance stepping exercises performed for 30 repetitions and three sets with 10 repetitions of mini squats in between each exercise. Other studies did not specify dosage parameters [40]. The frequency varied and the performance of the exercises was reported at two times/week [40, 118] to five times/week [116] for 5 weeks [118] up to 3 months [40]
A few studies emphasized motor control target tasks with individuals with knee OA. One study looked at a seated foot-and-leg task to target using a computer-simulated interface that heightened proprioceptive inputs by matching spatial and speed targets [97, 120]. This proprioceptive task was compared to closed kinetic chain exercises at 10–25 % of body weight using a sled-type machine where each was performed for 20 min three times per week for 6 weeks. There were no significant differences between the groups, and both groups improved outcomes illustrating that both lower extremity target tasks and light body weight exercise dosed for muscle endurance have beneficial effects for motor control with individuals with knee OA.
Multi-Modal Exercise
Outcomes with Multi-Modal Exercise
Reporting on the exact exercises and dosage of multi-modal exercise programs is varied and often difficult to replicate from the literature. Generally, multi-modal exercise will include some form of cardiovascular and resistance exercises along with other types of exercise that can include balance and flexibility-type exercises. A meta-analysis by Jull et al. [18••] found that exercise programs with a combination of cardiovascular, resistance, and performance or neuromuscular control-type exercise were not significantly better than control treatments for pain with a SMD of 0.16 (95 % CI 0.04, 0.37; I2 = 44.0 %), but there was a small effect reducing disability with a SMD of 0.22 (95 % CI 0.08, 0.37; I2 = 0 %). It is possible that the different modes of exercise have competing effects as discussed by Jull et al. [18••] and/or that the duration and intensity in session when using mixed modes are not high enough for any one mode to result in measurable changes across the studies.
As mentioned earlier, aquatic exercise is often multi-modal including cardiovascular, resistance, and flexibility components. A 2007 Cochrane Review of aquatic exercise for hip and knee OA found that aquatic exercise in the short term has small but statistically significant effect on function, quality of life, and mental health when compared to control groups [36]. Overall, this systematic review found that there are very few randomized controlled trials investigating the effects of aquatic exercise on knee or hip OA. A recent systematic review found that aquatic exercise has a small but significant effect on reducing disability but no effect on pain or quality of life [19]. Moreover, there is not a clear identification of what type of exercise and dose (intensity, frequency, and duration) that can best be applied using aquatic exercise with OA.
One study by Wyatt et al. [121] found a large significant effect for pain reduction in favor of aquatic exercise in the short term when compared to land-based exercise. Another study found significant quality of life improvements with regular aquatic exercise compared to controls [6]. Two studies reported that neither land-based nor aquatic exercise increased self-reported pain or other symptoms in individuals with knee or hip OA [39, 110], and one study reported that those who dropped out did not drop due to the exercise intervention causing problems [122]. No study found an improvement in walking ability or stiffness. One study looked at a 6-month follow-up of aquatic exercise and found that short-term improvements were not maintained and recommended that aquatic exercise be either continued or transferred to land-based exercise that may be easier and cheaper for individuals to be started and maintained [122].
Multimodal Exercise: Dosage
There are a few studies that use a multi-modal exercise program for individuals with knee OA. The Arthritis Foundation developed a People with Arthritis Can Exercise (PACE) program that includes a 60-min flexibility, balance, and cardiovascular training class, which describes exercises but not dosages for exercise [123]. Wang et al. [124] used the PACE program to evaluate a multi-modal program for individuals with knee OA. They had subjects perform a series of exercises three times/week for 12 weeks and found good outcomes including decreased pain, improved quality of life, increased ROM, and greater 6MWT distance. Several studies have used both cardiovascular and resistance exercises together in an exercise program [40, 45, 56, 77, 118, 125]. Messier et al. [125] used two 15-min walking sessions at 50–75 % HRR at the beginning and end of a 45-min exercise session with 15 min of resistance training including two sets at 12 repetitions of leg extension, leg curl, heel raise, and step ups using either cuff weights of weighted vest. There was no indication of what percent of maximal capacity that these resistance exercises were dosed; however, the researchers state that the weight load was increased every 2–3 weeks.
Finally, multi-modal exercises involving aquatic exercise training use a variety of dosages [124, 126, 127]. Most commonly, these programs have used the Arthritis Foundation Aquatics Program (AFAP) that includes a 60-min class emphasizing movement of most large muscles and joints of the body in a chest depth to emphasize ROM, multi-planar resistance, balance, coordination and cardiovascular training [124, 128]. Studies using the AFAP program or similar type programs have found good outcomes when individuals with knee OA perform the program two to three times/week for 12 weeks up to 12 months in a pool at 84–87 °F [124, 126–128].
Negative Effects of Exercise
There has been little other evidence showing detrimental effects found from any exercise in individuals with knee OA. One early study indicated that resistance exercise for strength gains could increase the OA progression if the individual has a varus malalignment higher than five degrees [129]. The effects of knee varus angle continue to be studied but are associated with the risk and progression of knee OA particularly in individuals who are overweight and obese [130, 131]. One early land-based study using resistance, flexibility, balance, and coordination for patients with knee OA indicated an increase in knee edema following exercise with several subjects, although it did not prevent exercise participation and no subjects dropped out from adverse effects of exercise [40]. Several RCTs have reported minor adverse events with exercise including back, hip, and knee pain [39, 41–45]. In all instances, individuals with knee OA have been able to continue and progress with exercise with minor modifications, increased physical tolerance, and reduced pain.
Conclusions
Exercise is beneficial for individuals with knee OA to improve function, reduce pain, minimize disability, decrease depression symptoms, and enhance quality of life. According to the literature, many types of exercise are effective in achieving positive outcomes in individuals with knee OA including cardiovascular, resistance, balance, and multi-modal exercise. Understanding the specific benefits of each type of exercise assists therapists in selecting the most appropriate exercise given an individual client’s situation. Further, insight gained from the literature into recommended parameters for exercise prescription allows therapists to prescribe the most efficacious, evidence-based exercise for clients. More research is needed to further elucidate optimal exercise prescription for individuals with knee OA, but current literature provides a strong foundation on which to build.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Felson DT. Risk factors for osteoarthritis: understanding joint vulnerability. Clin Orthop Relat Res. 2004;427:S16–21.
Cisternas MG, Murphy L, Sacks JJ, Solomon DH, Pasta DJ, Helmick CG. Alternative methods for defining osteoarthritis and the impact on estimating prevalence in a US population based survey. Arthritis care & research 2015.
Hootman JM, Helmick CG, Barbour KE, Theis KA, Boring MA. Updated projected prevalence of self-reported doctor diagnosed arthritis and arthritis attributable activity limitation among US adults, 2015–2040. Arthritis & rheumatology 2016.
Deshpande BR, Katz JN, Solomon DH, Yelin EH, Hunter DJ, Messier SP et al. The number of persons with symptomatic knee osteoarthritis in the United States: impact of race/ethnicity, age, sex, and obesity. Arthritis care & research 2016.
Showery J, Kusnezov N, Dunn JC, Bader JO, Belmont PJ, Waterman BR. The rising incidence of degenerative and post-traumatic osteoarthritis of the knee in the United States military. The Journal of Arthroplasty 2016.
Patrick DL, Ramsey SD, Spencer AC, Kinne S, Belza B, Topolski TD. Economic evaluation of aquatic exercise for persons with osteoarthritis. Med Care. 2001;39(5):413–24.
Glass G. Osteoarthritis. Disease-A-Month: DM [Dis Mon]. 2006;52(9):343–62.
Jordan JM, Luta G, Renner JB, Dragomir A, Hochberg MC, Fryer JG. Ethnic differences in self-reported functional status in the rural south: the Johnston County Osteoarthritis Project. Arthritis Rheum. 1996;9(6):483–91.
Dieppe PA, Lohmander LS. Pathogenesis and management of pain in osteoarthritis. Lancet. 2005;365(9463):965–73.
Rothfuss Jr, Mau W, Zeidler H, Brenner MH. Socioeconomic evaluation of rheumatoid arthritis and osteoarthritis: a literature review. Proceedings of the Seminars in arthritis and rheumatism: Elsevier; 1997.
Rodriguez-Merchan EC. Conservative treatment of acute knee osteoarthritis: a review of the Cochrane Library. Journal of Acute Disease 2016.
Miyagawa H, Ikemoto T, Honjo H, Akao M, Tsujimoto T, Ushida T. One-year results of voluntary-based supervised exercise or treatment at orthopedic clinic for radiographic severe knee osteoarthritis. J Phys Ther Sci. 2016;28(3):906–10.
Fitzgerald G, Fritz J, Childs J, Brennan G, Talisa V, Gil A et al. Exercise, manual therapy, and use of booster sessions in physical therapy for knee osteoarthritis: a multi-center, factorial randomized clinical trial. Osteoarthritis and Cartilage 2016.
French H, Brennan A, White B, Cusack T. Manual therapy for osteoarthritis of the hip or knee; a systematic review. Man Ther. 2011;16(2):109–17.
Gay C, Chabaud A, Guilley E, Coudeyre E. Educating patients about the benefits of physical activity and exercise for their hip and knee osteoarthritis. Systematic literature review. Annals of Physical and Rehabilitation Medicine 2016.
Haskell WL, Lee I-M, Pate RR, Powell KE, Blair SN, Franklin BA, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1081.
Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1094.
Juhl C, Christensen R, Roos EM, Zhang W, Lund H. Impact of exercise type and dose on pain and disability in knee osteoarthritis: a systematic review and meta-regression analysis of randomized controlled trials. Arthritis Rheumatol. 2014;66(3):622–36. Supervised exercise performed 3 times a week is optimal for individuals with knee OA. Exercise modes performed independently show higher benefit than mixed modes.
Wang S-Y, Olson-Kellogg B, Shamliyan TA, Choi J-Y, Ramakrishnan R, Kane RL. Physical therapy interventions for knee pain secondary to osteoarthritis: a systematic review. Ann Intern Med. 2012;157(9):632–44.
White J, Wright V, Hudson A. Relationships between habitual physical activity and osteoarthrosis in ageing women. Public Health. 1993;107(6):459–70.
Felson DT, Niu J, Clancy M, Sack B, Aliabadi P, Zhang Y. Effect of recreational physical activities on the development of knee osteoarthritis in older adults of different weights: the Framingham Study. Arthritis Care Res. 2007;57(1):6–12.
Spector TD, Harris PA, Hart DJ, Cicuttini FM, Nandra D, Etherington J, et al. Risk of osteoarthritis associated with long-term weight-bearing sports: a radiologic survey of the hips and knees in female ex-athletes and population controls. Arthritis Rheum. 1996;39(6):988–95.
Chakravarty EF, Hubert HB, Lingala VB, Zatarain E, Fries JF. Long distance running and knee osteoarthritis: a prospective study. Am J Prev Med. 2008;35(2):133–8.
Hunter DJ, Eckstein F. Exercise and osteoarthritis. J Anat. 2009;214(2):197–207.
Slemenda C, Heilman DK, Brandt KD, Katz BP, Mazzuca SA, Braunstein EM, et al. Reduced quadriceps strength relative to body weight: a risk factor for knee osteoarthritis in women? Arthritis Rheum. 1998;41(11):1951–9.
Hootman JM, FitzGerald SJ, Macera CA, Blair SN. Lower extremity muscle strength and risk of self-reported hip or knee osteoarthritis. J Phys Act Health. 2004;1(4):321.
Chang A, Hayes K, Dunlop D, Hurwitz D, Song J, Genge R, et al. Thrust during ambulation and the progression of knee osteoarthritis. Arthritis Rheum. 2004;50(12):3897–903.
Michalsson K, Byberg L, Ahlbom A, Melhus H, Farahmand BY. Risk of severe knee and hip osteoarthritis in relation to level of physical exercise: a prospective cohort study of long-distance skiers in Sweden. PLoS One. 2011;6(3):e18339.
Szoeke C, Dennerstein L, Guthrie J, Clark M, Cicuttini F. The relationship between prospectively assessed body weight and physical activity and prevalence of radiological knee osteoarthritis in postmenopausal women. J Rheumatol. 2006;33(9):1835–40.
Uthman OA, van der Windt DA, Jordan JL, Dziedzic KS, Healey EL, Peat GM, et al. Exercise for lower limb osteoarthritis: systematic review incorporating trial sequential analysis and network meta-analysis. BMJ. 2013;347:f5555.
Fransen M, McConnell S. Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev 2008;4(4).
Zhang W, Doherty M, Peat G, Bierma-Zeinstra SM, Arden N, Bresnihan B et al. EULAR evidence based recommendations for the diagnosis of knee osteoarthritis. Annals of the rheumatic diseases 2009.
Bosomworth NJ. Exercise and knee osteoarthritis: benefit or hazard? Can Fam Physician. 2009;55(9):871–8.
Smith T, Kirby E, Davies L. A systematic review to determine the optimal type and dosage of land-based exercises for treating knee osteoarthritis. Phys Ther Rev. 2014;19(2):105–13. Exercise modes and intensities do not have significantly different outcomes across studies.
Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL. Exercise for osteoarthritis of the knee: a Cochrane systematic review. Br J Sports Med. 2015;49(24):1554–7. Land-based exercise modes provide 2–6 month short-term benefits.
Bartels EM, Lund H, Hagen KrB, Dagfinrud H, Christensen R, Danneskiold-Samsoe B. Aquatic exercise for the treatment of knee and hip osteoarthritis. Cochrane Database Syst Rev 2007;4.
Medicine ACoS. ACSM’s guidelines for exercise testing and prescription. Lippincott Williams & Wilkins; 2013.
Messier SP, Mihalko SL, Legault C, Miller GD, Nicklas BJ, DeVita P, et al. Effects of intensive diet and exercise on knee joint loads, inflammation, and clinical outcomes among overweight and obese adults with knee osteoarthritis: the IDEA randomized clinical trial. JAMA. 2013;310(12):1263–73.
Foley A, Halbert J, Hewitt T, Crotty M. Does hydrotherapy improve strength and physical function in patients with osteoarthritis; a randomised controlled trial comparing a gym based and a hydrotherapy based strengthening programme. Ann Rheum Dis. 2003;62(12):1162–7.
Rogind H, Bibow-Nielsen B, Jensen B, Moller HC, Frimodt-Moller H, Bliddal H. The effects of a physical training program on patients with osteoarthritis of the knees. Arch Phys Med Rehabil. 1998;79(11):1421–7.
Bennell K, Hinman R, Metcalf B, Buchbinder R, McConnell J, McColl G, et al. Efficacy of physiotherapy management of knee joint osteoarthritis: a randomised, double blind, placebo controlled trial. Ann Rheum Dis. 2005;64(6):906–12.
Foroughi N, Smith RM, Lange AK, Baker MK, Singh MAF, Vanwanseele B. Lower limb muscle strengthening does not change frontal plane moments in women with knee osteoarthritis: a randomized controlled trial. Clinical Biomech. 2011;26(2):167–74.
Jan M-H, Lin C-H, Lin Y-F, Lin J-J, Lin D-H. Effects of weight-bearing versus nonweight-bearing exercise on function, walking speed, and position sense in participants with knee osteoarthritis: a randomized controlled trial. Arch Phys Med Rehabil. 2009;90(6):897–904.
Lim BW, Hinman RS, Wrigley TV, Sharma L, Bennell KL. Does knee malalignment mediate the effects of quadriceps strengthening on knee adduction moment, pain, and function in medial knee osteoarthritis? A randomized controlled trial. Arthritis Care Res. 2008;59(7):943–51.
Van Baar M, Dekker J, Oostendorp R, Bijl D, Voorn T, Lemmens J, et al. The effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a randomized clinical trial. J Rheumatol. 1998;25(12):2432–9.
Zhang W, Moskowitz R, Nuki G, Abramson S, Altman R, Arden N, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthr Cartil. 2008;16(2):137–62.
Pelland L, Brosseau L, Wells G, MacLeay L, Lambert J, Lamothe C, et al. Efficacy of strengthening exercises for osteoarthritis (part I): a meta-analysis. Phys Ther Rev. 2004;9(2):77–108.
Kelley GA, Kelley KS, Hootman JM. Effects of exercise on depression in adults with arthritis: a systematic review with meta-analysis of randomized controlled trials. Arthritis Res Therapy. 2015;17(1):21.
Kim I-S, Chung S-H, Park Y-J, Kang H-Y. The effectiveness of an aquarobic exercise program for patients with osteoarthritis. Appl Nurs Res. 2012;25(3):181–9.
Ettinger WH, Burns R, Messier SP, Applegate W, Rejeski WJ, Morgan T, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis: the Fitness Arthritis and Seniors Trial (FAST). JAMA. 1997;277(1):25–31.
Penninx BW, Messier SP, Rejeski WJ, Williamson JD, DiBari M, Cavazzini C, et al. Physical exercise and the prevention of disability in activities of daily living in older persons with osteoarthritis. Arch Intern Med. 2001;161(19):2309–16.
Kovar PA, Allegrante JP, MacKenzie CR, Peterson MG, Gutin B, Charlson ME. Supervised fitness walking in patients with osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 1992;116(7):529–34.
Bautch JC, Malone DG, Vailas AC. Effects of exercise on knee joints with osteoarthritis: a pilot study of biologic markers. Arthritis Rheum. 1997;10(1):48–55.
Bautch JC, Clayton MK, Chu Q, Johnson KA. Synovial fluid chondroitin sulphate epitopes 3B3 and 7D4, and glycosaminoglycan in human knee osteoarthritis after exercise. Ann Rheum Dis. 2000;59(11):887–91.
Thomas K, Muir K, Doherty M, Jones A, O’Reilly S, Bassey E. Home based exercise programme for knee pain and knee osteoarthritis: randomised controlled trial. BMJ. 2002;325(7367):752.
Rejeski WJ, Focht BC, Messier SP, Morgan T, Pahor M, Penninx B. Obese, older adults with knee osteoarthritis: weight loss, exercise, and quality of life. Health Psychol. 2002;21(5):419.
O’Reilly SC, Muir KR, Doherty M. Effectiveness of home exercise on pain and disability from osteoarthritis of the knee: a randomised controlled trial. Ann Rheum Dis. 1999;58(1):15–9.
Allison MA, Jensky NE, Marshall SJ, Bertoni AG, Cushman M. Sedentary behavior and adiposity-associated inflammation: the Multi-Ethnic Study of Atherosclerosis. Am J Prev Med. 2012;42(1):8–13.
Gleeson M, Bishop NC, Stensel DJ, Lindley MR, Mastana SS, Nimmo MA. The anti-inflammatory effects of exercise: mechanisms and implications for the prevention and treatment of disease. Nat Rev Immunol. 2011;11(9):607–15.
Petersen AMW, Pedersen BK. The anti-inflammatory effect of exercise. J Appl Physiol. 2005;98(4):1154–62.
Evcik D, Sonel B. Effectiveness of a home-based exercise therapy and walking program on osteoarthritis of the knee. Rheumatol Int. 2002;22(3):103–6.
Minor MA, Webel RR, Kay DR, Hewett JE, Anderson SK. Efficacy of physical conditioning exercise in patients with rheumatoid arthritis and osteoarthritis. Arthritis Rheum. 1989;32(11):1396–405.
Alkatan M, Machin DR, Baker JR, Akkari AS, Park W, Tanaka H. Effects of swimming and cycling exercise intervention on vascular function in patients with osteoarthritis. Am J Cardiol. 2016;117(1):141–5.
Penninx BW, Rejeski WJ, Pandya J, Miller ME, Di Bari M, Applegate WB, et al. Exercise and depressive symptoms a comparison of aerobic and resistance exercise effects on emotional and physical function in older persons with high and low depressive symptomatology. J Gerontol Ser B Psychol Sci Soc Sci. 2002;57(2):124–P32.
Salacinski AJ, Krohn K, Lewis SF, Holland ML, Ireland K, Marchetti G. The effects of group cycling on gait and pain-related disability in individuals with mild-to-moderate knee osteoarthritis: a randomized controlled trial. J Orthop Sports Phys Ther. 2012;42(12):985–95.
Mangione KK, McCully K, Gloviak A, Lefebvre I, Hofmann M, Craik R. The effects of high-intensity and low-intensity cycle ergometry in older adults with knee osteoarthritis. J Gerontol Ser A: Biol Sci Med Sci. 1999;54(4):M184–M90.
Hughes SL, Seymour RB, Campbell R, Pollak N, Huber G, Sharma L. Impact of the fit and strong intervention on older adults with osteoarthritis. The Gerontologist. 2004;44(2):217–28.
Talbot LA, Gaines JM, Huynh TN, Metter EJ. A home based pedometer driven walking program to increase physical activity in older adults with osteoarthritis of the knee: a preliminary study. J Am Geriatr Soc. 2003;51(3):387–92.
Toda Y. The effect of energy restriction, walking, and exercise on lower extremity lean body mass in obese women with osteoarthritis of the knee. J Orthop Sci. 2001;6(2):148–54.
Messier SP, Gutekunst DJ, Davis C, DeVita P. Weight loss reduces knee joint loads in overweight and obese older adults with knee osteoarthritis. Arthritis Rheum. 2005;52(7):2026–32.
Roper JA, Bressel E, Tillman MD. Acute aquatic treadmill exercise improves gait and pain in people with knee osteoarthritis. Arch Phys Med Rehabil. 2013;94(3):419–25.
Hunter GR, McCarthy JP, Bamman MM. Effects of resistance training on older adults. Sports Med. 2004;34(5):329–48.
Schilke JM, Johnson GO, Housh TJ, O’Dell JR. Effects of muscle-strength training on the functional status of patients with osteoarthritis of the knee joint. Nurs Res. 1996;45(2):68–72.
Peloquin L, Bravo G, Gauthier P, Lacombe G, Billiard J-S. Effects of a cross-training exercise program in persons with osteoarthritis of the knee a randomized controlled trial. JCR: J Clin Rheumatol. 1999;5(3):126–36.
Callaghan M, Oldham J. An evaluation of exercise regimes for patients with osteoarthritis of the knee: a single-blind randomized controlled trial. Clin Rehabil. 1995;9(3):213–8.
Borjesson M, Weidenhielm L, Elfving B, Olsson E. Tests of walking ability at different speeds in patients with knee osteoarthritis. Physiother Res Int. 2007;12(2):115–21.
Deyle GD, Henderson NE, Matekel RL, Ryder MG, Garber MB, Allison SC. Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee: a randomized, controlled trial. Ann Intern Med. 2000;132(3):173–81.
Escalante Y, Saavedra JM, Garcia-Hermoso A, Silva AJ, Barbosa TM. Physical exercise and reduction of pain in adults with lower limb osteoarthritis: a systematic review. J Back Musculoskelet Rehabil. 2010;23(4):175–86. The impact of exercise modes on cardiovascular fitness in individuals with OA is unknown and since exercise programs are heterogeneous, best dosage parameters are unclear. Land based exercise including tai chi, aerobic and mixed exercise provide the best results for individuals with lower extremity OA.
Lange AK, Vanwanseele B. Strength training for treatment of osteoarthritis of the knee: a systematic review. Arthritis Care Res. 2008;59(10):1488–94.
Tanaka R, Ozawa J, Kito N, Moriyama H. Efficacy of strengthening or aerobic exercise on pain relief in people with knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. Clin Rehabil. 2013;27(12):1059–71.
Eyigor S. A comparison of muscle training methods in patients with knee osteoarthritis. Clin Rheumatol. 2004;23(2):109–15.
Gur H, Cakin N, Akova B, Okay E, Kucukoglu S. Concentric versus combined concentric-eccentric isokinetic training: effects on functional capacity and symptoms in patients with osteoarthrosis of the knee. Arch Phys Med Rehabil. 2002;83(3):308–16.
Topp R, Woolley S, Hornyak J, Khuder S, Kahaleh B. The effect of dynamic versus isometric resistance training on pain and functioning among adults with osteoarthritis of the knee. Arch Phys Med Rehabil. 2002;83(9):1187–95.
Topp R, Boardley D, Morgan AL, Fahlman M, McNevin N. Exercise and functional tasks among adults who are functionally limited. West J Nurs Res. 2005;27(3):252–70.
Diracoglu D, Aydin R, Baskent A, Celik A. Effects of kinesthesia and balance exercises in knee osteoarthritis. JCR: J Clin Rheumatol. 2005;11(6):303–10.
Lin D-H, Lin Y-F, Chai H-M, Han Y-C, Jan M-H. Comparison of proprioceptive functions between computerized proprioception facilitation exercise and closed kinetic chain exercise in patients with knee osteoarthritis. Clin Rheumatol. 2007;26(4):520–8.
Mikesky AE, Mazzuca SA, Brandt KD, Perkins SM, Damush T, Lane KA. Effects of strength training on the incidence and progression of knee osteoarthritis. Arthritis Care Res. 2006;55(5):690–9.
Escalante Y, Saavedra JM, Garcia-Hermoso A, Silva AJ, Barbosa TM. Physical exercise and reduction of pain in adults with lower limb osteoarthritis: a systematic review. J Back Musculoskelet Rehabil. 2010;23(4):175–86.
Brosseau L, Pelland L, Wells G, Macleay L, Lamothe C, Michaud G, et al. Efficacy of aerobic exercises for osteoarthritis (part II): a meta-analysis. Phys Ther Rev. 2004;9(3):125–45.
Jorge RTB, de Souza MC, Chiari A, Jones A, Fernandes AdRC, Janior IL et al. Progressive resistance exercise in women with osteoarthritis of the knee: a randomized controlled trial. Clinical Rehabilitation 2015:0269215514540920.
Tanaka R, Ozawa J, Kito N, Moriyama H. Effect of the frequency and duration of land-based therapeutic exercise on pain relief for people with knee osteoarthritis: a systematic review and meta-analysis of randomized controlled trials. J Phys Ther Sci. 2014;26(7):969–75.
DiBrezzo R, Shadden BB, Raybon BH, Powers M. Exercise intervention designed to improve strength and dynamic balance among community-dwelling older adults. J Aging Phys Act. 2005;13(2):198–209.
Tanaka R, Ozawa J, Kito N, Moriyama H. Does exercise therapy improve the health-related quality of life of people with knee osteoarthritis? A systematic review and meta-analysis of randomized controlled trials. J Phys Ther Sci. 2015;27(10):3309.
Fleck SJ, Dean LS. Resistance-training experience and the pressor response during resistance exercise. J Appl Physiol. 1987;63(1):116–20.
Salli A, Sahin N, Baskent A, Ugurlu H. The effect of two exercise programs on various functional outcome measures in patients with osteoarthritis of the knee: a randomized controlled clinical trial. Isokinet Exerc Sci. 2010;18(4):201–9.
Bruce-Brand RA, Walls RJ, Ong JC, Emerson BS, OByrne JM, Moyna NM. Effects of home-based resistance training and neuromuscular electrical stimulation in knee osteoarthritis: a randomized controlled trial. BMC Musculoskelet Disord. 2012;13(1):1.
Jan M-H, Lin J-J, Liau J-J, Lin Y-F, Lin D-H. Investigation of clinical effects of high-and low-resistance training for patients with knee osteoarthritis: a randomized controlled trial. Phys Ther. 2008;88(4):427–36.
Petersen SG, Beyer N, Hansen M, Holm L, Aagaard P, Mackey AL, et al. Nonsteroidal anti-inflammatory drug or glucosamine reduced pain and improved muscle strength with resistance training in a randomized controlled trial of knee osteoarthritis patients. Arch Phys Med Rehabil. 2011;92(8):1185–93.
Hopman-Rock M, Westhoff MH. The effects of a health educational and exercise program for older adults with osteoarthritis for the hip or knee. J Rheumatol. 2000;27(8):1947–54.
Akyol Y, Durmus D, Alayli G, Tander B, Bek Y, Canturk F, et al. Does short-wave diathermy increase the effectiveness of isokinetic exercise on pain, function, knee muscle strength, quality of life, and depression in the patients with knee osteoarthritis? A randomized controlled clinical study. Eur J Phys Rehabil Med. 2010;46(3):325–36.
Beaupre LA, Lier D, Davies DM, Johnston DBC. The effect of a preoperative exercise and education program on functional recovery, health related quality of life, and health service utilization following primary total knee arthroplasty. J Rheumatol. 2004;31(6):1166–73.
Huang M-H, Lin Y-S, Yang R-C, Lee C-L. A comparison of various therapeutic exercises on the functional status of patients with knee osteoarthritis. Proceedings of the Seminars in arthritis and rheumatism: Elsevier; 2003.
McQuade KJ, de Oliveira AS. Effects of progressive resistance strength training on knee biomechanics during single leg step-up in persons with mild knee osteoarthritis. Clin Biomech. 2011;26(7):741–8.
Knutzen KM, BRILLA LR, CAINE D. Validity of 1RM prediction equations for older adults. J Strength Cond Res. 1999;13(3):242–6.
Sled EA, Khoja L, Deluzio KJ, Olney SJ, Culham EG. Effect of a home program of hip abductor exercises on knee joint loading, strength, function, and pain in people with knee osteoarthritis: a clinical trial. Phys Ther. 2010;90(6):895–904.
Topp R, Woolley S, Hornyak Iii J, Khuder S, Kahaleh B. The effect of dynamic versus isometric resistance training on pain and functioning among adults with osteoarthritis of the knee. Arch Phys Med Rehabil. 2002;83(9):1187–95.
Peterson MD, Rhea MR, Alvar BA. Application of the dose–response for muscular strength development: a review of meta-analytic efficacy and reliability for designing training prescription. J Strength Cond Res. 2005;19(4):950–8.
Hurley MV, Scott DL, Rees J, Newham DJ. Sensorimotor changes and functional performance in patients with knee osteoarthritis. Ann Rheum Dis. 1997;56(11):641–8.
Fitzpatrick R, McCloskey D. Proprioceptive, visual and vestibular thresholds for the perception of sway during standing in humans. J Physiol. 1994;478(Pt 1):173.
Wang C, Collet JP, Lau J. The effect of Tai Chi on health outcomes in patients with chronic conditions: a systematic review. Arch Intern Med. 2004;164(5):493–501.
Brismee J-M, Paige RL, Chyu M-C, Boatright JD, Hagar JM, McCaleb JA, et al. Group and home-based tai chi in elderly subjects with knee osteoarthritis: a randomized controlled trial. Clin Rehabil. 2007;21(2):99–111.
Ni G-X, Song L, Yu B, Huang C-H, Lin J-H. Tai chi improves physical function in older Chinese women with knee osteoarthritis. JCR: J Clin Rheumatol. 2010;16(2):64–7.
Song R, Lee E-O, Lam P, Bae S-C. Effects of tai chi exercise on pain, balance, muscle strength, and perceived difficulties in physical functioning in older women with osteoarthritis: a randomized clinical trial. J Rheumatol. 2003;30(9):2039–44.
Wang C, Schmid CH, Hibberd PL, Kalish R, Roubenoff R, Rones R, et al. Tai Chi is effective in treating knee osteoarthritis: a randomized controlled trial. Arthritis Care Res. 2009;61(11):1545–53.
Hall A, Maher C, Latimer J, Ferreira M. The effectiveness of Tai Chi for chronic musculoskeletal pain conditions: a systematic review and meta-analysis. Arthritis Care Res. 2009;61(6):717–24.
Chaipinyo K, Karoonsupcharoen O. No difference between home-based strength training and home-based balance training on pain in patients with knee osteoarthritis: a randomised trial. Aust J Physiother. 2009;55(1):25–30.
Fitzgerald GK, Piva SR, Gil AB, Wisniewski SR, Oddis CV, Irrgang JJ. Agility and perturbation training techniques in exercise therapy for reducing pain and improving function in people with knee osteoarthritis: a randomized clinical trial. Phys Ther. 2011;91(4):452–69.
Hurley M, Scott D. Improvements in quadriceps sensorimotor function and disability of patients with knee osteoarthritis following a clinically practicable exercise regime. Rheumatology. 1998;37(11):1181–7.
Ageberg E, Link A, Roos EM. Feasibility of neuromuscular training in patients with severe hip or knee OA: the individualized goal-based NEMEX-TJR training program. BMC Musculoskelet Disord. 2010;11(1):126.
Jan M-H, Tang P-F, Lin J-J, Tseng S-C, Lin Y-F, Un D-H. Efficacy of a target-matching foot-stepping exercise on proprioception and function in patients with knee osteoarthritis. J Orthop Sports Phys Ther. 2008;38(1):19–25.
Wyatt FB, Milam S, Manske RC, Deere R. The effects of aquatic and traditional exercise programs on persons with knee osteoarthritis. J Strength Cond Res. 2001;15(3):337–40.
Cochrane T, Davey RC, Edwards SMM. Randomised controlled trial of the cost-effectiveness of water-based therapy for lower limb osteoarthritis. Gray; 2005.
Boutaugh ML. Arthritis foundation community-based physical activity programs: effectiveness and implementation issues. Arthritis Care Res. 2003;49(3):463–70.
Wang TJ, Lee SC, Liang SY, Tung HH, Wu SFV, Lin YP. Comparing the efficacy of aquatic exercises and land based exercises for patients with knee osteoarthritis. J Clin Nurs. 2011;20(17):2609–22.
Messier SP, Loeser RF, Miller GD, Morgan TM, Rejeski WJ, Sevick MA, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the arthritis, diet, and activity promotion trial. Arthritis Rheum. 2004;50(5):1501–10.
Wang TJ, Belza B, Elaine Thompson F, Whitney JD, Bennett K. Effects of aquatic exercise on flexibility, strength and aerobic fitness in adults with osteoarthritis of the hip or knee. J Adv Nurs. 2007;57(2):141–52.
Lin SY, Davey R, Cochrane T. Community rehabilitation for older adults with osteoarthritis of the lower limb: a controlled clinical trial. Clin Rehabil. 2004;18(1):92–101.
Brady TJ, Kruger J, Helmick CG, Callahan LF, Boutaugh ML. Intervention programs for arthritis and other rheumatic diseases. Health Educ Behav. 2003;30(1):44–63.
Sharma L, Song J, Hayes K, Pai YC, Dunlop D. Physical functioning over three years in knee osteoarthritis: role of psychosocial, local mechanical, and neuromuscular factors. Arthritis Rheum. 2003;48(12):3359–70.
Brouwer G, Van Tol A, Bergink A, Belo J, Bernsen R, Reijman M, et al. Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum. 2007;56(4):1204–11.
Sharma L, Song J, Dunlop D, Felson D, Lewis CE, Segal N, et al. Varus and valgus alignment and incident and progressive knee osteoarthritis. Ann Rheum Dis. 2010;69(11):1940–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Wendy Anemaet and Amy Hammerich declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Physical Therapy and Rehabilitation
Rights and permissions
About this article
Cite this article
Hammerich, A.S., Anemaet, W.K. Applying the Evidence for Exercise Prescription in Older Adults with Knee Osteoarthritis. Curr Geri Rep 5, 179–190 (2016). https://doi.org/10.1007/s13670-016-0178-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13670-016-0178-5