Abstract
Aim
The aim of this study was to compare proprioceptive function between computerized proprioception facilitation exercise (CPFE) and closed kinetic chain exercise (CKCE) for knee osteoarthritis.
Design
Randomized–controlled.
Setting
Kinesiology laboratory.
Patients
Eighty-one patients with bilateral knee osteoarthritis were randomly assigned to CPFE, CKCE, and control groups.
Intervention
Both exercise groups underwent an 8-week program of three sessions per week. The control group received no training. The CPFE program included a 20-min computer game to be played by the trained foot of the subject. CKCE included 10 sets of 10 repetitions of repeated knee extension and flexion with resistance of 10–25% of body weight.
Main outcome measures
Absolute reposition error, functional score, walking speed, and knee muscle strength were assessed with an electrogoniometer, the physical function subscale of Western Ontario and McMaster Osteoarthritis Index, a CASIO stopwatch, and a Cybex 6000 dynamometer before and after the 8-week period.
Results
The results of this study showed that both CPFE and CKCE were effective in improving joint position sense, functional score, walking speed, and muscle strength. Furthermore, CKCE showed greater effect in increasing knee extensor torque in patients with knee osteoarthritis.
Conclusion
Clinical effects of CPFE were the same as those of CKCE except for knee extensor torque. The increase in knee extensor torque in CPFE patients was not as great as that seen in CKCE patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
People with knee osteoarthritis are usually frustrated by knee pain, joint stiffness, decrease of muscle strength, and proprioception deficits [1, 2]. Subsequently, these patients often exhibit poor neuromuscular control, slower walking, decreased functional ability, and increased susceptibility to falls [3–5]. Clinically, physical therapists often use strengthening exercise programs to increase muscle strength and facilitation techniques to improve proprioceptive function [6, 7].
Proprioception, an important sensory system, not only allows people to detect the position and motion of limbs, but also provides the sensation of force generation. From this, a person can better regulate force output [8–10]. With deficient proprioception, a person may exhibit muscular weakness [3, 6, 8, 11]. At the knee joint, proprioception is mediated by feedback from specialized receptors located in intra-articular tissues, such as ligaments and capsules, and also from those receptors located in extra-articular tissues, such as tendons and muscles [12]. Proprioception allows an individual to better maintain knee stability during static posture. Additionally, this sensation makes knee actions well coordinated and precise [9, 10], thus improving walking speed.
Exercise has been recommended by the American College of Rheumatology as a treatment for knee osteoarthritis on the basis of several small trials that demonstrated its efficacy for this condition [6, 7]. Previous studies had demonstrated comparable improvements in lower limb function with a variety of therapeutic exercises designed to increase muscle strength, including open kinetic exercises, closed kinetic exercises, and ordinary endurance training [13, 14]. However, few articles explored what exercise can improve proprioception for subjects with knee osteoarthritis. Given that there is stress feedback within a joint, closed kinetic exercise is supposed to play a dual role in strengthening muscle power and facilitating proprioceptive function [9, 10]. Previous reports have indicated that closed-chain exercises activate more muscle spindle and joint proprioceptors [5, 15, 16]. However, closed-chain exercises may aggravate symptoms, such as pain, swelling, and inflammation of knee osteoarthritis if the load on the joint during the exercise is not controlled properly [17, 18].
To avoid excessive loading on the knee joint, closed kinetic chain exercises (CKCEs) are often performed in the form of a leg press in a sitting or lying position. This is a rather boring exercise for the patient, because all they can do is flex and extend the knee joint with a certain load. Therefore, we designed a computer game that is operated by the foot to provide both exercise and entertainment for patients with knee osteoarthritis. The patient sits in front of a computer and tries to control a snake on the computer screen to go in the correct direction with his/her foot by pressing target pedals in four directions: up, down, right, and left. In addition to resistance, our computer game provides training of proprioception.
The purpose of this study was to compare the outcome of a closed-chain exercise with resistance and a multidirected proprioceptive facilitation exercise without resistance on patients with knee osteoarthritis. Outcome measurements included joint reposition error, physical function subscales of Western Ontario and McMaster Osteoarthritis Index (WOMAC), walking speed, and knee muscle strength. The present study was aimed to pose encouraging clinical implications of this device to train knee proprioception in patients with knee osteoarthritis.
Materials and methods
Subjects
Participants of this study were recruited from the Departments of Orthopedics at National Taiwan University Hospital and Taipei City Hospital. The inclusion criteria of participants were age of at least 50 years old, bilateral knee osteoarthritis of grade 3 or less on Kellgren/Lawrence classification on plain X-ray examination [19], and no treatment whatsoever for knee osteoarthritis within the past 3 months. Exclusion criteria included an existing comorbidity (such as cardiopulmonary, neurological, or other orthopedic diseases), participating in regular exercise at least three times per week, or having a job that required heavy lifting [20].
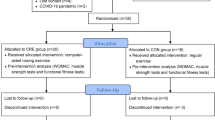
A total of 112 patients were enrolled in this study. Of these, 16 subjects did not meet inclusion criteria; seven refused to participate. All of the 89 patients who participated in this study signed an informed consent approved by the Ethics Committee of the National Taiwan University Hospital. The subjects were randomly assigned to the computerized proprioception facilitation exercise (CPFE) group (n=30), the CKCE group (n=29), or the control group (n=30). One patient in the CPFE group dropped out due to work affairs. Three patients in the CKCE group discontinued the training program due to personal reasons, and four patients in the control group dropped out of the study as well. A total of 81 patients (29 CPFE, 26 CKCE, and 26 control) completed the full course of the study (Fig. 1).
CPFE apparatus and the CPFE program
To avoid excessive loading on the knee joint and to increase entertainment, we designed an apparatus for facilitating knee proprioception in the sitting position. The custom-built apparatus used for the training in the CPFE program consisted of the following hardware and software components: The hardware components included a personal computer running on Windows 98 (Microsoft, Redmond, WA, USA), a color computer screen, and a plantar control board that measured 57 cm in length × 57 cm in width × 4 cm in thickness with a metal pedal located in each of the four quadrants (Fig. 2). Each pedal was 8 cm wide × 9 cm long. The distance between the center of the plantar control board and each pedal was 10 cm. A controlling driver was installed onto the computer (Acer, Taipei, Taiwan); as soon as the person’s foot pressed the pedal to the bottom, a snake’s head immediately appeared on the computer screen, ready to catch prey. This passed through the controlling driver, so that the signal of the controller could be simultaneously displayed on the computer screen. At the beginning of each trial of the game, a snake was displayed at the center of the computer screen, and a target prey was presented at one of the 4 quadrants on the screen. The prey moved on the screen according to a specified speed determined by the computer software. The up-and-down movements of the snake on the screen were controlled by the subject stepping onto the anterior and posterior pedals. The left-to-right movements of the snake were controlled by the subject stepping onto the left and right pedals, respectively. Participants scored points when the snake caught the prey. The game had nine speeds for the prey. Participants began with the slowest speed trials; when they achieved a specific score, the game progressed to the next faster speed.
Each participant sat 30 to 50 cm in front of the computer screen, and was asked to step onto the pedal with the trained foot to play the game displayed on the screen. Experimenters provided patients in the training group with verbal instructions as well as demonstrations. For each participant, each leg was trained for 20 min, with a 10-min break between trainings to prevent fatigue.
Closed kinetic chain exercise
Subjects performed CKCE of the knee in the supine position with their foot placed on the center of the pedal of the Shuttle Mini Clinic resistance device (Contemporary Design, Glacier, WA, USA). Subjects were asked to extend and flex the knee joint from 90 to 0° of knee flexion. Each action was completed rhythmically with the first second spent on extending the knee and the following second on flexing the knee.
All subjects in both exercise groups underwent an 8-week exercise program and trained for three sessions per week. For each participant in the CKCE group, each leg was trained by 10 sets of 10 repetitions per set. At the first training session, the resistance was set at 10% of body weight, and 5% of body weight was added progressively every 2 weeks. At the end of the training session, resistance was added to achieve 25% of body weight. Subjects rested for 1 min between every set. Both extremities were trained; there was a 5-min interval between the training sessions of each knee. Subjects in the control group did not receive exercise therapy, nor did they take any other medicine except health education regarding knee osteoarthritis during the study period.
Measurements
Absolute reposition error for measuring the proprioception of the knee
The knee joint position sense was measured as the subject’s ability to replicate target knee joint angles using an electrogoniometer (Biometrics, Gwent, UK) and Shuttle Mini Clinic resistance-measuring instrument. The tested ankle, joint, and foot were fixated with an air splint to reduce stimuli to the ankle and sole of the foot. The foot was placed in the center of the pedal of the instrument. The resistance of the pedal was set to 15% of the subject’s body weight. Therefore, the subjects needed to exert a force to resist against a force level of 15% of their body weight during the positioning and repositioning test. The experimenter was blinded to the patient’s grouping. During the test, the subject was in a supine position and blindfolded. An electrogoniometer was attached to the lateral side of the leg across the tested knee using 3M adhesive tape (3M, St. Paul, MN, USA), so that the electrogoniometer sensors corresponded with the axis of the leg when viewed in the sagittal plane. The subject’s starting angle of the knee was set at 90° of flexion. The subject then extended the knee joint to a self-determined target angle between 0 and 90°of knee flexion for 5 s. After returning to the starting angle and having remained there for 10 s, the subject was asked to extend the knee again to reach the target angle. The knee repositioning error was defined as the absolute difference between the reproduction angle and the target angle.
Physical function subscales of WOMAC (68 points)
The function of bilateral affected knees was assessed by the physical function subscales of the WOMAC [21]. There were 17 items in the assessment form, including stepping up and down stairs, standing up, taking socks on and off, bathing, house keeping, and so forth. If the patient scored higher on the scale, the subject had a lower functional performance. If an item was very hard to accomplish, the performance was scored 4 points; and on the other hand, if it was very easy to accomplish, it had a score of 0. The total score of the functional assessment was 68 points.
Walking speed over four different terrains
To test walking speeds, the subjects were asked to walk as fast as possible on a 60-m, level-ground, hard surface (a corridor), along a figure-8 pattern made of two circles (each with a 50-cm radius), and stepping up and down 13 stairs (each step was 16 cm high, 30 cm long, and 80 cm wide). Additionally, the subjects were asked to walk at a comfortable speed on a 12-m-long spongy surface measuring 10 cm in thickness and 21 shore 000 in hardness (medium hard). All walking trials were recorded with the CASIO stopwatch HS-20 (Casio, Tokyo, Japan), which could accurately measure time to 0.01 s.
Measurement of muscle torque in knee extensors and flexors
The muscle torque of bilateral knee extensors and flexors was tested at 60, 120, and 180°/s using a Cybex 6000 isokinetic dynamometer (Cybex International, Medway, MA, USA). A standard positioning method was used to test these muscles [22]. The subjects sat leaning against a backrest that inclined 15° backward from vertical. The backrest was secured to the machine at the upper chest, pelvis, and distal femur of the tested side. The subjects were instructed to extend the knee as far as possible and then to flex as far as the device allowed. Among the records of the three trials at each speed, the highest values were recorded as the peak torque. All data were corrected for gravity.
Procedure
All the subjects underwent an initial baseline assessment of knee reposition error, physical function subscale of WOMAC, walking speeds on four different terrains, and muscle strength in sequence. In the repositioning error test, the leg to be tested first was selected randomly to prevent a possible sequence effect [23]. During the test, the subject was in the supine position and blindfolded. For each subject, one self-determined larger (46–90°) target angle and one smaller (0–45°) target angle of knee flexion were tested. The absolute of each angle was used to indicate the subject’s proprioceptive function of the tested knee, with greater differences representing greater proprioceptive impairment. Afterwards, the functional score was calculated, and the walking speed test then followed. The physical function subscale of WOMAC was assessed by one of the authors (Y.C. Han), a senior physical therapist with 5 years of clinical experience. Then, each subject undertook the walking speed test, including two walking trials on each terrain, the level-ground hard surface, stepping up and down 13 stairs, the figure-8 route, and the 12-m-long spongy surface, in sequence. Subjects were instructed to walk as fast as possible except while walking on the spongy surface. While walking on the spongy surface, the subjects were instructed to walk at a comfortable speed to avoid falling down. Following the walking speed test, each subject underwent muscle torque tests using the Cybex 6000 isokinetic dynamometer at the velocities of 60, 120, and 180°/s performed on the bilateral knee extensors and flexors. Routine calibration for the Cybex machine was performed prior to the testing of each subject. The muscle torque testing of each muscle consisted of three trials in which the subject was asked to exert maximal effort against the testing pad without causing pain.
At the completion of the 8-week intervention period, all subjects took the follow-up assessments of knee repositioning error, physical function subscale of WOMAC, walking speeds on four different terrains, and muscle torque of the knee within 3 days. The testing procedures were the same as those used in the initial baseline assessment.
Statistical analysis
Descriptive statistics were used to depict subjects’ demographic characteristics, including age, height, weight, and X-ray grade of osteoarthritis. The average absolute repositioning error for larger and smaller angles of knee flexion and average walking time for each walking condition were calculated and were used for further statistical analysis.
The chi-square test was used to compare the distribution of gender and X-ray grade of osteoarthritis among the three groups. A one-way ANOVA procedure was used to compare the baseline values in absolute repositioning error, walking speeds on four different terrains, and muscle torque of the knee among the three groups. This tested whether the three groups were generally comparable to their pre-experiment physical status.
A two-way ANOVA (group X timing) was used with the factors of group (three study groups) and the factor of timing (pre- vs postintervention) serving as a between-subject factor and as within-subject factors to compare the significant effects of group and timing on knee repositioning error, walking speeds, and muscle strength. When two-way interaction was found, post hoc analysis with Bonferroni adjustment (p<0.016) was used as follow-up analysis. In addition, the Friedman test was used to test differences between the pre- and posttraining values in physical function subscales of WOMAC for all three groups. The Kruskal–Wallis rank test was used to compare the related difference between the initial baseline and posttraining in physical function subscales of WOMAC if any significance existed.
Results
Table 1 presents the demographic information of the three study groups. There was no significant difference in age, sex distribution, body height, weight, and distribution of the X-ray grade of osteoarthritis between the three groups (p>0.05). Figure 3 shows the knee reposition error and WOMAC functional scores of the three groups before and after the 8-week period. In those subjects in the CPFE and CKCE groups, there were significant reductions in both knee repositioning error and the WOMAC functional subscale after the 8-week exercise intervention. Figure 4 shows the walking speeds on four different terrains of the three groups before and after intervention. In all subjects in the CPFE and CKCE groups, there were significantly increased walking speeds on the four different terrains after exercise intervention (p<0.016). However, the control group showed no change in repositioning error, physical function subscales, and walking speed (p>0.05), except for the walking speed along the figure-8 route. The control subjects significantly reduced their walking speed along the figure-8 route (p<0.016).
Comparison of pre- and postintervention value in joint reposition error and physical function subscales of WOMAC for the three groups of subjects. * denotes that the difference between pre- and postintervention was significant (p<0.05). † denotes that the change value after intervention was significantly different between the CPFE and control groups (p<0.0083). ‡ denotes that the change value after intervention was significantly different between the CKCE and control groups (p<0.0083)
Comparison of pre- and postintervention values in time consumption for walking on four different terrains for the three groups of subjects. * denotes that the difference between pre- and postintervention was significant (p<0.05). † denotes that the decrease of time consumption for walking between the CPFE and control groups was significantly different (p<0.0083). ‡ denotes that the decrease of time consumption between the CKCE and control groups was significantly different (p<0.0083)
Using a 3×2 ANOVA with repeated measures revealed significant interaction effects of the group (exercise vs control group) and timing (pre- vs postintervention). The decreases in joint repositioning error and functional subscales of WOMAC in both the CPFE and CKCE groups were significantly different from those of subjects in the control group (Fig. 3). Regarding changes in walking speed after the 8-week period among the three groups, subjects in the two exercise groups showed significantly greater improvement of walking speed in a straight line, up and down stairs, in a figure-8 pattern, and on a spongy surface than those in the control group (Fig. 4, p<0.0005). This indicates that after exercise intervention by either CPFE or CKCE, there was a significant decrease of joint positioning error, functional subscales of WOMAC, and time consumption while walking in a straight line, up and down stairs, on a spongy surface, and along a figure-8 pattern (p<0.0005). However, there was no significant different improvement of joint repositioning error, functional subscales of WOMAC, and walking speed between the two exercise groups (Figs. 3 and 4). This indicates that the two exercise programs showed the same clinical effects in proprioception, functional performance, and walking speed. Furthermore, the improvement in walking speed on the spongy surface and the figure-8 pattern was greater than that seen on walking speed on the level ground and stairs (Fig. 4).
Further comparison of change in the peak torque of knee extensors and flexors at the velocities of 60, 120, and 180°/s of the three groups before and after the 8-week period was performed. The statistical results revealed that subjects of both exercise groups showed significantly increased knee muscle torque at three different velocities of muscle contraction—either extension or flexion. However, subjects in the control group showed no change in muscle torque. Upon statistically analysis, subjects in both the CPFE and CKCE groups demonstrated significantly greater improvement of all muscle torque at three different velocities of muscle contraction than those in the control group (Table 2, p<0.0005). Furthermore, there was also significant greater improvement of all extensor muscle torques in subjects of the CKCE group than those of the CPFE group. It is worthy to note that subjects in both CPFE and CKCE groups experienced greater improved joint position sense (40.4–42.9%) than muscle torque (6.1–21.9%).
Discussion
Results of this study revealed that both CPFE and CKCE programs were effective in decreasing knee repositioning error, physical function subscales of WOMAC, walking speed, and knee muscle torque in patients with knee osteoarthritis. However, the aforementioned effects were not significantly different between the two exercise groups except that knee extensor torques were improved to greater degree in the CKCE group. Additionally, the improvement in joint position sense (proprioception) was greater than that seen in muscle torque.
All of the patients in this study exhibited reduced joint position sense and muscle strength of both knees as compared to age-matched healthy controls reported in the literature [3, 5]. For these patients, selecting a better effect from an exercise regimen to recover functional performance is an important feature in their physical therapy. Most previous researches focused on improving muscle strength [24]. Recently, closed kinetic chain exercise has been frequently and effectively used to strengthen and facilitate knee muscle strength and joint proprioception [25, 26]. An exercise program with entertainment, like that experienced by the CPFE group in this study, produced the same clinical effects as CKCE.
Characteristics of CPFE and CKCE
The CPFE in this study was designed specifically for proprioception training in the sitting position. As long as the patient’s foot pressed the pedal, mechanoreceptors around the knee joint were activated simultaneously. Thus, the CPFE group executed open- and closed-chain exercises. The open-chain exercise occurred when the subjects attempted to press the pedal by moving their leg in the air. The closed-chain activity occurred when the pedal was pressed. The weight resistance of the closed-chain exercise activated the proprioceptors in the knee joint. Furthermore, to precisely place a foot on the correct pedal, each subject needed to pay attention to the computer screen. Overall, the CPFEP facilitated the proprioceptive receptors in muscle spindles, tendons, and knee joints over the long term. The subjects were trained with repetitive foot stepping by using primarily the knee joint motions. Visual receptors were recruited to provide feedback and enhance sensorimotor mapping of the movements of the knee joint. Therefore, we can conclude that the CPFE emphasized sensory proprioceptor facilitation of the knee joint.
The CKCE with Shuttle Mini Clinic resistance device emphasized strengthening the knee extensors, either from 90° of knee flexion to full knee extension or reverse motion. In addition, the cocontraction of knee flexors also occurred during the training process. The CKCE basically bore weight on the knee joint, as did patients performing the knee extension–flexion exercise. Subjects received resistance feedback from the footplate to activate the related mechanoreceptors and motor units of knee joint. Therefore, sensory proprioception was facilitated simultaneously in the CKCE program.
Improvement of knee reposition sense
Both the CPFE and CKCE have brought about significant improvement in the accuracy of knee repositioning sense. Although the decrease of knee repositioning error in both exercise groups is significantly greater than that in the control group, there is no significant difference between the CPFE and CKCE groups. The CKCE can be used to facilitate proprioception in athletes or young men as shown in previous reports [9, 10, 26, 27]. Our results prove that CPFE without weight bearing exercise has allowed good proprioception facilitation as that accomplished by CKCE for subjects with knee OA. The outcome of improving joint position sense was similar in both groups.
We hypothesized that such a repositioning accuracy effect results from the combined effect of stepping with the foot and of stimulating visual perception by using the computer screen. To execute visually guided movements of the leg, the central nervous system must transform a desired leg trajectory (kinematics) into appropriate muscle-related commands (dynamics) [28]. Some have hypothesized that repeated motions, either in short or long training periods, lead to cortical reorganization characterized by a small and efficient network specific to trained movement kinematics [29]. The 8-week CPFE consisted of practicing both spatial (joint angle and movement extent) and temporal (pace) movement parameters. To complete the CPFE, subjects with knee OA actually practiced great amounts of visual-motor transformation and parameter specification. Such experience is of great help in developing precise and efficient visual-motor mapping, as shown in by the patients’ improved accuracy in joint repositioning on kinematic testing. As indicated above, the muscle spindle is the only receptor system whose peripheral gain can be modulated by exercise [30]. Regarding the CKCE, previous reports have suggested that proprioception should be trained under weight-bearing, closed-chain conditions for an optimal effect [9, 10]. We hypothesize that 10 to 25% body weight as exercise resistance is enough to facilitate proprioception of the knee joint. With this regard, how much weight will optimize the effect of facilitation proprioception in the knee joint? Further research is needed in this area to elucidate this finding.
Joint repositioning sense and walking speed
Hurley et al. [31] and Sharma [32] reported that proprioception (joint position sense) is closely related the functional performance of the knee and to walking speed. We attained the same observations. In the literature, the effect of proprioceptive training on knee OA was rarely explored until Hurley and Scott performed their study [33]. Their experimental protocol consisted of 10 sessions of rehabilitation exercise, which included maximal isometric voluntary contractions of the quadriceps, riding a static exercise bicycle, isotonic knee extension and flexion by using an elastic band, and three functional exercises performed in the standing position. After this intervention, joint reposition error decreased by 0.47° (3.64–3.17°), a 12.9% improvement, in patients with knee OA. In addition, their aggregate functional performance time in four walking conditions improved by 13.7%. Marks et al. [5] also reported that there was a significant correlation between joint position sense and those of walking speed.
Our 8-week CPFE and CKCE also significantly improved joint repositioning error and walking speeds. In our study, both the CPFE and CKCE decreased the joint repositioning error by 2.1 and 1.9° (42.9 and 40.4%), respectively. In addition, both the CPFE and CKCE reduced aggregate walking times in the four conditions by 24.2 and 27.4%, respectively. In terms of walking difficulty, walking on the spongy surface and following a figure-8 pattern demanded a higher proprioceptive function to accomplish the task, which was harder than walking on level ground and stairs. Both CPFE and CKCE increased the walking speed on the spongy surface and figure-8 pattern (36.4–45.7%) to a greater degree than that of walking on the level ground and stairs (8.1–17.9%). We hypothesize that both CPFE and CKCE could increase greater joint positioning sense (42.9 and 40.4%, respectively) than muscle strength. Subsequently, both exercise groups promoted more joint proprioception and increased walking speeds on terrains demanding higher proprioception.
Muscle strength and walking speed
Our results showed significant improvement in knee extensor and flexor strength at 60, 120, and 180°/s after the 8-week exercise intervention in both groups. However, subjects in the control group did not improve their muscle strength of the knee extensors or flexors. Thus, our results suggest that both CPFE and CKCE were effective in improving knee muscle strength in knee OA patients (6.1–21.9%). However, this increase was not as great as the improvement of repositioning sense (40.4–42.9%). McAlindon et al. [33] declared that quadriceps weakness was found to be the greatest single predictor of lower limb functional limitation, exceeding that of knee pain. Therefore, the strengthening program of the CKCE emphasized the quadriceps. Correspondingly, the results of the CKCE increased the strength of the extensor (20.1–21.9%) over that of the flexor (16.4–18.3%). The CKCE also showed the greatest improvement of knee extensor torque among the three groups. In terms of demand on muscle strength of the knee extensors, walking up and down stairs is the greatest one among the four terrains [34]. The improvement of walking speed on stairs was greatest in CKCE subjects among the three groups, although the difference did not show statistical significance. Therefore, we hypothesize that CKCE even emphasized strengthening knee muscles as well as proprioception facilitation. Many researchers have suggested that improvement in proprioception can promote muscle strength and vice versa [14, 26, 27]. Of special interest is that CPFE training, regarded by participants as a particularly enjoyable program, enhanced long-term compliance as well.
Conclusion
Both 8-week CPFE and CKCE have been observed to improve proprioceptive functions, such as increasing joint position sense, functional performance, walking speed on level ground, stepping up and down stairs, traversing along a figure-8 pattern, and walking on a spongy surface, as well as increase knee muscle torque in patients with knee osteoarthritis. Subjects in the CKCE group have demonstrated a significantly increased extensor torque than those in the CPFE group. Either CPFE or CKCE can be considered an effective proprioceptive exercise for patients with knee osteoarthritis in clinical practice.
References
Eyigor S, Hepguler S, Capaci K (2004) A comparison of muscle training methods in patients with knee osteoarthritis. Clin Rheumatol 23:109–115
Vilalta C, Nunez M, Segur JM, Domingo A, Carbonell JA, Macule F (2004) Knee osteoarthritis: interpretation variability of radiological signs. Clin Rheumatol 23:501–504
Koralewicz LM, Engh GA (2000) Comparison of proprioception in arthritic and age-matched normal knees. J Bone Joint Surg Am 82:1582–1588
Lord SR, Clark RD, Webster IW (1991) Physical factors associated with falls in an elderly population. J Am Geriatr Soc 39:1194–1200
Marks R, Quinney HA, Wessel J (1993) Proprioceptive sensibility in women with normal and osteoarthritic knee joints. Clin Rheumatol 12:170–175
Bearne LM, Scott DL, Hurley MV (2002) Exercise can reverse quadriceps sensorimotor dysfunction that is associated with rheumatoid arthritis without exacerbating disease activity. Rheumatology 41:157–166
Geffen SJ (2003) Rehabilitation principles for treating chronic musculoskeletal injuries. Med J Aust 178:238–242
Borsa PA, Lephart SM, Irrgang JJ, Safran MR, Fu FH (1997) The effects of joint position and direction of joint motion on proprioceptive sensibility in anterior cruciate ligament-deficient athletes. Am J Sports Med 25:336–340
Lephart SM, Pincivero DM, Giraldo JL, Fu FH (1997) The role of proprioception in the management and rehabilitation of athletic injuries. Am J Sports Med 25:130–137
Lephart SM, Pincivero DM, Rozzi SL (1998) Proprioception of the ankle and knee. Sports Med 25:149–153
Ribot-Ciscar E, Roll JP (1998) Ago-antagonist muscle 1 spindle inputs contribute together to joint movement coding in man. Brain Res 791:167–176
Schmidt RA (1999) Sensory contributions to motor control. In: Schmidt RA, Lee TD (eds) Motor control and learning: a behavioral emphasis, 3rd edn. Human Kinetics, Champaign, pp 95–129
Jan MH, Lai JS (1991) The effect of physiotherapy on osteoarthritis knees of females. J Formos Med Assoc 90:1008–1013
Hurley MV, Scott DL (1998) Improvements in quadriceps sensorimotor function and disability of patients with knee osteoarthritis following a clinically practicable exercise regime. Br J Rheumatol 37:1181–1187
Baker V, Bennell K, Stillman B, Cowan S, Crossley K (2002) Abnormal knee joint position sense in individuals with patellofemoral pain syndrome. J Orthop Res 20:208–214
Kramer J, Handfield T, Kiefer G, Forwell L, Birmingham T (1997) Comparisons of weight-bearing and non-weight-bearing tests of knee proprioception performed by patients with patello-femoral pain syndrome and asymptomatic individuals. Clin J Sport Med 7:113–118
Baliunas AJ, Hurwitz DE, Ryals AB, Karrar A, Case JP, Block JA (2002) Increased knee joint loads during walking are present in subjects with knee osteoarthritis. Osteoarthritis Cartilage 10:573–579
Lucchinetti E, Adams CS, Horton WE, Torzilli PA (2002) Cartilage viability after repetitive loading. Osteoarthritis Cartilage 10:71–81
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteoarthrosis. Ann Rheum Dis 16:494–501
Kohatsu ND, Schurman DJ (1990) Risk factors for the development of osteoarthrosis of the knee. Clin Orthop 261:242–246
Tuzun EH, Eker L, Aytar A, Daskapan A, Bayramoglu M (2005) Acceptability, reliability, validity and responsiveness of the Turkish version of WOMAC osteoarthritis index. Osteoarthritis Cartilage 13(1):28–33
Dvir Z (1996) Isokinetics. Churchill Livingstone, New York
Shima N, Ishida K, Katayama K, Morotome Y, Sato Y, Miyamura M (2002) Cross education of muscular strength during unilateral resistance training and detraining. Eur J Appl Physiol 86:287–294
Gur H, Cakin N (2003) Muscle mass, isokinetic torque, and functional capacity in women with osteoarthritis of the knee. Arch Phys Med Rehabil 84:1534–1541
Stensdotter AK, Hodges PW, Mellor R, Sundelin G, Hager-Ross C (2003) Quadriceps activation in closed and in open kinetic chain exercise. Med Sci Sports Exerc 35:2043–2047
Bouet V, Gahery Y (2000) Muscular exercise improves knee position sense in humans. Neurosci Lett 289:143–146
Hewett TE, Paterno MV, Myer GD (2002) Strategies for enhancing proprioception and neuromuscular control of the knee. Clin Orthop 402:76–94
Padoa-Schioppa C, Li CS, Bizzi E (2004) Neuronal activity in the supplementary motor area of monkeys adapting to a new dynamic environment. J Neurophysiol 91:449–473
Morgen K, Kadom N, Sawaki L, Tessitore A, Ohayon J, Frank J et al (2004) Kinematic specificity of cortical reorganization associated with motor training. Neuroimage 21:1182–1187
Ashton-Miller JA, Wojtys EM, Huston LJ, Fry-Welch D (2001) Can proprioception really be improved by exercises? Knee Surg Sports Traumatol Arthrosc 9:128–136
Hurley MV, Scott DL, Rees J, Newham D (1997) Sensorimotor 1 changes and functional performance in patients with knee osteoarthritis. Ann Rheum Dis 56:641–648
Sharma L (1999) Proprioception impairment in knee osteoarthritis. Rheum Dis Clin North Am 25:299–314
McAlindon TE, Cooper C, Kirwan JR, Dieppe PA (1993) Determinants of disability in osteoarthritis of the knee. Ann Rheum Dis 52:258–262
Riener R, Rabuffetti M, Frigo C (2002) Stair ascent and descent at different inclinations. Gait Posture 15:32–44
Acknowledgement
Financial support from the National Science Council Grant in Taiwan (NSC 91-2218-E-002-033) is gratefully acknowledged.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s10067-007-0543-z
Rights and permissions
About this article
Cite this article
Lin, DH., Lin, YF., Chai, HM. et al. Comparison of proprioceptive functions between computerized proprioception facilitation exercise and closed kinetic chain exercise in patients with knee osteoarthritis. Clin Rheumatol 26, 520–528 (2007). https://doi.org/10.1007/s10067-006-0324-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-006-0324-0