Abstract
The relative pros and cons of robotic-assisted laparoscopic myomectomy (RALM) and laparoscopic myomectomy (LM) are still debated. The short-term surgical outcomes such as estimated blood loss, need for blood transfusion, intra-operative complications, and conversion to laparotomy are similar for RALM and LM. Although RALM was previously thought to require longer operative time when compared to LM, recent studies show comparative surgical duration. On longer follow-up, high pregnancy rates and low pregnancy morbidity have been reported for both surgical approaches. The increased cost of RALM when compared to LM may be amortized in high-volume surgical centers. Specimen removal via power morcellation is limited by the FDA safety communication, but strategies for “contained” power and cold-knife morcellation may prevent unintentional fibroid spread. To conclude, RALM and LM are both safe minimally invasive alternatives to open abdominal myomectomy. Future technical developments may allow for the widespread implementation of single-site RALM and LM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Uterine fibroids, also known as leiomyomas, are benign monoclonal growth of cells of the uterine smooth muscle. These benign tumors are relatively common, with an estimated prevalence of 20–35 % in reproductive age women and up to 70 % by 50 years of age [1]. However, only one in three women with fibroids reports fibroid-associated symptoms such as abnormal uterine bleeding, pelvic pressure and pain, urinary symptoms, and subfertility [2]. Women with symptomatic uterine fibroids may be offered non-surgical treatments such as hormonal medications, gonadotropin-releasing hormone antagonists, progesterone receptor modulators, and uterine artery embolization [2, 3]. The definitive treatment for symptomatic fibroids is hysterectomy or, for those women who wish to retain fertility, myomectomy. Smaller submucosal fibroids may be removed via hysteroscopic approach, with relatively fast recovery and minimal blood loss [4]. However, large submucosal fibroids as well as intramural and subserosal fibroids cannot be removed via hysteroscopy and require an abdominal approach, namely, laparotomy, laparoscopy, or robotic-assisted laparoscopy. Both laparoscopic myomectomy (LM) and robotic-assisted laparoscopic myomectomy (RALM) have advantages over open abdominal myomectomy in terms of post-operative pain, recovery period, and complications [5•], but the pros and cons of LM versus RALM are still debated. In this review, we will focus on the comparison of LM and RALM, evaluating their respective complications, reproductive outcomes, and cost.
Myomectomy: from Laparotomy to Laparoscopy to Robotics
Myomectomy was first performed abdominally in 1845 by Dr. Washington Atlee in Pennsylvania [6]. However, this procedure became prevalent only in the beginning of the twentieth century, following the work of Dr. Victor Bonney, who performed over 700 myomectomies. Dr. Bonney developed surgical techniques and instruments which enabled surgeons to perform myomectomies with relatively low rates of morbidity and mortality [6]. Subsequently, in the 1970s, the pioneer of laparoscopic surgery Dr. Kurt Semm developed LM as a minimally invasive surgical alternative [7]. Over the years, although laparoscopy became the standard surgical approach for adnexal surgery, it has not become the universal surgical approach for myomectomy [8]. The reasons for the relatively low adoption of this technique are the advanced laparoscopic skills required to perform it, and in particular the advanced laparoscopic suturing skills, which necessitate a long learning curve. The aim of the robotic platform, first approved by the FDA for marketing in 2005, was to overcome these drawbacks of laparoscopic surgery. In particular, the reduced tremor, improved 3D view, and higher degrees of movement freedom of the robotic platform facilitates laparoscopic suturing [9]. Apart from the use of the robotic platform, LM and RALM are very similar surgeries, consisting of pneumoperitoneum creation, setup of the laparoscopic or robotic system, and enucleation of the fibroids through one or more uterine incisions, followed by suture closure of the uterine defect and removal of the excised tissue via power or cold-knife morcellation. In view of the similar surgical steps, it is not surprising that outcomes of LM and RALM are overall similar. To date, eight studies have compared LM and RALM in single institutions, all of which have a retrospective cohort or case series design (Table 1) [10, 11•, 12–17]. Five of those studies included relatively large number of cases in each arm [10, 11•, 12, 15, 16]. In most of these studies, the same surgeons performed both the LM and RALM, while in the Brigham and Women’s hospital study the LM and RALM were performed separately by surgeons with specific skill sets in each respective technique [11•].
Comparison of Short-Term Outcomes and Complications
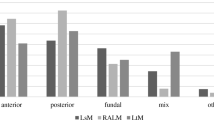
The short-term clinical and surgical outcomes which are of interest for patients undergoing LM or RALM include intra- and post-operative complications, blood loss and blood transfusion requirements, post-operative pain, length of hospital stay and recovery period, and need for readmission. Many of these parameters are greatly influenced by case selection, namely, the number, size, and location of the fibroids, with numerous, larger, and deep (i.e., submucosal or intramural as opposed to subserosal) fibroids likely to be associated with longer surgery and increased blood loss. Although most studies had similar fibroid characteristics in the LM and RALM groups, the study by Barakat et al. [10] reported that a large quantity of and heavier fibroids were removed in the RALM group compared with the LM group (Table 1).
Estimated blood loss and need for blood transfusion
One of the main advantages of LM and RALM over open abdominal myomectomy is the reduction in surgical blood loss [5•]. When comparing only LM and RALM, one study reported lower blood loss with RALM compared with LM [15] and another paper reported less surgical drainage on the first post-operative day [17]. However, in a meta-analysis design, the difference in blood loss between LM and RALM was only 42 ml, which was not statistically significant and is certainly not clinically significant [5•]. Similarly, the need for blood transfusion, which ranges from 0 to 12 % in the studies which reported this outcome, does not differ significantly between LM and RALM [10, 11•, 12–17]. Blood loss and blood transfusions may be reduced in both surgical approaches with the intra-myometrial injection of diluted vasopressin or with uterine artery occlusion [18•].
Operative time
Although some studies reported longer operative time for RALM compared with LM [11•, 17], a recent meta-analysis by Iavazzo et al. [5•] did not find any statistically significant difference in the operative time between these two groups. It is possible that the longer time required for the setup of the robotic platform for RALM (i.e., “docking time”) is compensated by the shorter time required for fibroid enucleation and uterine incision suture with this approach. Another parameter which could influence the operative time for all types of minimally invasive myomectomy is the use of barbed suture [11•, 19]. This suture allows for knotless suturing and equal distribution of suture strength along the closure. Its use has been shown to decrease operative time and blood loss both for LM and for RALM when compared to conventional sutures.
Intra- and post-operative complications
Complications with LM and RALM include intra-operative vascular and visceral injury, post-operative infections (i.e., wound infection, pneumonia, urinary tract infection, pelvic infection, etc.), ileus, and thromboembolic complications. The intra- and post-operative complications can be further classified into major and minor complications. The rate of major complications (such as vascular and visceral injuries) for LM and RALM is overall low and was not found to be significantly different between groups [5•]. The rate of minor complications is slightly higher, but again not different between groups. For example, incisional cellulitis requiring antibiotic treatment was described in the study by Gargiulo et al. [11•] for 9.1 % of LM patients and 3.4 % of RALM patients.
Readmission
This parameter is an important marker for significant post-operative complications which require hospital admission. Those complications may be directly related to the surgical procedure (i.e., wound infection) and indirectly related to it (i.e., pulmonary embolism). A recent study by Alton et al. [20•] described the outcomes of their same-day discharge protocol for minimally invasive myomectomies (334 cases of LM and 69 cases of RALM). The readmission rates were 0.6 and 1.4 % at 48 h and 3 months, respectively, including cases of post-operative fever, ileus, and pyelonephritis. The rates of readmission were not compared between LM and RALM in this study, but their findings may represent the low readmission rates for both of these surgeries.
Post-operative pain
None of the retrospective studies mentioned above compared post-operative pain in LM and RALM. However, a prospective randomized study comparing laparoscopic and robotic hysterectomy did not find any differences in post-operative pain [21, 22] while a prospective randomized study comparing laparoscopic and robotic sacrocolpopexy did find reduced post-operative pain in the traditional laparoscopic route [23]. This difference was explained by the difference in trocar size (5 mm for conventional laparoscopy versus 8 mm for the most common robotic ports) and the use of an additional port for the robotic procedure (i.e., a total of five ports versus four). Similar considerations may be applicable for LM and RALM. Nonetheless, both procedures are substantially superior to abdominal myomectomy with regards to immediate post-operative pain [24].
Length of hospital stay and recovery
The typical length of hospital stay after LM and RALM is 1–2 days and is not significantly different between these two surgeries [5•]. Hospitalization time longer than 2 days was reported for 23 % of LM cases compared with 12 % of RALM cases, but these rates were not statistically different [12]. Furthermore, in the USA, a same-day discharge protocol has been developed for minimally invasive myomectomies, which can be applied for more than 80 % of cases [20•].
Conversion to laparotomy
Conversion of a laparoscopic or robotic procedure to laparotomy may be required because of technical difficulties (i.e., difficulty in fibroid enucleation or during incision closure due to fibroid location or size) or complications (i.e., severe hemorrhage). Thus, the conversion rate is inherently affected by the case selection. The rate of conversion to laparotomy for LM and RALM was compared in a meta-analysis by Pundir et al. [25] which included four studies, and no significant differences were found. Furthermore, a large retrospective multi-center series of more than 800 RALM cases published in 2013 reported no conversion to laparotomy [26], while other large studies on LM reported low rates of conversion ranging from 2 to 5 % [27•].
Comparison of Fertility and Pregnancy Outcomes
Among the retrospective studies comparing LM and RALM, only two small studies reported the reproductive outcomes of patients, without any differences found between groups [13, 14]. However, several large series reported the reproductive outcomes of patients who underwent either LM or RALM [26, 27•, 28].
Fertility
Fibroids are thought to affect fertility via physical factors, alterations of uterine contractions, reduced endometrial receptivity, and alterations in the endo-myometrial junctional zone [29]. It is well recognized that submucosal fibroids and intramural fibroids causing distortion of the endometrial cavity should be removed in infertile women and in women undergoing fertility treatments (either via hysteroscopy or abdominally, depending on their type and size) [27•]. However, the removal of intramural fibroids which do not cause cavity distortion in infertile and asymptomatic women is controversial, with some studies reporting no significant differences in pregnancy rates with or without myomectomy [30], while a meta-analysis by Pritts et al. did show improved reproductive outcomes following myomectomy [31]. Regardless of the debate on the benefit of intramural fibroid removal in infertile women, the different impact of LM and RALM on infertility has not been well studied. It is difficult to compare the fertility rates after LM or RALM reported in various studies because of heterogeneity of infertility causes and workup, difference in rates of natural conception versus use of assisted reproductive techniques, and differences in follow-up time. Nevertheless, the rates of pregnancy reported in women who wished to conceive after LM and RALM range from 50 to 70 % for LM and around 70 % for RALM [27•, 28].
Pregnancy outcomes
A rare but potentially severe complication in pregnant women who underwent myomectomy is uterine rupture. The risk of uterine rupture has been linked to the use of electrosurgery and its potential myometrial injury, to the number of layers sutured, and to the number of uterine incisions. Accordingly, women who are considered to be at risk for uterine rupture because of numerous and/or deep uterine incisions are often counseled to undergo elective cesarean delivery, which could affect the ultimate rate of uterine rupture. The rate of uterine rupture reported for LM ranges from 0.26 to 1 %, with cesarean section performed in 38 to 78 % of cases [27•]. Pitter et al. reported the reproductive outcomes of 101 patients who conceived after RALM [26]. Of the 92 deliveries in this cohort, there was one case of uterine rupture, with a rate of 1.1 %.
Use of Power Morcellation in LM and RALM
The most common method for specimen removal during LM and RALM until recently has been power morcellation. Since November 2014, in view of the concerns regarding dissemination of undiagnosed leiomyosarcoma during power morcellation, and the FDA safety communication which effectively banned the use of non-contained power morcellation in peri-menopausal women, the use of this technique has been limited to younger women undergoing LM and RALM [32]. Not surprisingly, a 19 % decline in minimally invasive myomectomies has been reported in association with the FDA morcellation warning [33•]. The actual rate of undiagnosed leiomyosarcoma dissemination during power morcellation is still debated, with numbers ranging from 1/458 (per the FDA analysis) to 1/1960 per a recent large meta-analysis [34]. Furthermore, the overall benefit from the FDA’s safety communication has been questioned in view of its profound impact on the surgical route for hysterectomy and myomectomy and its probable impact on the associated surgical complications [35]. Nonetheless, the current aim of minimally invasive surgeons is to develop alternative techniques for fibroid removal which do not involve non-contained power morcellation. These techniques include cold-knife morcellation of the bagged specimen through the abdominal wall or through a posterior colpotomy and contained “in-bag” power morcellation. Despite concerns that in-bag morcellation would prolong operative time, a recent randomized controlled trial found similar morcellation time and total operative time for the non-contained and the in-bag morcellation [36].
Cost Comparison of LM and RALM
The overall economic burden of fibroid-associated medical care is high due to their widespread prevalence. In the USA, the annual direct and indirect costs for fibroid-associated medical care were estimated to reach $34.4 billion in 2010 [37]. As such, cost comparison for the different surgical routes of myomectomy is critical for healthcare policy. The cost of RALM ($7299) was found to be higher than LM ($6219), and both minimally invasive procedures were more expensive than open abdominal myomectomy (whose cost was calculated to be $4937, including hospitalization costs) [38]. However, these calculations do not include costs for treatment of complications and readmissions, as well as indirect societal costs such as work absence, all of which are typically higher for open abdominal myomectomy compared with minimally invasive routes. Thus, when all direct and indirect costs of the procedure are included, the robotic procedure may become cost effective when it allows converting an open myomectomy to a minimally invasive myomectomy.
The above direct cost estimations do not factor the cost of the robotic platform, which is typically around $1.5–$2 million. The translation of the cost of the robotic platform into the cost of individual surgeries is mainly dependent on the number of procedures performed with robot. For example, robotic hysterectomy costs per case were reduced by 41 % by increasing the weekly robotic case load from 3 to 9 in an Irish tertiary hospital [39].
Current and Future Developments in Surgical Techniques for Minimally Invasive Myomectomy
Single-site laparoscopic or robotic surgery may offer some advantages over multi-port surgery in terms of cosmetics and specimen extraction. Although single-site LM has been successfully performed with low rates of conversion to multi-port laparoscopy, it requires surgical expertise and, in particular, advanced laparoscopic surgical skills [40]. The parallel robotic surgery, single-site RALM, may allow for similar advantages with a relatively shorter learning curve. Using the existing Da Vinci Si and Xi robotic platforms, a specialized multi-lumen 2.5-cm port is introduced in the umbilicus. Subsequently, the robotic laparoscope, a bedside assistant port, and two robotic instruments are introduced into this port. The robotic instruments are operated through two curved cannulas (Fig. 1), thus enabling the triangulation which is essential for easier surgical maneuvers. To date, this configuration has been used for single-site RALM in small case series. Gargiulo et al. reported their experience with 10 cases of single-site RALM, all successfully completed without complications or conversions [41].
Current and future technological developments include specially designed single-site robotic systems, rather than a robotic platform adjusted for single-site surgery. Those specially designed single-site robotic platforms contain wristed robotic instruments, which are not available in the current platform. The new Da Vinci single port system is designed for urologic procedures and contains three articulating robotic instruments which are unfolded from a 25-mm guide. A somewhat similar system is the Titan Medical robotic platform, called SPORT. This system contains a three-dimensional laparoscope and two robotic arms deployed through a 15-mm incision. The Memic robotic system, currently under development, is aimed to provide a robotic platform for natural orifice transluminal endoscopic surgery (NOTES). It may be used for robotic myomectomy through the vagina. Lastly, The Medrobotics robotic system, Flex Robotic System, was recently approved for marketing by the FDA. The laparoscope of this system can be steered along non-linear paths, allowing for single-site and NOTES procedures. Other than offering advanced technologies, in order to prove superior to the current robotic system, the new robotic systems should offer reduced costs and easier and faster setup.
Conclusions
Minimally invasive myomectomy improves upon short-term surgical complications, post-operative pain, and recovery period when compared to laparotomic myomectomy. LM and RALM have overall similar benefits and reproductive outcomes, although the cost of RALM remains a significant drawback of this surgical approach. These two routes for minimally invasive myomectomy have been recently scrutinized in view of the possible risks associated with specimen removal via power morcellation, and future implementation of these surgeries will likely depend on development on safe and efficient techniques for morcellation.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Baird DD, Dunson DB, Hill MC, Cousins D, Schectman JM. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003;188:100–7.
Vilos GA, Allaire C, Laberge PY, Leyland N, Vilos AG, Murji A, Chen I. The management of uterine leiomyomas. J Obstet Gynaecol Can. 2015;37:157–81.
Stewart EA. Uterine fibroids. N Engl J Med. 2015;372:1646–55.
Di Spiezio Sardo A, Mazzon I, Bramante S, Bettocchi S, Bifulco G, Guida M, Nappi C. Hysteroscopic myomectomy: a comprehensive review of surgical techniques. Hum Reprod Update. 2008;14:101–19.
Iavazzo C, Mamais I, Gkegkes ID. Robotic assisted vs laparoscopic and/or open myomectomy: systematic review and meta-analysis of the clinical evidence. Arch Gynecol Obstet. 2016;295:5–17 A meta-analysis and comprehensive review of the literature on the relative pros and cons of laparotomic, laparoscopic, and robotic-assisted myomectomy.
Chamberlain G. The master of myomectomy. J R Soc Med. 2003;96:302–4.
Semm K, Mettler L. Technical progress in pelvic surgery via operative laparoscopy. Am J Obstet Gynecol. 1980;138:121–7.
Tsui C, Klein R, Garabrant M. Minimally invasive surgery: national trends in adoption and future directions for hospital strategy. Surg Endosc. 2013l;27:2253–7.
Advincula AP, Song A, Burke W, Reynolds RK. Preliminary experience with robot-assisted laparoscopic myomectomy. J Am Assoc Gynecol Laparosc. 2004;11:511–8.
Barakat EE, Bedaiwy MA, Zimberg S, Nutter B, Nosseir M, Falcone T. Robotic-assisted, laparoscopic, and abdominal myomectomy: a comparison of surgical outcomes. Obstet Gynecol. 2011;117:256–65.
Gargiulo AR, Srouji SS, Missmer SA, Correia KF, Vellinga TT, Einarsson JI. Robot-assisted laparoscopic myomectomy compared with standard laparoscopic myomectomy. Obstet Gynecol. 2012;120:284–91 The largest retrospective study comparing laparoscopic and robotic-assisted myomectomy.
Bedient CE, Magrina JF, Noble BN, Kho RM. Comparison of robotic and laparoscopic myomectomy. Am J Obstet Gynecol. 2009;201:566.e1–5.
Göçmen A, Şanlıkan F, Uçar MG. Comparison of robotic-assisted laparoscopic myomectomy outcomes with laparoscopic myomectomy. Arch Gynecol Obstet. 2013;287:91–6.
Nezhat C, Lavie O, Hsu S, Watson J, Barnett O, Lemyre M. Robotic assisted laparoscopic myomectomy compared with standard laparoscopic myomectomy: a retrospective matched control study. Fertil Steril. 2009;91:556–9.
Pluchino N, Litta P, Freschi L, Russo M, Simi G, Santoro AN, Angioni S, Gadducci A, Cela V. Comparison of the initial surgical experience with robotic and laparoscopic myomectomy. Int J Med Robot. 2014;10:208–12.
Gobern JM, Rosemeyer CJ, Barter JF, Steren AJ. Comparison of robotic, laparoscopic, and abdominal myomectomy in a community hospital. JSLS. 2013;17:116–20.
Hsiao SM, Lin HH, Peng FS, Jen PJ, Hsiao CF, Tu FC. Comparison of robot-assisted laparoscopic myomectomy and traditional laparoscopic myomectomy. J Obstet Gynaecol Res. 2013;39:1024–9.
Hickman LC, Kotlyar A, Shue S, Falcone T. Hemostatic techniques for myomectomy: an evidence-based approach. J Minim Invasive Gynecol. 2016;23:497–504 A review on the different techniques for reducing blood loss during myomectomy, applicable for all surgical routes.
Zhang Y, Ma D, Li X, Zhang Q. Role of barbed sutures in repairing uterine wall defects in laparoscopic myomectomy: a systemic review and meta-analysis. J Minim Invasive Gynecol. 2016;23:684–91.
Alton K, Sullivan S, Udaltsova N, Yamamoto M, Zaritsky E. Same-day discharge after minimally invasive myomectomy. Obstet Gynecol. 2016;127:539–44 Interesting study describing the protocol for same-day discharge following minimally invasive myomectomy, showing low rates of re-admissions.
Sarlos D, Kots L, Stevanovic N, von Felten S, Schär G. Robotic compared with conventional laparoscopic hysterectomy: a randomized controlled trial. Obstet Gynecol. 2012;120:604–11.
Paraiso MF, Ridgeway B, Park AJ, Jelovsek JE, Barber MD, Falcone T, Einarsson JI. A randomized trial comparing conventional and robotically assisted total laparoscopic hysterectomy. Am J Obstet Gynecol. 2013;208:368.e1–7.
Anger JT, Mueller ER, Tarnay C, Smith B, Stroupe K, Rosenman A, Brubaker L, Bresee C, Kenton K. Robotic compared with laparoscopic sacrocolpopexy: a randomized controlled trial. Obstet Gynecol. 2014;123:5–12.
Bhave Chittawar P, Franik S, Pouwer AW, Farquhar C. Minimally invasive surgical techniques versus open myomectomy for uterine fibroids. Cochrane Database Syst Rev. 2014;10:CD004638.
Pundir J, Pundir V, Walavalkar R, Omanwa K, Lancaster G, Kayani S. Robotic-assisted laparoscopic vs abdominal and laparoscopic myomectomy: systematic review and meta-analysis. J Minim Invasive Gynecol. 2013;20:335–45.
Pitter MC, Gargiulo AR, Bonaventura LM, Lehman JS, Srouji SS. Pregnancy outcomes following robot-assisted myomectomy. Hum Reprod. 2013;28:99–108.
Buckley VA, Nesbitt-Hawes EM, Atkinson P, Won HR, Deans R, Burton A, Lyons SD, Abbott JA. Laparoscopic myomectomy: clinical outcomes and comparative evidence. J Minim Invasive Gynecol. 2015;22:11–25 An Interesting review study summarizing clinically and surgically important data on laparoscopic myomectomy.
Pitter MC, Srouji SS, Gargiulo AR, Kardos L, Seshadri-Kreaden U, Hubert HB, Weitzman GA. Fertility and symptom relief following robot-assisted laparoscopic myomectomy. Obstet Gynecol Int. 2015;2015:967–8.
Purohit P, Vigneswaran K. Fibroids and infertility. Curr Obstet Gynecol Rep. 2016;5:81–8.
Metwally M, Cheong YC, Horne AW. Surgical treatment of fibroids for subfertility. Cochrane Database Syst Rev. 2012;11:CD003857.
Pritts EA, Parker WH, Olive DL. Fibroids and infertility: an updated systematic review of the evidence. Fertil Steril. 2009;91:1215–23.
Food and Drug Administration. Updated laparoscopic uterine power morcellation in hysterectomy and myomectomy: FDA safety communication. 2014. www.fda.gov/medicaldevices/safety/alertsandnotices/ucm424443.htm
Barron KI, Richard T, Robinson PS, Lamvu G. Association of the U.S. Food and Drug Administration morcellation warning with rates of minimally invasive hysterectomy and myomectomy. Obstet Gynecol. 2015;126:1174–80 A recent study demonstrating the large impact of the FDA morcellation warning on the rates of minimally invasive myomectomy.
Pritts EA, Vanness DJ, Berek JS, Parker W, Feinberg R, Feinberg J, Olive DL. The prevalence of occult leiomyosarcoma at surgery for presumed uterine fibroids: a meta-analysis. Gynecol Surg. 2015;12:165–77.
Parker WH, Kaunitz AM, Pritts EA, Olive DL, Chalas E, Clarke-Pearson DL, Berek JS, Leiomyoma Morcellation Review Group. U.S. Food and Drug Administration’s guidance regarding morcellation of leiomyomas: well-intentioned, but is it harmful for women? Obstet Gynecol. 2016;127:18–22.
Venturella R, Rocca ML, Lico D, La Ferrera N, Cirillo R, Gizzo S, Morelli M, Zupi E, Zullo F. In-bag manual versus uncontained power morcellation for laparoscopic myomectomy: randomized controlled trial. Fertil Steril. 2016;105:1369–76.
Cardozo ER, Clark AD, Banks NK, Henne MB, Stegmann BJ, Segars JH. The estimated annual cost of uterine leiomyomata in the United States. Am J Obstet Gynecol. 2012;206:211.e1–9.
Behera MA, Likes 3rd CE, Judd JP, Barnett JC, Havrilesky LJ, Wu JM. Cost analysis of abdominal, laparoscopic, and robotic-assisted myomectomies. J Minim Invasive Gynecol. 2012;19:52–7.
O’Sullivan OE, O’Carroll M, Hewitt M, O’Reilly BA. Gynaecological robotic surgery in an Irish setting—cost analysis. Gynecol Surg. 2013;10:129–35.
Song T, Kim TJ, Lee SH, Kim TH, Kim WY. Laparoendoscopic single-site myomectomy compared with conventional laparoscopic myomectomy: a multicenter, randomized, controlled trial. Fertil Steril. 2015;104:1325–31.
Gargiulo AR, Lewis EI, Kaser DJ, Srouji SS. Robotic single-site myomectomy: a step-by-step tutorial. Fertil Steril. 2015;104:e13.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
Joseph H. Nathan and Noam Smorgick declare that they have no conflict of interest.
Nir Shvalb declares having licensed the patent numbered US9039057 B2.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Minimally Invasive Gynecologic Surgery
Rights and permissions
About this article
Cite this article
Nathan, J.H., Shvalb, N. & Smorgick, N. Robotic-Assisted Laparoscopic Myomectomy versus Traditional Laparoscopic Myomectomy: Are They the Same?. Curr Obstet Gynecol Rep 5, 341–347 (2016). https://doi.org/10.1007/s13669-016-0182-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13669-016-0182-y