Abstract
Massive obstetric hemorrhage is the leading cause of maternal morbidity and direct obstetric death in developed countries. It is also the most frequent reason for maternal ICU admission. Mismanagement of maternal hemorrhage is one of the potentially preventable causes of maternal mortality in the USA. Thromboelastometry (TEM)—previously named rotational thromboelastography (ROTEG) or rotational thromboelastometry (ROTEM)—is an established viscoelastic method for hemostasis testing in whole blood. It investigates the interaction of coagulation factors, their inhibitors, anticoagulant drugs, and blood cells (especially platelets) during clotting and subsequent fibrinolysis. The rotational conditions mimic the sluggish flow of blood in veins. Introduction into clinical practice of point-of-care TEM provides prompt bedside analysis of hemostasis. Utilization of point-of-care TEM allows for the transition from one-size-fits-all fixed-ratio resuscitation to a personalized goal-directed transfusion strategy. Such an individualization of treatment for hemorrhage-related coagulopathy will almost certainly lead to improvements in clinical outcome and a reduced cost of care for patients with massive obstetric hemorrhage.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstetric hemorrhage is the leading cause of maternal mortality worldwide, accounting for 27 % of obstetric-related maternal deaths in 2014 [1]. In developed countries, maternal hemorrhage is the leading cause of direct obstetric death (i.e., death caused by complications of pregnancy itself as opposed to decompensation of preexisting medical conditions) [1, 2]. In the USA, obstetric hemorrhage is also a major cause of maternal morbidity and the most frequent reason for maternal ICU admission [3, 4]. Recent data suggests that the incidence of postpartum hemorrhage is increasing in the USA [5] and worldwide [6].
Mismanagement of obstetric hemorrhage has been recognized as a potentially preventable cause of maternal mortality [7, 8]. The development and implementation of massive obstetric hemorrhage protocols in all obstetric units was recommended in an attempt to improve the situation [9]. Massive obstetric hemorrhage protocols using the principles of damage control resuscitation and supporting fixed-ratio transfusion of blood products were developed and accepted in the USA and Great Britain [10–12].
Damage Control Resuscitation
The principles of damage control resuscitation were developed based on data from American military and civilian trauma medicine. The minimization of crystalloid infusion and the early transfusion of fresh frozen plasma (FFP) and platelets (in a ratio of as close as possible to 1:1:1 with packed red blood cells [PRBC]) was thought to decrease the risk of dilutional and consumptional coagulopathy and improve survival of trauma victims [13]. Adjustment of the ratio of transfused blood products based on the results of traditional coagulation tests was not recommended since doing so could lead to a delay in the administration of adequate amounts of coagulation factors.
Initial publications reported dramatic improvements in the survival of bleeding trauma patients after implementation of damage control resuscitation [14, 15]. However, later review of the data failed to demonstrate sufficient evidence to recommend damage control resuscitation as a standard of care [16]. Even the proponents of the damage control resuscitation strategy in their most recent study did not find any association between mortality and ratio of transfused FFP and platelets in the 24 h since admission [16]. Experts recommended adjustment of the blood product transfusions based on analysis of hemostasis, which may be especially important during management of obstetric hemorrhage [17].
Hemostasis During Pregnancy
Pregnancy is a hypercoagulable state. Indeed, the risk of deep venous thrombosis is five to six times greater for pregnant compared to non-pregnant women, with an absolute incidence of 1–3 per 1000 live births [18]. The plasma level of most coagulational factors, including fibrinogen, at term may be double that seen in non-pregnant women. In addition, the effectiveness of the anticoagulant system (i.e., protein S concentration and protein C activity) is significantly diminished during pregnancy [19]. Together with existing venous stasis in the lower extremities, one would expect such systemic changes in hemostasis to result in much greater incidence of deep venous thrombosis than is actually observed.
Holmes and Wallace [20] suggested that the existence of some other hemostatic alterations might partly balance the well-known procoagulation changes. For example, monocyte tissue factor expression (important for initiating the coagulation cascade by forming complexes with factor VII) and the activity of factor XI (important for thrombin generation) are decreased during pregnancy. The activity of plasminogen activator inhibitor is increased during pregnancy, which probably explains the decrease in the activity of tissue plasminogen activator [20]. At the same time, plasminogen level increases during pregnancy and alpha 2-antiplasmin concentration decreases during pregnancy, which may predispose patients to fibrinolysis. Finally, elevated concentration of D-dimer postpartum also suggests elevated fibrinolytic activity [21].
It seems possible that transfusion of FFP derived from non-pregnant donors may have a negative effect on pregnant recipients who have a markedly different hemostatic profile. The risk of progressive hemorrhage-induced imbalance of the coagulation system following inappropriate “blind” transfusion of blood products underlines the importance of prompt and individualized hemostasis analysis during the management of obstetric hemorrhage.
Assessment of Hemostasis
Traditional coagulation plasma tests—such as fibrinogen measurements, partial thromboplastin time (PTT), prothrombin time (PT), and international normalized ratio (INR)—do not provide information about the ultimate strength of the clot, the time required for propagation from initial clotting to the formation of a maximally functioning clot, or the magnitude of fibrinolysis. Viscoelastic testing for the evaluation of hemostasis in whole blood was developed by Hartert in 1948 [22]. It allows for the measurement of the interactions between coagulation factors, their inhibitors, anticoagulant drugs, and cellular components (especially platelets) during the sequential phases of clot formation and clot lysis over time. Unfortunately, early implementations of viscoelastic testing did not provide results rapidly enough to guide transfusion therapy of actively bleeding patients.
Rotational Thromboelastometry
Thromboelastometry (TEM), previously named rotational thromboelastography (ROTEG) or rotational thromboelastometry (ROTEM), is an established viscoelastic method for hemostasis testing in whole blood. The rotational conditions mimic the sluggish flow of blood in veins. Rotational TEM comprehensively assesses hemostasis at the bedside within 10 to 20 min of the acquisition of the blood sample, thus allowing clinicians to make individualized goal-directed adjustments to the transfusion. ROTEM® is a rotational thromboelastometry machine, which graphically displays the process of coagulation triggered in the blood sample by ellagic acid (INTEM assay) or tissue factor (EXTEM assay). It also demonstrates alterations in clot formation when platelets in the blood sample are deactivated by cytochalasin A (FIBTEM assay), when fibrinolytic activity is suppressed by aprotinin (APTEM assay), and when the anticoagulation effect of heparin is diminished by heparinase (HEPTEM assay).
The assessment of hemostasis is performed using the following parameters of the thromboelastogram (Fig. 1): Clotting time (CT) is the amount of time from the start of the test until the beginning of clot formation. A prolonged CT suggests a deficiency of one or more coagulation factors. CT prolongation in only EXTEM suggests a deficiency of coagulation factors in the extrinsic pathway (due, for example, to the effects of Coumadin). CT prolongation in only INTEM is seen most commonly in patients receiving heparin or low molecular weight heparin. A reduction of the CT in the HEPTEM assay (which includes the addition of heparinase) would confirm this effect.
Schematic TEMOGRAM with thromboelastometry parameters. Clotting time (CT) refers to the time measured from the beginning of the test until the beginning of clot formation. Clot formation time (CFT) refers to the time measured from the end of the CT interval until a 20-mm amplitude is reached on the TEMOGRAM. The maximum amplitude of the graph is measured either as an absolute parameter independent of time (maximum clot firmness [MCF]) or at a specific point in time after starting the test (e.g., A 5 refers to the maximum amplitude at 5 min, A 10 refers to the maximum amplitude at 10 min). Maximum lysis (ML) refers to the percentage of lost firmness of the clot at a given point in time or as a percentage of the remaining clot firmness comparing with MCF at 30 min (LI30), 45 min (LI45), or 60 min (LI60)
Clot formation time (CFT) refers to the amount of time measured from the end of the CT interval until a 20-mm amplitude is reached, and alpha angle describes the tangent at the 20-mm amplitude point. Both CFT and alpha angle reflect the speed of clot development. Prolonged CFT and/or low alpha angle are typically caused by one or more of the following conditions: thrombocytopenia, platelet dysfunction, hypofibrinogenemia, or dysfunctional fibrin polymerization.
The maximum amplitude of the graph is measured either as an absolute parameter independent of time (maximum clot firmness [MCF]) or at a specific point in time after starting the test (e.g., A 5 refers to the maximum amplitude at 5 min, A 10 refers to the maximum amplitude at 10 min). This measurement reflects the functionality (strength) of the clot. As with CFT and alpha angle, a decrease in the maximum amplitude suggests one or more of the following conditions: thrombocytopenia, platelet dysfunction, hypofibrinogenemia, or dysfunctional fibrin polymerization.
Maximum lysis (ML) refers to the percentage of lost firmness of the clot relative to MCF at the end of the test. The lysis index at 30 min (LI30) reflects the percentage of lost clot firmness at 30 min. An abnormally high ML index suggests the presence of hyperfibrinolysis and indicates that antifibrinolytic therapy may be needed.
The use of rotational TEM-based transfusion protocol during cardiac surgery resulted in a significant decrease in PRBC, FFP, and platelet transfusions; resulted in a reduced duration of postoperative mechanical ventilation and length of ICU stay; decreased the rate of composite adverse events; reduced costs of hemostatic therapy; and resulted in a diminished 6-month mortality rate [23]. Similarly, the use of ROTEM® for the management of hemorrhage in patients with end-stage liver disease was associated with decreased rates of blood transfusion and reduced costs of hospitalization [24]. Indeed, in a subsequent report, the use of rotational TEM in 1105 liver transplant surgeries demonstrated a 60 % reduction in PRBC transfusion and an 89 % reduction in FFP transfusion [25].
Rotational Thromboelastometry in Obstetric Practice
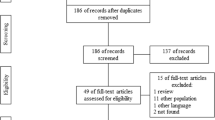
We are still accumulating data and gaining experience with the use of rotational TEM during the management of acute obstetric hemorrhage. In the absence of data from large randomized controlled studies, information about the use of TEM in obstetrics should be interpreted with caution.
In 2009, Huissoud et al. [26] reported on the normal values of rotational TEM during pregnancy. INTEM, EXTEM, and FIBTEM assays were measured in 84 pregnant patients (17 women in the first, 9 in the second, and 58 in the third trimester of pregnancy) and compared them to the TEM results from 20 healthy non-pregnant women. Pregnancy at term did not significantly alter CT or clot lysis index at 30 min (LI30), while MCF and clot amplitude at 5 and 15 min (A 5 and A 15) were significantly increased during the second and the third trimesters. The average MCF of FIBTEM in the third trimester was 19 mm (range, 17–23 mm) versus 13 mm (range, 11–16 mm) for non-pregnant women, which is consistent with the hyperfibrinogenemia of normal pregnancy. The addition of the antifibrinolytic agent aprotinin to the analyzed blood sample (APTEM test) did not change the results of thromboelastometry. Huissoud et al. concluded that “the hypercoagulability associated with pregnancy is not a consequence of hyperactivation of coagulation, but of an enhanced potential of the coagulation response once the process has been initiated” [26]. Moreover, the authors did not find any evidence of hyperfibrinolysis during pregnancy, based on the unchanged value of clot lysis index (LI30) and the absence of alteration of the APTEM results.
de Lange et al. [27••] reported similar hypercoagulable results (EXTEM: CT 31–63 s, CFT 41–120 s, and MCF 42–78 mm, INTEM: CT 109–225 s, CFT 40–103 s, and MCF 63–78 mm, FIBTEM: CT 31–79 s and MCF 13–45 mm) based on the analysis of hemostasis in 161 healthy parturients.
Charbit et al. [28] demonstrated that, for bleeding obstetrical patients, a plasma fibrinogen level below 2 g/L had a 100 % positive predictive value for severe hemorrhage. In a study comparing 37 bleeding obstetrical patients with 54 healthy non-bleeding parturients, Huissoud et al. [29] confirmed a strong correlation between FIBTEM results and plasma fibrinogen concentration. FIBTEM amplitude of 5 mm at 5 min (A 5) and 6 mm at 15 min (A 15) had 100 % sensitivity and 85 and 88 % specificity, respectively, for predicting severe hypofibrinogenemia (<1.5 g/L). Mallaiah et al. [30••] used ROTEM to detect severe hypofibrinogenemia (FIBTEM A 5 < 7 mm) and to guide administration of fibrinogen concentrate for 51 obstetric patients with severe hemorrhage. All the patients with FIBTEM A 5 lower than 7 mm were treated with the initial dose of 3 g of fibrinogen concentrate. Actively bleeding patients or those with a high risk of bleeding and FIBTEM A 5 within 7–12 mm also received 3 g of fibrinogen concentrate. Further treatment with fibrinogen concentrate was adjusted based on the results of ROTEM testing repeated in 10-min intervals. If patients had normal results of FIBTEM test but had EXTEM A 5 lower than 47 mm, then one unit of platelets was given. Two units of FFP were given to the patients, if EXTEM CT was longer than 100 s. This approach resulted in the avoidance of volume overload (p = 0.038) and a significantly decreased use of blood products (p = 0.0004).
In our experience, the use of point-of-care TEM allowed for the transition from damage control-based management of patients with severe postpartum hemorrhage to goal-directed transfusion with the goal of avoiding severe hypofibrinogenemia, defined as A 5 > 6 mm (Fig. 2). In the evaluation of the first 2 years of our experience with point-of-care rotational TEM, we compare clinical outcomes and direct cost of hospitalization between 85 consecutive patients with severe obstetric hemorrhage (estimated blood loss more than 1500 mL), who were either managed before (57 patients) or after (28 patients) ROTEM® became available at our hospital. The results of this retrospective analysis were presented at the 110th Annual Scientific Meeting of the American Society of Anesthesiologists (ASA) in 2015 [31]. Our algorithm was slightly different from that implemented by Mallaiah et al. [30••], and we used cryoprecipitate instead of fibrinogen concentrate to correct hypofibrinogenemia. Nevertheless, similar to the report by Mallaiah et al., the patients managed based on the results of point-of-care TEM received significantly lower volumes of blood products (p < 0.001), required fewer hysterectomies and ICU admissions (p < 0.001 for both), and had shorter durations of postpartum hospitalization (p < 0.001), probably due to faster correction of coagulopathy, diminished blood loss, and less frequent volume overload. Not surprisingly, among patients who gave birth within 36 h of admission to hospital, the average direct cost of hospitalization among 17 bleeding parturients managed with the use of TEM was around $6000 compared with $10,000 for the 37 patients who received fixed-ratio transfusions [31].
Abnormal TEMOGRAM of a patient with vaginal bleeding (due to placental abruption). (1) Normal clotting time (CT) in INTEM and EXTEM assays suggests the absence of clinically significant deficiency of the clotting factors in “extrinsic” and “intrinsic” pathways. There is no need for FFP transfusion. (2) Prolonged clot formation time (CFT) in INTEM and EXTEM and decreased maximum amplitude at 20 min (A 20) in EXTEM suggests deficiency of fibrinogen function and/or deficiency of platelet function. There are possible indications for cryoprecipitate and/or platelet transfusion. The analysis of FIBTEM assay results will help to discriminate between platelet and fibrinogen deficiency. (3) Significantly decreased maximum amplitude of FIBTEM assay at 10 and 20 min A 10 and A 20 suggests that profound deficiency of fibrinogen function is the main cause of hypocoagulation. The patient received an appropriate dose of fibrinogen (via cryoprecipitate transfusion), which normalized the patient’s hemostasis and stopped the bleeding
Conclusions
We are in the process of accumulating data to assess the value of point-of-care TEM in the management of patients with acute obstetric hemorrhage. Published results from small studies suggest that point-of-care TEM allows quick and accurate analysis of hemostasis of obstetric patients, thus providing information that will allow clinicians to pursue individualized, goal-directed transfusion therapy. The weight of evidence in the literature suggests that, in the setting of acute obstetrical hemorrhage, the use of point-of-care TEM may result in faster recognition and correction of coagulopathy, decreased use of blood products, diminished risk of volume overload, fewer ICU admissions, shortened length of hospitalization, and lower cost of hospitalization.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Global Health. 2014;2(6):e323–33.
Cristina Rossi A, Mullin P. The etiology of maternal mortality in developed countries: a systematic review of literature. Arch Gynecol Obstet. 2012;285(6):1499–503.
Callaghan WM, MacKay AP, Berg CJ. Identification of severe maternal morbidity during delivery hospitalizations, United States, 1991–2003. Am J Obstet Gynecol. 2008;199(2):133–e1.
Liu S, Joseph KS, Bartholomew S, Fahey J, Lee L, Allen AC, et al. Temporal trends and regional variations in severe maternal morbidity in Canada, 2003 to 2007. J Obstet Gynaecol Can. 2010;32(9):847–55.
Callaghan WM, Kuklina EV, Berg CJ. Trends in postpartum hemorrhage: United States, 1994–2006. Am J Obstet Gynecol. 2010;202(4):353–e1.
Knight M, Callaghan WM, Berg C, Alexander S, Bouvier-Colle MH, Ford JB, et al. Trends in postpartum hemorrhage in high resource countries: a review and recommendations from the International Postpartum Hemorrhage Collaborative Group. BMC Pregnancy Childbirth. 2009;9(1):55.
Fuchs KM, Miller RS, Berkowitz RL. Optimizing outcomes through protocols, multidisciplinary drills, and simulation. Semin Perinatol. 2009;33:104–8.
Brace V, Kernagham D, Penney G. Learning from adverse clinical outcomes: major obstetric haemorrhage in Scotland, 2003–05. BJOG. 2007;114:1388–96.
Joint Commission. Sentinel event alert, issue 44: preventing maternal death. (January 26, 2010).
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 76. Postpartum hemorrhage. Obstet Gynecol. 2006;108(4):1039–47.
CMQCC. Obstetric hemorrhage toolkit: obstetric hemorrhage care guidelines and compendium of best practices reviewed by CDPH-MCAH: 11/24/09. http://www.cdph.ca.gov/programs/mcah/Documents/MCAH-OBHemorrhageToolkit.pdf
Royal College of Obstetrician and Gynaecologists. Postpartum hemorrhage: prevention and management. 2011.
Holcomb JB, Jenkins D, Rhee P, Johannigman J, Mahoney P, Mehta S, et al. Damage control resuscitation: directly addressing the early coagulopathy of trauma. J Trauma. 2007;62:307–10.
Borgman MA, Spinella PC, Perkins JG, Grathwohl KW, Repine T, Beekley AC, et al. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma. 2007;63(4):805–13.
Holcomb JB, Wade CE, Michalek JE, Chisholm GB, Zarzabal LA, Schreiber MA, et al. Increased plasma and platelet to red blood cell ratios improves outcome in 466 massively transfused civilian trauma patients. Ann Surg. 2008;248(3):447–58.
Holcomb JB, Fox EE, Wade CE, PROMMTT Study Group. The Prospective Observational Multicenter Major Trauma Transfusion (PROMMTT) study. J Trauma Acute Care Surg. 2013;75:S1–2.
Dzik WH, Blajchman MA, Fergusson D, Hameed M, Henry B, Kirkpatrick AW, et al. Clinical review: Canadian National Advisory Committee on Blood and Blood Products—massive transfusion consensus conference 2011: report of the panel. Crit Care. 2011;15(6):242.
McColl MD, Ramsay JE, Tait RC, Walker ID, McCall F, Conkie JA, et al. Risk factors for pregnancy associated venous thromboembolism. Thromb Haemost. 1997;78(4):1183–8.
Younis JS, Shukha M, Ben-Ami M, Izhaki I, Blumenfeld Z, Brenner B, et al. Evaluation of protein C global assay during normal pregnancy and after assisted reproduction. Obstet Gynecol. 2010;115:969–74.
Holmes VA, Wallace JM. Haemostasis in normal pregnancy: a balancing act? Biochem Soc Trans. 2005;33(2):428–32.
Epiney M, Boehlen F, Boulvain M, Reber G, Antonelli E, Morales M, et al. D‐dimer levels during delivery and the postpartum. J Thromb Haemost. 2005;3(2):268–71.
Hartert H. Blutgerinnungsstudien mit der Thrombelastographie, einem neuen Untersuchungsvefahren. Klin Wochenschr. 1948;26:577–83.
Weber CF, Görlinger K, Meininger D, Herrmann E, Bingold T, Moritz A, et al. Point-of-care testing: a prospective, randomized clinical trial of efficacy in coagulopathic cardiac surgery patients. Anesthesiology. 2012;117(3):531–47.
Saner FH, Gieseler RK, Akız H, Canbay A, Görlinger K. Delicate balance of bleeding and thrombosis in end-stage liver disease and liver transplantation. Digestion. 2013;88(3):135–44.
Goerlinger K, Dirkmann D, Müller-Beissenhirtz H, Paul A, Hartmann M, Saner F. Thromboelastometry-based perioperative coagulation management in visceral surgery and liver transplantation: experience of 10 years and 1105 liver transplants. Liver Transpl. 2010;16(1):S86.
Huissoud C, Carrabin N, Benchaib M, Fontaine O, Levrat A, Massignon D, et al. Coagulation assessment by rotation thrombelastometry in normal pregnancy. Thromb Haemost. 2009;101(4):755–61.
de Lange NM, van Rheenen-Flach LE, Lancé MD, Mooyman L, Woiski M, van Pampus EC, et al. Peri-partum reference ranges for ROTEM® thromboelastometry. Br J Anaesth. 2014;112(5):852–9. One of the first articles, which examined ROTEM® thromboelastometry in the peri-partum period. Reference values for ROTEM ® parameters were reported for the 1st time.
Charbit B, Mandelbrot L, Samain E, Baron G, Haddaoui B, Keita H, et al. The decrease of fibrinogen is an early predictor of the severity of postpartum hemorrhage. J Thromb Haemost. 2007;5(2):266–73.
Huissoud C, Carrabin N, Audibert F, Levrat A, Massignon D, Berland M, et al. Bedside assessment of fibrinogen level in postpartum haemorrhage by thrombelastometry. BJOG. 2009;116(8):1097–102.
Mallaiah S, Barclay P, Harrod I, Chevannes C, Bhalla A. Introduction of an algorithm for ROTEM-guided fibrinogen concentrate administration in major obstetric haemorrhage. Anaesthesia. 2015;70(2):166–75. This is the first paper, which introduced an algorithm for ROTEM-guided fibrinogen concentrate administration in major obstetric hemorrhage. The study proved that fibrinogen concentrate allowed timely correction of coagulation deficits associated with major obstetric hemorrhage, which, in turn, reduced the requirement for blood component therapy and decreased the risks of recounted complications.
Abstract. 110th Annual Scientific Meeting of the American Society of Anesthesiologists
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Denis Snegovskikh, Zachary Walton, and Dmitri Souzdalnitski declare no potential conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with animal subjects performed by any of the authors. The analysis of utilization of ROTEM at Yale New Haven Hospital was performed after the approval of the Human Research Protection Program.
Additional information
This article is part of the Topical Collection on High-risk Gestation and Prenatal Medicine
Rights and permissions
About this article
Cite this article
Snegovskikh, D., Walton, Z. & Souzdalnitski, D. Point-of-Care Thromboelastometry in the Management of Acute Obstetric Hemorrhage. Curr Obstet Gynecol Rep 5, 244–249 (2016). https://doi.org/10.1007/s13669-016-0172-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13669-016-0172-0