Abstract
Purpose of Review
The objective of this review was to consolidate available published information on the implementation and evaluation of salt reduction interventions in low- and middle-income countries (LMICs).
Recent Findings
The Science of Salt database (made up of studies identified in a weekly Medline search) was used to retrieve articles related to the implementation of salt reduction interventions from June 2013 to February 2020. Studies that measured the effects of the interventions in LMICs, based on four outcome measures—salt intake; sodium levels in foods; knowledge, attitudes, and behaviours (KABs) towards salt; and blood pressure—were included. Results were summarised overall and according to subgroups of intervention type, duration, sample size, country’s income class, and regional classification. The review identified 32 studies, representing 13 upper middle-income and four lower middle-income countries. The main salt reduction interventions were education, food reformulation, and salt substitution; and many interventions were multi-faceted. More studies reported a positive effect of the interventions (decreased salt intake (12/17); lower sodium levels in foods or compliance with agreed targets (6/6); improved KAB (17/19); and decreased blood pressure (10/14)) than a null effect, and no study reported a negative effect of the intervention. However, many studies were of small scale and targeted specific groups, and none was from low-income countries.
Summary
Consumer education, food reformulation, and salt substitution, either alone or in combination, were effective in their target populations. Supporting scale-up of salt reduction interventions in LMICs is essential to cover broader populations and to increase their public health impact.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The most recent Global Burden of Disease (GBD) study estimated that cardiovascular disease (CVD) remains the leading cause of death and disability globally in 2019, causing around 19 million deaths and 393 million disability adjusted life years (DALYs) [1•]. High systolic blood pressure was the leading risk factor for CVD, responsible for around 10 million deaths and more than 50% of DALYs due to CVD [1•]. In the same year, of all the dietary risk factors, high salt intake accounted for the most deaths (1.7 million) and DALYs (40.5 million) due to CVD [2]. By the World Bank’s income levels [3], the contribution of high salt intake to CVD burden was largest in upper middle-income countries (about 60% of all deaths and DALYs), followed by lower middle-income countries (25%), high-income countries (11%), and low-income countries (4%) [2]. Undoubtedly, high salt intake is a public health problem, particularly in middle-income countries.
Population salt reduction is a priority action for the prevention and control of noncommunicable diseases (NCD), including CVD, and in 2013, Member States of the World Health Organization (WHO) committed to a global target to reduce salt consumption by 30% by 2025 [4]. In 2014, 75 countries had national salt reduction initiatives [5]. This represented a two-fold increase in the total number of initiatives identified in 2010 [6], and a huge increase in salt reduction strategies in low- and middle-income countries (LMIC), from seven in 2010 to 33 in 2014 [5]. A subsequent review showed a further increase in the number of initiatives in upper middle-income (from 21 to 30) and lower middle-income countries (from 11 to 13) [7••]. Still, more than half of the 96 national salt reduction initiatives in 2019 were from high-income countries [7••]. A review of the impact of population-level salt reduction interventions reported that several countries achieved substantial reductions in salt intake over time [8]. Further reviews have shown the same [9,10,11]; however, most of the evidence on salt reduction intervention effectiveness were from high-income countries, with limited information from LMICs [7••].
In 2016, the WHO published the SHAKE Technical Package for Salt Reduction, comprising simple, cost-effective interventions to support countries in the implementation of salt reduction strategies [12]. However, this was based mainly on the experience from high-income and upper middle-income countries; thus, there is limited knowledge and understanding about implementing these interventions in other contexts. Given that a considerable disease burden related to excessive salt intake is present in LMICs, it is important to consider how best to support these countries to implement effective programs to reduce population salt intake. The objective of this review was thus to consolidate knowledge on the implementation and evaluation of salt reduction interventions in LMICs, with a view to supporting scale-up of interventions across these settings.
Methods
Articles related to the implementation of salt reduction interventions in LMICs were identified through a weekly Medline literature search, which makes up the Science of Salt database. The detailed search methodologies for the Science of Salt Weekly have been published previously [13]. Briefly, articles identified each week are screened for eligibility based on established inclusion and exclusion criteria [13]. Eligible studies (related to the relationship of dietary salt and health, and achieving dietary salt reduction in populations) are included in the Science of Salt database.
For this review, articles identified during the runtime of the Science of Salt Weekly initiative from June 2013 to February 2020 were retrieved. Studies that reported on the effects of salt reduction interventions in LMICs were assessed for eligibility. Studies were included if they evaluated or measured the effects of salt reduction interventions, including national, sub-national, or pilot studies. Outcomes considered included changes in salt intake; salt/sodium levels in foods; knowledge, attitudes, and behaviours (KABs) towards salt; and blood pressure. In addition, studies that assessed compliance with targets for sodium levels in foods were considered. All types of population were considered, including population subgroups, high-risk groups, and sick populations (with the view to scaling up). On the contrary, modelling studies, reviews, taste-test interventions, and studies that only described baseline data without information on intervention effectiveness were excluded.
A narrative synthesis of findings was undertaken based on all included studies. Results were presented overall and based on the following subgroups: (1) type of intervention; (2) intervention duration; (3) evaluation sample size; (4) country’s income classification by the World Bank; and (5) country’s region based on the WHO classification [14]. Pooling of estimates was deemed inappropriate due to the heterogenous nature of the included studies.
Results
Search Results
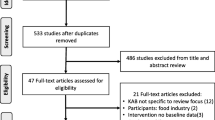
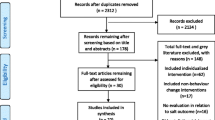
Between June 2013 and February 2020, the Science of Salt Weekly database contained 395 articles related to the implementation of salt reduction interventions. After title and abstract screening, 72 articles were deemed potentially relevant, and screened further for eligibility. Of these, 40 full texts were excluded for the following reasons: the effects of salt reduction interventions were not described (n = 12); the evaluation was not salt-specific (n = 8); the study was from a high-income country (n = 5); the study was a review (n = 8); the study was a protocol, modelling study or process evaluation (n = 4); and the study was a taste-test intervention (n = 3). Ultimately, 32 studies met our criteria, representing 13 upper middle-income and four lower middle-income countries (Fig. 1). None was conducted in low-income countries.
Study Characteristics
The studies varied by design, sample size, implementation scale, and intervention duration (Table 1). There were 14 randomised controlled trials (RCT) [15,16,17,18,19,20,21,22,23,24,25,26,27,28], seven repeated cross-sectional studies [29,30,31,32,33,34,35], five controlled or uncontrolled pre-post intervention [36,37,38,39,40], two quasi-experimental trials [41, 42], and four cross-sectional studies [43,44,45,46]. Three of the four cross-sectional studies assessed compliance with targets for salt/sodium levels in foods [44,45,46], while the other study evaluated the “China Healthy Lifestyles for All” initiative by comparing counties that implemented the initiative against non-participating counties [43]. Two studies were implemented in multiple countries [25, 37], while the rest involved a single country. Eleven studies were evaluations of government interventions, including the salt/sodium targets for processed foods in Brazil [29], South Africa [44], Argentina [45, 46], and Costa Rica [33]; the salt-restriction spoon in China [23]; the China Healthy Lifestyles for All [43]; the Healthy Bread Initiative in Iran [38]; the population salt reduction interventions in Fiji [31] and Samoa [32]; and the Integrating Nutrition Promotion and Rural Development (INPARD) study in Sri Lanka [41]. The other studies were research-driven.
Five studies used food products as the unit of analysis, and sample sizes ranged from 1320 to 11,065 food products [29, 33, 44,45,46]. In the other studies, sample sizes ranged from 18 to 351,319 individuals. The intervention duration ranged from 1 month to 6 years (median 1 year). Ten studies were implemented at a national scale [29,30,31,32,33, 41, 43,44,45,46], while nine studies were at community level [19, 23, 27, 34,35,36,37,38, 40]. The remaining 13 studies were small-scale or pilot studies, or were aimed at specific groups (e.g. households with a hypertensive member [24], persons at risk of developing hypertension [26], school children and their families [20], and workers at a private company [42]).
Type of Interventions Implemented and Target Population
Education interventions were the most commonly evaluated salt reduction interventions, and these were carried out through group discussions [15, 20, 21, 26, 28], individual sessions (such as dietary counselling) [17, 18, 25, 39], or community-based implementation [36, 40, 41, 43] (Table 1). Voluntary or mandatory targets for sodium levels in foods were evaluated in four countries (Argentina [45, 46], Brazil [29], Costa Rica [33], and South Africa [44]), while the use of salt substitutes was tested in two (Brazil [16] and China [22, 24]). Nine studies carried out multi-faceted interventions (defined here as the combination of two or more approaches), all of which involved some form of education [19, 23, 27, 31, 32, 34, 35, 37, 38]. Some interventions covered institutional settings, including schools, hospitals, workplaces, and government offices [20, 31, 32, 34, 35, 37, 39, 40]. Other types of interventions implemented were reducing salt in meals [42] and discounts on healthy food purchases [30].
Consumer education studies targeted pre-hypertensive and hypertensive adults or at-risk population groups [15, 17, 18, 21, 25, 26, 28, 39], or were conducted in the general population [36, 40, 41, 43] or amongst school children [20]. The salt substitution studies targeted pre-hypertensive and hypertensive adults of different age groups [16, 22, 24]. Food reformulation studies targeted the general population through the changes made by the food industry to food composition (bread for example), although the range of processed foods targeted varied across the studies [29, 33, 44,45,46]. Multi-faceted interventions targeted either the general population directly or as a result of the food industry making changes to food composition [19, 23, 27, 31, 32, 34, 35, 37, 38].
Outcome Measures Reported
Changes in KAB and salt intake were the most commonly reported outcome measures (n = 19 and 17, respectively), followed by changes in blood pressure (n = 14). Six studies looked at salt/sodium levels in foods, one of which reported changes over time [34], three assessed the compliance of salt/sodium contents of foods with targets [44,45,46], while two assessed both [29, 33]. Of the 32 studies, 19 (59%) reported more than one outcome measure. The method of assessment varied across the studies, but the most common approach used was 24-h urine collection for salt intake (n = 12) and food label survey for sodium levels in foods (n = 5). Consumer KAB was measured using self-reported tools, while blood pressure was assessed using standard procedures (i.e. average of two or three blood pressure readings).
Effects of the Interventions
Overall, more studies reported a positive effect (i.e. decreased salt intake, lower sodium levels in foods, reduced blood pressure, and improved KAB) than a null effect (i.e. no change), and no study reported a negative effect (e.g. increase in salt intake) of the interventions on any of the outcome measures (Fig. 2). Twelve studies (of 17; 71%) reported a reduction in salt intake, 17/19 (89%) reported improvements in KAB, 6/6 (100%) reported lower sodium levels in foods or showed compliance of sodium levels with agreed targets, and 10/14 (71%) reported a decrease in blood pressure. In the majority of subgroups (by intervention type, intervention duration, sample size, country’s income class, and country’s region), there were more studies that demonstrated a positive effect of the intervention than a null effect (Supplementary File 1).
Magnitude of Effect on Salt Intake and Blood Pressure
For studies that measured salt intake using the gold standard 24-h urine collection (n = 12), the magnitude of effect of the interventions on salt intake ranged from −3.8 (95% CI −5.9 to −1.8) to −0.4 g/day (−1.6 to 0.9) for RCTs, and from −2.8 (−3.9 to −1.8) to 0.19 g/day (−0.50 to 0.88) for non-RCTs (Fig. 3). For systolic blood pressure (SBP), the magnitude of effect ranged from −10.1 (95% CI −22.4 to 2.3) to 1.8 mmHg (−1.4 to 5.0) for RCTs, and from −8.3 (−11.7 to −4.9) to −3.1 mmHg (−4.3 to −2.0) for non-RCTs (Fig. 4). Furthermore, the magnitude of effect on diastolic blood pressure (DBP) ranged from −6.8 (95% CI −14.2 to 0.6) to 1.9 mmHg (−1.1 to 5.0) for RCTs, and from −6.4 (−8.3 to −4.5) to −2.9 mmHg (−3.8 to −2.0) for non-RCTs (Fig. 5).
Discussion
This review identified 32 studies related to the implementation and evaluation of salt reduction interventions in LMICs from June 2013 to February 2020. Overall, more studies demonstrated that the interventions led to positive effects (i.e. decreased salt intake, lower salt/sodium levels in foods, decreased blood pressure, and improved KAB) compared to no effect, and there was no study that presented an adverse effect of the interventions. However, there were considerable differences in study characteristics, and the studies adopted a variety of implementation strategies to reduce salt and different measures of impact. We conducted five subgroup analyses (by intervention type, intervention duration, sample size, income class, and region) to take into account these differences, and observed a similar finding in most. However, we speculate that these sub-analyses were not able to fully explain the differences between the studies; hence, the results should be interpreted with caution.
Most of the studies were from upper middle-income countries (n = 28), four from lower middle-income countries, and none from low-income countries—a distribution that reflects the order of these income groups in terms of CVD burden related to a diet high in salt [1•, 2]. While most of the studies were from upper middle-income countries, it is notable that more than 50% of the studies were from four countries (nine studies from China, five from Brazil, and three studies each from Argentina and Iran). However, the studies included covered five of the six WHO regions, and the only region for which data were not available was Europe. The regions with the highest number of studies were Western Pacific (n = 13) and the Americas (n = 10), while the regions of Africa, Eastern Mediterranean, and South East Asia had at most 4 studies each. This means that the applicability of findings may be limited in other contexts and suggests the need for further salt reduction intervention and evaluation studies in other settings.
Consumer Education Interventions
Our review found that education interventions resulted in improvements in salt-related KAB. However, most of these studies were individual or group interventions, which may not be suitable for large-scale implementation due to the interventions being resource-intensive. Nevertheless, all multi-faceted interventions that had an education component, and were of larger scale, also showed positive changes in KAB. This suggests that education interventions, either alone or in combination with other interventions, could potentially produce favourable KAB outcomes. This finding is in line with previous reviews [47, 48]. However, it is important to note that the tools or questionnaires used to measure changes in KAB differed across the studies, and were based on self-report; thus, they were subjective and might not have precisely reflected the participant’s actual behaviour and what they actually consumed. For instance, three studies [15, 28, 32] that measured both changes in KAB and salt intake showed contrasting results, presenting positive changes in KAB but not in salt intake. Previous studies have shown that self-reported KABs are not always related to salt intakes [49, 50]; therefore, it is important to consider the subjective nature of KABs when evaluating salt reduction intervention effectiveness, and where possible, use more objective outcome assessment methods [47].
We found some evidence that the use of theoretical frameworks (such as the self-care deficit theory, salt-efficacy theory, the Theory of Planned Behaviour, or the Communication for Behavioural Impact) was helpful for successful behaviour change interventions [15, 17, 26, 28, 35, 40]. This is in line with a previous systematic review that reported that theory-based behaviour change interventions lead to improvements in either salt intake or salt-related behaviours [47]. Some theoretical frameworks support identification of specific behaviours to target, so the activities or interventions can be designed specifically to change those behaviours. For example, the study in Vietnam, which utilised the Communication for Behavioural Impact (COMBI) framework, set three behaviour change targets: to reduce salt use in cooking, to reduce salt use at the table, and to improve selection of foods low in salt [35]. The activities carried out mainly focused on addressing these behaviours, and the study was successful in meeting the targets following the intervention. Furthermore, many studies considered the importance of cultural eating habits when designing behaviour change interventions. One study reported the ingrained habit of salt use as the strongest factor preventing behaviour change [15], and another showed that counselling calls and text messages were not effective in promoting good habits [25]. In contrast, a school-based education program amongst school children and their families in China was successful in reducing salt intake, and the authors suggested that this strategy has the potential to set good habits that will likely continue throughout adulthood [20].
Food Reformulation Interventions
The food reformulation interventions included in this review were of national scale, and were implemented in the real world, led by government institutions. All five studies were from upper middle-income countries (i.e. Argentina, Brazil, Costa Rica, and South Africa) [29, 33, 44,45,46], and showed successful reductions in salt/sodium levels in foods over time or compliance with meeting the sodium targets. However, the degree of reduction in sodium varied across the food categories, and some categories had little to no change over time. This echoes the findings of a recent global review of changes in sodium levels in foods [51], which showed a modest overall reduction in mean sodium content of foods by 36 mg/100 g, and significant reductions in only five out of 10 categories examined. Thus, it is important to establish a robust monitoring scheme, to assess compliance with agreed targets across food categories, and to ensure that targets cover a large enough proportion of foods that impact population salt intake [52].
There were insufficient studies to show whether voluntary or mandatory targets were more effective for reducing salt/sodium levels in foods. Previous work has demonstrated that mandatory approaches may be more effective for producing changes [53, 54]; yet, voluntary initiatives found in this review appear to be working. For instance, Argentina started with voluntary agreements with the food industry before legislating the targets, which resulted in more than 80% of the food categories already meeting the targets set by the national law prior to its introduction [45]. Pooled analysis of change in sodium levels in foods showed that voluntary schemes lead to about 40 mg/100 g sodium reduction in packaged food products over time [51]. Regardless of the approach, the success of food reformulation interventions relies on the commitment of the food industry, so it is essential to create partnerships with the food industry, negotiate agreements, and hold them to account, continuously engage, and monitor progress, and provide adequate technical support (for small manufacturers) where needed [52]
Salt Substitution Interventions
The studies that used salt substitutes demonstrated that the intervention was effective in reducing both salt intake and blood pressure [16, 22, 24]. It is important to note, however, that these studies targeted pre-hypertensives and hypertensives, and seemingly, it is easier to reduce blood pressure when the baseline level is high [55]. There was one study that measured the effects of salt substitutes combined with consumer education in the general population [19], which showed a reduction in salt intake but not blood pressure. This suggests the potential for scale-up of using salt substitutes, but more research is needed to understand how salt substitutes could complement other salt reduction interventions to further reduce population salt intake (and at the same time increase potassium intake). The China Salt Substitute and Stroke Study (SSASS), a large-scale cluster RCT in China, has been investigating the effects of salt substitutes on cardiovascular outcomes and total mortality [56]. Interim results showed that there have been reductions in SBP in the intervention group [57]. Further findings from this study will be important in identifying the long-term benefits of using salt substitutes, and in encouraging governments to use a salt substitute-based salt reduction strategy (if the intervention is effective).
An important consideration relating to the use of salt substitutes is cost. One study showed that the higher cost of salt substitute compared to regular salt influenced its uptake, such that when authors subsidised its price, its uptake almost doubled [19]. This suggests that the full potential of this intervention could be realised if the difference in price is removed. Another consideration is consumer taste acceptability. One study reported a low acceptance rate of a salt substitute due to its peculiar taste [16]. This is in contrast to previous studies, which demonstrated that they are generally accepted, and that most consumers were unable to taste the difference between foods containing salt substitutes and regular salt [58,59,60,61]. These considerations will be beneficial in informing future salt reduction interventions that involve salt substitution.
Multi-faceted Interventions
The most common theme found in the studies was that a combination of salt reduction interventions is needed to achieve the largest health benefits. This is in line with past reviews which show that multi-faceted interventions are likely to be more effective in reducing population salt intake [53, 62]. The many multi-faceted interventions we identified in this review is itself a positive finding, as it suggests these approaches are being considered and/or are feasible, even in resource-limited settings. Although the mix of interventions used in the studies was diverse, the studies consistently showed that the interventions lead to positive outcomes. Of the five studies that assessed both change in KAB and salt intake [19, 23, 32, 34, 35], all showed improvements in KAB while four also showed reductions in salt intake. The study that showed a null effect on salt intake was carried out in Samoa [32], and the authors suggested that this was due to a number of factors, such as the differences in the characteristics of recruited samples and methodologies between the baseline and follow-up surveys, limited duration, and dose of intervention [63], and the already increasing trend in salt intake in Samoa that negated the effect of the interventions. This example demonstrates that implementing and evaluating salt reduction interventions come with challenges for different settings. Interim evaluations of the interventions might be helpful to identify issues and areas that require variation, and ensure that the interventions are being delivered as planned [64•].
Effect on Salt Intake and Blood Pressure
In terms of magnitude of effect of the interventions on salt intake and blood pressure, the study design, method of assessment, target population, and measures of change varied across the included studies, so the results should be interpreted in light of such differences. Controlled studies reported either the net difference between the control group and intervention group or the difference between groups at follow-up, while uncontrolled studies reported the change pre- and post-intervention. For both salt intake and blood pressure, the majority of studies were RCTs and were targeted at pre-hypertensive and hypertensive adults; thus, there is a need for more studies on the effects of carrying out the interventions in the general population. It is also worth noting that of the studies that showed decreases in salt intake over time, all salt intake estimates at follow-up were still higher than the recommended intake of 5 g/day, which clearly supports the need for continued efforts to reduce salt intake.
Strengths and Limitations
Strengths of this review include the systematic approach through the Science of Salt Weekly, and the inclusion of all articles during the lifetime of the initiative. All LMICs were considered based on the current World Bank income classification. A limitation of this review is the restriction by language (the Science of Salt Weekly search only includes articles in English), so it is possible that we have missed salt reduction interventions published in other languages. It is also possible that implementation and evaluation data are available from other LMICs but unpublished or not available through Medline, hence beyond the scope of the Science of Salt Weekly search. It was deemed inappropriate to pool the measure of effect reported in the studies due to the heterogeneity of the included studies. Lastly, we cannot preclude the possibility of publication bias. It is likely that studies with positive findings are published more than negative or null results, amplifying the effects of the interventions on the outcome measures.
Conclusion
In conclusion, this study found that salt reduction interventions have the potential to be successful in LMICs. The majority of studies demonstrated that the interventions were effective in their target populations, based on a range of outcome measures. Interventions implemented alone, or combined with other approaches, were successful in producing positive outcomes (decreased salt intake, lower sodium levels in foods, improved KAB towards salt, and decreased blood pressure). However, many studies were of small scale, targeted specific groups, and were concentrated in a few upper middle-income countries. Supporting scale-up of salt reduction interventions is essential to cover broader populations and to increase their public health impact.
Data Availability
The data used for this study are available from the authors upon reasonable request.
Code Availability
Not applicable
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease study 2019. Lancet (London, England). 2020;396(10258):1204–22. https://doi.org/10.1016/s0140-6736(20)30925-9This most recent study from the Global Burden of Disease Collaborative Network presented the disproportionately large burden of noncommunicable diseases, including cardiovascular disease, in low- and middle-income countries. The study showed that of all dietary risk factors, a diet high in salt was the largest contributor to disease burden.
Global Burden of Disease Collaborative Network. Global Burden of Disease study 2019 (GBD 2019) results. Seattle: Institute for Health Metrics and Evaluation (IHME); 2020.
The World Bank. World Bank country and lending groups: country classification 2019 [Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
World Health Organization. Global action plan for the prevention and control of NCDS 2013-2020. Geneva: World Health Organization; 2013.
Trieu K, Neal B, Hawkes C, et al. Salt reduction initiatives around the world - a systematic review of progress towards the global target. PLoS One. 2015;10(7):e0130247. https://doi.org/10.1371/journal.pone.0130247.
Webster JL, Dunford EK, Hawkes C, Neal BC. Salt reduction initiatives around the world. 2011;29(6):1043–50. https://doi.org/10.1097/HJH.0b013e328345ed83.
Santos JA, Tekle D, Rosewarne E, et al. A systematic review of salt reduction initiatives around the world: a midterm evaluation of progress towards the 2025 global non-communicable diseases salt reduction target. Adv Nutri (Bethesda, Md). 2021. https://doi.org/10.1093/advances/nmab008This systematic review examined countries’ progress towards achieving the global target of a 30% reduction in salt intake from baseline. The review found a further increase in the number of national salt reduction initiatives around the world since 2014, but no country has yet met the salt reduction target to be achieved by 2025.
McLaren L, Sumar N, Barberio AM, et al. Population-level interventions in government jurisdictions for dietary sodium reduction. Cochrane Database Syst Rev. 2016;(9). https://doi.org/10.1002/14651858.CD010166.pub2.
Christoforou A, Trieu K, Land MA, Bolam B, Webster J. State-level and community-level salt reduction initiatives: a systematic review of global programmes and their impact. J Epidemiol Community Health. 2016;70(11):1140–50. https://doi.org/10.1136/jech-2015-206997\.
Santos JA, Trieu K, Raj TS, et al. The Science of Salt: a regularly updated systematic review of the implementation of salt reduction interventions (March-August 2016). J Clin Hypertens (Greenwich, Conn). 2017;19(4):439–51. https://doi.org/10.1111/jch.12971.
Johnson C, Santos JA, McKenzie B, et al. The Science of Salt: a regularly updated systematic review of the implementation of salt reduction interventions (September 2016-February 2017). J Clin Hypertens (Greenwich, Conn). 2017;19(10):928–38. https://doi.org/10.1111/jch.13099.
World Health Organization. Shake the salt habit: the shake technical package for salt reduction. Geneva: World Health Organization; 2016.
Arcand J, Webster J, Johnson C, et al. Announcing “up to date in the science of sodium”. 2016;18(2):85–8. https://doi.org/10.1111/jch.12732.
World Health Organization. Who regional offices 2020 [Available from: https://www.who.int/about/who-we-are/regional-offices.
Cornelio ME, Godin G, Rodrigues RC, de Freitas AR, Alexandre NM, Gallani MC. Effect of a behavioral intervention of the SALdavel program to reduce salt intake among hypertensive women: a randomized controlled pilot study. Eur J Cardiovasc Nurs. 2016;15(3):e85–94. https://doi.org/10.1177/1474515115589275.
Barros CL, Sousa AL, Chinem BM, et al. Impact of light salt substitution for regular salt on blood pressure of hypertensive patients. Arq Bras Cardiol. 2015;104(2):128–35. https://doi.org/10.5935/abc.20140174.
de Freitas AR, Cornelio ME, Rodrigues RC, Gallani MC. Implementation intentions on the effect of salt intake among hypertensive women: a pilot study. Nurs Res Pract. 2014;2014:1964. https://doi.org/10.1155/2014/196410.
Lima ST, da Silva Nalin de Souza B, Franca AK, Salgado Filho N, Sichieri R. Dietary approach to hypertension based on low glycaemic index and principles of dash (dietary approaches to stop hypertension): a randomised trial in a primary care service. Br J Nutr. 2013;110(8):1472–9. https://doi.org/10.1017/s0007114513000718.
Li N, Yan LL, Niu W, et al. The effects of a community-based sodium reduction program in rural china – a cluster-randomized trial. PLoS One. 2016;11(12):e0166620. https://doi.org/10.1371/journal.pone.0166620.
He FJ, Wu Y, Feng XX, et al. School based education programme to reduce salt intake in children and their families (School-EduSalt): cluster randomised controlled trial. BMJ (Clinical research ed). 2015;350:h770. https://doi.org/10.1136/bmj.h770.
Lu CH, Tang ST, Lei YX, et al. Community-based interventions in hypertensive patients: a comparison of three health education strategies. BMC Public Health. 2015;15:33. https://doi.org/10.1186/s12889-015-1401-6.
Zhao X, Yin X, Li X, et al. Using a low-sodium, high-potassium salt substitute to reduce blood pressure among Tibetans with high blood pressure: a patient-blinded randomized controlled trial. PLoS One. 2014;9(10):e110131. https://doi.org/10.1371/journal.pone.0110131.
Chen J, Tian Y, Liao Y, et al. Salt-restriction-spoon improved the salt intake among residents in china. PLoS One. 2013;8(11):e78963. https://doi.org/10.1371/journal.pone.0078963.
Zhou B, Wang HL, Wang WL, Wu XM, Fu LY, Shi JP. Long-term effects of salt substitution on blood pressure in a rural north Chinese population. J Hum Hypertens. 2013;27(7):427–33. https://doi.org/10.1038/jhh.2012.63.
Rubinstein A, Miranda JJ, Beratarrechea A, et al. Effectiveness of an mHealth intervention to improve the cardiometabolic profile of people with prehypertension in low-resource urban settings in Latin America: a randomised controlled trial. Lancet Diabetes Endocrinol. 2016;4(1):52–63. https://doi.org/10.1016/s2213-8587(15)00381-2.
Rahimdel T, Morowatisharifabad MA, Salehi-Abargouei A, Mirzaei M, Fallahzadeh H. Evaluation of an education program based on the Theory of Planned Behavior for salt intake in individuals at risk of hypertension. Health Educ Res. 2019;34(3):268–78. https://doi.org/10.1093/her/cyz007.
Jafari M, Mohammadi M, Ghazizadeh H, Nakhaee N. Feasibility and outcome of reducing salt in bread: a community trial in Southern Iran. Glob J Health Sci. 2016;8(12):163. https://doi.org/10.5539/gjhs.v8n12p163.
Irwan AM, Kato M, Kitaoka K, Ueno E, Tsujiguchi H, Shogenji M. Development of the salt-reduction and efficacy-maintenance program in Indonesia. Nurs Health Sci. 2016;18(4):519–32. https://doi.org/10.1111/nhs.12305.
Nilson EAF, Spaniol AM, Goncalves VSS, et al. Sodium reduction in processed foods in Brazil: analysis of food categories and voluntary targets from 2011 to 2017. Nutrients. 2017;9(7). https://doi.org/10.3390/nu9070742.
An R, Patel D, Segal D, Sturm R. Eating better for less: a national discount program for healthy food purchases in South Africa. Am J Health Behav. 2013;37(1):56–61. https://doi.org/10.5993/ajhb.37.1.6.
Pillay A, Trieu K, Santos JA, et al. Assessment of a salt reduction intervention on adult population salt intake in Fiji. Nutrients. 2017;9(12). https://doi.org/10.3390/nu9121350.
Trieu K, Ieremia M, Santos J, et al. Effects of a nationwide strategy to reduce salt intake in Samoa. J Hypertens. 2018;36(1):188–98. https://doi.org/10.1097/hjh.0000000000001505.
Vega-Solano J, Blanco-Metzler A, Benavides-Aguilar KF, Arcand J. An evaluation of the sodium content and compliance with the national sodium reduction targets among packaged foods sold in Costa Rica in 2015 and 2018. Nutrients. 2019;11(9). https://doi.org/10.3390/nu11092226.
Enkhtungalag B, Batjargal J, Chimedsuren O, Tsogzolmaa B, Anderson CS, Webster J. Developing a national salt reduction strategy for Mongolia. Cardiovasc Diagn Ther. 2015;5(3):229–37. https://doi.org/10.3978/j.issn.2223-3652.2015.04.11.
Do HT, Santos JA, Trieu K, et al. Effectiveness of a Communication for Behavioral Impact (COMBI) intervention to reduce salt intake in a Vietnamese province based on estimations from spot urine samples. J Clin Hypertens (Greenwich, Conn). 2016;18(11):1135–42. https://doi.org/10.1111/jch.12884.
Chan EYY, Lam HCY, Lo ESK, Tsang SNS, Yung TKC, Wong CKP. Food-related health emergency-disaster risk reduction in rural ethnic minority communities: a pilot study of knowledge, awareness and practice of food labelling and salt-intake reduction in a Kunge community in China. Int J Environ Res Public Health. 2019;16(9). https://doi.org/10.3390/ijerph16091478.
Dyson PA, Anthony D, Fenton B, et al. Successful up-scaled population interventions to reduce risk factors for non-communicable disease in adults: results from the international community interventions for health (CIH) project in China, India and Mexico. PLoS One. 2015;10(4):e0120941. https://doi.org/10.1371/journal.pone.0120941.
Talaei M, Mohammadifard N, Khaje MR, Sarrafzadegan N, Sajjadi F, Alikhasi H, et al. Healthy bread initiative: methods, findings, and theories--Isfahan healthy heart program. J Health Popul Nutr. 2013;31(1):49–57.
Walsh JL, Aridi H, Fathallah J, et al. Impact of a hospital-based educational intervention on dietary salt-related knowledge and behaviour in a cardiac care unit population in Lebanon. Cardiovasc Diagn Ther. 2018;8(2):146–55. https://doi.org/10.21037/cdt.2017.12.02.
Borah PK, Kalita HC, Paine SK, et al. An information, education and communication module to reduce dietary salt intake and blood pressure among tea garden workers of Assam. Indian Heart J. 2018;70(2):252–8. https://doi.org/10.1016/j.ihj.2017.08.008.
Liyanage IK, Wickramasinghe K, Katulanda P, et al. Integrating the development agenda with noncommunicable disease prevention in developing countries: a quasi-experimental study on inter-sectoral action and its impact on self-reported salt consumption-the INPARD study. Cardiovasc Diagn Ther. 2019;9(2):120–8. https://doi.org/10.21037/cdt.2018.10.19.
Reynoso-Marreros IA, Piñarreta-Cornejo PK, Mayta-Tristán P, Bernabé-Ortiz A. Effect of a salt-reduction strategy on blood pressure and acceptability among customers of a food concessionaire in Lima. Peru. 2019;76(3):250–6. https://doi.org/10.1111/1747-0080.12449.
Zhang J, Astell-Burt T, Seo DC, et al. Multilevel evaluation of ‘China Healthy Lifestyles for All’, a nationwide initiative to promote lower intakes of salt and edible oil. Prev Med. 2014;67:210–5. https://doi.org/10.1016/j.ypmed.2014.07.019.
Peters SAE, Dunford E, Ware LJ, et al. The sodium content of processed foods in South Africa during the introduction of mandatory sodium limits. Nutrients. 2017;9(4):404. https://doi.org/10.3390/nu9040404.
Allemandi L, Tiscornia MV, Ponce M, Castronuovo L, Dunford E, Schoj V. Sodium content in processed foods in Argentina: compliance with the national law. Cardiovasc Diagn Ther. 2015;5(3):197–206. https://doi.org/10.3978/j.issn.2223-3652.2015.04.01.
Allemandi L, Tiscornia MV, Guarnieri L, Castronuovo L, Martins E. Monitoring sodium content in processed foods in Argentina 2017-2018: compliance with national legislation and regional targets. Nutrients. 2019;11(7):1474. https://doi.org/10.3390/nu11071474.
Trieu K, McMahon E, Santos JA, et al. Review of behaviour change interventions to reduce population salt intake. Int J Behav Nutr Phys Act. 2017;14(1):17. https://doi.org/10.1186/s12966-017-0467-1.
McKenzie B, Santos JA, Trieu K, et al. The Science of Salt: a focused review on salt-related knowledge, attitudes and behaviors, and gender differences. J Clin Hypertens (Greenwich, Conn). 2018;20(5):850–66. https://doi.org/10.1111/jch.13289.
Land MA, Webster J, Christoforou A, et al. The association of knowledge, attitudes and behaviours related to salt with 24-hour urinary sodium excretion. Int J Behav Nutr Phys Act. 2014;11(1):47. https://doi.org/10.1186/1479-5868-11-47.
Johnson C, Mohan S, Rogers K, et al. The association of knowledge and behaviours related to salt with 24-h urinary salt excretion in a population from north and south India. Nutrients. 2017;9(2). https://doi.org/10.3390/nu9020144.
Santos JA, Sparks E, Thout SR, et al. The Science of Salt: a global review on changes in sodium levels in foods. J Clin Hypertens (Greenwich, Conn). 2019;21(8):1043–56. https://doi.org/10.1111/jch.13628.
Webster J, Trieu K, Dunford E, Hawkes C. Target salt 2025: a global overview of national programs to encourage the food industry to reduce salt in foods. Nutrients. 2014;6(8):3274–87. https://doi.org/10.3390/nu6083274.
Hyseni L, Elliot-Green A, Lloyd-Williams F, et al. Systematic review of dietary salt reduction policies: evidence for an effectiveness hierarchy? PLoS One. 2017;12(5):e0177535. https://doi.org/10.1371/journal.pone.0177535.
Nghiem N, Blakely T, Cobiac LJ, Pearson AL, Wilson N. Health and economic impacts of eight different dietary salt reduction interventions. PLoS One. 2015;10(4):e0123915. https://doi.org/10.1371/journal.pone.0123915.
Hu H, Zhang J, Wang Y, et al. Impact of baseline blood pressure on the magnitude of blood pressure lowering by nifedipine gastrointestinal therapeutic system: refreshing the wilder’s principle. Drug Des Dev Ther. 2017;11:3179–86. https://doi.org/10.2147/DDDT.S143551.
Neal B, Tian M, Li N, et al. Rationale, design, and baseline characteristics of the Salt Substitute and Stroke Study (SSASS)-a large-scale cluster randomized controlled trial. Am Heart J. 2017;188:109–17. https://doi.org/10.1016/j.ahj.2017.02.033.
Huang L, Tian M, Yu J, Li Q, Liu Y, Yin X, et al. Interim effects of salt substitution on urinary electrolytes and blood pressure in the China Salt Substitute and Stroke Study (SSASS). Am Heart J. 2020;221:136–45. https://doi.org/10.1016/j.ahj.2019.12.020.
Saavedra-Garcia L, Bernabe-Ortiz A, Gilman RH, et al. Applying the triangle taste test to assess differences between low sodium salts and common salt: evidence from Peru. PLoS One. 2015;10(7):e0134700. https://doi.org/10.1371/journal.pone.0134700.
Li N, Prescott J, Wu Y, et al. The effects of a reduced-sodium, high-potassium salt substitute on food taste and acceptability in rural northern China. Br J Nutr. 2009;101(7):1088–93. https://doi.org/10.1017/s0007114508042360.
Maleki A, Soltanian AR, Zeraati F, Sheikh V, Poorolajal J. The flavor and acceptability of six different potassium-enriched (sodium reduced) iodized salts: a single-blind, randomized, crossover design. Clin Hypertens. 2016;22(1):18. https://doi.org/10.1186/s40885-016-0054-9.
Girgis S, Neal B, Prescott J, et al. A one-quarter reduction in the salt content of bread can be made without detection. Eur J Clin Nutr. 2003;57(4):616–20. https://doi.org/10.1038/sj.ejcn.1601583.
Regan Á, Kent MP, Raats MM, McConnon Á, Wall P, Dubois L. Applying a consumer behavior lens to salt reduction initiatives. Nutrients. 2017;9(8):901. https://doi.org/10.3390/nu9080901.
Trieu K, Webster J, Jan S, et al. Process evaluation of Samoa’s national salt reduction strategy (Masima): what interventions can be successfully replicated in lower-income countries? Implement Sci. 2018;13(1):107. https://doi.org/10.1186/s13012-018-0802-1.
Trieu K, Michael V, Mustapha F, Lo Y-R, Webster J. Midterm evaluation of Malaysia’s national salt reduction strategy – lessons learned on adapting salt reduction ‘best buys’ to the local context. Curr Dev Nutri. 2020;4(Supplement_2):288. https://doi.org/10.1093/cdn/nzaa043_139This report highlighted the importance of interim evaluations of salt reduction interventions to make sure that they are being delivered as intended. The report presented lessons learned and recommendations that can be adopted to strengthen implementation of salt reduction interventions.
Funding
This manuscript is based on a previous work funded through a partnership between the World Health Organization and Vital Strategies (Resolve to Save Lives). J Santos is supported by a National Health and Medical Research Council (NHMRC) Postgraduate scholarship (1168948). B McKenzie is supported by a University of New South Wales (UNSW) Scientia Postgraduate Scholarship. E Rosewarne is supported by UNSW Postgraduate Award (00889665) and George Institute Top-Up Scholarship. K Trieu is supported by an NHMRC Early Career Fellowship (1161597) and a Postdoctoral Fellowship (102140) from the National Heart Foundation of Australia. JW is supported by a National Heart Foundation Future Leaders Fellowship II on strengthening and monitoring food policy interventions (1082924). She receives additional funding for work on salt reduction from NHMRC, the Victorian Health Promotion Foundation, Vital Strategies, and the World Health Organization. K Trieu and J Webster are supported by an NHMRC Centre of Research Excellence on food policy interventions to reduce salt (1117300).
Author information
Authors and Affiliations
Contributions
J Webster and LK Cobb conceived the study. J Santos conducted the search and analysed the data. B McKenzie, E Rosewarne, M Hogendorf, K Trieu, M Woodward, and R Dodd provided input on the preliminary draft of the manuscript. All authors reviewed subsequent versions of the manuscript and approved the final paper.
Corresponding author
Ethics declarations
Ethics Approval
Not applicable
Consent to Participate
Not applicable
Consent for Publication
Not applicable
Conflict of Interest
Joseph Alvin Santos declares that he has no conflict of interest. Briar McKenzie declares that she has no conflict of interest. Emalie Rosewarne declares that she has no conflict of interest. Martyna Hogendorf declares that she has no conflict of interest. Kathy Trieu declares that she has no conflict of interest. Mark Woodward has received compensation from Amgen, Freeline, and Kyowa Kirin for service as a consultant. Laura K. Cobb declares that she has no conflict of interest. Rebecca Dodd declares that she has no conflict of interest. Jacqui Webster is the Director of the World Health Organization Collaborating Centre on Population Salt Reduction with a remit to support countries to implement and evaluate salt reduction programs in line with the WHO target for all countries to reduce population salt intake by 30% by 2025.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Public Health Nutrition
Supplementary Information
ESM 1
(DOCX 6918 kb)
Rights and permissions
About this article
Cite this article
Santos, J.A., McKenzie, B., Rosewarne, E. et al. Strengthening Knowledge to Practice on Effective Salt Reduction Interventions in Low- and Middle-Income Countries. Curr Nutr Rep 10, 211–225 (2021). https://doi.org/10.1007/s13668-021-00365-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13668-021-00365-1