Abstract
Malignant pleural effusion remains a distressing and unfortunately common occurrence. Pleural palliation should be focused on relieving dyspnea with as few procedures as possible. The introduction of the indwelling tunneled pleural catheter has been shown to fulfill these goals; however, it is not without limitations. The ability to potentially combine the results of a long-term pleurodesis procedure without the need for a prolonged hospitalization remains an attractive option. While no large-scale trials have been completed nor is there widespread acceptance, the introduction of “rapid” or “accelerated” pleurodesis procedures, often using tunneled indwelling pleural catheters, have the potential to significantly change the current paradigm of malignant pleural effusion management. This article reviews the current data available for “rapid” and “accelerated” pleurodesis protocols and their outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malignant pleural effusion (MPE) affects more than 150,000 patients each year within the USA [1] with lung and breast carcinomas being the most common cancers complicated by MPE [2, 3]. The development of MPE can frequently lead to debilitating dyspnea, which may significantly impact upon a patients’ functional status and quality of life [1, 2, 4, 5].
Current options for MPE management are targeted toward palliation as the development of a MPE usually represents incurable, metastatic disease. The more commonly utilized available therapeutic options include the following:
-
Pharmacologic agents to palliate the sensation of dyspnea (i.e., oxygen and morphine)
-
Repeated pleural drainage via thoracentesis
-
Tube thoracostomy drainage with instillation of a sclerosant to induce pleurodesis
-
Indwelling tunneled pleural catheter (IPC) placement
-
Thoracoscopy with sclerosant instillation to induce pleurodesis
Pleural palliation should be offered to all patients presenting with MPE who demonstrate symptomatic relief after pleural drainage. Current British Thoracic Society and American College of Chest Physicians guidelines promote definitive procedures to achieve this goal, namely a pleurodesis procedure or placement of an IPC due to the known high rate of recurrence in MPE with simple thoracentesis [2, 5]. Previous guidelines have often recommended sclerosant-induced pleurodesis as the procedure of choice for MPE management [1, 4], but data continue to accrue regarding the benefits of IPCs [6•, 7], and newer guidelines have recognized the importance and benefits of IPC placement [2, 5]. In patients with trapped lung physiology, the placement of IPC remains the treatment of choice [2, 5].
Current use of pleurodesis and IPC
While treatment options exist for MPE management, each clearly has its advantages and disadvantages that must be considered. The placement of an IPC commits patients to the long-term management of an indwelling catheter and potential complications such as infection [6•, 8••, 9, 10], catheter blockage [6•, 10], and metastatic disease at the catheter site [11]. Although many of these complications are not life-threatening and may not require hospitalization, they often represent a need for repeated healthcare interactions with associated cost escalation, potentially undermining the purpose of an ambulatory drainage system. While pleurodesis procedures (either via poudrage or slurry) may represent a definitive procedure, they are unfortunately not always successful or free from complications. A significant disadvantage to pleurodesis remains the requirement for hospitalization, operating room costs (if performed in association with thoracoscopy), as well as a 3–14 % risk of respiratory complications when using non-graded talc [12, 13]. In patients with a median survival of 3–6 months, the need for a week of hospitalization may represent almost 10 % of their remaining lifetime. This potential impact may again defeat a major goal of pleural palliation.
As a result of these issues, research into improving current MPE management persists. The ideal pleural palliative procedure would possess the following qualities:
-
Effective relief of dyspnea
-
Outpatient performance (or potentially very limited hospital stay (<24 h))
-
Minimal need for re-intervention/limitation of contact with the healthcare system
-
Minimal adverse effects
-
Cost-effective
Current research and potential advances in MPE management appear to involve attempts at hastening the pleurodesis process, allowing it to occur as an outpatient, or with minimal hospitalization times. The three most promising theories involve the use of more aggressive ambulatory pleural drainage, performance of “rapid pleurodesis” procedures, and the use of sclerosant-coated IPC’s to promote pleurodesis.
Aggressive pleural drainage
One of the disadvantages of IPCs for MPE management remains the requirement for ongoing care of an indwelling catheter as well as the costs associated with prolonged drainage. Promoting early spontaneous pleurodesis and therefore early removal of the IPC address both of these concerns.
Spontaneous pleurodesis is often identified by the presence of decreased IPC fluid output (<50–100 mL) on three consecutive drainages without radiographic or symptomatic recurrence of pleural effusion [14••, 15]. The occurrence of spontaneous pleurodesis has been reported in multiple studies after IPC placement, and rates of spontaneous pleurodesis appear to vary between studies. The largest systematic review to date examined 943 patients undergoing IPC placement with 45.6 % achieving spontaneous pleurodesis, on average, 52 days post insertion [10].
While the mechanism of spontaneous pleurodesis during IPC placement remains unclear, some believe that the presence of foreign material may promote inflammation and a subsequent pleural reaction when the pleural space is emptied on a frequent basis [2]. Others have theorized that the continued and aggressive drainage of the pleural space may lead to sustained inflammation during pleura-pleura apposition and increased spontaneous pleurodesis rates [16].
Current recommendations for pleural drainage after IPC placement are lacking, as evident by the reported drainage schedules in the literature. Drainage schedules may range from daily to only with the development of symptoms [14••, 15–18]. No drainage schedule patterns have been directly compared. Examples of initial drainage patterns include, “…three times weekly at home, allowing flexibility in the frequency and volume drained according to symptoms…” [14••].
Questions regarding particular drainage schedules and subsequent outcomes remain, which have promoted further research. Two current studies are registered on the ClinicalTrials.gov website [19, 20] that examine the role of different drainage schedules and the subsequent rates of pleurodesis. The first study [19] is a multicenter, randomized trial comparing the impact of aggressive (daily) versus standard (every other day) IPC drainage. The primary endpoint chosen was the rate of spontaneous pleurodesis at 2, 6, and 12 weeks, and approximately 150 patients were enrolled. At the time of writing, this trial has completed accrual and awaiting results of publication. The second study [20] is also a randomized, open-label trial comparing daily to thrice weekly IPC drainage. The primary endpoint chosen was the time to spontaneous pleurodesis with an estimated enrollment of 250 patients. Both studies have interestingly defined the use of once daily drainage as aggressive with slightly differently defined standard therapies and primary endpoints.
It remains unknown if more aggressive drainage will induce early spontaneous pleurodesis and retard pleural fluid reaccumulation; hopefully, these two trials will provide an answer. As the final data is not available, we must remain mindful of the economic impact that daily drainage may incur. As the use of drainage bottles appears to represent the larger, long-term drainage cost associated with IPC use [21–23], conversion to a daily drainage protocol may significantly increase the cost burden, depending on the total number of bottles used (i.e., more bottles over a shorter duration vs. fewer bottles over a longer duration).
Rapid pleurodesis
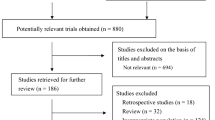
The true definition of “Rapid Pleurodesis” is not readily apparent within the literature; however, it appears to define a pleurodesis procedure that is not associated with the traditional 5–7 days of tube thoracostomy drainage and hospital stay. In some articles, it appears related to the in situ dwell time of the pleural drainage catheter [24–27], whereas in others, it appears related to the duration of tube thoracostomy drainage with inpatient hospitalization [28–30]. No large randomized trials have been performed utilizing a rapid pleurodesis protocol, nor is the literature specific about a particular protocol of rapid pleurodesis. Table 1 offers a review of the current literature of self-proclaimed “Rapid Pleurodesis” protocols.
As mentioned previously, the long-standing problem with pleurodesis remains the requirement for inpatient management of tube thoracostomy drainage. Subjecting end-stage cancer patients to hospital admission and all its subsequent complications remains undesirable. Attempts to reconcile this problem have been addressed in a number of ways.
Initial studies of rapid pleurodesis describe the use of small-bore catheters for pleural drainage, followed by early tube removal, usually within the first 24–48 h and frequently without regard for the current pleural fluid output. Very little data are available regarding the impact these procedures have on hospitalization; however, one would assume that patients admitted with dyspnea related to MPE, the early evacuation of effusion and sclerotherapy may permit for faster discharge than the traditional 5- to 7-day protocols. Pleurodesis success rates within these cohorts seem reasonable, with successful pleurodesis rates reported in the 80 % range or better in each study [24–27, 29].
Two more recent studies use a different description of rapid pleurodesis (Fig. 1, Video 1). They describe the use of medical thoracoscopy with IPC placement followed by talc poudrage [28, 30]. Both series recorded overall tube drainage (often only the IPC drainage on an ambulatory basis) and total hospital days. The median hospital stay ranged from 1 to 1.8 days with IPC removal occurring at 7.5–16 days. This significant reduction in hospital days required for pleurodesis as well as the duration with IPC in situ before onset of pleurodesis can potentially offer benefits in healthcare costs and quality of life.
These time and cost benefits remain theoretical at this point. No large prospective trials have been performed utilizing this approach; however, one is currently recruiting. Clinical trial NCT00758316 is attempting to randomize patients to talc poudrage versus talc poudrage and IPC placement, assessing pleurodesis rates, hospitalization times, complication rates, and quality of life scores [31].
Accelerodesis
The notion of “accelerodesis” has not been well accepted into the current management options for MPE, as evident by its lack of prominence within review articles on the subject. However, the hastening of pleurodesis during IPC usage appears to show promise. The term “accelerodesis” is currently under patent protection by Carefusion, Inc. [32]; therefore, its design and current iterations are somewhat limited.
The available data on “accelerodesis” are limited to animal models. Two animal studies by Trembley et al. have demonstrated the successful delivery of a low-dose sclerosant (silver nitrate) over a prolonged time course achieving subsequent pleurodesis [33, 34]. The initial study utilized a rabbit model during which silver nitrate was delivered over a 1, 5, and 14 day schedule in order to help determine the feasibility and effectiveness for intrapleural administration. A low dose of 0.05 % silver nitrate was able to achieve an effective pleurodesis score when examined histologically at autopsy [33]. A follow-up study by the same group utilized a rabbit and lamb model to help determine the effectiveness of a chitosan-silver nitrate-hyaluronic acid hydrogel-coated pleural catheter. In both animal types, the silver nitrate-coated catheters were placed for a total of 14 days and subsequently removed. Both studies demonstrated successful pleurodesis results from visual inspection and histologically. This low-dose, prolonged delivery system may help obviate the need for a large single-dose delivery of drug and the resultant associated adverse events.
Marchi et al. first identified that low-dose sequential dosing of sclerosants such as silver nitrate and talc caused effective pleurodesis; however, his initial outcomes were related to markers of systemic inflammation [35, 36]. Trembley et al. identified that the use of silver nitrate could be delivered over 1, 5, or 14 days and still achieve effective pleurodesis, despite the use of an overall lower daily dosage [33]. The use of lose-dose silver nitrate appears to result in a lower systemic response (white count elevation, neutrophila, vascular endothelial growth factor levels, etc.) compared to higher doses [35, 36], potentially allowing for a safer pleurodesis procedure. Trembley et al. have gone on to demonstrate the successful use of a silver nitrate-coated IPC within rabbit and sheep models. They concluded that the use of a coated IPC to promote “accelerodesis” may retain the advantages of IPC placement (minimally invasive, outpatient) while increasing earlier and successful pleurodesis rates [34].
As noted above, the concept of accelerodesis has only been tested in animals, and no human studies are currently available. A study involving the use of an IPC coated with silver nitrate (a known effective sclerosant agent) is currently in the early planning stages [personal communication]. While silver nitrate is being tested, the use of any sclerosant agent (talc, bleomycin, silver nitrate, etc.) could potentially be placed on the IPC and subsequently within the pleural space to help promote spontaneous pleurodesis.
Conclusion
The debate between IPC use and pleurodesis remains a common one, and rightfully so as both procedures have their own limitations. Current research attempting to combine the benefits of both procedures is exciting. The creation of a procedure that can improve outcomes by decreasing hospital stay, reducing costs, and increasing spontaneous pleurodesis rates is an active field of MPE research. The authors remain excited about the renewed research interest in MPE management and the future impact we may be able to offer for this oftentimes debilitating disease.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Antony VB, Loddenkemper R, Astoul P, et al. Management of malignant pleural effusions. Eur Respir J. 2001;18:402–19.
Roberts ME, Neville E, Berrisford RG, Antunes G, Ali NJ. Management of a malignant pleural effusion: British Thoracic Society pleural disease guideline 2010. Thorax. 2010;65:ii32–40.
Chernow B, Sahn S. Carcinomatous involvement of the pleura. Am J Med. 1977;63:695–702.
Antunes G, Neville E, Duffy J, Ali N. BTS guidelines for the management of malignant pleural effusions. Thorax. 2003;58 Suppl 2:ii29–38.
Simoff MJ, Lally B, Slade MG, et al. Symptom management in patients with lung cancer: diagnosis and management of lung cancer, 3rd ed: American college of chest physicians evidence-based clinical practice guidelines. CHEST J. 2013;143:e455S–97.
Davies HE, Mishra EK, Kahan BC, et al. Effect of an indwelling pleural catheter vs chest tube and talc pleurodesis for relieving dyspnea in patients with malignant pleural effusion: the TIME2 randomized controlled trial. JAMA. 2012;307:2383–9. This randomized study compared IPCs to talc slury and found no significant differences in relief of dyspnea or quality of life, though the IPC group experienced more adverse events.
Putnam Jr JB, Light RW, Rodriguez RM, et al. A randomized comparison of indwelling pleural catheter and doxycycline pleurodesis in the management of malignant pleural effusions. Cancer. 1999;86:1992–9.
Fysh ETH, Tremblay A, Feller-Kopman D, et al. Clinical outcomes of indwelling pleural catheter-related pleural infections: an international multicenter study. CHEST J. 2013;144:1597–602. This is the largest study investigating the risk of infection using IPCs in patients with malignant pleural effusions. In 1,021 patients the overall risk of pleural infection was 4.9 %, and overall mortality was 0.29 %. Antibiotics should cover S. aureus and gram negative infections until microbiology is confirmed. In patients who do develop pleural infection, the mortality rate is 6 %.
Mekhaiel E, Kashyap R, Mullon JJ, Maldonado F. Infections associated with tunnelled indwelling pleural catheters in patients undergoing chemotherapy. J Bronchology Interv Pulmonol. 2013;20:299–303.
Van Meter ME, McKee KY, Kohlwes RJ. Efficacy and safety of tunneled pleural catheters in adults with malignant pleural effusions: a systematic review. J Gen Intern Med. 2011;26:70–6.
Thomas R, Budgeon CA, Kuok YJ, et al. Catheter tract metastasis associated with indwelling pleural catheters. Chest 2014.
Dresler CM, Olak J, Herndon 2nd JE, et al. Phase III intergroup study of talc poudrage vs talc slurry sclerosis for malignant pleural effusion. Chest. 2005;127:909–15.
Gonzalez AV, Bezwada V, Beamis Jr JF, Villanueva AG. Lung injury following thoracoscopic talc insufflation: experience of a single North American center. Chest. 2010;137:1375–81.
Tremblay A, Michaud G. Single-center experience with 250 tunnelled pleural catheter insertions for malignant pleural effusion. Chest. 2006;129:362–8. One of the largest studies of IPC, showing efficacy in approximately 90 % of patients. Mean duration of catheter days was 56 days.
Putnam Jr JB, Walsh GL, Swisher SG, et al. Outpatient management of malignant pleural effusion by a chronic indwelling pleural catheter. Ann Thorac Surg. 2000;69:369–75.
Musani AI, Haas AR, Seijo L, Wilby M, Sterman DH. Outpatient management of malignant pleural effusions with small-bore, tunneled pleural catheters. Respiration. 2004;71:559–66.
Pien GW, Gant MJ, Washam CL, Sterman DH. Use of an implantable pleural catheter for trapped lung syndrome in patients with malignant pleural effusion. Chest. 2001;119:1641–6.
Putnam Jr JB. Malignant pleural effusions. Surg Clin N Am. 2002;82:867–83.
Impact of aggressive versus standard drainage regimen using a long term indwelling pleural catheter (ASAP). In: ClinicalTrial.gov, 2014. Accessed 20140918, at https://clinicaltrials.gov/ct2/show/NCT00978939?term=pleurodesis&rank=19.
Intrapleural catheter daily versus three times a week drainage. In: ClinicalTrials.gov, 2014. Accessed 20140918, at https://clinicaltrials.gov/ct2/show/NCT00761618?term=pleurodesis&rank=26.
MacEachern P, Tremblay A. Pleural controversy: pleurodesis versus indwelling pleural catheters for malignant effusions. Respirology. 2011;16:747–54.
Olden AM, Holloway R. Treatment of malignant pleural effusion: PleuRx catheter or talc pleurodesis? A cost-effectiveness analysis. J Palliat Med. 2010;13:59–65.
Penz ED, Mishra EK, Davies HE, Manns BJ, Miller RF, Rahman NM. Comparing cost of indwelling pleural catheter vs. talc pleurodesis for malignant pleural effusion. Chest. 2014;146(4):991–1000.
Spiegler P, Hurewitz A, Groth M. Rapid pleurodesis for malignant pleural effusions. Chest. 2003;123:1895–8.
Hsu WH, Chiang CD, Chen CY, Kwan PC, Hsu JY. Ultrasound-guided small-bore Elecath tube insertion for the rapid sclerotherapy of malignant pleural effusion. Jpn J Clin Oncol. 1998;28:187–91.
Sartori S, Tombesi P, Tassinari D, et al. Sonographically guided small-bore chest tubes and sonographic monitoring for rapid sclerotherapy of recurrent malignant pleural effusions. J Ultrasound Med. 2004;23:1171–6.
Porcel JM, Salud A, Nabal M, Vives M, Esquerda A, Rodriguez-Panadero F. Rapid pleurodesis with doxycycline through a small-bore catheter for the treatment of metastatic malignant effusions. Support Care Cancer. 2006;14:475–8.
Reddy C, Ernst A, Lamb C, Feller-Kopman D. Rapid pleurodesis for malignant pleural effusions: a pilot study. Chest. 2011;139:1419–23.
Yildirim E, Dural K, Yazkan R, et al. Rapid pleurodesis in symptomatic malignant pleural effusion. Eur J Cardiothoracic Surg. 2005;27:19–22.
Folch E, Santacruz JF. Rapid pleurodesis: an outpatient alternative. Chest. 2011;140:1665–6.
Singapore General Hospital. A prospective, randomized controlled trial for a rapid pleurodesis protocol for the management of pleural effusions. NLM Identifier: NCT00758316. Bethesda (MD): In: ClinicalTrials.gov; 2014.
Active Pleurodesis Catheter. 2012. Accessed 18 Sept 2014, at http://www.sumobrain.com/patents/wipo/Active-pleurodesis-catheter/WO2012161954.html.
Tremblay A, Stather DR, Kelly MM. Effect of repeated administration of low-dose silver nitrate for pleurodesis in a rabbit model. Respirology. 2011;16:1070–5.
Tremblay A, Dumitriu S, Stather DR, Maceachern P, Illanes O, Kelly MM. Use of a drug eluting pleural catheter for pleurodesis. Exp Lung Res. 2012;38:475–82.
Marchi E, Vargas FS, Acencio MM, Antonangelo L, Teixeira LR, Light RW. Low doses of silver nitrate induce pleurodesis with a limited systemic response. Respirology. 2009;14:885–9.
Marchi E, Vargas FS, Teixeira LR, Acencio MM, Antonangelo L, Light RW. Intrapleural low-dose silver nitrate elicits more pleural inflammation and less systemic inflammation than low-dose talc. Chest. 2005;128:1798–804.
Compliance with ethics guidelines
Conflict of interest
Dr. Christopher Gilbert has no conflict of interest to disclose.
Dr. David Feller-Kopman reports personal fees from CareFusion, during the conduct of the study.
Human and animal rights and informed consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Pleural Diseases and Mesothelioma
Electronic supplementary material
Below is the link to the electronic supplementary material.
IPC in place with Talc Poudrage (AVI 34138 kb)
Rights and permissions
About this article
Cite this article
Gilbert, C.R., Feller-Kopman, D. Adjunct strategies to enhance the efficacy of indwelling pleural catheters. Curr Pulmonol Rep 4, 28–33 (2015). https://doi.org/10.1007/s13665-015-0110-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-015-0110-z