Abstract
Malignant pleural effusion (MPE) results from primary mesothelioma or the spreading of metastatic cancer. Both talc pleurodesis (TP) and indwelling pleural catheter (IPC) improve MPE symptoms. We performed a meta-analysis of randomized controlled trials to compare the efficacy of TP with that of IPC in patients with MPE. PubMed, EMBASE, Cochrane Library, and ClinicalTrials.gov databases were searched for studies published before February 2020. Individual effect sizes were standardized, and a meta-analysis was conducted to calculate a pooled effect size by using random effects models. In total, 4 trials with 500 patients were reviewed. Difference in pleurodesis success rate and change in dyspnea scores at 4 and 6 weeks between MPE patients treated with IPC and those treated with TP for pleurodesis were nonsignificant. The number of hospital inpatient days was significantly lower among patients who were treated with IPC (weight mean difference: 2.19; 95% confidence interval 0.70–3.67) than among those who were treated with TP. No significant difference was shown in adverse event profile between patients treated with IPC and those treated with TP for pleurodesis. In conclusion, both TP and IPC are equally effective in treating patients with MPE. The number of hospitalization days was significantly lower for patients who were treated with IPC, but the magnitude of the difference is of uncertain clinical importance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malignant pleural effusion (MPE) is a condition where excess fluid accumulates in the pleural cavity, resulting in increased permeability of pleural microvessels and involvement of local lymph nodes, thus reducing fluid reabsorption [1, 2]. MPE is usually the result of pleural mesothelioma, or the spread of metastatic cancers, often leading to distressing symptoms and mental stress [3]. Therefore, palliative management of patients with cancer and MPE involves effective alleviation of symptoms, mainly dyspnea, with minimal adverse effects and hospitalization.
Pleurodesis is currently the preferred treatment for MPE, which can be performed chemically through instillation of chemical sclerosants by using a chest tube or surgically through physical abrasion of pleural surfaces during thoracoscopy or thoracotomy [4, 5]. Meta-analyses have concluded that talc is the most effective means for pleurodesis treatment [2, 6]. However, it typically involves an inpatient stay of 4 to 7 days. In patients receiving palliative care, it may represent a substantial portion of their remaining life [2].
Indwelling pleural catheter (IPC) is increasingly used as an alternative to talc pleurodesis (TP), offering an advantage of outpatient management [7]. Clinical studies have shown that patients who received IPC without chemical pleurodesis had a lower spontaneous pleurodesis rate [8, 9]. Nevertheless, as a short-stay procedure, IPC allows ambulatory drainage, which mitigates breathlessness and pain among other symptoms [10].
In view of the recent emergence of an alternative MPE management technique, by performing a systematic review and meta-analysis of evidence available to date, we compared the outcome of patients with MPE treated with IPC with or without TP.
Materials and methods
Inclusion criteria
Randomized controlled trials (RCTs) that evaluated the outcome of IPC or chest drain plus TP versus IPC alone were included. Furthermore, studies were required to clearly report inclusion and exclusion criteria for patients, treatment protocols, drainage procedures, and definitions and evaluations of outcome parameters. We excluded RCTs that included patients aged < 18 years, patients who had previously undergone pleurodesis, or duplicate patient cohorts.
Search strategy and study selection
Relevant studies published before February 2020 were identified from PubMed, Embase, and Cochrane databases. The following Medical Subject Headings (MeSH) terms were used: talc pleurodesis OR pleural catheter AND malignant pleural effusion. All abstracts, studies, and citations retrieved were reviewed. In addition, we reviewed the reference sections of relevant papers to identify studies matching our criteria. No language restrictions were applied. The systematic review described herein has been accepted by PROSPERO, an online international prospective register of systematic reviews, curated by the National Institute for Health Research (CRD42018103935).
Data extraction
Baseline and outcome data were independently abstracted by 2 reviewers; in addition, study population characteristics, inclusion and exclusion criteria, drainage techniques, TP strategies, adverse events, and outcome parameters were extracted. Decisions recorded individually by the reviewers were compared, and disagreements were resolved by a third reviewer.
Methodological quality appraisal
Two reviewers independently assessed the methodological quality of each trial by using the revised tool for assessing risk of bias in randomized trials (RoB 2.0). Studies were awarded an overall risk of bias grade of high, some, or low [11]. This grade was calculated by assessing 5 domains: bias arising from the randomization process, bias owing to deviation from the intended intervention, bias owing to missing outcome data, bias in the measurement of the outcome, and bias in the selection of reported results.
Outcomes
The primary outcomes were the pleurodesis success rate and dyspnea score. Secondary outcomes were the number of hospital inpatient days, number of adverse events, and quality of life (QoL). The occurrence of adverse events, including infection, catheter blockage or loculations, pain, dyspnea, and death, were recorded.
Statistical analyses
Data were entered into and analyzed using the Review Manager, version 5.3 (The Cochrane Collaboration, Oxford, England). We followed the standards set by the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) for the reporting of our study [12]. Standard deviations were estimated from provided confidence interval (CI) limits or standard errors. Dichotomous outcomes were analyzed using risk ratios (RRs) as the summary statistic. Effect sizes of continuous outcomes were reported as the weighted mean difference (WMD). The precision of effect sizes was reported as 95% CIs. A pooled estimate of the RR and WMD was computed using the DerSimonian and Laird random-effect model [13].
To evaluate the statistical heterogeneity and inconsistency of treatment effects across studies, Cochrane Q tests and I2 statistics, respectively, were used. Statistical significance was set at P < .10 for Cochrane Q tests. Statistical heterogeneity across studies was assessed using the I2 test, which quantified the proportion of total outcome variability across studies. Moreover, subgroup analyses were performed by pooling available estimates for similar subsets of patients across trials.
Results
Trial characteristics
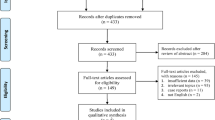
Figure 1 is a flowchart describing the screening and selection of trials. The initial search strategy yielded 880 citations, of which 694 were found to be ineligible based on criteria used for screening titles and abstracts. Thus, the full texts of 186 studies were retrieved. However, most of them were excluded from our final review because of the following reasons: 18 were retrospective studies or prospective articles; 124 included treatment for other diseases, such as nonmalignant pleural effusion; 8 evaluated the effects of MPE by using different interventions; and 32 were review articles. Thus, 4 studies were finally eligible for inclusion [2, 7,8,9].
These 4 trials were published between 2012 and 2018 and had sample sizes ranging from 94 to 154 patients. All trials had recruited patients with histologically proven MPE or recurrent exudate pleural effusions with extrapleural cancer. Three trials compared patients who underwent IPC alone and TP through chest tube [7,8,9]. In one trial, all patients received IPC insertion, who subsequently underwent outpatient drainage for 10 days. If no evidence of substantial lung entrapment, patients were randomized to TP or placebo groups [2]. The baseline characteristics of the treatment groups of 4 RCTs were balanced [2, 7,8,9] (Table 1).
The methodological quality of the included trials is summarized in Table 2. Three trials reported acceptable methods of randomization [2, 7, 8]. One trials did not describe the concealment of the allocation sequence [9]. All trials used the intention-to-treat analysis. Per-protocol analysis was included additionally in 2 studies [8, 9]. Loss to follow-up was high (> 30%) in 1 trial [9]. One trial did not describe the blinding of outcome assessors [9]. Other biases in the selected studies included incomplete treatments [9] and differences in the cancer type proportion between TP and IPC groups [8].
Pleurodesis success rate
All RCTs compared the pleurodesis success rate of patients with MPE treated with IPC with those treated with TP. In 3 trials, pleurodesis was defined as unsuccessful if there was a need for further ipsilateral pleural intervention [7,8,9]. In one trial, pleurodesis failure was defined when pleural fluid reaccumulation was confirmed through thoracocentesis or radiography or when > 50 mL of the fluid was drained on 3 consecutive occasions through IPC [2]. One RCT was excluded in this analysis as it lacked data of the control group [7]. The meta-analysis revealed no significant difference (RR 1.04; 95% CI 0.54–1.98) between the TP and IPC groups (Fig. 2). In the excluded RCT, the pleurodesis success rate was 88.8% (48 of 54) in the TP group; data for the IPC group were not provided [7].
Change in the dyspnea score
The degree of dyspnea was assessed in 4 trials [2, 7,8,9] by using a 100-point VAS (0 = no dyspnea and 100 = maximum possible dyspnea) in 2 trials [2, 7], a 100-point VAS (0 = maximum possible dyspnea and 100 = no dyspnea) in 1 RCT [8], and a 12-point Modified Borg Scale (MBS) consisting of (0, 0.5, and 1–10) in 1 trial [9]. One of the 4 RCTs was excluded from the analysis as data for the standard deviation were not provided [9]. Results of the 3 included trials were converted into a 100-point scale (0 = no dyspnea and 100 = maximum possible dyspnea) [2, 7, 8]. The pooled mean difference in the increase of dyspnea score was − 2.16 (95% CI −7.59 to 3.27) at week 4 and − 0.42 (95% CI −5.94 to 5.10) at week 6 after the procedure. The meta-analysis revealed no significant difference between TP and IPC groups regarding the change in dyspnea scores (Fig. 3). In the excluded RCT, the improvement median in MBS dyspnea scores at rest at week 6 was 3 in the TP group and 1.2 in the IPC group (P = .25) [9].
Hospital inpatient days
The number of hospital inpatient days was recorded in 4 RCTs [2, 7,8,9]. One of the 4 RCTs was excluded from the analysis due to the absence of the standard deviation [9]. The IPC group showed a significantly shorter duration of hospital stay (WMD 2.19 days; 95% CI 0.70–3.67) than did the TP group (Fig. 4). One RCT measured all-cause hospital inpatient days from randomization to 70 days after randomization [2], whereas 2 others measured effusion or drainage-related hospital inpatient days from randomization to 12 months after randomization [7, 8]. In the excluded RCT, the median hospital duration since randomization was 7 days in the TP group and 2 days in the IPC group [9].
Adverse events
The incidence of adverse events was reported in 4 trials [2, 7,8,9]. No significant differences were observed in TP and IPC groups’ infection occurrence (RR 0.49; 95% CI 0.12–2.02) [2, 7,8,9], catheter blockage or loculations (RR 0.42; 95% CI 0.08–2.09) [2, 7, 8], pain (RR 0.68; 95% CI 0.33–1.44) [2, 8, 9], dyspnea (RR 1.15; 95% CI 0.42–3.14) [8, 9], and death (RR 0.83; 95% CI 0.33–2.10) (Fig. 5) [2, 8].
Quality of life
Quality of life was measured in 3 trials [2, 7, 8]. QoL was measured with the EuroQoL Group 5-Dimensions 5-Level Questionnaire (EQ-5D-5 L) [14] in Thomas et al. [8], while the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire-Core 30 (QLQ-C30) [15] was used in Davies et al. [7]. Bhatnagar et al. included QoL measurement by both EQ-5D-5 L and QLQ-C30 [2]. Data pooling for QoL measurement could not be performed because clinical parameters among the selected trials were not uniformly reported. Davies et al. and Thomas et al. reported no significant difference in quality of life between TP and IPC groups [7, 8]. However, Bhatnagar et al. showed that patients in the TP group reported better quality of life scores than did those in the IPC group [2].
Discussion
Time spent in a hospital is often the main concern in the palliative management of MPE. The results of our study did not reveal significant differences in pleurodesis success rate, dyspnea scores, and adverse events, between the groups. However, the meta-analysis revealed that treatment with IPC resulted in fewer hospital inpatient days compared with treatment with TP.
According to the current British Thoracic Society guidelines, TP is the first-line therapy for MPE management [4]. However, as the procedure typically requires hospitalization for 4 to 7 days, it may take up a significant portion of a patient’s remaining lifespan [2, 16]. The results of two retrospective studies are in agreement with the findings of the current study. These studies indicated that both total and effusion-related hospital bed days were significantly fewer among patients receiving IPC [17, 18]. The phenomenon can be explained by the difference in procedural administration. IPCs were placed as day-case or overnight procedures, whereas TP involved chest tube insertion, complete evacuation of the fluid, talc instillation, and hospitalization until fluid drainage ceased [8]. A shorter length of hospital stay may allow end-stage patients to spend less of their limited remaining lifetime in the hospital. However, although IPC may be a better treatment option, patients need to frequent hospital and clinic visits to troubleshoot IPC related issues, and require close outpatient support [19]. In Bhatnagar et al., the authors compared IPC plus TP with placebo, the mean number of days that patients spent in the hospital until day 70 was not significant difference between groups, indicated that patients required long-term treatment due to the inconvenience of regular drainage [2]. Therefore, despite significant evidence revealing a shorter hospital stay for patients with MPE who received IPC in this analysis, the clinical significance is currently uncertain.
Several studies comparing IPC and TP for patients with MPE have suggested that treatment with IPC results in a greater improvement in dyspnea and more effective pleural effusion control [17, 18, 20]. A retrospective study revealed 15.7% of MPE patients receiving TP required secondary intervention, while only 6.3% of that receiving IPC required reintervention [21]. An multicenter prospective study with 160 patients recruited revealed IPC offered a more effective fluid control over TP (86.5% vs. 67.7%). The study also suggested more patients in IPC group perceived improvement in dyspnea (93.3%) when compared to TP group (78.6%) [18]. However, the results in our meta-analysis suggested that both procedures are equally effective for pleurodesis and relieving dyspnea, reflecting no significant difference in the pleurodesis success rate and dyspnea improvement.
Spontaneous pleurodesis is an important issue in treating MPE. A systematic review suggested an average incidence of spontaneous pleurodesis to be 45.6% (at approximately 2 months) [22], this result was similar to Davies et al. which presented 51% of spontaneous pleurodesis in IPC group [7]. However, in Muruganandan et al., spontaneous pleurodesis rate at 2 months was reported to be 37.2% in the aggressive drainage group and 11.4% in the symptom-guided group [23]. These data may imply that the true incidence of spontaneous pleurodesis may be lower than the figures previously reported in retrospective studies. In our included trials, although Bhatnagar et al. revealed IPC plus TP had a greater chance of pleurodesis than IPC alone, TP followed by IPC drainage for 10 days before TP administration may also play a role in the success of pleurodesis [2].
Our study revealed similar safety profiles for both IPC and TP groups, which echoes with a multicenter prospective study of 160 patients indicating comparable safety profiles between two groups [18]. However, the mortality rates of patients with MPE undergoing IPC and TP are controversial. In a retrospective study which included 360 patients, the median survival time was longer in patients receiving IPC (148 days) than in those receiving TP (133 days) [17]. Nevertheless, a review of an American cancer center database with a total of 238 patients, indicated that patients treated with TP had significantly higher survival compared with IPC (18.7 vs. 4.1 months, P < .001) [21]. Our meta-analysis results reflected comparable adverse event occurrence and mortality rates for IPC and TP. In Davies et al., one pleural infection in the IPC group was considered to have contributed to the patient’s death [7]. However, the cause of death was not documented in most of the included trials. Thus, whether mortality was caused by the choice of procedure or underlying disease could not be determined.
Our included trials displayed considerable heterogeneity because of various factors. First, the measurement of hospitalization days was not uniform across the studies; some of them measured all-cause hospitalization [2], whereas some measured effusion-related hospitalization [7, 8]. Second, pleurodesis success was defined differently across the studies. Finally, adverse event measurement may have differed across the trials.
This study has several limitations. First, some trials had a small sample size of patients recruited per treatment group; the small sample size may undermine the power of their study [9]. Second, some trials had a high dropout rate of participants; this may lead to bias in patient randomization, thereby potentially leading to bias in our analysis [9]. Third, QoL is an important indicator when comparing palliative procedures, however, data pooling for QoL measurements could not be performed in this review due to ununiform clinical parameters across included studies [2, 7, 8]. This may limit the comprehensiveness of the study. Finally, several primary and secondary outcomes were variably reported; the dyspnea score is a self-reported severity score and is therefore subjective, thereby potentially limiting the inference of our analysis.
In conclusion, our meta-analysis revealed that managing patients with MPE by IPC resulted in a significantly shorter hospital stay, but the magnitude of the difference is of uncertain clinical importance. Differences in the pleurodesis success rate, dyspnea improvement, and adverse event occurrence between the IPC and TP groups were nonsignificant. Therefore, beyond to TP, IPC is one of the suitable option for patients with MPE to manage for pleural effusion.
Abbreviations
- CI:
-
Confidence interval
- EQ-5D-5 L:
-
EuroQoL Group 5-Dimensions 5-Level Questionnaire
- IPC:
-
Indwelling pleural catheter
- MBS:
-
Modified Borg Scale
- MeSH:
-
Medical subject headings
- MPE:
-
Malignant pleural effusion
- QLQ-C30:
-
quality of life questionnaire-core 30
- QoL:
-
Quality of life
- RCT:
-
Randomized controlled trials
- RoB:
-
Risk of bias
- RR:
-
Risk ratios
- TP:
-
Talc pleurodesis
- WMD:
-
Weighted mean difference
References
Clive AO, Jones HE, Bhatnagar R, Preston NJ, Maskell N (2016) Interventions for the management of malignant pleural effusion: a network meta-analysis. Cochrane Database Syst Rev 5:CD010529. https://doi.org/10.1002/14651858.CD010529.pub2
Bhatnagar R, Keenan EK, Morley AJ, Kahan BC, Stanton AE, Haris M, Harrison RN, Mustafa RA, Bishop LJ, Ahmed L, West A, Holme J, Evison M, Munavvar M, Sivasothy P, Herre J, Cooper D, Roberts M, Guhan A, Hooper C, Walters J, Saba TS, Chakrabarti B, Gunatilake S, Psallidas I, Walker SP, Bibby AC, Smith S, Stadon LJ, Zahan-Evans NJ, Lee YCG, Harvey JE, Rahman NM, Miller RF, Maskell NA (2018) Outpatient talc administration by indwelling pleural catheter for malignant effusion. N Engl J Med 378:1313–1322. https://doi.org/10.1056/NEJMoa1716883
Porcel JM, Sole C, Salud A, Bielsa S (2017) Prognosis of cancer with synchronous or metachronous malignant pleural effusion. Lung 195:775–779. https://doi.org/10.1007/s00408-017-0050-1
Roberts ME, Neville E, Berrisford RG, Antunes G, Ali NJ, BTS Pleural Disease Guideline Group (2010) Management of a malignant pleural effusion: British Thoracic Society pleural disease guideline 2010. Thorax 65 (Suppl 2):ii32–i40. https://doi.org/10.1136/thx.2010.136994
Xia H, Wang XJ, Zhou Q, Shi HZ, Tong ZH (2014) Efficacy and safety of talc pleurodesis for malignant pleural effusion: a meta-analysis. PLoS ONE 9:e87060. https://doi.org/10.1371/journal.pone.0087060
Porcel JM, Lui MM, Lerner AD, Davies HE, Feller-Kopman D, Lee YC (2017) Comparing approaches to the management of malignant pleural effusions. Expert Rev Respir Med 11:273–284. https://doi.org/10.1080/17476348.2017.1300532
Davies HE, Mishra EK, Kahan BC, Wrightson JM, Stanton AE, Guhan A, Davies CW, Grayez J, Harrison R, Prasad A, Crosthwaite N, Lee YC, Davies RJ, Miller RF, Rahman NM (2012) Effect of an indwelling pleural catheter vs chest tube and talc pleurodesis for relieving dyspnea in patients with malignant pleural effusion. JAMA 307:2383–2389. https://doi.org/10.1001/jama.2012.5535
Thomas R, Fysh ETH, Smith NA, Lee P, Kwan BCH, Yap E, Horwood FC, Piccolo F, Lam DCL, Garske LA, Shrestha R, Kosky C, Read CA, Murray K, Lee YCG (2017) Effect of an indwelling pleural catheter vs talc pleurodesis on hospitalization days in patients with malignant pleural effusion: the AMPLE Randomized Clinical Trial. JAMA 318:1903–1912. https://doi.org/10.1001/jama.2017.17426
Boshuizen RC, Vd Noort V, Burgers JA, Herder GJM, Hashemi SMS, Hiltermann TJN, Kunst PW, Stigt JA, van den Heuvel MM (2017) A randomized controlled trial comparing indwelling pleural catheters with talc pleurodesis (NVALT-14). Lung Cancer 108:9–14. https://doi.org/10.1016/j.lungcan.2017.01.019
Sørensen PG, Svendsen TL, Enk B (1984) Treatment of malignant pleural effusion with drainage with and without instillation of talc. Eur J Respir Dis 65:131–135
Higgins JPT, Green S (2011) Cochrane handbook for systematic reviews of interventions version 5.1.0 [updated March 2011]. The Cochrane Collaboration. http://www.cochrane-handbook.org
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62:e1–e34. https://doi.org/10.1016/j.jclinepi.2009.06.006
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7:177–188. https://doi.org/10.1016/0197-2456(86)90046-2
Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, Bonsel G, Badia X (2011) Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res 20:1727–1736. https://doi.org/10.1007/s11136-011-9903-x
Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, Fleishman SB, de Haes JC et al (1993) The European Organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85:365–376. https://doi.org/10.1093/jnci/85.5.365
Gawron G, Gabrys J, Barczyk A (2013) Talc slurry pleurodesis via chest tube in department of pulmonology: a 24-case study. Pneumonol Alergol Pol 81:439–447
Hunt BM, Farivar AS, Vallières E, Louie BE, Aye RW, Flores EE, Gorden JA (2012) Thoracoscopic talc versus tunneled pleural catheters for palliation of malignant pleural effusions. Ann Thorac Surg 94:1053–1057. https://doi.org/10.1016/j.athoracsur.2012.01.103
Fysh ETH, Waterer GW, Kendall PA, Bremner PR, Dina S, Geelhoed E, McCarney K, Morey S, Millward M, Musk AWB, Lee YCG (2012) Indwelling pleural catheters reduce inpatient days over pleurodesis for malignant pleural effusion. Chest 142:394–400. https://doi.org/10.1378/chest.11-2657
Asciak R, Hallifax RJ, Mercer RM, Hassan M, Wigston C, Wrightson JM, Psallidas I, Rahman NM (2018) The hospital and patient burden of indwelling pleural catheters: a retrospective case series of 210 indwelling pleural catheter insertions. Respiration 97:70–77. https://doi.org/10.1159/000491934
Srour N, Amjadi K, Forster AJ, Aaron S (2013) Management of malignant pleural effusion with indwelling pleural catheters or talc pleurodesis. Can Respir J 20:106–110. https://doi.org/10.1155/2013/842768
Liou DZ, Serna-Gallegos D, Chan JL, Borgella J, Akhmerov S, Soukiasian HJ (2016) Survival difference in patients with malignant pleural effusions treated with pleural catheter or talc pleurodesis. Am Surg 82:995–999
Van Meter ME, McKee KY, Kohlwes RJ (2011) Efficacy and safety of tunneled pleural catheters in adults with malignant pleural effusions: a systematic review. J Gen Intern Med 26:70–76. https://doi.org/10.1007/s11606-010-1472-0
Muruganandan S, Azzopardi M, Fitzgerald DB, Shrestha R, Kwan BCH, Lam DCL, De Chaneet CC, Rashid Ali MRS, Yap E, Tobin CL, Garske LA, Nguyen PT, Stanley C, Popowicz ND, Kosky C, Thomas R, Read CA, Budgeon CA, Feller-Kopman D, Maskell NA, Murray K, Lee YCG (2018) Aggressive versus symptom-guided drainage of malignant pleural effusion via indwelling pleural catheters (AMPLE-2): an open-label randomised trial. Lancet Respir Med 6:671–680. https://doi.org/10.1016/S2213-2600(18)30288-1
Acknowledgements
We thank Mr. Eugene, Chun-Chit Cheng for assistance with data collection, and Wallace Academic Editing for edition of the manuscript.
Funding
This research received no specific Grant from any funding agency in the public, commercial, or not-for-profit sector.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
The authors Maggie Yeung, El-Wui Loh, Tung-Yu Tiong, and Ka-Wai Tam have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yeung, M., Loh, EW., Tiong, TY. et al. Indwelling pleural catheter versus talc pleurodesis for malignant pleural effusion: a meta-analysis. Clin Exp Metastasis 37, 541–549 (2020). https://doi.org/10.1007/s10585-020-10042-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10585-020-10042-2