Abstract
We report on the systematic review and meta-analysis concerning the efficacy of R. officinalis in treating diabetes mellitus (DM) in animals. This study followed the PRISMA guideline and the protocol was registered in PROSPERO (CRD42021250556). The research was duplicated in the PubMed, Scopus, ScienceDirect, Web of Science, and Virtual Health Library (VHL) databases until December 31st, 2022. No restrictions have been set for language publication. Twenty-three (23) experimental studies of type-1 diabetes mellitus (T1DM) met the eligibility criteria and were included in the qualitative analysis, whereas eighteen (18) underwent a meta-analysis. The R. officinalis derivatives significantly decreased fasting plasma glucose (MD: −120.84 [95% CI; −157.09, −84.59]); increased insulin release (MD; +3.73 [95% CI; +3.17, +4.29]); dwindled blood urea nitrogen (MD: −24.84 [95% CI; −34.78, −14.90]) and creatinine (MD: −0.40 [95% CI; −0.74, −0.06]) levels; and ameliorated liver function or repaired liver damage by decreasing ALT (MD: −36.42; [95% CI; −55.69, −17.14]) and AST (MD: −24.05 [95% CI; −37.84, −10.27]) enzyme levels compared to vehicle control group. Moreover, R. officinalis derivatives improved the lipid profile of diabetic animals by reducing LDL-c levels (MD: −11.74 [95% CI; −21.27, −2.21]). R. officinalis is a nutraceutical that may help in the management of T1DM and its complications. However, some gaps need to be taken into account for this evidence. Greater attention is needed for an analytical standardization of Rosemary extracts besides the demand for high-quality clinical studies dealing with the efficacy of this phytomedicine.
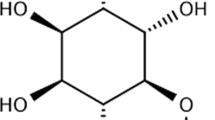
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
DM is a metabolic disorder characterized by persistent hyperglycemia due to a deficiency in insulin production or its action or in both mechanisms. This chronic ailment has been classified as a troubling disease for the twenty-first century. According to the International Diabetes Federation Global Diabetes Atlas (10th Edition), DM reached about 537 million adults in 2021 was responsible for around 6.7 million deaths, and cost USD 966 billion in health spending in the last 15 years (International Diabetes Federation 2021).
Uncontrolled DM has deleterious consequences and several complications, such as circulatory problems (increased risk of heart disease, stroke, and peripheral blood vessels), kidney diseases, arterial hypertension, and a higher mortality rate when compared with non-diabetic and healthy patients; which can impair affected patients’ quality of life and also reduction or loss of productive capacity (Almutlaq et al. 2021; Bjornstad et al. 2022; de Souza Stork et al. 2022; Shrestha and Ghimire 2012).
It is known that OS, which is a state of imbalance between the production of ROs and endogenous antioxidant capacity; triggers the complications of DM (Reis et al. 2021). The main molecular mechanisms associated with OS in DM are related to glucose and lipid metabolism (Giacco and Brownlee 2010).
Under conditions of hyperglycemia, the excessive production of ROs during glycolysis reactions leads to damage in both DNA and DNA repair enzymes, causing accumulation of glyceraldehyde-3-phosphate content, which is responsible for the activation of other pro-oxidant pathways and the auto-oxidation of glucose. Thus, a boost in the production of hydrogen peroxide, a precursor of oxidizing substances, is observed. Furthermore, the auto-oxidation of glucose leads to the formation of glyoxal, an advanced glycation end-product precursor, which promotes cellular OS (Darenskaya et al. 2021).
Even though the complications of DM are diverse and clinically relevant, the pharmacological treatment options for either T1DM or T2DM are narrowed to a few common approaches. The treatment of T1DM involves the administration of insulin, but there is a chance of developing so-called insulin resistance, manifesting in most cases itself at the cellular level through post-receptor defects in insulin signaling. In another hand, T2DM is treated with oral antihyperglycemic drugs, which are associated with several side effects. Therefore, more patients seek lifestyle modifications combined with natural and safer options like nutraceuticals for the management of DM (Buzzetti et al. 2020; Shi et al. 2019).
Some nutraceuticals, like super fruits and spices exhibiting high anti-radical and anti-inflammatory activity, are sources of copious phytochemicals that can regulate alpha-glucosidase and lipase activities, improve pancreatic function and insulin release and reduce blood glucose levels, boosting the effects of hypoglycemic or antihyperglycemic agents (Alhujaily et al. 2022; Dehdashtian et al. 2020). Thus, they act as antioxidants, mitigating the imbalance of ROs and blocking the synthesis of prostaglandins, pro-inflammatory cytokines, and transcription factors, mainly the NF-κB factor. Consequently, such foodstuffs may be highly effective in the management of DM and its worsening (Alhujaily et al. 2022; Derosa et al. 2022; Zhang et al. 2015).
Rosemary (Rosmarinus officinalis L., Lamiaceae) is an aromatic household spice that has been used worldwide for culinary, food preservative, and medicinal purposes owing to its powerful antioxidant properties (Sánchez-Camargo and Herrero 2017). There is increasing scientific evidence supporting its efficacy in preclinical models in which the OS is involved, such as inflammation (Gonçalves et al. 2022), neurodegeneration (Capatina et al. 2020), cancer (Pérez-Sánchez et al. 2019) and DM (Bao et al. 2020; Hassani et al. 2016; Naimi et al. 2017). Its wide range of bioactivities can be due to the synergism of antioxidant phytochemicals such as diterpenes, triterpenes, phenolic acids, flavonoids, and volatile compounds (Ulbricht et al. 2010; Yashin et al. 2017).
Despite plenty of original papers and narrative reviews reporting the healing properties of R. officinalis, its efficacy in DM and DM complications has not been systematically reviewed and statistically compared so far. Therefore, healthcare professionals across the globe still lack high-level evidence that supports the use of R. officinalis in complementary and integrative medicine as a coadjutant in the management of DM.
Motivated by this scientific and clinical gap, this investigation aimed to provide a systematic review and meta-analysis concerning the effects of R. officinalis in the biochemical outcomes of animals that underwent pre-clinical models of DM. Insights on the overall methodological quality and bias of the included primary studies are also presented. Our findings are consistent with using R. officinalis in traditional medicine for managing DM. Besides, this scientific contribution is a step forward in evidence-based practices related to the rationale use of R. officinalis in primary healthcare and poses this nutraceutical as the target of further clinical investigations associated with DM and its complications.
Material and methods
Study design and guiding question
This systematic review was carried out according to the PRISMA guideline (Page et al. 2021). This study was registered in PROSPERO with protocol number CRD42021250556 (https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021250556). Our guiding question was: Does R. officinalis improve the biochemical outcomes of animals in experimental models of diabetes mellitus?
Sources of information and search strategies
The electronic databases PubMed (MEDLINE), Scopus, ScienceDirect, Web of Science (Science Citation Index), and VHL were used for the search of relevant publications issued until December 31st, 2022. The authors also searched citation reference lists of relevant included studies and any previously published reviews and gray literature to include other studies in Google Scholar, through the D.O.I of the intended study. Thus, all the searches were performed by two independent researchers (V.M.O and L.R.S) on January 13th, 2023.
None of the collection language was restricted during the identification of the studies. The authors of the unavailable articles were contacted twice by e-mail, through which they were requested access to the articles and other information (raw data).
The descriptors were delimited and defined from the MeSH and DeCS tools. The research strategies used in this review were carried out using the PECOS acronym, i.e.: population (P); exposure (E); comparator (C); outcomes (O); and study design (S). The research terms were combined using the Boolean logical terms “AND” and “OR”. Research filters (document type = “article”) for the identification of preclinical studies in the Web of Science and VHL were applied to increase filtering and research efficiency. The research strategies used for each database are detailed in Table S1 of the Supplementary Material.
Eligibility criteria
The eligible and selected articles from the databases were read in full and evaluated according to the inclusion and exclusion criteria predefined from the PROSPERO protocol prioritized in terms of i) type of exposure/intervention, ii) type of population, iii) study design and, iv) type of publication.
Inclusion criteria:
-
(i)
treatment with preparations of R. officinalis at any dosage, administered at any time, by any administration route, and any dose frequency;
-
(ii)
all animal models of DM (deficiency in insulin production and failure of β cells to ensure construct validity), all sexes, all ages, and all species of animals/strains;
-
(iii)
experimental studies with separate control groups; cross-design, randomized, and non-randomized study designs;
-
(iv)
original articles and short communications (published or ahead of print) were considered.
Exclusion criteria:
-
(i)
combined treatment of R. officinalis L., or isolated pure compounds or R. officinalis combined with standard oral hypoglycemic agents;
-
(ii)
studies in humans, animals with any other comorbidity
-
(iii)
in vitro and ex vivo study designs, in silico, studies before and after without a control group;
-
(iv)
case reports, review articles, editorials, letters to the editor, and articles presented at scientific events, news, comments, dissertations, and thesis were excluded.
After searching the databases, the articles were transferred to the Rayyan QCRI application (Ouzzani et al. 2016) to organize, remove duplicates, and apply the eligibility criteria of each article and thus associate them with eligible or not for inclusion.
Throughout the selection of the articles, each reviewer (VMO, LRS) was blinded about the other’s decisions, and the discrepancies were discussed until a consensus or, if it was not possible, a third author (ROC) was consulted. It is noteworthy that the final decision of the articles to be included is made by consensus among all the researchers involved.
The Kappa coefficient (Landis and Koch 1977) was used to assess the level of agreement between the two authors (VMO, LRS). In this pursuit, we considered a 95% CI and used the Stata 11.0 software package.
Data extraction
The primary and secondary data of the included studies were extracted for a standardized and pre-formatted electronic spreadsheet. Data were collected considering the animal models (species/strains of animals used; sex of animals; number of animals per group; age and weight of animals; type of feeding used); study design (number of experimental groups and duration of follow-up; method of allocation to the treatment group; type of diabetes whether T1DM or T2DM; and blind or non-blind evaluation method); intervention characteristics (taxonomic identification of the herb; voucher number; method of preparation of R. officinalis extract; methods and parameters of quality control; chemical composition; dose; dose frequency; time and route of administration; method of induction of DM and time to begin exposure; parameters to be considered diabetic; whether nephrectomy was performed or not); identification of the study (authors; year of publication; country where the research was conducted); and publishing language.
The main results evaluated were: FPG (mg/dL); HbA1c (%); SIL (mU/L); lipid profile [Tg (mg/dL), HDL-c (mg/dL), LDL-c (mg/dL), and TC (mg/dL); ALP (U/L), ALT (U/L), AST (U/L), and Alb (g/dL) for liver function; BUN (mg/dL), AUR (mg/dL), and CRE (mg/dL) for renal function.
Taxonomic evaluation
Taxonomic and nomenclature accuracy was evaluated by comparing the taxonomic information reported with existing patterns in an open botanical database accessible at https://wfoplantlist.org/plant-list. A classification was then elaborated according to methods proposed elsewhere (Rivera et al. 2014) to evaluate the taxonomy and identification of plant species used.
For studies that included complete information on plant species, identification and proof of the specimen presented, it was qualified as “LEVEL 1”. For studies that did not present information on identification and proof of the specimen, a classification of “LEVEL 2” was then assigned; finally, studies with incomplete information or that did not present any information about the species, collection, identification, and proof of specimens, received a classification of “LEVEL 3” (Rivera et al. 2014).
Data synthesis
The qualitative data of the included studies were described in narrative synthesis and summarized in tables to establish patterns and variations. Statistically, we used signs to indicate significant increment (↑), decrement (↓), or equality ( ↔) effect size measured between treatment and control groups.
Quantitative data were grouped into a statistical meta-analysis using RevMan 5.3 (Copenhagen: The Nordic Cochrane Centre). The meta-analysis was carried out exclusively for two or more studies depicting data on a specific outcome of interest. Herein, given the great diversity of the experimental models, only the most effective dose and the greatest frequency of exposure were considered. As the same outcome could be reported in different measurement scales, we performed mathematic conversions to the same scale. Data of FPG (mg/dL), HbA1c (%), SIL (mU/L), Tg (mg/dL), HDL (mg/dL), LDL (mg/dL), TC (mg/dL), ALP (U/L), ALT (U/L), AST (U/L), Alb (g/dL), BUN (mg/dL), AUR (mg/dL), and CRE (mg/dL) underwent metanalysis. MD and SD were used to assess continuous variables with a 95% CI. The p-value < 0.05 was considered statically significant. For studies reporting, the standard errors of means, and the corresponding SD were calculated by multiplying by the square root of the respective sample size.
The inverse method of weighted variance was used to attribute the relative contribution of each study included to the effect of the grouped standard deviation of R. officinalis and its 95% CI. The random effects model was used for pooling effect estimates because the effect sizes from animal studies probably differ more due to the distinction in design features (Peter et al. 2021).
Heterogeneity assessment
We used the I2 statistic to evaluate the severity of heterogeneity. The I2 ≥ 75% was considered indicative of substantial heterogeneity (Borenstein et al. 2010). Subgroup analysis was carried out to identify potential factors that influence heterogeneity in the FPG and SIL.
Assessment of the risk of bias and quality of the included articles
Two reviewers (VMO and LRS) independently evaluated the risk of bias using SYRCLE’s tool (Hooijmans et al. 2014b). By using this tool, it was possible to evaluate selection bias, performance bias, detection bias, friction bias, reporting bias, and other types of biases.
The ten domains evaluated in this tool are random sequence generation; basic characteristics; allocation concealment; random housing; blinding of participants and staff; evaluation of random results; incomplete results data; reports of selective results; and other sources of bias. The risk of bias was assessed using RevMan 5.3 (Copenhagen: The Nordic Cochrane Centre). Then, two independent researchers (VMO and LRS) evaluated all the studies included through the CAMARADES checklist (Bahor et al. 2021) for study quality. Disagreements were resolved with discussion.
Results
Search results
Figure 1 depicts the PRISMA flowchart with the selection of studies performed in this systematic review. A total of 4909 studies were identified in the electronic databases search. After reviewing the title and abstract, 322 papers were excluded for being duplicates (coming from the two different databases). During the title, keywords, and abstract screening 4876 articles were further discarded. The full text of the 33 potentially relevant articles was assessed and 15 papers were excluded due to the following reasons: not an R. officinalis preparation (n = 6), not a DM model (n = 4), dissertation (n = 1), wrong experimental design (n = 1), in vitro experiments (n = 2), unseparated control group (n = 1).
After carrying out a thorough review of the literature, including both published articles and gray literature, a total of five articles were selected for full-text reading. In addition, two articles were identified as potentially relevant (Erenmemisoglu et al. 1997; Malek et al. 2020) and we contacted the authors requiring full access, but only one was obtained (Malek et al. 2020).
The study comprised 23 articles (Al-badry 2017; Al-Hader et al. 1994; Alnahdi 2012; Ayaz 2012; Bakirel et al. 2008; Belmouhoub et al. 2016, 2017, 2020; Benkhedir et al. 2022; El-Boshy et al. 2015; Emam 2012; Khalil et al. 2012; Koga et al. 2006; Malek et al. 2020; Mohamed 2021; Nazem et al. 2015; Ramadan et al. 2013; Rasoulian et al. 2019; Sebai et al. 2015; Selmi et al. 2017; Shen et al. 2020; Silva et al. 2011; Wahba 2022), of which 18 were eligible for the meta-analysis (Al-Hader et al. 1994; Alnahdi 2012; Ayaz 2012; Bakirel et al. 2008; Benkhedir et al. 2022; El-Boshy et al. 2015; Emam 2012; Khalil et al. 2012; Malek et al. 2020; Mohamed 2021; Nazem et al. 2015; Ramadan et al. 2013; Rasoulian et al. 2019; Sebai et al. 2017; Shen et al. 2020; Silva et al. 2011; Wahba 2022). Throughout the eligibility evaluation, the degree of agreement between the two researchers (Kappa coefficient) was of 0.992, which is considered almost perfect (Landis and Koch 1977).
Description of the included studies
General Features
Table 1 summarizes the experimental design of the studies herein included, Moreover, Table 2 presents the qualitative synthesis of their main findings. The majority of included studies used rats (69.6%; n = 16), while 21.7% (n = 5) used mice and 8.7% (n = 2) used rabbits. A total of 21 studies (91.3%) used only male animals, 1 (4.3%) study used only females and 1 (4.3%) used both sexes. About 56.5% of the studies (n = 13) did not specify the animal’s age, being that the age of the animals ranged from 13 days to 3 months.
About 47.8% (n = 11) of studies used R. officinalis aqueous extract, 34.8% (n = 8) used hydroalcoholic extract, 8.7% (n = 2) used fortified power diet and 8.7% used the volatile oil. A total of 10 studies (43.5%) presented data of qualitative and quantitative analysis of the phytochemicals contained in the extracts.
The doses of R. officinalis administered ranged from 25 to 800 mg/kg (200.7 ± 156.8 mg/kg). Only two studies (8.7%) did not specify the dose (mg/kg) used, and the other 2 studies (8.7%) blended leaves powder in animals’ diets with doses ranging from 0.05% to 10%.
Oral administration was the most frequent among studies (82.6%; n = 19), while 3 studies (13%) used intraperitoneal administration and 1 study (4.3%) used intramuscular administration. The once-a-day regimen of administration was performed in all the included studies (100%).
The histopathology and anatomopathological analysis were assessed in 8 studies (34.8%), which related to nonharmful effects in the evaluated organs. R. officinalis reduced histopathological changes induced by DM on the kidney and liver of the treated animals, also displayed amelioration in the degeneration of Langerhans islets, attenuated hepatic DM-induced alteration in hepatocytes, preserved renal architecture, decreased plasma inflammatory cytokine and enhanced the reproductive performance by reversing semen abnormalities.
Table S2 of the Supplementary Material presents the characteristics of DM induction protocols in the included studies. All of the studies carried out T1DM experimental models, with FPG levels at baseline greater than 200 mg/dL; since the researchers chemically induced the illness by using alloxan or streptozotocin (STZ) (King 2012).
About 39.1% of the studies (n = 9) used alloxan and 60.9% (n = 14) used STZ. The STZ doses used range from 40 to 110 mg/kg (60.8 ± 28.3 mg/kg). In turn, the doses of alloxan used ranged from 120 to 220 mg/kg (146.1 ± 32.0 mg/kg). The time taken to confirm that the diabetes is stabilized after the exposure to induction material was between 2 and 7 days. Only 5 studies (21.7%) reported pancreatectomy, which was used to prevent pancreatic beta regeneration.
The animal’s diet was assessed in 13 studies (56.5%), in which 2 studies (8.7%) reported the amount of nutrients contained in the food. Concerning the exposure time, 5 studies (21.7%) carried out acute follow-up (up to 24 h), while 13 (56.5%) studies performed subacute follow-up (from 1 up to 21 days) and 7 studies (30.4%) performed subchronic follow-up (>22 days). Noteworthy, in some studies more than one follow-up period was investigated depending on the outcome assessed.
Taxonomic evaluation
The full taxonomic analysis of the included studies is presented in Fig. S1 of the Supplementary Material. The majority of the studies (56.5%, n = 13) were classified as LEVEL 1, with higher quality and complete information about the specimens; 8 studies (34.8%) were classified as LEVEL 2 because they did not use an appropriate style to formally differentiate the nomenclature from other text, and/or provide data and evidence of specimens used and/or provided data on how these specimens were identified. Finally, 2 studies (8.7%) were classified as LEVEL 3, because did not fulfill 3 or more specified items.
The effects of R. officinalis in the biochemical parameters of animals with DM
Lowering the FPG, but not the HbA1c levels
As can be seen in Fig. 2A, seventeen preclinical studies (n = 256) were pooled and indicated that R. officinalis derivatives significantly reduced FPG compared with vehicle control groups, representing −120.84 of MD (95% CI; −157.09, −84.59), I2 = 99% (indicating a heterogeneity between the groups). The great majority of the studies (88.2%; n = 15) favored R. officinalis. In turn, Fig. 2B showcases that R. officinalis did not significantly reduce HbA1c as compared to the control groups (2 studies, n = 28; MD = −1.77 [95% CI; −6.16, + 2.61]; I2 = 70%).
Boosting the insulin release
Figure 2C depicts the metanalysis for SIL. The data from nine studies were pooled and provided evidence that R. officinalis significantly increases the release of insulin (n = 138; MD = + 3.73 [95% CI; + 3.17, + 4.29]) in comparison to the vehicle control groups. The I2 was 100%, which showcases heterogenicity between the groups. Noteworthy, all studies consistently favored R. officinalis.
Decreasing hepatic damage
As reported in Fig. 3A, B, respectively, data of three studies (n = 38) were pooled and indicated that treating the animals with R. officinalis significantly reduced both ALT (MD = −36.42; [95% CI; −55.69, −17.14]; I2 = 99%) and AST (MD = −24.05; [95% CI; −37.84, −10.27]; I2 = 85%) enzyme levels compared to vehicle control groups. On the other hand, R. officinalis did not significantly decrease the ALP enzyme levels (MD = −13.28; [95% CI; −33.08, +6.52]; I2 = 88%) as shown in Fig. 4C. Moreover, the Alb levels (Fig. 4D) were not significantly affected following the treatment with R. officinalis (3 studies, n = 36; MD = + 2.00 [95% CI; −0.86, + 4.86]; I2 = 100%).
Slightly recovering the kidney function
Figures 4A–C show the metanalysis for the several biochemical markers herein used to assess the kidney function of the diabetic animals treated with R. officinalis or vehicle. The data of 4 studies (n = 48) were pooled and indicate that R. officinalis significantly decreased both BUN (MD = −24.84 [95% CI; −34.78, −14.90]; I2 = 93%) and CRE (MD = −0.40 [95% CI; –0.74, −0.06]; I2 = 98%) levels compared to vehicle control groups. However, the data of these same studies were pooled and indicate that R. officinalis did not significantly reduce AUR (MD = −0.43 [95% CI; −2.05, + 1.19]; I2 = 100%) level in comparison to the vehicle control group.
Improving the lipid profile
Figure 5A indicates that there was a significant lowering in LDL-c level of diabetic animals receiving R. officinalis compared to the vehicle control group (3 studies, n = 38; MD = −11.74 [95% CI; −21.27, −2.21]; I2 = 92%). Nor the HDL (3 studies, n = 38; MD = + 3.66 [95% CI; −1.89, + 9.20]; I2 = 93%), neither the TC (4 studies, n = 52; MD = −27.18 [95% CI; −60.21, + 5.86]; I2 = 99%) or Tg (4 studies, n = 52; MD = −18.52 [95% CI; −37.96, + 0.93]; I2 = 97%) serum levels were significantly affected following the treatments with R. officinalis in comparison to vehicle control groups (Fig. 5B–D, respectively).
Subgroup analysis
The subgroup analyses for FPG enabled us to compare the results for the exposure time and type of extracts. As shown in Fig. S2, there was a subgroup effect statistically significant (p < 0.00001; I2 = 79.3%), i.e., the exposure time and/or the extract type impact the antihyperglycemic effect of R. officinalis.
Based on this analysis it’s possible to assert that either the volatile oil (2 studies, n = 24; MD = −18.20 [95% CI; −188.89, + 152.50]; I2 = 98%) or the acute exposure (2 studies, n = 26; MD = −19.45 [95% CI; −195.76, + 156.86]; I2 = 97%) do not yield significant outcomes in decreasing the FPG.
Concerning the SIL, it was possible to compare the results for the type of extract and animal strain whether rabbits or rats. The results of the subgroup analyses are presented in Fig. S3. The test for subgroup differences indicated that there was a significant subgroup effect statistically (p < 0.00001; I2 = 96.6%) so that both extract type and animal strain significantly impact the efficacy of R. officinalis in increasing the release of insulin when compared to vehicle control.
The treatment effect favored R. officinalis over vehicle control for all animal strains and extract types; which suggests that the subgroup effect is quantitative. Both FPG and SIL heterogeneity between results in studies within sub-groups requires further exploration.
Risk of bias and methodological quality
Figure 6A displays the summary of the results concerning the bias risk assessment according to the SYRCLE tool for controlled preclinical trials herein included. The results reveal that all studies did not perform allocation concealment, blinding of outcome assessment, and blinding of evaluation of random results. In addition, an important risk of bias was verified by checking whether there was a pancreatectomy to assess outcome bias or indicating that there was no pancreatic beta regeneration not attributed to R. officinalis exposure.
Complementarily, Fig. 6B reports the methodological quality evaluated by the CAMARADES checklist for the pre-clinical studies included. The quality score of the majority of studies in this analysis was in mean, 5.3 ± 1.0, indicating an average methodological quality. All 23 studies reported statements of compliance with regulatory requirements and the use of animals with hypertension or diabetes.
However, none of these studies described the blinded assessment of outcome and sample size calculation, and 15 studies did not report how the animals used in the study were euthanized (avoidance of anesthetics with marked intrinsic properties).
Discussion
The efficacy and safety of R. officinalis
To the best of our knowledge, this is the first systematic review and meta-analysis shedding light on the antihyperglycemic, hepatoprotective, nephroprotective, and antihyperlipidemic effects of R. officinalis extracts in preclinical experimental models of T1DM. Our meta-analysis confirmed the beneficial effect of this nutraceutical in reducing FPG besides kidney and hepatic injury markers; in decreasing the LDL-c and increasing SIL in animals.
The reduction in the FPG of the diabetic animals treated with the different R. officinalis extracts is outstanding and, on average, greater than that observed with Momordica charantia L. (n = 815; SMD = −6.86 [95% CI; −7.95, −5.77]; I2 = 90%), which is a nutraceutical widely consumed in Asia and Africa as adjuvant in the management of DM (Peter et al. 2021). Moreover, R. officinalis displays a more appreciable antihyperglycemic effect when compared to the Brazilian superfruit Eugenia uniflora (n = 36; MD = −49.97 [95% CI; −57.18, −42.75]; I2 = 67%) (Máximo et al. 2022) and to the medicinal plant Moringa oleifera (n = 699; MD = −3.92, [95% CI; − 4.65, − 3.19; I2 = 90.15%) (Watanabe et al. 2021).
It’s important to consider that in all studies herein included, the treatment with R. officinalis was not able to reduce the FPG to normal levels, i.e., < 100 mg/dL (Elsayed et al. 2023). Therefore, using R. officinalis does not ensure controlling the hyperglycemia by itself but may be helpful to enhance the hypoglycemic effects achieved with insulin administration. In turn, decreasing the dose of insulin or its administration frequency can increase patient compliance and adherence to the treatment, and reduce the adverse effects often associated with insulin administration errors.
The chance of herb-drug interactions following the long-term intake of R. officinalis with either insulin or oral hypoglycemic drug administration is to be taken into account because this may exacerbate the hypoglycemic effect. On one hand, it would be beneficial when envisioning the deprescribing of oral hypoglycemic drugs and decreasing their major side effects such as vomiting, flatulence, and diarrhea, which impair the patient’s adherence to the treatment (Ghadge and Kuvalekar 2017). On the other hand, it could provoke hypoglycemia (FPG < 70 mg/dL) which brings several undesired symptoms to patients (e.g., shakiness, sweating, fatigue, difficulty concentrating, etc.) (Nakhleh and Shehadeh 2021).
Still, in the wake of this food or herb-drug interaction scenario, it has been witnessed in the literature that the rosmarinic acid, the major phytochemical comprising R. officinalis acts in vitro as a weak or moderate inhibitor (even mixed or competitive mechanisms) of some human cytochrome P450 monooxygenases (CYP2C19 and CYP2E1) and, mainly, uridine diphosphate glucuronosyltransferases (UGT1A1/1A6/2B7) isoforms (Kim et al. 2019). This last group of enzymes is needful for the hepatic metabolism of some antidiabetic drugs such as canagliflozin and troglitazone (Zhou et al. 2016), besides antitumoral (etoposide and SN-38), antilipidemic (ezetimibe) and non-steroidal anti-inflammatory (acetaminophen, diclofenac, and naproxen) drugs (Kim et al. 2019).
These concerns are of utmost importance because diabetic patients can be up to two-fold more susceptible to using oral anti-diabetic agents associated with medicinal plants (Chelghoum et al. 2021). Therefore, the use of R. officinalis in association with other pharmaceutical drugs in the management of DM must be closely accompanied by a multidisciplinary healthcare professional team.
The overall mechanisms of action behind the antihyperglycemic effect of R. officinalis are not yet fully understood, but it has been suggested that the increment in insulin secretion somehow plays a key role in lowering the FPG (Bao et al. 2020). This is because an increased insulin level can help to the lowering of glucose levels by promoting glucose uptake and storage in the cells, then, inhibiting glucose production in the liver, and stimulating glycogen synthesis while inhibiting glycogenolysis (Rahman et al. 2021).
For clarification sake of this hypothesis, herein we plotted the MD obtained for SIL versus the respective MD of FPG arising from our meta-analyses (Figs. 2A and 3, respectively). There was a very low correlation between the increment of SIL and the decrement of FPG (R2 = 0.027, data not shown), thus further investigations with a greater number of studies are still required to ratify or refute this.
Non-alcoholic fatty liver disease and chronic kidney disease, which are metabolic conditions putatively interdependent, are often reported as DM complications (Byrne and Targher 2020). In a study included in the meta-analysis regarding the biochemical markers of hepatic damage related to DM (Selmi et al. 2017), the administration of R. officinalis lowered the ALT and AST serum levels to normal values, i.e., < 40 U/L (Kim et al. 2004).
Even though all the treatment effects favored R. officinalis over vehicle control in the meta-analysis of BUN, the decrement observed for this parameter associated with kidney injury did not reach normal levels, i.e., 5 ≤ BUN ≤ 20 mg/dL (Hosten 1990). Nonetheless, in the group treatment with R. officinalis the CRE blood levels have been lowered to the normal ranges, which are 0.7–1.3 mg/dL for adult males and 0.6–1.2 mg/dL for adult females (Hosten 1990). Therefore, R. officinalis may promote hepatoprotection more markedly than nephroprotective effects in DM.
The hepatoprotective effects of R. officinalis have been confirmed by several in vitro and in vivo investigations irrespective of the method used to induce liver damage (Amin and Hamza 2005; Guimarães et al. 2023; Hegazy et al. 2018; Ielciu et al. 2021; Mohamed et al. 2022; Rašković et al. 2014). The lipid alterations that occur in DM, such as the increment of the LDL-c, are related to cardiovascular diseases, one of the main causes of mortality and morbidity in people with DM (Cole and Florez 2020).
Among the hypotheses related to these alterations, we have the high formation of advanced glycation end products and the increment in reactive oxygen species that are favored by hyperglycemia (Méndez et al. 2010). This process can lead to the accumulation of oxidized lipids, which can contribute to the development of lipid metabolism disorders and the progression of related diseases. Furthermore, a study published by Jiang et al. 2020, suggested that oxidative stress-induced lipid peroxidation can contribute to the development of insulin resistance, which is a key feature of DM.
Thence, besides the other benefits aforementioned, R. officinalis may reduce cardiovascular risk to a certain extent by decreasing the serum LDL-c level and avoiding the fatty deposits assembled in the arteries.
The role of OS in the pathogenesis of DM is extensively revised elsewhere (Darenskaya et al. 2021). Since R. officinalis is an outstanding source of antioxidants (Andrade et al. 2018; Celiktas et al. 2007; Gonçalves et al. 2011; Sánchez-Camargo and Herrero 2017; Takayama et al. 2022), several studies herein included assessed in vivo antioxidant activity of the tested extracts (Bakirel et al. 2008; El-Boshy et al. 2015; Emam 2012; Khalil et al. 2012; Mohamed 2021; Nazem et al. 2015; Sebai et al. 2015; Selmi et al. 2017; Shen et al. 2020; Silva et al. 2011; Wahba 2022). However, the methods used by the authors in pursuit of this and the antioxidant outcomes varied widely. For this reason, it was not possible neither to perform metanalysis nor to correlate the in vivo biochemical markers of antioxidant activities with the preventive effect in DM.
Noteworthy, none of the preclinical studies included in this systematic review reported any adverse effects, mortality, or behavioral changes in the tested animals that were attributed to R. officinalis exposure. These findings hint that R. officinalis is safe in all of the tested doses (25–800 mg/kg for extracts and 0.5% to 10% for leaves powder). Indeed, the European Food Safety Authority has classified R. officinalis extracts as a Generally Recognized as Safe (GRAS) food (CFR182.10; 182.20)(Aguilar et al. 2008), not showing high levels of toxicity at therapeutic doses.
Study limitations
Some studies evaluated in this work reported having assessed FPG in diabetic animals but did not demonstrate the raw results in the tables or figures (Belmouhoub et al. 2016, 2017, 2020; Ramadan et al. 2013). Hence, as we did not receive any answer about these raw data from the authors, it was not possible to include them in our meta-analysis.
Regarding the experimental design of the included articles, a large number of studies included only male rats in their experimental protocols, and it was not possible to compare the effects between males and females.
We also point out the lack of standardization when reporting the dose of extract administered to the animals. One study did not report the weight of the animals or the concentration of extract administered (Al-badry 2017), so it was not possible to define the dose administered (mg/Kg).
Many articles did not inform how the sample size calculation, housing, allocation, and blinding were carried out, thus revealing a high risk of bias for these domains and impairing the internal validity of these investigations. This trend is not an exclusivity of our findings, since it has been very often reported in systematic reviews and meta-analyses dealing with preclinical trials in animals (Gupta 2019; Máximo et al. 2022; Mignini and Khan 2006; Peter et al. 2021; Rostamkhani et al. 2022; Shojaei-Zarghani et al. 2022).
Furthermore, a scanty number of studies assessing the HbA1c levels in the animals was included, and R. officinalis displayed no appreciable impact in this parameter, which represents an index of average glucose and is considered the gold standard for monitoring the patient’s glucose control over time (Sherwani et al. 2016). This inefficacy is likely related to the short-lasting of the studies assessing this biochemical marker., i.e., much lower than 90 days (the average time required for erythrocyte turnover). which might have been insufficient to adequately capture such effects.
The meta-analysis of animal studies has been considered a valuable statistical toolset for improving healthcare since it can be further used to generate new hypotheses and guide the design of clinical trials in humans (Hooijmans et al. 2014a; Sauvant et al. 2020).
The high heterogeneity displayed in our meta-analysis is likely attributed to the various methodological design aspects of the included articles, e.g., variability related to the animals used (strains, age, etc.), small sample sizes, different drugs administrated to induce DM and their doses, diverse intervention features (plant origin, harvesting time, solvents and procedures used to prepare the extract, route of administration, doses administrated, and treatment period), distinct outcome measurement methods, etc. This is also a recurrent trend for animal studies, that can restrict but not prevent the animal-to-human translation of findings arising from systematic reviews and meta-analyses (Bahadoran et al. 2020).
Finally, a few articles reported the accurate quantitative phytochemical analysis of the extracts administered in the animals (Rasoulian et al. 2019; Sebai et al. 2015; Shen et al. 2020), thereby revealing warning analytical standardization issues. Although displaying a great challenge, the standardization of herbal extracts plays a key role throughout the rationale development of phytopharmaceuticals once it is required for i) assessing the seasonal and batch-to-batch variability to assure consistent chemical profile; ii) identifying and controlling critical processing parameters such as extraction, drying, transportation and storage; iii) establishing the major active compounds involved in the biological activities and their putative mechanisms of action; and iv) enabling to achieve improved and reproducible treatment outcomes (Alamgir 2017).
Conclusions
The administration of R. officinalis derivatives dwindles the FPG besides hepatic damage in diabetic animals, thence this nutraceutical may help in the management of DM and some of its complications. The pre-clinical trials herein analyzed display relevant issues concerning the risk of bias and methodological quality. Therefore, although plausible, so far, it’s not possible to draw a solid conclusion regarding the efficacy of this nutraceutical as an alternative in the primary care of DM.
Patients and healthcare professionals would greatly benefit from further high methodological quality studies, especially controlled randomized clinical trials performed with accurately standardized extracts and assessing HbA1c as a primary outcome.
Abbreviations
- Alb:
-
Albumin
- ALP:
-
Alkaline phosphatase
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- AUR:
-
Uric acid
- BUN:
-
Blood urea nitrogen
- CAMARADES:
-
Collaborative Approach to Meta Analysis and Review of Animal Experimental Studies
- CI:
-
Confidence interval
- CRE:
-
Creatinine
- D.O.I:
-
Digital Object Identifier System
- DeCS:
-
Health Sciences Descriptors
- DM:
-
Diabetes mellitus
- FPG:
-
Fasting plasma glucose
- HbA1c:
-
Serum glycated hemoglobin
- HDL-c:
-
High density lipoprotein cholesterol
- LDL-c:
-
Low density lipoprotein cholesterol
- MD:
-
Mean difference
- MeSH:
-
Medical Subject Headings
- OS:
-
Oxidative stress
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RevMan:
-
Review Manager software
- ROs:
-
Reactive oxygen species
- SD:
-
Standard deviation
- SIL:
-
Serum insulin level
- SYRCLE:
-
Systematic Review Center for Laboratory animal Experimentation
- T1DM:
-
Type-1 diabetes mellitus
- T2DM:
-
Type-2 diabetes mellitus
- TC:
-
Total cholesterol
- Tg:
-
Total triglycerides
- VHL:
-
Virtual Health Library
References
Aguilar F, Autrup H, Barlow S, Castle L, Crebelli R, Engel K, Gontard N, Gott D, Grilli S, Gürtler R, Larsen C, Leclercq C, Leblanc J, Malcata FX, Mennes W, Milana MR, Pratt I, Rietjens I, Tobback P, Toldrá F (2008) Scientific opinion of the panel on food additives, flavourings, processing aids and materials in contact with food. EFSA J 721:1–29
Alamgir ANM (2017) Herbal drugs: their collection, preservation, and preparation; evaluation, quality control, and standardization of herbal drugs BT – therapeutic use of medicinal plants and their extracts: volume 1: pharmacognosy. In: Alamgir ANM (ed) Therapeutic use of medicinal plants and their extracts: volume 1. Springer International Publishing, pp 453–495. https://doi.org/10.1007/978-3-319-63862-1_10
Al-badry FAM (2017) Effect of aqueous extract of Rosmarinus officinalis on kidney and liver of male rats experimentally infected with diabetic. J Coll Educ Pure Sci 7(3):171–186
Al-Hader AA, Hasan ZA, Aqel MB (1994) Hyperglycemic and insulin release inhibitory effects of Rosmarinus officinalis. J Ethnopharmacol 43(3):217–221. https://doi.org/10.1016/0378-8741(94)90046-9
Alhujaily M, Dhifi W, Mnif W (2022) An overview of the potential of medicinal plants used in the development of nutraceuticals for the management of diabetes mellitus: proposed biological mechanisms. Processes 10(10). https://doi.org/10.3390/pr10102044
Almutlaq N, Neyman A, Dimeglio LA (2021) Are diabetes microvascular complications risk factors for fragility fracture? In: Current opinion in endocrinology, diabetes and obesity, vol 28, Issue 4, pp 354–359. https://doi.org/10.1097/MED.0000000000000642
Alnahdi HS (2012) Effect of Rosmarinus officinalis extract on some cardiac enzymes of streptozotocin-induced diabetic rats. Int J Health Sci 2(4):33–37. https://doi.org/10.5923/j.health.20120204.03
Amin A, Hamza AA (2005) Hepatoprotective effects of Hibiscus, Rosmarinus and Salvia on azathioprine-induced toxicity in rats. Life Sci 77(3):266–278. https://doi.org/10.1016/j.lfs.2004.09.048
Andrade JM, Faustino C, Garcia C, Ladeiras D, Reis CP, Rijo P (2018) Rosmarinus officinalis L.: an update review of its phytochemistry and biological activity. Future Sci OA 4(4). https://doi.org/10.4155/fsoa-2017-0124
Ayaz NO (2012) Antidiabetic and renoprotective effects of water extract of Rosmarinus officinalis in streptozotocin-induced diabetic rat. Afr J Pharm Pharmacol 6(37):2664–2669. https://doi.org/10.5897/AJPP12.319
Bahadoran Z, Mirmiran P, Kashfi K, Ghasemi A (2020) Importance of systematic reviews and meta-analyses of animal studies: challenges for animal-to-human translation. J Am Assoc Lab Anim Sci 59(5), 469–477. https://doi.org/10.30802/AALAS-JAALAS-19-000139
Bahor Z, Liao J, Currie G, Ayder C, MacLeod M, McCann SK, Bannach-Brown A, Wever K, Soliman N, Wang Q, Doran-Constant L, Young L, Sena ES, Sena C (2021) Development and uptake of an online systematic review platform: the early years of the CAMARADES Systematic Review Facility (SyRF). BMJ Open Science 5(1):1–10. https://doi.org/10.1136/bmjos-2020-100103
Bakirel T, Bakirel U, Keleş OU, Ulgen SG, Yardibi H (2008) In vivo assessment of antidiabetic and antioxidant activities of rosemary (Rosmarinus officinalis) in alloxan-diabetic rabbits. J Ethnopharmacol 116(1):64–73. https://doi.org/10.1016/j.jep.2007.10.039
Bao TQ, Li Y, Qu C, Zheng ZG, Yang H, Li P (2020) Antidiabetic effects and mechanisms of rosemary (Rosmarinus officinalis L.) and its phenolic components. Am J Chin Med 48(6):1353–1368. https://doi.org/10.1142/S0192415X20500664
Belmouhoub M, Bribi N, Iguer-ouada M (2016) Alpha-glucosidase inhibition and antihyperglycemic activity of flavonoids rich fractions of Rosmarinus officinalis in normal and streptozotocin diabetic mice. Orient Pharm Exp Med 17(1):29–39. https://doi.org/10.1007/s13596-016-0252-8
Belmouhoub M, Khellouf A, Ouatah Z, Belkacem O, Djermoune S, Khanouche S, Iguer-Ouad M (2020) Protective effect of Rosmarinus officinalis flavonoids rich fractions against testicular and reproductive dysfunction in streptozotocin-induced diabetic mice. Asian J Biol Sci 13(2):194–200. https://doi.org/10.3923/ajbs.2020.194.200
Belmouhoub M, Chebout I, Iguer-ouada M (2017) Antidiabetic and anti-hypercholesterolemic effects of flavonoid-rich fractions of Rosmarinus officinalis in streptozotocin-induced diabetes in mice. Phytothérapie Dm 1–7. https://doi.org/10.1007/s10298-017-1103-6
Benkhedir A, Boussekine S, Saker H, Gasmi S, Benali Y (2022) Beneficial effects of Rosmarinus officinalis and Thymus numidicus on key enzymes of carbohydrate metabolism in alloxan-induced diabetic rats. J Microbiol Biotechnol Food Sci 12(4):1–8. https://doi.org/10.55251/jmbfs.9507
Bjornstad P, Drews K, Caprio S, Gubitosi-Klug R, Nathan D, Tesfaldet B, Tryggestad J, White N, Zeitler P (2022) Long-term complications in youth-onset type 2 diabetes. Yearb Paediatr Endocrinol 385(5):416–426. https://doi.org/10.1530/ey.19.12.3
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR (2010) A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods 1(2):97–111. https://doi.org/10.1002/jrsm.12
Buzzetti R, Tuomi T, Mauricio D, Pietropaolo M, Zhou Z, Pozzilli P, Leslie RD (2020) Management of latent autoimmune diabetes in adults: a consensus statement from an international expert panel. Diabetes 69(10):2037–2047. https://doi.org/10.2337/dbi20-0017
Byrne CD, Targher G (2020) NAFLD as a driver of chronic kidney disease. J Hepatol 72(4):785–801. https://doi.org/10.1016/j.jhep.2020.01.013
Capatina L, Boiangiu RS, Dumitru G, Napoli EM, Ruberto G, Hritcu L, Todirascu-Ciornea E (2020) Rosmarinus officinalis essential oil improves scopolamine-induced neurobehavioral changes via restoration of cholinergic function and brain antioxidant status in Zebrafish (Danio rerio). Antioxidants 9(1):62. https://doi.org/10.3390/antiox9010062
Celiktas O, Bedir E, Sukan F (2007) In vitro antioxidant activities of Rosmarinus officinalis extracts treated with supercritical carbon dioxide. Food Chem 101(4):1457–1464. https://doi.org/10.1016/j.foodchem.2006.03.055
Chelghoum M, Khitri W, Bouzid S, Lakermi AR (2021) New trends in the use of medicinal plants by Algerian diabetic patients, considerations of herb-drug interactions. Journal of Ethnopharmacology 274(November 2020):113984. https://doi.org/10.1016/j.jep.2021.113984
Cole JB, Florez JC (2020) Genetics of diabetes mellitus and diabetes complications. Nat Rev Nephrol 16(7):377–390. https://doi.org/10.1038/s41581-020-0278-5
Darenskaya MA, Kolesnikova LI, Kolesnikov SI (2021) Oxidative stress: pathogenetic role in diabetes mellitus and its complications and therapeutic approaches to correction. In: Bulletin of experimental biology and medicine, vol 171, Issue 2, pp 179–189. https://doi.org/10.1007/s10517-021-05191-7
Dehdashtian E, Pourhanifeh MH, Hemati K, Mehrzadi S, Hosseinzadeh A (2020) Therapeutic application of nutraceuticals in diabetic nephropathy: Current evidence and future implications. Diabetes Metab Res Rev 36(8):1–21. https://doi.org/10.1002/dmrr.3336
Derosa G, D’Angelo A, Maffioli P (2022) The role of selected nutraceuticals in management of prediabetes and diabetes: an updated review of the literature. Phytother Res 36(10):3709–3765. https://doi.org/10.1002/ptr.7564
El-Boshy M, Header E, ElSawy N, Basalamah M, Mubarak M, Hadda T (2015) Studies on the constituents of Rosmarinus officinalis and Their synergistic effect in experimental diabetic rats. J Invest Biochem 4(1):36. https://doi.org/10.5455/jib.20150519104925
Elsayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, Collins BS, Hilliard ME, Isaacs D, Johnson EL, Kahan S, Khunti K, Kosiborod M, Leon J, Lyons SK, Murdock L, Perry M. Lou, Prahalad P, Pratley RE et al (2023) 2. Classification and diagnosis of diabetes: standards of care in diabetes—2023. Diabetes Care 46(Supplement_1):S19–S40. https://doi.org/10.2337/dc23-S002
Emam M (2012) Comparative evaluation of antidiabetic activity of Rosmarinus officinalis L. and Chamomile recutita in streptozotocin induced diabetic rats. Agric Biol J North Am 3(6):247–252. https://doi.org/10.5251/abjna.2012.3.6.247.252
Erenmemisoglu A, Saraymen R, Ustun S (1997) Effect of a Rosmarinus officinalis leave extract on plasma glucose levels in normoglycaemic and diabetic mice. Pharmazie 52(8):645–646
Ghadge AA, Kuvalekar AA (2017) Controversy of oral hypoglycemic agents in type 2 diabetes mellitus: novel move towards combination therapies. Diabetes Metab Syndr 11:S5–S13. https://doi.org/10.1016/j.dsx.2016.08.009
Giacco F, Brownlee M (2010) Oxidative stress and diabetic complications. Circ Res 107(9):1058–1070. https://doi.org/10.1161/CIRCRESAHA.110.223545
Gonçalves D, Couto RO, Conceição EC, Reis NS, Gil ES (2011) Voltametria de pulso diferencial (VPD) em estado sólido de manchas de cromatografia de camada delgada (CCD): UM novo método de análise para fitoativos antioxidantes. Quim Nova 34(2):330–334. https://doi.org/10.1590/S0100-40422011000200028
Gonçalves C, Fernandes D, Silva I, Mateus V (2022) Potential anti-inflammatory effect of Rosmarinus officinalis in preclinical in vivo models of inflammation. Molecules 27(3):609. https://doi.org/10.3390/molecules27030609
Guimarães NSS, Ramos VS, Prado-Souza LFL, Lopes RM, Arini GS, Feitosa LGP, Silva RR, Nantes IL, Damasceno DC, Lopes NP, Rodrigues T (2023) Rosemary (Rosmarinus officinalis L.) glycolic extract protects liver mitochondria from oxidative damage and prevents acetaminophen-induced hepatotoxicity. Antioxidants 12(3):628. https://doi.org/10.3390/antiox12030628
Gupta SK (2019) A study to assess the methodological quality of in vivo animal experiments published in Indian Journal of Pharmacology: a retrospective, cross-sectional, observational study. Indian J Pharmacol 51(1):11–16. https://doi.org/10.4103/ijp.IJP_536_18
Hassani FV, Shirani K, Hosseinzadeh H (2016) Rosemary (Rosmarinus officinalis) as a potential therapeutic plant in metabolic syndrome: a review. Naunyn-Schmiedeberg’s Arch Pharmacol 389(9):931–949. https://doi.org/10.1007/s00210-016-1256-0
Hegazy AM, Abdel-Azeem AS, Zeidan HM, Ibrahim KS, El-Sayed EM (2018) Hypolipidemic and hepatoprotective activities of rosemary and thyme in gentamicin-treated rats. Hum Exp Toxicol 37(4):420–430. https://doi.org/10.1177/0960327117710534
Hooijmans CR, IntHout J, Ritskes-Hoitinga M, Rovers MM (2014a) Meta-analyses of animal studies: An introduction of a valuable instrument to further improve healthcare. ILAR J 55(3):418–426. https://doi.org/10.1093/ilar/ilu042
Hooijmans CR, Maroeska MR, de Vries RB, Leenaars M, Ritskes-Hoitinga M, Langendam MW (2014b) SYRCLE’s risk of bias tool for animal studies. Chin J Evid Based Med 14(10):1281–1285. https://doi.org/10.7507/1672-2531.20140206
Hosten AO (1990) BUN and creatinine. In: Walker H, Hall W, Hurst J (eds) Clinical methods: the history, physical, and laboratory examinations, 3rd ed. Butterworths, pp 874–878. https://doi.org/10.7326/0003-4819-113-7-563_2
Ielciu I, Sevastre B, Olah NK, Turdean A, Chișe E, Marica R, Oniga I, Uifălean A, Sevastre-Berghian AC, Niculae M, Benedec D, Hanganu D (2021) Evaluation of hepatoprotective activity and oxidative stress reduction of rosmarinus officinalis l. Shoots tincture in rats with experimentally induced hepatotoxicity. Molecules 26(6):1737. https://doi.org/10.3390/molecules26061737
International Diabetes Federation (2021) International Diabetes Federation. IDF Diabetes Atlas. https://doi.org/10.1016/j.diabres.2013.10.013
Jiang S, Young JL, Wang K, Qian Y, Cai L (2020) Diabetic-induced alterations in hepatic glucose and lipid metabolism: the role of type 1 and type 2 diabetes mellitus (Review). Mol Med Rep 22(2):603–611. https://doi.org/10.3892/mmr.2020.11175
Khalil OA, Ramadan KS, Danial EN, Alnahdi HS, Ayaz NO (2012) Antidiabetic activity of Rosmarinus officinalis and its relationship with the antioxidant property. Afr J Pharm Pharmacol 6(14):1031–1036. https://doi.org/10.5897/ajpp12.162
Kim HC, Nam CM, Jee SH, Han KH, Oh DK, Suh I (2004) Normal serum aminotransferase concentration and risk of mortality from liver diseases: prospective cohort study. BMJ 328(7446):983–986. https://doi.org/10.1136/bmj.38050.593634.63
Kim SB, Kim KS, Kim DD, Yoon IS (2019) Metabolic interactions of rosmarinic acid with human cytochrome P450 monooxygenases and uridine diphosphate glucuronosyltransferases. Biomed Pharmacother 110(May 2018):111–117. https://doi.org/10.1016/j.biopha.2018.11.040
King AJF (2012) The use of animal models in diabetes research. Br J Pharmacol 166(3):877–894. https://doi.org/10.1111/j.1476-5381.2012.01911.x
Koga K, Shibata H, Yoshino K, Nomoto K (2006) Effects of 50% ethanol extract from rosemary (Rosmarinus officinalis) on α-glucosidase inhibitory activity and the elevation of plasma glucose level in rats, and its active compound. J Food Sci 71(7). https://doi.org/10.1111/j.1750-3841.2006.00125.x
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159–174
Malek AM, Sadaka MW, Hamo S, Al-Mahbashi HM (2020) Evaluation of antidiabetic activity of Rosmarinus officinalis var. prostratus growing in Syria in alloxan diabetic rats. Curr Bioact Comp 17(2):187–193. https://doi.org/10.2174/1573407216999200426235739
Máximo AS, do Couto RO, Domingueti CP (2022) Employment of Eugenia uniflora in glycemic control and prevention of diabetes mellitus complications: a systematic review and meta-analysis. Revista Brasileira de Plantas Medicinais 24(2):99–111
Méndez JD, Xie J, Aguilar-Hernández M, Méndez-Valenzuela V (2010) Trends in advanced glycation end products research in diabetes mellitus and its complications. Mol Cell Biochem 341(1–2):33–41. https://doi.org/10.1007/s11010-010-0434-5
Mignini LE, Khan KS (2006) Methodological quality of systematic reviews of animal studies: a survey of reviews of basic research. BMC Med Res Methodol 6(September). https://doi.org/10.1186/1471-2288-6-10
Mohamed SS (2021) Effects of Rosmarinus officinalis and/or Ocimum basilicum supplementation on induced diabetes in adult male albino rats. Al-Azhar Med J 50(4):2915–2926. https://doi.org/10.21608/amj.2021.201565
Mohamed ME, Younis NS, El-Beltagi HS, Mohafez OM (2022) The synergistic hepatoprotective activity of rosemary essential oil and curcumin: the role of the MEK/ERK pathway. Molecules 27(24):1–18. https://doi.org/10.3390/molecules27248910
Naimi M, Vlavcheski F, Shamshoum H, Tsiani E (2017) Rosemary extract as a potential anti-hyperglycemic agent: current evidence and future perspectives. Nutrients 9(9):1–19. https://doi.org/10.3390/nu9090968
Nakhleh A, Shehadeh N (2021) Hypoglycemia in diabetes: An update on pathophysiology, treatment, and prevention. World J Diabetes 12(12):2036–2049. https://doi.org/10.4239/wjd.v12.i12.2036
Nazem F, Farhangi N, Neshat-Gharamaleki M (2015) Beneficial effects of endurance exercise with Rosmarinus officinalis labiatae leaves extract on blood antioxidant enzyme activities and lipid peroxidation in streptozotocin-induced diabetic rats. Can J Diabetes 39(3):229–234. https://doi.org/10.1016/j.jcjd.2014.11.003
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan–-a web and mobile app for systematic reviews. Syst Rev 5(1):210. https://doi.org/10.1186/s13643-016-0384-4
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (Clinical Research Ed.) 372:n71. https://doi.org/10.1136/bmj.n71
Pérez-Sánchez A, Barrajón-Catalán E, Ruiz-Torres V, Agulló-Chazarra L, Herranz-López M, Valdés A, Cifuentes A, Micol V (2019) Rosemary (Rosmarinus officinalis) extract causes ROS-induced necrotic cell death and inhibits tumor growth in vivo. Sci Rep 9(1):1–11. https://doi.org/10.1038/s41598-018-37173-7
Peter EL, Nagendrappa PB, Kaligirwa A, Ogwang PE, Sesaazi CD (2021) The safety and efficacy of Momordica charantia L. in animal models of type 2 diabetes mellitus: A systematic review and meta-analysis. Phytother Res 35(2):637–656. https://doi.org/10.1002/ptr.6853
Rahman MS, Hossain KS, Das S, Kundu S, Adegoke EO, Rahman MA, Hannan MA, Uddin MJ, Pang M-G (2021) Role of insulin in health and disease: an update. Int J Mol Sci 22(12):6403. https://doi.org/10.3390/ijms22126403
Ramadan KS, Khalil OA, Danial EN, Alnahdi HS, Ayaz NO (2013) Hypoglycemic and hepatoprotective activity of Rosmarinus officinalis extract in diabetic rats. J Physiol Biochem 69(4):779–783. https://doi.org/10.1007/s13105-013-0253-8
Rašković A, Milanović I, Pavlović N, Ćebović T, Vukmirović S, Mikov M (2014) Antioxidant activity of rosemary (Rosmarinus officinalis L.) essential oil and its hepatoprotective potential. BMC Complement Altern Med 14(225) https://doi.org/10.1186/1472-6882-14-225.
Rasoulian B, Hajializadeh Z, Esmaeili-Mahani S, Rashidipour M, Fatemi I, Kaeidi A (2019) Neuroprotective and antinociceptive effects of rosemary (Rosmarinus officinalis L.) extract in rats with painful diabetic neuropathy. J Physiol Sci 69(1):57–64. https://doi.org/10.1007/s12576-018-0620-x
Reis JS, Veloso CA, Mattos RT, Purish S, Nogueira-Machado JA (2021) Oxidative stress: a review on metabolic signaling in type 1 diabetes. Arq Bras Endocrinol Metabol 52(7):1096–1105. https://doi.org/10.1590/s0004-27302008000700005
Rivera D, Allkin R, Obón C, Alcaraz F, Verpoorte R, Heinrich M (2014) What is in a name? The need for accurate scientific nomenclature for plants. J Ethnopharmacol 152(3):393–402. https://doi.org/10.1016/j.jep.2013.12.022
Rostamkhani H, Faghfouri AH, Veisi P, Rahmani A, Noshadi N, Ghoreishi Z (2022) The protective antioxidant activity of ginger extracts (Zingiber Officinale) in acute kidney injury: a systematic review and meta-analysis of animal studies. J Funct Foods 94(April):105111. https://doi.org/10.1016/j.jff.2022.105111
Sánchez-Camargo AdP, Herrero M (2017) Rosemary (Rosmarinus officinalis) as a functional ingredient: recent scientific evidence. Curr Opin Food Sci 14:13–19. https://doi.org/10.1016/j.cofs.2016.12.003
Sauvant D, Letourneau-Montminy MP, Schmidely P, Boval M, Loncke C, Daniel JB (2020) Review: use and misuse of meta-analysis in animal science. Animal 14:s207–s222. https://doi.org/10.1017/S1751731120001688
Sebai H, Selmi S, Rtibi K, Gharbi N, Sakly M (2015) Protective effect of Lavandula stoechas and Rosmarinus officinalis essential oils against reproductive damage and oxidative stress in alloxan-induced diabetic rats. J Med Food 18(2):241–249. https://doi.org/10.1089/jmf.2014.0040
Selmi S, Rtibi K, Grami D, Sebai H, Marzouki L (2017) Rosemary (Rosmarinus officinalis) essential oil components exhibit anti-hyperglycemic, anti-hyperlipidemic and antioxidant effects in experimental diabetes. Pathophysiology 24(4):297–303. https://doi.org/10.1016/j.pathophys.2017.08.002
Shen Y, Han J, Zheng X, Ai B, Yang Y, Xiao D, Zheng L, Sheng Z (2020) Rosemary leaf extract inhibits glycation, breast cancer proliferation, and diabetes risks. Appl Sci (Switzerland) 10(7):2248. https://doi.org/10.3390/app10072249
Sherwani SI, Khan HA, Ekhzaimy A, Masood A, Sakharkar MK (2016) Significance of HbA1c test in diagnosis and prognosis of diabetic patients. Biomark Insights 11:95–104. https://doi.org/10.4137/Bmi.s38440
Shi J, Hu H, Harnett J, Zheng X, Liang Z, Wang YT, Ung COL (2019) An evaluation of randomized controlled trials on nutraceuticals containing traditional Chinese medicines for diabetes management: a systematic review. Chin Med (united Kingdom) 14(1):1–20. https://doi.org/10.1186/s13020-019-0276-3
Shojaei-Zarghani S, Fattahi MR, Kazemi A, Safarpour AR (2022) Effects of garlic and its major bioactive components on non-alcoholic fatty liver disease: a systematic review and meta-analysis of animal studies. J Funct Foods 96(August):105206. https://doi.org/10.1016/j.jff.2022.105206
Shrestha P, Ghimire L (2012) A review about the effect of life style modification on diabetes and quality of life. Global J Health Sci 4(6):185–190. https://doi.org/10.5539/gjhs.v4n6p185
Silva AM, de Andrade-Wartha ERS, de Carvalho EBT, de Lima A, Novoa AV, Mancini-Filho J (2011) Efeito do extrato aquoso de alecrim (Rosmarinus officinalis L.) sobre o estresse oxidativo em ratos diabéticos. Rev Nutr 24(1):121–130. https://doi.org/10.1590/S1415-52732011000100012
de Souza Stork S, Hübner M, Biehl E, Danielski LG, Bonfante S, Joaquim L, Denicol T, Cidreira T, Pacheco A, Bagio E, Lanzzarin E, Bernades G, de Oliveira MP, da Silva LE, Mack JM, Bobinski F, Rezin GT, Barichello T, Streck EL, Petronilho F (2022) Diabetes exacerbates sepsis-induced neuroinflammation and brain mitochondrial dysfunction. Inflammation 0123456789. https://doi.org/10.1007/s10753-022-01697-y
Takayama KS, Monteiro MC, Saito P, Pinto IC, Nakano CT, Martinez RM, Thomaz DV, Verri WA Jr, Baracat MM, Arakawa NS, Russo HM, Zeraik ML, Casagrande R, do Couto RO, Georgetti SR (2022) Rosmarinus officinalis extract-loaded emulgel prevents UVB irradiation damage to the skin. Anais Da Academia Brasileira de Ciências 94(4):e20201058. https://doi.org/10.1590/0001-3765202220201058
Ulbricht C, Abrams TR, Brigham A, Ceurvels J, Clubb J, Curtiss W, Kirkwood CD, Giese N, Hoehn K, Iovin R, Isaac R, Rusie E, Serrano JMG, Varghese M, Weissner W, Windsor RC (2010) An evidence-based systematic review of rosemary (Rosmarinus officinalis) by the Natural Standard Research Collaboration. J Dietary Suppl 7(4):351–413. https://doi.org/10.3109/19390211.2010.525049
Wahba HMA (2022) Protective effect of Echinacea (Echinacea Angustifolia), Rosemary (Rosmarinus officinalis, L.) and Dandelion (Taraxacum Officinal) powder in alloxan-diabetic rats. Res J Specif Educ 2022(69):1–24. https://doi.org/10.21608/mbse.2022.141682.1197
Watanabe S, Okoshi H, Yamabe S, Shimada M (2021) Moringa oleifera lam. In diabetes mellitus: a systematic review and meta-analysis. Molecules 26(12):1–18. https://doi.org/10.3390/molecules26123513
Yashin A, Yashin Y, Xia X, Nemzer B (2017) Antioxidant activity of spices and their impact on human health: a review. Antioxidants 6(3):1–18. https://doi.org/10.3390/antiox6030070
Zhang Y-J, Gan R-Y, Li S, Zhou Y, Li A-N, Xu D-P, Li H-B (2015) Antioxidant phytochemicals for the prevention and treatment of chronic diseases. Molecules (Basel, Switzerland) 20(12):21138–21156. https://doi.org/10.3390/molecules201219753
Zhou X, Rougée LRA, Bedwell DW, Cramer JW, Mohutsky MA, Calvert NA, Moulton RD, Cassidy KC, Yumibe NP, Adams LA, Ruterbories KJ (2016) Difference in the pharmacokinetics and hepatic metabolism of antidiabetic drugs in Zucker diabetic fatty and sprague-dawley rats. Drug Metab Dispos 44(8):1184–1192. https://doi.org/10.1124/dmd.116.070623
Acknowledgements
We appreciate Dr. Zbys Fedorowicz (Veritas Health Sciences Consultancy) and Gesner Francisco Xavier Junior (librarian of the Medical School – Federal University of Minas Gerais) for their valuable support with the review protocol.
Funding
Virgínia Moura Oliveira received a scientific initiation grant (PIBIC) from the Universidade Federal de São João del- Rei and Fundação de Amparo à Pesquisa do Estado de Minas Gerais (UFSJ/FAPEMIG; grant number 21092). Kitete Tunda Bunnel received a Master’s grant from the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brazil (CAPES; grant number 88887.824838/2023-0). This study was also funded in part by the CAPES - Financial Code 001.
Author information
Authors and Affiliations
Contributions
ROC: Conceptualization, Funding acquisition, Project administration, Supervision, Writing—review & editing; NRB and CPD: Methodology, Formal analysis, Software, Writing—review & editing; VMO: Data curation, Formal analysis, Investigation, Writing—original draft; LRS: Investigation, Validation; KTB and AOB: Writing—review & editing.
Corresponding author
Ethics declarations
Ethical statement
This article does not contain any studies involving animals performed by any of the authors. This article does not contain any studies involving human participants performed by any of the authors.
Conflict of interest
Virginia Moura Oliveira has no conflict of interest. Letícia Rafaela Silveira has no conflict of interest. Kitete Tunda Bunnel has no conflict of interest. Caroline Pereira Domingueti has no conflict of interest. André Oliveira Baldoni has no conflict of interest. Nayara Ragi Baldoni has no conflict of interest. Renê Oliveira do Couto has no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Oliveira, V.M., Silveira, L.R., Bunnel, K.T. et al. Rosemary (Rosmarinus officinalis L.) improves biochemical outcomes in diabetes mellitus: a systematic review and meta-analysis of animal studies. ADV TRADIT MED (ADTM) (2024). https://doi.org/10.1007/s13596-024-00742-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13596-024-00742-5