Abstract
Gastric ulcer is a serious global health challenge, and various natural products are being investigated to prevent and manage the condition. This study evaluated the gastroprotective and ulcer healing potentials of Nigerian bee propolis flavonoid-rich extract (NPE) on acetic acid-induced gastric ulcers in albino rats. Sixty adult male albino rats (222 ± 6.4 g) randomised into 5 groups (n = 12) were studied. Group A (SHAM) was left untreated, while gastric ulcer was induced in groups B (NPE), C (omeprazole) and D (saline). Group E (PRPE) was pre-treated with NPE prior to ulcer induction. The rate of ulcer contraction, volume and pH of gastric juice, and histopathological parameters were evaluated. The results showed a significantly higher rate of contraction (P = 0.001) between days 9 and 12 (NPE > OME > PRPE > SAL) and a significant decrease (P = 0.003) in the volume of gastric juice between days 9 and 12 (NPE < OME < PRPE). Gradual increase in pH was observed in all the groups from days 3 to 12, with a significantly higher rate (P < 0.001) between day 6 and 12 (SHAM > NPE > OME > PRPE > SAL). Histological evaluation showed significantly high neutrophils and macrophages on day 6 (P = 0.006) and lymphocytes (P = 0.004) between day 6 and 12 in the OME and NPE groups. NPE showed gastroprotective and ulcer healing properties by inhibiting ulcer formation and facilitating the curation of induced ulcers and is, therefore, a valuable alternative to conventional gastric ulcer therapy, especially in poor resource settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric ulcers are defects in the stomach seen as sores or erosions in the gastric mucosa and sub-mucosa which may extend through the muscularis and serosa (Bukhari et al. 2011). Gastric mucosal injuries occur when a disequilibrium between gastric acid secretion and gastric mucosal defense systems leads to a disruption in the balance between the aggressive nature of the gastric acid and protective factors of the stomach (Lima et al. 2006; Tulassay & Herszényi 2010; Zatorski et al., 2017).
Gastric ulcers are induced by various factors, disease conditions and drugs with prolonged non-steroidal anti-inflammatory drug (NSAID) therapy as the most common inducing factor in dogs (Wallace, 1992; Laine et al. 2008). Other inducing factors include bacterial infection (Helicobacter pylori), nutritional deficiencies, ingestion of irritant 'chemicals' or drugs, stress, physical burns (Curling’s ulcer) and age-related decline in prostaglandin levels (Belaiche et al. 2002). The condition may also be induced by pre-existing hepatic or renal disease (Kang 1994; Liang et al. 2014). The clinical signs in ulcer patients vary but mainly include vomiting, hematemesis (Fitzgerald et al. 2017; Pennick et al. 1997), abdominal pain, melena, erratic anorexia and weight loss (Pennick et al. 1997). Chronic gastritis, anaemia and shock may be present in severe cases (Pennick et al. 1997). Diagnosis of gastric ulcers basically involves patient’s signalment, history and physical examination. Blood and serum analysis as well as diagnostic imaging techniques (radiography, endoscopy, gastro-camera photography and ultrasonography) may also provide vital information leading to definitive diagnosis of the condition (Parrah et al. 2013).
Medical and surgical methods have been employed to manage gastric ulcers (Fossum and Hedlund 2003). In the sequence of gastric ulcer management, it is usually expedient to exhaust conservative medical management before attempting surgical intervention, with proper consideration of the severity of the condition. Antacids, sucralfate, H2-receptor antagonists and proton-pump inhibitors are current inorganic medical remedies used in the management of gastric ulcers (Manonmani et al. 1995; Bighetti et al. 2005). In more recent times, investigations have focused on exploring the gastric ulcer healing potentials of organic products, including propolis, following reports of efficacy in the management of several other health conditions (Kuropatnicki et al. 2013). Studies have since shown the efficacy of Brazilian green, Indian, Egyptian and southern-Poland propolis in the treatment of gastric ulcers in experimental rat models (de Barros et al 2007).
In Nigeria, however, little is known about propolis and only a few studies have been conducted using propolis (Babatunde et al. 2015). Although the cutaneous wound healing potential of the Nigeria bee propolis was recently investigated (Eyarefe et al. 2019a, b), its gastroprotective and ulcer healing potentials are yet to be reported. This requires further research that may lead to new discoveries of its compositions and possible applications. This study therefore investigated the gastroprotective and ulcer healing effects of Nigeria bee propolis flavonoid-rich extract on acetic acid- induced gastric ulcer in albino rats (Wistar strain).
Materials and methods
Ethical approval
Ethical approval (Ethic no. UI-ACUREC/19/0151) was obtained from the Animal Care and Use Ethical Committee, University of Ibadan before commencement of the study.
Experimental animal management
Sixty (60) male Albino rats (Wistar strain) weighing 222.2 ± 6.4 g were used for this study. They were acquired from a commercial breeding unit, housed in well ventilated 12 × 15 inches individual cages (27 ± 1 °C, and 12 h light/dark cycle) at the Laboratory Animal house, Faculty of Veterinary medicine, University of Ibadan (UI) and fed with commercial rat pellets (Breedwell feeds limited, Nigeria) and water ad-libitum. All animals received humane care and experiments were preceded by a 2-week acclimatization period, during which they were monitored once a day to check their health status as well as food intake and any behavioural changes.
Preparation of propolis extract
Crude Bee propolis was obtained from the Iwo, Osun state beehive site of the University of Ibadan Apiary unit and stored in a dark waterproof container. Extraction was carried out using a standard extraction technique (Couto 2001).
Study design
A simple randomized controlled design was adopted for this study. The rats were randomly assigned to one of five (5) treatment groups: Sham (SHAM), propolis extract (NPE), omeprazole (OME), saline (SAL) and propolis extract pretreated (PRPE).
Experimental induction of gastric ulcer
Anaesthesia: Each rat was fasted for 24 h and the body weight was determined using an electronic weighing scale (Camry Electrinic Limited, China) prior to anaesthetic induction. Anesthetic induction and maintenance were achieved by single doses each of 2% Xylazine HCl (Bioveta, Czech Republic) (5.0 mg/kg) and 5% Ketamine (Kwality Pharmaceuticals Limited, India) (35.0 mg/kg) via intramuscular injection at the quadriceps group of muscles (Eyarefe and Amid 2010).
Aseptic protocol: Following anaesthesia, the rats were placed on dorsal recumbency and the ventral abdomen of each rat was prepared for aseptic surgery by carefully shaving, followed by scrubbing and sterilization with alcohol and povidone iodine (Khoo et al. 2010).
Surgical Technique: The abdominal cavity was accessed via a 1.5–2 cm left paramedian incision. The stomach was exteriorized, stabilized with chalazion eye forceps and 0.03mls of normal saline was carefully injected into the gastric lumen of rats in Group A; while those in groups B to E were injected with 0.03 ml of 30% acetic acid solution at the area limited by the forceps. The stomach was returned into the abdominal cavity and the laparotomy incision closed with nylon sutures (Huaian Amgel Medical Instruments Co. Ltd, Jiangsu China) in cruciate suture pattern.
Post-operative care: Following surgical procedures, the rats were placed in plastic cages padded with cotton wool and warm water bags to provide a warm environment. Each rat received 5 ml of Dextrose saline (Unique Pharmaceuticals Limited, Nigeria) by oral gavage four times at 15 min interval after recovery from anaesthesia to prevent hypoglycemia, and placed on blenderized diet (corn, edible common salt and milk with vanilla flavour) post-operatively till day 6. The rat pellets (Breedwell feeds limited, Nigeria) were gradual re-introduced from day 7 and water was provided ad-libitum.
Rats monitoring and establishment of gastric ulcer
The rats were carefully monitored for 3 days post-induction for clinical signs of gastric ulcers (dark tarry stool, reduced activities, arching of the back, vocalization) and scored (Table 1). Three rats each from groups A to D were sacrificed on day 3 to establish the presence of gastric ulcer, after which the treatment protocol was commenced.
Treatment protocol
Group A rats were left untreated, while rats in group B were treated with 30 mg/kg Propolis extract daily, those in group C were treated with 20 mg/kg Omeprazole daily and those in group D received 2mls normal saline daily, all by oral gavage.
Rats in group E however were pretreated with 30 mg/kg bw Propolis extract daily (till end of study) before the induction of gastric ulcers in 3 rats each on days 3, 6, 9 and 12. All drugs were administered orally.
Euthanasia
Three rats each in groups A to D were sacrificed with euthanizing doses of Xylazine (Bioveta, Czech Republic) (70 mg/kg) and Ketamine (Kwality Pharmaaceuticals Limited, India) (15 mg/kg) on days 6, 9 and 12 respectively followed by evaluation (gastric juice collection and measurement of ulcer size). The rats in group E were sacrificed 72 h post ulcer induction and evaluation was carried out as described for groups A to D.
Evaluation of gastric ulcer healing
Gastric juice collection and pH determination
Following euthanasia, a paramedian laparotomy incision was made to access the stomach, which was exteriorized, carefully tied around both openings (cardiac & pyloric sphincters) and harvested. The ligature at one end was loosened and the gastric content was carefully collected in sterile sample tubes and centrifuged at 500 rpm, for 5 min using a tube centrifuge (Celtech 800D Centrifuge, China). The supernatant was carefully aspirated using a Pasteur pipette and the volume of gastric juice was measured using graduated 1 ml syringe.
The pH of the gastric juice of each rat was evaluated using a pH strip with colour indicator (AtFipan pH Universal indicator paper).
Gross evaluation of gastric mucosa and ulcer size determination
The stomach of each rat was incised longitudinally along the greater curvature, gently rinsed with saline and examined grossly for ulcers. The size of the ulcer was measured (in cm3) using a transparent graph sheet as previously described (Majeske 1992) to evaluate rate of ulcer contraction. The obtained ulcer size was used to calculate the percentage of wound contraction with the formula:
Pictures of each wound were also taken on each day of observation.
Histopathological examination
After gross evaluation, the harvested stomach was fixed in 10% neutral buffered formalin and submitted for independent histological examination by pathologists blinded to the groupings. The lesions were scored and categorised (Table 1) as described by Andrew et al. (2002) with slight modifications. Representative sections were stained with haematoxylin and eosin (H&E) for microscopic evaluation of inflammatory cells.
Statistical analysis
Data generated from rate of ulcer contraction, volume of gastric juice and pH were descriptively presented as ‘mean ± standard deviation’, using SPSS version 16.0. Significant differences between groups were assessed using one-way ANOVA followed by post-hoc multiple comparison test. Values of P < 0.05 were considered statistically significant. Fig 1.
Results
Clinical signs of gastric ulcers
Following induction of gastric ulcers, clinical signs such as dark tarry faeces, vocalisation and arching of the back attributed to the presence of gastric ulcers were prominent in the rats in NPE, OME, SAL and PRPE groups on day 3 compared with the SHAM group in which these signs were not as prominent (Table 2). The clinical signs progressively diminished following the commencement of treatments in the four groups. However, in SAL group, it was observed that the signs persisted for a longer period, not reducing at the same pace as the NPE, OME and PRPE groups, but no visible or palpable clinical signs were observed in the SHAM groups. Table 3.
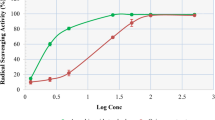
Gastric ulcer contraction
Ulcers were not observed in the SHAM group. Fig 2 Ulcer contraction was gradual in all the other groups from day 3 to day 12, with a significantly higher rate of contraction (P = 0.001) between days 9 and 12 in the NPE, OME and PRPE groups compared with the SAL group with the trend being (NPE > OME > PRPE > SAL). Almost complete wound closure occurred on day 12 in the NPE group.
Volume of gastric juice
The volume of gastric juice obtained from the stomach of rats in the SHAM group was significantly lower when compared with the other groups. There was a significant decrease in the volume of gastric juice in the NPE, OME and PRPE groups (P = 0.003) between days 9 and 12, with the trend being (NPE < OM < PRPE), but there was non-significant decrease in the SAL group.
pH of gastric juice
There was gradual increase in pH in all the groups from day 3 to day 12, with significantly higher rate (P < 0.001) between days 6 and 12 in the NPE, OME and PRPE groups compared with the SAL group with the trend being (SHAM > NPE > OME > PRPE > SAL).
Inflammatory Cell response
Across the five groups, inflammatory cellular response was significantly higher (P < 0.05) in the NPE, OME and SHAM groups when compared with the PRPE and SAL groups. The number of neutrophils was significantly high in the OME group (P < 0.05); macrophages was significantly high in the OME, SHAM and NPE groups (P = 0.02); Lymphocytes was significantly high in the SHAM and OM groups (P = 0.006).
The number of neutrophils and macrophages was significantly high in the OME and NPE group on day 6 (P = 0.006), with the trend being (OME > NPE > SHAM > PRPE > SAL). The number of lymphocytes was significantly high (P = 0.004) in the OME and NPE group between day 6 and day 12, with the trend being (SHAM > OME > NPE > PRPE > SAL). There was no significant difference in the Plasma cell count across the groups. Moreover, there was significant reduction in the neutrophil and macrophage counts observed in the NPE, OME and PRPE treatments (P < 0.05). Fig 3.
Discussion
Gastric ulcer disease is a global health challenge in both human and animal population with complications that include haemorrhage, perforation, gastrointestinal obstruction, and malignancy with high morbidity, mortality and economic loss to animal owners (Dimaline and Varro 2007). Many factors and mechanisms are implicated in the ulcerogenesis and gastric mucosal damage induced by different models which result in an imbalance between the gastric mucosa defence system and gastric acid production. The ability of the gastric mucosa to resist injury by endogenous secretions (acid, pepsin, and bile) and by ingested irritants can be attributed to several factors that have been generally referred to as mucosal defence system (Wallace 2001).
There has been a considerable interest in finding natural products for effective gastric ulcer management. In this study, Nigerian bee propolis elicited gastroprotective and ulcer-healing potential in acetic acid induced ulcer model. It is noteworthy that gastric ulcer has been most studied the rat model (Pillai et al. 2010). Injection of acetic acid into the stomach resulted in the induction of gastric ulcer as well as a remarkably significant increase in severity, gastric juice production, and total gastric acidity. The clinical signs observed in this study following gastric ulcer induction such as: dark tarry faeces, vocalisation and arching of the back corroborates with previous findings by Parrah, et al., (2013). The ulcer induced by acetic acid has been attributed to generation of reactive oxygen species, initiation of lipid peroxidation, infiltration of leukocytes, induction of apoptosis, and inhibition of prostaglandin synthesis (Bech-Hansen et al. 2000). Decreased prostaglandin levels impair almost all aspects of gastro-protection and increases acid secretions which, in turn, aggravate the ulcer (Miller, et al 2012).
The Nigeria Bee Propolis produced both gastroprotective and ulcer healing potentials similar to that observed with the Egyptian Propolis (Pillai, et al. 2010; Abd El-Hady, et al. 2013). The gastroprotective and ulcer curative effects of propolis are ascribed to the anti-ulcer properties of flavonoids such as quercetin, naringenin and caffeic acid phenethyl ester (CAPE) present in bee propolis samples and known to reduce the production and release of histamine and other inflammatory mediators such as interleukins and tumour necrotic factor- ∝ (Moura, 2011).
Nigerian Bee propolis accelerated the healing of gastric ulcers in rats (Wistar strain) at a rate similar to Omeprazole, a known ulcer healing agent that served as positive control in this study (Blandizzi et al. 1995; Biswas et al. 2003). Oral administration of Nigerian bee propolis significantly reduced the ulcer area, gastric acid output and acidity of the studied rats. Ulcer contraction that was gradual in all the groups from day 3 to day 12, was significantly higher between days 9 and 12 (P = 0.001) in the propolis extract, omeprazole and the pre-treated groups than in the saline treated group. This could be due to the ability of propolis to influence the production of transforming growth factor –alpha and beta 1 (TGF- ∝ and TGF –ß1) by immune cells which stimulates cell growth (Martinotti and Ranzato 2015). Wound contraction was slower in the saline treated group which could be as a result of extended inflammatory and debridement phases (Rosique et al. 2015). There was a significant decrease in the volume of gastric juice in the NPE, OME and PRPE groups (P < 0.001) between days 9 and 12. The observed decrease in gastric acid volume in the NPE group could be attributed to propolis’ ability to antagonise the binding of histamine to the H2 receptor on the parietal cells (Banji et al. 2010). The gradual increase in pH in all the groups from day 3 to 12, with significantly higher rate (P = 0.001) between days 6 and 12 in the NPE, OME and PRPE groups compared with the SAL group could be attributed to reduction in hydrogen ion concentration in the gastric juice (Lüllmann et al. 2000). This showed that propolis is a good gastroprotective agent since the gastric ulcer indices were lowest on the day of induction in the pre-treated group in comparison with the other groups.
The significant level of inflammatory cellular infiltrates (neutrophils and macrophages) in the Propolis and Omeprazole treated groups confirms an acute phase response to injury and healing of induced ulcer. The wound healing process is composed mainly of three overlapping phases: inflammation, proliferation and remodelling phases Baum and Arpey, 2005; Liu and Velazquez 2008). After injury ensues, platelets are activated at the site of blood vessel rupture, promoting clot formation to halt blood loss. Platelets also release factors that attract immune cells from the circulation into the wound. This marks the commencement of the inflammatory phase. Polymorphonuclear cells (neutrophils) arrive first, and then monocytes which rapidly differentiate into macrophages (Sindrilaru and Scharffetter-Kochanek 2013). Neutrophils produce high levels of reactive oxygen species (ROS), proteases and pro-inflammatory cytokines to sanitise the wound. When this process is complete, neutrophils apoptose and become phagocytosed by the newly arrived macrophages. There is considerable evidence that macrophages are key regulators of the wound healing process, during which they take on distinctive roles to ensure proper healing (Mosser and Edwards 2008).
Macrophages continue to phagocytose bacteria and debris to further clean the wound (Frykberg and Banks, 2015), during which the wound is sterilised and prepared for tissue regrowth in the proliferative phase (Baum and Arpey, 2005). Macrophages also play particularly important roles in vascularisation, by positioning themselves nearby newly emerging blood vessels and aiding in their stabilisation and fusion (Fantin et al. 2010; Ogle et al. 2016).
During the remodelling phase, Vascularised Extracellular Matrix (ECM) is laid down and gastric mucous cells migrate upon it to close the wound or ulcer (Falanga 2005). In the beginning of the final remodelling phase, macrophages release matrix metalloproteinases (MMPs) to breakdown the provisional extracellular matrix, and then apoptose so that the tissue or mucosal surface can mature to its original, non-wounded state (Vannella and Wynn 2017).
Also noteworthy is the lymphocytes number in the gastric mucosa of the NPE group that signifies some level of adaptive immunity. This immune cellular infiltration into the stomach tissues aids in autolytic debridement and growth of new tissues, thus the healing properties of propolis as observed in this study could also be attributed to propolis immune stimulating effect (Dimov et al. 1991). This information is of essence in clinical practice where Nigerian bee propolis could serve for prophylactic management patients at risk of gastric ulcer (Oyetayo et al. 2022).
In conclusion, results from this study showed that Nigerian bee propolis flavonoid extract is a potent gastroprotective and ulcer healing natural agent. It is therefore recommended as an alternative to current conventional antiulcer treatments and for prophylactic management of patients at risk of gastric ulcer disease.
References
Abd El-Hady FK, El Awdan SA, Ibrahim AM (2013) Anti-ulcerative potential of Egyptian propolis against oxidative gastric injury induced by indomethacin in rats. Asian J Med Pharm Res 3:35–42
Andrews FM, Reinemeyer CR, McCracken MD, Blackford JT, Nadeau JA, Saabye L, Sötell M, Saxton A (2002) Comparison of endoscopic, necropsy and histology scoring of equine gastric ulcers. Equine Vet J 34(5):475–478. https://doi.org/10.2746/042516402776117827
Babatunde IR, Abdulbasit A, Oladayo MI, Olasile OI, GbolahanBW OFR (2015) Hepatoprotective and pancreatoprotective properties of the ethanolic extract of nigerian propolis. J Intercult Ethnopharmacol 4:102–108. https://doi.org/10.5455/jice.20150202023615
Banji D, Singh J, Banji OJ, Shanthamurthy M (2010) Scrutinizing the aqueous extract of leaves of pedalium murex for the antiulcer activity in rats. Pak J Pharm Sci 23:295–299
Baum CL, Arpey CJ (2006) Normal cutaneous wound healing: clinical correlation with cellular and molecular events. Dermatol Surg 31(6):674–686. https://doi.org/10.1111/j.1524-4725.2005.31612
Bech-Hansen NT, Naylor MJ, Maybaum TA, Sparkes RL, Koop B, Birch DG, Bergen AA, Prinsen CF, Polomeno RC, Gal A, Drack AV (2000) Mutations in NXY, encoding the leucine-rich proteoglycan nyctalopin, cause X-linked complete congenital stationary night blindness. Nat Genet 26(3):319–332
Belaiche J, Burette A, De Vos M, Louis E, Huybrechts M, Deltenre M (2002) Observational survey of NSAID-related upper gastro-intestinal adverse events in Belgium. Acta Gastroenterol Belg 65(2):65–73
Bighetti AE, Antonio MA, Kohn LK, Rehder VL, Foglio MA, Possenti A, Vilela L, Carvalho JE (2005) Antiulcerogenic activity of a crude hydroalcoholic extract and coumarin isolated from Mikania laevigata Schultz Bip. Phytomedicine 12(1–2):72–77. https://doi.org/10.1016/j.phymed.2003.09.006
Biswas K, Bandyopadhyay U, Chattopadhyay I, Varadaraj A, Ali E, Banerjee RK (2003) A novel antioxidant and antiapoptotic role of omeprazole to block gastric ulcer through scavenging of hydroxyl radical. J Biol Chem 278(13):10993–11001. https://doi.org/10.1074/jbc.M210328200
Blandizzi C, Gherardi G, Marveggio C, Natale G, Carignani D, Del Tacca M (1995) Mechanisms of protection by omeprazole against experimental gastric mucosal damage in rats. Digestion 56(3):220–229. https://doi.org/10.1159/000201247
Bukhari MH, Khalil J, Qamar S, Qamar Z, Zahid M, Ansari N, Bakhshi IM (2011) Comparative gastroprotective effects of natural honey, Nigella sativa and cimetidine against acetylsalicylic acid induced gastric ulcer in albino rats. J Coll Physicians Surg Pak 21(3):151–156
Couto A (2001) How to process raw propolis into propolis extracts by Food and Agricultural Organization of the United Nations. In: ‘Value added products of the beehive’. www.fao.org/teca.fao.org/pt-br/read/8580. Accessed 2 Feb 2021
de Barros MP, Sousa JP, Bastos JK, de Andrade SF (2007) Effect of Brazilian green propolis on experimental gastric ulcers in rats. J Ethnopharmacol 110(3):567–571. https://doi.org/10.1016/j.jep.2006.10.022
Dimaline R, Varro A (2007) Attack and defence in the gastric epithelium–a delicate balance. Exp Physiol 92(4):591–601. https://doi.org/10.1113/expphysiol.2006.036483
Dimov V, Ivanovska N, Manolova N, Bankova V, Nikolov N, Popov S (1991) Immunomodulatory action of propolis Influence on anti-infectious protection and macrophage function. Apidologie 22(2):155–162
Eyarefe OD, Amid SA (2010) Small bowel wall response to enterotomy closure with polypropylene and polyglactin 910 using simple interrupted suture pattern in rats. Adv Anim Vet Sci 2(3):72–75
Eyarefe OD, Ozota CA, Jarikre TA, Emikpe BO (2019a) Pathological and immunohistochemical evaluation of wound healing potential of Nigerian bee propolis in albino rats. Comp Clin Path 28(2):455–466. https://doi.org/10.1007/s00580-018-2873-4
Eyarefe OD, Ozota CA, Jarikre TA, Emikpe BO (2019b) Pathological and immunohistochemical evaluation of wound healing potential of Nigeria bee propolis in albino rats. Comp Clin Path 28(2):455–466
Falanga V (2005) Wound healing and its impairment in the diabetic foot. The Lancet 366(9498):1736–1743. https://doi.org/10.1016/S0140-6736(05)67700-8
Fantin A, Vieira JM, Gestri G, Denti L, Schwarz Q, Prykhozhij S, Peri F, Wilson SW, Ruhrberg C (2010) Tissue macrophages act as cellular chaperones for vascular anastomosis downstream of VEGF-mediated endothelial tip cell induction. Blood J Am Soc Hematol 116(5):829–840. https://doi.org/10.1182/blood-2009-12-257832
Fitzgerald E, Barfield D, Lee KCL, Lamb CR (2017) Clinical findings and results of diagnostic imaging in 82 dogs with gastrointestinal ulceration. J Small Anim Pract 58:211–218
Fossum TW, Hedlund CS (2003) gastric and intestinal surgery. Vet Clin North Am Small Anim Pract 33(5):1117–1145
Frykberg RG (2015) Challenges in the treatment of chronic wounds. Adv Wound Care 4:560–582. https://doi.org/10.1089/wound.2015.0635
Kang JY (1994) Peptic ulcer in hepatic cirrhosis and renal failure. J Gastroenterol Hepatol 9(S1):S20-23
Khoo YT, Halim AS, Singh KKB, Mohammed NS (2010) Wound contraction effects and antibacterial properties of Tualang honey on full thickness burn wounds in rats in comparison to hydrofibre. BMC Complement Altern Med 10(48). https://doi.org/10.1186/1472-6882-10-48
Kuropatnicki AK, Szliszka E, Krol W (2013) Historical aspects of propolis research in modern times. Evid Based Complement Altern Med 2013:964149. https://doi.org/10.1155/2013/964149
Laine L, Takeuchi K, Tarnawski A (2008) Gastric mucosal defense and cytoprotection: bench to bedside. Gastroenterology 135(1):41–60. https://doi.org/10.1053/j.gastro.2008.05.030
Liang CC, Muo CH, Wang IK, Chang CT, Chou CY, Liu JH, Yen TH, Huang CC, Chung CJ (2014) Peptic ulcer disease risk in chronic kidney disease: ten-year incidence, ulcer location, and ulcerogenic effect of medications. PLoS ONE 9(2):e87952. https://doi.org/10.1371/journal.pone.0087952
Lima ZP, Severi JA, Pellizzon CH, Brito AR, Solis PN, Cáceres A, Girón LM, Vilegas W, Hiruma-Lima CA (2006) Can the aqueous decoction of mango flowers be used as an antiulcer agent? J Ethnopharmacol 106(1):29–37. https://doi.org/10.1016/j.jep.2005.11.032
Liu ZJ, Velazquez OC (2008) Hyperoxia, endothelial progenitor cell mobilization, and diabetic wound healing. Antioxid Redox Signal 10(11):1869–1882. https://doi.org/10.1089/ars.2008.2121
Lüllmann H, Mohr K, Hein L, Bieger D (2000) Color atlas of pharmacology. Thieme Publishing, New York
Majeske C (1992) Reliability of wound surface area measurements. Phys Ther 72(2):138–141. https://doi.org/10.1093/ptj/72.2.138
Manonmani S, Viswanathan VP, Subramanian S, Govindasamy S (1995) Biochemical studies on the antiulcer activity of polyalthia longifolia (Sonn). Indian J Pharmacol 40:126–128
Martinotti S, Ranzato E (2015) Propolis: a new frontier for wound healing? Burns Trauma 3(1):9. https://doi.org/10.1186/s41038-015-0010-z
Miller AC, Rashid RM, Falzon L, Elamin M, Zehtabchi S (2012) Silver sulfadiazine for the treatment of partial thickness burns and venous stasis ulcer. J Am Acad Dermatol 66:159–165
Mosser DM, Edwards JP (2008) Exploring the full spectrum of macrophage activation. Nat Rev Immunol 8(12):958–969. https://doi.org/10.1038/nri2448
Moura SA, Negri G, Salatino A, Lima LD, Dourado LP, Mendes JB, Andrade SP, Ferreira MA, Cara DC (2011) Aqueous extract of Brazilian green propolis: primary components, evaluation of inflammation and wound healing by using subcutaneous implanted sponges. Evid Based Complement Altern Med 2011:748283. https://doi.org/10.1093/ecam/nep112
Ogle ME, Segar CE, Sridhar S, Botchwey EA (2016) Monocytes and macrophages in tissue repair: Implications for immunoregenerative biomaterial design. Exp Biol Med 241(10):1084–1097. https://doi.org/10.1177/1535370216650293
Oyetayo NS, Kodie DO, Awoyemi OS, Afolabi OO, Eyarefe OD, Emikpe BO (2022) Prevalence and associated factors of gastric and intestinal ulcers in companion and exotic animal patients at a university veterinary teaching hospital in Nigeria: a preliminary report. Niger Vet J in Press 42(1):71–77
Parrah JD, Moulvi BA, Gazi MA, Makhdoomi DM, Athar H, Dar S, Mir AQ (2013) Gastric ulceration in dog: A review. Vet World 6(7):449–454
Pennick D, Matz M, Tidwell A (1997) Ultrasonography of gastric ulceration in the dog. Vet Radiol Ultrasound 38(4):308–312. https://doi.org/10.1111/j.1740-8261.1997.tb00860.x
Pillai SI, Kandaswamy M, Subramanian S (2010) Antiulcerogenic and ulcer healing effects of Indian propolis in experimental rat ulcer models. J ApiProduct ApiMed Sci 2(1):21–28. https://doi.org/10.3896/ibra.4.02.1.02
Rosique RG, Rosique MJ, Farina Junior JA (2015) Curbing inflammation in skin wound healing: a review. Int J Inflam 2015:316235. https://doi.org/10.1155/2015/316235
Sindrilaru A, Scharffetter-Kochanek K (2013) Disclosure of the culprits: macrophages—versatile regulators of wound healing. Adv Wound Care 2(7):357–368. https://doi.org/10.1089/wound.2012.0407
Tulassay Z, Herszényi L (2010) Gastric mucosal defense and cytoprotection. Best Pract Res Clin Gastroenterol 24(2):99–108
Vannella KM, Wynn TA (2017) Mechanisms of organ injury and repair by macrophages. Annu Rev Physiol 79:593–617. https://doi.org/10.1146/annurev-physiol-022516-034356
Wallace JL (1992) Prostaglandins, NSAIDs, and cytoprotection. Gastroenterol Clin North Am 21(3):631–641. https://doi.org/10.1016/S0889-8553(21)00052-2
Wallace JL (2001) Mechanisms of protection and healing: current knowledge and future research. Am J Med 110(1):S19-23. https://doi.org/10.1016/S0002-9343(00)00631-8
Zatorski H, Mosinska P, Salaga M, Wlodarczyk M, Siwinski P, Wlodarczyk AS, Wasilewski A, Fabisiak A, Fabisiak N. Peptic ulcer disease. In: Introduction to gastrointestinal diseases. Switzerland AG: Springer; 2017:2:1–96.
Acknowledgements
The authors would like to acknowledge Mrs. Adekunle, Mr R.O. Lasisi, Mrs Ogundiran and Mr. A.J. Davidson of the Department of Surgery and Radiology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Ethical approval (Ethic no. UI-ACUREC/19/0151) was obtained from the Animal Care and Use Ethical Committee, University of Ibadan for the use of experimental animals before the commencement of the study. All animals received humane care and all methods were performed in accordance with the relevant guidelines and regulations stipulated in the ARRIVE guidelines.
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Oyetayo, N.S., Kodie, D.O., Nwakasi, M.I. et al. Gastroprotective and ulcer healing potentials of Nigerian Bee Propolis flavonoid extract on acetic acid-induced gastric ulcers in albino rats (Wistar Strains). ADV TRADIT MED (ADTM) 23, 1221–1230 (2023). https://doi.org/10.1007/s13596-022-00674-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13596-022-00674-y