Abstract
Thermal skin burn injury affects both adults and children globally. Severe burn injury affects a patient’s life psychologically, cosmetically, and socially. The pathophysiology of burn injury is well known. Due to the complexity of burn pathophysiology, the development of specific treatment aiding in tissue regeneration is required. Treatment of burn injury depends on burn severity, size of the burn and availability of donor site. Burn healing requires biochemical and cellular events to ensure better cell response to biochemical signals of the healing process. This led to the consideration of using cell therapy for severe burn injury. Adult mesenchymal stem cells have become a therapeutic option because of their ability for self-renewal and differentiation. Adipose stromal vascular fraction (SVF), isolated from adipose tissues, is a heterogeneous cell population that contains adipose-derived stromal/stem cells (ADSC), stromal, endothelial, hematopoietic and pericytic lineages. SVF isolation has advantages over other types of cells; such as heterogeneity of cells, lower invasive extraction procedure, high yield of cells, and fast and easy isolation. Therefore, SVF has many characteristics that enable them to be a therapeutic option for burn treatment. Studies have been conducted mostly in animal models to investigate their therapeutic potential for burn injury. They can be used alone or in combination with other treatment options. Treatment with both ADSCs and/or SVF enhances burn healing through increasing re-epithelization, angiogenesis and decreasing inflammation and scar formation. Research needs to be conducted for a better understanding of the SVF mechanism in burn healing and to optimize current techniques for enhanced treatment outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Skin is the largest organ in the human body that has many functions, including homeostasis and barrier protection. It consists of three main layers, epidermis, dermis, and subcutaneous tissue, with appendages such as hairs and glands. The epidermis contains keratinocytes, which regenerate every 2–4 weeks, and melanocytes, which regenerate slower than keratinocytes thus leading to pigmentation during burn healing. Epidermis also contains the nerves’ endings that arise from the dermis. The dermis contains blood vessels, sensory nerves, sebaceous glands, sweat glands, and hair follicles. It heals by scarring and fibrosis instead of regeneration [80]. Any damage to the skin will inevitably compromise its function, exposing individuals to other health complications.
A wound is characterized by discontinuation of skin tissue resulting in disruption of cellular structure or function by any physical, chemical or biological sources [55]. Burn wounds can be caused by chemical, heat, electrical, radiation, or freezing materials. In the United States, one million burn injuries are recorded annually [9, 80]. More than 100,000 burned patients are hospitalized from severe burn injuries [20]. Out of 0.5 million burns recorded annually, about 3000 people lost their lives and 40,000 require hospitalization, according to the National Burn Repository of the American Burn Association [3]. According to the World Health Organization, burn is the fifth most common factor causing non-fatal injuries. Severe burn injury affects a patient’s life psychologically, cosmetically, and socially. Therefore, burn is detrimental to patients and sufficient treatment is essential for a better quality of life.
Burn treatment depends on the burn size, depth and the viability of donor site. The standard care for severe burn injury is using autologous skin grafts or skin substitutes. However, in burned patients with large total body surface area (TBSA), treatment options are limited and interventions are required.
The objective of this review is to give an overview of the pathophysiology of burn injury, highlight the currently available treatment and provide insights about future possible interventions focusing on using stromal vascular fraction (SVF), methods of its isolation, and the mechanism of action.
Classification of burn
Different classifications of burn can be considered depending on the appearance, duration, or nature of healing. Burn is classified depending on the depth of injury and the appearance into four degrees: first (superficial), second (superficial partial-thickness and deep partial-thickness), third (full thickness) and fourth (extend through other layers up to the subcutaneous fat and down to the bone, fascia, and tendons) [80]. It can also be subdivided according to the affected surface area into local burn injury (< 20% of TBSA) and severe burn injury (> 20–30% of TBSA) [102]. Burn wounds could be acute or chronic depending on the nature of healing.
Thermal burn wound is divided based on the nature of healing by Jackson [48] (Hettiaratchy and Dziewulski [47]) into three zones:
-
1.
Coagulation zone: it is the deepest and most damaged zone among the three layers due to the coagulation of constituent proteins. It consists of inevitable tissues that cannot be regenerated due to the ceased circulation in this zone. It needs surgical excision and grafting [80]
-
2.
Stasis zone: it is the middle zone that consists of dermal burn, vascular stasis, ischemia, and low tissue perfusion. Often, this zone could become necrotic within 48 h after thermal injury [78]. This zone is challenging since it can be recovered; it has the potential to heal or progress to the full-thickness lesion. Healing can be achieved by increasing tissue perfusion and preventing further damage before it becomes irreversible.
-
3.
Hyperemia zone: it is the outermost layer and the least damaged area that is characterized by vasodilation, and inflammatory change without structural damage. Tissues are regenerated unless there is sepsis or prolonged hypoperfusion.
Physiological changes during severe burn injury
Unlike local burn injury, severe burn injury affects the whole body. Severe burn injury consists of two phases: the resuscitation phase and the hyperdynamic hypermetabolic phase. The Resuscitation phase (also called hypodynamic or ebb phase) occurs immediately after severe burn injury (24–72 h). It is characterized by increased vascular permeability, edema formation, and inflammatory response syndrome. Thermal burn injury starts with denaturation after long-term exposure to heat (more than 40 °C). This leads to protein misfolding (morphological dysregulation) and loss of plasma membrane integrity [55]. Moreover, released mediators alter vascular permeability and increase the inflammatory response. Increased vascular permeability causes the release of proteins and large molecules from vessels. This leads to the imbalance between oncotic and hydrostatic forces which results in the shift of fluids from intravascular space into the interstitial space resulting in edema formation. Severe burn injury decreases cellular membrane potential due to the disruption of sodium-ATPase pumps. This leads to increased sodium uptake that results in cellular swelling [102]. Therefore, this phase results from hypovolemic and inflammatory mediators’ effects to restore and preserve tissue perfusion.
After-burn’s shock, the body releases biochemical mediators as a defensive mechanism against injury. Many mediators control vasodilation, such as histamine, kinins (Bradykinin) and xanthine oxidase [102]. The xanthine oxidase leads to the release of free radicals. The balance between the production of free radicals and detoxification is a determinant of clinical response to a burn. Histamine, released by mast cells, causes capillary leakage (arteriolar dilation and venular contraction) and increases hydrostatic pressure [33, 90]. This could lead to loss of circulating plasma volume and edema formation. However, the role of histamine in severe burn injury remains controversial since the administration of histamine receptor antagonists did not show a reduction in edema formation [87]. Reactive oxygen species (ROS), released from neutrophils, infiltrate (approximately after 72 h) at the site of injury. ROS causes the release of lipid peroxidation (LPO), which regulates plasma membrane permeability. Production of ROS and LPO are involved in the biosynthesis of Prostaglandin (PGE2) and prostacyclin (PGI2), hormones, leukotrienes and thromboxane A2 (TXA2) [78]. Both PGE2 and PGI2 increase microvascular permeability and edema formation. Thromboxane A2 (TXA2), a vasoconstrictor produced by platelets, decreases blood flow and could contribute to the zone of ischemia and thrombus formation [102]. Bradykinin is released at the site of injury and exerts it is effect locally and systemically. It increases venular dilation, smooth muscle contraction and pain. Therefore, edema formation is a result of interaction between many factors, including histamine, ROS, LPO, PGE2, thromboxane and kinins.
Many agents are activated and released during burn healing and can be targeted as therapeutic agents. In severe burn injury, agents enhancing dendritic cells are released to ensure cell proliferation and accelerate wound healing. Angiogenic agents, such as hypoxia-induced factor 1 and cytokines (ex. VEGF and CXCL12) ensure endothelial progenitor cell proliferation. Wound contraction is ensured by the activation of the transforming growth factors-β (TGF-β) pathway for scar formation. During this phase, many inflammatory mediators are released against injury systemically or locally. This results in systemic inflammatory response syndrome. Macrophage migration inhibitor factor (MIF) can be released from the basal layer of the epidermis in response to thermal injury. It plays a role as an inflammatory cytokine in the innate and adaptive immunity, a neuroendocrine hormone, and a catalytic enzyme [102]. Nuclear factor-κB (NF-κB) is a transcription factor that is released after severe burn injury and regulates several inflammatory mediators, such as tumor necrosis factor (TNF), interleukin-6 (IL-6) and IL-1β, from cardiomyocytes causing cardiac dysfunction [68]. Studies have shown elevated levels of cytokines post-burn, such as IL-6, IL-8, IL-2, IL-13, I-10, and IL-17. It was suggested that pro-inflammatory cytokines that are activated by macrophages, such as IL-1, IL-6, TNF, and PGE-2, are involved in complications of severe burns [49]. Systemically, the release of TNF and IL-6 at the site of the burn is responsible for increasing infectious risk, organ failure, and death [91]. These changes in pro-inflammatory cytokines are part of the immune and endocrine response to burn injury to enhance survival. This phase of activity is followed by an anti-inflammatory response where there is a reduction in immune cells’ count to return to normal status after a few weeks [50]. Therefore, mediators involved in the healing process can be enhanced and targeted as a treatment for severe burn injury.
Hyperdynamic hypermetabolic phase (also called flow phase) occurs as a response to heat loss and downregulation of thermoregulation within 3–5 days post-burn. This phase is characterized by a reduction in vascular permeability, exacerbation in the circulation of blood, heart rate thus cardiac output to restore microvascular integrity and peripheral blood flow [102]. It is also characterized by increased metabolic rate, body temperature and oxygen consumption [50]. This phase could last up to 24 months. This phase is driven by regulators, such as catecholamine, glucagon, stress hormones and pro-inflammatory cytokines. The metabolic rate could be increased up to 3 times higher compared to the basal metabolic rate. [102]. The anti-inflammatory effect is characterized by increased T-lymphocytes helper (Th-2) and the release of three main mediators, IL-4, IL-10 and TGF. This phase is characterized by an increased metabolic rate, heart rate and cardiac output and decreased vascular permeability and lean body mass as a result of the overproduction of stress hormones.
Possible treatment
Due to the complexity of burn pathophysiology, the development of a specific treatment that aids in the regeneration of new tissues and limits further complications is required.
Nutrition and rehabilitation
Fluid replacement treatment has been adopted for resuscitation and respiratory care, such as ringer lactate or NaCl solutions. However, fluid replacement does not improve complications associated with burn injury. Significant edema in all tissues leads to complications, such as respiratory failure, and abdominal compartment syndrome, which cannot be prevented only by preventing hypovolemic shock and tissue hypoxia [86]. Several approaches have been used to control hyper-metabolic rates, such as hyperglycemia, to improve patients’ outcomes [50].
Infection control
Due to the compromised barrier function of the skin, tissues can become rapidly infected with pathogens. Moreover, hyperinflammation after-burn could cause immunosuppression and increase the infectious risk. Therefore, many topical antimicrobial agents have been developed, including bacitracin, mupirocin, and silver sulfadiazine (SSD) and aqueous solutions (e.g. mafenide acetate aka Sulfamylon and silver nitrate) [95]. The silver-based dressing was found to combat infection and eschar formation and control wound exudate. Unlike other dressing, silver-based dressing has the advantage of needing to be applied less frequently which reduces patients’ pain due to the consistent release of silver ions to the wound bed. However, topical antimicrobial agents could have their risks, including delayed healing, incomplete re-epithelization, discolored scar, hypersensitivity and ineffectiveness against some pathogens [95].
Surgical control
Deep-partial and full-thickness burns usually require multiple surgeries and repeated wound care, depending on the injured TBSA. Clinically, burn wound management includes the excision of necrotic tissues until punctate bleeding in the wound bed is visible. Then permanent autologous skin graft or a temporary skin substitute is applied. This could help in reducing infectious risk and lead to better healing results. However, this procedure could lead to loss of blood and hyperemia. Different techniques could be applied to reduce blood loss, such as thrombin spray, epinephrine soaked gauze and fibrin sealants [110]. To have a successful graft, complete homeostasis is required to prevent hematoma formation [12].
Permanent wound coverage: autograft
Autograft is the first option for physicians, and it is the current standard of care for deep-partial thickness and full-thickness burns with small TBSA. Autologous skin graft requires sufficient availability of donor’s skin, usually the epidermis layer with the papillary dermis. However, wounds heal with some degree of contraction [11].
Mesh autograft is usually used when there is a limited source of donor site to cover the wound. This technique depends on using cut slits of skin in a mesh. Applying a high mesh autograft area could delay re-epithelization and thus could increase the risk of infection, contraction, and scarring. The Head, neck and face are among the most important areas. Using meshed autografts in these areas could lead to dramatic cosmetic issues and affect patients’ quality of life. Using thick autografts could modulate contraction but increase other complications [94]. Even though using autograft is safe and promising, it is limited by the size of the burn wound, the availability of healthy skin, the time it takes for engrafting, and the healing of the donor site.
Temporary wound coverage: allograft
Autograft is the first choice of treatment when donor skin is available. In case of burn with high TBSA, skin autograft cannot be applied due to the lack of donor site. Temporary wound coverage is the available option in this situation with fresh or cryopreserved allograft. Temporary skin graft was first achieved by James Brown in 1942. It was used until the permanent cover is achieved. Temporary covering provides burn coverage, desiccation, formation of granulation tissues, and protection from microbial contamination.
For temporary burn wound coverage, several options are available. One of which is to use cryopreserved cultured epidermal allograft. This technique has many advantages, such as the ability of repeating the application, availability of frozen tissues at any time, and the possibility of giving early wound closure [105]. The other option is using skin substitute until the availability of donor sites. This includes epidermal substitute by extracting epithelial autologous cells from small biopsy of patient’s own skin. These cells are then used to form sheets called cultured epithelial autografts (CEA), such as Epicel, to apply on the burn bed or spray epithelial cells directly on the burn wound after excision such as ReCell [22, 46, 95]. However, it is complex and costly and could not replace all components of the skin [22, 104]. Treatment of burn injury with cultured epidermal grafts consisting of keratinocytes had a risk of reopening and fragility of the wound, and increase wound contraction [103]. Tissue engineered dermo-epidermal skin substitute is a treatment option, but it is sophisticated, costly, and commonly increases the risk of infection and unstable scars. These drawbacks have restricted using them worldwide and directed the research to using cell therapy.
Hypertrophic scar prevention
One of the common complications of severe burn is developing hypertrophic scar, especially when healing process is delayed or un-succeeded. Young age, darker skin color, female gender, and burn severity are among the risk factors of hypertrophic scar formation [95]. Currently, there is no affective therapy for preventing hypertrophic scar formation. Some of the used techniques include messaging, moisturizing, using pressure garments or silicone gel sheets [4]. These techniques are not costly or risky and applicable but are not completely effective.
Burn healing requires biochemical and cellular events. However, many factors could interfere with healing process and delay healing. For instance, persistent inflammatory state could delay healing and lead to complications. Macrophages mediate inflammation through different approaches. When macrophages’ functions are dysregulated by development of persistent inflammatory state, they become a type I inflammatory phenotype and impede progress toward burn repair regeneration [32]. Therefore, one of the reasons behind healing’s delay is the presence of unresponsive cells that are incapable of responding to normal biochemical signals. These findings led investigators to consider using cell-based therapy as a solution of delayed healing in wound. Since using autograft or allografts have their limitations, stem cells have become a therapeutic option for their ability to self-renew and differentiation to other cell types.
Cell therapy
Burn healing is a process aiming in restoring the normal structure of the skin. Some of the available treatments are promising. However, new therapeutic approaches are needed to improve burn care and wound repair. The alternative of the pharmaceutical treatments could be cell therapy through the application of stem cells. Endogenous stem cells are found in the inter-follicular epidermis and sebaceous glands. Studies have showed rapid healing in superficial burns where hair follicles are intact. However, in severe burn injury, where hair follicles are damaged, burn healing demonstrated scarring and lacked adnexal structure [63]. Therefore, the presence of stem cells in the injured site is crucial for healing process in severe burn injury.
Stem cells can be derived from a variety of sources, including embryonic (pluripotent) or adult tissues (multipotent), such as bone marrow, adipose tissue, and hair follicles. Due to ethical and logistical issues, research has shifted from employing embryonic stem cells to adult stem cells. Several studies have investigated different types of stem cells in burn healing. For instance, amniotic stem cells enhanced re-epithelization, angiogenesis, wound closure compared to collagen gel in treated mice [92]. Bone marrow-derived mesenchymal stem cells combined with an artificial dermal substitute promoted healing in a full-thickness burn by enhancing vascularization and re-epithelization in mice [64]. Compared to bone marrow, adipose tissue can provide a higher yield of adipose-derived stem cells (ADSC), also called mesenchymal stem cells, which can be acquired readily with a less invasive technique and donor site morbidity. Therefore, ADSCs present a better substitute for bone marrow-derived stem cells in many therapeutic applications.
ADSC in burn healing
ADSCs are among the stem cells that are candidates for burn treatment for many reasons; ADSCs are multipotent and can be easily isolated, have paracrine, tropic, and immune-modulating properties that enable using them in clinical settings. Studies have shown positive outcomes using ADSCs in burn injury [18, 35, 39, 82]. Treatment with ADSCs improved re-epithelization, angiogenesis, collagen deposition, and decreased inflammation and scar formation. ADSCs transplant effectiveness in burn healing depends on the cells’ count (optimal dose of 1–3 million cells), timing, and the site of cells infusion. Administration of ADSCs at two-time points (0 and 4 days) post-burn enhanced wound contraction, collagen deposition, and lymphatic vessels and reduced scar formation in the full-thickness burn rat model [38]. Multiple injections of ADSCs improved neovascularization [109]. In other burn models, positive effects were also observed with a single dosage of ADSCs. The majority of ADSCs were administered intradermally or subcutaneously. Intravenous administration of ADSCs, on the other hand, enhanced meshed autologous slit thickness skin transplant for deep- and full-thickness burn injuries [37]. Furthermore, administration of ADSCs could be at the edge or the center of the burn wound. Chang et al. [17] showed that the injection of ADSCs at the four edges of the burn wound improved wound healing when compared to injections at the center of the wound [17]. Optimization of the ADSC delivery method is required for better healing results.
In burn injury, ADSCs can be delivered to the damaged site topically, as a spray, injected at the wound bed, or administered with different dressing materials, such as hydrogel, scaffolds, etc. [21, 76, 79]. One of the treatment applications of ADSCs for skin tissue regeneration is the administration with other dressing materials. For instance, the addition of ADSCs to fat isograft or collagen scaffold improved the maturation of wound bed via boosting certain healing indicators, angiogenesis, and collagen deposition [36, 65]. ADSCs can also be used in combination with other biomaterials, such as platelet-rich plasma (PRP) and hyaluronic acid (HA). Research has been conducted to evaluate the effects of PRP and HA in tissue engineering or tissue repair, favoring wound healing. Clinical application of mixed PRP with fat graft in different dermal diseases (wounds, maxillofacial atrophy, and others) increased re-epithelization significantly when compared to HA and collagen medication [14]. In vitro, PRP increased cell proliferation and synthesis of collagen type I and HA [14]. However, employing the right concentration of PRP cell concentration could affect the outcomes. A systemic review analysis revealed that PRP/media ratio of 1 × 106 Plt/µl provides optimum nutritious supply by avoiding starvation of cells [40]. Therefore, combined administration of PRP or HA with ADSC could enhance the therapeutic effect, in comparison with isolated ADSC administration. The burn treatment therapeutic potential of using ADSCs alone or with platelet-rich plasma (PRP) was previously investigated [17, 18, 37, 38, 70, 71]. In a diabetic burned rat model, combined treatment of PRP and keratinocyte-like cells, isolated from fat, enhanced wound contraction and reduced inflammatory markers [71]. When ADSCs were seeded into PRP gel, they improved skin grafts by enhancing angiogenesis, skin thickness, and collagen arrangement [97]. Recently, it was reported that the treatment with ADSCs seeded in hyaluronic acid hydrogel or gelatin hydrogel provided an effective niche that protects ADSCs and augments their therapeutic potential for burn injury [30, 66]. ADSCs can be combined with other materials and/or used instead of synthetic materials that require a more sophisticated approach.
The other treatment application of ADSC is using ADSC-exosomes. Exosomes are membrane vesicles secreted by cells that operate as a paracrine factor in cell-to-cell communication by regulating inflammatory responses, cell proliferation and differentiation, and neovascularization. ADSC-exosome is composed of different growth factors, such as TGF- β, Growth Differentiation Factor 11 (GDF-11), Insulin-like Growth Factor (IGF) and Wingless 10b (Wnt10b), cytokines, such as IL-6, IL-8, IL-10, TNF, and IL-1 beta, and toll-like receptors (TLR2 and TLR4) [73]. These exosomes direct signaling pathways between and within cells and exert similar effects as their origin cells. Evidence has indicated the secretion of ADSC-exosomes in tissue regeneration and repair. Therefore, exosomes could play a role in burn healing similarly to ADSCs. Recently, research has shifted toward investigating the impact of ADSC-exosome in wound healing and other diseases. ADSC-exosome promotes wound healing by enhancing proliferation and angiogenesis, mainly when derived from ADSCs overexpressing nuclear factor-E2-related factor2 (Nrf2) [85]. They positively affect wound healing models via Wnt/ß-catenin, PI3K/Akt, and ncRNA H19/miR-19b/SOX9 axis signaling pathways [45, 67, 85, 108]. Consequently, this increases cell proliferation and migration, collagen deposition, and inhibition of inflammation. When ADSC-exosome was co-transplanted on fat graft, it promoted fat graft survival, reduced inflammatory infiltrate, and improved neovascularization [44]. However, the exact underlying mechanism is still unclear, either in the wound or burn healing mechanisms.
A skin substitute is an alternative to a skin graft. Reconstruction of skin substitutes from ADSCs was achieved with promising outcomes [100]. ADSCs were used to regenerate the extracellular matrix endogenously. Then keratinocytes were seeded to achieve the formation of a three-layered skin substitute. With severe burn injuries involving broad TBSA, therapeutic choices are restricted owing to the absence of the donor area. Developing skin substitutes from ADSCs isolated from adipose tissue of the surgically debrided burned skin was achieved, demonstrating vascularized skin structure [16, 74]. Cells differentiated into fibroblast-like cells when seeded into a collagen I-based matrix. They also differentiated into an epithelial layer, a vascularized dermal layer, and a hypodermal layer when seeded into a PEGylated-fibrin-based matrix. Moreover, culturing ADSCs in tropoelastin biometric skin substitute enhanced wound closure and re-epithelization in the animal model [69]. This emphasizes the beneficial role of ADSCs in skin homeostasis and healing and their ability to provide an alternative to wound coverage without the need for exogenous factors. Outcomes from these techniques in severe burn injury are required.
ADSC mechanism of action
ADSCs secrete anti-inflammatory cytokines such as interleukin-10 (IL-10) and tumor necrosis factor inducible gene siRNA6 (TSG-6) and pro-inflammatory cytokines, such as IL-1 beta and IL-17 [32]. Therefore, they can modulate the inflammatory response and reduce healing duration, especially the inflammatory phase. They are approved to be safe for clinical use and improve wound healing and other diseases [61]. Fibrogenesis’s reduction, angiogenesis, lymphogenesis, skin tissue regeneration instead of scar formation and attenuation of inflammation are crucial characteristics of ADSC in wound healing. However, there are limitations in using ADSC in wound healing that includes cell delivery methods, cell viability, heterogeneity in preparation methods and inconsistent micro-environmental cues [32].
ADSCs have anti-inflammatory and angiogenic effects; which are essential for burn healing. Several experiments in animal models have been undertaken to study the role of ADSCs in thermal burn injuries. ADSCs promoted the proliferation of keratinocytes by mediating keratinocyte growth factor- 1 (KGF-1) and platelet-derived growth factor-BB (PDGF-BB) in mice [2]. ADSC in a conditioned medium lowered apoptosis via the regulation of Bcl-2 and caspase-3 [51]. When ADSCs were compared to bone marrow stem cells and dental pulp stem cells, they showed higher myeloperoxidase activity than other sources [1]. Recently, it was reported that ADSCs reduced scar formation and lymphogenesis and increased collagen III deposition [38]. Others found that ADSC differentiated adipocytes have similar abilities to ADSC and fat grafts [18]. Therefore, ADSCs have therapeutic potential for treating severe burn injuries. However, the long process of isolation, culturing, and expansion of ADSCs increases the risk of contamination, therefore, limiting their usage in clinical applications.
Adipose stromal vascular fraction (SVF)
In the last decade, research has focused on the use of SVF produced from adipose tissues. Since the 1960s, stromal and connective tissue cells were distinguished in adipose tissues. Although adipose tissues were discarded as medical waste in surgical abdominoplasties and lipoaspirates, plastic surgeons and other researchers have documented that this tissue has a regenerative capability [8]. SVF contains a heterogeneous cell population, including adipose stromal/stem cells, endothelial, hematopoietic and pericytic lineages, representing 15–30%, 10–20%, 25–45% and 3–5%, respectively of the total nucleated cells [8]. According to the International Federation of Adipose Therapeutics and Sciences (IFATS) and the International Society for Cellular Therapy (ISCT), stromal cells within the SVF include both non-adherent cells, that cannot be cultured, and cultured stromal/stem cells, called adipose derived-stromal/stem cells [8]. This variation of cells can accelerate healing, modulate immunity, reduce inflammation and communicate locally and systemically through different signaling pathways. They can be phenotypically verified by surface antigen markers, such as CD45−, CD31−, CD34+, CD73+, CD90+, and CD105+ [8]. Even though ADSCs are effective in burn treatment, their isolation from SVF is time-consuming, complicated, and costly. Therefore, it is efficient to use the heterogeneous mix of SVF.
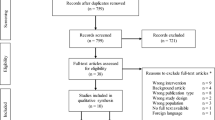
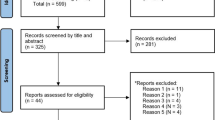
After liposuction, SVF can be isolated directly from the lipoaspirate. To isolate SVF, the standard procedure used initially was the chemical digestion of fat by collagenase, dispase, trypsin or related enzymes. Then, mechanical, non-enzymatic techniques for SVF isolation were developed and applied in clinical practice to avoid contamination of SVF, reduce the duration of the procedure, avoid practical and culturing issues, lower the cost, reduce regulatory burden, and avoid ethical issues (Fig. 1) [99]. For clinical application, many automated devices have been developed to standardize the isolation procedure, increase cell yields, and avoid contamination [57]. The automated isolation of SVF from freshly isolated lipoaspirate is a reliable method as well as the manual isolation, showing similarities in regards to cell yield, viability, and differentiation potential [28]. Developing automated isolation is a promising technique in clinical applications. Due to SVF feasibility and clinical applicability, recent research has shifted to applying SVF for burn or wound injury. Both methods were effective in clinical studies [93]. Research needs to be conducted with standardized isolation methods to compare results.
SVF in burn treatment
SVF has shown positive effects in burn healing (Table 1). SVF was used in burn injury alone or combined with other biomaterials. Fat graft burns improved vascularity and decreased fibrosis in burn beds to protect from hypertrophic scar formation [96]. The mechanism behind fat graft treatment includes acceleration of vascular endothelial growth factor (VEGF), stromal cell-derived factor-1 (SDF-1) and decreased fibrotic markers, such as TGF-β and matrix metallopeptidase 9 (MMP-9) [96]. Injection of SVF in the stasis zone of the burn wound preserved cell viability, enhanced re-epithelization and vascularization, and decreased inflammation in the burn model [34]. SVF's effect on vascularization could be due to ADSC’s ability to secrete VEGF, FGF2, glutathione, superoxide dismutase, and N-acetylcysteine [34, 77]. Treatment with SVF in deep-partial thickness burned rats showed a reduction in inflammation and increased vascularization and tissue regeneration [5]. Re-epithelization was not measured in this study. Treatment with fat isograft or ADSC or both contributed to scar remodeling by reducing wound depth, area, and apoptotic activity but did not improve vascularization in a mouse model of burn injury [65]. When compared to wound dressing (2% silver sulfadiazine), SVF increased infiltration of the polymorphonuclear cell, fibrin and fibroblast migration, angiogenesis and collagen deposition in the full-thickness burn model [13]. When SVF was compared to human mesenchymal cells in treating a hypertrophic scar, both showed positive results [29]. However, human MSC demonstrated higher expression of anti-fibrotic mediators, such as TGF-β3 and hepatocyte growth factor (HGF), and fibrosis remodeling mediators, such as MMP-2. This suggests that fat not only contribute by biochemical markers but also by improving burn wound outcomes.
Enzymatic isolation, using the collagenase method, is used in the laboratory isolation of SVFs. In clinical practice, mechanical isolation is safer and more reliable. Therefore, Karakol et al. investigated the effect of the isolation method on full-thickness burn using SVF isolated enzymatically and enzyme-free mechanical isolation of skin cell suspension (EMI) as an alternative treatment for burn injury [53]. When SVF treatment was compared with EMI, both applications improved healing histologically. Combined treatment of both applications provided better results than applying each one alone. Both applications can be isolated easily and timelessly, which makes them good alternatives for severe burn injury.
The fate and quality of SVF cells are controlled by the microenvironment that surrounds its niche. Severe burn injury response is affected by the quality of SVF or ADSC via increasing the inflammatory response in subcutaneous fat in the un-burned region. To demonstrate the suitable time for SVF or ADSC isolation after burn injury, Prasai et al. [83] demonstrated that SVF and ADSC isolated post-burn injury showed an increase in inflammatory markers and DNA damage (24–48 h) post-burn in an animal model [83]. This suggests that, in severely burned patients, isolation of SVF is recommended after inflammation is resolved.
Regarding using SVF with other biomaterials, researchers investigated the subcutaneous injection of SVF combined with PRP. In the last few years, most studies supported the combined treatment of SVF and platelet-rich plasma (PRP). PRP contains growth factors that are essential for neovascularization. The addition of PRP to SVF was reported to accelerate burn healing by increasing re-epithelization, angiogenesis, fibrosis, and collagen formation. Clinically, treatment with autologous fat graft with SVF or PRP improved graft function and maintenance in burned patients with face scars [41]. In wound injury, the treatment with SVF + PRP enhanced re-epithelization and angiogenesis and decreased inflammation when compared to using SVF or PRP alone [54]. In burn injury, the combined application of SVF and PRP, either by injection or topical administration, was found to accelerate the angiogenic growth factor VEGF serum levels during the healing [60]. VEGF is a growth factor that mediates vascular permeability and regulation during angiogenesis. The injection route was more effective than the topical application for increasing VEGF release. However, both routes were found to increase the expression of TGF-beta up to 14 days [60]. The combined treatment of both SVF and PRP decreased oxidative stress products, such as malondialdehyde, and nitric oxide, in both blood and tissues post-burn [52]. SVF therapeutic potential can be enhanced with other biomaterials, such as PRP or non-cultured stem cells. Further research is required to assess the effectiveness of using biomaterials with SVF and the optimum methods and dose for severe burn injury.
In wound and burn injury, several studies investigated the role of LASER and LED in the healing process. Both of them promoted healing by reducing inflammation, increasing proliferation, angiogenesis, and forming collagen and granulation tissue [26, 27, 56]. Treatment with both SVF and photobiomodulation enhanced burn healing in a dose-dependent manner [62]. The addition of photobiomodulation (L30) promoted healing by augmentation of the inflammatory response, angiogenesis, fibrosis contraction and collagen concentration. Low-level light using pulsed light-emitting diode light on SVF enhanced cells’ vascularization and proliferation capacity [84]. Moreover, clinically, combined treatment of fractional laser and microfat improved scar appearance in burned patients [81]. Therefore, combined administration of SVF with photomodulation could improve treatment outcomes.
Fat grafting is one of the treatment options for severe burn injury [96]. Fat grafting has been used effectively to treat numerous skin abnormalities since it requires minimal invasive procedures (liposuction). Sometimes the repeated transfer is required. However, grafting could lead to scarring, when incorporated more than 2 mm away from the blood supply, and retention, due to poor vascularization and loss of applied fat. Therefore, extensive research has been conducted to improve fat grafting survival. Cell-enriched fat grafting could include either ADSCs or SVF. ADSCs-enriched fat grafting improved graft retention and fat survival significantly in the animal models [72, 89]. SVF-enriched fat grafting improved face scar appearance in burned patients [41]. SVF-enriched fat graft increased elasticity and resilience and decreased skin contraction [19]. Histological and molecular analysis revealed that SVF increased the thickness and vascularization of the skin by elevating the expression of different growth factors, such as endothelial growth factor (EGF), basic fibroblast growth factor, and hepatocyte growth factor.
Clinically, patients with burns sequelae treated with SVF-enhanced autologous fat graft showed around 63% maintenance contour restoring when compared to patients treated with fat graft alone (39%) [41]. SVF was used to treat post-burn scars showing promising results with improvement in the scar appearance, Vancouver Scar Scale (VSS), and patient satisfaction following treatment [42, 93, 107]. In a case study report of second-degree deep facial burn, applying SVF on the burned face provided good cosmetic outcomes and functional results for the face [106]. Previous investigations were conducted in a smaller group, therefore there is a need to conduct more studies with larger cohort groups.
SVF demonstrated positive effects in the wound and burned injuries treatment either when used alone or combined with other treatment options. However, the exact mechanism behind SVF healing properties for burn injury is not fully understood. Differences in application techniques, including cell counts, purification and delivery methods, lead to a lack of consistency in the documented results. For instance, most of the studies reported that SVF was administered by injection, intradermally or subcutaneously. In contrast, others did not specify the route of administration and the site, such as stasis zone, center, or edges of the burn wound. Therefore, there is a need for establishing the optimal cell count and isolation methods regarding injured surface area to have better healing outcomes.
SVF mechanism of action
SVF transplantation can have direct (differentiation into other cell types) or indirect (paracrine) effects. SVF could be the differentiation into endothelial cells, keratinocytes or fibroblasts, etc. The paracrine role is crucial for burn healing through modulating growth factors, inflammatory, angiogenic, and fibrosis mediators. This leads to the activation of different signaling pathways. The differentiation capability of cells within SVF is well-documented [8, 18].
Even though lots of researchers investigated the effect of SVF in wound healing, the exact mechanism behind its healing effect remains unclear. Recent research has investigated the mechanisms behind SVF healing properties. Different signaling pathways are activated in animal models in wounded skin samples treated with SVF [7]. During wound healing, dermal fibroblasts play an important role in dermal thickness by activating extracellular matrix synthesis and growth factors. Fibroblast migration and angiogenesis are crucial for providing blood supply to the wound bed. One of the involved factors in vessel contraction is Leiomodin 1, which plays an important role in vasoconstriction. In wound injury, RNA seq analysis revealed that treatment with SVF decreases the mRNA expression of Endothelin1 and Leiomodin 1, thus leading to vasodilation and improving local blood supply in the wound bed. Moreover, immunohistochemical analysis showed higher vascular endothelial growth factor (VEGF) expression in stromal cells post-burn in rats treated with SVF compared to control [5]. This indicates an increase in blood supply to the wound bed, which indicates SVF's role in angiogenesis.
One of the most activated pathways in wound injury treated with SVF was cytokine-cytokine interaction and chemokines [7]. Gene expression analysis revealed that the cytokine-cytokine receptor interaction” pathway is activated post-SVF treatment and upregulated Osm, Ccl4, and Ccr1 gene expressions. The Cytoscape analysis showed an increase in OSM, an IL-6 family protein, which is secreted by macrophages and inhibits the expression of inflammatory cytokines (TNF and IL-1B). Different chemokines are activated after SVF treatment, including CCL2, CCL4, CCL6, CCL7, and CCL9, which attract macrophages to the wound site. Both OSM and chemokines are upregulated by SVF, which chemoattracts macrophages and activates the anti-inflammatory response in the wound site.
Laminins play an important role in re-epithelization and angiogenesis by regulating growth factors that aid in cell adhesion. After treatment with SVF, Lama3, Lamb3, and Lamc3 were upregulated in fibroblasts and endothelial cells in the wound site to promote wound healing [7]. Integrins, transmembrane cell surface receptors that regulate cell adhesion and migration, were found to be upregulated after treatment with SVF, such as a2b, a6, a7, b4, and b7 [7]. Treatment with SVF upregulates gene expression of re-epithelization growth factors, such as EGF, stromal cell-derived factor (SDF-1 or CXCL12), neutrophil-activating protein-2 (NAP-2 or CXCL7) [15]. This shows the role of SVF in regulating the interaction in the extracellular matrix and collagen deposition in wound injury.
It was suggested that both SVF and ADSCs regulate fibroblast and endothelial functions by mediating different signaling pathways that regulate angiogenesis, cell adhesion, collagen deposition, and reducing inflammation in wound injury [7]. It was reported the mechanism of SVF treatment in wounded animal models. However, SVF healing mechanism in the burn was not investigated yet. Further studies are required to fully understand the exact mechanism behind the healing capacity of SVF in burn injury. To our best knowledge, the morphological and histological properties of exosomes isolated from SVF were not studied in burn injury.
Discussion
Thermal burn injury is one of the common health problems globally. A remarkable understanding of the pathophysiology of thermal burn has been achieved so far. Severe burn injury is associated with many complications, including social, functional, and psychological conditions. However, effective treatment of severe burns is still under development. The standard care for severe burn injury is early excision of necrotic tissue and autografting. This treatment minimizes infection hospitalization and reduces hypertrophic scar formation. Standard of care for burn injury is sufficient for superficial, partial- and deep partial-thickness but not for a full-thickness burn with high TBSA. In severe burns with large TBSA, wound closure could delay the healing process, which may increase the risk of infection result in poor aesthetic and functional results. Therefore, interventions are required for best wound closure of severe burn injury.
One of the promising treatments in burn healing is cell therapy. Mesenchymal stem cells from different tissues can be isolated and used for tissue regeneration. Isolation methods, cells’ yield, and application techniques are crucial factors in choosing the best candidates for treating severe burn injury. Several studies have investigated the effect of ADSCs in the burn’s healing process. ADSCs can improve burn healing by reducing scar formation, cell infiltration, and inflammation, increasing angiogenesis, re-epithelization, granulation, and forming hair follicles and sebaceous glands. Different applications have been developed for using ADSCs in severe burn treatment, either alone or combined with other treatments, such as forming scaffolds with several biomaterials. Promising results were reported from treatment with ADSCs when combined with PRP. However, optimal methodology, including the administration route, timing, dose, and duration, should be optimized for better results. The long time needed for ADSCs culture, which might lead to contamination, highlighted the importance of using uncultured SVFs.
The discovery of SVF from adipose tissues evoked their use for the reconstruction of skin tissues. Many reasons favored using SVF, including cell’s heterogeneity, applicability in clinical settings, avoidance of contamination, culturing and ethical issues, reduction of isolation time and cost. SVF is used to amplify the human natural repair and regenerative system by accelerating the number of autologous healing cells into damaged tissues. Autologous stem cells are personalized with a person’s DNA and biological profile. SVF cannot be manufactured since it has four different stem cells (mesenchymal, hematopoietic, endothelial, and pericytic progenitors). In contrast, treatment with one type of stem cells, such as ADSC, contains one type of cells and may or may not be autologous. Moreover, stem cells’ healing properties could be achieved through their differentiation capability and their paracrine effect. Therefore, SVF has several key advantages that favor using it for severe burn injury.
SVF was first isolated using enzymatic methods since they were proven to be effective. However, enzymatic isolation is a time consuming, expensive, requires purification and destroys cell niche. Therefore, research was directed to use mechanical isolation of SVF. The advantage of mechanical isolation is its reliability, simplicity, minimal tissue manipulation, and protection of extracellular matrix and stromal cells. Tonnard was the first to use the term ‘nanofat’ for the mechanical isolation of SVF [98]. Many authors then rejected this term since it is not a fat; it consists of stromal cells obtained from adipose tissues. After that, many terms were used for the mechanical isolation, such as fragmented fat, mechanical stromal cell and total-stromal cells [25]. To our best knowledge, there is no standard methodology or protocols for the mechanical isolation of SVFs. The isolation depends on shifting lipoaspirate between Luer-lock or by adenizing [24]. New automated devices have been invented to isolate SVF from lipoaspirate for clinical applications. They showed reliability for cells’ viability and differentiation.
SVF’s quality could be affected by several factors, such as harvesting site, age, isolation techniques, and health condition. For instance, SVF’s isolation from subcutaneous fat in the abdomen demonstrated the best results when compared to other sites of the body since it has richer soluble factors [43]. In females, cell yields obtained from SVF significantly declined with age [31]. Enzymatic harvesting methods give higher cell yields when compared to the mechanical method. However, the enzymatic method is time-consuming (80 min) compared to the mechanical method (15 min) [88]. All these factors should be considered to choose the best method for patients with severe burn injury. All these factors should be considered to choose the best applications for patients with severe burn injury.
The fat injection has been used in severe burn injury and was found to enhance tissue regeneration and improve scar quality [58]. For SVF feasibility, cellular abundance, multilineage differentiation potential, and heterogeneity, SVF has been investigated for burn injury. SVF enhanced burn healing by stimulating angiogenesis, re-epithelization, and reducing inflammation and scarring. The inconsistency in documented results could be due to the differences in therapeutic dose of cells, in the stage of replication and differentiation and in the isolation procedure of SVF. More research is required to optimize the use of SVF in severe burn injury and to understand the underlying mechanisms behind its healing properties. In animal models, a dose of 10 × 106 cells or more can induce a therapeutic effect on burn healing. Route of administration can be intradermally or subcutaneously. Injection could be in the stasis zone, at the edge or the center of the burn injury. The timing of SVF injection for severe burn injury is crucial and was not consistent in most studies. Some suggested that stem cell quality is better after the resolution of the inflammatory phase [10]. However, others injected SVF directly or within 24–48 h post-burn and healing was improved significantly [83].
Research has revealed the capability of SVF to activate different signaling pathways. SVF accelerates vasodilation mediators to improve the blood supply to the injured tissues, cytokine-cytokine interaction to attract macrophages and reduce inflammation, growth factors that improve adhesion, re-epithelization, and angiogenesis. Further investigation is required to understand the exact mechanism of SVF injection post-injury. Moreover, the role of exosomes in burn injury should be investigated.
Both ADSCs and SVF can be used alone or combined with other biomaterials to develop skin substitutes. Most research has investigated ADSCs effect when combined with other treatments, such as PRP, HA, scaffolds and grafts. However, further investigation is needed to better understand the effect of using SVF alone or combined with other treatments in severe burn injury. SVF therapeutic potential can be enhanced when combined with other biomaterials, such as collagen and PRP. Most studies supported the combined treatment of both SVF and PRP for burn injury [52, 60]. Treatment with SVF and PRP or non-cultured stem cells improved graft function and maintenance in burned patients with facial scars. Combined treatment with both SVF and photobiomodulations enhanced burn healing through increased proliferation and neovascularization in a dose-dependent manner.
The standard care of severe burn injury includes the surgical debridement of necrotic tissues with eschar, which involves the removal of subcutaneous tissues and intact adipose tissues. A new approach of using debrided skin from severe burn as a source of adipose-derived stem cells has been investigated by Natesan [75]. The hypodermal adipose region has viable stem cells that can differentiate into multilineages. When isolated stem cells from debrided skin were used to create scaffolds, they decreased wound contraction and enhanced re-epithelization [101]. This new approach is promising for patients with high TBSA burn and lower donor sites. This approach could be investigated in different experimental clinical settings. In addition, fat-cellular bio-banking should be considered as a treatment option in the future [40].
Treatment with SVF is safe and appropriate in medical intervention because it’s easy to apply and does not cause an allogenic reaction or ethical problems. However, it is difficult to perform it in the emergency setting. Treatment with SVF needs a sterilized surgical room supplied with a centrifuge or automated SVF device which cannot be performed in the clinical setting.
With advances in burn wound treatment, patients’ quality of life will be improved. The majority of patients willing to choose autologous stem cells application for burn injury or other diseases [23]. In massive burn, covering TBSA around 81%, treatment with cultured epithelial autografts showed satisfying results specially in young age patients and with low level of infectious complications. Currently, new techniques have promising therapeutic potential for severe burn injury but need further investigation. Without a standardized procedure for using SVF in severe burn injury, its treatment outcome would not be reliable.
References
Abbas OL, Özatik O, Gönen ZB, Öğüt S, Özatik FY, Salkın H, Musmul A. Comparative analysis of mesenchymal stem cells from bone marrow, adipose tissue, and dental pulp as sources of cell therapy for zone of stasis burns. J Invest Surg. 2019. https://doi.org/10.1080/08941939.2018.1433254.
Alexaki VI, Simantiraki D, Panayiotopoulou M, Rasouli O, Venihaki M, Castana O, Alexakis D, Kampa M, Stathopoulos EN, Castanas E. Adipose tissue-derived mesenchymal cells support skin reepithelialization through secretion of KGF-1 and PDGF-BB: comparison with dermal fibroblasts. Cell Transplant. 2012;21(11):2441–54. https://doi.org/10.3727/096368912X637064.
American Burn Association. Burn Incidence and Treatment in the United States: 2016. Burn Incidence Fact Sheet. 2016.
Anthonissen M, Daly D, Janssens T, Van Den Kerckhove E. The effects of conservative treatments on burn scars: a systematic review. Burns. 2016;42(3):508–18. https://doi.org/10.1016/j.burns.2015.12.006.
Atalay S, Coruh A, Deniz K. Stromal vascular fraction improves deep partial thickness burn wound healing. Burns. 2014;40(7):1375–83. https://doi.org/10.1016/j.burns.2014.01.023.
Bertrand B, Eraud J, Velier M, Cauvin C, Macagno N, Boucekine M, Philandrianos C, Casanova D, Magalon J, Saatier F. Supportive use of platelet-rich plasma and stromal vascular fraction for cell-assisted fat transfer of skin radiation-induced lesions in nude mice. Burns. 2020;46(7):1641–52.
Bi H, Li H, Zhang C, Mao Y, Nie F, Xing Y, Sha W, Wang X, Irwin DM, Tan H. Stromal vascular fraction promotes migration of fibroblasts and angiogenesis through regulation of extracellular matrix in the skin wound healing process. Stem Cell Res Ther. 2019;10(1):1–22. https://doi.org/10.1186/s13287-019-1415-6.
Bourin P, Bunnell BA, Casteilla L, Dominici M, Katz AJ, March KL, Redl H, Rubin JP, Yoshimura K, Gimble JM. Stromal cells from the adipose tissue-derived stromal vascular fraction and culture expanded adipose tissue-derived stromal/stem cells: a joint statement of the International Federation for Adipose Therapeutics and Science (IFATS) and the International So. Cytotherapy. 2013. https://doi.org/10.1016/j.jcyt.2013.02.006.
Burn incidence fact sheet. 2016. American Burn Association. https://ameriburn.org/who-we-are/media/burn-incidence-fact-sheet/
Burt RK, Loh Y, Cohen B, Stefoski D, Balabanov R, Katsamakis G, Oyama Y, Russell EJ, Stern J, Muraro P, Rose J, Testori A, Bucha J, Jovanovic B, Milanetti F, Storek J, Voltarelli JC, Burns WH. Autologous non-myeloablative haemopoietic stem cell transplantation in relapsing-remitting multiple sclerosis: a phase I/II study. Lancet Neurol. 2009, 8(3), pp. 244–53. https://doi.org/10.1016/S1474-4422(09)70017-1. [Erratum. In: Lancet Neurol. 2009;8(4):309].
Bush K, Gertzman AA. Process development and manufacturing of human and animal acellular dermal matrices. Skin Tissue Eng Regen Medi. 2016. https://doi.org/10.1016/B978-0-12-801654-1.00005-X.
Butts CC, Bose K, Frotan MA, Hodge J, Gulati S. Controlling intraoperative hemorrhage during burn surgery: a prospective, randomized trial comparing NuStat® hemostatic dressing to the historic standard of care. Burns. 2017. https://doi.org/10.1016/j.burns.2016.08.026.
Cardoso AL, Bachion MM, de Morais JM, Fantinati MS, De Almeida VLL, Lino Júnior RS. Adipose tissue stromal vascular fraction in the treatment of full thickness burns in rats. Acta Cirurgica Brasileira. 2016;31(9):578–85. https://doi.org/10.1590/S0102-865020160090000002.
Cervelli V, Gentile P, Scioli MG, Grimaldi M, Casciani CU, Spagnoli LG, Orlandi A. Application of platelet-rich plasma in plastic surgery: clinical and in vitro evaluation. Tissue Eng Part C Methods. 2009;15(4):625–34. https://doi.org/10.1089/ten.TEC.2008.0518.
Chae D-S, Han S, Son M, Kim S-W. Stromal vascular fraction shows robust wound healing through high chemotactic and epithelialization property. Cytotherapy. 2017;19(4):543–54. https://doi.org/10.1016/j.jcyt.2017.01.006.
Chan RK, Zamora DO, Wrice NL, Baer DG, Renz EM, Christy RJ, Natesan S. Development of a vascularized skin construct using adipose-derived stem cells from debrided burned skin. Stem Cells Int. 2012;2012: 841203. https://doi.org/10.1155/2012/841203.
Chang YW, Wu YC, Huang SH, Wang HMD, Kuo YR, Lee SS. Autologous and not allogeneic adipose-derived stem cells improve acute burn wound healing. PLoS ONE. 2018;13(5):1–16. https://doi.org/10.1371/journal.pone.0197744.
Chen YW, Scutaru TT, Ghetu N, Carasevici E, Lupascu CD, Ferariu D, Pieptu D, Coman CG, Danciu M. The effects of adipose-derived stem cell-differentiated adipocytes on skin burn wound healing in rats. J Burn Care Res. 2017;38(1):1–10. https://doi.org/10.1097/BCR.0000000000000466.
Cheng C, Sheng L, Li H, Mao X, Zhu M, Gao B, Li Q. Cell-assisted skin grafting: improving texture and elasticity of skin grafts through autologous cell transplantation. Plast Reconstr Surg. 2016;137(1):58e–66e. https://doi.org/10.1097/PRS.0000000000001949.
Choudhry MA, Chaudry IH. Alcohol intoxication and post-burn complications. Front Biosci. 2006. https://doi.org/10.2741/1857.
Chung E, Rybalko VY, Hsieh P-L, Leal SL, Samano MA, Willauer AN, Stowers RS, Natesan S, Zamora DO, Christy RJ, Suggs LJ. Fibrin-based stem cell containing scaffold improves the dynamics of burn wound healing. Wound Repair Regen. 2016;24(5):810–9. https://doi.org/10.1111/wrr.12459.
Cirodde A, Leclerc T, Jault P, Duhamel P, Lataillade JJ, Bargues L. Cultured epithelial autografts in massive burns: a single-center retrospective study with 63 patients. Burns. 2011;37(6):964–72. https://doi.org/10.1016/j.burns.2011.03.011.
Clover AJP, Lane O’Neill B, Kumar AHS. Patient’s attitudes to progenitor cell therapy. Wound Repair Regen. 2012;20(3):311–6. https://doi.org/10.1111/j.1524-475X.2012.00779.x.
Copcu H, Oztan S. New mechanical fat separation technique: ARAT and MEST. Aesthet Surg J Open Forum. 2020. https://doi.org/10.1093/asjof/ojaa035.
Copcu HE, Oztan S. Not stromal vascular fraction (SVF) or nanofat, but total stromal-cells (TOST): a new definition systemic review of mechanical stromal-cell extraction techniques. Tissue Eng Regen Med. 2021;18(1):25–36. https://doi.org/10.1007/s13770-020-00313-0.
de Chaves MEA, de Araújo AR, Piancastelli ACC, Pinotti M. Effects of low-power light therapy on wound healing: LASER x LED. An Bras Dermatol. 2014;89(4):616–23. https://doi.org/10.1590/abd1806-4841.20142519.
de Sousa APC, de Aguiar Valença Neto AAP, Marchionni AMT, de Araújo Ramos M, dos Reis Júnior JA, Pereira MCMC, Cangussú MCT, de Almeida Reis SR, Pinheiro ALB. Effect of LED phototherapy (λ700 ± 20 nm) on TGF-β expression during wound healing: an immunohistochemical study in a rodent model. Photomed Laser Surg. 2011;29(9):605–11. https://doi.org/10.1089/pho.2010.2833.
Doi K, Tanaka S, Iida H, Eto H, Kato H, Aoi N, Kuno S, Hirohi T, Yoshimura K. Stromal vascular fraction isolated from lipo-aspirates using an automated processing system: bench and bed analysis. J Tissue Eng Regen Med. 2013;7(11):864–70. https://doi.org/10.1002/term.1478.
Domergue S, Bony C, Maumus M, Toupet K, Frouin E, Rigau V, Vozenin MC, Magalon G, Jorgensen C, Noël D. Comparison between stromal vascular fraction and adipose mesenchymal stem cells in remodeling hypertrophic scars. PLoS ONE. 2016;11(5):1–16. https://doi.org/10.1371/journal.pone.0156161.
Dong Y, Cui M, Qu J, Wang X, Kwon SH, Barrera J, Elvassore N, Gurtner GC. Conformable hyaluronic acid hydrogel delivers adipose-derived stem cells and promotes regeneration of burn injury. Acta Biomater. 2020;108:56–66. https://doi.org/10.1016/j.actbio.2020.03.040.
Dos-Anjos Vilaboa S, Navarro-Palou M, Llull R. Age influence on stromal vascular fraction cell yield obtained from human lipoaspirates. Cytotherapy. 2014;16(8):1092–7. https://doi.org/10.1016/j.jcyt.2014.02.007.
Ennis WJ, Sui A, Bartholomew A. Stem cells and healing: impact on inflammation. Adv Wound Care. 2013;2(7):369–78. https://doi.org/10.1089/wound.2013.0449.
Evers LH, Bhavsar D, Mailänder P. The biology of burn injury. Exp Dermatol. 2010;19(9):777–83. https://doi.org/10.1111/j.1600-0625.2010.01105.x.
Eyuboglu AA, Uysal CA, Ozgun G, Coskun E, Markal Ertas N, Haberal M. The effect of adipose derived stromal vascular fraction on stasis zone in an experimental burn model. Burns. 2018;44(2):386–96. https://doi.org/10.1016/j.burns.2017.08.016.
Feng C-J, Lin C-H, Tsai C-H, Yang I-C, Ma H. Adipose-derived stem cells-induced burn wound healing and regeneration of skin appendages in a novel skin island rat model. J Chin Med Assoc: JCMA. 2019;82(8):635–42. https://doi.org/10.1097/JCMA.0000000000000134.
Foubert P, Barillas S, Gonzalez AD, Alfonso Z, Zhao S, Hakim I, Meschter C, Tenenhaus M, Fraser JK. Uncultured adipose-derived regenerative cells (ADRCs) seeded in collagen scaffold improves dermal regeneration, enhancing early vascularization and structural organization following thermal burns. Burns. 2015;41(7):1504–16. https://doi.org/10.1016/j.burns.2015.05.004.
Foubert P, Liu M, Anderson S, Rajoria R, Gutierrez D, Zafra D, Tenenhaus M, Fraser JK. Preclinical assessment of safety and efficacy of intravenous delivery of autologous adipose-derived regenerative cells (ADRCs) in the treatment of severe thermal burns using a porcine model. Burns. 2018;44(6):1531–42. https://doi.org/10.1016/j.burns.2018.05.006.
Franck CL, Senegaglia AC, Leite LMB, De Moura SAB, Francisco NF, Ribas Filho JM. Influence of adipose tissue-derived stem cells on the burn wound healing process. Stem Cells Int. 2019. https://doi.org/10.1155/2019/2340725.
Fujiwara O, Prasai A, Perez-Bello D, El Ayadi A, Petrov IY, Esenaliev RO, Petrov Y, Herndon DN, Finnerty CC, Prough DS, Enkhbaatar P. Adipose-derived stem cells improve grafted burn wound healing by promoting wound bed blood flow. Burns Trauma. 2020;8:tkaa009. https://doi.org/10.1093/burnst/tkaa009.
Gentile P, Garcovich S. Systematic review-the potential implications of different platelet-rich plasma (PRP) concentrations in regenerative medicine for tissue repair. Int J Mol Sci. 2020;21(16):5702. https://doi.org/10.3390/ijms21165702.
Gentile P, De Angelis B, Pasin M, Cervelli G, Curcio CB, Floris M, Di Pasquali C, Bocchini I, Balzani A, Nicoli F, Insalaco C, Tati E, Lucarini L, Palla L, Pascali M, De Logu P, Di Segni C, Bottini DJ, Cervelli V. Adipose-derived stromal vascular fraction cells and platelet-rich plasma: basic and clinical evaluation for cell-based therapies in patients with scars on the face. J Craniofac Surg. 2014;25(1):267–72. https://doi.org/10.1097/01.scs.0000436746.21031.ba.
Giudice G, Filoni A, Maggio G, et al. Use of the stromal vascular fraction in intermediate-deep acute burns: a case with its own control. J Burn Care Res. 2018;39(5):846–9.
Grasys J, Kim B-S, Pallua N. Content of soluble factors and characteristics of stromal vascular fraction cells in lipoaspirates from different subcutaneous adipose tissue depots. Aesthet Surg J. 2016;36(7):831–41. https://doi.org/10.1093/asj/sjw022.
Han Y, Bai Y, Yan X-L, Ren J, Zeng Q, Li X-D, Pei X-T, Han Y. Co-transplantation of exosomes derived from hypoxia-preconditioned adipose mesenchymal stem cells promotes neovascularization and graft survival in fat grafting. Biochem Biophys Res Commun. 2018;497(1):305–12. https://doi.org/10.1016/j.bbrc.2018.02.076.
He L, Zhu C, Jia J, Hao X-Y, Yu X-Y, Liu X-Y, Shu M-G. ADSC-Exos containing MALAT1 promotes wound healing by targeting miR-124 through activating Wnt/β-catenin pathway. 2020. Biosci Rep. https://doi.org/10.1042/BSR20192549.
Hernon CA, Dawson RA, Freedlander E, Short R, Haddow DB, Brotherston M, MacNeil S. Clinical experience using cultured epithelial autografts leads to an alternative methodology for transferring skin cells from the laboratory to the patient. Regen Med. 2006;1(6):809–21. https://doi.org/10.2217/17460751.1.6.809.
Hettiaratchy S, Dziewulski P. Pathophysiology and types of burns. BMJ. 2004;328(7453):1427. https://doi.org/10.1136/bmj.328.7453.1427.
Jackson DM (1953) The diagnosis of the depth of burning. Br J Surg 40:588–596
Jeschke MG, Gauglitz GG, Kulp GA, Finnerty CC, Williams FN, Kraft R, Suman OE, Mlcak RP, Herndon DN. Long-term persistance of the pathophysiologic response to severe burn injury. PLoS ONE. 2011. https://doi.org/10.1371/journal.pone.0021245.
Jewo PI, Fadeyibi IO. Progress in burns research: a review of advances in burn pathophysiology. Ann Burns Fire Disasters 2015;28(2):105–115. http://www.ncbi.nlm.nih.gov/pubmed/27252608%0A. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC4837486
Jia W, Hu D, Wang H, Chen D, Bai X, Li N, Han F, Fang X, Yang L. Effects of mouse adipose-derived stem cell conditioned medium on the apoptosis of keratinocytes induced by thermal injury in vitro. Chin J Burns. 2014. https://doi.org/10.3760/cma.j.issn.1009-2587.2014.02.003.
Josh F, Soekamto TH, Adriani JR, Jonatan B, Mizuno H, Faruk M. The combination of stromal vascular fraction cells and platelet-rich plasma reduces malondialdehyde and nitric oxide levels in deep dermal burn injury. J Inflamm Res. 2021;14(June):3049–61. https://doi.org/10.2147/JIR.S318055.
Karakol P, Bozkurt M, Gelbal C, Tuglu MI. Efficacy of stromal vascular fraction and enzyme-free mechanical isolation therapy in experimental full thickness burn wounds. J Plast Surg Hand Surg. 2021. https://doi.org/10.1080/2000656X.2021.1993234.
Karina, Samudra MF, Rosadi I, Afini I, Widyastuti T, Sobariah S, Remelia M, Puspitasari RL, Rosliana I, Tunggadewi TI. Combination of the stromal vascular fraction and platelet-rich plasma accelerates the wound healing process: pre-clinical study in a Sprague-Dawley rat model. Stem Cell Investig. 2019;6:1–8. https://doi.org/10.21037/sci.2019.06.08.
Kaushik P, Sharma S, Rana A, Kaushik D, Kamboj S. Burn wound: Pathophysiology and its management by herbal plants. Chron Young Sci. 2013;4(2):86. https://doi.org/10.4103/2229-5186.115537.
Khan I, Rahman SU, Tang E, Engel K, Hall B, Kulkarni AB, Arany PR. Accelerated burn wound healing with photobiomodulation therapy involves activation of endogenous latent TGF-β1. Sci Rep. 2021;11(1):13371. https://doi.org/10.1038/s41598-021-92650-w.
Klar AS, Zimoch J, Biedermann T. Skin tissue engineering: application of adipose-derived stem cells. Biomed Res Int. 2017;2017:9747010. https://doi.org/10.1155/2017/9747010.
Klinger M, Marazzi M, Vigo D, Torre M. Fat injection for cases of severe burn outcomes: a new perspective of scar remodeling and reduction. Aesthet Plast Surg. 2020;44(4):1278–82. https://doi.org/10.1007/s00266-020-01813-z.
Laidding SR, Josh F, Battung S, Bukhari A, Warsinggih, Patellongi IJ, Massi MN, Islam AA, Dososaputro I, Faruk M. Combination of platelet rich plasma and stromal vascular fraction on the level of vascular endothelial growth factor in rat subjects experiencing deep dermal burn injury. Ann Med Surg. 2012;64:102254. https://doi.org/10.1016/j.amsu.2021.102254.
Laidding SR, Josh F, Francisca, Faruk M, Palissei AS, Satria B, Warsinggih, Bukhari A, Massi MN, Islam AA. Combination of platelet-rich plasma and stromal vascular fraction on the level of transforming growth factor-β in rat subjects experiencing deep dermal burn injury. Ann Med Surg. 2020;60(November):737–42. https://doi.org/10.1016/j.amsu.2020.11.088.
Lalu MM, McIntyre L, Pugliese C, Fergusson D, Winston BW, Marshall JC, Granton J, Stewart DJ. Safety of cell therapy with mesenchymal stromal cells (SafeCell): a systematic review and meta-analysis of clinical trials. PLoS ONE. 2012. https://doi.org/10.1371/journal.pone.0047559.
Lamaro-Cardoso A, Bachion MM, Morais JM, Fantinati MS, Milhomem AC, Almeida VL, Vinaud MC, Lino-Júnior RS. Photobiomodulation associated to cellular therapy improve wound healing of experimental full thickness burn wounds in rats. J Photochem Photobiol B Biol. 2019;194:174–82. https://doi.org/10.1016/j.jphotobiol.2019.04.003.
Langton AK, Herrick SE, Headon DJ. An extended epidermal response heals cutaneous wounds in the absence of a hair follicle stem cell contribution. J Investig Dermatol. 2008;128(5):1311–8. https://doi.org/10.1038/sj.jid.5701178.
Leonardi D, Oberdoerfer D, Fernandes MC, Meurer RT, Pereira-Filho GA, Cruz P, Vargas M, Chem RC, Camassola M, Nardi NB. Mesenchymal stem cells combined with an artificial dermal substitute improve repair in full-thickness skin wounds. Burns. 2012;38(8):1143–50. https://doi.org/10.1016/j.burns.2012.07.028.
Loder S, Peterson JR, Agarwal S, Eboda O, Brownley C, Delarosa S, Ranganathan K, Cederna P, Wang SC, Levi B. Wound healing after thermal injury is improved by fat and adipose-derived stem cell isografts. J Burn Care Res. 2015. https://doi.org/10.1097/BCR.0000000000000160.
Lu T-Y, Yu K-F, Kuo S-H, Cheng N-C, Chuang E-Y, Yu J-S. Enzyme-crosslinked gelatin hydrogel with adipose-derived stem cell spheroid facilitating wound repair in the murine burn model. Polymers. 2020;12(12):2997. https://doi.org/10.3390/polym12122997.
Ma T, Fu B, Yang X, Xiao Y, Pan M. Adipose mesenchymal stem cell-derived exosomes promote cell proliferation, migration, and inhibit cell apoptosis via Wnt/β-catenin signaling in cutaneous wound healing. J Cell Biochem. 2019;120(6):10847–54. https://doi.org/10.1002/jcb.28376.
Maass DL, Hybki DP, White J, Horton JW. The time course of cardiac Nf-κB activation and TNF-α secretion by cardiac myocytes after burn injury: Contribution to burn-related cardiac contractile dysfunction. Shock. 2002;17(4):293–9. https://doi.org/10.1097/00024382-200204000-00009.
Machula H, Ensley B, Kellar R. Electrospun tropoelastin for delivery of therapeutic adipose-derived stem cells to full-thickness dermal wounds. Adv Wound Care. 2014;3(5):367–75. https://doi.org/10.1089/wound.2013.0513.
Mahmood R, Mehmood A, Choudhery MS, Awan SJ, Khan SN, Riazuddin S. Human neonatal stem cell-derived skin substitute improves healing of severe burn wounds in a rat model. Cell Biol Int. 2019;43(2):147–57. https://doi.org/10.1002/cbin.11072.
Mansoub NH, Gürdal M, Karadadas E, Kabadayi H, Vatansever S, Ercan G. The role of PRP and adipose tissue-derived keratinocytes on burn wound healing in diabetic rats. BioImpacts. 2018;8(1):5–12. https://doi.org/10.15171/bi.2018.02.
Matsumoto D, Sato K, Gonda K, Takaki Y, Shigeura T, Sato T, Aiba-Kojima E, Iizuka F, Inoue K, Suga H, Yoshimura K. Cell-assisted lipotransfer: supportive use of human adipose-derived cells for soft tissue augmentation with lipoinjection. Tissue Eng. 2006;12(12):3375–82. https://doi.org/10.1089/ten.2006.12.3375.
Mazini L, Rochette L, Hamdan Y, Malka G. Skin immunomodulation during regeneration: emerging new targets. J Pers Med. 2021;11(2):85. https://doi.org/10.3390/jpm11020085.
Monfort A, Soriano-Navarro M, García-Verdugo JM, Izeta A. Production of human tissue-engineered skin trilayer on a plasma-based hypodermis. J Tissue Eng Regen Med. 2013;7(6):479–90. https://doi.org/10.1002/term.548.
Natesan S, Wrice NL, Baer DG, Christy RJ. Debrided skin as a source of autologous stem cells for wound repair. Stem Cells. 2011;29(8):1219–30. https://doi.org/10.1002/stem.677.
Natesan S, Zamora DO, Wrice NL, Baer DG, Christy RJ. Bilayer hydrogel with autologous stem cells derived from debrided human burn skin for improved skin regeneration. J Burn Care Res. 2013;34(1):18–30. https://doi.org/10.1097/BCR.0b013e3182642c0e.
Nie C, Yang D, Xu J, Si Z, Jin X, Zhang J. Locally administered Adipose-derived stem cells accelerate wound healing through differentiation and vasculogenesis. Cell Transplant. 2011;20(2):205–16. https://doi.org/10.3727/096368910X520065.
Nielson CB, Duethman NC, Howard JM, Moncure M, Wood JG. Burns: pathophysiology of systemic complications and current management. J Burn Care Res. 2017;38(1):e469–81. https://doi.org/10.1097/BCR.0000000000000355.
Nishiwaki K, Aoki S, Kinoshita M, Kiyosawa T, Suematsu Y, Takeoka S, Fujie T. In situ transplantation of adipose tissue-derived stem cells organized on porous polymer nanosheets for murine skin defects. J Biomed Mater Res B Appl Biomater. 2019;107(5):1363–71. https://doi.org/10.1002/jbm.b.34228.
Nowak TJ. Burn pathophysiology. Perioper Nurs Clin. 2012;7(1):9–17. https://doi.org/10.1016/j.cpen.2011.10.003.
Onur Erol O, Agaoglu G, Jawad MA. Combined non-ablative laser and microfat grafting for burn scar treatment. Aesthet Surg J. 2019;39(4):NP55–67. https://doi.org/10.1093/asj/sjy291.
Oryan A, Alemzadeh E, Moshiri A. Biological properties and therapeutic activities of honey in wound healing: a narrative review and meta-analysis. J Tissue Viability. 2016. https://doi.org/10.1016/j.jtv.2015.12.002.
Prasai A, El Ayadi A, Mifflin RC, Wetzel MD, Andersen CR, Redl H, Herndon DN, Finnerty CC. Characterization of adipose-derived stem cells following burn injury. Stem Cell Rev Rep. 2017;13(6):781–92. https://doi.org/10.1007/s12015-017-9721-9.
Priglinger E, Maier J, Chaudary S, Lindner C, Wurzer C, Rieger S, Redl H, Wolbank S, Dungel P. Photobiomodulation of freshly isolated human adipose tissue-derived stromal vascular fraction cells by pulsed light-emitting diodes for direct clinical application. J Tissue Eng Regen Med. 2018;12(6):1352–62. https://doi.org/10.1002/term.2665.
Qian L, Pi L, Fang B-R, Meng X-X. Adipose mesenchymal stem cell-derived exosomes accelerate skin wound healing via the lncRNA H19/miR-19b/SOX9 axis. Lab Invest. 2021;101(9):1254–66. https://doi.org/10.1038/s41374-021-00611-8.
Rae L, Fidler P, Gibran N. The physiologic basis of burn shock and the need for aggressive fluid resuscitation. Crit Care Clin. 2016;32(4):491–505. https://doi.org/10.1016/j.ccc.2016.06.001.
Räntfors J, Cassuto J. Role of histamine receptors in the regulation of edema and circulation postburn. Burns. 2003;29(8):769–77. https://doi.org/10.1016/S0305-4179(03)00203-1.
Raposio E, Simonacci F, Perrotta RE. Adipose-derived stem cells: Comparison between two methods of isolation for clinical applications. Ann Med Surg. 2017;2012(20):87–91. https://doi.org/10.1016/j.amsu.2017.07.018.
Rasmussen BS, Sørensen CL, Vester-Glowinski PV, Herly M, Kurbegovic S, Ørholt M, Svalgaard JD, Kølle S-FT, Kristensen AT, Talman M-LM, Drzewiecki KT, Fischer-Nielsen A. A novel porcine model for future studies of cell-enriched fat grafting. Plast Reconstr Surg Glob Open. 2018;6(4): e1735. https://doi.org/10.1097/GOX.0000000000001735.
Sazegar G, Hosseini SRA, Behravan E. The effects of supplemental zinc and honey on wound healing in rats. Iran J Basic Med Sci. 2011. https://doi.org/10.22038/ijbms.2011.5029.
Shpichka A, Butnaru D, Bezrukov EA, Sukhanov RB, Atala A, Burdukovskii V, Zhang Y, Timashev P. Skin tissue regeneration for burn injury. Stem Cell Res Ther. 2019;10(1):1–16. https://doi.org/10.1186/s13287-019-1203-3.
Skardal A, Mack D, Kapetanovic E, Atala A, Jackson JD, Yoo J, Soker S. Bioprinted amniotic fluid-derived stem cells accelerate healing of large skin wounds. Stem Cells Transl Med. 2012;1(11):792–802. https://doi.org/10.5966/sctm.2012-0088
Stachura A, Paskal W, Pawlik W, Mazurek MJ, Jaworowski J. The use of adipose-derived stem cells (ADSCs) and stromal vascular fraction (SVF) in skin scar treatment-a systematic review of clinical studies. J Clin Med. 2021;10(16):3637. https://doi.org/10.3390/jcm10163637.
Stekelenburg CM, Simons JM, Tuinebreijer WE, van Zuijlen PPM. Analyzing contraction of full thickness skin grafts in time: choosing the donor site does matter. Burns. 2016. https://doi.org/10.1016/j.burns.2016.02.001.
Stone R, Natesan S, Kowalczewski CJ, Mangum LH, Clay NE, Clohessy RM, Carlsson AH, Tassin DH, Chan RK, Rizzo JA, Christy RJ. Advancements in regenerative strategies through the continuum of burn care. Front Pharmacol. 2018. https://doi.org/10.3389/fphar.2018.00672.
Sultan SM, Barr JS, Butala P, Davidson EH, Weinstein AL, Knobel D, Saadeh PB, Warren SM, Coleman SR, Hazen A. Fat grafting accelerates revascularisation and decreases fibrosis following thermal injury. J Plast Reconstr Aesthet Surg. 2012;65(2):219–27. https://doi.org/10.1016/j.bjps.2011.08.046.
Sun M, He Y, Zhou T, Zhang P, Gao J, Lu F. Adipose extracellular matrix/stromal vascular fraction gel secretes angiogenic factors and enhances skin wound healing in a murine model. Biomed Res Int. 2017. https://doi.org/10.1155/2017/3105780.
Tonnard P, Verpaele A, Peeters G, Hamdi M, Cornelissen M, Declercq H. Nanofat grafting: basic research and clinical applications. Plast Reconstr Surg. 2013;132(4):1017–26. https://doi.org/10.1097/PRS.0b013e31829fe1b0.
Trivisonno A, Alexander RW, Baldari S, Cohen SR, Di Rocco G, Gentile P, Magalon G, Magalon J, Miller RB, Womack H, Toietta G. Intraoperative strategies for minimal manipulation of autologous adipose tissue for cell- and tissue-based therapies: concise review. Stem Cells Transl Med. 2019;8(12):1265–71. https://doi.org/10.1002/sctm.19-0166.
Trottier V, Marceau-Fortier G, Germain L, Vincent C, Fradette J. IFATS collection: using human adipose-derived stem/stromal cells for the production of new skin substitutes. Stem Cells. 2008;26(10):2713–23. https://doi.org/10.1634/stemcells.2008-0031.
van der Veen VC, Vlig M, van Milligen FJ, de Vries SI, Middelkoop E, Ulrich MMW. Stem cells in burn eschar. Cell Transplant. 2012;21(5):933–42. https://doi.org/10.3727/096368911X600993.
Vaughn L, Beckel N. Severe burn injury, burn shock, and smoke inhalation injury in small animals. Part 1: Burn classification and pathophysiology. J Vet Emerg Crit Care. 2012;22(2):179–86. https://doi.org/10.1111/j.1476-4431.2012.00727.x.
Wood FM, Kolybaba ML, Allen P. The use of cultured epithelial autograft in the treatment of major burn injuries: a critical review of the literature. Burns. 2006;32(4):395–401. https://doi.org/10.1016/j.burns.2006.01.008.
Wurzer P, Keil H, Branski LK, Parvizi D, Clayton RP, Finnerty CC, Herndon DN, Kamolz LP. The use of skin substitutes and burn care—a survey. J Surg Res. 2016;201(2):293–8. https://doi.org/10.1016/j.jss.2015.10.048.
Yanaga H, Udoh Y, Yamauchi T, Yamamoto M, Kiyokawa K, Inoue Y, Tai Y. Cryopreserved cultured epidermal allografts achieved early closure of wounds and reduced scar formation in deep partial-thickness burn wounds (DDB) and split-thickness skin donor sites of pediatric patients. Burns. 2001;27(7):689–98. https://doi.org/10.1016/S0305-4179(01)00008-0.
Yastı AÇ, Akgün AE, Akın M. Use of stromal vascular fraction stem cell therapy for functional and cosmetic outcomes in a young female patient with deep dermal flame burns on the face. Burns Open. 2022;6(3):116–9. https://doi.org/10.1016/j.burnso.2022.03.005.
Zahorec P, Sarkozyova N, Ferancikova N, Bukovcan P, Danisovic L, Bohac M, Tomas M, Koller J. Autologous mesenchymal stem cells application in post-burn scars treatment: a preliminary study. Cell Tissue Banking. 2021;22(1):39–46. https://doi.org/10.1007/s10561-020-09862-z.
Zhang W, Bai X, Zhao B, Li Y, Zhang Y, Li Z, Wang X, Luo L, Han F, Zhang J, Han S, Cai W, Su L, Tao K, Shi J, Hu D. Cell-free therapy based on adipose tissue stem cell-derived exosomes promotes wound healing via the PI3K/Akt signaling pathway. Exp Cell Res. 2018;370(2):333–42. https://doi.org/10.1016/j.yexcr.2018.06.035.
Zhou X, Ning K, Ling B, Chen X, Cheng H, Lu B, Gao Z, Xu J. Multiple injections of autologous adipose-derived stem cells accelerate the burn wound healing process and promote blood vessel regeneration in a rat model. Stem Cells Dev. 2019;28(21):1463–72. https://doi.org/10.1089/scd.2019.0113.
Zuo KJ, Medina A, Tredget EE. Important developments in burn care. Plast Reconstr Surg. 2017. https://doi.org/10.1097/PRS.0000000000002908.
Acknowledgements
The author acknowledges the contributions of University of Jeddah.
Author information
Authors and Affiliations
Contributions
Severe burn is a global incidental injury. The mechanism behind it is well-known. However, treatment options need to be developed for better results. This review presented the advantages and disadvantages of available treatments. Recently, SVF has been used clinically as a therapeutic option for severe burn injury showing promising results in both human and animal models. However, the mechanism behind its effect still needs to be discovered.
Corresponding author
Ethics declarations
Conflict of interest
The author declare that they have no competing interests of any commercial or financial relationships.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fakiha, K. Adipose stromal vascular fraction: a promising treatment for severe burn injury. Human Cell 35, 1323–1337 (2022). https://doi.org/10.1007/s13577-022-00743-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13577-022-00743-z