Abstract
To determine the prevalence of microvascular complications and associated risk factors among subjects with type 2 diabetes reported at a tertiary care unit of Karachi, Pakistan. This retrospective observational study was carried out in the outpatient department of Baqai Institute of Diabetology and Endocrinology (BIDE), a tertiary care diabetes center of Karachi from January 2005 to April 2016. Data records of patients with type 2 diabetes at presentation were analyzed. Selected data was extracted from Health Management System (HMS) including basic demographics, anthropometric measurements, biochemical results, medical information, and microvascular complications results. Data analysis was performed on Statistical Package for Social Sciences (SPSS) version 20.0. Overall, prevalence of at least one microvascular complication was 56.9%, retinopathy 15.8%, nephropathy 31.0%, and neuropathy 48.7% were noted. Male gender, age ≥ 40 years, duration of diabetes > 10 years, obesity, hypertension, HbA1c > 7%, and low HDL were found to be significant risk factors for microvascular complication. Hypertriglyceridemia and hypercholesterolemia were significantly associated with nephropathy and neuropathy, whereas no significant association of high LDL was found with any complication. High prevalence of microvascular complications was observed among type 2 diabetic subjects visited first time at a tertiary care hospital. Early identification and effective management are required at primary and secondary care levels to combat this situation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
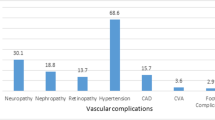
Diabetes mellitus is an important global health issue as the number of people with diabetes are rising every year, particularly of type 2 diabetes [1]. Pakistan had an estimated population of 7.5 million diabetics as of 2017, and this population is predicted to near 16.1 million in 2045 [2]. The recent National diabetes survey of Pakistan is just completed and reports are sent for publication. People with type 2 diabetes mellitus have a considerably higher risk of both macrovascular complications (peripheral vascular disease, coronary artery disease, and cerebrovascular disease) and microvascular complications (nephropathy, neuropathy, and retinopathy) [3]. These complications result in significantly high morbidity and mortality. People with long duration of diabetes or uncontrolled disease are usually affected by microvascular complications. However, the complications can already be present at the time of diagnosis [4].
The increasing trend in the prevalence of microvascular complications of type 2 diabetes has been observed in various epidemiological studies [5,6,7,8]. Joint Asia Diabetes Evaluation (JADE) reported that in seven countries of Asia, retinopathy, neuropathy, and nephropathy affected 20.4, 15.0, and 7.5% of diabetic subjects, respectively [9]. Previous studies identified that the prevalence of microvascular complications was more common in Asians as compared to Europeans [10, 11] and Caucasians [8]. Data on prevalence rate of microvascular complications in Pakistan is scarce. However, a few small hospital-based studies highlighted high prevalence of microvascular complications ranged from 12 to 31% for retinopathy, 28 to 56% for nephropathy, and 36 to 68% for neuropathy [12,13,14,15,16,17]. The issue of rising type 2 diabetes in young individuals makes it significantly more important to identify and treat the disease earlier as the long-term microvascular complications are related with hyperglycemia and duration of the disease. Thus, the present study aims to assess the prevalence of microvascular complications and associated risk factors among subjects with type 2 diabetes reported at a tertiary care unit of Karachi, Pakistan.
Methodology
This retrospective study was conducted at Baqai Institute of Diabetology and Endocrinology (BIDE). Ethical approval for the study was obtained from the institutional review board (IRB) of BIDE. For this study, data records of the first visit of type 2 diabetic subjects (the time when the patient first consulted our institute for management) who attended outpatient department (OPD) of the institute from January 2005 to April 2016 were analyzed without any breach of confidentiality. Subjects of type 1 diabetes and gestational diabetes were not included in the study. Data obtained from computerized hospital management system (HMS) included risk factors of diabetes along with its microvascular complications. For screening of diabetic retinopathy, fundus was examined using Vista 20 direct ophthalmoscope by a diabetologist. The retinopathy was classified as normal background (presence of microdots and hard exudates), pre-proliferative and proliferative (presence of soft exudates and new vessels), or maculopathy [12, 13]. It also included subjects who had prior laser photocoagulation for diabetic retinopathy. Peripheral neuropathy was defined as absent touch or vibratory sensations of the feet. Touch sensation was assessed by 10 g monofilament and vibration sensation by 128 Hz tuning fork [12, 13]. Nephropathy was classified as protein > 1 plus on dipstick (Combur 10, Rouche Diagnostics) with no other abnormal findings on urinary examination [12, 13]. In case of urine dipstick negative, microalbuminuria was done by quantitative analysis. A result of more than 30 mg on at least two consecutive occasions is considered as positive for nephropathy [13].
Biochemical parameters were measured by standard laboratory test methods. A triglyceride > 150 mg/dl was considered to be hypertriglyceridemia. LDL cholesterol concentration was stated to be abnormal if it was > 100 mg/dl. Low HDL was considered at < 40 mg/dl for male and < 50 mg/dl for female. Hypercholesterolemia was defined as cholesterol over 160 mg/dl [18, 19].
HbA1c value of ≤ 7% and > 7% were taken as good and poor control. Body mass index (BMI) was calculated by the standard formula and obesity was taken as BMI > 25 kg/m2 [12, 13].
Statistical analysis
Descriptive analysis included the estimation of mean values and standard deviations for continuous variables. Prevalence or frequencies were expressed in terms of percentage. The Student’s t-test (for continuous variables) and chi-square test (for categorical variables) were employed to compare differences among the subgroups of the population. Association between microvascular complications and risk factors were examined using logistic regression. Variables significant at p value ≤ 0.25 in an initial univariate regression analysis were entered in a multiple regression model. Backward stepwise regression analysis was undertaken for model building. Odd ratios and 95% confidence interval were generated as a measure of association. The level of significance was set at p value < 0.05. All descriptive and comparative analyses were conducted in SPSS version 20.
Results
A total of 28,601 type 2 diabetic subjects were included in the study. Among them, 56.9% subjects had at least one microvascular complication. Subjects with microvascular complications were older than subjects without microvascular complication (54.4 ± 11.1 vs 50.1 ± 11.1 years) with longer duration of diabetes (9.8 ± 7.7 vs 6.0 ± 6.0 years) and increased BMI (28.3 ± 5.2 vs 27.8 ± 5.6 kg/m2). Significant differences were found between the groups in biochemical parameters except for triglycerides (Table 1).
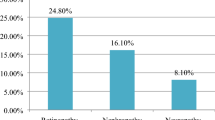
Figure 1 showed prevalence of various microvascular complications. Among the studied subjects, 15.8% had retinopathy, 31% had nephropathy, and 48.7% had neuropathy. High prevalence of all three microvascular complications was seen in subjects of older age and subjects who had poor glycemic control and longer duration of diabetes (Table 2).
Table 3 shows the results of univariate regression analysis demonstrating relationship between microvascular complications and their risk factors. Significant differences were observed between all the risk factors and microvascular complications except retinopathy which was not significantly associated with components of dyslipidemia.
Potential risk factors which were significantly associated in univariate analysis were considered for inclusion in a multivariate logistic regression analysis. In multivariate analysis, the risk factors for having at least one microvascular complication were found to be male gender, age ≥ 40 years, duration of diabetes > 10 years, obesity, hypertension, HbA1c > 7%, and low high-density lipoprotein.
Nephropathy was found to be significantly associated with male gender, duration of diabetes > 10 years, hypertension, hbA1c > 7%, hypercholesterolemia, and low high-density lipoprotein. Additionally, male gender, age > 40 years, duration of diabetes > 10 years, obesity, hypertension, and HbA1c > 7% were found to be significant predictors of developing retinopathy. Moreover, it was observed that presence of neuropathy was associated with male gender, age ≥ 40 years, duration of diabetes > 10 years, obesity, hypertension, HbA1c > 7%, hypercholesterolemia, hypertriglyceridemia, and low HDL (Table 4).
Discussion
The present study analyzed the microvascular complication profile of T2DM subjects at presentation for the first time attending a tertiary care unit of Karachi, Pakistan. The occurrence of any one of the microvascular complications in this study was 56.9% which was comparable to a study by Santos AD et al. in which they observed microvascular complications in 53.8% of type 2 diabetics [20]. Current study observed similar prevalence of microvascular complications as reported by us from the same tertiary care unit 13 years back except for neuropathy which is slightly higher as compared to previous one [12, 14,15,16]. According to our findings, neuropathy was the most common complication as compared to other complications. Similar outcomes were observed in previous studies from India and other countries from the region [21, 22]. However, some studies conducted in Hong Kong, Jammu and Kashmir, India reported nephropathy as the most common microvascular complication [23, 24].
Retinopathy seems to be the least common microvascular complication in this study population, and the findings are consistent with the earlier study done in Faisalabad, Pakistan [25]. In contrast, a study by Sohail observed higher prevalence of retinopathy (56.9%) among Pakistani individuals [26]. More sensitive screening tool along with the involvement of a trained ophthalmologist could have a better screening result for future studies.
Poor glycemic control, hypertension, gender, and longer duration of diabetes were found to be prominent risk factors of microvascular complications in this study. Comparable findings have been recorded where these factors were reported as contributing factors in progression of microvascular complications [7, 16, 27,28,29].
Results of the present study provide evidence that older people were at greater risk for the development of diabetes complications particularly retinopathy and neuropathy as reported by other researchers [5, 28, 30, 31]. Previous studies examined positive relationship between obesity and microvascular complications in type 2 diabetes [32, 33]. Similar outcomes were observed in current study. Previously, it was well defined that dyslipidemia causes risk of developing microvascular complications [5, 28, 34]. Our findings also showed significant association of hypercholesterolemia, hypertriglyceridemia, and low HDL with neuropathy and nephropathy. In contrast, no significant association of LDL cholesterol was found with any microvascular complication.
Limitations of this study include its retrospective design focusing only microvascular complications. Another limitation was the diagnosis of retinopathy, based on fundoscopy instead of using more sensitive screening tool like fundal photography. Additionally, it was single tertiary care center-based study and not a community survey as prevalence of diabetic complications may vary in a community-based survey.
Conclusion
High prevalence of microvascular complications was observed among type 2 diabetic subjects who visited for the first time in a tertiary care hospital. Male gender, age ≥ 40 years, duration of diabetes > 10 years, obesity, hypertension, HbA1c > 7%, and low HDL were strongly associated with any type of microvascular complication. These outcomes need to be validated by multicentered or larger-scale community-based studies. Early identification and effective management are required at primary and secondary care levels to combat this situation.
References
Zimmet PZ. Diabetes and its drivers: the largest epidemic in human history? Clin Diabetes Endocrinol. 2017;3(1):1. https://doi.org/10.1186/s40842-016-0039-3
International Diabetes Federation. IDF Atlas. 8th edition. retrieved from: http://www.diabetesatlas.org. (last accessed: Feb 2018).
Abougalambou SS, Hassali MA, Sulaiman SA, Abougalambou AS. Prevalence of vascular complications among type 2 diabetes mellitus outpatients at teaching hospital in Malaysia. J Diabetes Metab. 2011;2(115):1–4. https://doi.org/10.4172/2155-6156.1000115.
Valencia WM, Florez H. How to prevent the microvascular complications of type 2 diabetes beyond glucose control. BMJ. 2017;356:i6505. https://doi.org/10.1136/bmj.i6505.
Agrawal R, Ola V, Bishnoi P, Gothwal S, Sirohi P, Agrawal R. Prevalence of micro and macrovascular complications and their risk factors in type-2 diabetes mellitus. JAPI. 2014;62:505.
Alaboud AF, Tourkmani AM, Alharbi TJ, Alobikan AH, Abdelhay O, Al Batal SM, et al. Microvascular and macrovascular complications of type 2 diabetic mellitus in central, Kingdom of Saudi Arabia. Saudi Med J. 2016;37(12):1408. https://doi.org/10.15537/smj.2016.12.17062.
Yokoyama H, Oishi M, Takamura H, Yamasaki K, Shirabe SI, Uchida D, et al. Large-scale survey of rates of achieving targets for blood glucose, blood pressure, and lipids and prevalence of complications in type 2 diabetes (JDDM 40). BMJ Open Diabetes Res Care. 2016;4(1):e000294. https://doi.org/10.1136/bmjdrc-2016-000294.
Rhee EJ. Diabetes in Asians. Endocrinol Metab. 2015;30(3):263–9.
So WY, Raboca J, Sobrepena L, Yoon KH, Deerochanawong C, Ho LT, et al. Comprehensive risk assessments of diabetic patients from seven Asian countries: the Joint Asia Diabetes Evaluation (JADE) program. J Diabetes. 2011;3(2):109–18. https://doi.org/10.1111/j.1753-0407.2011.00115.x.
Shah AD, Kandula NR, Lin F, Allison MA, Carr J, Herrington D, et al. Less favorable body composition and adipokines in south Asians compared with other US ethnic groups: results from the MASALA and MESA studies. Int J Obes. 2016;40(4):639–45. https://doi.org/10.1038/ijo.2015.219.
Chowdhury TA, Lasker SS. Complications and cardiovascular risk factors in south Asians and Europeans with early-onset type 2 diabetes. QJM. 2002;95(4):241–6.
Basit A, Hydrie MZ, Hakeem R, Ahmedani MY, Masood Q. Frequency of chronic complications of type 2 diabetes. J Coll Physicians Surg Pak 2004;14(2):79–83. 02.2004/JCPSP.7983.
Eboh C, Chowdhury TA. Management of diabetic renal disease. Ann Transl Med. 2015;3(11):154.
Ahmedani MY, Hydrie MZ, Iqbal A, Gul A, Mirza WB, Basit A. Prevalence of microalbuminuria in type 2 diabetic patients in Karachi: Pakistan a multi-center study. Hypertension (n= 1226). 2005; 2194:99–7.
Ahsan S, Basit A, Ahmed KR, Ali L, Khanam R, Fawwad A, et al. Risk indicators of diabetic retinopathy in patients with type 2 diabetes screened by fundus photographs: a study from Pakistan. Int J Diabetes Dev Ctries. 2015;35(3):333–8. https://doi.org/10.1007/s13410-014-0277-9.
Hydrie MZ, Basit A. Prevalence of diabetic retinopathy. J Baqai Med Univ. 2002;5(2):6–11.
Ali A, Iqbal F, Taj A, Iqbal Z, Amin MJ, Iqbal QZ. Prevalence of microvascular complications in newly diagnosed patients with type 2 diabetes. Pakistan J Med Sci. 2013;29(4):899–902.
ATP III Guidelines At-A-Glance Quick Desk Reference. Available at: https://www.nhlbi.nih.gov/files/docs/guidelines/atglance.pdf (last assessed on March 15, 2018).
Let patients manage their own cholesterol. Available at: https://www.medscape.com/viewarticle/783728 (last assessed on 15 Mar 2018.
Santos AD, Cecílio HP, Teston EF, Arruda GO, Peternella FM, Marcon SS. Microvascular complications in type 2 diabetes and associated factors: a telephone survey of self-reported morbidity. Cien Saude Colet. 2015;20(3):761–70. https://doi.org/10.1590/1413-81232015203.12182014.
Pradeepa R, Anjana RM, Unnikrishnan R, Ganesan A, Mohan V, Rema M. Risk factors for microvascular complications of diabetes among South Indian subjects with type 2 diabetes—the Chennai Urban Rural Epidemiology Study (CURES) eye study-5. Diabetes Technol Ther. 2010;12(10):755–61. https://doi.org/10.1089/dia.2010.0069
Pradeepa R, Rema M, Vignesh J, Deepa M, Deepa R, Mohan V. Prevalence and risk factors for diabetic neuropathy in an urban south Indian population: the Chennai urban rural epidemiology study (CURES-55). Diabet Med. 2008;25(4):407–12. https://doi.org/10.1111/j.1464-5491.2008.02397.
Wani FA, Koul RK, Raina AA, Nazir A, Maqbool M, Bhat MH, et al. Prevalence of microvascular complications in newly diagnosed type-2 diabetes mellitus. Int J Sci Study. 2016;3(10):102–5. https://doi.org/10.17354/ijss/2016/21.
Kung K, Chow KM, Hui EM, Leung M, Leung SY, Szeto CC, et al. Prevalence of complications among Chinese diabetic patients in urban primary care clinics: a cross-sectional study. BMC Fam Pract. 2014;15(1):8. https://doi.org/10.1186/1471-2296-15-8
Jamil K, Iqbal Y, Zia S, Khan QA. Frequency of retinopathy in newly diagnosed patients of type 2 diabetes mellitus. Pakistan J Ophthalmol. 2014;30(1):38.
Sohail M. Prevalence of diabetic retinopathy among type–2 diabetes patients in Pakistan—vision registry. Pak J Ophthalmol. 2014;30(4):204–12.
Zoungas S, Woodward M, Li Q, Cooper ME, Hamet P, Harrap S, et al. Impact of age, age at diagnosis and duration of diabetes on the risk of macrovascular and microvascular complications and death in type 2 diabetes. Diabetologia. 2014;57(12):2465–74. https://doi.org/10.1007/s00125-014-3369-7.
Bansal D, Gudala K, Esam HP, Nayakallu R, Vyamusani RV, Bhansali A. Microvascular complications and their associated risk factors in newly diagnosed type 2 diabetes mellitus patients. Int J Chronic Dis. 2014;2014 https://doi.org/10.1155/2014/201423.
Haque HF, Afroz F, Afroze SR, Mitra P, Rahim MA, Ahmed AS, et al. Frequency and risk factors of diabetic complications among selected group of diabetic patients: real-life scenario from a developing country, Bangladesh. BIRDEM Med J. 2017;7(2):143–7.
Timar B, Timar R, Gaiță L, Oancea C, Levai C, Lungeanu D. The impact of diabetic neuropathy on balance and on the risk of falls in patients with type 2 diabetes mellitus: a cross-sectional study. PloS One. 2016;11(4):e0154654. from this region and from other parts of the world.
Vinik AI, Strotmeyer ES, Nakave AA, Patel CV. Diabetic neuropathy in older adults. Clin Geriatr Med. 2008;24(3):407–35. https://doi.org/10.1016/j.cger.2008.03.011.
Dirani M, Xie J, Fenwick E, Benarous R, Rees G, Wong TY, et al. Are obesity and anthropometry risk factors for diabetic retinopathy?: the diabetes management project. Invest Ophthalmol Vis Sci. 2011;52(7):4416–21. https://doi.org/10.1167/iovs.11-7208.
Hozumi J, Sumitani M, Matsubayashi Y, Abe H, Oshima Y, Chikuda H, et al. Pain Res Manag. 2016;2016 https://doi.org/10.1155/2016/2487924.
Themeli Y, Bajrami V, Barbullushi M, Idrizi A, Teferici D, Muka L, Ktona E. Diabetic nephropathy and risk factors associated with DM in newly diagnosed type 2 diabetics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval for the study was obtained from the institutional review board (IRB) of BIDE.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Abro, M., Zafar, A.B., Fawwad, A. et al. Prevalence of diabetic micro vascular complications at a tertiary care unit of Karachi, Pakistan. Int J Diabetes Dev Ctries 39, 325–330 (2019). https://doi.org/10.1007/s13410-018-0683-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-018-0683-5