Abstract
The incidence of delayed wound healing in patients with diabetes has increased in recent years. However, the reason of delayed diabetic wound healing and the changes of human adipose stem cells (hASCs) in the diabetic environment are still unclear. We simulated diabetic microenvironment with high glucose and glycation end products (AGEs) in vitro. CCK-8 and flow cytometry were used to study the proliferation and apoptosis of hASCs in the simulated diabetic microenvironment. The paracrine of hASCs was studied by transwell co-culture system. Protein chip was used to measure the expression of cytokines in hASCs. We found that high glucose and AGEs did not affect the proliferation of hASCs but arrested them in the S phase. More hASCs appeared early apoptosis in the simulated diabetic microenvironment. The promoting effect on the proliferation of fibroblasts and endothelial cells was weakened when hASCs were cultured in diabetic microenvironment for 6 days. The five cell factors, granulocyte colony-stimulating factor (G-CSF), transforming growth factor-α (TGF-α), hepatocyte growth factor (HGF), tissue inhibitor of metalloproteinases-1 (TIMP-1), and vascular endothelial growth factor (VEGF), were all downregulated in hASCs of AGEs and the high glucose group. In this study, we simulated diabetic microenvironment with high glucose and AGEs in vitro to evaluate the changes of proliferation, apoptosis, paracrine, and cytokine expression of hASCs in the diabetic environment and tried to find the possible reason of delayed diabetic wound healing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The advanced glycation end products (AGEs) are latter products of Maillard reaction or glycation and adversely affect the functional properties of proteins, lipids, and DNA [1]. In many clinical researches, AGEs in the diabetic skin are higher than normal tissue [2]. Also, positive correlations are found between the concentration of skin AGEs and age or incidence of foot ulcer [3]. A group of studies indicated that the AGEs inhibit the proliferation of endothelial cell [4], fibroblast [5], and nerve cell [6] and induce apoptosis. The former experiments indicated AGEs inhibit the proliferation and lead to human adipose stem cell (hASCs) apoptosis, decreasing the proliferation-promoting effect of hASCs on fibroblasts and endothelial cells. The formation of AGEs is closely related to the high concentration of tissue glucose, and AGEs accompany by high glucose can simulate a diabetic environment better. hASCs sited in skin follicles and subcutaneous fat may be important seed cells in wound repair [7]. The aim of our research was to study the changes of hASCs in the high glucose and AGE-simulated diabetic microenvironment, and refer another theoretical basis for diabetic wound healing and stem cell therapy.
Material and methods
Material
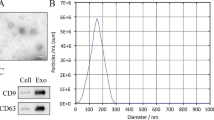
Human adipose-derived stem cells were provided by the stem cell technology platform of Shanghai Biochemistry and Cell Biology Institute (commercial cell line, cell No.: SCSP-404). The hASCs are derived from adipose tissue of an adult female donor and are negative for CD14, CD31, CD34, and CD45 and positive for CD29, CD44, CD73, CD90, CD105, and CD166.
Human fibroblasts were provided by Dr. Ying-kai Liu of Shanghai Burn Institute of Rui Jin Hospital.
Human umbilical vein endothelial cells were provided by ATCC (strain, PCS-100-010).
Methods
Preparing and grouping of hASCs
The hASCs were cultured in a mesenchymal stem cell growth medium (serum and antibiotics free, ready-to-use, PromoCell, Heidelberg, Germany) and were detached by a low serum detach kit (0.04% trypsin, PromoCell, Heidelberg, Germany). The primary hASCs were passed to passage 7 (P7) before experiment. The primary, passage 7 and passage 10 (P10) hASCs was photographed under a microscope (200×).
Three groups were designed as follows: hASCs cultured in a medium contained 100 mg/L AGEs (AGE full length protein, Abcam, Cambridge, MA, USA) and 28 mmol/L high glucose as an experimental group (AG group), 100 mg/L BSA and 28 mmol/L mannitol as a control group (BM group) [8], and normal hASCs without any addition in the medium as a blank group (BK group).
Culturing the hASCs in simulated diabetic microenvironment
The hASCs were cultured in the mesenchymal stem cell growth medium with 100 mg/L AGEs and 28 mmol/L high glucose. The medium was changed every 48 h and remove the non-adherent cells. The hASCs cultured 2, 4, and 6 days were collected to be used in the following experiments. Three groups of hASCs were photographed after 6 days culture.
Proliferation and apoptosis of hASCs
The CCK-8 assay (Dojindo Laboratories, Tokyo, Japan) was applied to study the proliferation of hASCs cultured 2, 4, and 6 days. The CCK-8 test sample was measured three times, and the average OD value was taken as the final data. Ten repeat samples were collected from each group.
On day 2, day 4, and day 6, hASCs were stained by AnnexinV/PI (BD Pharmingen™, San Jose, CA, USA) to detect the percentage of early, late, and total apoptotic hASCs in each group by flow cytometry. Four repeat samples were collected from each group.
Cell cycle detection of hASCs
The hASCs cultured in simulated diabetic microenvironment for 6 days were fixed with 75% ethanol 30 min. The fixed hASCs were stained with PI/RNase staining buffer (BD Pharmingen™, San Jose, CA, USA) and detected by flow cytometry. Three repeat samples were collected in each group; the experiment was repeated three times.
Co-culture of hASCs with human fibroblasts and endothelial cells
Human fibroblasts (1 × 104) were seeded into the upper compartments of 24-well transwell inserts (Membrane pore size 0.4um, Corning, USA). 1 × 105, 0.5 × 105, and 0.25 × 105 hASCs suspended in a 500-μl stem cell growth medium were seeded into the lower compartments. Culture media was added into the lower compartment as the control group.
Endothelial cells (1 × 104) were seeded into the upper compartments. 1 × 105 hASCs in the 500-μl stem cell growth medium were seeded into the lower compartments. Culture media was added into the lower compartment as the control group.
Human fibroblasts (1 × 104) and endothelial cells (1 × 104) were seeded into the lower compartments. The upper compartments were seeded by 1 × 104 hASCs. The same volume of culture media was added into the lower compartment as the control group.
Human fibroblasts (1 × 104) and endothelial cells (1 × 104) were seeded into the upper compartments. 1 × 105 hASCs cultured in AGEs and high glucose for 6 days were seeded into the lower compartments (AG co-culture group). 1 × 105 hASCs cultured in BSA and mannitol for 6 days were seeded into the lower compartments as the control group (BM co-culture group). 1 × 105 hASCs were seeded into the lower compartments (BK co-culture group). Culture media were added into the lower compartment as the blank group (BK group).
All the co-culture systems (the upper and lower compartments) lasted for 4 days and we changed the medium on the second day. Then the cell proliferation of upper compartments was detected by CCK-8. Each co-culture system had 12 repeat samples.
Cytokine expression of hASCs in simulated diabetic microenvironment
Total cell proteins from 0, 2, 4, and 6 days intervened hASCs were extracted and the expressions were measured by using QAH-ANG-1000-2 protein chip (RayBiotech, Norcross, GA, USA). Data of five interested cytokines were statistically analyzed. Each group on each time point had four repeat samples.
Data analysis
The cytokine data in the best confidence interval was chosen to be statistically analyzed. All data was identified by the normal distribution test (W test) and homogeneity test of variance (F test) with SPSS19.0. The data of each group were compared by t test using SPSS19.0. p value <0.05 indicates statistically significant difference.
Result
Cell culture and morphology of hASCs
Primary hASCs showed spindle, fusiform shape, 2–3 pseudopodia, large and oval nucleus and one to three nucleoli. The hASCs attached the culture dish firmly and distribution patterns were swirling or radial (Fig. 1a Primary). The shape and structure of P7 cells were not different from primary cells (Fig. 1a P7). P10 hASC volume increased, and the body became long and narrow with more pseudopodia. Some cells had intracellular clusters of vacuoles, transparent nuclei, and nucleolus pyknosis which were like “fried egg.” Cell growth became slow and the number of floating cells increased (Fig. 1a P10).
The morphology and proliferation of hASCs in simulated diabetic microenvironment. The P10 hASCs contained more “fried egg” like cells than primary hASCs (arrow) (a P10) (200×). The hASCs in AG group could be found a few “fried egg” like cells on day 6 (arrow) (a AG6d) (200×).The differences of hASC proliferation between AG group and BM group (b) BM group and BK group (c). *p < 0.05, **p < 0.01
The morphology of hASCs in simulated diabetic microenvironment
The AG group hASCs proliferated rapidly, reaching the peak in 2–4 days; cell count did not significantly increase in 4–6 days, and some cells became larger. The “fried egg”-like cells were more than the BM group and BK group (Fig. 1a).
The proliferation of hASCs cultured in simulated diabetic microenvironment
The OD values of three groups on days 2, 4, and 6 measured by CCK-8 are compared. The AG group is not different with the BM group on day 2 and day 6, but higher than the BM group on day 4. There were no significant differences between the BM group and BK group (Fig. 1b).
The apoptosis of hASCs cultured in simulated diabetic microenvironment
The difference of apoptosis between the AG group and BM group was not significant on day 2 and day 4. The early apoptosis (AnnexinV+/PI-) and total apoptosis (early + late) of the AG group was higher than those of the BM group on day 6. The late apoptosis (AnnexinV+/PI+) of the AG and BM groups had no significant difference on day 6. The apoptosis of the BM and BK groups showed no significant difference (Fig. 2).
Cell cycle of hASCs in simulated diabetic microenvironment
The percentage of the G1 phase between the AG group and BM group showed no significant difference on day 6. The S phase percentage of the AG group was higher than that of the BM group, but the G2 phase percentage was lower than the BM group on day 6. The S/G2 value of the AG group was also higher than the BM group on day 6. The results of the BM and BK groups showed no significant difference (Fig. 3b).
The paracrine of hASCs in simulated diabetic microenvironment
The number of fibroblast in the 1 × 105 hASC co-culture group was significantly higher than that in the control group after 4 days (Fig. 4a). The number of fibroblast cultured with 0.5 × 105 or 0.25 × 105 hASCs was not significantly higher than that in the control group (Fig. 4b, c). The number of fibroblast in the 1 × 105 hASC group was significantly higher than that in the 0.5 × 105 hASC group and 0.25 × 105 hASC group. The number of endothelial cells co-cultured with 1 × 105 hASCs was significantly higher than that in the control group (Fig. 4d).
The results of transwell co-culture system. The proliferation of fibroblasts co-culture with 1 × 105(a), 0.5 × 105(b), and 0.25 × 105(c) hASCs seeded in the lower compartments and with 1 × 105 hASCs of AG group in the lower compartments (g, h). The proliferation of endothelial cells co-culture with 1 × 105 hASCs seeded in the lower compartments (d) and with 1 × 105 hASCs of AG group in the lower compartments (i, j). The proliferation of hASCs co-culture with 1 × 105 \fibroblasts seeded in the lower compartments (e) and with 1 × 105 endothelial cells of the AG group in the lower compartments (f)
There were no significant differences between the number of hASCs in the upper compartments co-cultured with fibroblasts or endothelial cells and the number of hASCs in the control group (Fig. 4e, f).
The number of fibroblasts in the AG co-culture group was significantly lower than that in the BM co-culture group (Fig. 4g) but was still higher than that in the BK group (Fig. 4h).
The number of endothelial cells in the AG co-culture group was not different with that in the BM co-culture group (Fig. 4i). The endothelial cells in the AG co-culture group were no more than the BK group (Fig. 4j).
The number of endothelial cells and fibroblasts in BM co-culture group were not different with those in the BK co-culture group.
The protein expression of hASCs in simulated diabetic microenvironment
The expression of five interested cytokine, hepatocyte growth factor (HGF), granulocyte colony-stimulating factor (G-CSF), transforming growth factor-α (TGF-α), tissue inhibitor of metalloproteinases-1 (TIMP-1), and vascular endothelial growth factor (VEGF), were measured in the AG, BM, and BK groups on day 2, day 4, and day 6.
In simulated diabetic microenvironment, HGF was downregulated on day 2, day 4, and day 6 (p < 0.01). The expressions of G-CSF, TGF-α, and TIMP-1 in the AG group were not different from the BM group on day 2 and day 4. On day 6, the expressions of the three factors were downregulated (p < 0.05). VEGF expression was not different between the AG group and BM group on day 2, while the expression was downregulated on day 4 (p < 0.05) and day 6 (p < 0.01) (Fig. 5).
Discussion
The primary hASCs will grow old with time, morphology of P10 hASCs has changed, and the “fried egg”-like cells may no longer have stem cell properties [9]. P7 hASCs were chosen for experiments because they had enough number, morphology as primary cells, stable proliferation rate, and low apoptosis. The BK group was used to verify whether the BSA and mannitol environment has effect on hASCs.
The AGEs in our study were produced by the Maillard reaction of BSA and glucose which was similar to in vivo [10]. The combination of AGEs and high glucose in the culture medium can simulate the micro environment of diabetic tissues better than adding AGEs or high glucose only. The 28 mmol/L glucose can simulate the hyperglycemia of a diabetic patient [11]; while not reaching the blood glucose of ketoacidosis (33 mmol/L), 100 mg/L AGEs was chosen as former research [12].
The growth of hASCs in high glucose and AGEs was not inhibited; the simulated diabetic microenvironment might even promote the growth of hASCs on day 4. Many former researchers found that only high glucose would promoted the growth of hASCs [13, 14]. In our study, the promoting effect was not continuous for the number of hASCs in the AG group on day 6 and was no more than the BM group. In the cell cycle experiment, more hASCs in simulated diabetic environment were blocked in the S phase and unable to complete cell division. This may explain the low proliferation of hASCs on day 6.
The percentage of early apoptotic hASCs increased in in vitro diabetic environment. Those early apoptotic hASCs could not complete differentiation and might not participate in wound healing. These results happened on hASCs just had been cultured in simulated diabetic environment for 6 days. The hASCs of diabetic patients may stay in the high glucose and AGE environment for several months or even years. It may lead to more severe cell cycle arrest and apoptosis [15, 16], may reduce the wound healing ability of hASCs, and may finally cause the delayed wound healing. AGEs and high glucose may also affect hASCs (local or transplanted) in the diabetic wound and weaken the efficacy of stem cell therapy.
The hASCs might promote the proliferation of fibroblasts and endothelial cells by paracrine [17]. The promoting effect of hASCs was positively correlated with cell number. In diabetic patients, apoptosis induced by AGEs in the diabetic microenvironment may decrease the number of hASCs and may weaken the paracrine promoting effect of hASCs on proliferation of fibroblasts and endothelial cells.
The HGF can upregulate the expression of VEGF and TIMP-1 by activating a tyrosine kinase signaling cascade after binding to the proto-oncogenic c-Met receptor [18]. HGF plays a central role in angiogenesis and tissue regeneration. VEGF promotes the proliferation of vascular endothelial cells and angiogenesis [19]. The expression of HGF in hASCs of AG group was decreased, which may weaken the promoting effect of hASCs on the proliferation of endothelial cells. VEGF in hASCs was decreased on day 4 and day 6 after HGF which may further weaken the angiogenic promoting effect of hASCs and reduce the proliferative activity of endothelial cells.
The G-CSF can promote endothelialization of injured vascular. It may reduce expression of pro-inflammatory cytokines and enhance neurogenesis [20]. The low expression of G-CSF in the AG group may lead to decreased proliferation of endothelial cells and delayed repair of vascular injury.
The TGF-α is a member of the epidermal growth factor (EGF) family, which activates cell proliferation and differentiation. TGF-α is also believed to promote angiogenesis and protect endothelial cell from apoptosis [21]. The TGF-α was downregulated in the AG group, which may decrease epithelial regeneration and may affect diabetic wound healing.
The TIMP-1 promotes cell migration and proliferation and is involved in degradation and remodeling of the wound matrix. Bullen et al. [22] found TIMP-1 levels were lower in chronic than in healing wounds. Imbalance of TIMPs and MMPs is a necessary factor for chronic wound formation [23]. TIMP-1 in AG group was decreased, which may accelerate the wound tissue degradation and aggravate the spread of inflammatory factors. The downregulation of growth factors such as G-CSF and TGF-α will reduce the proliferation of wound healing cells [24]. Fewer mesenchymal cells will lead to the decrease of HGF expression and further decrease the expression of VEGF and TIMP-1. A vicious cycle of wound healing factors was formed, and it may explain the causes of delayed diabetic wound healing.
Conclusions
High glucose and AGEs do not inhibit the proliferation but arrest the hASCs in the S phase. High glucose and AGEs lead to hASC apoptosis, decreasing the paracrine-promoting effect of hASCs on proliferation of fibroblasts and endothelial cells. The decrease of growth factors HGF, G-CSF, and TGF-α in hASCs may influence the proliferation of endothelial and epithelial cells. All the changes may lead to delayed diabetic wound repair and regeneration. The results of this study suggest that decreasing glucose and AGEs in the microenvironment of hASCs or increasing the expression of HGF and TGF in hASCs may be a new therapeutic option in clinical to speed up diabetic wound healing. This study is not without limitations. We did not carry out these experiments on cells obtained from diabetic patients. More experiments are needed to study the changes of diabetic hASCs in the simulated diabetic microenvironment.
References
Vlassara H, Brownlee M, Cerami A. Accumulation of diabetic rat peripheral nerve myelin by macrophages increases with the presence of advanced glycosylation endproducts. J Exp Med. 1984;160(1):197–207.
Niu YW, Miao MY, Dong W, Dong JY, Cao XZ, Lu SL. Effects of advanced glycation end products and its receptor on oxidative stress in diabetic wounds [in Chinese]. Zhonghua Shao Shang Za Zhi. 2012;28(1):32–5.
Vouillarmet J, Maucort-Boulch D, Michon P, Thivolet C. Advanced glycation end products assessed by skin autofluorescence: a new marker of diabetic foot ulceration. Diabetes Technol Ther. 2013;15(7):601–5. doi:10.1089/dia.2013.0009.
Zhuang X, Pang X, Zhang W, Wu W, Zhao J, Yang H, et al. Effects of zinc and manganese on advanced glycation end products (AGEs) formation and AGEs-mediated endothelial cell dysfunction. Life Sci. 2012;90(3–4):131–9. doi:10.1016/j.lfs.2011.10.025.
Alikhani Z, Alikhani M, Boyd CM, Nagao K, Trackman PC, Graves DT. Advanced glycation end products enhance expression of pro-apoptotic genes and stimulate fibroblast apoptosis through cytoplasmic and mitochondrial pathways. J Biol Chem. 2005;280(13):12087–95. doi:10.1074/jbc.M406313200.
Chen B, Niu YW, Xie T, Miao MY, Tian M, Ji XY, et al. Relationship between cutaneous glycometabolic disorders and cutaneous neuropathy in diabetic rats [in Chinese]. Zhonghua Shao Shang Za Zhi. 2011;27(2):139–44.
Zuk PA, Zhu M, Mizuno H, Huang J, Futrell JW, Katz AJ, et al. Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng. 2001;7(2):211–28. doi:10.1089/107632701300062859.
Dong J, Takami Y, Tanaka H, Yamaguchi R, Jingping G, Chun Q, et al. Protective effects of a free radical scavenger, MCI-186, on high-glucose-induced dysfunction of human dermal microvascular endothelial cells. Wound Repair Regen. 2004;12(6):607–12. doi:10.1111/j.1067-1927.2004.12607.x.
Fu Q, Qin Z, Jin X, Zhang L, Chen Z, He J, et al. Generation of functional lentoid bodies from human induced pluripotent stem cells derived from urinary cells. Invest Ophthalmol Vis Sci. 2017;58(1):517–27. doi:10.1167/iovs.16-20504.
Xie T, Lu SL, Ge K, Niu YW, Wang MJ, Shu L, et al. Effects of arginine on cutaneous underlying disorder in diabetic rats [in Chinese]. Zhonghua Yi Xue Za Zhi. 2005;85(21):1501–3.
Oyama T, Miyasita Y, Watanabe H, Shirai K. The role of polyol pathway in high glucose-induced endothelial cell damages. Diabetes Res Clin Pract. 2006;73(3):227–34. doi:10.1016/j.diabres.2006.02.010.
Lin WD, Lu SL, Qing C, Yao M, Chen XF, Xiang J, et al. Proliferation-inhibiting effect of advanced glycation end products modified human serum albumin to vascular endothelial cell ECV304 [in Chinese]. Zhonghua Yi Xue Za Zhi. 2003;83(7):572–6.
Barale C, Dentelli P, Togliatto G, Trombetta A, Olgasi C, Scozzari G, et al. High glucose via NOX-dependent ROS generation and AKT activity promotes adipose-derived stem cell de-differentiation. Stem Cells Dev. 2012; doi:10.1089/scd.2011.0699.
Kim YH, Han HJ. High-glucose-induced prostaglandin E(2) and peroxisome proliferator-activated receptor delta promote mouse embryonic stem cell proliferation. Stem Cells. 2008;26(3):745–55. doi:10.1634/stemcells.2007-0786.
Acosta L, Hmadcha A, Escacena N, Perez-Camacho I, de la Cuesta A, Ruiz-Salmeron R, et al. Adipose mesenchymal stromal cells isolated from type 2 diabetic patients display reduced fibrinolytic activity. Diabetes. 2013;62(12):4266–9. doi:10.2337/db13-0896.
Piran M, Enderami SE, Piran M, Sedeh HS, Seyedjafari E, Ardeshirylajimi A. Insulin producing cells generation by overexpression of miR-375 in adipose-derived mesenchymal stem cells from diabetic patients. Biologicals. 2017;46:23–8. doi:10.1016/j.biologicals.2016.12.004.
Ong HT, Redmond SL, Marano RJ, Atlas MD, von Unge M, Aabel P, et al. Paracrine activity from adipose-derived stem cells on in vitro wound healing in human tympanic membrane keratinocytes. Stem Cells Dev. 2017;26(6):405–18. doi:10.1089/scd.2016.0204.
Yamauchi Y, Ueki S, Konno Y, Ito W, Takeda M, Nakamura Y, et al. The effect of hepatocyte growth factor on secretory functions in human eosinophils. Cytokine. 2016;88:45–50. doi:10.1016/j.cyto.2016.08.013.
Anderson JE. Hepatocyte growth factor and satellite cell activation. Adv Exp Med Biol. 2016;900:1–25. doi:10.1007/978-3-319-27511-6_1.
Wils J, Favre J, Bellien J. Modulating putative endothelial progenitor cells for the treatment of endothelial dysfunction and cardiovascular complications in diabetes. Pharmacol Ther. 2017;170:98–115. doi:10.1016/j.pharmthera.2016.10.014.
Ferrer I, Alcantara S, Ballabriga J, Olive M, Blanco R, Rivera R, et al. Transforming growth factor-alpha (TGF-alpha) and epidermal growth factor-receptor (EGF-R) immunoreactivity in normal and pathologic brain. Prog Neurobiol. 1996;49(2):99–123.
Bullen EC, Longaker MT, Updike DL, Benton R, Ladin D, Hou Z, et al. Tissue inhibitor of metalloproteinases-1 is decreased and activated gelatinases are increased in chronic wounds. J Invest Dermatol. 1995;104(2):236–40.
Ligi D, Mosti G, Croce L, Raffetto JD, Mannello F. Chronic venous disease—part II: Proteolytic biomarkers in wound healing. Biochim Biophys Acta. 2016;1862(10):1900–8. doi:10.1016/j.bbadis.2016.07.011.
Han P, Cui Q, Yang S, Wang H, Gao P, Li Z. Tumor necrosis factor-alpha and transforming growth factor-beta1 facilitate differentiation and proliferation of tendon-derived stem cells in vitro. Biotechnol Lett. 2017; doi:10.1007/s10529-017-2296-3.
Acknowledgements
The authors gratefully acknowledge Ying-kai Liu, Lei Yi, and Qing Pei for the technical assistance and Shu-wen Jin for the systematic guidance.
Author information
Authors and Affiliations
Contributions
Conceived and designed the study: JHG, SLL, JYD. Performed the experiments: JHG. Analyzed the data: JHG. Contributed reagents/materials/analysis tools: JHG, SLL, TX. Wrote the manuscript: JHG, SLL. Experiment skill advising: JYD, SLL. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Funding
This study was funded by the Chinese National Natural Science Foundation (81071566) and Key Project of Chinese National Programs for Fundamental Research and Development (973 program, 2012CB518105).
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Gong, JH., Dong, JY., Xie, T. et al. Influence of high glucose and AGE environment on the proliferation, apoptosis, paracrine effects, and cytokine expression of human adipose stem cells in vitro. Int J Diabetes Dev Ctries 38, 228–237 (2018). https://doi.org/10.1007/s13410-017-0574-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-017-0574-1