Abstract
This study aims to investigate the changing characteristics of glucose regulation after gastric surgery for normal gastric cancer patients with type 2 diabetes mellitus (T2DM) (T2DM group) and without T2DM (normal group) in a tertiary hospital located in western China. We conducted a case-control study which retrospectively collected the data of 73 patients: (1) diagnosed as gastric cancer, (2) underwent sub-gastrectomy and Billroth II gastrointestinal anastomosis between October 2007 and December 2012, and (3) did not suffer a recurrent cancer and with sufficient clinical data. Fasting blood glucose (FBG), glycated hemoglobin (HbA1c), insulin sensitive index (HOMA-IS), insulin resistance index (HOMA-IR), and beta cell function index (HOMA-BCF) were compared at baseline and postoperative 7, 14, 28, 56, 120, and 356 days. Baseline FBG, HbA1c, HOMA-IS, HOMA-IR, and HOMA-BCF in the T2DM group were significantly higher than those in the normal group. Immediate postoperative glucose changed significantly, and it became stable and normal during follow-up period in both the T2DM and normal group that there was no significance anymore after postoperative 28 days between them. Normal patients with T2DM would benefit from gastric surgery in glucose control, and it may involve not only decreased food intake and weight loss but also gastrointestinal reconstruction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
More than 221 million people around the world are suffering from type 2 diabetes mellitus (T2DM) [1], which has a really high threat to public health. The prevalence of diabetes in China is about 4.6 % of the whole population in western region and 8 % in eastern region, and the prevalence of diabetes was sharply increasing during past decades [2, 3]. Also, diabetes conveys a higher risk of gastric cancer mortality [4]. The continued medical care including moderate diet, intensified exercise, oral drugs, and insulin injection could hardly cure T2DM, especially obesity-related T2DM [5, 6].
Surgery has been applied regularly in obese patients with a body mass index (BMI) >40 kg/m2 or >35 kg/m2 when serious co-morbidities are associated with them [7]. It was reported that 85.4 % of 485 patients undergoing bariatric surgery experienced resolution or improvement in T2DM, and the follow-up results also revealed a significant weight loss and an effective controlment of the co-morbidities such as high blood pressure, insulin resistance, and dyslipidemia [8]. Meanwhile, a cohort study found that the patients who adopted bariatric surgery achieved a significant reduction of 40 % in the overall mortality, 56 % in specific mortality due to coronary heart disease [9]. Besides bariatric surgery, gastric surgery including sub-gastrectomy and Billroth II reconstruction was also demonstrated to have positive effects on T2DM improvement [10–12]. Due to unclear mechanisms responsible for the improvement in DM, the clinical outcome could not be clearly explained. It was certain that decreased food intake because of gastric restriction or intestinal malabsorption played an important role [13]. Meanwhile, some studies mentioned that postoperative weight loss may be another important factor as it can to some extent reduce insulin resistance; however, T2DM resolution achieved by surgery happens mostly in 2–3 weeks when a high proportion of cases still did not acquire a significant weight loss yet.
Recently, more and more evidence revealed that for patients with normal or lower BMI, who would not acquire a significant weight loss compared with obese patients, surgery also achieved a significant improvement in T2DM remission. It was supposed that weight loss may not be important as considered for both normal and low-weight patients. As glucose regulation which mainly includes insulin release and sensitive was systematically impaired in T2DM, in order to investigate the changing characteristic of glucose regulation after gastric surgery, we performed this retrospective study to compare the relevant index before and after operation in T2DM patients with normal BMI patients.
Methods
Patients
We retrospectively included patients with normal BMI who had curative intent for primary gastric cancers (TNM stage, T1-2 N1-2 M0) in our hospital between October 2007 and December 2012 and finally underwent sub-gastrectomy and Billroth II gastrointestinal anastomosis, and the postoperative survival time was more than 1 year in the study. Patients with (1) severe plasma insulin deficiency, (2) autoimmune antibody positive, (3) unresectable stomach carcinoma, (4) age >70 years, and (5) heart, lung, or kidney failure were excluded. Also, patient with insufficient follow-up data and/or a recurrence were also excluded. A total of 79 cases underwent gastric surgery, in which 73 patients were included and 6 of them were excluded (4 of them was lost to follow-up, and 2 of them suffered a recurrent gastric cancer). A fasting blood glucose (FBG) reduction of at least 1.5 mmol/L with a maximum standard deviation of 3 mmol/L when α = 0.05 and β = 0.8 is performed. According to the T2DM history and check result in admission, there were 33 patients in the T2DM group and 40 patients in the normal group. The study was approved by Lanzhou University Second Hospital ethics committee. All patients provided written informed consort of potential risks before operation and made verbal agreement of collecting their information for scientific study.
Surgery procedures
Gastric surgery was mainly recommended by a doctor according to pathology and imaging data and determined by the patients. Four experienced surgeons participated in this study, and each of them had performed more than 50 cases of sub-gastrectomy and Billroth II reconstruction. In all cases, distal subtotal gastric resection is indicated to the tumor located in the lower one third of the stomach. The standard lymphadenectomy (LAD) is the D2-LAD without distal pancreatectomy or splenectomy. The extended organ resection is only indicated in cases where R0 resection is possible. In China, the main goal of surgical intervention is the complete removal of the tumor. An indication for performing subtotal gastrectomy is based on tumor location, histological type, and trial for achieving surgical tumor-free margins.
The reconstruction of the digestive tract is performed by adopting Billroth II reconstruction after subtotal gastrectomy. For Billroth II reconstruction, 8–10 cm midline incision is made 2–3 cm below the xiphoid process, and wound is protected with wound protector. Then, the stomach is resected with adequate margins proximal to the tumor using tube-type staplers. An end-to-side anatomist is undertaken after the small bowel, and 15–20 cm distal to the Treitz ligament has been pulled up antecolically. The anastomosis is performed by hand sewing or by using staplers. Stapler inlet site is hand-sewn or closed with double clipping of staplers.
Data collection
Basic information of the patients including age, sex, BMI, pre- and postoperative treatment approaches to diabetes, preoperative fasting plasma glucose, glycated hemoglobin, and fasting plasma insulin were recorded. During the time of operation completion to discharge, fasting plasma glucose and fasting plasma insulin were measured twice. Sensitivity index of insulin (SEN) was calculated as: SEN = ‐ In(FBG × FINS) [14]. Homeostasis model assessment-insulin resistance (HOMA-IR) index and homeostasis model assessment-derived beta cell function (HOMA-B) index [15] were calculated as follows: HOMA ‐ IR = FIRI × FBG/22.5, HOMA ‐ B = 20 × FIRI/(FBG ‐ 3.5), where FIRI represents fasting plasma insulin level (μU/mL) and FBG represents fasting blood glucose level (mmol/L).
Follow-up
A follow-up at postoperative 28, 56, 120, and 356 days were then performed, and the data were collected according to the most recent blood check results through outpatient service. To ensure the comparability between the T2DM and control group, radiographical check was also conducted at postoperative 3, 6, and 12 months.
Statistical analysis
Data were collected and represented as mean ± standard deviation for continuous variables and number of patients (percentage) for dichotomous variables. Levene’s test was adopted for equality of variances, and then, the difference of continuous variables between groups was analyzed by Student t test. Also, the difference of dichotomous variables between groups was analyzed by χ 2 test or Fisher exact test. Both are considered with statistical significance when p < 0.05. For statistical analysis, the SPSS for Windows 17.0 (SPSS, Chicago, IL, USA) was used.
Results
A total of 73 gastric cancer patients were analyzed in the study, 33 cases in the T2DM group and 40 cases in the normal group. There were 41 males and 32 females, and the average age was 65.48 years (range, 45–69). There were no significant differences between the two groups in terms of age, sex, BMI, TNM stage, weight loss, and fast plasma insulin level (FPI). In the T2DM group, the level of FBG, the level of glycated hemoglobin (HbA1c), and homeostasis model assessment-insulin resistance (HOMA-IR) were significantly higher than those in the normal group (p < 0.01), while homeostasis model assessment-insulin sensitivity (HOMA-IS) and homeostasis model assessment-derived beta cell function (HOMA-BCF) were significantly lower than those in the normal group. All the patients in the T2DM group have diabetes with a medical history ranged from 3 months to 13 years and received medical treatment including oral drugs and/or insulin injection and after operation had a response rate of 76.5 % (26/33) at postoperative 14 days and 93.9 % (31/33) at postoperative 28 days, as presented in Table 1.
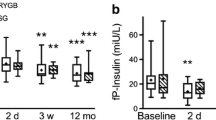
Fasting blood glucose
The FBG level in T2DM was significantly higher than that in the normal group at baseline (9.74 ± 2.13 vs. 6.63 ± 0.85, t = 7.38, p < 0.01), while this trend changed until postoperative 28 days (6.05 ± 0.96 vs. 5.41 ± 0.68, t = −0.46, p = 0.65). From the 4th week to the 12th month postoperatively, there was no significant difference between the groups (Fig. 1).
Glycated hemoglobin
The HbA1c level in the T2DM group was higher than that in the normal group at baseline (7.36 ± 1.11 vs. 5.75 ± 0.45, t = 7.16, p < 0.01). It decreased after operation, and 28 days later, the level tended to be stable with non-significant difference between the groups (5.53 ± 1.32 vs. 5.12 ± 1.03, t = 1.49, p = 0.14) (Fig. 2).
Homeostasis model assessment-insulin resistance
The Home-IR was higher in the T2DM group than that in the normal group at baseline (1.31 ± 0.22 vs. 0.95 ± 0.10, t = 8.73, p < 0.01), and it gradually decreased until postoperative 28 days when the difference between the groups was not statistically significant (0.78 ± 0.11 vs. 0.73 ± 0.10, t = 1.93, p = 0.06) (Fig. 3).
Homeostasis model assessment-insulin sensitivity
At baseline, the Home-IS in the T2DM group was lower (0.30 ± 0.01 vs. 0.36 ± 0.02, t = −10.73, p < 0.01). After surgery, it was not significantly influenced, while it persistently increased in the normal group. From postoperative 28 days, there was no significant difference between the groups (0.35 ± 0.02 vs. 0.36 ± 0.02, t = −1.84, p = 0.07) (Fig. 4).
Homeostasis model assessment-derived beta cell function
The Home-BCF was obviously changed in both groups, and no stable or routine trends were found. At baseline, it was lower in the T2DM group than that in the normal group (12.03 ± 4.47 vs. 23.17 ± 10.48, t = −6.09, p < 0.01); then it increased and there was no significant difference between the groups at postoperative 28 days (42.02 ± 19.29 vs. 37.23 ± 18.49, t = 1.08, p = 0.28) (Fig. 5).
Complications
Gastric surgery was a safe procedure for gastric cancer patients, and there was no significant difference between the groups in aspects of complication incidence. There were four patients in the T2DM group and three patients in the normal group who had delayed healing (3/34 vs. 4/40, p = 0.81), and five patients in the T2DM group and six patients in the normal group had postoperative wound bleeding (5/34 vs. 6/40, p = 0.97). Besides, long-term radiographical follow-up result showed that there was no evidence and incidence of recurrence and metastasis in primary gastric cancer.
Discussion
There is a strong relationship between obesity and T2DM, and approximately half of those patients diagnosed with T2DM are obese [3]. Surgical procedures were demonstrated to be able to provide durable weight loss in obese people effectively [16]. Also, it was reported that reducing body weight through operations involving intestinal diversions improved glucose homeostasis in obesity-related T2DM. Meanwhile, few studies are currently available on how certain surgery influences the glucose regulation in non-obese T2DM patients.
Our hospital is located in a western province of China, which is one of the highest incidence areas of gastric cancer. Due to the specific area and the disease, all the patients in this study were not obesity-related T2DM, with normal BMI 18.5 to 24.99 kg/m2. Except for FPI, FPG, HbA1c, home-IS, home-IR, and home-BCF were all significantly differentiated between T2DM group and normal group at baseline. After surgery, all the indexes began to change and eventually achieved responses that there was no significant difference in T2DM compared with normal patients at postoperative 28 days. And all the patients in the T2DM group took insulin and oral drugs before surgery, while only 6.1 % of them need continued medical treatment at postoperative 28 days to maintain an adaptable glucose level. Therefore, the results suggested that glucose status was significantly improved in non-obesity-related T2DM group after gastric surgery.
Some studies found that T2DM was typically resolved within a few days to weeks following malabsorptive procedures before significant weight loss was achieved [17]. Compared with obese patients, current patients in this study with normal BMI lost less weight in the follow-up period (approximately 1/5 vs. 1/3) [18, 19]. Although patients in the T2DM group achieved significant response and diabetes remission in the follow-up periods, the study showed that no significant difference existed between the groups in terms of weight loss. Thus, surgery-induced weight loss may also to some extent influence glucose, but does not play important roles in controlling the glucose level in normal-BMI patients who underwent gastric surgery.
Nowadays, bariatric surgery was performed in many different procedures, which mainly included conventional surgical procedures (e.g., roux-en-y gastric bypass, laparoscopic adjustable gastric band, sleeve gastrectomy, and biliopancreatic diversion) and novel surgical procedures (duodenal-jejunal bypass and ileal interposition) [20]. In this study, because the patients were also diagnosed as gastric cancer, we failed to performed bariatric surgery in any of them. As the procedure of Billroth II surgery was similar to biliopancreatic diversion, compared with Mingrone et al. [21], patients undergoing biliopancreatic diversion achieved better, fast plasma glucose and glycated hemoglobin control at postoperative 1 month. Despite that the food did not pass through the duodenum anymore in both studies, compared with biliopancreatic diversion, Billroth II surgery had different lengths of proximal bowel loop and distal bowel loop and different cavities of remnant stomach. So, it was indicated that the mechanism of different surgical procedures may be the same that both remnant stomach and bowel loop contributed to the bariatric remission. Restrictive and malabsorptive procedures involving rerouting of food and vacant intestine might improve T2DM by enhancing insulin sensitivity and/or by improving beta cell function [22, 23].
And obviously, it was different from operation completion to postoperative 28 days of the changing trend of relevant index in the T2DM group and normal group. Except for diabetes diagnosis, the two groups had completely the same interventions. Gastric surgery as one of the most invasive gastric procedure put an enormous burden on physical condition. And it led to wasting condition, and glucose metabolism was changed and complicated. With limitation of food intake, there were many kinds of potential factors to influence glucose regulation and relevant indexes. When discharged from the hospital, patients began to adopt usual activities, diets, and life, and only gastrointestinal reconstruction was still existed. Compared with the normal group, patients in T2DM group had a similar trend but showed a slower speed and lower ability to go back to the baseline and relative high glucose level. Thus, it may be supposed that weakened absorption function as well as improved insulin sensitivity [24, 25]. In our study, home model index was improved much more quickly than the level of plasma glucose and glycated hemoglobin.
Otherwise, in this study, no mortality was observed. Major and minor surgery-related complication rate was also low. For the treatment of T2DM, prevention of diabetes-related complications such as macro- and microvascular diseases are as important as glycemic control. To prevent these diabetes-related complications, blood pressure needs to be controlled below 130/80 mmHg, cholesterol level below 200 mg/dL, and HbA1C level below 7 % [26, 27]. Unfortunately, only 7.3 % of adults with diabetes achieved all three recommended goals with conventional medical treatment [28, 29]. In contrast, most of the patients could control cholesterol levels below 200 mg/dL and HbA1C levels below 7 %.
Conclusions
Immediate postoperative glucose changed significantly, and it became stable and normal during follow-up period in both the T2DM and normal groups. Patients with non-obese T2DM benefited from gastric surgery in glucose controlment may involve decreased food intake, weight loss, and gastrointestinal reconstruction.
References
Adeghate E, Schattner P, Dunn E. An update on the etiology and epidemiology of diabetes mellitus. Ann N Y Acad Sci. 2006;1084:1–29.
Zuo H, Shi Z, Hussain A. Prevalence, trends and risk factors for the diabetes epidemic in china: a systematic review and meta-analysis. Diabetes Res Clin Pract. 2014;104(1):63–72.
Du T, Sun X, Huo R, et al. Visceral adiposity index, hypertriglyceridemic waist and risk of diabetes: the china health and nutrition survey 2009. Int J Obes. 2014;38(6):840–7.
Tseng CH. Diabetes conveys a higher risk of gastric cancer mortality despite an age-standardised decreasing trend in the general population in Taiwan. Gut. 2011;60:774e779.
Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes, 2015: a patient-centered approach: update to a position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care. 2015;38(1):140–9.
Musella M, Milone M, Bellini M, Sosa Fernandez L, Leongito M, et al. Effect of bariatric surgery on obesity-related infertility. Surg Obes Relat Dis. 2012;8:445–9.
Klein S, Ghosh A, Cremieux PY, et al. Economic impact of the clinical benefits of bariatric surgery in diabetes patients with BMI≥ 35 kg/m2. Obesity. 2011;19(3):581–7.
Lifshitz F, Hall J. Reduction in the incidence of type II diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403.
Heymsfield S, Segal K, Hauptman J, Lucas C, Boldrin M, et al. Effects of weight loss with orlistat on glucose tolerance and progression to type 2 diabetes in obese adults. Arch Intern Med. 2000;160:1321–6.
Picot J, Jones J, Colquitt J, Gospodarevskaya E, Loveman E, et al. The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation. Health Technol Assess. 2009;13:1–190.
Zhu Z, Shan X, Cheng Y, et al. Clinical course of diabetes after gastrectomy according to type of reconstruction in patients with concurrent gastric cancer and type 2 diabetes. Obes Surg. 2015;25(4):673–9.
Liu T, Xie G, Tian Q, et al (2015) Radical gastrectomy combined with modified gastric bypass surgery for gastric cancer patients with type 2 diabetes. Cell Biochem Biophys: 1–6
Zimmet P, Shaw J, Alberti K. Preventing type 2 diabetes and the dysmetabolic syndrome in the real world: a realistic view. Diabet Med. 2003;20:693–702.
Emoto M, Nishizawa Y, Maekawa K, Hiura Y, Kanda H, et al. Homeostasis model assessment as a clinical index of insulin resistance in type 2 diabetic patients treated with sulfonylureas. Diabetes Care. 1999;22:818–22.
Levy J, Matthews D, Hermans M. Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care. 1998;21:2191–2.
O’Brien PE, McPhail T, Chaston TB, Dixon JB. Systematic review of medium-term weight loss after bariatric operations. Obes Surg. 2006;16:1032–40.
Schauer PR, Burguera B, Ikramuddin S, Cottam D, Gourash W, et al. Effect of laparoscopic roux-en Y gastric bypass on type 2 diabetes mellitus. Ann Surg. 2003;238:467.
Li Q, Chen L, Yang Z, Huang Y, He M, et al. Metabolic effects of bariatric surgery in type 2 diabetic patients with body mass index < 35 kg/m2. Diabetes Obes Metab. 2012;14:262–70.
Shimizu H, Timratana P, Schauer P, Rogula T. Review of metabolic surgery for type 2 diabetes in patients with a BMI <35 Kg/M 2. J Obes. 2012;2012:147256.
Dixon J, le Roux C, Rubino F, Zimmet P. Bariatric surgery for type 2 diabetes. Lancet. 2012;379:2300–11.
Mingrone S, Panunzi A, Mingrone G, Panunzi S, de Gaetano A, Guidone C, et al. Bariatric surgery versus conventional medical therapy for type 2 diabetes. N Engl J Med. 2012;366:1577–85.
Camastra S, Manco M, Mari A, Greco A, Frascerra S, et al. β-cell function in severely obese type 2 diabetic patients long-term effects of bariatric surgery. Diabetes Care. 2007;30:1002–4.
Rao RS, Kini S. GIP and bariatric surgery. Obes Surg. 2011;21:244–52.
Rubino F, Schauer P, Kaplan L, Cummings D. Metabolic surgery to treat type 2 diabetes: clinical outcomes and mechanisms of action. Annu Rev Med. 2010;61:393–411.
Buchwald H, Avidor Y, Braunwald E, Jensen M, Pories W, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–37.
Ali M, Bullard K, Saaddine J, Cowie C, Imperatore G, et al. Achievement of goals in US diabetes care, 1999–2010. N Engl J Med. 2013;368:1613–24.
Bakris G. Clinical guidelines: blood pressure goals in T2DM: a Latin American perspective. Nat Rev Endocrinol. 2013;9:138–9.
Massi-Benedetti M. Changing targets in the treatment of type 2 diabetes. Curr Med Res Opin. 2006;22:S5–S13.
Guo X, Liu X, Wang M, Wei F, Zhang Y, et al. The effects of bariatric procedures versus medical therapy for obese patients with type 2 diabetes: meta-analysis of randomized controlled trials. BioMed Res Int. 2013;2013:410609.
Compliance with ethical standards
Funding
This study was funded by Gansu Provincial Health Department of Research Projects (grant number WST07-07).
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Authors’ contributions
Zhang YC, Wang HL, Zhang YW, and Xu XD were involved in the study conception and design. Wei FX, Han W, and Zhang HH participated in the acquisition of data. Wei ZG, Zhang YW, Wang MC, and Xu XD were involved in the analysis and interpretation of data. Wei FX and Han W participated in the drafting of manuscript. Zhang YC and Wang HL were involved in the critical revision of manuscript.
Conflict of interest
You Cheng Zhang, Feng Xian Wei, Wei Han, Hui Lin Wang, Man Cai Wang, Ya Wu Zhang, Xiao Dong Xu, and Hui Han Zhang declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, Y.C., Wei, F.X., Han, W. et al. Impact of sub-gastrectomy on glucose regulation in gastric cancer patients with T2DM: a follow-up study. Int J Diabetes Dev Ctries 36, 89–94 (2016). https://doi.org/10.1007/s13410-015-0437-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13410-015-0437-6